When switching antidepressants how long does it take to work
Strategies, Side Effects, and More
People may need to switch antidepressants if their existing medication isn’t working as intended. Several strategies can help ease this transition.
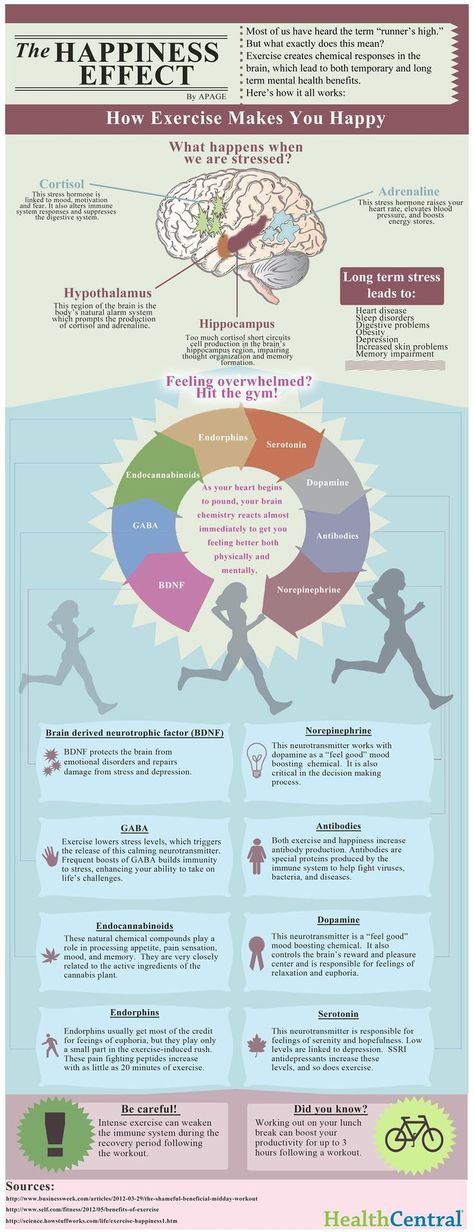
If you’re living with depression, your doctor will likely start you on a treatment plan of antidepressants such as a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI).
It can take a few weeks on one of these drugs to see an improvement. However, not everyone will feel better with the first antidepressant they try.
When an antidepressant doesn’t work as intended, doctors can increase the dose or add other treatments such as cognitive behavioral therapy. These strategies sometimes work — but not always.
In other cases, a change of antidepressants is necessary.
Only one in three people will be symptom-free after taking one type of antidepressant. People who don’t respond to the first drug they try may need to switch to a different antidepressant.
You may also need to switch medications if the first drug you try causes side effects you can’t tolerate, such as weight gain or lowered sex drive.
Don’t stop taking your medication without first checking with your doctor. Switching treatment is a careful process. Stopping your current medication too quickly can lead to withdrawal symptoms or cause your depression symptoms to return. Your doctor must monitor you for side effects or problems during the switch.
Doctors use four different strategies to switch people from one antidepressant to another:
- Direct switch: In a direct switch, you stop taking your current drug and start on a new antidepressant the next day. It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class.
- Taper and immediate switch: In this switching method, you gradually taper off your current drug. As soon as you’ve fully stopped the first drug, you start taking the second drug.
- Taper, washout, and switch: This is a conservative method of switching in which you gradually taper off the first drug and wait for it to leave your system before switching to the new medication.
- Cross taper: You gradually taper off the first drug while increasing the second dose. This can be beneficial when switching to a drug in a different antidepressant class.
The strategy your doctor will choose will depend on factors such as:
- The severity of your symptoms: It isn’t safe for some people to go off their antidepressants for
several days or weeks. - Concerns over symptoms: Cross-tapering can help prevent you from having withdrawal symptoms.
- Which drugs you take: Certain antidepressants can interact in dangerous ways and
can’t be cross-tapered. For example, doctors won’t combine clomipramine (Anafranil) with SSRIs, duloxetine (Cymbalta), or venlafaxine (Effexor XR).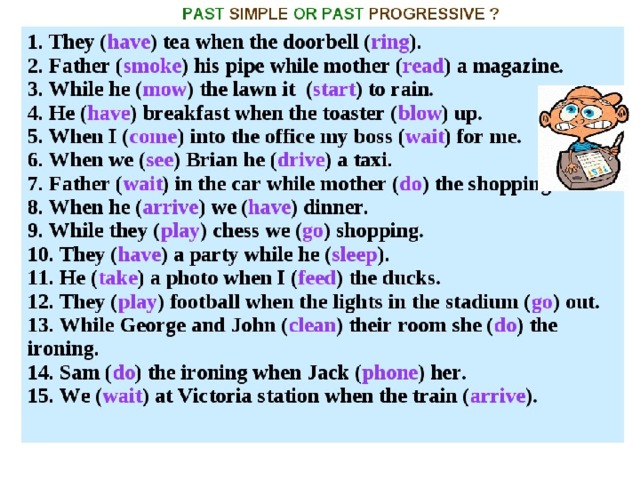
Here’s a chart with information about how your doctor may switch your drugs.
| From | To | How to switch |
|---|---|---|
| SSRI or SNRI | SSRI or SNRI | • Direct switch • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Tricyclic antidepressant (TCA) | • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Non-SSRI, non-SNRI, non-TCA | • Cross taper • Taper, washout, switch • Taper and switch |
| TCA | Any antidepressant | Cross taper |
| Monoamine oxidase inhibitors (MAOI) | Any antidepressant | Taper, washout, switch |
| Any antidepressant | MAOI | Taper, washout, switch |
| Bupropion | Any antidepressant | Cross taper |
Changing from one antidepressant to another can cause side effects.
