Is psychosurgery still used today
Types of Psychosurgery
- Download PDF Copy
By Dr. Liji Thomas, MDReviewed by Afsaneh Khetrapal, BSc
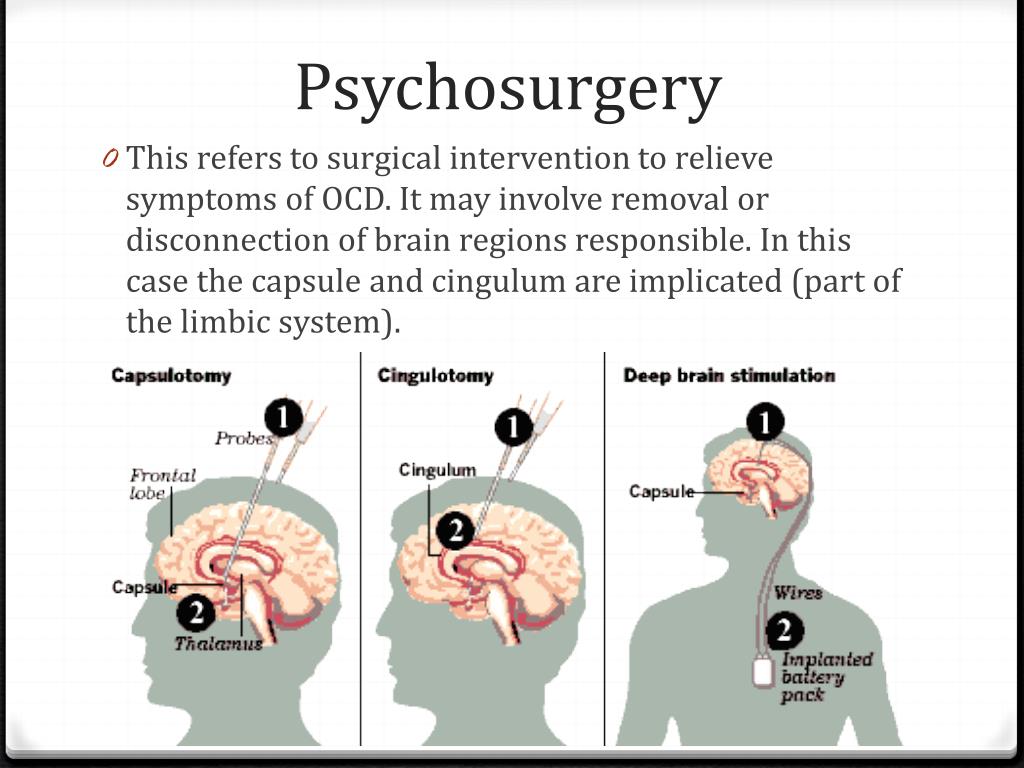
Psychosurgery is a field of surgery which consists of stereotactic operations on the brain aimed at altering abnormal physiology by severing certain connections between the frontal lobe and the rest of the brain, including the cortex, the nuclei or other brain pathways, which may appear to function normally or abnormally, in order to reduce mental and/or physical suffering in otherwise untreatable patients.
While it was introduced by Moniz in 1936, its popularity and applications boomed for a brief period, only to collapse like a deflated balloon within a few decades. The primary cause of this wane in the practice of psychotherapy was the inappropriate and nonselective use of the operation for all kinds of indications, without regard to the evidence for a good outcome.
The lack of accurate diagnostic criteria for many psychiatric disorders, coupled with poor recording and regulation, led to the rise of immense controversy surrounding this field.
Psychosurgery currently refers to operations of the frontal lobe, because no other part of the brain has been found to be sensitive to surgery in such a way as to produce an improvement in affective and anxiety disorders. The only possible exception is resection of the postcentral cortex to relieve the intractable pain in some cases of phantom limb. Recently, interest has been shown in creating lesions in the thalamus and hypothalamus, but the results are far from being translated to the stage of clinical practice.
Lobotomy - PBS documentary, on Walter Freeman.mp4
Frontal Lobotomy
Operations on the frontal lobe may use various approaches, namely, from the top as Moniz did, laterally, or through the orbit from the inferior aspect. The frontal lobe is the most anterior part of the brain and lies behind the forehead.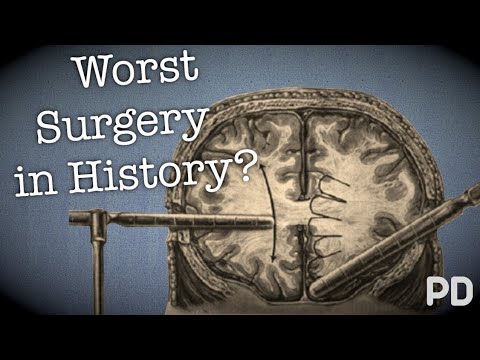 It ends at the Rolandic fissure behind and the sylvian fissure below. The most posterior parts have to do with the regulation of muscular and visceral functions and should be left untouched for fear of severe disability and even death if they are encroached upon during the operation. For the rest, the frontal lobe has the same structure and so accuracy of lesion location is somewhat flexible, but not the depth of the lesions produced during the operation.
It ends at the Rolandic fissure behind and the sylvian fissure below. The most posterior parts have to do with the regulation of muscular and visceral functions and should be left untouched for fear of severe disability and even death if they are encroached upon during the operation. For the rest, the frontal lobe has the same structure and so accuracy of lesion location is somewhat flexible, but not the depth of the lesions produced during the operation.
The aim of the operation is to sever some vital connections between this part of the brain and the rest. These include the fronto-thalamic pathways, upon which the cells in the medial nucleus (of the thalamus) depend for survival in a one-on-one manner. Within the nucleus the cells project to the orbit, the frontal pole and the convexity of the frontal lobe, from medial to lateral, respectively. The neurons in the frontal lobe project to the internal capsule and the peduncle, and indirectly to the basal ganglia for the most part. While other frontal lobe-cortical connections do exist, the only important pathway for the purpose of psychosurgery is this pathway. Thus, cutting this pathway at thalamic level (thalamotomy) or during its course (frontal lobotomy), or at its end (topectomy, lobectomy or cortical undercutting) is the aim of psychosurgery.
While other frontal lobe-cortical connections do exist, the only important pathway for the purpose of psychosurgery is this pathway. Thus, cutting this pathway at thalamic level (thalamotomy) or during its course (frontal lobotomy), or at its end (topectomy, lobectomy or cortical undercutting) is the aim of psychosurgery.
