Adhd and obsessions
Am I Too Clingy, Insecure?
Obsessing and ruminating are often part of living with attention deficit hyperactivity disorder (ADHD). No matter how hard you try to ignore them, those negative thoughts just keep coming back, replaying themselves in an infinite loop. You know it’s not healthy, but you can’t seem to stop yourself.
It makes sense. As adults with ADHD, we’re so often burned by our own impulsivity that we sometimes go to the opposite extreme and micro-analyze. Our minds are always on, often running laps around the same track. So it’s no wonder you find yourself drawn to thoughts of your beloved and what he or she is up to when you’re not around.
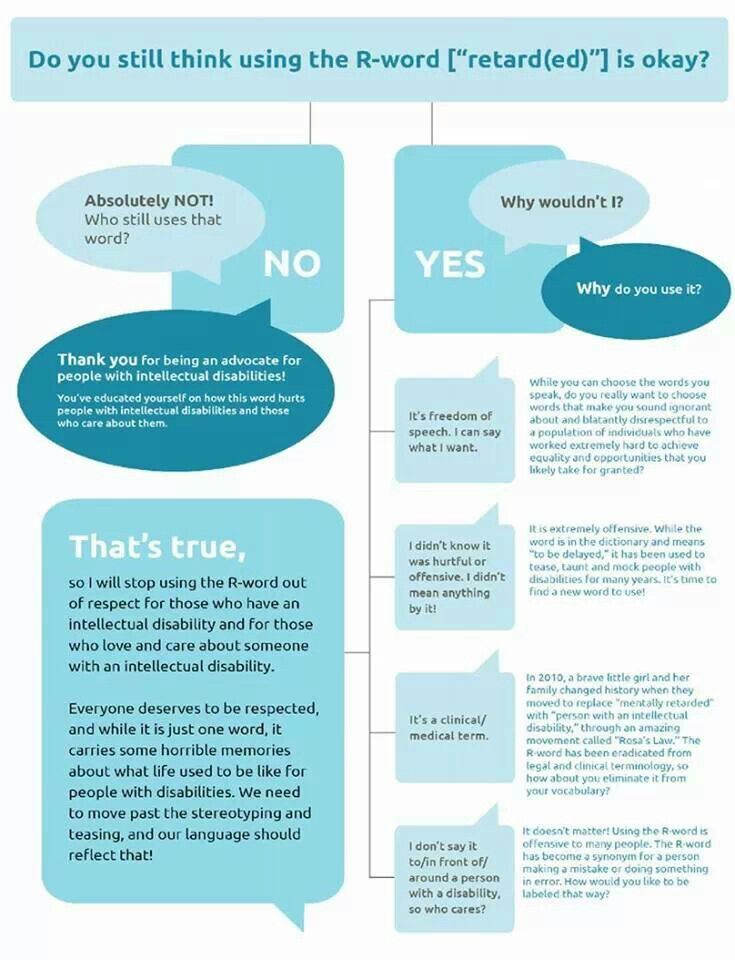
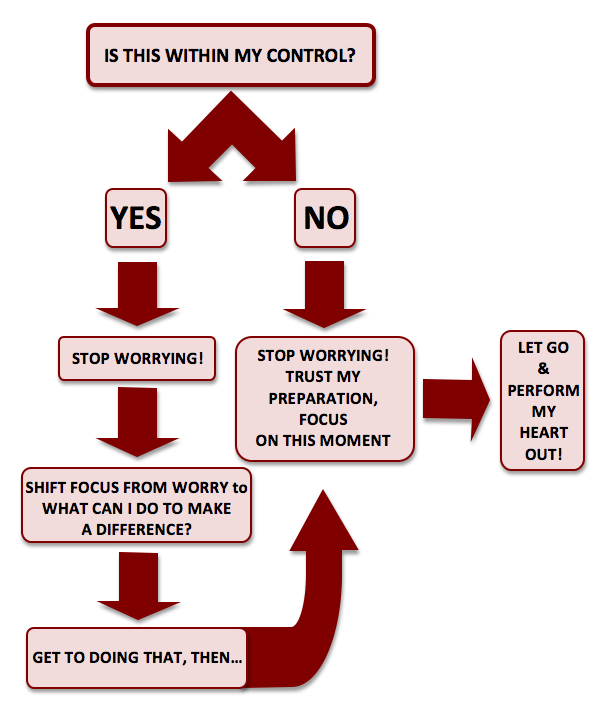
What you resist persists. The more you try to ignore these thoughts, the more persistent they become. Like many things related to ADHD, “just try harder” isn’t a solution. Here are some ideas that might work better:
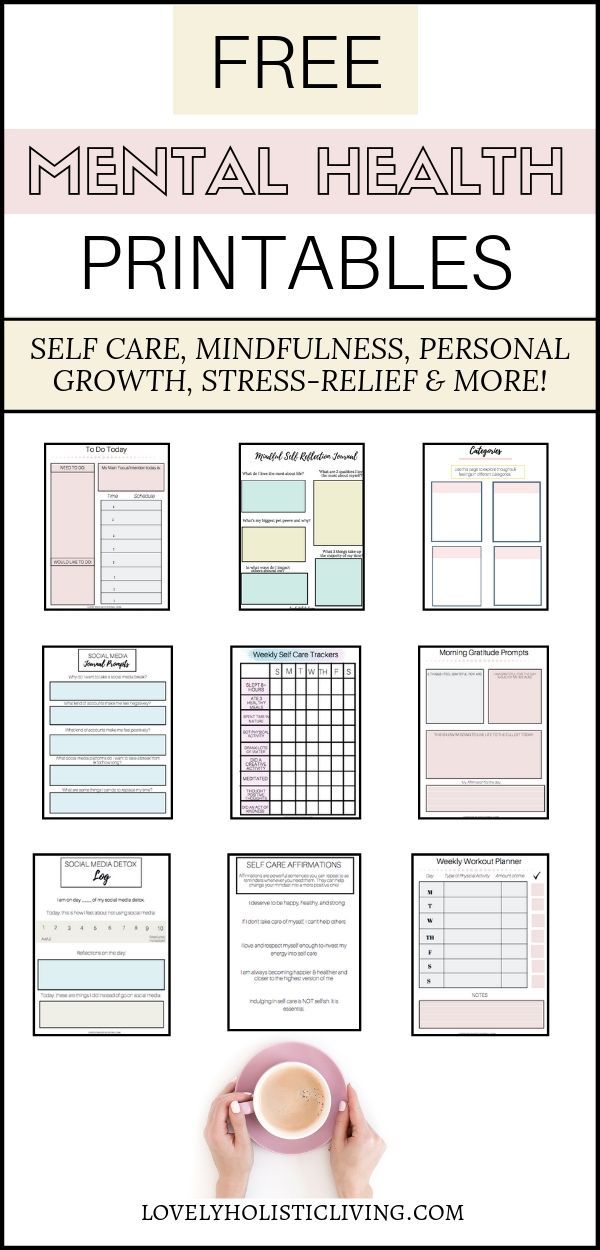
[Free Download: Get a Grip on Tough Emotions]
Journal. Putting those thoughts down on paper gives them a home, another place they can stick besides your brain. Also, the writing process puts you closer in touch with subconscious beliefs that may be the root of your concerns.
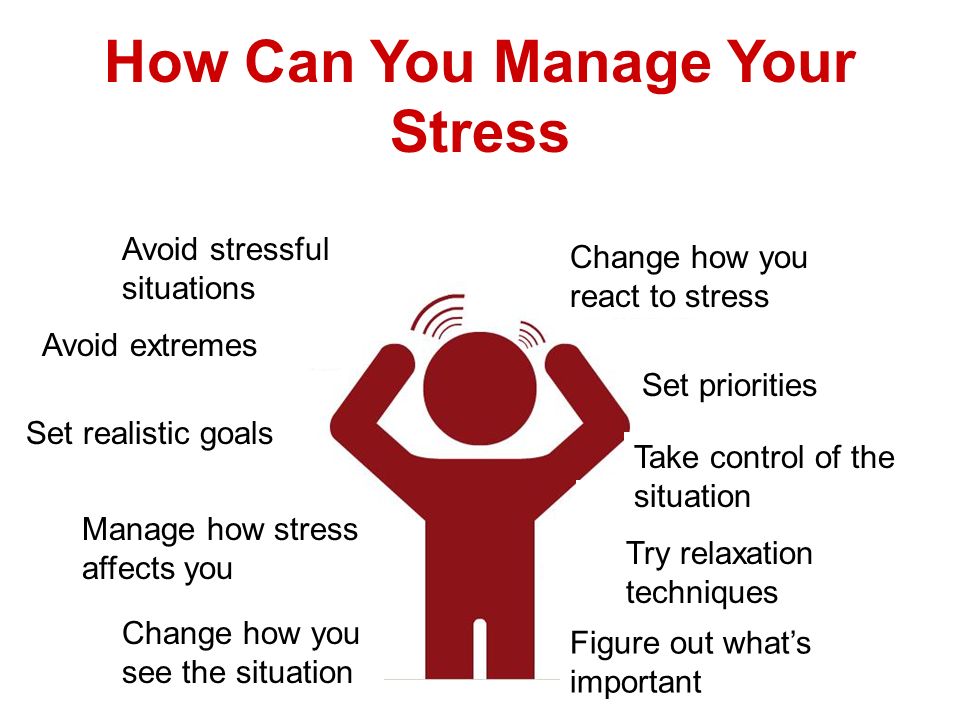
Focus on something outside of your mind. In other words, distract yourself by staying busy. Do something intense that you’re naturally drawn to — for example, playing a video game or mountain biking. You want it to be something that will captivate 100 percent of your attention. Doing something out in nature is particularly effective.
Write down the exact opposite of your concern and visualize it. For example, you might write, She’s at the mall, shopping for my birthday gift. Then play out that scene in your mind.
Change your thinking. Related to the above, decide in advance how you would like to view the situation. Then, whenever you find your thoughts turning negative, consciously replace them with the positive scenario.
[Free Webinar Replay: The ADHD-Anxiety Link: How Mindfulness Helps You Feel Less Overwhelmed and Be More Productive]
Repeat a mantra.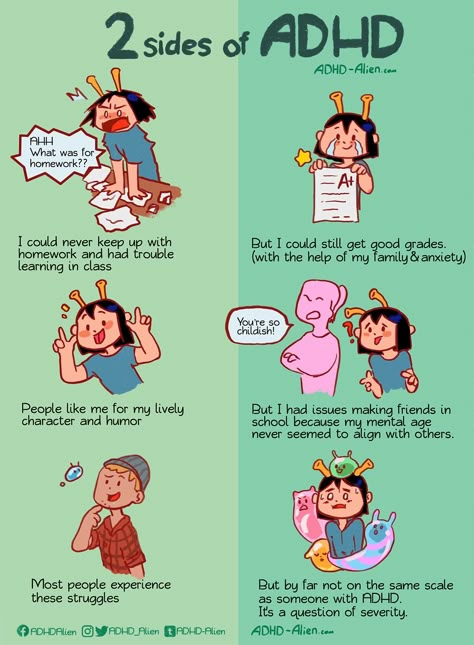 Think of a short, comforting phrase and repeat it over and over. Say it out loud. For example, “He is worthy of my trust,” or “I am a prize.” Successful mantras are both positive and believable. There’s no room for ruminations if you’re focused on your mantra.