Withdrawal
Reducing your antidepressant dose or stopping medication entirely can cause withdrawal symptoms, including:
- restlessness
- trouble sleeping
- stomach problems
- sweating
- unsteadiness
Serotonin syndrome
If you start taking a new medication before the old one is out of your system, you can develop a rare but serious condition called serotonin syndrome.
Certain antidepressants work by increasing the amount of the chemical serotonin in your brain. The added effects of more than one antidepressant can lead to an excess of serotonin in your body.
Symptoms of serotonin syndrome include:
- agitation
- nervousness
- tremor
- shivering
- heavy sweating
- diarrhea
- fast heart rate
- confusion
More severe cases can cause symptoms such as:
- hyperthermia
- coma
- seizures
- delirium
- muscle rigidity
Call your doctor or go to an emergency room right away if you have any of these symptoms.
Talk with a doctor if you have side effects that don’t improve. You might need to make another medication switch.
Once you’ve been on antidepressants, your body gets used to the drug. When you try to stop taking the antidepressant, you can experience withdrawal symptoms. Slowly tapering off your antidepressant can help you avoid these symptoms.
Doctors will typically lower your antidepressant dose over the course of 4 or more weeks.
A washout period is the waiting time of a few days or weeks after stopping the old drug before starting the new one. This lets your body clear the old drug out of your system. This often takes 2 to 5 days.
Once the washout period is over, you’ll usually start with a low dose of the new drug. Your doctor will slowly increase the dose, titrating up until it starts to relieve your symptoms.
There are different types of antidepressants, and people respond to them differently. Only one-third of people experience symptoms remission from their first course of antidepressants.
If your antidepressants don’t work, you may need to switch medications.
When switching antidepressants, it’s common to taper down your medications before switching, and doctors may also require you to wait days or weeks before taking a new medication. These strategies can help lower the risk of adverse drug interactions.
Strategies, Side Effects, and More
People may need to switch antidepressants if their existing medication isn’t working as intended. Several strategies can help ease this transition.
If you’re living with depression, your doctor will likely start you on a treatment plan of antidepressants such as a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI).
It can take a few weeks on one of these drugs to see an improvement. However, not everyone will feel better with the first antidepressant they try.
When an antidepressant doesn’t work as intended, doctors can increase the dose or add other treatments such as cognitive behavioral therapy.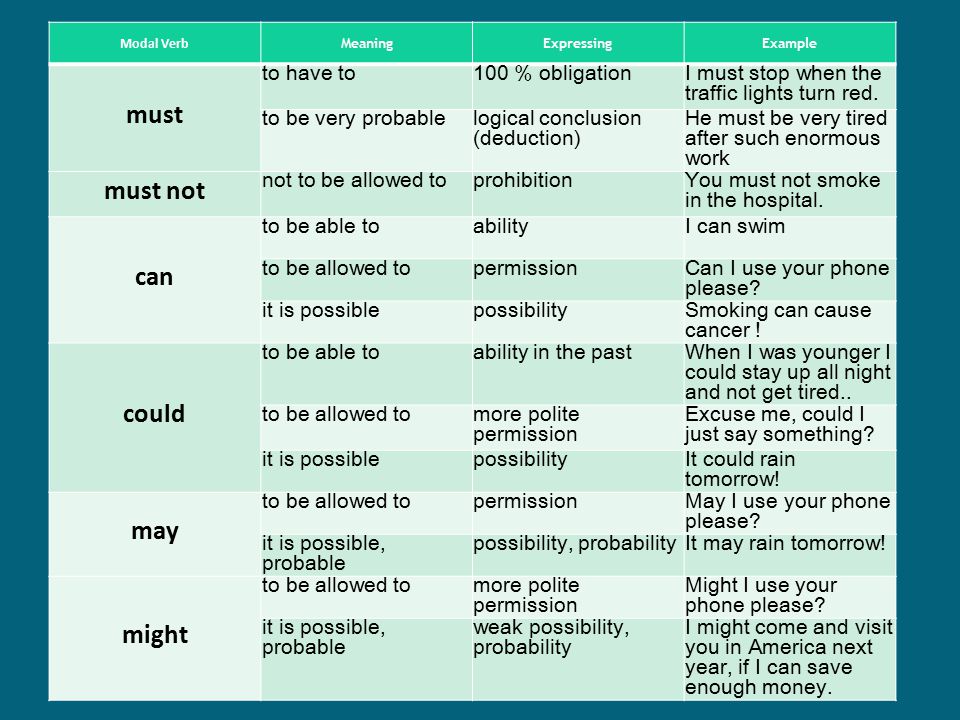 These strategies sometimes work — but not always.
