Alcohol induced mood disorder symptoms
Substance Induced Mood Disorders - StatPearls
Continuing Education Activity
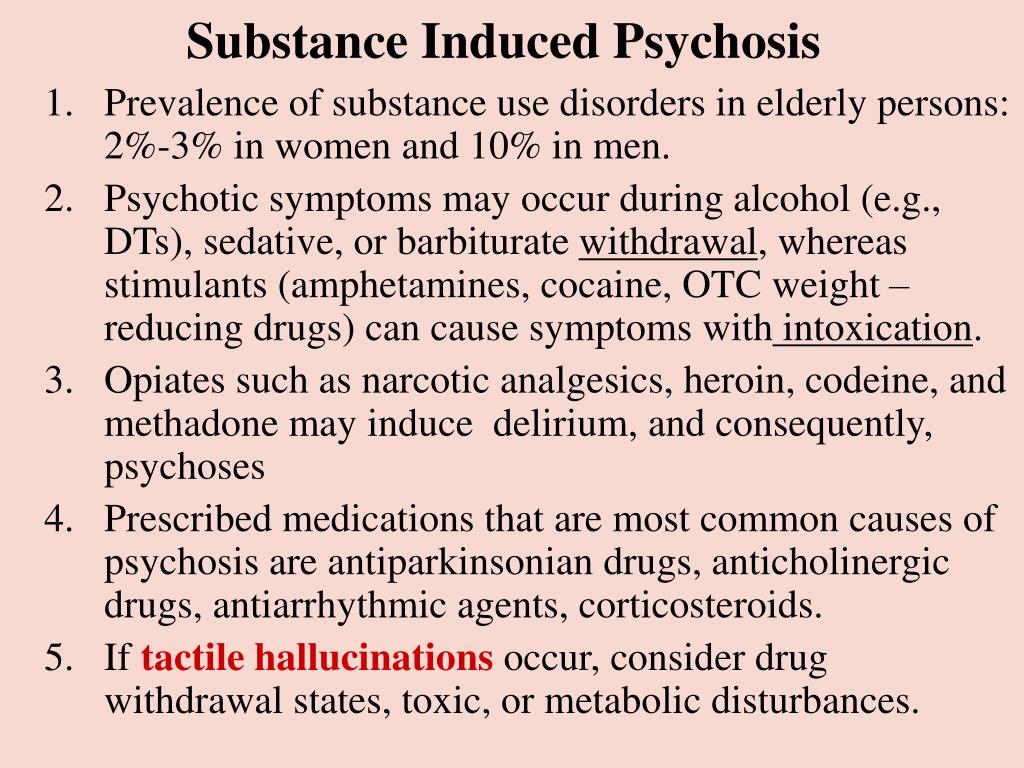
Substance-induced disorders include, among other disorders, substance/medication-induced mental disorders. Substance/medication-induced mental disorders refer to depressive, anxiety, psychotic, or manic symptoms that occur as a physiological consequence of the use of substances of abuse or medications. It may occur during active use, intoxication or withdrawal. This activity outlines the epidemiology, presentation, diagnosis, clinical evaluation, psychopathology, and treatment of substance/medication-induced mental disorders covering depression and bipolar by an interprofessional team.
Objectives:
Describe the epidemiology of substance/medication-induced disorders.
Outline the typical presentation of alcohol, cocaine, or opioid-induced mood disorders.
Summarize the treatment options for substance/medication-induced disorders.
Review the importance of an interprofessional approach in treating patients with substance/medication-induced disorders.
Access free multiple choice questions on this topic.
Introduction
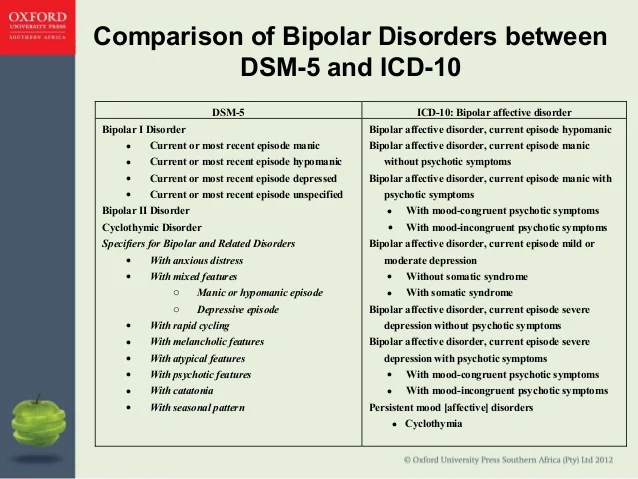
Although, both illicit substances and iatrogenic medications are ingested with the impetus to alleviate mood, a substantial proportion of patients experience paradoxical affective disorders following the ingestion of said substances. Instead of the prosaic euphoria experienced while intoxicated or the subsequent day 'hangover,' some individuals will become manic or enter into a state of depression. Mood disorders that precipitate only in association with substance use are specified as 'substance-induced.' Affective disorders that can precipitate in the setting of substance use include both bipolar and related disorders and depressive disorders. These disorders were previously found within the nosological category of substance-induced mood disorders, in DSM-IV. However, in the current DSM 'substance-induced' is now a specifier for mood disorders.
Depression and bipolar disorder frequently co-occur with substance use disorders (SUDs) and are prevalent in the general population.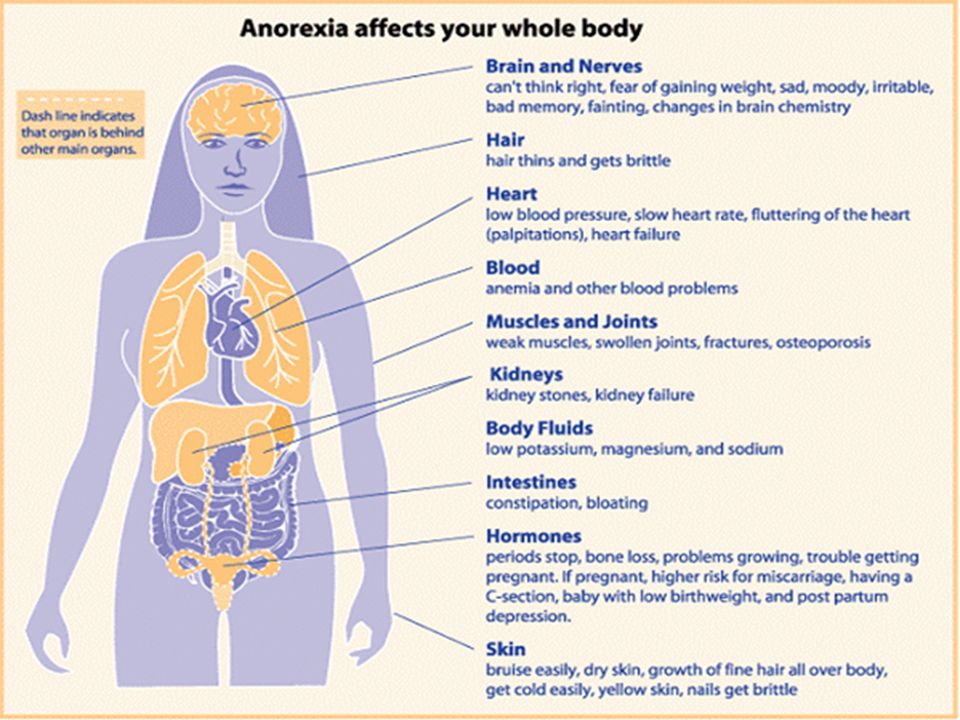 [1][2] This review will reflect on both substance-induced depressive disorder and substance-induced bipolar and related disorders, and further elaborate on how they can be distinguished from mood disorders that are comorbid with SUDs.
[1][2] This review will reflect on both substance-induced depressive disorder and substance-induced bipolar and related disorders, and further elaborate on how they can be distinguished from mood disorders that are comorbid with SUDs.
For the purpose of this review, the designation of substance-induced mood disorders - although no longer a distinct category in DSM-V - will represent both substance-induced depression and bipolar disorders.