Transorbit lobotomy and MRI examination of living lobotomized patient s brain
The goal of surgery has not changed over the decades, but the technique has been highly refined and altered to make the lesions very reliable as to location, using modern imaging techniques and stereotactic surgery. The most recent trend is to forego surgery in favor of non-ablative techniques, namely, deep brain stimulation (DBS) for the same conditions that psychosurgery was indicated in. These include depression and obsessive-compulsive disorder (OCD) resistant to other therapies.
Frontal lobotomy is carried out by the closed (or precision) and the open methods. The open method uses trephine holes to gain access to the frontal lobe close to the coronal suture, preferably from the frontal pole. The cortex at the thalamofrontal radiation is incised using a leucotome or by suction-cautery, and iodized oil is instilled into the incisions finally for X-ray verification of the accurate placement of the lesions. The mortality is about 3%, due mainly to hemorrhage or infection.
The open method uses trephine holes to gain access to the frontal lobe close to the coronal suture, preferably from the frontal pole. The cortex at the thalamofrontal radiation is incised using a leucotome or by suction-cautery, and iodized oil is instilled into the incisions finally for X-ray verification of the accurate placement of the lesions. The mortality is about 3%, due mainly to hemorrhage or infection.
Topectomy uses a little larger opening, to resect symmetrical areas of the frontal cortex which are carefully plotted.
Cortical undercutting refers to cutting under the cortex rather than lifting it off, thus limiting blood loss since cerebral arteries travel inwards from the surface of the brain. Described way back in 1949 by Scoville, it makes lesions in Brodmann areas 9 and 10, the cingulate gyrus, and the orbital surface of the frontal lobe, all of which are associated with emotions. This was modified in 1955, by Knight, to restricted orbital undercutting. Lateral dissection was cut short to avoid destroying unnecessary fibers and to avoid extreme personality alterations postoperatively. The improvement in OCD and other psychiatric disorders following this procedure is of the order of 70% to 85%.
Lateral dissection was cut short to avoid destroying unnecessary fibers and to avoid extreme personality alterations postoperatively. The improvement in OCD and other psychiatric disorders following this procedure is of the order of 70% to 85%.
All these techniques carry a mortality of 3% or more depending upon operator experience, and a significant risk of epilepsy postoperatively, though this tends to be controlled in about a year.
The transorbital route is simple and suited to poor-risk patients, since it requires no opening of the skull. Instead it uses a pointed tool pushed right through the orbital bone at the back of the socket along the top of the frontal lobe towards the coronal suture, the tool being manipulated to destroy much of the thalamofrontal pathways. This is not otherwise used due to its blind nature and lower effectiveness in psychiatric disorders.
These techniques are being replaced by stereotactic gamma-knife surgery.
Modern Psychosurgery
Modern stereotactic psychosurgery depends upon four procedures:
- anterior cingulotomy
- subcaudate tractotomy
- limbic leucotomy
- anterior capsulotomy
Since all these techniques cause lesions of the limbic system or adjoining structures, this type of surgery may also be called limbic system surgery. All are comparable in their results and are relatively safe.
All are comparable in their results and are relatively safe.
- Cingulotomy or anterior cingulotomy refers to placing stereotactic lesions in the anterior cingulate to sever the cingulum bundle. Placing anterior lesions and having a lower total volume of lesions are associated with better outcomes. With significant improvement in symptoms and very few cognitive ill-effects, this procedure shows promise in refractory OCD cases.
Cingulotomy coupled with anterior capsulotomy on both sides can reduce aggressiveness and improve the general state of the patient, with apparently few complications.
- Stereotactic subcaudate tractotomy (SCT) was described by Knight in 1964. It focuses on the destruction of bifrontal pathways in front of the caudate nucleus using radioactive Yttrium implants, connecting the fibers from the frontal cortex and the amygdala to the hypothalamus, to modulate the intensity of emotional reactions. Cognitive deficits were not observed, but memory loss does occur, and some tasks are performed poorly.
 However, these are transient and thought to be due to postoperative frontal lobe edema than subcaudate damage. The response rates range from 70% to 100%.
However, these are transient and thought to be due to postoperative frontal lobe edema than subcaudate damage. The response rates range from 70% to 100%. - Limbic leucotomy was described in 1973 by Kelly and Richardson. In this stereotactic technique, cingulotomy is paired with SCT to make use of the effects on the autonomic nervous system and the patient’s responses. The improvement was seen in up to 80% of patients.
- Anterior capsulotomy consists of making lesions in the anterior part of the internal capsule. It was introduced by Lars Leksell in Sweden to interrupt the fronto-thalamic radiation. He reported a 78% improvement in symptoms of intractable OCD.
The results of these procedures have been described as excellent in several smaller studies on patients with pharmacoresistant affective disorders or OCD. More than half of treated patients appear to score much higher across the scale of wellbeing and task performance. In OCD, cingulotomy, subcaudate tractotomy, limbic leucotomy, and capsulotomy achieve good results in 56%, 50%, 61% and 67% respectively.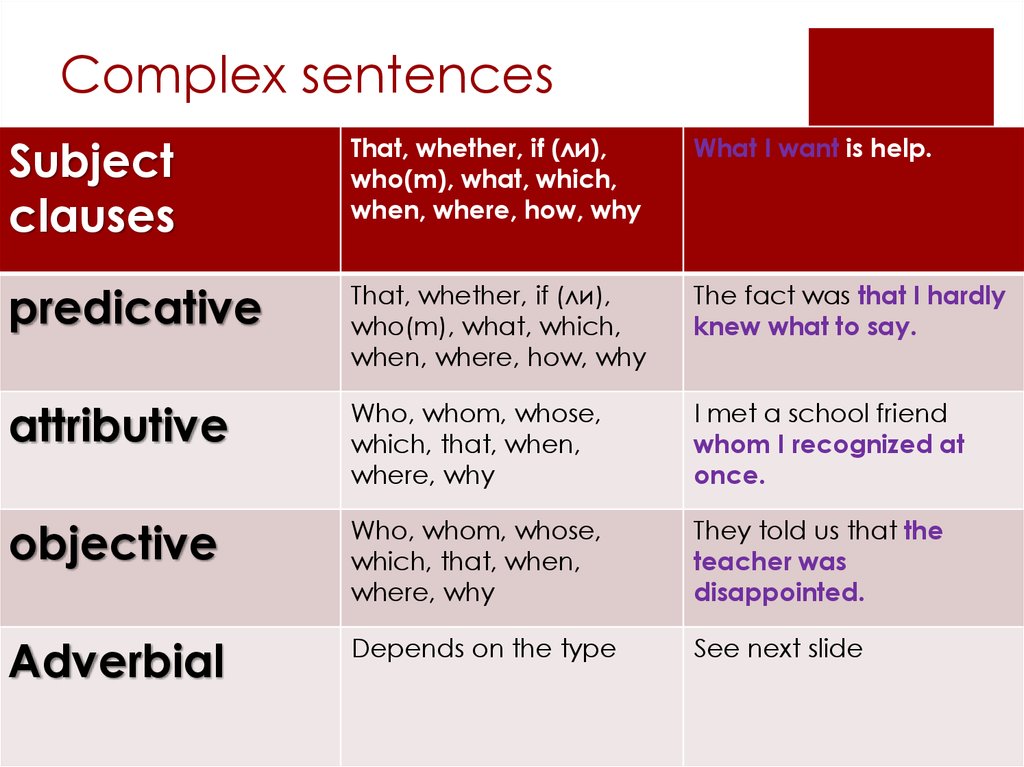 In the case of affective disorders, the corresponding rates were 65%, 68%, 78% and 55% respectively. Overall, it is suggested that anterior capsulotomy or limbic leucotomy may be preferred in OCD, while cingulotomy has the lowest rate of adverse effects.>
In the case of affective disorders, the corresponding rates were 65%, 68%, 78% and 55% respectively. Overall, it is suggested that anterior capsulotomy or limbic leucotomy may be preferred in OCD, while cingulotomy has the lowest rate of adverse effects.>
The similarity of effect rates suggests that these operations are not specific in their benefits and may therefore be used across the spectrum of mental disorder with predictably high rates of success in cases which remain intractable despite adequate and appropriate medical therapy. To quote one study, even by the strictest standards, one-fourth to one-half of patients with intractable OCD benefit from these, and if more general criteria are substituted, this improvement is measurably and significantly present in 50% to 70% of patients.