These strategies sometimes work — but not always.
In other cases, a change of antidepressants is necessary.
Only one in three people will be symptom-free after taking one type of antidepressant. People who don’t respond to the first drug they try may need to switch to a different antidepressant.
You may also need to switch medications if the first drug you try causes side effects you can’t tolerate, such as weight gain or lowered sex drive.
Don’t stop taking your medication without first checking with your doctor. Switching treatment is a careful process. Stopping your current medication too quickly can lead to withdrawal symptoms or cause your depression symptoms to return. Your doctor must monitor you for side effects or problems during the switch.
Doctors use four different strategies to switch people from one antidepressant to another:
- Direct switch: In a direct switch, you stop taking your current drug and start on a new antidepressant the next day.
 It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class.
It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class. - Taper and immediate switch: In this switching method, you gradually taper off your current drug. As soon as you’ve fully stopped the first drug, you start taking the second drug.
- Taper, washout, and switch: This is a conservative method of switching in which you gradually taper off the first drug and wait for it to leave your system before switching to the new medication.
- Cross taper: You gradually taper off the first drug while increasing the second dose. This can be beneficial when switching to a drug in a different antidepressant class.
The strategy your doctor will choose will depend on factors such as:
- The severity of your symptoms: It isn’t safe for some people to go off their antidepressants for
several days or weeks. - Concerns over symptoms: Cross-tapering can help prevent you from having withdrawal symptoms.
- Which drugs you take: Certain antidepressants can interact in dangerous ways and
can’t be cross-tapered. For example, doctors won’t combine clomipramine (Anafranil) with SSRIs, duloxetine (Cymbalta), or venlafaxine (Effexor XR).
Here’s a chart with information about how your doctor may switch your drugs.
| From | To | How to switch |
|---|---|---|
| SSRI or SNRI | SSRI or SNRI | • Direct switch • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Tricyclic antidepressant (TCA) | • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Non-SSRI, non-SNRI, non-TCA | • Cross taper • Taper, washout, switch • Taper and switch |
| TCA | Any antidepressant | Cross taper |
| Monoamine oxidase inhibitors (MAOI) | Any antidepressant | Taper, washout, switch |
| Any antidepressant | MAOI | Taper, washout, switch |
| Bupropion | Any antidepressant | Cross taper |
Changing from one antidepressant to another can cause side effects.
Withdrawal
Reducing your antidepressant dose or stopping medication entirely can cause withdrawal symptoms, including:
- restlessness
- trouble sleeping
- stomach problems
- sweating
- unsteadiness
Serotonin syndrome
If you start taking a new medication before the old one is out of your system, you can develop a rare but serious condition called serotonin syndrome.
Certain antidepressants work by increasing the amount of the chemical serotonin in your brain. The added effects of more than one antidepressant can lead to an excess of serotonin in your body.
Symptoms of serotonin syndrome include:
- agitation
- nervousness
- tremor
- shivering
- heavy sweating
- diarrhea
- fast heart rate
- confusion
More severe cases can cause symptoms such as:
- hyperthermia
- coma
- seizures
- delirium
- muscle rigidity
Call your doctor or go to an emergency room right away if you have any of these symptoms.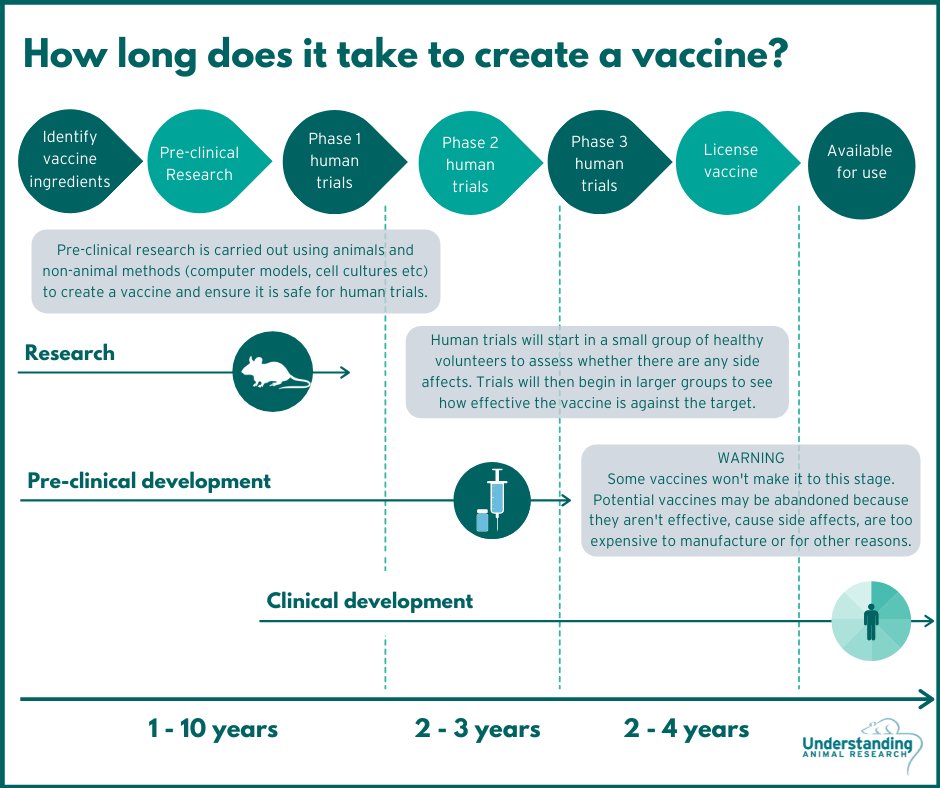
Talk with a doctor if you have side effects that don’t improve. You might need to make another medication switch.