Etiology
Substance-induced disorders may develop in the context of either intoxication or withdrawal. Of the depressive episodes occurring in the general population, nearly half precipitate in the context of heavy alcohol use.[3][4][5] The next most frequently associated substances are cocaine and opioids, especially heroin. Iatrogenic substances can also induce pathological affective states. Examples of such medications include interferon (IFN), corticosteroids, digoxin, and antiepileptic drugs.[6][7] Either class - substance or medication - can induce states of mania or depression.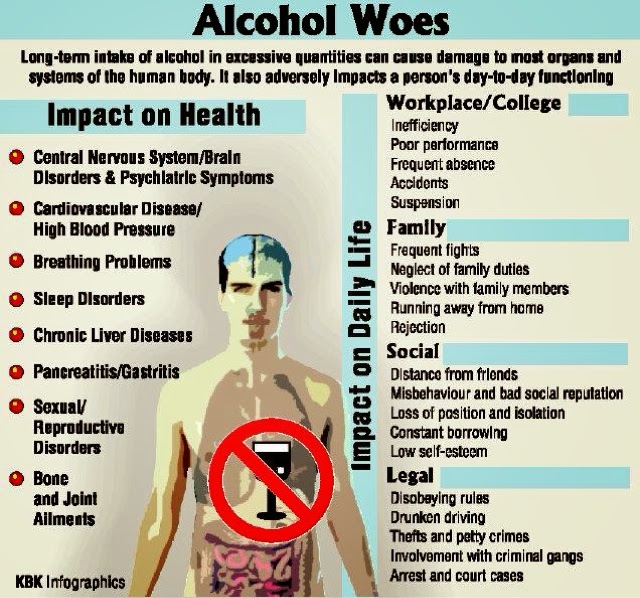 Current theorists posit that the aforementioned substances alter neurotransmitter transmission within important neural circuits, such as the mesolimbic tract and Papez circuit.[8]
Current theorists posit that the aforementioned substances alter neurotransmitter transmission within important neural circuits, such as the mesolimbic tract and Papez circuit.[8]
Recent evidence has also revealed that genes increase diathesis for both substance use disorders as well as mood disorders.[9]
Epidemiology
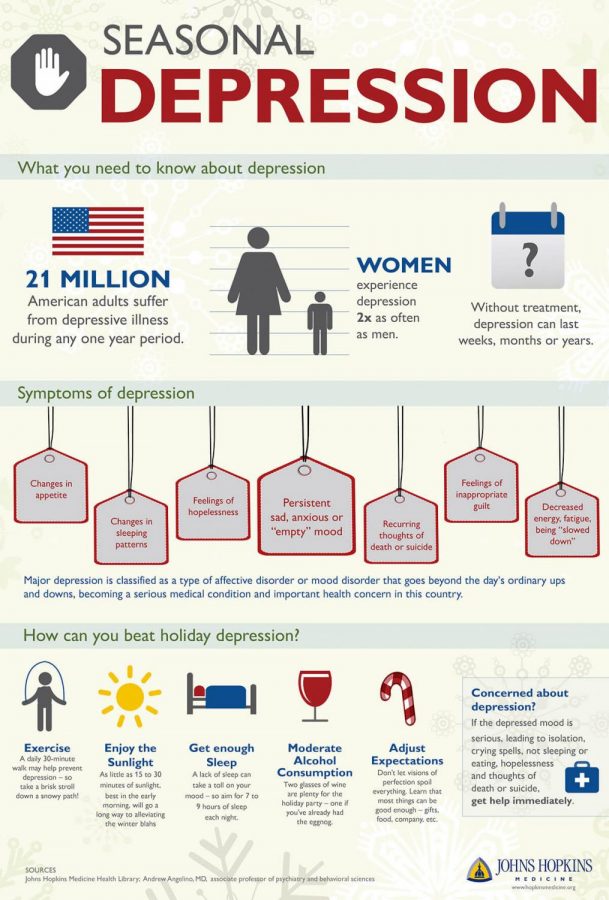
Current research estimates the lifetime prevalence of substance-induced depressive disorders between 0.26% and 1%.[10][1] Of those with alcohol use disorder, it is estimated that 40-60% experience substance-induced depression.[5][11][12] Data gathered from outpatient participants with opioid use disorder reported that around 55% of these participants had a substance-induced depression.[13] Of the individuals with major depression, 16.5% have an alcohol use disorder, and 18% have a drug use disorder. Additionally, data indicate that the lifetime prevalence of substance use disorders in bipolar I patients is 61%.[14]
Pathophysiology
The pathophysiology of substance-induced disorders remains a topic of ongoing discussion. Drug-induced mood symptoms precipitate changes in cerebral structures, such as the frontal cortex, nucleus accumbens, olfactory tubercle, hippocampus, amygdala, and hypothalamus.[15] Drug-induced mood symptoms involve alterations of serotonergic, dopaminergic, corticotropin-releasing factor (CRF), and neuropeptide Y (NPY) neurotransmitter activity.[16][17]
Drug-induced mood symptoms precipitate changes in cerebral structures, such as the frontal cortex, nucleus accumbens, olfactory tubercle, hippocampus, amygdala, and hypothalamus.[15] Drug-induced mood symptoms involve alterations of serotonergic, dopaminergic, corticotropin-releasing factor (CRF), and neuropeptide Y (NPY) neurotransmitter activity.[16][17]
History and Physical
Patients with substance-induced affective disorders will present similarly to patients with independent mood disorders with or without comorbid substance use disorders. Thus, patients may endorse sad mood, insomnia, feelings of guilt, suicidal ideation, psychomotor retardation, distractibility, hopelessness, helplessness, irritability, decreased libido, anergy, or anorexia if depressed. In the setting of mania, the patient will endorse grandiosity, distractibility, impulsivity, pressured speech, racing thoughts, sexual promiscuity, irritability, insomnia, and increased energy.
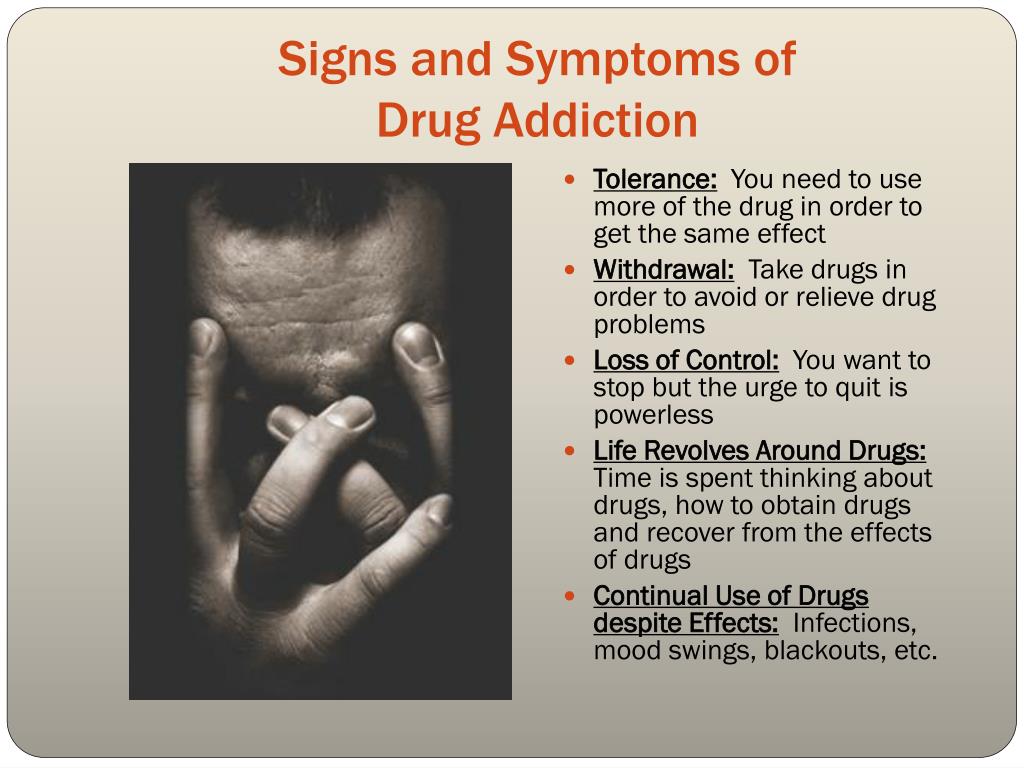
The anamnesis of a patient experience a substance-induced affective disorder will consist of mood symptomatology in direct temporal relation to the ingestion of the substance. These symptoms will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month). Generally, severe intoxication produces symptoms consistent with mania or hypomania, whereas withdrawal manifests as symptoms of depression. Depressants (e.g. alcohol, sedative-hypnotics, analgesics, etc) may induce states of euphoria, decreased impulse control, or mood lability. This intoxication phase is then supplanted by a withdrawal phase, most notable for irritability, agitation, and dysphoria. Stimulant use (e.g. cocaine, amphetamines, etc.) can mimic bipolar spectrum disorders by producing euphoria, increased energy, anorexia, grandiosity, and paranoia. Stimulant withdrawal can cause anhedonia, apathy, depressed mood, and suicidal ideation.[9]
These symptoms will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month). Generally, severe intoxication produces symptoms consistent with mania or hypomania, whereas withdrawal manifests as symptoms of depression. Depressants (e.g. alcohol, sedative-hypnotics, analgesics, etc) may induce states of euphoria, decreased impulse control, or mood lability. This intoxication phase is then supplanted by a withdrawal phase, most notable for irritability, agitation, and dysphoria. Stimulant use (e.g. cocaine, amphetamines, etc.) can mimic bipolar spectrum disorders by producing euphoria, increased energy, anorexia, grandiosity, and paranoia. Stimulant withdrawal can cause anhedonia, apathy, depressed mood, and suicidal ideation.[9]
Evaluation
The substance-induced mood disorder will mimic its corresponding independent affective disorder. Thus, substance-induced depression will follow diagnostic criteria used to evaluate for depressive disorders, and substance-induced bipolar disorder will reflect that of the bipolar spectrum disorders.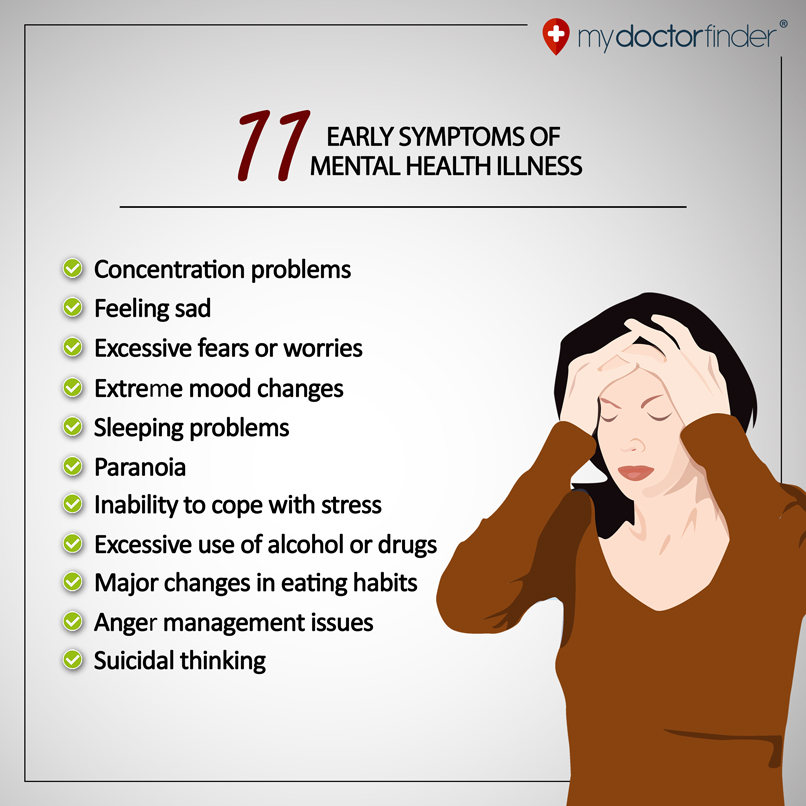 As implied by the title 'substance-induced', either admission of the ingestion of a substance or a positive laboratory test is necessary for a valid diagnosis. Temporality is the easiest feature to differentiate an independent affective disorder from a substance-induced one. As mentioned previously, symptoms of a substance-induced mood disorder will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month).[14] For substance-induced depressive disorder, the clinical picture is characterized by a depressed mood or a markedly diminished interest or pleasure in all spheres of life, and the symptomatology is corroborated with the history, physical examination, or laboratory findings. For the substance/medication-induced bipolar, the clinical picture is delineated by an elevated, expansive, or irritable mood, with or without depressed mood, or markedly diminished interest or pleasure in all spheres of life. Clinical evidence is corroborated with the history, physical examination, or laboratory findings.