Sources
- https://www.ncbi.nlm.nih.gov/pubmed/7696872
- https://www.ncbi.nlm.nih.gov/pubmed/1842976
- https://www.ncbi.nlm.nih.gov/pubmed/12856490
- https://www.
 ncbi.nlm.nih.gov/pubmed/17916331
ncbi.nlm.nih.gov/pubmed/17916331 - https://www.ncbi.nlm.nih.gov/pubmed/12662251
- https://www.ncbi.nlm.nih.gov/pubmed/7726719
- www.ncbi.nlm.nih.gov/pmc/articles/PMC2616681/pdf/jnma00632-0011.pdf
- https://www.ncbi.nlm.nih.gov/pubmed/1782537
- https://www.ncbi.nlm.nih.gov/pubmed/27900544
- https://neurosurgery.mgh.harvard.edu/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221188/
Further Reading
- All Psychosurgery Content
- What is Psychosurgery?
- Psychosurgery Complications and Outcomes
Last Updated: Dec 29, 2022
- Download PDF Copy
Please use one of the following formats to cite this article in your essay, paper or report:
APA
Thomas, Liji. (2022, December 29). Types of Psychosurgery. News-Medical. Retrieved on January 11, 2023 from https://www.news-medical.net/health/Types-of-Psychosurgery.
 aspx.
aspx.MLA
Thomas, Liji. "Types of Psychosurgery". News-Medical. 11 January 2023. <https://www.news-medical.net/health/Types-of-Psychosurgery.aspx>.
Chicago
Thomas, Liji. "Types of Psychosurgery". News-Medical. https://www.news-medical.net/health/Types-of-Psychosurgery.aspx. (accessed January 11, 2023).
Harvard
Thomas, Liji. 2022. Types of Psychosurgery. News-Medical, viewed 11 January 2023, https://www.news-medical.net/health/Types-of-Psychosurgery.aspx.
Psychosurgeons Use Lasers to Burn Away Mental Illness
"It lies at the intersection of our cognitive brain and emotional part of our brains," says Sameer Sheth, a Columbia University Medical Center surgeon who performs psychosurgeries targeting OCD. Functionally, the anterior cingulate is involved in allocating brainpower to certain tasks.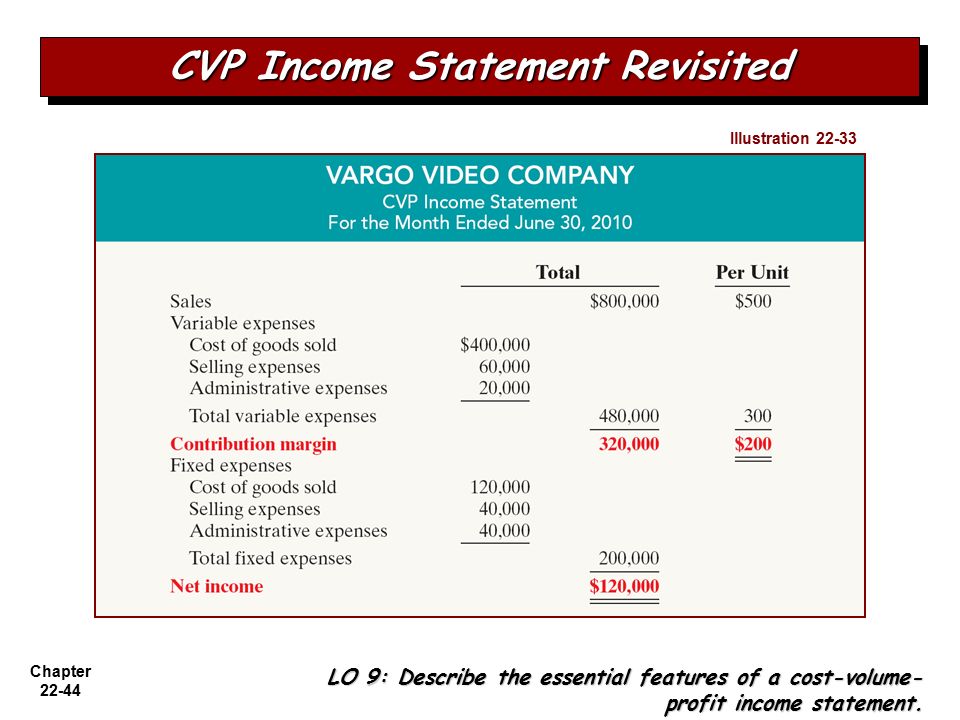 That involves alerting you to a task's urgency and giving you a feeling of satisfaction when the task is complete. "If you’re struggling on a particular project, this part of the brain will help you allocate resources and expend the right cognitive energy," says Sheth.
That involves alerting you to a task's urgency and giving you a feeling of satisfaction when the task is complete. "If you’re struggling on a particular project, this part of the brain will help you allocate resources and expend the right cognitive energy," says Sheth.