Once you’ve been on antidepressants, your body gets used to the drug. When you try to stop taking the antidepressant, you can experience withdrawal symptoms. Slowly tapering off your antidepressant can help you avoid these symptoms.
Doctors will typically lower your antidepressant dose over the course of 4 or more weeks.
A washout period is the waiting time of a few days or weeks after stopping the old drug before starting the new one. This lets your body clear the old drug out of your system. This often takes 2 to 5 days.
Once the washout period is over, you’ll usually start with a low dose of the new drug. Your doctor will slowly increase the dose, titrating up until it starts to relieve your symptoms.
There are different types of antidepressants, and people respond to them differently. Only one-third of people experience symptoms remission from their first course of antidepressants.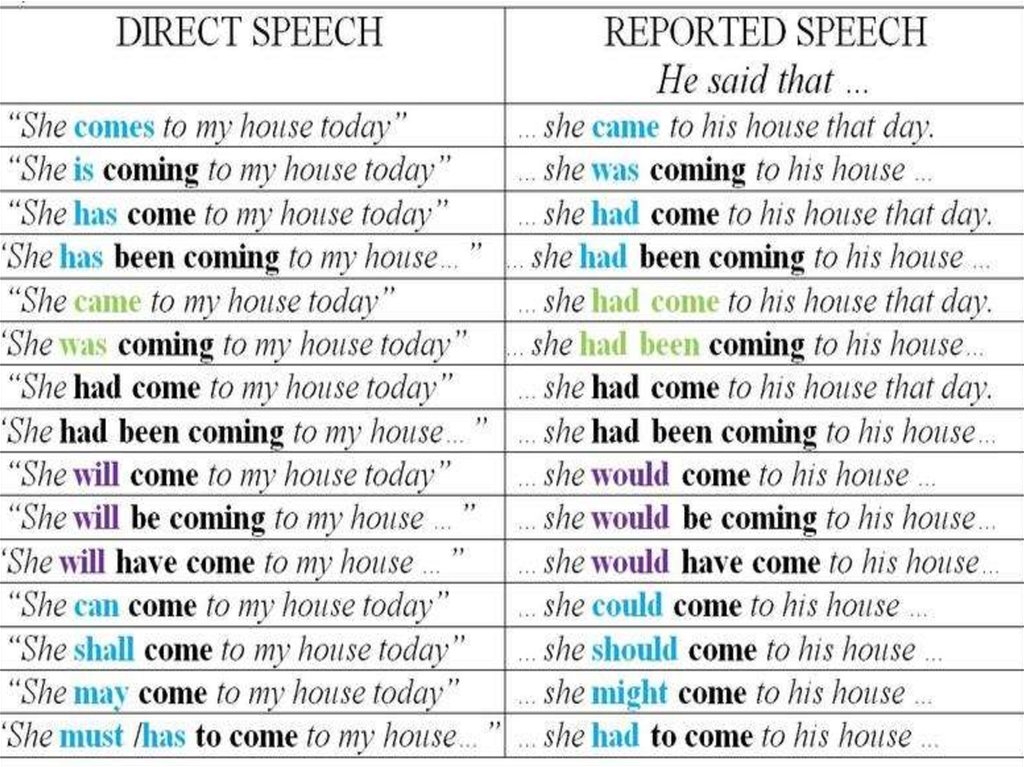
If your antidepressants don’t work, you may need to switch medications.
When switching antidepressants, it’s common to taper down your medications before switching, and doctors may also require you to wait days or weeks before taking a new medication. These strategies can help lower the risk of adverse drug interactions.
Changing first-line antidepressants | Attending Doctor is a professional medical publication for physicians. Science articles.
| To achieve the desired clinical effect of antidepressants, it is recommended to switch from tricyclic antidepressants to drugs with a similar mechanism of action, in particular venlafaxine, a modern serotonin and norepinephrine reuptake inhibitor | |
partners Keywords / keywords: Antidepressants, Velaxin, Venlafaxine, Depression, Noradrenergic system, Neuropsychiatry, Serotonergic system, Thymoanaleptic therapy
VEL 25. 09.2020/7
09.2020/7
Thymoanaleptic therapy is a dynamic process, the scenario of which depends on the characteristics of the disease and the response to treatment. According to the current recommendations, the clinical effect of an antidepressant (BP) of more than 50% within 3-4 weeks is considered sufficient [1]. According to statistics, such effectiveness is not achieved in 30-50% of patients with initial therapy with the first-line drug [1]. In such cases, it is recommended to increase the dose of blood pressure to the maximum, and in some cases, especially with the use of SSRIs, improvement still develops: a full effect can be achieved at 4-6 or even 8 weeks of treatment [1]. If this does not happen, and also in cases where increasing the dose is impractical (for example, in case of poor tolerance), it is recommended to change the blood pressure to a drug within the same pharmacological class or with a different mechanism of action [1]. In this case, a special algorithm should be followed.