As implied by the title 'substance-induced', either admission of the ingestion of a substance or a positive laboratory test is necessary for a valid diagnosis. Temporality is the easiest feature to differentiate an independent affective disorder from a substance-induced one. As mentioned previously, symptoms of a substance-induced mood disorder will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month).[14] For substance-induced depressive disorder, the clinical picture is characterized by a depressed mood or a markedly diminished interest or pleasure in all spheres of life, and the symptomatology is corroborated with the history, physical examination, or laboratory findings. For the substance/medication-induced bipolar, the clinical picture is delineated by an elevated, expansive, or irritable mood, with or without depressed mood, or markedly diminished interest or pleasure in all spheres of life. Clinical evidence is corroborated with the history, physical examination, or laboratory findings.
Laboratory results and imaging, as well as a detailed history, should rule out other etiologies of the ongoing affective disorder.
Treatment / Management
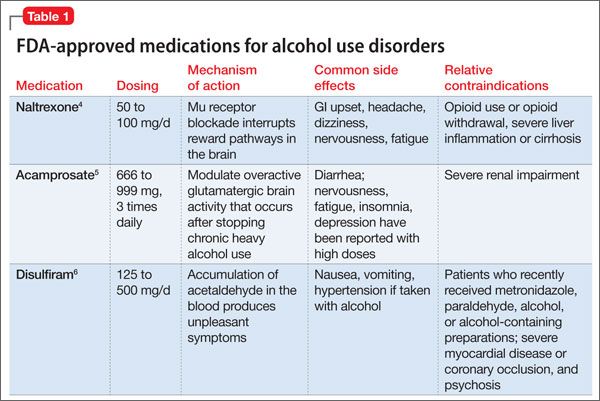
Implicit with the diagnosis of substance-induced mood disorder is the implication that the disorder should resolve spontaneously, following the cessation of the inciting irritant. However, the severity of a substance-induced affective episode may necessitate the application of medication. Clinical judgment, corroborated with a proper history and collateral information, will aid the clinician's decision whether to simply offer supportive care while observing the patient in a safe environment during the withdrawal period or to treat the active affective disorder. Because of the relative safety of most antidepressants, some studies suggest the empiric application of antidepressants in the setting of depressive symptomatology and co-occurring substance use.[14] For manic episodes, guidelines recommend second-generation antipsychotics, such as quetiapine or olanzapine, as they are faster acting than mood stabilizers.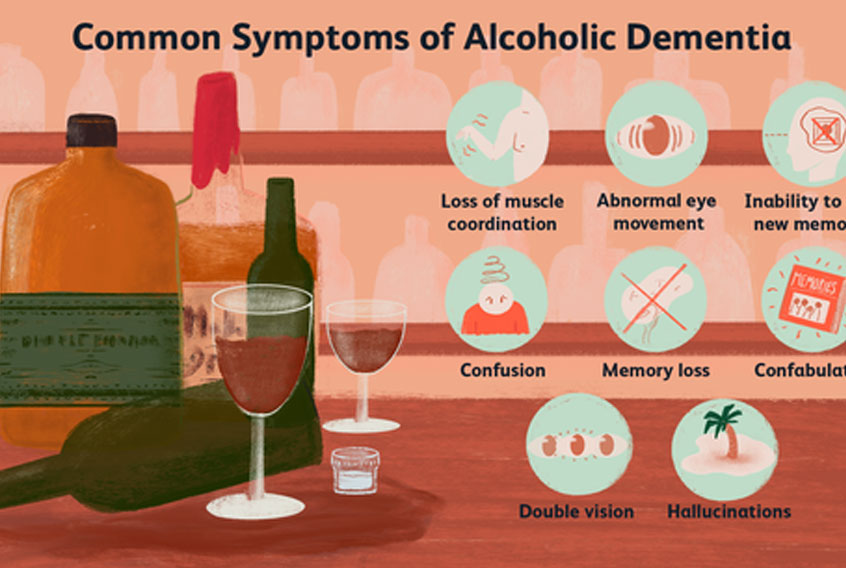 [18][19][20]
[18][19][20]
The most essential feature of treatment should be the emphasis on abstinence from the inciting substance. The treatment modality will vary depending on the substance of preference of the patient.
Differential Diagnosis
Transient substance-induced disorders may be differentiated from a primary psychiatric illness through observation during a period of abstinence with a temporal association of the intake of a substance. A family history of a primary psychiatric illness may also facilitate distinction. For substance-induced symptoms of mania, the differentiation may be more complex because of a high probability of temporal association or causality of mood symptoms after substance use.[9][3][4]
Prognosis
In theory, the mood symptoms should extenuate following a period of sobriety. Maintenance of said abstinence is the most robust prognosticative factor for subsequent episodes. Thus, invariably, factors that promote sobriety will potentiate remission.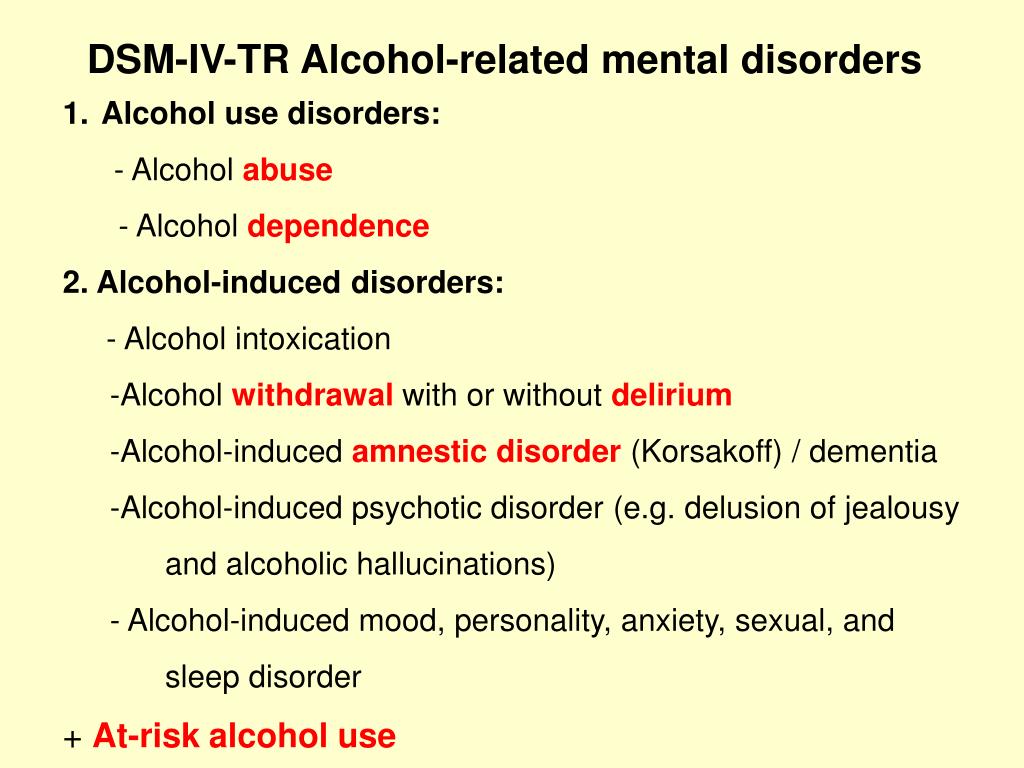 Familial support, psychotherapy, financial stability, and medication compliance are all factors that promote sobriety. Recipricolaly, settings which increase the risk of substance use are associated with poorer prognoses.
Familial support, psychotherapy, financial stability, and medication compliance are all factors that promote sobriety. Recipricolaly, settings which increase the risk of substance use are associated with poorer prognoses.
Complications
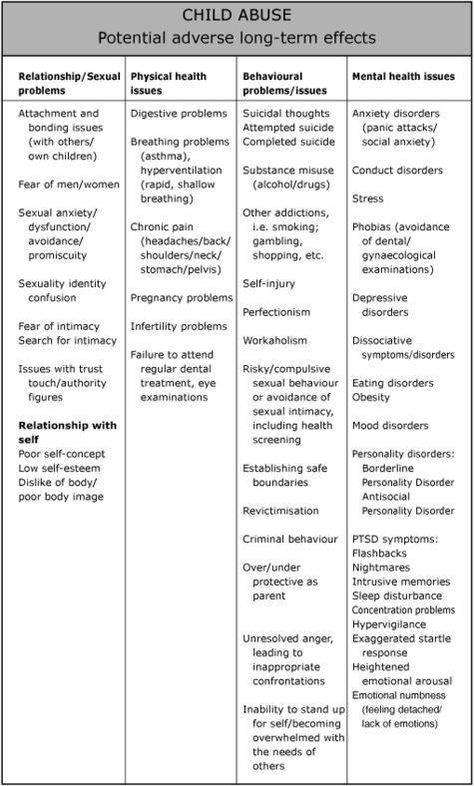
The most significant complication looming over substance-induced mood disorders is suicide. Studies reveal that suicide attempts are more common in affective disorders that are substance-induced. One study estimated an almost four-fold increased risk of suicide attempts when the mood disorder precipitates in the setting of substance use.[21]
Deterrence and Patient Education
Refrain from the use of alcohol or illicit drugs.
Avoid people or milieu that most likely trigger the use of alcohol or illicit drugs.
Consider psychosocial interventions like AA and NA to promote recovery from alcohol and substance abuse.
Discuss with a physician about any new medication prescribed by another physician because some medications can cause mania or depression.
Contact a physician if having concerns regarding over the counter medicines because some OTCs can augment the effects of other medications and may cause mania or depression.
Eat a healthy diet, limit caffeine, and quit smoking.
Be aware of depression or mania that result after the initiation of substance use or use of medication and discuss them with your primary care physician or psychiatrist.
Enhancing Healthcare Team Outcomes
Managing substance-induced disorders disorder requires a multidisciplinary approach involving the patient, the patient’s family, physician, nurse, and therapist. Although substance-induced disorders (depression and bipolar) subside after the biological effects of the drug fade, vulnerable individuals can develop a full-blown major depressive disorder or bipolar disorder, without proper management, psychiatric and medical complications can be fatal.