For people with OCD, this part of the brain can go haywire: Sufferers pay too much attention to a particular stimulant and don't get a satisfactory brain response. Obsessive cleanliness is a pretty typical symptom. Think about the last time you went a few days without a shower, and the relief you felt after finally hosing off. For a person with OCD, a single hand washing doesn’t eliminate the alarm signals in the brain; the constant stimulation can overwhelm their ability to do just about anything else.
Of course, cleanliness isn't the only way OCD messes with people. Some need to check and recheck and check and recheck the same thing over and over and over. Some must perform little physical rituals. Others hoard. Among the worst symptoms are intrusive thoughts, ranging from obsessing over the meaning of words to inescapable ruminations about committing acts of violence. "There are really severe cases of OCD where people are incapacitated by their intrusive thoughts and rituals," says James Wilcox, a biological psychiatrist at the University of Arizona in Tucson. "It’s one of the few areas where psychosurgery is still done."
Among the worst symptoms are intrusive thoughts, ranging from obsessing over the meaning of words to inescapable ruminations about committing acts of violence. "There are really severe cases of OCD where people are incapacitated by their intrusive thoughts and rituals," says James Wilcox, a biological psychiatrist at the University of Arizona in Tucson. "It’s one of the few areas where psychosurgery is still done."
Not everyone qualifies. First, the patient's symptoms must cross a certain threshold of severity, measured on the Yale-Brown Obsessive Compulsive Scale. Their symptoms also must be resistant to pharmaceuticals and cognitive behavioral therapy. Only about 20 percent of all OCD patients qualify. Far fewer go under the knife.
Before any cutting or drilling, the surgeon pins what looks like a giant protractor to the patient's head---a stereotactic frame. Then using CT and MRI scans, the surgeon builds a map the patient's brain and draws a safe path from the skull to the burn zone, accurate to within fractions of a millimeter.
But because the brain is malfunctioning in invisible ways, the surgeons draw upon laboratory studies from animal and human experiments. "This whole field relies on improving our understanding of how the brain works," Sheth says. That requires a lot of back and forth, beginning with lab work on animal brains. Once neuroscientists figure out how a certain brain circuit works in a fish or a rat, they step the research up in human studies. This involves using functional magnetic resonance imaging or EEG readings to judge what parts of the brain are most important to certain behaviors.
From there, surgeons like Sheth design their interventions, targeting a specific area of the brain as closely as possible. "We do a small procedure, see how patients respond, and from that we can learn how to better do the next experiments," he says. The changes are incremental, and in surgery they only burn away as much as they know is safe.
Psychosurgeries aren't the only way to treat mental illness. Besides the standard stuff, like therapy, medication, and exercise, surgeons often recommend a procedure called deep brain stimulation. For this, a surgeon attaches electrodes to a different part of the brain, called the ventral striatium. "That area is a crossroads of activity, close to a lot of important brain pathways," says Sheth. DBS---which started as a treatment for Parkinson's---sends low voltage electricity to the targeted area, soothing compulsive thoughts. And though OCD is the only mental illness that is FDA-cleared for psychosurgery, clinical trials for depression look somewhat promising.
Besides the standard stuff, like therapy, medication, and exercise, surgeons often recommend a procedure called deep brain stimulation. For this, a surgeon attaches electrodes to a different part of the brain, called the ventral striatium. "That area is a crossroads of activity, close to a lot of important brain pathways," says Sheth. DBS---which started as a treatment for Parkinson's---sends low voltage electricity to the targeted area, soothing compulsive thoughts. And though OCD is the only mental illness that is FDA-cleared for psychosurgery, clinical trials for depression look somewhat promising.
While this may seem like a better option than burning away a lump of neurons, the advantage of psychosurgery is you don't have to have a device embedded in your brain. Devices need maintenance, they can fail, their batteries run out, and they can get infected. And for people who need them, psychosurgeries can be highly effective. Success rates are relatively high---about half of all patients who undergo anterior cingulotomy recover to completely normal levels of brain function.
Psychosurgery: yesterday and today (review of foreign publications)
Psychosurgery, the neurosurgical treatment of mental disorders, has a long history. This review is prepared on the basis of foreign publications devoted to this method, it examines the history, development in the 19th century, use and abuse in the 20th century, and the current state of psychosurgery. Due to past abuses, the use of psychosurgical interventions is severely limited and is indicated for a very small number of patients with severe and treatment-resistant psychiatric disorders. nine0005
Origins of psychosurgery
The origins of psychosurgery can be found in ancient times, as evidenced by the practice of trepanation. Carbon dating of skulls with trepanation holes found in a burial in France showed that trepanation was performed in the Stone Age, in 5100 BC, and it was more “healing” than traumatic [1]. The first written mention of trepanation dates back to 1500 BC and indicates that this method was used to treat mental disorders. It can be considered that the history of the treatment of mental disorders originates from trepanation [2]. nine0006
It can be considered that the history of the treatment of mental disorders originates from trepanation [2]. nine0006
The foundations of modern psychosurgery were laid in the middle of the 19th century. This was facilitated by the understanding of the relationship between behavior, mental activity and the brain, in particular the description of Broca's and Wernicke's aphasias. An important date in the history of psychosurgery and neuroscience in general is September 13, 1848. Dr. John Harlow described the case of railroad worker Phineas Gage. During the explosion, a sharp branch 103 cm long and 3 cm thick pierced through his skull, hitting the eye socket and coming out in the occipital region. Many were surprised by the consequences of this injury. Gage soon recovered, but from an intelligent person and a decent citizen, he turned into an unrestrained tramp, and one of his acquaintances noted: “Gage has already ceased to be Gage” [3]. Almost 150 years later, Damasio et al. [4] published data on Gage's skull, suggesting that the ventromedial part of the prefrontal cortex was damaged as a result of the injury. nine0006
nine0006
The birth of psychosurgery is associated with the name of the Swiss doctor Gottlieb Burckhardt, who performed the first psychosurgical intervention in 1888 [5], he performed excision of cortical areas in the frontal, parietal and occipital regions of the cortex (the so-called topectomy) in six patients. In three patients, the operation was successful, in one - it ended in death.
