Why does life not feel real
Why Doesn't Reality Feel Real to Me? Depersonalization Disorder
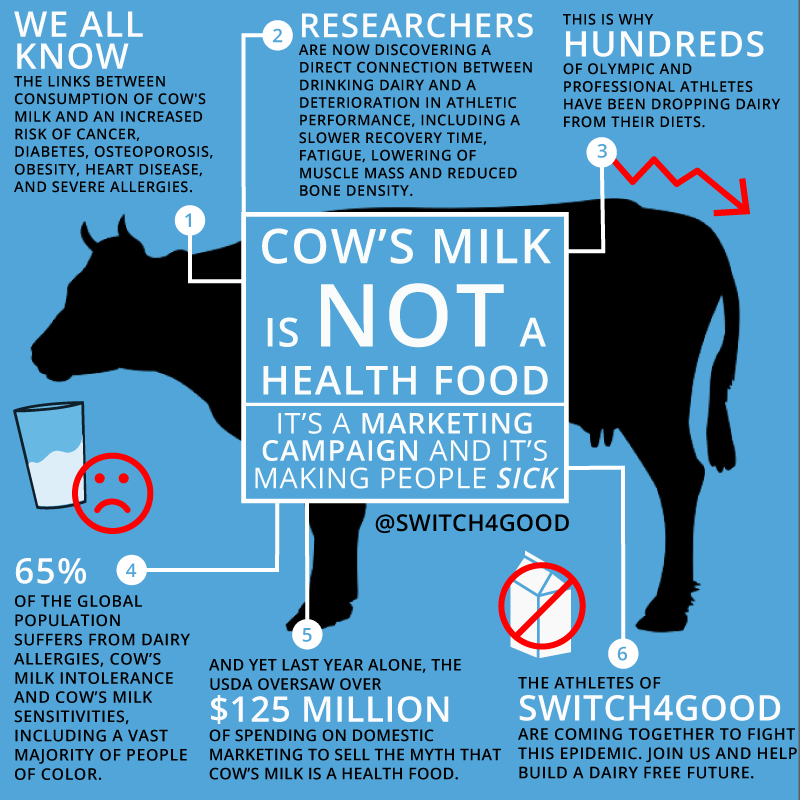
What is depersonalization (derealization) disorder? Have you ever experienced segments of time when the world around you felt distinctly surreal? Or detached from your surroundings? Maybe you often find yourself “outside of yourself” and “looking in from outside to observe your own life?” You’re not alone; it very well may not be your imagination. This phenomenon really “is a thing.”
Depersonalization disorder is a type of dissociative disorder that characteristically manifests itself through persistent/recurring feelings of detachment (dissociation) from one’s body and/or cognitive processes, not unlike a psychotic episode.
While that may not seem like the worst thing that could happen to you, some patients find the experience nothing short of terrifying. One such notable case is Adam Duritz of the Counting Crows, who deals with depersonalization disorder on a regular, daily basis.
It’s common for those with the disorder to feel as if the world were lifeless, colorless, and even “fake. ” They may feel as though they were dreaming, in a fog, or as though a veil or glass wall separated them from their immediate surroundings. A subjective sense of distortion may also occur, e.g. unusually blurry or sharply clear objects, objects that may seem smaller, larger, or visibly “flat.” Often time may seem to be going much slower or faster than usual, and sounds and noises may seem unbearably louder or softer than they actually are.
Such symptoms of depersonalization disorder can typically be distressing, and some patients feel as though they may have irreversible cerebral damage, or even that they are losing their minds. Some patients may obsess over whether or not they really exist, or may compulsively check over and over to verify whether or not their perceptions are for real. Most patients, however, are able to maintain an awareness of the fact that these experiences are unreal, and this is what differentiates the disorder from a psychotic episode, where such awareness is absent. A memory may frequently lapse, and patients may not be able to feel, identify, or express their emotions.
A memory may frequently lapse, and patients may not be able to feel, identify, or express their emotions.
What are the causes of depersonalization disorder? The disorder is typically triggered by acute stress and may be accompanied by depression and/or anxiety. Driving stress factors often involve one or more of the following:
- Losing a close a family member or friend unexpectedly
- Having a severely impaired or mentally ill parent
- Emotional or physical abuse or being neglected as a child (probably the most common cause)
- Exposure to domestic violence
Other triggers include financial, relationship, or job-related stress, and the use of illegal drugs such as hallucinogens, marijuana, and ketamine.