The classical scheme suggests the gradual withdrawal of the initially prescribed drug, and after a washout period, the appointment of a new one with the selection of its therapeutic dose [2]. This method is used if there is a likely risk of an unwanted interaction that occurs when switching from drugs with a long half-life (such as fluoxetine), if the activity of the liver enzyme systems is reduced in the patient, or if the drugs differ radically in the mechanism of action (for example, when switching from mirtazapine or mianserin to milnacipran).
Both the patient and the doctor are much more comfortable with the one-time method of “switching” between drugs with a similar mechanism of action, when one day the first drug is canceled, and the second is prescribed immediately in a therapeutic dose. In this context, it seems convenient to switch patients from tricyclic antidepressants, fluvoxamine, sertraline, paroxetine, and milnacipran to a modern serotonin and norepinephrine reuptake inhibitor (SSRI) venlafaxine ( Velaxin ® [3]). The need for such a transition arises in clinical practice, because. the effectiveness of venlafaxine is somewhat higher than that of SSRIs due to a wider spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4].
The need for such a transition arises in clinical practice, because. the effectiveness of venlafaxine is somewhat higher than that of SSRIs due to a wider spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4].
It should be taken into account that the transition from fluoxetine to Velaxin ® should be gradual due to the aforementioned long half-life of fluoxetine, in order to avoid unwanted interactions. When switching to Velaxin ® from mirtazapine, you will also have to observe the transition interval of 1-2 weeks, but in this case, due to the fundamentally different mechanisms of action of these drugs [2].
When switching to Velaxin ® from mirtazapine, you will also have to observe the transition interval of 1-2 weeks, but in this case, due to the fundamentally different mechanisms of action of these drugs [2].
- Russian Society of Psychiatrists. Depressive episode, Recurrent depressive disorder. Clinical guidelines. 2019.
- D.V. Hawks. Changing antidepressant therapy: causes and tactics. Medical business. 2007; 3:53-59.
- Instructions for medical use of the drug Velaksin® capsules LSR 000030 dated 05/24/2017.
- R.A. Becker, Yu.V. Bykov. Velaxin® capsules: presentation of a new long-acting form and review of the latest data on efficacy and safety. Psychiatry and psychopharmacotherapy. T.20. No. 1. 2018.
The material is intended for medical professionals.
What you need to know about antidepressants
Ekaterina Kushnir
treats anxiety disorder
I have generalized anxiety disorder.
For a long time I coped without pills and other help, but one day I got tired of constant anxiety and began to interfere with my normal life. As a result, I turned to a private psychiatrist.
The doctor prescribed an antidepressant from the SSRI group - these are selective serotonin reuptake inhibitors. Such drugs are the first thing prescribed in the treatment of depression and a number of other conditions, including my illness.
The doctor immediately warned me about some peculiarities associated with taking the drug. Some of them I then felt on myself. I think everyone who plans to be treated with antidepressants should know about them.
At the same time, it should be taken into account that most of the negative effects of therapy are temporary and not dangerous, and if they do not go away, one medicine can be replaced with another. Antidepressants help many people with mental disorders and other illnesses get rid of their symptoms and return to a full life, so you definitely should not be afraid of them. The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control.
The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Fact No. 1
Antidepressants may make symptoms worse at firstAntidepressants can increase anxiety in anxiety disorders, as well as cause irritability and agitation - the so-called causeless motor agitation, the inability to sit still. It's not dangerous, but rather unpleasant. This condition is sometimes referred to as initial anxiety, that is, the anxiety of starting therapy. Up to 65% of people face it.
Antidepressant-induced anxiety syndrome - a systematic review in the British Journal of Psychiatry
There is also evidence that some classes of antidepressants, including SSRIs, may increase suicidal ideation in depression in young people aged 18 to 24 years. These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
Without treatment, depression is more likely to lead to suicidal thoughts, and in case of anxiety, you just need to prepare for such an effect, then it will be easier to survive the attacks.
The doctor told me that in the first two or three weeks there may be an increase in anxiety, but I did not take it too seriously.
Everything was fine for the first week. After about seven days, I became nervous and irritable. And then I woke up at night and after a while I felt an incomprehensible fear. My heartbeat increased, my head was spinning, my throat was constricted. Because of this, I felt a real panic - I spent the rest of the night fighting with terrible thoughts, in the morning I got up completely broken.
/list/antidepressant-myths/
8 myths about antidepressants
I have never had such panic attacks before medication - my anxiety was background, general. I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
After that, I was already expecting these panic attacks, I immediately tried to relax, calm down, remember that this was just a temporary effect of drugs. And they ended faster, and then they completely disappeared.