In the emergency department, physicians and assigned nurses are responsible for coordinating the care, which includes the following:
Drug levels in the blood and or urine
Monitor the patient for signs and symptoms of respiratory depression and cardiac arrhythmias.
Administer benzodiazepines or antipsychotics for acute mania.
Creatine phosphokinase (CPK) to rule out rhabdomyolysis
Provide rehydration with normal saline
Provide 1:1 for safety (suicide and injury to others)
Consider involuntary status for imminent threats to self and others
Physical restraints as the last result
Consult an addiction specialist
In the outpatient clinic physician and assigned nurse are responsible for:
Assure the patient’s safety and others in case of acute mania or severe depression.
Transport the patient to the emergency department.
Consider an involuntary commitment to a psychiatric hospital for imminent threats to self and others.
Physicians, nurses, and therapists should discuss and involve the family in the treatment plan. An interprofessional team that provides a holistic and integrated approach can help achieve the best possible outcomes.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004 Aug;61(8):807-16. [PubMed: 15289279]
- 2.
Tolliver BK, Anton RF. Assessment and treatment of mood disorders in the context of substance abuse. Dialogues Clin Neurosci. 2015 Jun;17(2):181-90. [PMC free article: PMC4518701] [PubMed: 26246792]
- 3.
Brown SA, Inaba RK, Gillin JC, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: clinical course of depressive symptoms. Am J Psychiatry. 1995 Jan;152(1):45-52. [PubMed: 7802119]
- 4.
Davidson KM.
 Diagnosis of depression in alcohol dependence: changes in prevalence with drinking status. Br J Psychiatry. 1995 Feb;166(2):199-204. [PubMed: 7728364]
Diagnosis of depression in alcohol dependence: changes in prevalence with drinking status. Br J Psychiatry. 1995 Feb;166(2):199-204. [PubMed: 7728364]- 5.
Schuckit MA, Smith TL, Danko GP, Pierson J, Trim R, Nurnberger JI, Kramer J, Kuperman S, Bierut LJ, Hesselbrock V. A comparison of factors associated with substance-induced versus independent depressions. J Stud Alcohol Drugs. 2007 Nov;68(6):805-12. [PubMed: 17960298]
- 6.
Patten SB, Barbui C. Drug-induced depression: a systematic review to inform clinical practice. Psychother Psychosom. 2004 Jul-Aug;73(4):207-15. [PubMed: 15184715]
- 7.
Anisman H, Kokkinidis L, Merali Z. Further evidence for the depressive effects of cytokines: anhedonia and neurochemical changes. Brain Behav Immun. 2002 Oct;16(5):544-56. [PubMed: 12401468]
- 8.
Markou A, Kosten TR, Koob GF. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis.
 Neuropsychopharmacology. 1998 Mar;18(3):135-74. [PubMed: 9471114]
Neuropsychopharmacology. 1998 Mar;18(3):135-74. [PubMed: 9471114]- 9.
Quello SB, Brady KT, Sonne SC. Mood disorders and substance use disorder: a complex comorbidity. Sci Pract Perspect. 2005 Dec;3(1):13-21. [PMC free article: PMC2851027] [PubMed: 18552741]
- 10.
Blanco C, Alegría AA, Liu SM, Secades-Villa R, Sugaya L, Davies C, Nunes EV. Differences among major depressive disorder with and without co-occurring substance use disorders and substance-induced depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2012 Jun;73(6):865-73. [PubMed: 22480900]
- 11.
Gilder DA, Wall TL, Ehlers CL. Comorbidity of select anxiety and affective disorders with alcohol dependence in southwest California Indians. Alcohol Clin Exp Res. 2004 Dec;28(12):1805-13. [PubMed: 15608596]
- 12.
Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN.
 Addiction. 1999 Sep;94(9):1361-70. [PubMed: 10615721]
Addiction. 1999 Sep;94(9):1361-70. [PubMed: 10615721]- 13.
Ahmadi J, Majdi B, Mahdavi S, Mohagheghzadeh M. Mood disorders in opioid-dependent patients. J Affect Disord. 2004 Oct 01;82(1):139-42. [PubMed: 15465588]
- 14.
Myrick H, Cluver J, Swavely S, Peters H. Diagnosis and treatment of co-occurring affective disorders and substance use disorders. Psychiatr Clin North Am. 2004 Dec;27(4):649-59. [PubMed: 15550285]
- 15.
Peroutka SJ, Snyder SH. Long-term antidepressant treatment decreases spiroperidol-labeled serotonin receptor binding. Science. 1980 Oct 03;210(4465):88-90. [PubMed: 6251550]
- 16.
Parsons LH, Smith AD, Justice JB. Basal extracellular dopamine is decreased in the rat nucleus accumbens during abstinence from chronic cocaine. Synapse. 1991 Sep;9(1):60-5. [PubMed: 1796352]
- 17.
Kosten TR, Markou A, Koob GF. Depression and stimulant dependence: neurobiology and pharmacotherapy.
 J Nerv Ment Dis. 1998 Dec;186(12):737-45. [PubMed: 9865811]
J Nerv Ment Dis. 1998 Dec;186(12):737-45. [PubMed: 9865811]- 18.
Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmelhoch JM, Thase ME. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005 Jan;62(1):37-45. [PubMed: 15630071]
- 19.
Salloum IM, Douaihy A, Cornelius JR, Kirisci L, Kelly TM, Hayes J. Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addict Behav. 2007 Feb;32(2):410-5. [PubMed: 16814474]
- 20.
Brown ES, Nejtek VA, Perantie DC, Bobadilla L. Quetiapine in bipolar disorder and cocaine dependence. Bipolar Disord. 2002 Dec;4(6):406-11. [PubMed: 12519101]
- 21.
Conner KR, Gamble SA, Bagge CL, He H, Swogger MT, Watts A, Houston RJ. Substance-induced depression and independent depression in proximal risk for suicidal behavior. J Stud Alcohol Drugs. 2014 Jul;75(4):567-72.
 [PMC free article: PMC9798469] [PubMed: 24988255]
[PMC free article: PMC9798469] [PubMed: 24988255]
Substance Induced Mood Disorders - StatPearls
Continuing Education Activity
Substance-induced disorders include, among other disorders, substance/medication-induced mental disorders. Substance/medication-induced mental disorders refer to depressive, anxiety, psychotic, or manic symptoms that occur as a physiological consequence of the use of substances of abuse or medications. It may occur during active use, intoxication or withdrawal. This activity outlines the epidemiology, presentation, diagnosis, clinical evaluation, psychopathology, and treatment of substance/medication-induced mental disorders covering depression and bipolar by an interprofessional team.
Objectives:
Describe the epidemiology of substance/medication-induced disorders.
Outline the typical presentation of alcohol, cocaine, or opioid-induced mood disorders.
Summarize the treatment options for substance/medication-induced disorders.

Review the importance of an interprofessional approach in treating patients with substance/medication-induced disorders.
Access free multiple choice questions on this topic.
Introduction
Although, both illicit substances and iatrogenic medications are ingested with the impetus to alleviate mood, a substantial proportion of patients experience paradoxical affective disorders following the ingestion of said substances. Instead of the prosaic euphoria experienced while intoxicated or the subsequent day 'hangover,' some individuals will become manic or enter into a state of depression. Mood disorders that precipitate only in association with substance use are specified as 'substance-induced.' Affective disorders that can precipitate in the setting of substance use include both bipolar and related disorders and depressive disorders. These disorders were previously found within the nosological category of substance-induced mood disorders, in DSM-IV. However, in the current DSM 'substance-induced' is now a specifier for mood disorders.
However, in the current DSM 'substance-induced' is now a specifier for mood disorders.
Depression and bipolar disorder frequently co-occur with substance use disorders (SUDs) and are prevalent in the general population.[1][2] This review will reflect on both substance-induced depressive disorder and substance-induced bipolar and related disorders, and further elaborate on how they can be distinguished from mood disorders that are comorbid with SUDs.
For the purpose of this review, the designation of substance-induced mood disorders - although no longer a distinct category in DSM-V - will represent both substance-induced depression and bipolar disorders.