A proper diagnosis is driven by certain symptoms, but only after other possible causes are ruled out.
Three of the dynamics that may lead to a clinical diagnosis include persistent or recurring experiences with depersonalization, an awareness that the depersonalization episodes are only a subjective experience and not real, and symptoms that cause the patient acute distress, or that may greatly impair occupational/social functioning.
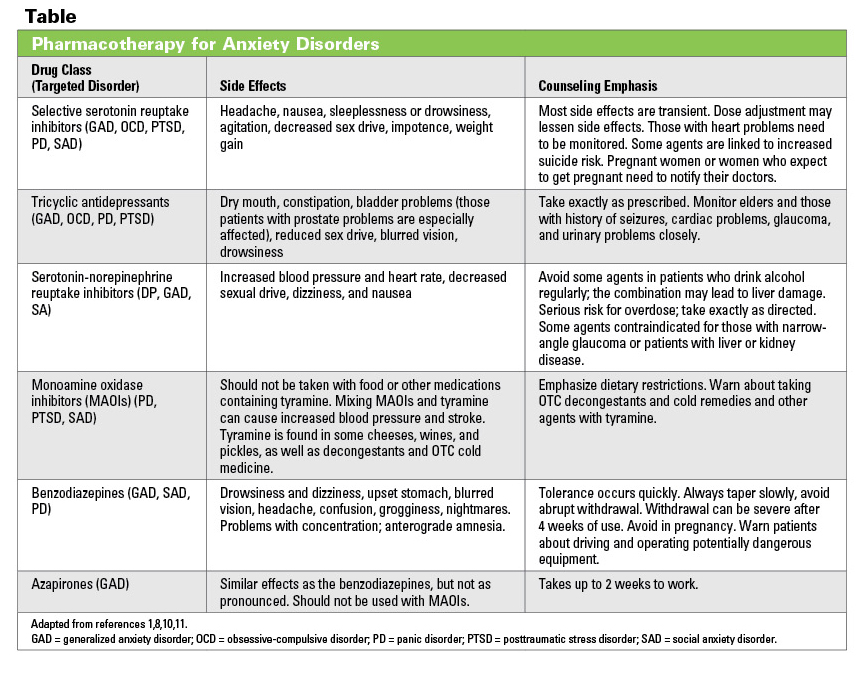
If all this seems relatable to you or someone you care about, there is treatment and help. Treatment of depersonalization disorder will typically involve psychotherapy, and possibly medication. Treatment for depression and/or anxiety may also be administered concurrently.
One thing to keep in mind is that depersonalization disorder, though stressful at times, is manageable, and you will still be able to live a normal life.
Are you struggling with feelings of life being surreal? Not to worry, you’re not going crazy, and it is treatable. If you or someone close to you need to talk to someone about mental health issues that seem overwhelming, we can help. Consider reaching out to our expert team at Solara Mental Health at 844-600-9747.
When Life Doesn't Feel Real Anymore
“This just doesn’t feel real anymore.” Perhaps that statement echoes an experience you have had recently that felt surreal? For many, this experience of “unreality” became more prolific during 2020 with the sudden changes brought forth by the pandemic.
I remember this feeling when standing in a grocery store and finding conspicuously empty shelves due to shortages while also witnessing the frenzy of shoppers nervously loading carts with whatever they could find.
During stressful experiences, a person may feel like their perception of reality has suddenly shifted into something strangely unfamiliar. They may also feel disconnected from their sense of “self.” Life can bring about impactful events that change or alter our reality, such as the sudden and unanticipated loss of a loved one, exposure to intensely frightening situations, or when presented with any stressful discrepant event. Some of my patients have conveyed their reactions to such events as feeling beside themselves, detached, out of their body, or like living in a dream.
Unreality
Source: Natallia/Adobe Stock Photos', 'Social Issues, licensed for use'.'.
These are all emotional responses to situations that can produce destabilizing effects on one’s self and perception, resulting in the experiences of
depersonalization and derealization. Depersonalization and derealization are complex reactions that used to be considered differing disorders until 2013 when the American Psychiatric Association consolidated them as a depersonalization-derealization disorder or DP/DR.