My letter to a psychiatrist. I was scared: I expected an increase in background anxiety, but not panic attacks. I even thought about giving up the medicineFact No. 2
The effect of antidepressant treatment will not be immediateIncrease the dose of antidepressants gradually to reduce side effects. They usually start with the minimum, and then bring it up to the working one. For example, for SSRIs with the active ingredient "sertraline", the working dose is from 100 mg per day. I started taking such a drug with 25 mg, and then gradually, in several steps, under the supervision of a doctor, raised the dose to 100 mg.
SSRI dosage - NHS
What doses of antidepressants will be optimal - an article in The Lancet
The process of reaching a working dose can take from two weeks to a month or more. It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
The full therapeutic effect, that is, the disappearance or a strong improvement in the symptoms of the disease, occurs some time after reaching the working dosage. As a rule, this is a week or two, although some positive changes may be earlier. For some people, this process stretches for a longer period: 6-12 weeks. Minimum initial doses of drugs usually do not work.
It is better to get ready for the fact that the symptoms of the disease will not disappear in the first weeks of treatment. And remember - this does not always mean that the drug needs to be changed, sometimes you just need to wait or further increase the dosage under the supervision of a doctor.
Fact No. 3
3
Another way to mitigate the side effects of antidepressants is to prescribe an additional drug along with them: for example, from the group of tranquilizers. Such drugs may have their own side effects, they should not be taken for a long time. Unlike antidepressants, some of them can be addictive. They are usually appointed for a month, but this period may be shorter or longer.
Antidepressants together with benzodiazepines work better for depression - BMJ magazine
My doctor prescribed a rather mild drug. However, he did not suit me. At first, it caused increased drowsiness: during the period of increased anxiety, it went away for a while, but then returned - even with half a pill I turned off and could sleep all day. And if I drank at night, I woke up with difficulty in the morning. The psychiatrist prescribed another medicine, but I could not buy it: the drug was not available in any pharmacy nearby.
As a result, I simply endured all the side effects of therapy - they were unpleasant, but tolerable. When discussing with the doctor, she called this option acceptable if the side effects of the second medicine only worsen the situation.
My prescriptions for drugs. I never used one, because there was no such medicine in pharmaciesFact No. 4
Side effects are not always, but they areModern antidepressants, including SSRIs, are mild and have almost no side effects. Older drugs - tricyclic antidepressants and monoamine oxidase inhibitors - cause more side effects. Doctors usually use them when milder first-line drugs don't work or when they can't be prescribed.
For the first couple of weeks of taking it, there is a risk that you will not feel well - it's worth thinking about. It may be worth scheduling the start of therapy on vacation.
I work remotely, and it was easier for me: the first pill was taken on Saturday, I slept through the weekend. Then she continued to work, but refused any additional loads: housework, part-time jobs, training and everything else.
Then she continued to work, but refused any additional loads: housework, part-time jobs, training and everything else.
It was hard to work: I wanted to sleep, then I began to worry and get distracted. I also had diarrhea, nausea, headaches, tremors, i.e. hand trembling, hot flashes, sweating, palpitations. At night, panic attacks began, in the morning I had difficulty getting up because I was in pain and dizzy.
There are mixed data on how common the side effects of antidepressants are. If we summarize them, then the numbers look something like this:
- nausea - about 25% feel it;
- diarrhea - it happens in 15% of people, and 5%, on the contrary, will have constipation;
- sweating and a feeling of heat occur in about 20% of people;
- sexual dysfunction, decreased libido may occur in 80% of cases;
- insomnia - in 11% of cases;
- headache and dizziness - in about 10-11% of cases;
- weight gain - not all drugs give this effect.
 Some, on the contrary, can reduce weight. On my medicine, I lost 2 kilograms in the first month, despite the fact that I quit training due to poor health. True, then they returned back.
Some, on the contrary, can reduce weight. On my medicine, I lost 2 kilograms in the first month, despite the fact that I quit training due to poor health. True, then they returned back.
It can be seen that most side effects occur in less than half of the cases. In addition, in most cases they pass in the first weeks and are not dangerous.
Side effects not listed above are very rare. I was "lucky", and I faced one such - a decrease in visual acuity. Once in the morning I noticed that I see worse without glasses. A little later, I realized that something was wrong with the glasses.
I wrote to the doctor, she replied that this happens, as a rule, is not dangerous and passes, but it is better to visit an ophthalmologist. I went to the ophthalmologist, everything was fine with my eyes, there was nothing terrible, but my vision really worsened - it was not a subjective feeling. On the right eye, it was -0.5 diopters, it became -0.75, and on the left eye it was -1. 5, and it became -3.5.
5, and it became -3.5.
I was offered to try changing the drug, but I decided to wait. Vision was then restored. I have not yet gone to the doctor to have it measured, but according to subjective feelings, it is at the same level as before: I am comfortable again in my glasses.
Side effects should not be tolerated - if something greatly worries, scares or interferes with life, it is better to tell the doctor right away. The psychiatrist will be able to determine whether the side effect of the drug is dangerous and whether it is worth continuing to take it. There are several antidepressants of the SSRI group, in addition, there are groups of drugs with a slightly different mechanism of action. As a rule, doctors manage to find a medicine that gives a good effect without side effects.