Etiology
Substance-induced disorders may develop in the context of either intoxication or withdrawal. Of the depressive episodes occurring in the general population, nearly half precipitate in the context of heavy alcohol use.[3][4][5] The next most frequently associated substances are cocaine and opioids, especially heroin. Iatrogenic substances can also induce pathological affective states. Examples of such medications include interferon (IFN), corticosteroids, digoxin, and antiepileptic drugs.[6][7] Either class - substance or medication - can induce states of mania or depression. Current theorists posit that the aforementioned substances alter neurotransmitter transmission within important neural circuits, such as the mesolimbic tract and Papez circuit.[8]
Iatrogenic substances can also induce pathological affective states. Examples of such medications include interferon (IFN), corticosteroids, digoxin, and antiepileptic drugs.[6][7] Either class - substance or medication - can induce states of mania or depression. Current theorists posit that the aforementioned substances alter neurotransmitter transmission within important neural circuits, such as the mesolimbic tract and Papez circuit.[8]
Recent evidence has also revealed that genes increase diathesis for both substance use disorders as well as mood disorders.[9]
Epidemiology
Current research estimates the lifetime prevalence of substance-induced depressive disorders between 0.26% and 1%.[10][1] Of those with alcohol use disorder, it is estimated that 40-60% experience substance-induced depression.[5][11][12] Data gathered from outpatient participants with opioid use disorder reported that around 55% of these participants had a substance-induced depression.[13] Of the individuals with major depression, 16.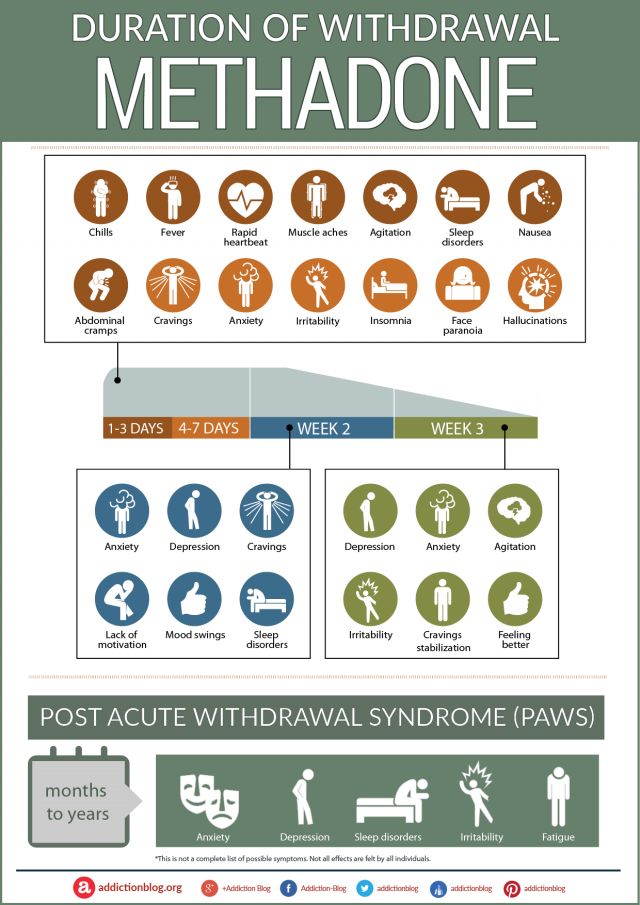 5% have an alcohol use disorder, and 18% have a drug use disorder. Additionally, data indicate that the lifetime prevalence of substance use disorders in bipolar I patients is 61%.[14]
5% have an alcohol use disorder, and 18% have a drug use disorder. Additionally, data indicate that the lifetime prevalence of substance use disorders in bipolar I patients is 61%.[14]
Pathophysiology
The pathophysiology of substance-induced disorders remains a topic of ongoing discussion. Drug-induced mood symptoms precipitate changes in cerebral structures, such as the frontal cortex, nucleus accumbens, olfactory tubercle, hippocampus, amygdala, and hypothalamus.[15] Drug-induced mood symptoms involve alterations of serotonergic, dopaminergic, corticotropin-releasing factor (CRF), and neuropeptide Y (NPY) neurotransmitter activity.[16][17]
History and Physical
Patients with substance-induced affective disorders will present similarly to patients with independent mood disorders with or without comorbid substance use disorders. Thus, patients may endorse sad mood, insomnia, feelings of guilt, suicidal ideation, psychomotor retardation, distractibility, hopelessness, helplessness, irritability, decreased libido, anergy, or anorexia if depressed.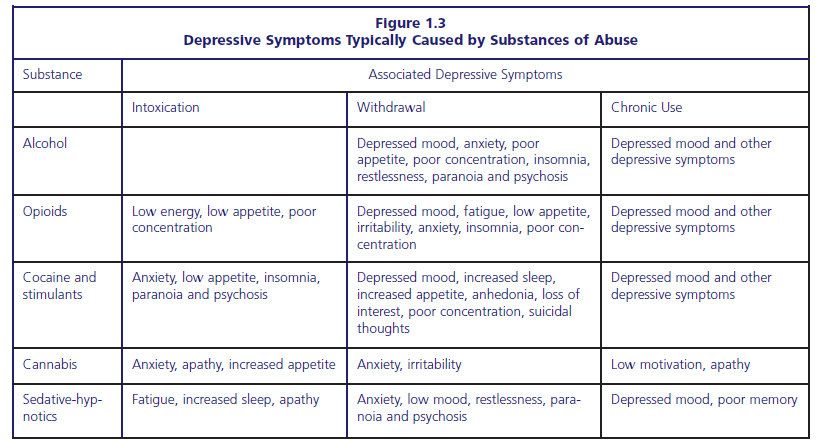 In the setting of mania, the patient will endorse grandiosity, distractibility, impulsivity, pressured speech, racing thoughts, sexual promiscuity, irritability, insomnia, and increased energy.
In the setting of mania, the patient will endorse grandiosity, distractibility, impulsivity, pressured speech, racing thoughts, sexual promiscuity, irritability, insomnia, and increased energy.
The anamnesis of a patient experience a substance-induced affective disorder will consist of mood symptomatology in direct temporal relation to the ingestion of the substance. These symptoms will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month). Generally, severe intoxication produces symptoms consistent with mania or hypomania, whereas withdrawal manifests as symptoms of depression. Depressants (e.g. alcohol, sedative-hypnotics, analgesics, etc) may induce states of euphoria, decreased impulse control, or mood lability. This intoxication phase is then supplanted by a withdrawal phase, most notable for irritability, agitation, and dysphoria. Stimulant use (e.g. cocaine, amphetamines, etc.) can mimic bipolar spectrum disorders by producing euphoria, increased energy, anorexia, grandiosity, and paranoia.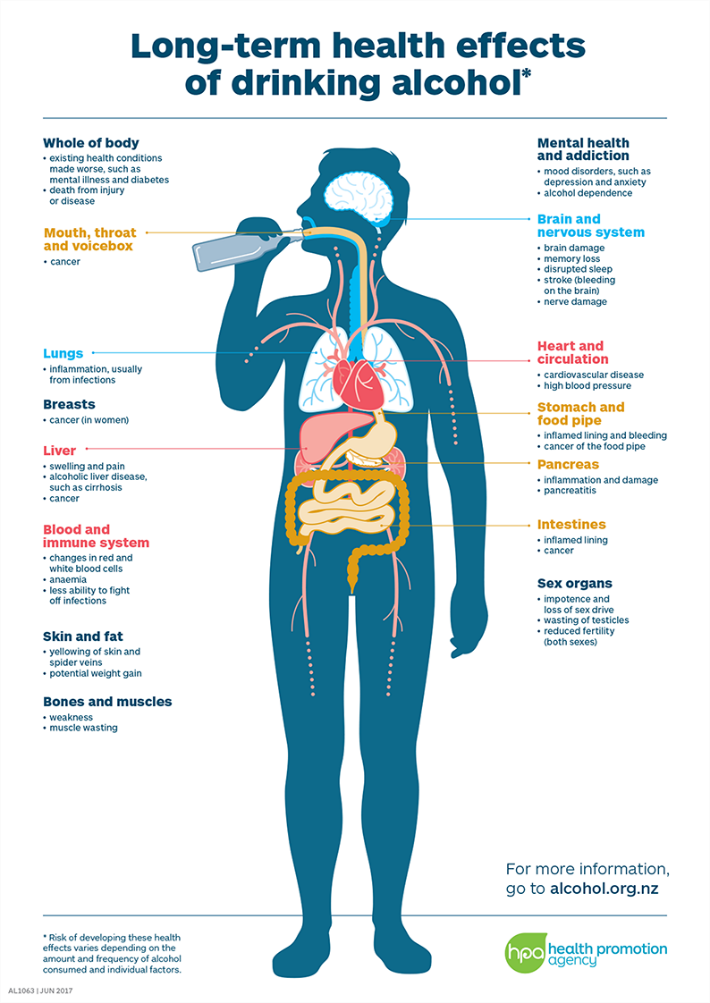 Stimulant withdrawal can cause anhedonia, apathy, depressed mood, and suicidal ideation.[9]
Stimulant withdrawal can cause anhedonia, apathy, depressed mood, and suicidal ideation.[9]
Evaluation
The substance-induced mood disorder will mimic its corresponding independent affective disorder. Thus, substance-induced depression will follow diagnostic criteria used to evaluate for depressive disorders, and substance-induced bipolar disorder will reflect that of the bipolar spectrum disorders. As implied by the title 'substance-induced', either admission of the ingestion of a substance or a positive laboratory test is necessary for a valid diagnosis. Temporality is the easiest feature to differentiate an independent affective disorder from a substance-induced one. As mentioned previously, symptoms of a substance-induced mood disorder will resolve following the cessation of severe intoxication or acute withdrawal (up to 1 month).[14] For substance-induced depressive disorder, the clinical picture is characterized by a depressed mood or a markedly diminished interest or pleasure in all spheres of life, and the symptomatology is corroborated with the history, physical examination, or laboratory findings. For the substance/medication-induced bipolar, the clinical picture is delineated by an elevated, expansive, or irritable mood, with or without depressed mood, or markedly diminished interest or pleasure in all spheres of life. Clinical evidence is corroborated with the history, physical examination, or laboratory findings.
For the substance/medication-induced bipolar, the clinical picture is delineated by an elevated, expansive, or irritable mood, with or without depressed mood, or markedly diminished interest or pleasure in all spheres of life. Clinical evidence is corroborated with the history, physical examination, or laboratory findings.
Laboratory results and imaging, as well as a detailed history, should rule out other etiologies of the ongoing affective disorder.
Treatment / Management
Implicit with the diagnosis of substance-induced mood disorder is the implication that the disorder should resolve spontaneously, following the cessation of the inciting irritant. However, the severity of a substance-induced affective episode may necessitate the application of medication. Clinical judgment, corroborated with a proper history and collateral information, will aid the clinician's decision whether to simply offer supportive care while observing the patient in a safe environment during the withdrawal period or to treat the active affective disorder. Because of the relative safety of most antidepressants, some studies suggest the empiric application of antidepressants in the setting of depressive symptomatology and co-occurring substance use.[14] For manic episodes, guidelines recommend second-generation antipsychotics, such as quetiapine or olanzapine, as they are faster acting than mood stabilizers.[18][19][20]
Because of the relative safety of most antidepressants, some studies suggest the empiric application of antidepressants in the setting of depressive symptomatology and co-occurring substance use.[14] For manic episodes, guidelines recommend second-generation antipsychotics, such as quetiapine or olanzapine, as they are faster acting than mood stabilizers.[18][19][20]
The most essential feature of treatment should be the emphasis on abstinence from the inciting substance. The treatment modality will vary depending on the substance of preference of the patient.