In the early 20th century, interest in clinicopathological relationships between the brain and behavior continued. By the beginning of World War II, psychiatry and neurology were finally separated, and several types of biological therapies were proposed for the treatment of mental disorders (most of them were developed by non-psychiatrists), in particular hydrotherapy, insulin coma therapy, electroconvulsive therapy (ECT) and psychosurgical techniques. nine0006
After Burckhardt, neurosurgeons continued to explore ablative (removal) surgeries of the frontal lobe. Ludwig Puusepp (founder of neurosurgery in Russia, born in Kyiv, studied neurology under the guidance of Vladimir Bekhterev, lived and worked most of his life in Estonia, was a professor at the Department of Neurology at the University of Tartu) [6] performed a frontal lobotomy, Wilder Penfield [7] described the improvement psychiatric symptoms after removal of tumors, abscesses and other brain damage. nine0006
nine0006
The name of the charismatic neurologist Egas Moniz is associated with the emergence of the term "psychosurgery" and the spread of the infamous method of lobotomy. Moniz hypothesized that the intersection of afferent and efferent fibers in the frontal lobe could be effective in the treatment of mental disorders. His colleague Almeida Lima performed the first series of experimental interventions using ethanol injections [8, 9]. The lobotomy procedure consisted of the following: a loop was inserted into the brain with the help of a conductor, and the brain tissue was damaged by rotational movements. After performing about a hundred such operations and conducting a follow-up observation of patients, which consisted of a subjective assessment of the mental state, Moniz reported the success of this operation and began to popularize it. In fact, Moniz observed only a few patients, and most of them were never seen again after the operation [10]. Although the quality of the research was criticized in scientific audiences, Moniz wrote hundreds of articles and books on lobotomy. At 19In 1949 he was awarded the Nobel Prize in Medicine and Physiology, it is interesting that his achievements in brain angiography were indicated in the nomination application.
At 19In 1949 he was awarded the Nobel Prize in Medicine and Physiology, it is interesting that his achievements in brain angiography were indicated in the nomination application.
In the United States, lobotomy was brought into disrepute by Walter Freeman and James Watts. They modified the method of Moniz and Lima [11] and reported success in several hundred patients. Severe consequences and complications of this operation became apparent later [10, 12]. Freeman was enthusiastic about spreading the new method and blamed the indecisiveness of physicians who did not use it. The method gained popularity, and often lobotomy was performed by doctors who did not have surgical training, which was one of the abuses of this psychosurgical intervention. nine0006
In the 40s of the twentieth century, lobotomy in the United States became more common for purely economic reasons, since the “cheap” method made it possible to “treat” about 1.5 million Americans who were then held in assilums [10], and could reduce the cost of psychiatric institutions $1 million a day [13]. The successes of the lobotomy were reported in the leading newspapers at the time, drawing public attention to it. It should be noted that at that time there were no effective means for the treatment of mental disorders, and cases of the return of patients from Assilum to society were extremely rare, which is why the widespread use of lobotomy was welcomed [14]. nine0006
The successes of the lobotomy were reported in the leading newspapers at the time, drawing public attention to it. It should be noted that at that time there were no effective means for the treatment of mental disorders, and cases of the return of patients from Assilum to society were extremely rare, which is why the widespread use of lobotomy was welcomed [14]. nine0006
The decline of lobotomy began after the serious neurological complications of frontal lobotomy became apparent. The popularity of lobotomy began to fall sharply, in the early 50s the first antipsychotics appeared; later lobotomy was declared illegal in many countries.
After the decline of lobotomy, the development of psychosurgery did not stop; its further development was associated with the advent of stereotactic surgical techniques in the late 40s of the last century [15]. Stereotactic surgery resulted in a more precise and gentle excision of brain tissue, leading to fewer side effects and less mortality. Advances in neurobiology made it possible to identify new goals in psychosurgery. After several decades of psychopharmacotherapy of psychiatric disorders, it has become clear that psychosurgical interventions can be considered in a small proportion of patients with refractory psychiatric disorders. nine0006
Advances in neurobiology made it possible to identify new goals in psychosurgery. After several decades of psychopharmacotherapy of psychiatric disorders, it has become clear that psychosurgical interventions can be considered in a small proportion of patients with refractory psychiatric disorders. nine0006
In the 1960s and 1970s, on the one hand, society was careful to ensure that psychosurgery was not used for the purpose of abuse, on the other hand, the idea of the possibility of controlling dangerous psychiatric patients and criminals by controlling aggressive impulses using implanted electrodes was actively discussed in society. , which regulate the activity of the limbic system [16–19].
Modern psychosurgery
Currently, four neurosurgical interventions are used to treat mental disorders. Indications for them are more often affective or anxiety disorders, but not cognitive impairment. At the present stage, psychosurgery is a destructive rather than a constructive method of treatment; the destruction of neuronal structures is used, and not their stimulation.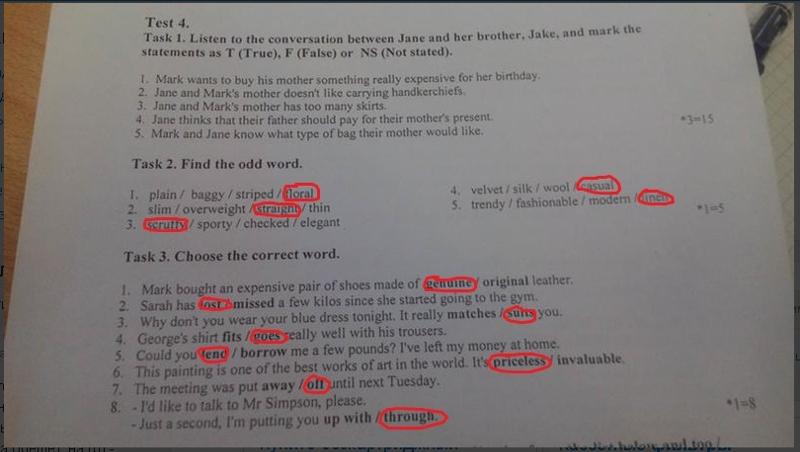 These four interventions are briefly described below: anterior cingulotomy, subcaudal tractotomy, limbic leucotomy, and anterior capsulotomy. nine0006
These four interventions are briefly described below: anterior cingulotomy, subcaudal tractotomy, limbic leucotomy, and anterior capsulotomy. nine0006
Anterior cingulotomy was first performed in the early 1950s [20–22]. Non-surgical damage to the anterior cingulate gyrus leads to severe attention deficits (profound inattention) and akinetic mutism. The procedure consists in bilateral stereotaxic thermocoagulation of parts of the cingulate gyrus [23].