If there is no danger, the doctor can adjust the dose or increase it more gradually - this often helps to cope with unpleasant effects.
I wrote to the doctor again when my visual acuity decreased Fact No. 5
5
Antidepressants are not drugs that you can stop drinking as soon as you get better. They are taken for a long time: usually from several months, less often several years.
Anxiety Therapy - UpToDate
For example, for generalized anxiety disorder, the duration of treatment is at least a year. Moreover, the date is not counted from the very beginning, but from the moment when a lasting effect appeared from the pills. In fact, they will have to be drunk for about 1.5 years - it depends on how long it takes to reach the working dosage of the medicine.
The cost of a package of the most famous antidepressant "Zoloft" is about 700 R, enough for about a month. That is, a course of therapy will cost about 10,000 R - maybe more or less, depending on which drug is selected.
Psychotherapy review - UpToDate
Another drug of the same group already costs more than 2000 R per pack. Source: rigla.ru The cost of an appointment with a good psychiatrist in Moscow is 3000-5000 R. At first, you will need to visit him about once every 1-1.5 months, then less often.
At first, you will need to visit him about once every 1-1.5 months, then less often.
You can apply to the psycho-neurological dispensary at the place of residence under compulsory medical insurance - it's free. At the same time, they will not put you on psychiatric registration: it was canceled in 1993. People with disorders that do not threaten their lives or those around them are on consultative and diagnostic care. If you stop going to the doctor, he will not find out what happened: a person seeks help at will.
Psychotherapy, usually cognitive-behavioral, is also commonly prescribed to enhance and consolidate the effect of antidepressants. In many cases, it improves the effectiveness of drugs, including depression and generalized anxiety disorder. An appointment with a psychotherapist in Moscow costs an average of 5000 R. For treatment, you will need about 10 sessions or more.
/psychotherapy/
How psychotherapy works
Fact No. 6
6
Antidepressants do not develop dependence. However, if you abruptly stop drinking them, there will be a withdrawal syndrome. This is felt as electric current discharges while moving or turning the head, headaches, dizziness, insomnia. Many people experience symptoms similar to the flu or an intestinal virus: low fever, diarrhea, general malaise, chills. Often there is anxiety, there are intrusive images.
Withdrawal symptoms after taking serotonin reuptake inhibitors - Journal of Clinical Psychiatry
How difficult it is to stop taking antidepressants - American Psychological Association
Stopping antidepressants in adults - UpToDate
treatment, they should be canceled only under the supervision of a doctor.
Antidepressant withdrawal occurs as gradually as the start of treatment. The dosage is slowly reduced, usually at this time again a cover-up drug is prescribed to alleviate side effects. As a rule, this is the same medicine that was at the beginning of the intake.
As a rule, this is the same medicine that was at the beginning of the intake.
Withdrawal is usually harmless and resolves within the first weeks of stopping the drug. Sometimes even within a few days - it still depends on which medicine was prescribed. If severely disturbing symptoms appear during the withdrawal period, you should consult a doctor.
Fact No. 7
If you need to change the drug, everything will start overIt is far from always possible to immediately find the right antidepressant - sometimes the side effects do not go away and you need to take a new one.
Changing antidepressants in adults - UpToDate
Serotonin syndrome - MSD
Most often, it is started again with a small dosage, this delays the process of obtaining the effect of treatment. The new drug may also have side effects - the same or different. We will have to wait again until they pass.
You won't be able to change the drug on your own, since all antidepressants are sold only by prescription - and that's good. Switching from one drug to another can be dangerous if you do not know the characteristics of different groups of drugs.
Switching from one drug to another can be dangerous if you do not know the characteristics of different groups of drugs.
For example, taking SSRIs is possible only some time after the withdrawal of antidepressants from the group of monoamine oxidase inhibitors - due to the risk of developing serotonin syndrome. This is a potentially fatal condition, accompanied by a change in mental state, high fever, increased muscle tone and other symptoms.
If the drug is changed correctly, there will be no dangerous negative effects, so consultation with a doctor is required.
/psychotherapy-search/
How to choose a psychotherapist
Fact No. 8
Among antidepressants there are original drugs and generics Preparations may be original or generic. Originals are medicines first released by some pharmaceutical company that have passed all clinical trials and checks. Generics are drugs with the same active ingredient from another pharmaceutical company, that is, copied from the original drug.
Theoretically, the effect of generic drugs should not differ from the effect of original drugs. However, this is possible, since generics may contain other additional substances or the manufacturer may use other raw materials.
Due to my anxiety, I did not read anything in detail about specific drugs before I bought my first antidepressant in a pharmacy so as not to be scared and not think about taking it. I also didn’t think to ask the doctor about this question.
/list/covid-depression/
Psychoneurological complications after covid: memory problems and depression
As a result, I first bought a generic because it was in stock. Then it turned out that, after all, according to the experience of my psychiatrist, the original drug often gives fewer side effects and is better tolerated. As a result, I changed the generic to the original drug - and, indeed, the side effects softened.
In my subjective opinion, which is supported by some data, in the case of antidepressants and other psychotropic drugs, you should always choose the original medicine. Moreover, the cost of originals and generics is not always very different.