Differential Diagnosis
Transient substance-induced disorders may be differentiated from a primary psychiatric illness through observation during a period of abstinence with a temporal association of the intake of a substance. A family history of a primary psychiatric illness may also facilitate distinction. For substance-induced symptoms of mania, the differentiation may be more complex because of a high probability of temporal association or causality of mood symptoms after substance use.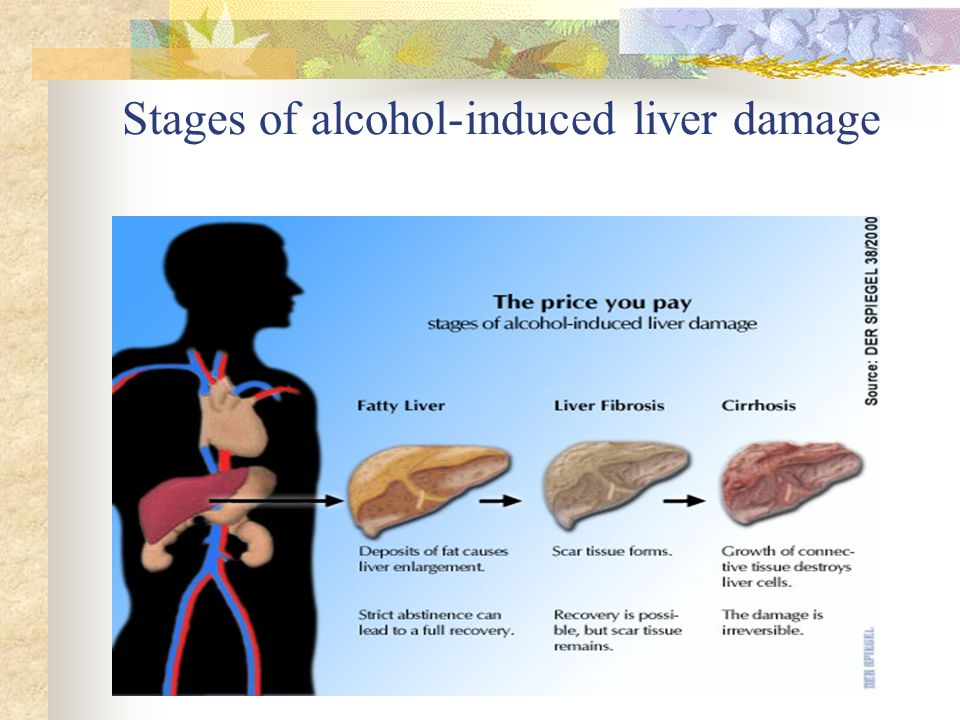 [9][3][4]
[9][3][4]
Prognosis
In theory, the mood symptoms should extenuate following a period of sobriety. Maintenance of said abstinence is the most robust prognosticative factor for subsequent episodes. Thus, invariably, factors that promote sobriety will potentiate remission. Familial support, psychotherapy, financial stability, and medication compliance are all factors that promote sobriety. Recipricolaly, settings which increase the risk of substance use are associated with poorer prognoses.
Complications
The most significant complication looming over substance-induced mood disorders is suicide. Studies reveal that suicide attempts are more common in affective disorders that are substance-induced. One study estimated an almost four-fold increased risk of suicide attempts when the mood disorder precipitates in the setting of substance use.[21]
Deterrence and Patient Education
Refrain from the use of alcohol or illicit drugs.
Avoid people or milieu that most likely trigger the use of alcohol or illicit drugs.
Consider psychosocial interventions like AA and NA to promote recovery from alcohol and substance abuse.
Discuss with a physician about any new medication prescribed by another physician because some medications can cause mania or depression.
Contact a physician if having concerns regarding over the counter medicines because some OTCs can augment the effects of other medications and may cause mania or depression.
Eat a healthy diet, limit caffeine, and quit smoking.
Be aware of depression or mania that result after the initiation of substance use or use of medication and discuss them with your primary care physician or psychiatrist.
Enhancing Healthcare Team Outcomes
Managing substance-induced disorders disorder requires a multidisciplinary approach involving the patient, the patient’s family, physician, nurse, and therapist. Although substance-induced disorders (depression and bipolar) subside after the biological effects of the drug fade, vulnerable individuals can develop a full-blown major depressive disorder or bipolar disorder, without proper management, psychiatric and medical complications can be fatal.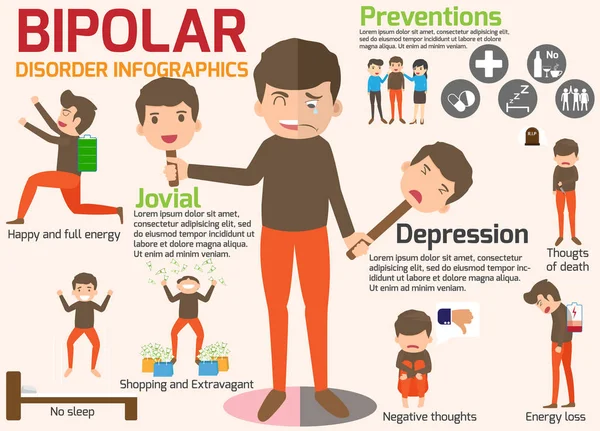
In the emergency department, physicians and assigned nurses are responsible for coordinating the care, which includes the following:
Drug levels in the blood and or urine
Monitor the patient for signs and symptoms of respiratory depression and cardiac arrhythmias.
Administer benzodiazepines or antipsychotics for acute mania.
Creatine phosphokinase (CPK) to rule out rhabdomyolysis
Provide rehydration with normal saline
Provide 1:1 for safety (suicide and injury to others)
Consider involuntary status for imminent threats to self and others
Physical restraints as the last result
Consult an addiction specialist
In the outpatient clinic physician and assigned nurse are responsible for:
Assure the patient’s safety and others in case of acute mania or severe depression.
Transport the patient to the emergency department.

Consider an involuntary commitment to a psychiatric hospital for imminent threats to self and others.
Physicians, nurses, and therapists should discuss and involve the family in the treatment plan. An interprofessional team that provides a holistic and integrated approach can help achieve the best possible outcomes.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004 Aug;61(8):807-16. [PubMed: 15289279]
- 2.
Tolliver BK, Anton RF. Assessment and treatment of mood disorders in the context of substance abuse. Dialogues Clin Neurosci.
 2015 Jun;17(2):181-90. [PMC free article: PMC4518701] [PubMed: 26246792]
2015 Jun;17(2):181-90. [PMC free article: PMC4518701] [PubMed: 26246792]- 3.
Brown SA, Inaba RK, Gillin JC, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: clinical course of depressive symptoms. Am J Psychiatry. 1995 Jan;152(1):45-52. [PubMed: 7802119]
- 4.
Davidson KM. Diagnosis of depression in alcohol dependence: changes in prevalence with drinking status. Br J Psychiatry. 1995 Feb;166(2):199-204. [PubMed: 7728364]
- 5.
Schuckit MA, Smith TL, Danko GP, Pierson J, Trim R, Nurnberger JI, Kramer J, Kuperman S, Bierut LJ, Hesselbrock V. A comparison of factors associated with substance-induced versus independent depressions. J Stud Alcohol Drugs. 2007 Nov;68(6):805-12. [PubMed: 17960298]
- 6.
Patten SB, Barbui C. Drug-induced depression: a systematic review to inform clinical practice. Psychother Psychosom. 2004 Jul-Aug;73(4):207-15. [PubMed: 15184715]
- 7.
Anisman H, Kokkinidis L, Merali Z.
 Further evidence for the depressive effects of cytokines: anhedonia and neurochemical changes. Brain Behav Immun. 2002 Oct;16(5):544-56. [PubMed: 12401468]
Further evidence for the depressive effects of cytokines: anhedonia and neurochemical changes. Brain Behav Immun. 2002 Oct;16(5):544-56. [PubMed: 12401468]- 8.
Markou A, Kosten TR, Koob GF. Neurobiological similarities in depression and drug dependence: a self-medication hypothesis. Neuropsychopharmacology. 1998 Mar;18(3):135-74. [PubMed: 9471114]
- 9.
Quello SB, Brady KT, Sonne SC. Mood disorders and substance use disorder: a complex comorbidity. Sci Pract Perspect. 2005 Dec;3(1):13-21. [PMC free article: PMC2851027] [PubMed: 18552741]
- 10.
Blanco C, Alegría AA, Liu SM, Secades-Villa R, Sugaya L, Davies C, Nunes EV. Differences among major depressive disorder with and without co-occurring substance use disorders and substance-induced depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2012 Jun;73(6):865-73. [PubMed: 22480900]
- 11.
Gilder DA, Wall TL, Ehlers CL.
 Comorbidity of select anxiety and affective disorders with alcohol dependence in southwest California Indians. Alcohol Clin Exp Res. 2004 Dec;28(12):1805-13. [PubMed: 15608596]
Comorbidity of select anxiety and affective disorders with alcohol dependence in southwest California Indians. Alcohol Clin Exp Res. 2004 Dec;28(12):1805-13. [PubMed: 15608596]- 12.
Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN. Addiction. 1999 Sep;94(9):1361-70. [PubMed: 10615721]
- 13.
Ahmadi J, Majdi B, Mahdavi S, Mohagheghzadeh M. Mood disorders in opioid-dependent patients. J Affect Disord. 2004 Oct 01;82(1):139-42. [PubMed: 15465588]
- 14.
Myrick H, Cluver J, Swavely S, Peters H. Diagnosis and treatment of co-occurring affective disorders and substance use disorders. Psychiatr Clin North Am. 2004 Dec;27(4):649-59. [PubMed: 15550285]
- 15.
Peroutka SJ, Snyder SH. Long-term antidepressant treatment decreases spiroperidol-labeled serotonin receptor binding. Science. 1980 Oct 03;210(4465):88-90. [PubMed: 6251550]
- 16.
Parsons LH, Smith AD, Justice JB. Basal extracellular dopamine is decreased in the rat nucleus accumbens during abstinence from chronic cocaine. Synapse. 1991 Sep;9(1):60-5. [PubMed: 1796352]
- 17.
Kosten TR, Markou A, Koob GF. Depression and stimulant dependence: neurobiology and pharmacotherapy. J Nerv Ment Dis. 1998 Dec;186(12):737-45. [PubMed: 9865811]
- 18.
Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmelhoch JM, Thase ME. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005 Jan;62(1):37-45. [PubMed: 15630071]
- 19.
Salloum IM, Douaihy A, Cornelius JR, Kirisci L, Kelly TM, Hayes J. Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addict Behav. 2007 Feb;32(2):410-5. [PubMed: 16814474]
- 20.
Brown ES, Nejtek VA, Perantie DC, Bobadilla L. Quetiapine in bipolar disorder and cocaine dependence.
 Bipolar Disord. 2002 Dec;4(6):406-11. [PubMed: 12519101]
Bipolar Disord. 2002 Dec;4(6):406-11. [PubMed: 12519101]- 21.