Think of a short, comforting phrase and repeat it over and over. Say it out loud. For example, “He is worthy of my trust,” or “I am a prize.” Successful mantras are both positive and believable. There’s no room for ruminations if you’re focused on your mantra.
Of course, it’s entirely possible that your ruminations are not solely related to ADHD. The suggestions above assume that there are no underlying psychological issues, like childhood abandonment or abuse, or a painful past relationship. You’ll need to resolve these issues before you can move on. A therapist or other qualified mental-health professional can help.
[Hit the Panic Button: Stopping Anxiety Triggers in Their Tracks]
SUPPORT ADDITUDE
Thank you for reading ADDitude. To support our mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
Previous Article Next Article
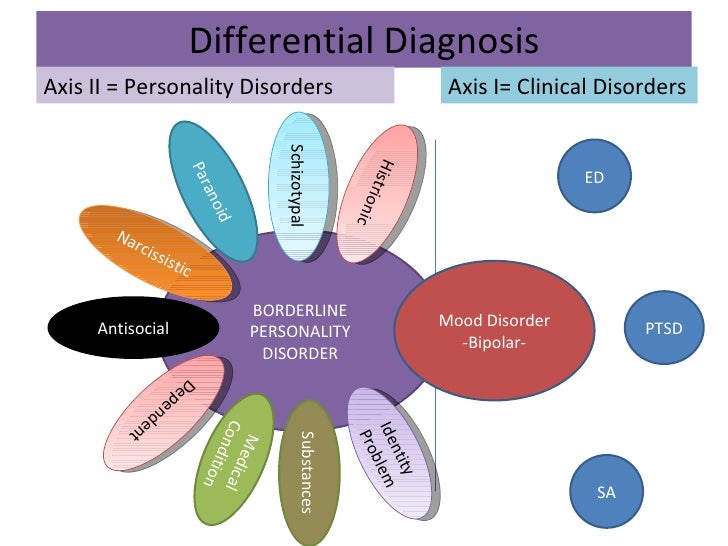
Unique Symptoms of Similar Conditions
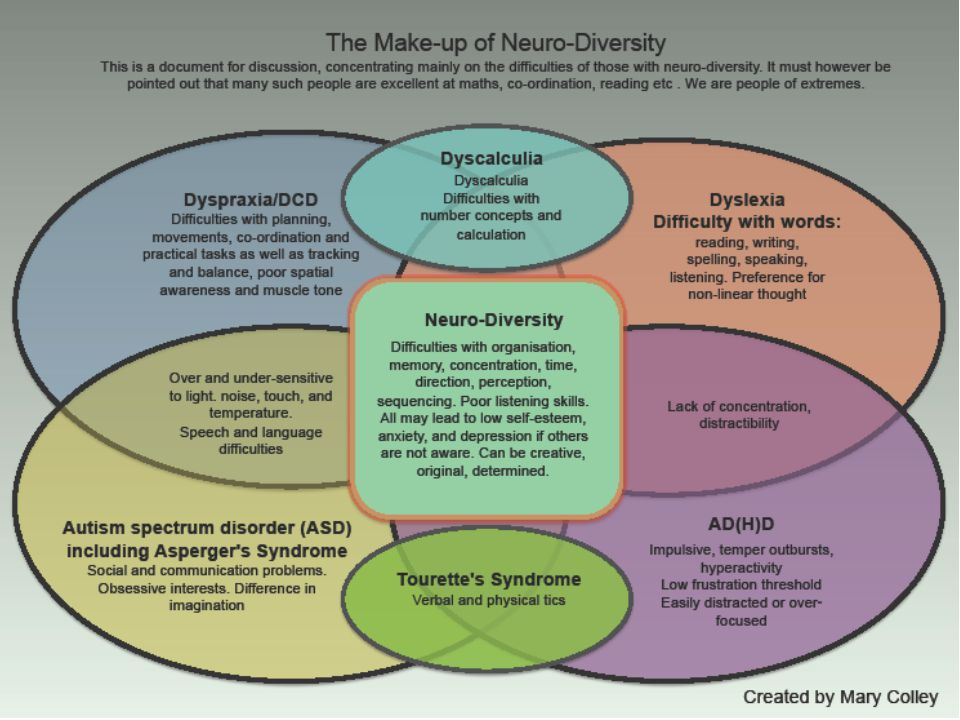
Some diagnoses of attention deficit disorder (ADHD or ADD) are more difficult to make than others. Because many disorders “look like” ADHD, it is not always easy to determine whether the hyperactivity and/or inattention and/or impulsivity is caused by ADHD or another condition called an ADHD comorbidity.
Because many disorders “look like” ADHD, it is not always easy to determine whether the hyperactivity and/or inattention and/or impulsivity is caused by ADHD or another condition called an ADHD comorbidity.
Thirty to 50 percent of individuals with ADHD also have a learning disability, difficulty regulating emotions (anxiety, mood disorder), anger, obsessive-compulsive disorder (OCD), and/or a tic disorder. It is essential to identify each problem and treat it appropriately.
Here is what you need to know about OCD and ADHD, including symptoms, so you can begin to differentiate the two.
Franklin’s OCD Story
Franklin’s symptoms highlight the diagnostic difficulties of discerning between OCD and ADHD.
I consulted with the 15 year old and his parents when he was in tenth grade. Franklin couldn’t stay on task and fidgeted in class, and while doing homework. At a recent school meeting, a teacher suggested that Franklin may have ADHD. Franklin’s parents had him examined by his family doctor, who started him on a trial of methylphenidate.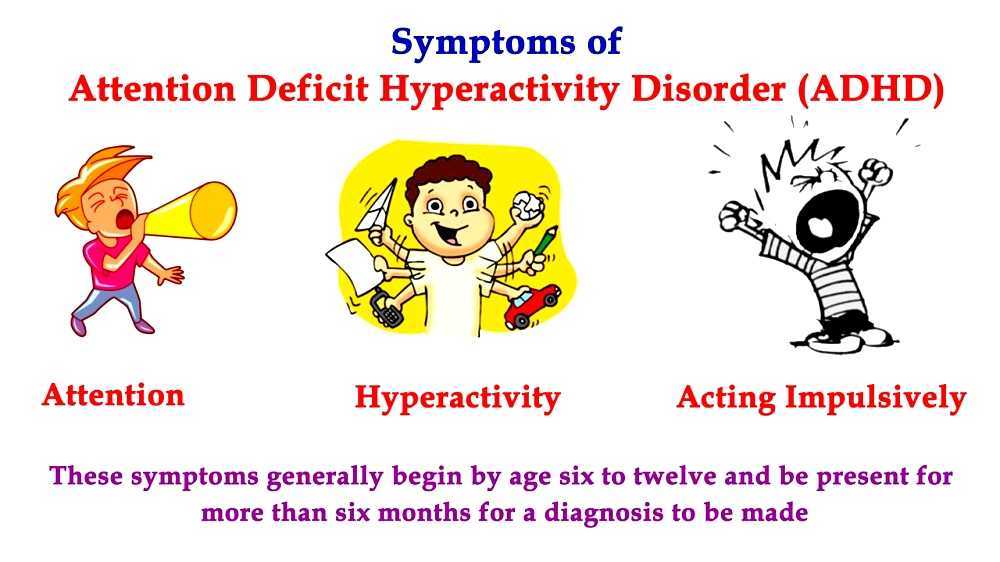 His problems got worse.
His problems got worse.
When Franklin visited with me, I discovered that his teachers and doctors had never asked him why he acted the way he did. He told me that he could not stop his behaviors.
[Self-Test: Could Your Child Have OCD?]
“I can’t start schoolwork until everything is in its place,” he said. He told me that his pen had to be at the top of, and parallel with, the desktop. The paper he wrote on had to be positioned at a 45-degree angle. He stacked books only on the right corner of his desk. He “had to” do these tasks.
“Sometimes it takes so long to get everything where I need it to be that I run out of time,” he said.
When he writes, each letter and word has to be formed perfectly. If it isn’t, he erases it and writes it again — and again. Sometimes the paper tears, and he has to start over. “Doing schoolwork in class or at home is exhausting,” Franklin said.
He went on to describe another frustration when he did homework. “I keep wondering whether I locked the front door before coming upstairs. I have to go down and see that it is locked — even if I know that I already checked.” Franklin told me that these behaviors started in fourth grade. He managed them well until high school, when written work started to overwhelm him.
I have to go down and see that it is locked — even if I know that I already checked.” Franklin told me that these behaviors started in fourth grade. He managed them well until high school, when written work started to overwhelm him.
Franklin’s OCD Diagnosis
Even though the minutes from his teachers’ conference strongly suggested that he had ADHD, I was fairly certain he had obsessive-compulsive disorder (OCD), a neurologically based disorder that causes anxiety.
[Learn OCD Management Tips in The Truth About Obsessive Compulsive Disorder]
Classroom teachers often interpret inattention and poor classroom performance as ADHD. Many teachers are familiar with the symptoms, but they may not know that a diagnosis requires that the observed behaviors be chronic and pervasive. Franklin’s behaviors were first noticed in middle school, and they occurred only when doing written work in class or homework.
When I met with Franklin and his parents to discuss my impressions, his mother was surprised.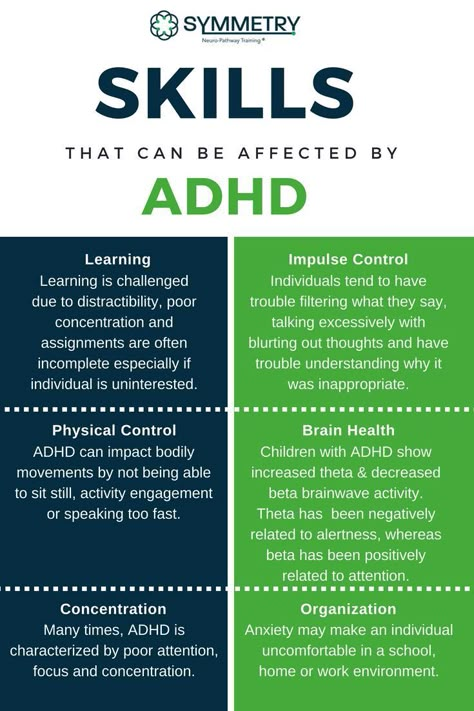 His father smiled and admitted that he had some of the same symptoms. I explained that the stimulant medication Franklin was taking for his misdiagnosed ADHD could make his OCD symptoms worse. I took him off the stimulant and put him on a selective serotonin reuptake inhibitor (SSRI). I also recommended that he see a cognitive behavioral therapist.
His father smiled and admitted that he had some of the same symptoms. I explained that the stimulant medication Franklin was taking for his misdiagnosed ADHD could make his OCD symptoms worse. I took him off the stimulant and put him on a selective serotonin reuptake inhibitor (SSRI). I also recommended that he see a cognitive behavioral therapist.