Depersonalization and derealization are complex reactions that used to be considered differing disorders until 2013 when the American Psychiatric Association consolidated them as a depersonalization-derealization disorder or DP/DR.
We Count on Stability
All of us depend on a degree of stability to go about our daily lives. For the most part, our experience and sense of self within our environment are typically stable and coherent. A person’s sense of orientation, such as who they are and where they are calibrated through an array of complex cognitive functions like perception.
Perception
Source: ' 1STunningART/Adobe Stock Photos', 'licensed for use'.
Perception allows us to recognize a friend’s face, experience the world through our senses, and more. However, in the presence of extreme stressors, such perceptual processes may be affected harshly, and symptoms may start to surface. Let’s take a look at a few of the symptoms associated with the depersonalization-derealization disorder (Depersonalization-Derealization Disorder, 2017).
Symptoms of Depersonalization
- Feeling like an outside observer to your experience, remote from body or parts of your body, as if “floating above one’s self.”
- Feeling as though your body is distorted exaggeratedly.
- Physical or emotional numbness of senses in response to your environment.
Symptoms of Derealization
- Unlike depersonalization’s “out of body” experience, derealization may feel more like “alienation” or unfamiliarity to one’s surroundings.
- Surroundings become distorted, blurry, artificial, or have a "dreamlike" effect.
- Distortions in time, distance, and sound are common.
According to researchers Schlax et al. (2020), many of the symptoms of DP/DR result from an impairment regarding the capacity to regulate one’s own emotions. Most often, passing feelings of both depersonalization and derealization are common. About 50% of people have had at least one such experience in their lifetime. However, when these feelings persist, it is an excellent time to seek out the assistance of a healthcare professional.
However, when these feelings persist, it is an excellent time to seek out the assistance of a healthcare professional.
Treatment for DP/DR
Typically, an excellent place to start is with your local physician. Physicians have access to imaging tests such as MRI’s, EEG’s, and basic toxicology tests to rule out anything of a physical nature and will probably recommend seeing a therapist.
Within the field of mental health, psychotherapy is considered one of the primary options in treating DP/DR. Psychotherapy offers clients opportunities to unburden themselves by sharing their experiences and can benefit a person experiencing DP/DR by helping them understand their experiences and make sense of things.
Modifying Intense Feelings
When symptoms from DP/DR begin, you can immediately use some grounding principles to stay rooted, calm, and re-orient yourself.
Modify Feeling
Source: galitskaya/Adobe Stock Photo, Man doing yoga, licensed for use.
Here are a few you can try:
Engage a symbolically activating practice–Some creative Cognitive Behavioral Therapy (CBT) may help. Rooted in modifying behaviors, CBT can engage techniques like self-talk and symbolic activities for changing thoughts.
Rooted in modifying behaviors, CBT can engage techniques like self-talk and symbolic activities for changing thoughts.
One strategy I use with anxious patients is to invoke a powerful symbolic act with self-talk like washing their hands. Water is grounding, and it is also seen as purifying. While washing hands, we say, "I release the anxiety I feel right now, I am washing it away, letting my senses engage calmness and the gentle sensation of the cleansing water in the here and now."
In such an activity, you create powerful imagery while using self-talk to help guide your way out of intense feelings. Additionally, you are connecting mind and body while modifying the moment.
Try a chant–You may know of the Om chant used by Monks in both Hindu and Buddhist traditions. The practice of the vocal chant can be used to stimulate the vagus nerve. The gliding vowel sound can be felt throughout the body and is a good distraction for the mind and body.
Listen to music–Music can be a suitable grounding mechanism as music has been shown to reduce cortisol levels which affect stress.
Read a book–From a study at the University of Sussex, participants who read for six minutes had displayed lower heart rates and reduced stress. Reading fiction engages our imagination, stimulates our subjective mode of thinking, and involves dynamic imagery.
Journaling–Once you have down-regulated the moment's intensity, find time to journal your experience as another powerful symbolic way to process your feelings.