According to published studies, cingulotomy has been used in patients with severe refractory obsessive-compulsive disorder (OCD). After the intervention, improvement was noted in a third of patients [24], the risk of postoperative complications (convulsive seizures) was about 1% [25]. nine0006
The subcaudal tractotomy was developed by Geoffrey Knight in the UK in 1964 as a technique to minimize damage to the frontal lobe by cutting fibers from the frontal lobe to subcortical structures such as the amygdala [26]. The procedure is indicated for refractory depression and OCD. The original operation was performed by introducing radioactive implants into the frontal lobes. The therapeutic response was observed in a third of patients, postoperative complications were observed in the form of seizures (up to 2%) and negative personality traits (up to 7%) [27, 28]. nine0006
The original operation was performed by introducing radioactive implants into the frontal lobes. The therapeutic response was observed in a third of patients, postoperative complications were observed in the form of seizures (up to 2%) and negative personality traits (up to 7%) [27, 28]. nine0006
Limbic leucotomy is essentially a combination of anterior cingulotomy and subcaudal tractotomy. The method has been used in recurrent depression and OCD, and therapeutic response has been reported in 36–50% of patients and transient side effects have been reported [29]. Successful interventions have been reported in patients with schizoaffective disorder who self-injure themselves [30].
The anterior capsulotomy was developed by the French neurosurgeon John Talerac in the late 1940s. Currently, it is performed using thermocoagulation or gamma knife by stereotaxic damage to the frontal limbic fibers of the internal capsule [31, 32]. A therapeutic response has been reported in 70% of patients with OCD [33]. nine0006
nine0006
Guidelines for the Clinical Application of Psychosurgery
Neurosurgical procedures for the treatment of psychiatric disorders are reserved for patients who are refractory to medication, psychotherapy, and ECT treatments. The attending psychiatrist is the only specialist who can recommend psychosurgical intervention to the patient, and he must provide detailed documentation of the treatment carried out and the reasons for its termination. It is the responsibility of the psychiatrist to monitor the recovery of the patient in the postoperative period. nine0006
Different institutions have specific requirements and criteria for referring patients with mental disorders for neurosurgical treatment. As a general rule, the severity of the condition should persist for at least five years despite attempts at pharmacological or other treatment, and the patient should be seen by a psychiatrist, neurosurgeon, and neurologist who jointly perform a clinical evaluation of the patient. The patient should undergo an ECG, MRI, neuropsychological tests and necessary laboratory tests. In addition to the patient, consent to surgery must be given by members of his family [34]. nine0006
The patient should undergo an ECG, MRI, neuropsychological tests and necessary laboratory tests. In addition to the patient, consent to surgery must be given by members of his family [34]. nine0006
The experience of developed countries indicates that psychosurgical interventions are performed extremely rarely and only in a few highly specialized neurosurgical clinics [35].
Perspectives of psychosurgery
The development of psychosurgery in the twentieth century was complex and controversial, due to its invasiveness and the use of refractory mental disorders in the most severe cases, today it is difficult to talk about psychosurgical interventions in the language of evidence-based medicine, i.e. to demonstrate their efficacy and safety in various psychiatric disorders in double-blind controlled trials and meta-analyses. The further development of psychosurgery is closely related to past and future advances in psychiatry, neurology, neurosurgery, and neuroscience [36]. Animal experimental studies are currently being actively pursued to try to develop interventions that would stimulate the work of neurons in various brain structures. In animal models of Parkinson's disease, epilepsy, affective and anxiety disorders, the implantation of cellular material, such as stem cells, into areas of brain degeneration or damage is being studied. However, the development and implementation of such methods of psychosurgical interventions for the treatment of mental disorders will require the resolution of ethical issues and the definition of procedures for regulating the use of these methods in patients with severe mental disorders. nine0006
Animal experimental studies are currently being actively pursued to try to develop interventions that would stimulate the work of neurons in various brain structures. In animal models of Parkinson's disease, epilepsy, affective and anxiety disorders, the implantation of cellular material, such as stem cells, into areas of brain degeneration or damage is being studied. However, the development and implementation of such methods of psychosurgical interventions for the treatment of mental disorders will require the resolution of ethical issues and the definition of procedures for regulating the use of these methods in patients with severe mental disorders. nine0006
Prepared by Stanislav Kostyuchenko
Bibliography
1. Alt K.W. et al. Evidence for stone age cranial surgery // Nature. - 1997. - 387. - 360.
2 Baer L. et al. Cingulotomy for intractable obsessivecompulsive disorder: prospective longterm followup of 18 patients // Arch. Gen. Psychiatry. - 1995. - 52. - 384392.
Gen. Psychiatry. - 1995. - 52. - 384392.
3. Harlow J.M. Recovery from the passage of an iron bar through the head // N. Engl. J. Med. - 1848. - 389392.
4 Damasio H. et al. The return of Phineas Gage: clues about the brain from the skull of a famous patient // Science. - 1994. - 264. - 11021105.
5. Mairet A. De la demence melancolique: contribution a l'etude de la periencephalite localisee, et a le'etude des localisations cerebrales d'ordre psychique. — Paris & Masson, 1883.
6. Puusepp L. Alcune considerazioni sugli interventi chirugici nelle malattie mentali // G. Accad. Med. Torino. - 1937. - 100. - 316. nine0006
7. Penfield W., Evans J. The frontal lobe in man: a clinical study of maximal removals // Brain. - 1935. - 58. - 115133.
8. Moniz E. Essai d'un traitement chirugical de certaine psychoses // Bull. Acad. Med. - 1936. - 115. - 385393.
9. Moniz E. Prefrontal leucotomy in the treatment of mental disorders // Am. J. Psychiatry. - 1937. - 93. - 13791385.
10. Valenstein E.S. Great and Desperate Cures. — New York: Basic Books, 1986.
11. Freeman W., Watts J.W. Prefrontal leucotomy in the treatment of mental disorders // South Med. J-1937. - 30. - 2331.
12. Rodgers J.E. Psychosurgery: Damaging the Brain to Save the Mind. — New York: HarperCollins, 1992.
13. Fulton J.F. The Frontal Lobes: Research Publication for the Association for Research in Nervous and Mental Disease. — Baltimore: Williams & Wilkins, 1948.
14. Valenstein E.S. The history of psychosurgery // Greenblatt S.H. (Ed.) The History of Neurosurgery. — AANS: Park Ridge, 1997.
15. Spiegel E.A. et al. Stereotaxic apparatus for operations on the human brain // Science. - nineteen47. - 106. - 349350.
16 Fins J.J. From psychosurgery to neuromodulation and palliation: history’s lessons for the ethical conduct and regulation of neuropsychiatric research // Neurosurg. Clin. N. Am. - 2003. - 14. - 303319.
17. Delgado J.M., Anshen R.N. Physical Control of the Mind: Toward a Psychocivilized Society. — New York: Harper and Row, 1969.
18. Mark V.H., Ervin F.R. Violence and the Brain. — New York: Harper & Row, 1970.
nineteen. New World, Future of psychosurgery in doubt // Nature. - 1973. - 224. - 128129.
20. Ballantine H.T. Jr. et al. Stereotaxic anterior cingulotomy for neuropsychiatric illness and intractable pain // J. Neurosurg. - 1967. - 26. - 488495.