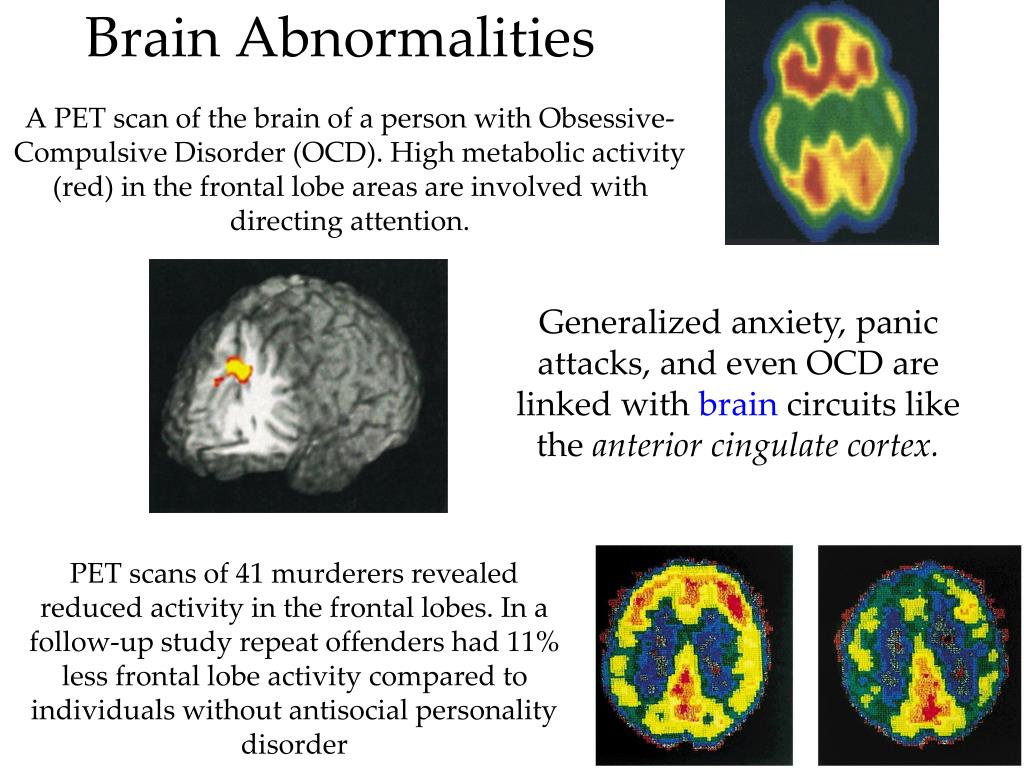
What to Know About OCD
OCD is a neurologically based disorder characterized by recurrent, unwanted thoughts (obsessions) and/or repetitive behaviors (compulsions) that the child realizes are senseless. OCD may start at age five or six, sometimes even earlier. OCD results from a deficiency of a neurotransmitter, serotonin, in specific areas of the brain. (New research suggests that the more severe forms of the condition, in which obsessive thoughts “lock” and cannot be relieved, involve more than a neurotransmitter shortfall.) OCD is treated with an SSRI, which increases serotonin levels in the brain.
Obsessions can take many forms: repetitive words, thoughts, fears, memories, pictures. Compulsive behaviors, such as hand-washing, counting, checking, or cleaning, are performed in hope of preventing obsessive thoughts or making them go away. Obsessions and compulsions are often viewed as being unnecessary, but they can’t be stopped. Although doing these “rituals” provides only temporary relief, not doing them dramatically increases anxiety.
Compulsive behaviors, such as hand-washing, counting, checking, or cleaning, are performed in hope of preventing obsessive thoughts or making them go away. Obsessions and compulsions are often viewed as being unnecessary, but they can’t be stopped. Although doing these “rituals” provides only temporary relief, not doing them dramatically increases anxiety.
OCD and ADHD
It is not uncommon for someone to have both ADHD and OCD. Since the presenting behaviors might look the same, it is important to know whether both problems exist.
For reasons that are not known, stimulant medications may exacerbate an existing case of OCD. Or, if the OCD behaviors are minimal and not obvious to parents, a stimulant may make them clinically apparent. The first clue that someone has ADHD and OCD — or may have OCD rather than ADHD — is a significant increase in OCD behaviors after taking a stimulant medication.
If you or your child has both conditions, it is best to treat the OCD first. Once these behaviors are under control, the stimulant can often be reintroduced without causing a flare-up of the OCD behaviors. If you think that your son or daughter may have ADHD and OCD, see a professional who understands the concept of treating someone with more than one disorder.
Once these behaviors are under control, the stimulant can often be reintroduced without causing a flare-up of the OCD behaviors. If you think that your son or daughter may have ADHD and OCD, see a professional who understands the concept of treating someone with more than one disorder.
Common OCD Obsessions
The most frequent worries in children and adolescents are about picking up germs and becoming sick or dying, or about getting sick and throwing up. Other fears include: If I don’t act/do a specific behavior: I will lose someone’s love; I will fail a test; God may punish me; a natural disaster will occur.
Common OCD Compulsions
Counting or repeating: the need to touch something a certain number of times; the need to repeat a specific behavior or pattern of behaviors
Checking or questioning: the need to check and recheck something (e.g., whether the stove is off, the car keys are on the key rack, the closet light is off)
Arranging and organizing: the need to tie shoes or to dress or undress in a certain sequence; the need to organize toys, dolls, or other items in a certain way; becoming upset if anything is changed
Collecting or hoarding: saving books, magazines, ticket stubs, birthday cards, or other items in the belief that they are important and cannot be thrown away
Cleaning and/or washing: the need to lather and rinse an exact number of times in the shower or to brush one’s hair a certain number of times in a pattern
“Preening”: behaviors that “must be done,” even if the result is discomfort or pain. Examples are nail or cuticle biting, picking at sores or scabs, twirling or pulling hair, eye-brows, or eyelashes, “cleaning off” dry skin.
Examples are nail or cuticle biting, picking at sores or scabs, twirling or pulling hair, eye-brows, or eyelashes, “cleaning off” dry skin.
Previous Article Next Article
How to remove obsessive thoughts from the head?
Researchers at the University of Texas have studied how different ways we control our thoughts affect the content of working memory. They conducted three experiments in which they found that consciously suppressing negative thoughts is the best strategy to clear working memory. This study, published in Nature Communications, may provide new tools for the treatment of a variety of disorders, including rumination, attention deficit hyperactivity disorder (ADHD), and various types of anxiety. nine0004
Credit: public domain
Our thoughts are processed in working memory. Here we add and subtract, compare and connect. At the same time, how effectively we use working memory depends on how successful we will be in life.
Here we add and subtract, compare and connect. At the same time, how effectively we use working memory depends on how successful we will be in life.
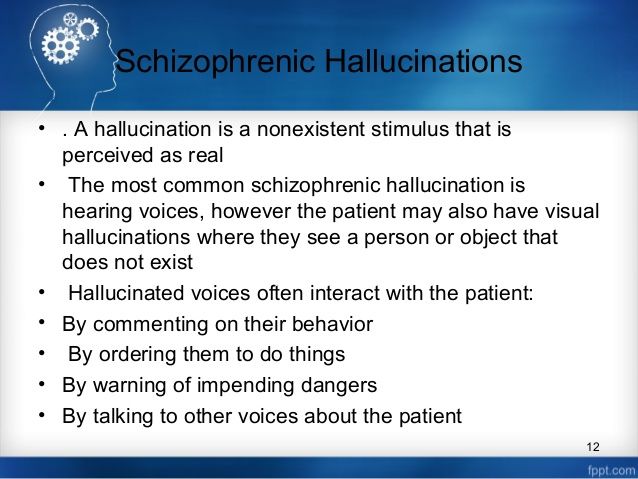
One of the important functions of working memory is renewal. It allows us to forget unnecessary information, thereby freeing up our cognitive resource for other thoughts and actions. Sometimes this feature messes up. We fail to successfully update thoughts in working memory, which causes them to repeat over and over again. We cannot forget them. The same thought is running through my head. If this thought is also emotional, then it negatively affects us. This disorder is called rumination (obsessive thoughts). nine0009
It turns out that a person loses the ability to control his working memory, control his thoughts. And problems with controlling the contents of working memory can cause attention deficit hyperactivity disorder (ADHD), lead to depression, anxiety disorders, obsessive-compulsive disorder.
Forgetting in working memory is associated with the activity of the prefrontal cortex - that part of the brain that is responsible for the conscious control of our activity, for the inhibition of our thoughts. To forget a negative thought, the prefrontal cortex can suppress it, replace one thought with another, or clear the entire contents of working memory. nine0009
To forget a negative thought, the prefrontal cortex can suppress it, replace one thought with another, or clear the entire contents of working memory. nine0009
Scientists decided to investigate how the brain inhibits thought. In three experiments, they studied three operations that we can use to control thoughts: suppression, replacement, and purification.
The first experiment was to understand how each operation affects the neural activity of the brain. During the second, it was necessary to characterize the success of each operation (that is, how much brain activity associated with an unwanted thought decreases). Finally, the third assessed how controlling our thoughts affects subsequent behavior. nine0009
Number one
In a functional MRI, scientists asked participants to remember three categories of images: faces, fruits, or scenes. Participants saw the images and then held them in their imagination (i.e. working memory). This allowed scientists to see the brain activity associated with a particular memorized category.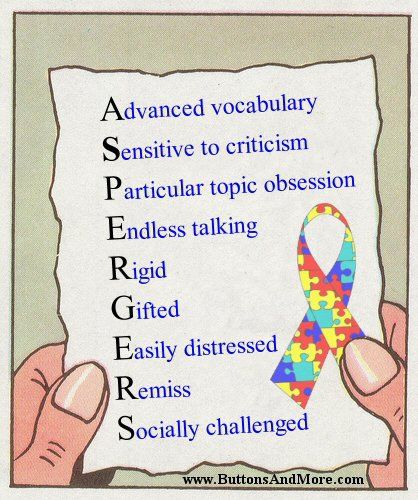
Detection of neural representation of mental images . Credit: Kim, H. et al./ Nat Commun 2020
The researchers were then asked to perform one of four operations with these stimuli: continue to hold the image in the head, replace it with another mental image (from another category: if we kept the face in the head, we should have replaced it with the image of a fruit), suppress or clear the working memory of all thoughts.