Education is power, and there are many helpful resources, such as this video by Melissa Shepard on DP/DR. The good news is that DP/DR disorder is often only a transient condition during stressful times, and most people fully recover. With good self-care and treatment, you can stay in control and maintain a better quality of life.
Depersonalization: a syndrome that interferes with feeling - BBC News
Image caption,Sarah says that because of her illness, familiar places seem like decorations
People with depersonalization syndrome see the world as unreal, two-dimensional, as if in a fog. Every hundredth suffers from this disorder, but despite this, British doctors are not taught to work with such patients, experts say.
Every hundredth suffers from this disorder, but despite this, British doctors are not taught to work with such patients, experts say.
"The connections you think are valuable lose their original meaning. You know you love your family. But the thing is, you're more aware of it than you feel it," says Sarah on Victoria Derbyshire's BBC program. -bc.
Sarah is an actress, she constantly tries on different images and reproduces other people's emotions. But in reality, for most of her conscious life, she is emotionally paralyzed and unable to experience any feelings.
The reason for this is a little-studied mental disorder called depersonalization.
Sarah had the syndrome three times. The first time it happened was when she was preparing for her final exams.
The main sign of depersonalization is the feeling that a person loses physical connection with the world around him and his own body.
It is believed that this is how a defense mechanism manifests when, during stress or a serious shock, consciousness is disconnected from reality. Some drugs, such as marijuana, can cause the same effect.
Some drugs, such as marijuana, can cause the same effect.
- Depression: a breakthrough in understanding the nature of the disease and its
- What your selfies say about you
- Google helps users recognize depression
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
For people with depersonalization syndrome, the world can change in a second.
"It was an unexpected switch. Everything around seemed alien and even intimidating. Suddenly, the apartment and other places where you used to be become a film set for you, and all your things become scenery," says Sarah.
Other patients report feeling that they are outside their body, that it does not belong to them, and that the world around them seems two-dimensional and flat.
This happened to Sarah during the second episode.
"I was reading, I had a book in my hands. And suddenly my hands began to look like a picture on which two hands were drawn. There was a feeling that the real world and my perception of it did not coincide."
Sarah's disorder is not uncommon. Three independent studies have proven that it occurs in one person out of a hundred.
Experts say the disorder has long been recognized as a medical condition. It is as common as obsessive-compulsive disorder or schizophrenia.
Some untreated patients may suffer lifelong depersonalization symptoms. And yet, not all doctors know what it is.
A doctor who recently graduated and suffers from this disorder himself stated that depersonalization was not taught in medical school or in continuing education courses for therapists.
He admitted that he misdiagnosed his patients at least twice. According to him, he will be very surprised if it turns out that at least one of his colleagues has heard about this syndrome.
Sarah says that in her life she encountered at least 20 professionals who had no idea what she was talking about. Among them are consultants, therapists, district psychiatrists and doctors.
The Royal College of General Practitioners (RCGP) in London said that mental health was a key element of an expanded curriculum for physicians.
The institute added that the study of more complex psychological problems is still in development.
The Royal College of Psychiatry stressed the need to ensure that these disorders are properly understood.
Image caption,Dr Elaine Hunter runs the only referral center in the UK that treats patients with depersonalization
Poor diagnosis is only part of the problem, access to treatment is another complication.
There is only one specialist clinic in the UK. Its resources are limited, it can only accept 80 patients a year. Despite the fact that 650 thousand people can potentially suffer from this disease.
To access this health center free of charge, a referral from a local doctor is required. And even if the patient is diagnosed with depersonalization, treatment will have to wait several months or longer.
After a year of waiting in line, Sarah decided that the only way out was to pay for the treatment herself.
"I used to have panic attacks all the time. It's really scary. I knew it was a crisis," she says.
A specialist center for patients with depersonalization syndrome operates at the Maudsley Hospital in south London. However, there are restrictions for patients under 18 years of age; the center only treats adults.
Often the disease occurs in adolescence. Dr. Elaine Hunter, who heads the center, is concerned that she has to withhold care for children and adolescents.
"Sometimes 15-year-old patients come to us deeply depressed and frightened, but we have nothing to offer them," she says.
One of the adult patients of the center developed the syndrome at the age of 13. For two years she could not leave the house, she experienced ten panic attacks a day caused by the disorder.