21. Binder D.K., Iskandar B.J. Modern neurosurgery for psychiatric disorders // Neurosurgery. - 2000. - 47. - 923.
22. Whitty C.W.M. et al. Anterior cingulectomy in the treatment of mental disease // Lancet. - 1952. - 1. - 475481. nine0006
23. Martuza R.L. et al. Stereotactic radiofrequency thermal cingulotomy for obsessive compulsive disorder // J. Neuropsychiatry Clin. neurosci. - 1990. - 2. - 331336.
24. Jenike M.A. et al. Cingulotomy for refractory obsessivecompulsive disorder: a longterm followup of 33 patients // Arch. Gen. Psychiatry. - 1991. - 48. - 548555.
Gen. Psychiatry. - 1991. - 48. - 548555.
25. Dougherty D.D. et al. Prospective longterm followup of 44 patients who received cingulotomy for treatmentrefractory obsessivecompulsive disorder // Am. J. Psychiatry. - 2002. - 159. — 269275.
26. Knight G.C. The orbital cortex as an objective in the surgical treatment of mental illness: the development of the stereotactic approach // Br. J. Surg. - 1964. - 53. - 114124.
27. Goktepe E.O., Young L.B., Bridges P.K. A further review of the results of stereotactic subcaudate tractotomy // Br. J. Psychiatry. - 1975. - 126. - 270280.
28. Hodgkiss A.D. et al. Outcomes after the psychosurgical operation of stereotactic subcaudate tractotomy // J. Neuropsychiatry Clin. neurosci. - nineteen95. - 7. - 230234.
29 Montoya A. et al. Magnetic resonance imagingguided stereotactic limbic leukotomy for treatment of intractable psychiatric disease // Neurosurgery. - 2002. - 50. - 10431049.
30. Price B.H. et al. Cassem, Improvement in severe selfmutilation following limbic leucotomy: a series of 5 consecutive cases // J. Clin. Psychiatry. - 2001. - 62. - 925932.
Cassem, Improvement in severe selfmutilation following limbic leucotomy: a series of 5 consecutive cases // J. Clin. Psychiatry. - 2001. - 62. - 925932.
31. Leksell L. A stereotaxic apparatus for intracerebral surgery // Acta Chir. Scand. - nineteen49. - 99. - 229233.
32. Leksell L., Backlund E.O. Stereotactic gamma capsulotomy // Hitchcock E.R., Ballantine H.T. Jr., Meyerson B.A. (Eds.) Modern Concepts in Psychiatric Surgery, Elsevier. - New York: North Holland Biomedical Press, 1979. - 213216.
33 Bingley T. et al. Longterm results of stereotactic capsulotomy in chronic obsessivecompulsive neurosis // Sweet W.H., Obrador S., MartinRodriguez J.G. (Eds.) Neurosurgical Treatment in Psychiatry, Pain, and Epilepsy. — Baltimore: University Park Press, 1977. - 287299.
34. Diering S.L., Bell W.O. Functional neurosurgery for psychiatric disorders: a historical perspective // Stereotact. Funct. neurosurgery. - 1991. - 57. - 175194.
35. Neurosurgery working group of the Royal College of Psychiatrists. Neurosurgery for mental disorders. Council Report CR89. — London, June 2000.
Neurosurgery for mental disorders. Council Report CR89. — London, June 2000.
36 Vilela Filho O. et al. SPECTbased tailoring of psychosurgical procedures: is it possible? // Stereotact. Funct. neurosurgery. - 2001. - 76. - 256261. nine0006
Psychosurgery
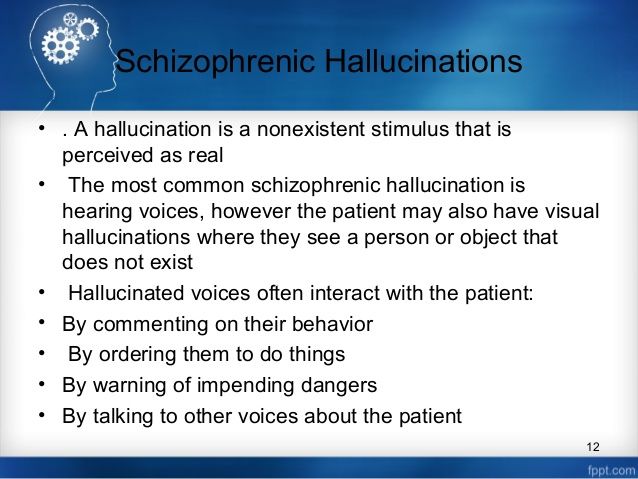
In foreign literature, it is generally accepted that only in 1935, psychosurgical treatment began to be used for the treatment of schizophrenia - prefrontal lobotomy. However, back in 1907 in the clinic of V.M. Ankylosing spondylitis, leucotomy was performed.
L.M. Pussep. In 1908 V.M. Bekhterev and L.M. Pussep recognized the operation as inexpedient. Somewhat earlier, G. Burkhart advised treating severe mental illness by excising various areas of the cerebral cortex. In 1888, he removed part of the right temporal lobe from a patient suffering from hallucinations and delusions. nine0006
In 1927, the Portuguese physician E. Moniz suggested that certain mental disorders are the result of pathologically stable connections between groups of neurons. He believed that there were "destructive psychoses" and "psychofunctional psychoses" due to special formations in cell groups related to obsessive thoughts and delirium. The goal of psychosurgery, in his opinion, should be the destruction of the bonds of pathological cell groups. This hypothesis, according to P. Pichot (1983), was the result of moving into the psychological sphere of neuronal associationism and neurophysiological interpretation of conditioned reflexes by I.P. Pavlova.
He believed that there were "destructive psychoses" and "psychofunctional psychoses" due to special formations in cell groups related to obsessive thoughts and delirium. The goal of psychosurgery, in his opinion, should be the destruction of the bonds of pathological cell groups. This hypothesis, according to P. Pichot (1983), was the result of moving into the psychological sphere of neuronal associationism and neurophysiological interpretation of conditioned reflexes by I.P. Pavlova.
E. Moniz's hypothesis contributed to the interest in leukotomy (leuxos - white, touh - dissection). On the advice of E. Moniz, the neurosurgeon A. Lima in 1936 performed a leucotomy - a dissection of the white fibers connecting the frontal lobes with the central structures of the brain. E. Monitz called this operation "prefrontal lobotomy".