Scheme of the first experiment . Credit: Kim, H. et al./ Nat Commun 2020
Comparing patterns of brain activity, scientists have noticed that cleansing and replacing operations take a thought out of focus while keeping it in working memory. The neural activity for these operations dropped back to baseline faster than if the participant had continued to hold the image in their head. The strategy of thought suppression, on the contrary, weakened it, thus freeing up the possibilities of working memory for encoding other information.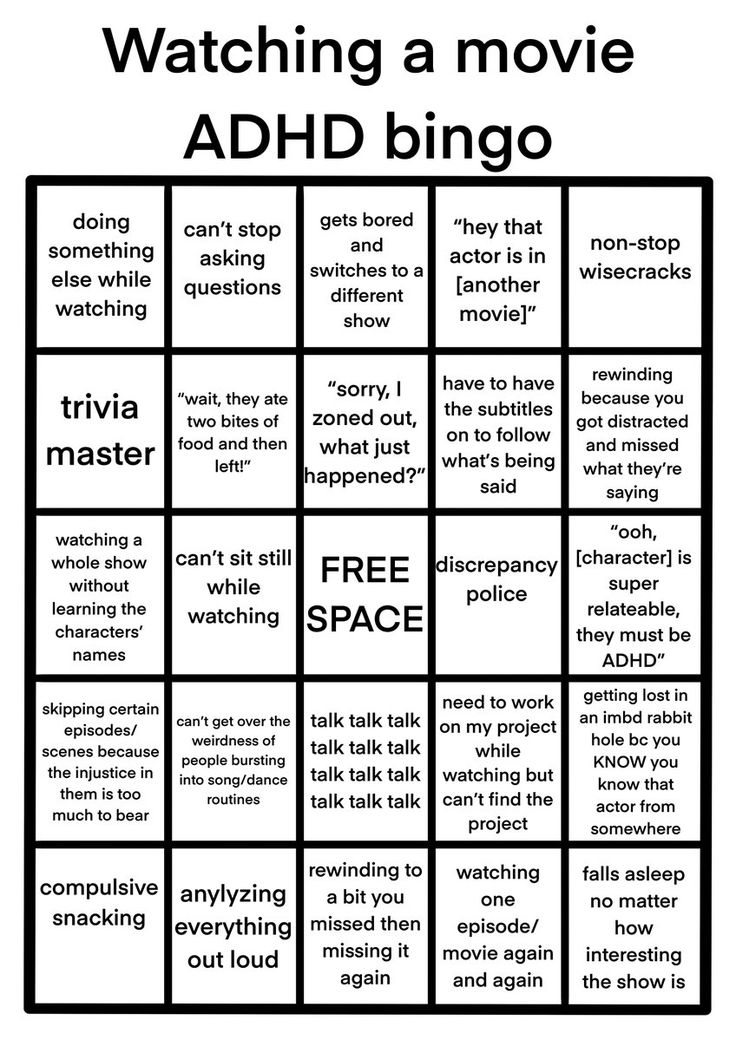 nine0009
nine0009
Dynamics of neural encoding of an element in working memory . Credit: Kim, H. et al./ Nat Commun 2020
Obviously, each of the thought control operations had its own temporal dynamics. The graph clearly shows that the dynamics of neural activity during the replacement of one information with another (old) is similar to that which was during the retention operation. Paradoxically, when a thought was replaced with new information, the neuronal dynamics of the operation corresponded to that during suppression or purification (gray line) - at first there was a slight increase, after which there was a decrease in activity. It turns out that both mental substitution and suppression are active processes that require the brain to detect the target thought and keep it out of focus. It's not a simple exclusion of this thought from the neural activity of working memory. nine0009
Number two
The second experiment allowed scientists to answer the question, can these strategies remove a thought from working memory?
Here, scientists examined the impact of each operation on subsequent memorization.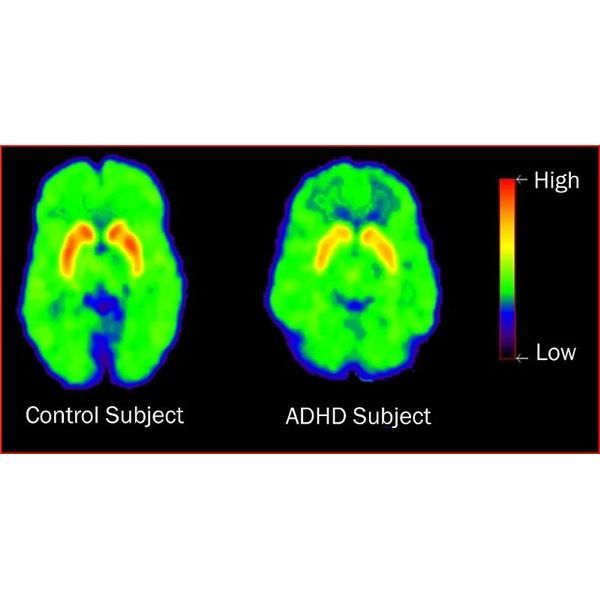 The logic was extremely simple: based on the theory that more or less the same neural networks encode the same information, it can be assumed that if a person turned off some thought, but it is still in working memory, then it will prevent us from remembering the same material in the future. This phenomenon is called proactive interference, when previously learned information affects the next (increasing the number of errors during playback and playback time). If the thought is not in working memory, then no problems arise in memorization. nine0009
The logic was extremely simple: based on the theory that more or less the same neural networks encode the same information, it can be assumed that if a person turned off some thought, but it is still in working memory, then it will prevent us from remembering the same material in the future. This phenomenon is called proactive interference, when previously learned information affects the next (increasing the number of errors during playback and playback time). If the thought is not in working memory, then no problems arise in memorization. nine0009
The only operation that did not result in proactive interference was suppression. Apparently, only suppression really removed the thought from the content of working memory.
Influence of mental control operations on memorization . Credit: Kim, H. et al./ Nat Commun 2020
Paradoxically, suppression is what alters neural activity in a way that allows us to effectively clear our working memory.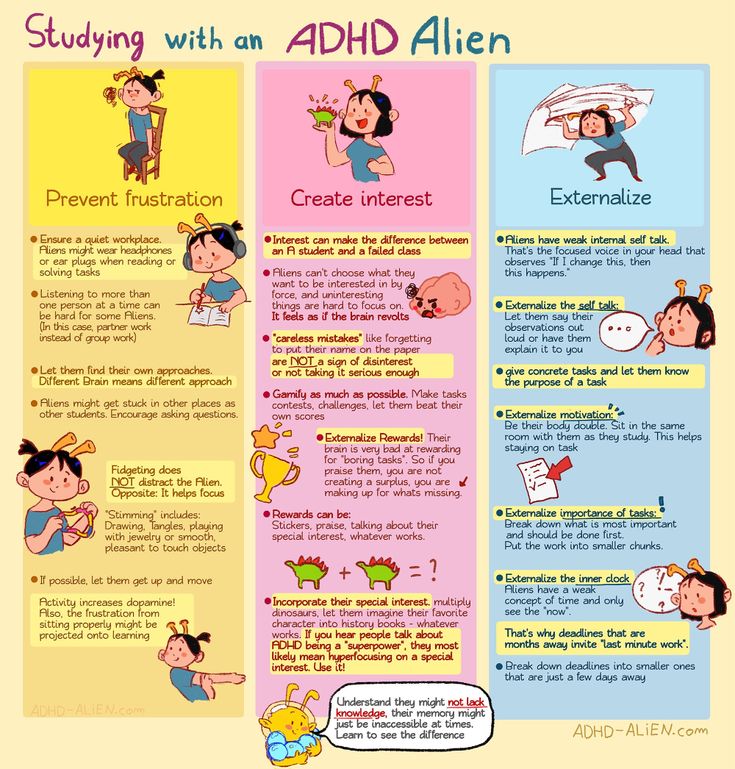 And this is because repression is an active process, as explained earlier. For a thought to actually leave working memory, it is not enough to deactivate it. It is necessary first to isolate this thought, to identify it in working memory. nine0009
And this is because repression is an active process, as explained earlier. For a thought to actually leave working memory, it is not enough to deactivate it. It is necessary first to isolate this thought, to identify it in working memory. nine0009
Number three
The question remains: how does controlling our thoughts affect subsequent behavior? To do this, scientists examined the impact of each of the operations on decision making. Participants sat in front of a screen on which they were shown two images (a face and a stage). After a while, the images would disappear and a hint would appear. She said what a person needs to do (hold, suppress, replace, and so on) with the information that was previously in the place of the clue. Then one of the images reappeared on the screen. The participant was supposed to answer as quickly as possible whether this stimulus was shown at the beginning of the experiment or not. nine0009
Scheme of the third experiment .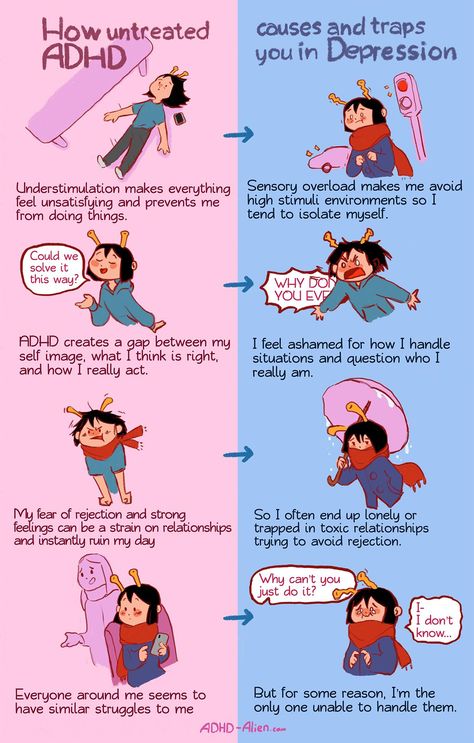 Credit: Kim, H. et al./ Nat Commun 2020
Credit: Kim, H. et al./ Nat Commun 2020
As expected, when the mental image had to be held, response time was shorter than when the image had to be suppressed.
It turns out that if the participant continued to keep the image in his head or replaced it, he activated it more quickly if necessary. But when suppressed, the participant needed more time to remember the image. This confirms that suppression reduced the influence of thoughts on our decisions. nine0009
“Ignoring does not free us from the influence of negative thoughts. You can temporarily distract yourself from the thought by turning your attention to something else, try to clear your mind. However, none of these strategies will get rid of the thought itself. Our study suggests that in order to discard a thought, you must first activate it, find it in memory, and only then will you have the opportunity to get rid of it, suppress it, ”says Jerred Lewis-Peacock, lead author of the study.
nine0004
The results of the study show the role of working memory in emotional control, its important place in the study of diseases that disrupt the normal flow of thoughts. Suppression removes negative memories from working memory. This can be a good way to stop rumination, interrupt strange disturbing thoughts and images.
Text: Nikita Otstavnov
Changes to information in working memory depend on distinct removal operations by Kim, H., Smolker, H.R., Smith, L.L. et al. Nat Commun11, 6239 (2020).
https://doi.org/10.1038/s41467-020-20085-4
causes, symptoms, diagnosis and treatment of attention deficit hyperactivity disorder
. It is important to understand when the cause of "unworthy" behavior is the child's temperament, age crises or the result of upbringing, and when a serious diagnosis is attention deficit hyperactivity disorder (ADHD). nine0009
As a rule, the diagnosis is made by a neurologist after complaints from parents or teachers, and medical and corrective treatment is prescribed. In this case, it can last for years and require constant renewal, as often happens in traditional medicine.
In this case, it can last for years and require constant renewal, as often happens in traditional medicine.
Osteopathic practitioners look at ADHD from a different perspective, identifying and eliminating the source of the disease irrevocably. This happens due to the restoration of the position of the bones of the skull and the removal of barriers to the proper nutrition of the brain. nine0009
Symptoms of ADHD in a child
ADHD is classified as a neurological-behavioral disorder. In the latest version of the International Classifier of Diseases, the disorder is registered as a separate diagnosis under the number 6A05 with subparagraphs depending on the predominance of certain manifestations.