At the beginning of the treatment, she did not even recognize her own parents.
Dr. Hunter hopes that over time, the right treatment will be available to underage patients.
She believes that treatment should be organized in every district. Physicians in local centers for psychological assistance should undergo special training, then disseminate information among other specialists.
Image caption,Sarah Ashley couldn't eat or sleep until she was treated by Dr. Hunter
Hunter developed Cognitive Behavioral Therapy (CBT) specifically for patients with depersonalization. She believes that she will be easily mastered by doctors who already have experience in talking therapy.
She believes that she will be easily mastered by doctors who already have experience in talking therapy.
Sarah Ashley, a patient of Dr. Hunter, says she was initially skeptical about the technique, but after a while she felt a huge difference.
"[Before CBT] I looked at my own hands or other body parts and felt like they weren't mine. I looked at myself in the mirror and didn't realize it was me," explains Sarah.
"I couldn't eat or sleep, and due to stress I lost 42 kg. Now I still have some symptoms, but I can get over them quickly," she continues.
Treatment is available but difficult to obtain.
As Dr. Hunter says, we need to correct the situation in which patients are forced to look up information about their disorder on the Internet, and then explain to the doctor what it is about. Instead of, on the contrary, the doctor told the patient about his illness.
What is it like to live when you do not feel reality
Imagine: one day you wake up, look in the mirror and try to recognize yourself in it. Worse, you feel like you're watching your life from the sidelines, like you're watching a bad and boring movie. It becomes increasingly difficult for you to interact with others, because too much energy is spent trying to deal with strange sensations.
These are all frightening symptoms of a dissociative disorder called depersonalization/derealization syndrome, or DP-DR. It appears as a result of psychological trauma or drug use and can last from a couple of hours to several years. This strange, little-talked about condition causes people to lose touch with their body, emotions, environment, and even family. From the moment the first symptoms appear, life turns into a constant struggle with a sense of the unreality of what is happening, in which it is almost impossible to catch one's own "I".
As part of Mental Health Week, we interviewed several people to find out what it's like to constantly feel out of touch with reality.
SOPHIE, 19, LONDON
With DP-DR, looking at your reflection in the mirror or hearing your own voice is quite strange, because they seem not real. Then this feeling grows, and everything around seems unreal. You feel like a thread of emotions and thoughts, alone in this alien world. Usually this condition goes away in a few hours or days, but I have been living like this for two and a half years.
DP-DR often complements and exacerbates nervousness and depression. In fact, symptoms are common. Many experience similar feelings due to overwork or stress. Smoking weed or using hallucinogenic drugs can also trigger self-perception disorders. Sensation of complete exhaustion of consciousness, like a fog in the head. Right now my head is wadded, my eyes are sticking together, I want to lie down. Thoughts are scattered, it is difficult to focus on something that requires critical thinking or memory work. I tried to practice mindfulness, but it only got worse.
Mental illness dooms a person to loneliness. Friends can accept your feelings and support, but this is of little use. At school, it seems to me, everyone only pretended to understand. Despite the support system, I had the feeling that others believed that I was playing the victim. It seems to me that such judgments are a label that society hangs on everyone with a mental illness. You know, kind of like the typical Tumblr teen talking about anxiety, depression, and "reveling in self-pity" all the time.
It is unfortunate that the words "depersonalization" and "derealization" are so long and hard to pronounce - it is not easy to use them in speech and discuss these disorders with people in ordinary conversation.
JOE, 19, LONDON
I remember the fear and confusion I felt when I first experienced the symptoms of DP-DR. I told my parents that something was wrong with me. Everything around me and in my head felt wrong. Many who suffer from this disorder describe the condition as a dream or the feeling of watching a movie about themselves. I was walking. It was already late when I got home and lay down with depressive thoughts, trying to sleep. Then I suddenly had a panic attack. My heart was beating fast and there was no air in my chest. Rolling onto my back, I tried to control my breathing. And then a switch seemed to flip in my head, and almost instantly the state of DP-DR set in.
I was walking. It was already late when I got home and lay down with depressive thoughts, trying to sleep. Then I suddenly had a panic attack. My heart was beating fast and there was no air in my chest. Rolling onto my back, I tried to control my breathing. And then a switch seemed to flip in my head, and almost instantly the state of DP-DR set in.