For the operation of prefrontal leukotomy, E. Moniz was awarded, according to many psychiatrists, an undeserved Nobel Prize. However, a tragic end awaited him. One of those patients who underwent a psychosurgical operation "went into a frenzy" and shot at Moniz. After that, the doctor became a severe invalid due to spinal damage (Dobrokhotova T.A., Bragina N.N., 2006). nine0006
One of those patients who underwent a psychosurgical operation "went into a frenzy" and shot at Moniz. After that, the doctor became a severe invalid due to spinal damage (Dobrokhotova T.A., Bragina N.N., 2006). nine0006
The Californian psychologist R. Sperri was also awarded the Nobel Prize for describing the mental state of patients after brain-split surgery.
In Europe, leucotomy became widely used after World War II. In 1942, W. Freeman and J. Watts proposed an "affective hypothesis" of prefrontal leucotomy, according to which the transection of the frontal-thalamic joints leads to retrograde degeneration of the dorsomedial nucleus of the thalamic thalamus, which, according to the authors of the hypothesis, plays an important role in establishing connections between the ideational and affective area. At the same time, scientists noted that satisfactory results are possible after a fairly extensive lobotomy. After the operation, out of 80 operated patients, 4 patients died, 3 patients developed convulsive seizures, and a number of individuals developed explosiveness and tactlessness instead of preoperative anxiety, nervous tension, obsessive thinking, depression, hallucinations and delirium. nine0006
nine0006
Patients who underwent prefrontal leukotomy rarely came into conflict with the law, because "lack of imagination did not give them the opportunity to think of new atrocities", in addition, they simply did not have the strength to implement them in practice (Older J., 1974 ).
In the USSR at the Institute of Neurosurgery, headed by A.S. Shmaryan, a group of psychiatrists left a detailed description of the condition of patients with schizophrenia before and after prefrontal leukotomy (Golodets R.Kh., 1948; Goldenberg S.I., 1948; Zeigarnik B.V., Galperin P.Ya., 1948; Luria A.R., Rozinsky Yu.B., 1948 and others).
VA Gilyarovsky (1950) believed that leucotomy as a method of therapy requires great care and can be used only if schizophrenia continues for a sufficiently long time without revealing the severity of the process. According to the scientist, leucotomy quite often led to adverse consequences 2-3 years after the operation. The issue of gross pathohistological and architectonic changes after prefrontal leucotomy in the domestic literature was once covered in sufficient detail by Yu. G. Shevchenko (1954). In the end, the operation of prefrontal leukotomy was banned in the USSR.
G. Shevchenko (1954). In the end, the operation of prefrontal leukotomy was banned in the USSR.
T. Dobrokhotova et al. (2006) in their book "Neuropsychiatry" present the results of a study by F.I. Sluchevsky and M.E. Petsevich of the outcomes of prefrontal leukotomy in 15 patients operated on in 1948.
The authors identified three types of schizophrenia outcomes:
- "gradual and typical transformation of the syndrome to paraphrenic with its subsequent disintegration and the formation of a" schizophrenic defect "; nine0180
- transformation of the syndrome with manifestations of an organic psychosyndrome;
- manifestations of only the latter (euphoria, complacency, intellectual-mnestic decline).
Scientists suggested that leucotomy in its mechanism of action resembles the effect of sedatives, eliminating primarily the affective component of painful experiences. At the same time, the side effects of the operation, unfortunately, were irreversible, as a result of which such interventions were proposed to be considered unacceptable, neither from the point of view of therapeutic efficacy, nor from the point of view of medical ethics. nine0006
nine0006
Observations on patients subjected to frontal leucotomy showed that hallucinations, in the case when they are secondary and grow as a result of delusional experiences, can disappear as a result of surgical intervention (Rozinsky Yu.B., 1950).
In the works of M.A. Goldenberg (1950) showed that the second leukotomy operation, performed on the opposite side, often led to an improvement in the condition of patients, where the first operation did not give the desired effect. The author came to the conclusion that frontal leukotomy is especially indicated for chronic forms of schizophrenia and presenile depression. The mechanism of the therapeutic effect of M.A. Goldenberg explained that the mildly expressed symptoms of the frontal lobes, as it were, overlapped the schizophrenic symptoms observed before the operation. nine0006
Interest in prefrontal leucotomy increased after F. Jacobson, a scientist at Yale University in the United States, discovered that cutting the fibers of the prefrontal lobes in monkeys leads to greater obedience and also contributes to stress tolerance. It should be noted that despite the indignation of many psychiatrists, in the 50s of the 20th century, about 10,000 prefrontal leukotomy operations were performed in patients with schizophrenia in England alone. The total number of patients with schizophrenia operated on for 25 years, according to some researchers, was 100,000 people. In the late 1980s, the use of prefrontal leucotomy practically ceased. nine0006
It should be noted that despite the indignation of many psychiatrists, in the 50s of the 20th century, about 10,000 prefrontal leukotomy operations were performed in patients with schizophrenia in England alone. The total number of patients with schizophrenia operated on for 25 years, according to some researchers, was 100,000 people. In the late 1980s, the use of prefrontal leucotomy practically ceased. nine0006
It is currently believed that the high requirements for the operation of prefrontal leukotomy (the operation consists in one- and / or bilateral cutting of the fronto-thalamic pathways connecting the frontal hemispheres with subcortical formations), its complexity and complications, have reduced the popularity of this method of treating schizophrenia . An important role here was also played by the moral and ethical aspects of this operation, which, in fact, sharply limit the rights of the patient.
In the last quarter of the twentieth century, psychosurgery began to experience a new stage in its development. Doctors began to use ultrasound, perform “local” lobotomy, cingulotomy, gyrectomy, bimedial leucotomy and other surgical methods of influencing brain tissue (Shevitz S., 1976).
Doctors began to use ultrasound, perform “local” lobotomy, cingulotomy, gyrectomy, bimedial leucotomy and other surgical methods of influencing brain tissue (Shevitz S., 1976).
Psychosurgery began to move from a blind method with the destruction of large areas of the gray and white matter of the brain with a surgeon's scalpel to more conservative and pinpoint surgery: radiofrequency thermoregulation, cryotherapy, exposure to gamma radiation ("gamma knife").
Traumatic operations have given way to stereotaxic interventions: subcaudate tractomy (penetration takes place at the level of the rostral part of the orbital cortex), anterior cingulotomy, libibular leucotomy (subcaudate tractomy is combined with scurvy), anterior capsulotomy. The most popular operations in Europe (UK) are anterior capsulotomy and anterior cingulotomy. nine0006
Modern psychosurgery today can be effective for severe depression in almost 60% of cases (Royal College of Psychiatrists., 2000).
Complications of modern methods of psychosurgery include headaches, nausea, general malaise, which are observed in almost 10% of patients who have undergone such an intervention.