The signs of ADHD make themselves felt already in early childhood. However, the diagnosis is usually not made to children younger than 3 years, since these signs are quite natural in babies.
In schoolchildren and preschool children, the syndrome is marked by the following features:
- Difficulties with directing and keeping attention on tasks, object, information;
- Disinhibition, senseless actions, chaotic hand movements, need to grab something, fidgeting and desire to get up from a chair;
- Forgetfulness, distraction;
- Delayed psycho-social, intellectual development;
- Impulsiveness and emotionality, sometimes aggressiveness.

These disorders in childhood lead to problems with adaptation in preschool, at school - to poor academic performance and constant violations of discipline. Schoolchildren suffering from this syndrome find it difficult to sit through a lesson, memorize information, perform tasks that require thoughtfulness and perseverance. In a team, children with ADHD demonstrate violations of the rules of behavior: they take other people's things, skip the queue, interrupt teachers, and sometimes they are whiny and capricious.
Patients with ADHD may be predominately attention deficit (more common in girls) or hyperactivity (more likely to be boys). In general, the symptoms are mixed. nine0009
Early childhood, and especially infancy, is the best time for osteopathic treatment. You don't have to wait until a diagnosis of ADHD is made to see a specialist with disturbing symptoms. The younger the children, the more likely it is to eliminate brain disorders permanently and with less time.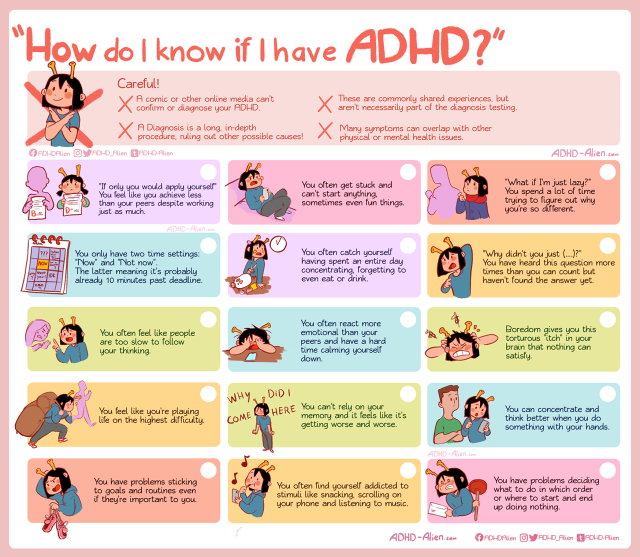 Do not rely on spontaneous recovery.
Do not rely on spontaneous recovery.
ADHD is not only a problem for children. In adolescence, the syndrome is exacerbated by changes in hormonal levels, uneven acceleration of the growth of body parts. Socialization, self-knowledge, new emotions and a great mental load are also added here. Puberty is already considered one of the most difficult life periods, and complicated by hyperactivity and absent-mindedness, it often pushes boys and girls into the abyss of depression and rash acts. nine0009
In adults, impairments persist but may be less pronounced. Mature thinking allows you to adhere to socially desirable norms of behavior, restrain impulsiveness and emotions. Some children outgrow the syndrome, but more than half of the adults, having not received adequate treatment in time, live with impaired attention and other related problems:
- Difficulties with planning, motivation, goal setting, decision making;
- Infantilism, irresponsibility; nine0004
- Tendency to depression, addictions;
- Inability to build long-term relationships, affective behavior and conflict in communication;
- Obsessive thoughts.
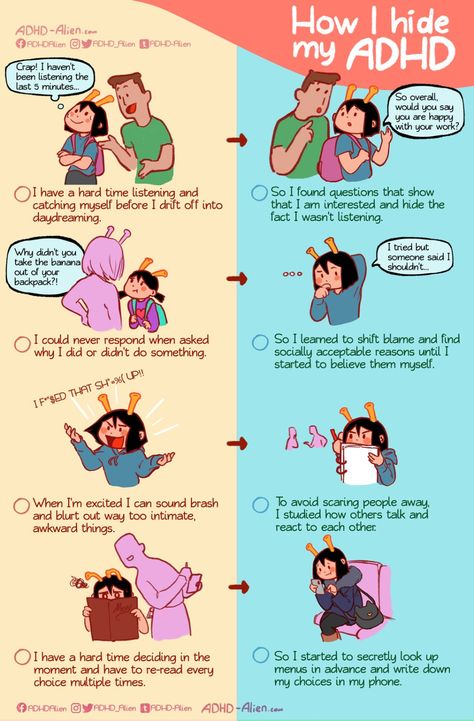
Sometimes ADHD makes itself felt for the first time in the period of growing up after a completely prosperous childhood. Hyperactivity is no longer so pronounced.
Almost always, various spheres of life suffer, a person is “in the clouds”, is not able to properly perceive and process information, generate new ideas. During work, he is constantly distracted, but he does not know how to fully relax, he tends to involuntarily switch his attention to minor details. nine0009
ADHD is rare in adults. Artificial suppression of emotions and a sense of guilt for failures lead to discord with oneself and neurosis, to low self-esteem (this can start from childhood). Approximately 20% of patients lead an asocial lifestyle.
History of the study of ADHD
Hyperactivity has been recognized as a disease relatively recently, but even now disputes about the existence of such a diagnosis do not subside. For a long time, symptoms were considered simply personality traits. In the middle of the 19th century, a German neuropsychiatrist first drew attention to the problem of hyperactivity in children, describing in his works a very active boy known as “Fidget Phil”. nine0004
In the middle of the 19th century, a German neuropsychiatrist first drew attention to the problem of hyperactivity in children, describing in his works a very active boy known as “Fidget Phil”. nine0004
Subsequently, foreign scientists actively studied this pathology along with other anomalies among children and adolescents that interfere with learning and socialization.
Gradually, neurologists from different countries agreed that ADHD is a minimal brain dysfunction, and not at all a problem of raising children. Since 1947, the disease has been officially recognized by medical experts; at least 100 manifestations have been identified that are regularly observed by parents, teachers and doctors in children with this diagnosis. nine0009
In the 1970s, domestic neurologists and pediatricians took up the problem of “difficult” children. International standards for criteria and diagnostics have emerged.
Causes of hyperactivity and attention disorders
The disease is based on physiological prerequisites:
- genetic aspects, heredity.
 It often turns out that parents, more often mothers of patients, had or have similar symptoms, are prone to stress and increased anxiety;
It often turns out that parents, more often mothers of patients, had or have similar symptoms, are prone to stress and increased anxiety; - Complicated pregnancy, chronic or acute maternal illness, drugs, alcohol, smoking;
- Intrauterine infection of the fetus, perinatal hypoxia;
- Unfavorable delivery: asphyxia, long waterless period, use of obstetric benefits;
- Severe infectious diseases in infancy, accompanied by an increase in the child's body temperature, traumatic brain injury in early childhood.
Other factors during gestation may also affect the formation of ADHD: environmental problems, excessive physical and emotional stress in the mother, malnutrition, stress.
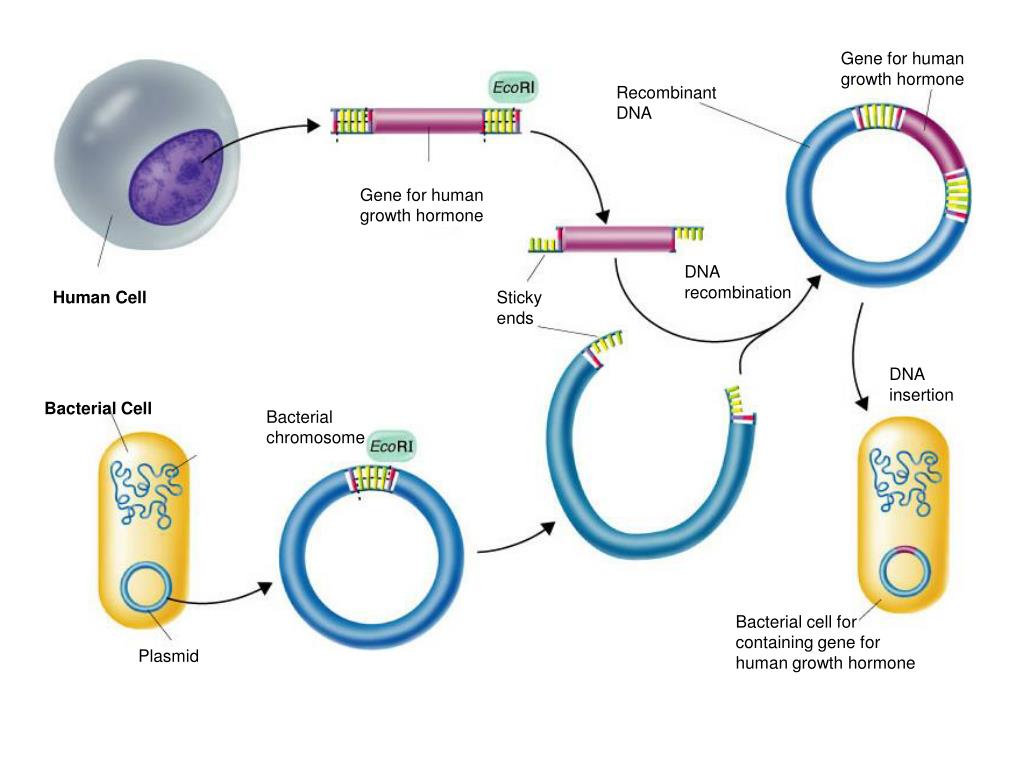
ADHD is based on a lack of bioactive neurotransmitter elements - dopamine and norepinephrine, in combination with CNS damage, which can result from any of the factors described above. Brain structures are damaged as a result of trauma, hypoxia or chemical, toxic poisoning.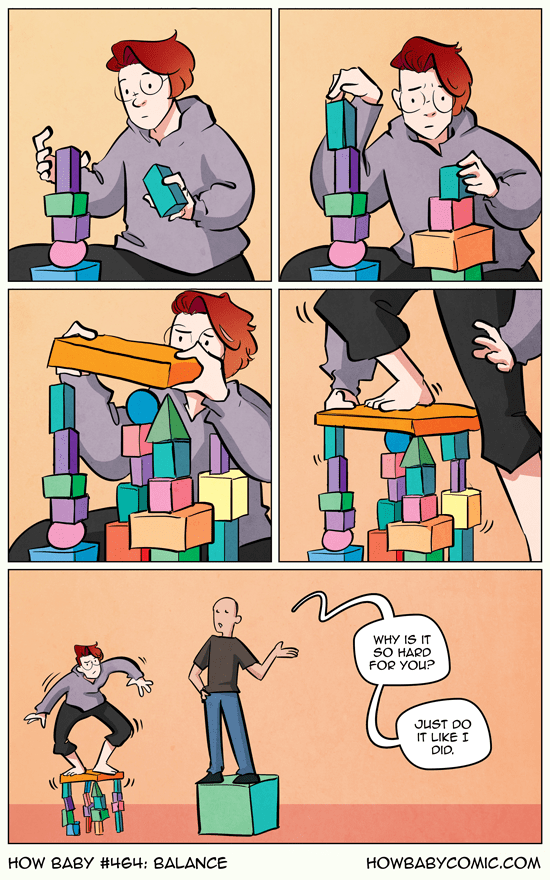 nine0009
nine0009
According to the results of an MRI study, which involved more than 3 thousand people at various ages, it was found that the brains of those suffering (half of the sample), although slightly, are smaller in size than those of healthy people. The data were published in the specialized British journal The Lancet Psychiatry. A number of other hardware studies have also revealed differences in the structure of the brain, which confirms the physiological nature of ADHD.