Conner KR, Gamble SA, Bagge CL, He H, Swogger MT, Watts A, Houston RJ. Substance-induced depression and independent depression in proximal risk for suicidal behavior. J Stud Alcohol Drugs. 2014 Jul;75(4):567-72. [PMC free article: PMC9798469] [PubMed: 24988255]
Alcoholic depression - symptoms, causes, diagnosis and treatment of alcoholic depression
Article reviewed by an expert:
MAKE AN APPOINTMENT
Alcoholic depression is an affective disorder that occurs in people suffering from alcoholism. Usually lasts from 2 weeks to 1 month. The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness.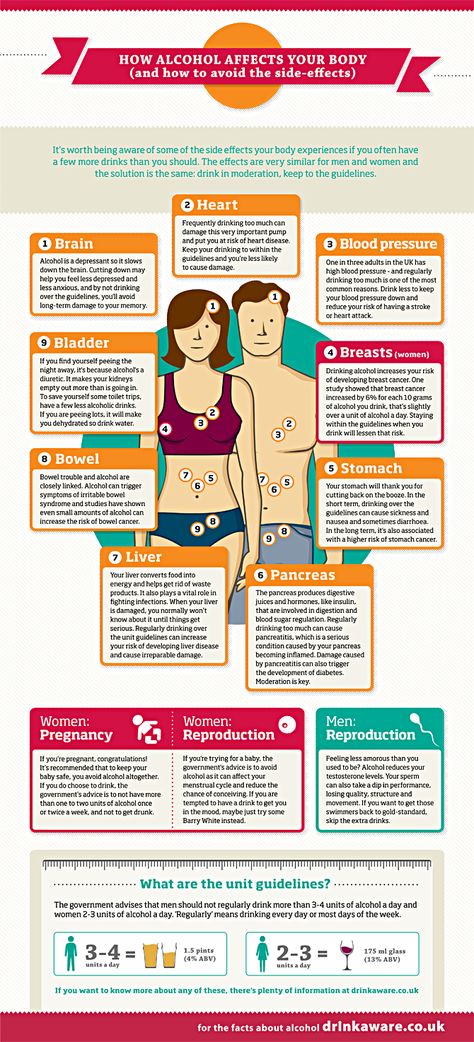 Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy. nine0003
Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy. nine0003
Alcoholic depression - what is it?
Depression in alcoholism was described by Bleuler in 1920 under the name "alcoholic melancholia". Subsequent studies have confirmed both the presence of specific depressive and subdepressive conditions in alcoholics, and the complex, diverse links between alcoholism and depressive disorders. The frequency of development of the disease and the severity of symptoms directly correlates with the duration and severity of alcoholism. Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age. nine0003
The average duration of post-alcoholic depression in alcoholism ranges from 2 weeks to 1 month. In severe cases, symptoms may persist for a year or more.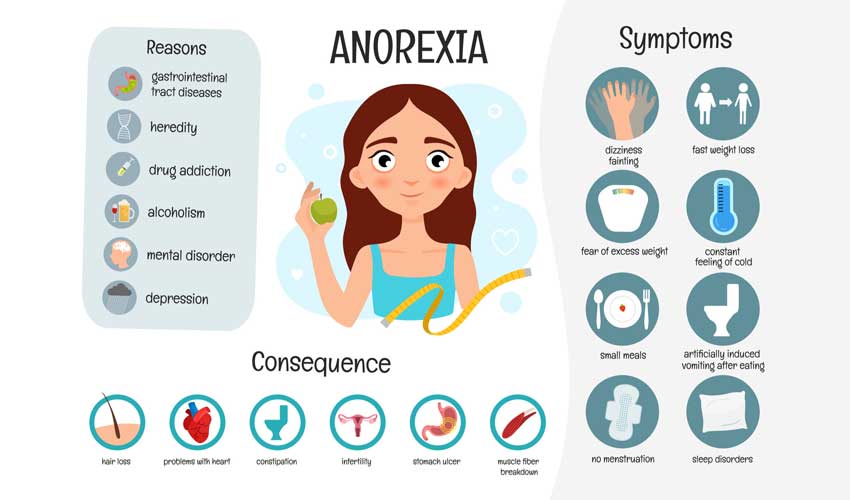 The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry. nine0003
The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry. nine0003
Causes of alcohol depression
Depression in alcoholism is a multifactorial disease. A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations. nine0003
Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations. nine0003
Alcoholic depression is part of the symptom complex of deprivation syndrome, acute alcohol intoxication, binge drinking and uncontrolled craving for alcohol. The most common cause of depressive mental disorder in alcoholics is withdrawal symptoms. Mental suffering of patients is provoked by severe physical and psychological discomfort and social problems, combined with a pathological need for alcohol.
Several bouts of depression occur in patients undergoing treatment for alcoholism in specialized clinics. In the initial stages of therapy, such patients develop a "sobriety phobia" - a pronounced fear of the possibility of life without alcohol. This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore. nine0003
Longing for alcohol and psychological problems come to the fore. nine0003
Sometimes depressive disorders develop against the background of remission, when a person feels lost, unable to fit in, “fallen out” of the normal rhythm of life and social environment, suffering from changes in habitual patterns of behavior, forced to solve numerous problems that arose during the period of alcoholism, without having enough external support and internal reserves. Such depressions can cause a breakdown and further alcoholization of the patient.
It should be borne in mind that the premorbid background is of some importance in the development of alcoholism. Even before the start of alcohol consumption, many patients have an increased tendency to mood swings, the development of asthenic conditions, depressive neurosis, subdepression and all kinds of borderline disorders. As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes.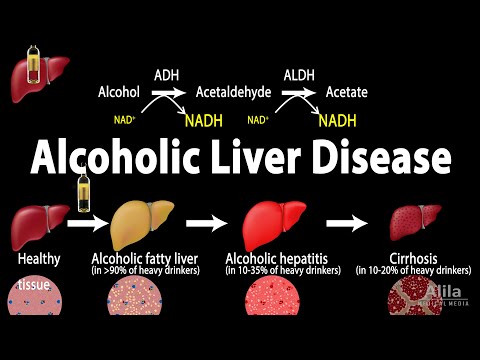 There are also complications and neurosis after a complete rejection of alcohol. nine0003
There are also complications and neurosis after a complete rejection of alcohol. nine0003
Symptoms and differential diagnosis of alcohol depression
Symptoms of depression in alcoholism are usually mild. Severe affective disorders are relatively rare. The mood is constantly depressed, the patient suffers from a feeling of emptiness and meaninglessness of existence. There is a feeling of loss of colors, the emotional colorlessness of the world, characteristic of depressive disorders. This perception causes depression and anxiety. Anhedonia develops - a person loses the ability to rejoice, cannot enjoy. nine0003
Psychological changes are combined with motor and intellectual retardation. Gait and movements slow down, the voice becomes quiet, monotonous. Mimic diversity disappears, the patient's face almost constantly retains a sad expression. The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction.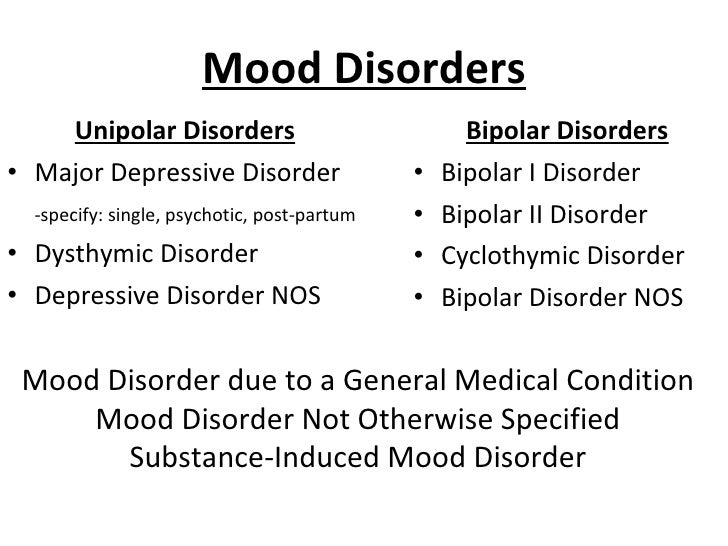 It is difficult for him to think and formulate statements. nine0003
It is difficult for him to think and formulate statements. nine0003
Hallucinations and delusions are usually absent. Often there are overvalued ideas of one's own guilt, uselessness, uselessness, fatal inadequacy and inadequacy. There is a tendency to self-abasement and self-accusation. The future looks bleak, hopeless, unpromising. Some patients consider some of their own previous actions as a serious crime. Many patients have thoughts of suicide, suicide attempts are possible. Sometimes (mainly in older patients) alcoholic depression is combined with increased anxiety. nine0003
Alcoholic depression is differentiated from other depressive disorders and conditions that include individual symptoms of depression. Unlike a depressive disorder, "drunken grief" is not accompanied by a sense of the colorlessness of the world and the loss of the ability to feel a variety of emotions. This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.
Separate elements of depression are often observed in withdrawal syndrome, but, unlike real alcoholic depression, they disappear after abstinence from drinking alcohol for 1-3 days. Reactive depression on the background of alcoholism in patients develops against the background of severe traumatic events (death of a relative, divorce, etc.); with alcoholic depression, there are no such events in the recent past of patients. Alcohol intake can provoke an exacerbation of other mental illnesses (psychogenic depression, depressive phase of bipolar affective disorder), therefore, when affective symptoms appear in patients with alcoholism, a thorough history taking is necessary. nine0003
Treatment and prognosis for alcoholic depression
Treatment of depression in alcoholism is carried out in a narcological hospital. In the process of treatment, drugs, psychotherapy and non-drug methods are used. Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors). With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance. nine0003
With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance. nine0003
With early detection and timely hospitalization, the prognosis for alcoholic depression in most cases is relatively favorable. Single depressive episodes, as a rule, quickly stop, suicidal intentions disappear, working capacity is restored (if it was not impaired due to other diseases). However, if the patient continues to drink alcohol, these conditions may recur and worsen as alcoholism develops.
Treatment of mood disorders in Moscow. Symptoms, causes, methods
I tried spice and got hooked. When the parents found out, they immediately sent him for treatment. The clinic treated me very kindly. They quickly and clearly explained how quickly I could lose my health. Now I understand how careless and stupid I was. I am very grateful to the doctors and my family.
Now I understand how careless and stupid I was. I am very grateful to the doctors and my family.