At first I noticed that I had completely lost my emotions. I felt nothing but horror. Looking in the mirror, it was as if I could not recognize myself in the reflection - I knew who I was, but did not understand. I was so excited that I decided to wake up my parents. Mom tried to calm me down, and I felt her hand on my body, but only as a physical sensation of her attempts to calm me down. I didn't realize that I knew her. I thought I would never feel my mother's love again. I looked out the window and looked at the backyard where I spent my childhood, and I was not sure that this place was familiar to me. It felt like my memories no longer belonged to me.
Depersonalization is a terrifying condition. According to psychologists, the brain uses it as a tool for survival or protection. By "paralyzing" emotions, DP-DR allows people to think rationally in stressful situations. For example, during a fire, DP-DR syndrome would help a person not to panic, but to focus on escaping. But then the dissociative state must pass. However, if this does not happen, then DP-DR develops into a disorder, life with which is a nightmare.
I'm on medication and sometimes I feel like I'm crazy. I worry about the constant confusion in my head. My ambitions and hopes for the future seem lost. Lately I've begun to wonder how strange my feelings are. My own brain is against me. How can all my sensations and emotions be the product of gray matter under my skull? Nothing else makes sense.
I am trying to distract myself by reading. I also do music. It's a good way - the music really pulls me in. I bought a self-help book about DP-DR syndrome, and it, along with stories of people who have successfully overcome depersonalization, helps the most.
For those who also suffer from DP-DR, I would advise you to keep yourself busy, even if it is extremely difficult in the beginning. Even if the world seems different, go back to your old hobbies. It will get better after a while. If you feel that you are on the verge of insanity, just breathe and try to focus on your surroundings. Chat with friends and don't avoid people.
AUSTIN, 25, SAN FRANCISCO
I had DP-DR symptoms very early, at 15 years old. Of course, initially they were rare and did not bring significant harm. I had a kind of feeling when you look around and think "What?" or when life seems somehow unreal. At the age of 17, they began to manifest themselves stronger and more often. I began to wonder at times if there was something wrong with me or if this is a normal state of any person. I allowed the thought that perhaps this is how adults perceive reality.
Last year, when I graduated from college, my condition worsened dramatically. Now I don't feel alive. I don’t feel emotions and I don’t worry about relationships. I have problems with long term memory. Everything around me seems flat and blurry. It is hard to explain. In this state, you get the feeling that you are a small person inside your own head and looking at the world as if through a TV screen. Communication is very difficult for me, because there is a direct relationship between interest in people and symptoms of DP-DR. It also seems that time flies very quickly.
Now I don't feel alive. I don’t feel emotions and I don’t worry about relationships. I have problems with long term memory. Everything around me seems flat and blurry. It is hard to explain. In this state, you get the feeling that you are a small person inside your own head and looking at the world as if through a TV screen. Communication is very difficult for me, because there is a direct relationship between interest in people and symptoms of DP-DR. It also seems that time flies very quickly.
As a result, my life deteriorated significantly. I became more depressed and less sociable, interested and self-confident. It is hard for me to maintain friendly relations with anyone, because the disease robs me of emotions, and I am simply not able to experience love or affection. But that doesn't mean I feel at ease. The only benefit is that I can keep my cool in stressful situations. I am quite efficient, but I am in a state of constant discomfort 24 hours 7 days a week. I go to a psychotherapist to try to understand the causes of my condition.
It is difficult for me to make friends or make new acquaintances. I had to literally fight with myself in order to maintain a relationship that lasted for four whole years, due to the fact that it is difficult for me to experience love or affection. As friendships begin to fade, I have to remind myself that deep down I love these people and that it's my mental illness that makes me think I don't care about them. But despite this, my friends are happy that I try to be better.
As an artist, I have to work hard to feel inspired. It is very difficult when something that was previously inspiring ceases to cause a surge of dopamine. Escapism is a great way out of this situation. Since reality only provokes discomfort, Netflix and the Internet immerse me in alternate realities over which I have more control. My life improved a lot and my productivity increased a lot when I watched all the episodes of Girls.
Many of those who have been successfully treated talk about the need to stop thinking about DP-DR and try to live as if they never had the disorder.