The following factors may exacerbate the manifestation of symptoms: tense atmosphere in the family, lack of attention from parents, excessive demands and punishments, lack of sleep and rest, lack of daily routine, prolonged exposure to a screen or display. nine0004
Heredity affects ADHD not only through genetics. Parents who are at the mercy of the syndrome are likely to raise their children accordingly. Unwillingness to be a parent, irascibility, disorganization - all this increases the disorder and shatters the already weak psyche of the child.
The development of ADHD in children provokes a complex of factors, some of which may become decisive, for example, birth trauma. Addressing the source of the problem early can prevent or alleviate future symptoms and avoid long-term treatment. nine0009
Diagnosis of ADHD
According to international statistics, the disorder is observed in an average of 5-7% of children, and these are only confirmed diagnoses.
Not every overly active child suffers from attention deficit hyperactivity disorder. There are noisy, inquisitive, sociable children with an explosive choleric temperament. Toddlers of the first years of life are simply not physically able to control themselves, and in school-age children, through these manifestations, perseverance, determination and leadership qualities can be formed. Children with ADHD are active aimlessly, their lives are filled with meaningless fuss. nine0009
An experienced eye can easily distinguish pathological hyperactivity from healthy children's activity.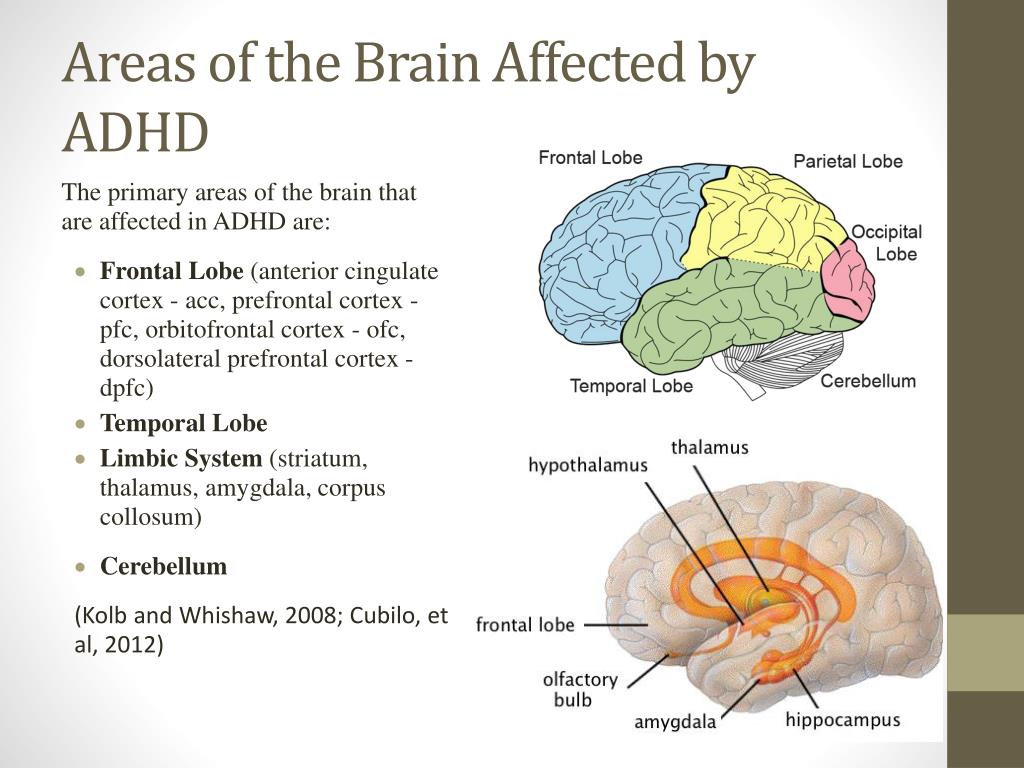
Another explanation for the impossibility of diagnosing ADHD in a 2-3-year-old child is the lack of observation of him in various conditions. If, according to the parents, he “is on his ears, and he is not interested in anything”, it is necessary to get comments from third parties - teachers in kindergarten, school. If for several months the symptoms persist in different situations, the stage of diagnostic procedures begins. nine0004
According to international classifiers, it is customary to officially diagnose the syndrome no earlier than 6-7 years. Recently, the age has decreased to 5.
First of all, organic or mental disorders with similar manifestations, exposure to alcohol, drugs and medicines, conscious demonstration of deviant behavior are excluded. The intra-family situation, the child's lifestyle, concomitant diseases are taken into account. Often, after a change in one factor, the condition returns to normal and the diagnosis changes. Or other diseases are detected. nine0009
nine0009
The examination is carried out on the basis of international documents, including the general classifier of diseases and the diagnostic manual for mental disorders. Diagnostic criteria vary, which is why the percentage of children with ADHD in Russia, according to official data, is lower than, for example, in the United States.
A child may be diagnosed with ADHD if symptoms persist in at least two different environments for six months. nine0004
The questionnaire according to the ICD-10 classifier consists of items for groups of symptoms: hyperactivity, attention deficit, impulsivity. It is necessary to match at least 3, 6 and 1 points for each group, respectively. There are no special diagnostic tools - laboratory, genetic or hardware - for making a diagnosis, it is made only on the basis of the results of an assessment of symptoms, observation, testing.
If disorders go beyond hyperactivity, absent-mindedness, accompanied by painful conditions, paroxysmal tantrums, this is a reason to suspect serious diseases (epilepsy, tumors) associated with the functioning and structure of the brain, and undergo a comprehensive examination.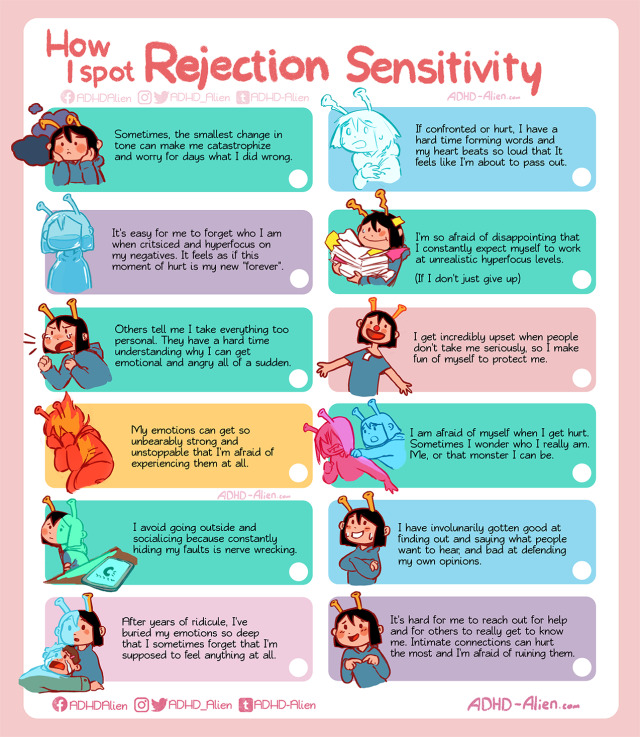 nine0009
nine0009
Despite the fact that a neurologist performs diagnostics and treatment, sometimes a consultation with a psychoneurologist, psychiatrist, psychologist, endocrinologist, ophthalmologist, etc. is required. There are diseases that symptomatically resemble ADHD: autism or ASD, schizophrenia.
Specialists can offer their own tests to differentiate between hyperactivity disorder and attention deficit disorder, send them to auxiliary examinations:
- blood test to determine lead poisoning; nine0004
- thyroid dysfunction test;
- EEG reading electrical impulses of the brain. In children with ADHD, beta and theta rhythms are elevated (which, however, is also found in other nervous disorders, as well as in a state of increased anxiety in healthy people). A 10-minute session is quite enough;
- MRI to assess neuronal function of the brain when solving a task and detecting an organic anomaly.
Treatment by an osteopathic doctor can eliminate the symptoms, and most importantly, the source long before the diagnosis is made.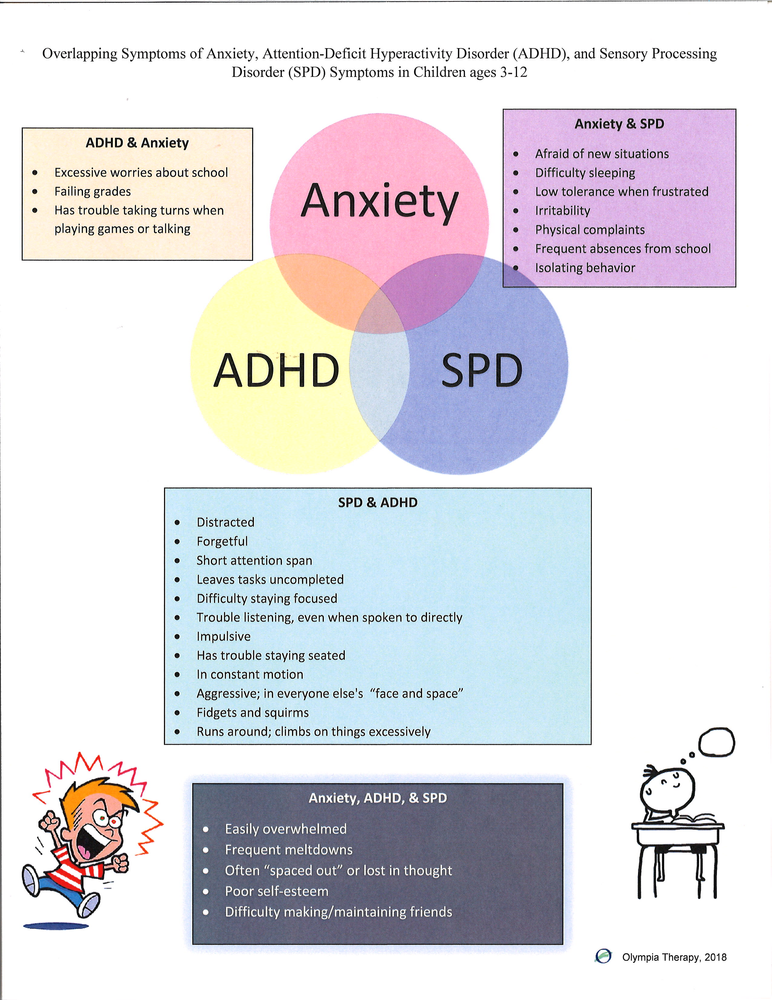 Traditional neurology suggests waiting for a conscious age, then observing for a long time, as a result, precious time is lost. An osteopath does not need diagnoses, therefore, with the appearance of the first alarming “bells”, you should visit him, especially if there were complications in the perinatal, birth and early postnatal periods. nine0009
Traditional neurology suggests waiting for a conscious age, then observing for a long time, as a result, precious time is lost. An osteopath does not need diagnoses, therefore, with the appearance of the first alarming “bells”, you should visit him, especially if there were complications in the perinatal, birth and early postnatal periods. nine0009
Mistakes in diagnosis can have sad consequences: a child with true ADHD is “missed out” without noticing his problems; aggravate the disorder with harsh methods of education; try to solve problems with learning or socialization without eliminating the source.