Moreover, the cost of originals and generics is not always very different.
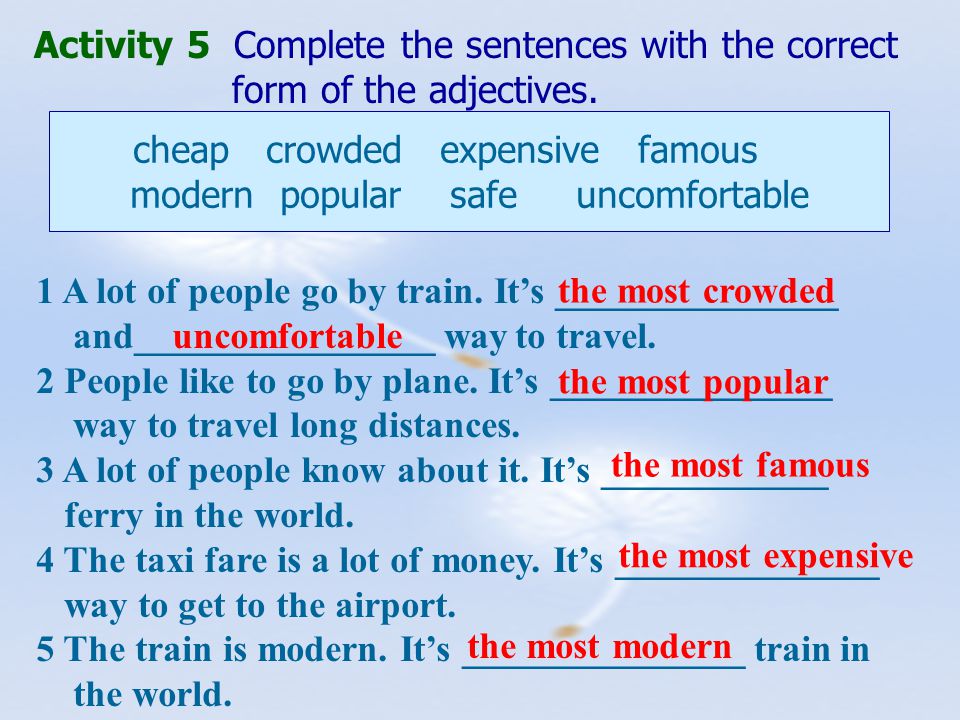
Originals and generics of some SSRIs
| Active ingredient | Original | Original price | Generics | Cost of generics |
|---|---|---|---|---|
| Sertraline | Zoloft | About 700 R, 100 mg tablets | "Serenata", "Sirlift" | 500-600 R, tablets 100 mg |
| Escitalopram | "Cipralex" | 3000 R, tablets 10 mg | "Selektra", "Elicea" | 500-1300 R, tablets 10 mg |
| Fluoxetine | Prozac | About 350 R, 20 mg tablets | Profluzak, Fluoxetine | 100-200 R, tablets 20 mg |
CERTRALIN
Original
"Zoloft"
The cost of the original
about 700 r, tablets 100 mg
Generic
"Serenata", "Serlift"
Cost of Jenaerac , tablets 100 mg
Escitalopram
Original
Cipralex
Original price
3000 r, tablets 10 mg
generics
"Selectra", "Elice"
The cost of generics
500-1300 p, tablets 10 mg
" original
About 350 R, tablets 20 mg
Generics
Profluzak, Fluoxetine
Cost of generics
100-200 R, tablets 20 mg
one remained unclaimed Fact No. 9
9
Drinking alcohol while taking antidepressants may exacerbate unpleasant side effects. Also, alcohol is a depressant, that is, it has the opposite effect, and its intake can adversely affect the results of treatment.
Why you shouldn't mix antidepressants and alcohol - Mayo Clinic
Alcohol is strictly forbidden to drink with some groups of antidepressants, for example, tricyclic antidepressants and monoamine oxidase inhibitors: combination with the latter, for example, can lead to an uncontrolled increase in pressure. MAO inhibitors in general require a special diet - it is unlikely that a doctor will prescribe such drugs as the first antidepressants, but if necessary, he will issue a list of what is allowed and prohibited.
With other antidepressants, moderate use may not be dangerous and even pass without consequences, but doctors still recommend abstaining so as not to increase side effects and improve treatment outcome.
The main thing is not to temporarily stop taking the drug in order to drink. This can lead to the development of a withdrawal syndrome.
/trevoga/
How I Treated Generalized Anxiety Disorder under CHI
Fact No. 10
Antidepressants are incompatible with certain drugs and have contraindicationsIt is important to tell your doctor what medications you are taking and what chronic illnesses you have. For example, SSRIs may not be suitable for epilepsy and bleeding disorders, and tricyclic antidepressants are usually not prescribed for those who have recently had a heart attack, suffer from glaucoma, or porphyria.
Antidepressant Warnings - NHS
Drug Compatibility Test - Drugs.com
It is also important to be careful if you are about to take any over-the-counter medication. For example, ibuprofen, which people often take on their own to relieve pain and reduce fever. It should not be taken with SSRIs as it increases the risk of gastrointestinal side effects.