Yaroslav
This spring, a tragedy happened in my family. For a long time and constantly drinking, her husband began to become an inveterate drunkard catastrophically quickly. This threatened the loss of a job, the loss of everything that was earned by a long and successful service - authority, respect from colleagues, friends, family, and most importantly, physical and mental health. We turned to the Unika+ clinic to get him out of the binge. They put the spouse in the clinic and prescribed a course of treatment. He has not been drinking for three months, he is in a good mood, he fulfills all the prescriptions of our doctor. Many thanks to the specialists of the clinic! nine0003
Tatyana
A close friend suffered from hard drinking for quite a long time - several years. There was no one closer to me. His wife left a long time ago, he did not communicate with the children. Barely managed to persuade to be treated. They called a doctor to the house, who advised to go to the clinic. I had to be transported to the clinic by hospital transport, accompanied by a narcologist. Thanks to the staff. Treatment has not yet been completed, but strong progress is visible.
Barely managed to persuade to be treated. They called a doctor to the house, who advised to go to the clinic. I had to be transported to the clinic by hospital transport, accompanied by a narcologist. Thanks to the staff. Treatment has not yet been completed, but strong progress is visible.
Alexandra
I am very grateful to the Lord God, my family and the staff of the clinic. It happened - I became a different person. But already at work they threatened with dismissal, and my wife endured my drinking with the last of her strength. They brought me here in a semi-conscious state. He left as a cheerful and self-confident person. nine0003
Anatoly
My niece is addicted to spice. Parents didn't notice right away. Were in shock. She persuaded me to go to the clinic. The doctors persuaded me to lie down, clean myself, and a psychologist Safarov Rustam (a specialist and just a good sympathetic person) joined in the process. After discharge, she herself asked to be like an outpatient monthly program. Everyone is happy. The girl was cured, thank you!
Everyone is happy. The girl was cured, thank you!
Dmitry
For a long time I did not want to admit to myself that I was addicted to alcohol. We often celebrate birthdays at work. I did not want to break away from the team. And rolled down the slope. Schoolchildren began to be ashamed of me. The wife signed up for a family consultation at the clinic. Finally, I came to my senses and realized: this should not continue. He stayed in the clinic for 5 days, and went on an outpatient basis for 3 days. Many thanks to the staff - Natalya Alexandrovna Koshel, Rustam Zelemkhanovich and all the junior staff for their professionalism and goodwill. The conditions are excellent. nine0003
Alexander
Wonderful clinic, attentive, pleasant staff, very helpful to people who find themselves in a difficult situation. The conditions in the clinic are comfortable. I express my gratitude to Mikhail Vasilievich, he is a doctor from God, I recommend!
Valery
I would like to express my gratitude for the warm attitude of doctors and staff to our patients, I am very grateful for the comfort and good care of my brother, whom we sent to you for treatment.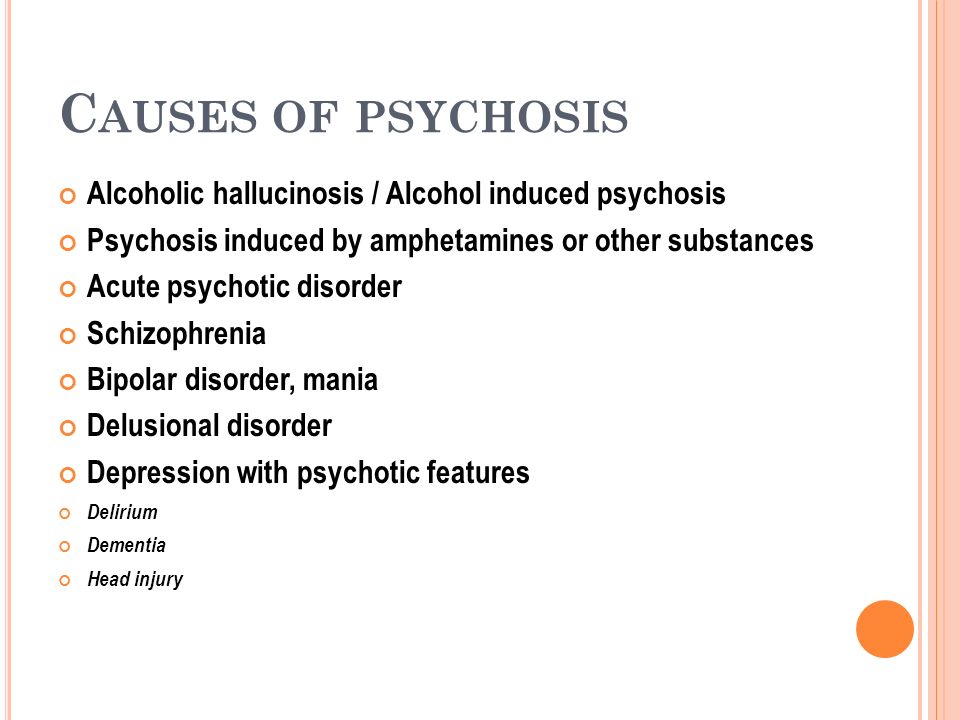 Many thanks to his doctor Natalya Anatolyevna, for saving me, you give a second life. Thank you! nine0003
Many thanks to his doctor Natalya Anatolyevna, for saving me, you give a second life. Thank you! nine0003
Evgenia
Thank you very much to the clinic for the individual approach to my son and professional treatment. I also want to thank the doctor Krasilnikov Dmitry Sergeevich. The son entered the clinic in poor condition, drinking alcohol for about 2 months somewhere. We received urgent professional and psychological assistance. We are 100% satisfied with the clinic. We will recommend you to our friends.
Maria
I would like to thank the doctors of the Unika+ clinic! Now that I'm all right, I want to leave a good review. In short: the first days I wondered why there is such a kind, homely attitude, it even surprised me. But the doctors really penetrate our problems, help, talk, I did not feel flawed, there was a desire to live. I completed the full course - 21 days. The days passed not so painfully, because you go for walks without any problems, talk with psychologists, get treatment and already start making plans.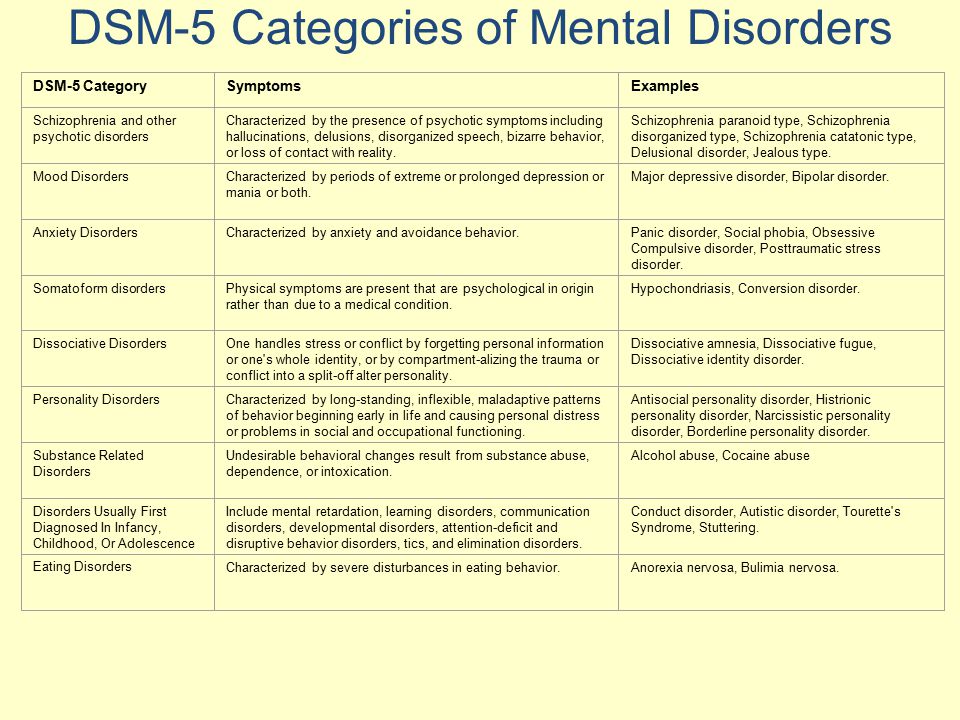 In general, undergo treatment and restore your life! nine0003
In general, undergo treatment and restore your life! nine0003
Michael
I am an alcoholic, yes I abused alcohol. Thanks to my relatives for getting me here on time, I would not have been able to stop it all myself. I have not regretted a single day that I went here for treatment. The experts were very helpful. Special thanks to psychiatrist Dadashev R.Kh. The doctor became like a family to me, as a person she is just wonderful, it was a pleasure to talk with her. She listened to me, asked questions, gave advice. If you want 100% results, then go see her! nine0003
Alexander
Thank you very much Dr. Saakov! I visited Alexander Arsenievich for the third time. His professionalism is visible, a very competent doctor, he always listens and gives competent recommendations, I am pleased to communicate with him! I trust my doctor, not for a second doubting the recommendations and prescribed medications, thank you!
Anna
I was treated at this clinic because I had problems with alcohol. There were problems with my husband, he cheated on me and only alcohol helped me. I thought so then. As a result, my husband brought me to the clinic. When I entered the clinic, it was scary. But the doctor was very kind and told me everything and reassured me. They put me on drips, the medical staff here is excellent. The psychologist Anatoly Maletsky came to me, I am very grateful to him for the psychological support. Many thanks to the clinic and the doctor. nine0003
There were problems with my husband, he cheated on me and only alcohol helped me. I thought so then. As a result, my husband brought me to the clinic. When I entered the clinic, it was scary. But the doctor was very kind and told me everything and reassured me. They put me on drips, the medical staff here is excellent. The psychologist Anatoly Maletsky came to me, I am very grateful to him for the psychological support. Many thanks to the clinic and the doctor. nine0003
Victoria
I want to say a huge thank you to all the medical staff, everyone treated our situation with understanding. Many thanks to Safarov Rustam Zelemkhanovich, because only thanks to his help we were able to save my husband. the doctor not only listened to me and my husband, but also helped us cope with our misfortune. People take care of yourself, do not use drugs! THANK YOU FOR EVERYTHING!
Yuliya
Thanks to the UNIQA clinic, you helped pull my friend out of the bottom and set him on the right path.