At the same time, other neurological and behavioral disorders often masquerade as hyperactivity or inattention. By blaming the symptoms on ADHD, there is a danger of missing another disease or being treated for a non-existent diagnosis. Perhaps it is enough to reduce the load, improve the intra-family atmosphere, improve nutrition and sleep. nine0009
The treatment of ADHD is complex.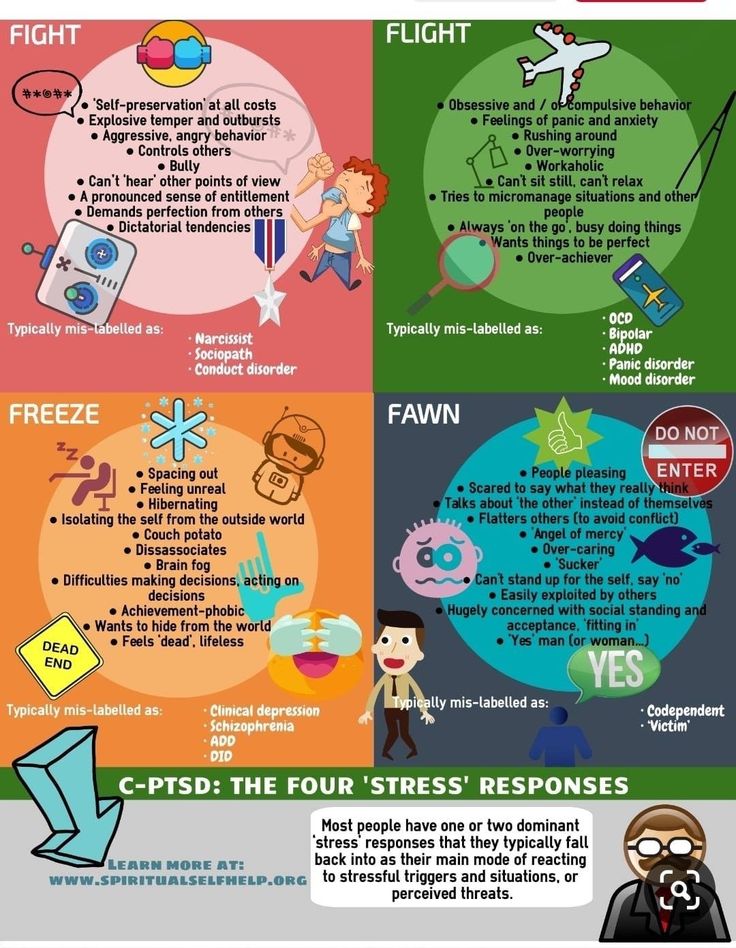
A neurologist in a traditional clinic prescribes treatment to a child, which includes three components: medications, group or personal therapy with a psychologist-defectologist to correct behavior and develop missing skills, and create favorable conditions. Relaxing techniques are recommended: massage, swimming.
The task of drugs is to suppress excitability, to activate brain activity. The effect is not always achieved or it is temporary. As a rule, there are a lot of side effects, including addiction. Potent drugs, especially for children, are prescribed with great care, constant monitoring by a doctor and dose control are necessary. Means with a softer spectrum of action do not bring noticeable results. nine0009
Children with ADHD rarely feel better, this gives only a temporary respite for them and others, but any external circumstance, life changes, troubles or the most common infectious disease can cancel out the results achieved.
ADHD is not considered to be curable.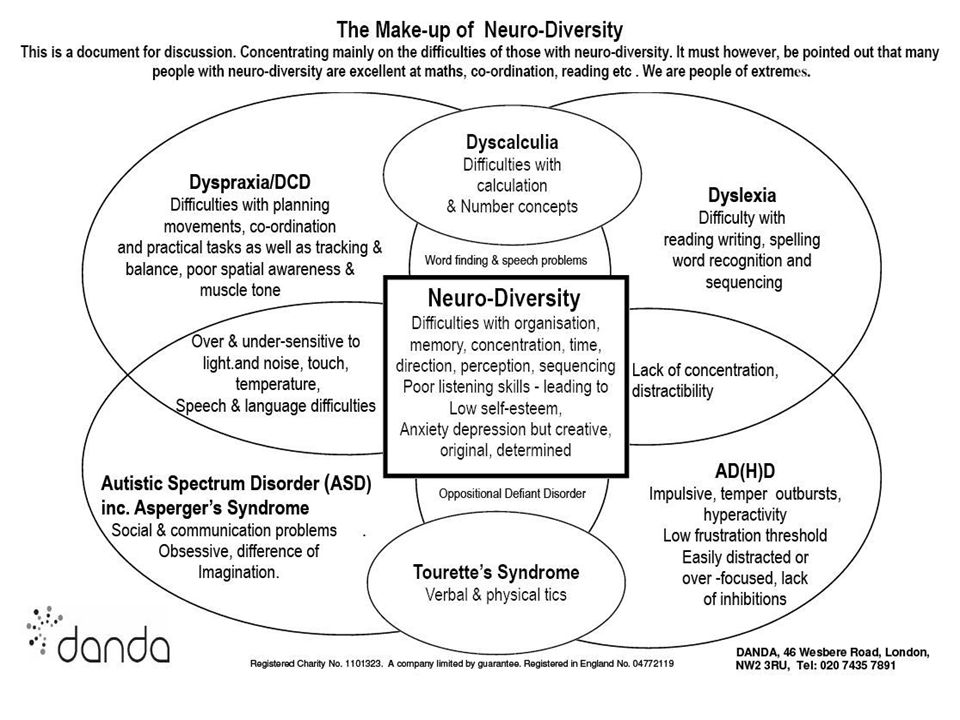 Classical medicine and psychology are focused on relieving symptoms, accepting the situation, adaptability and, ultimately, the constant need for treatment. Many children and adults have been registered for years with a specialist who cannot offer them anything significant. nine0009
Classical medicine and psychology are focused on relieving symptoms, accepting the situation, adaptability and, ultimately, the constant need for treatment. Many children and adults have been registered for years with a specialist who cannot offer them anything significant. nine0009
The essence of the diagnosis and treatment of ADHD in osteopathy
Osteopathy offers a fundamentally different approach to the treatment of hyperactivity and attention disorders.
This science is built on the basis of rehabilitation therapy, when instead of suppressing individual symptoms, work is carried out to restore the body as a whole.
Ideally, it is recommended to show the child to an osteopath immediately after birth, even with a successful delivery (and many are considered as such only due to the absence of obvious injuries). Prematurity, prolonged or short-lived labor, drug stimulation, and obstetrical benefits all pose an increased risk for developing ADHD in the future.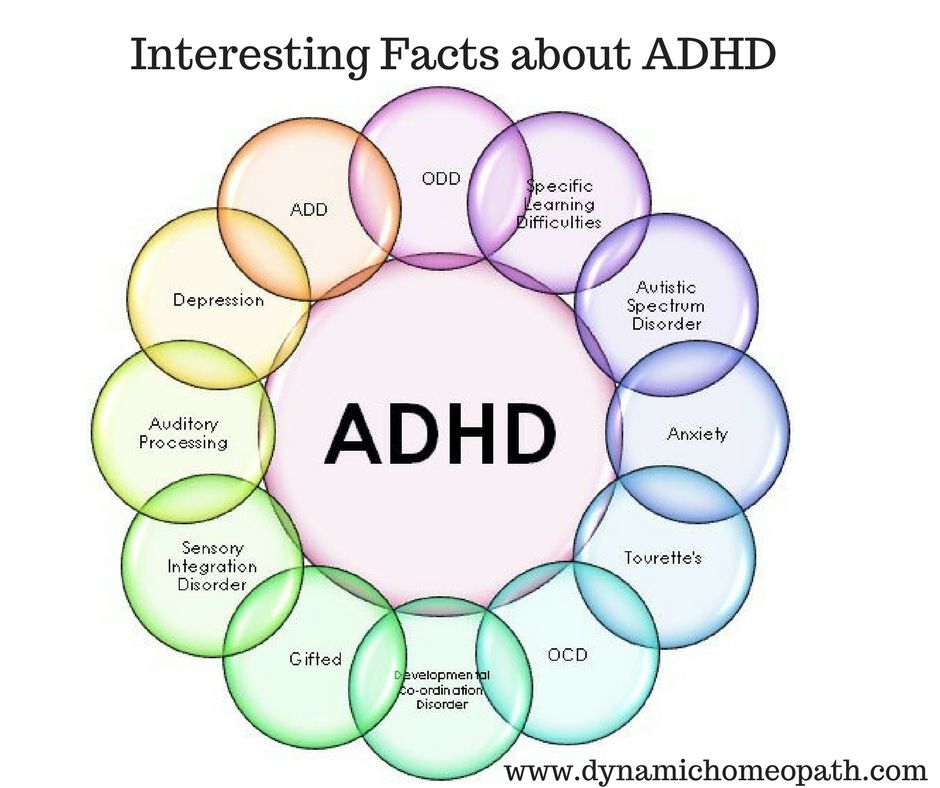 Such children from birth may show excessive anxiety, they have difficulty eating, gaining weight and sleeping, and frequent spitting up. Unfortunately, these phenomena are considered the norm, especially if the baby acquires a standard set of skills in due time. nine0004
Such children from birth may show excessive anxiety, they have difficulty eating, gaining weight and sleeping, and frequent spitting up. Unfortunately, these phenomena are considered the norm, especially if the baby acquires a standard set of skills in due time. nine0004
Often several sessions are enough to completely eliminate the problem in the first months of life, eliminating the development of ADHD. The fact is that, according to the concept of self-regulation, the body is able to independently neutralize the negative consequences of traumatic factors (hypoxia, infection). In young children, compensatory properties are still well developed. But for this, the body must be brought into an appropriate state, which is what osteopathic activity is aimed at.
At an older age, the treatment of ADHD is delayed due to the accumulated defects, in the elimination of which, along with osteopathic treatment, traditional methods will have to be used. It makes sense to connect psychological correction and, in the most extreme case, pharmacological drugs after the osteopath has eliminated the root cause.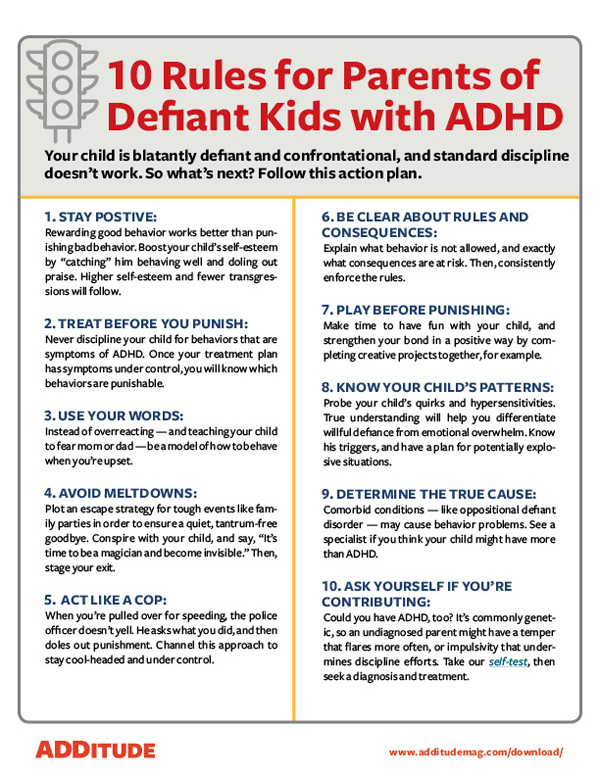 nine0009
nine0009
Osteopathic treatment is based on a proven theory of skull mobility. Even microscopic displacements of parts of the skull or cervical, sacral regions can lead to compression of the brain and blood vessels. In osteopathy, the body is a single whole, therefore, an injured sacrum or neck (often in childbirth, including through a caesarean section) affects the brain structures, provoking ADHD and other dysfunctions.
Osteopathy heals by returning body parts to their natural place, restoring their correct interaction. The osteopathic doctor is fluent in knowledge about the structure of the body, the location of organs, bone structure. Barely touching the body, he determines the displacement of structures, changes in tone, literally feels the energy of the body's vital activity. nine0004
Already after 1-2 sessions parents can see positive changes. A child who has been tormenting himself and those around him with his hyperactivity for years suddenly becomes balanced and assiduous.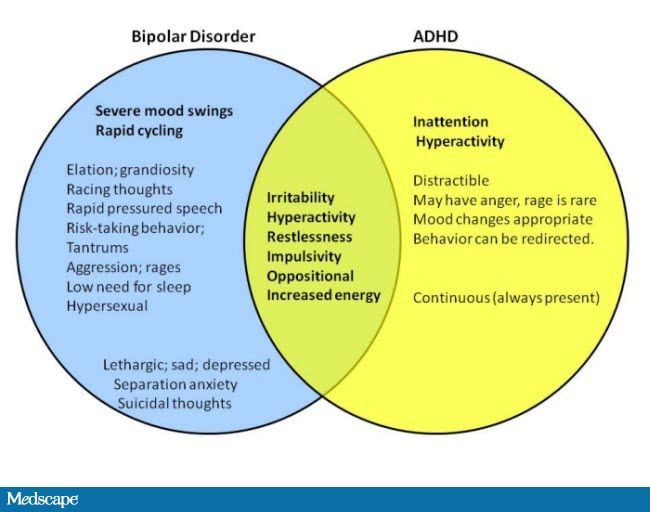
The concentration of attention increases, the child manages to control himself and form goals.
Adults feel unusual lightness and energy.
Types of osteopathic care for ADHD
Craniosacral osteopathy
Structural osteopathy
Visceral osteopathy
1. Craniosacral osteopathy
Osteopaths use craniosacral techniques to treat ADHD in children. According to him, the human skull is mobile and “breathes” due to elastic seams connecting the ossified parts. Normally, the frequency is 6-10 “breaths” and “exhalations” per minute. The movement of cerebrospinal fluid from the ventricles of the brain through the spinal column to the sacrum occurs in accordance with this rhythm, and its failures lead to various diseases, including the nervous system. nine0009
To feel these movements, determine the shape and temperature of the head, the doctor puts his hands on the patient's head and freezes briefly, then changes the position of the hands.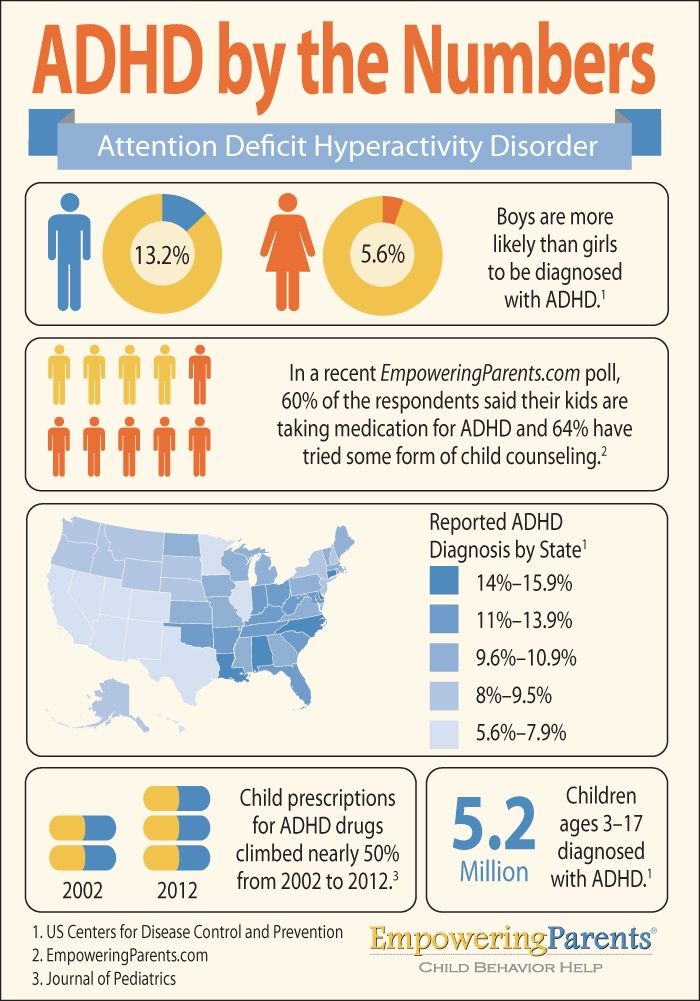
From the outside, nothing seems to be happening. The procedure does not cause any discomfort to the patient himself.
As well as the subsequent treatment, in which the osteopath corrects the cranial, cervical, pelvic bones, “listening” to the flow of energy between them.
You might think that we are talking about work on the energy level, but no, everything is quite physiological. The osteopath strives to ensure that the oscillations of the skull and sacrum occur synchronously, eliminating displacements and obstacles in the way of the movement of the cerebrospinal fluid. nine0009
For the treatment of children with ADHD, the craniosacral method is the most optimal and sufficient. Adults suffering from this syndrome need additional adjustment, as brain dysfunctions destroy the work of the whole organism over the years. This is often overlooked in the absence of specific complaints.
2. Structural osteopathy
Field of activity - bone and muscle structures, ligaments, joints. Any element of the system is somehow connected with the spine and skull. Distortions, asymmetric tone, sprains, old injuries and bruises (for example, injury to the coccyx) increase the symptoms of ADHD. nine0009
Any element of the system is somehow connected with the spine and skull. Distortions, asymmetric tone, sprains, old injuries and bruises (for example, injury to the coccyx) increase the symptoms of ADHD. nine0009
This direction successfully eliminates accompanying ADHD ailments: sleep disturbance, headaches, chronic fatigue.
3. Visceral osteopathy
Based on knowledge of the location and function of internal organs. Exacerbation of symptoms is often associated with their dysfunction and displacement, in which they can pinch blood vessels and squeeze each other. The doctor works with systems that directly affect brain activity. Here are just a few examples. nine0009
- Endocrine system. Produces hormones - substances that stimulate the brain;
- Digestive. In particular, the liver - helps with the removal of toxins;
- Respiratory - supplies oxygen to the brain.
Releasing the blood flow, removing the clamps, the specialist restores the normal functionality of internal organs and systems using visceral techniques.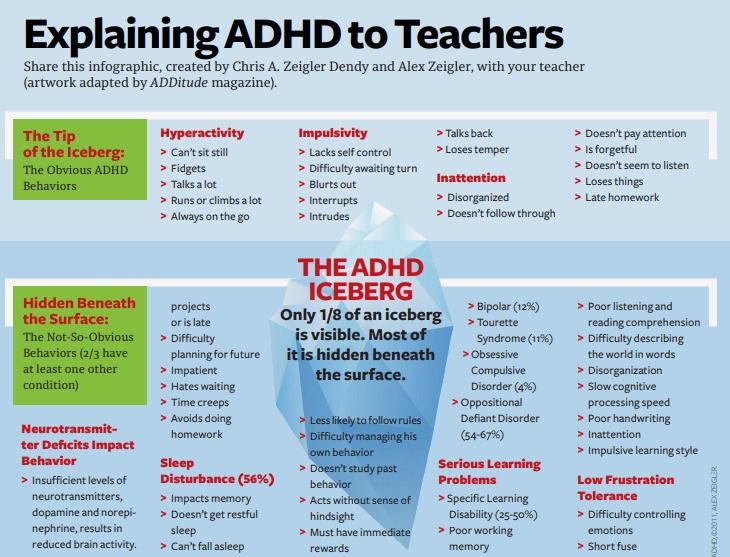
Treatment of the disorder at the Osteopathy Center
All of our physicians are experienced in restorative medicine. A pediatric neurologist, a neonatologist, a rehabilitation specialist, and a surgeon who have been trained in osteopathy schools conduct appointments at the clinic. nine0004
A preliminary conversation with a patient or parents of a patient with hyperactivity and other disorders allows you to quickly and accurately determine the causes of the disease.
When working with ADHD, the doctor examines the entire anamnesis: chronic conditions of the parents, the course of pregnancy and childbirth, the drugs used, the results of tests and examinations, if the patient has already been observed somewhere. If pathology is suspected, the osteopath directs for diagnosis.
A session for the youngest children lasts an average of 25 minutes, the next sessions are scheduled with a break of a week or two. This time is necessary for the restructuring of the body, getting used to the correct healthy state. At each meeting, the doctor evaluates the ongoing changes. nine0009
At each meeting, the doctor evaluates the ongoing changes. nine0009
Adult children and adults spend about an hour in the office to completely eliminate attention deficit hyperactivity disorder. They need a longer course with breaks of several weeks. Despite positive changes, the course should be continued in order to avoid relapse.
Recommendations for self-help
The osteopathic clinic, like the traditional clinic, has a certain opinion.
Therapeutic procedures may not give the desired result if the patient with ADHD is not provided with the proper environment and attention is not paid to his needs, especially with children. The syndrome is more difficult to eliminate in sensitive and inert people. Over the years of illness, they have become accustomed to demonstrating impulsivity and certain behavioral patterns. The task of relatives is to keep calm, maintain a friendly atmosphere. nine0009
Important components of successful therapy of the syndrome are
- Nutrition rich in vitamins and minerals;
- Sufficient sleep;
- Emotional release;
- Walking, outdoor recreation, moderate exercise.
Learn more