Treatments for schizophrenia include
Schizophrenia - Diagnosis and treatment
Diagnosis
Diagnosis of schizophrenia involves ruling out other mental health disorders and determining that symptoms are not due to substance abuse, medication or a medical condition. Determining a diagnosis of schizophrenia may include:
- Physical exam. This may be done to help rule out other problems that could be causing symptoms and to check for any related complications.
- Tests and screenings. These may include tests that help rule out conditions with similar symptoms, and screening for alcohol and drugs. The doctor may also request imaging studies, such as an MRI or CT scan.
- Psychiatric evaluation. A doctor or mental health professional checks mental status by observing appearance and demeanor and asking about thoughts, moods, delusions, hallucinations, substance use, and potential for violence or suicide. This also includes a discussion of family and personal history.
- Diagnostic criteria for schizophrenia. A doctor or mental health professional may use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
More Information
- CT scan
- MRI
Treatment
Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. In some cases, hospitalization may be needed.
A psychiatrist experienced in treating schizophrenia usually guides treatment. The treatment team also may include a psychologist, social worker, psychiatric nurse and possibly a case manager to coordinate care. The full-team approach may be available in clinics with expertise in schizophrenia treatment.
Medications
Medications are the cornerstone of schizophrenia treatment, and antipsychotic medications are the most commonly prescribed drugs. They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
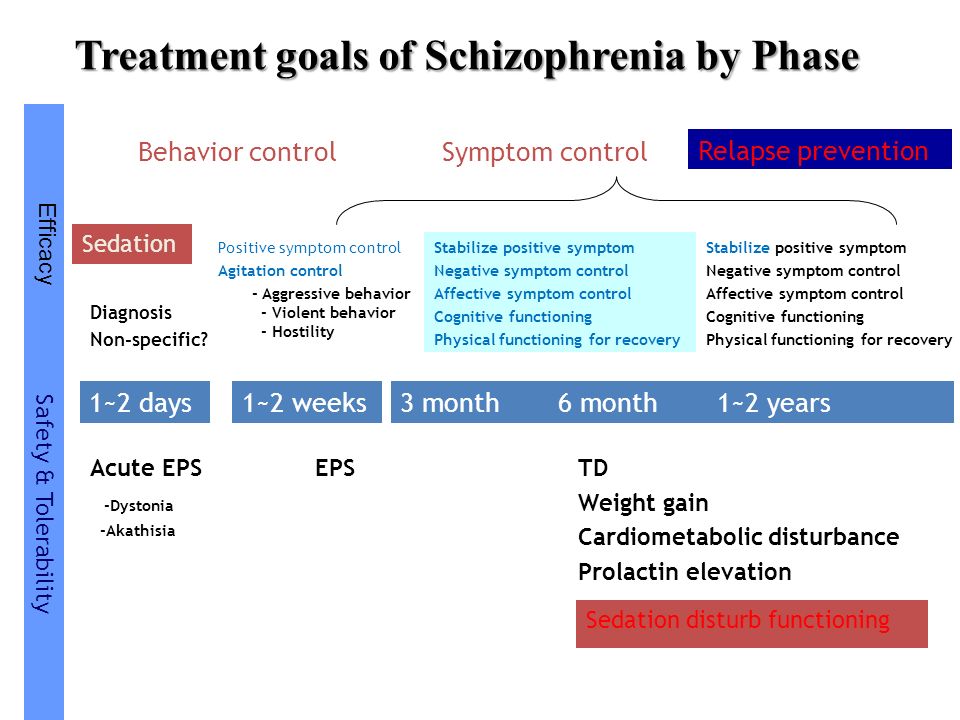
The goal of treatment with antipsychotic medications is to effectively manage signs and symptoms at the lowest possible dose. The psychiatrist may try different drugs, different doses or combinations over time to achieve the desired result. Other medications also may help, such as antidepressants or anti-anxiety drugs. It can take several weeks to notice an improvement in symptoms.
Because medications for schizophrenia can cause serious side effects, people with schizophrenia may be reluctant to take them. Willingness to cooperate with treatment may affect drug choice. For example, someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill.
Ask your doctor about the benefits and side effects of any medication that's prescribed.
Second-generation antipsychotics
These newer, second-generation medications are generally preferred because they pose a lower risk of serious side effects than do first-generation antipsychotics.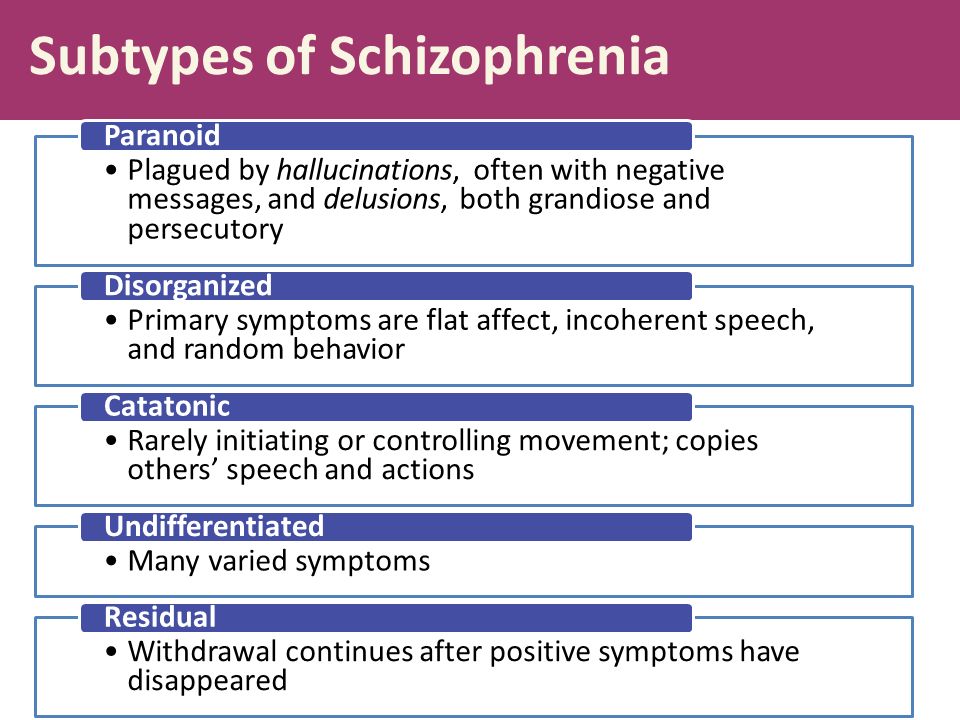 Second-generation antipsychotics include:
Second-generation antipsychotics include:
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Brexpiprazole (Rexulti)
- Cariprazine (Vraylar)
- Clozapine (Clozaril, Versacloz)
- Iloperidone (Fanapt)
- Lurasidone (Latuda)
- Olanzapine (Zyprexa)
- Paliperidone (Invega)
- Quetiapine (Seroquel)
- Risperidone (Risperdal)
- Ziprasidone (Geodon)
First-generation antipsychotics
These first-generation antipsychotics have frequent and potentially significant neurological side effects, including the possibility of developing a movement disorder (tardive dyskinesia) that may or may not be reversible. First-generation antipsychotics include:
- Chlorpromazine
- Fluphenazine
- Haloperidol
- Perphenazine
These antipsychotics are often cheaper than second-generation antipsychotics, especially the generic versions, which can be an important consideration when long-term treatment is necessary.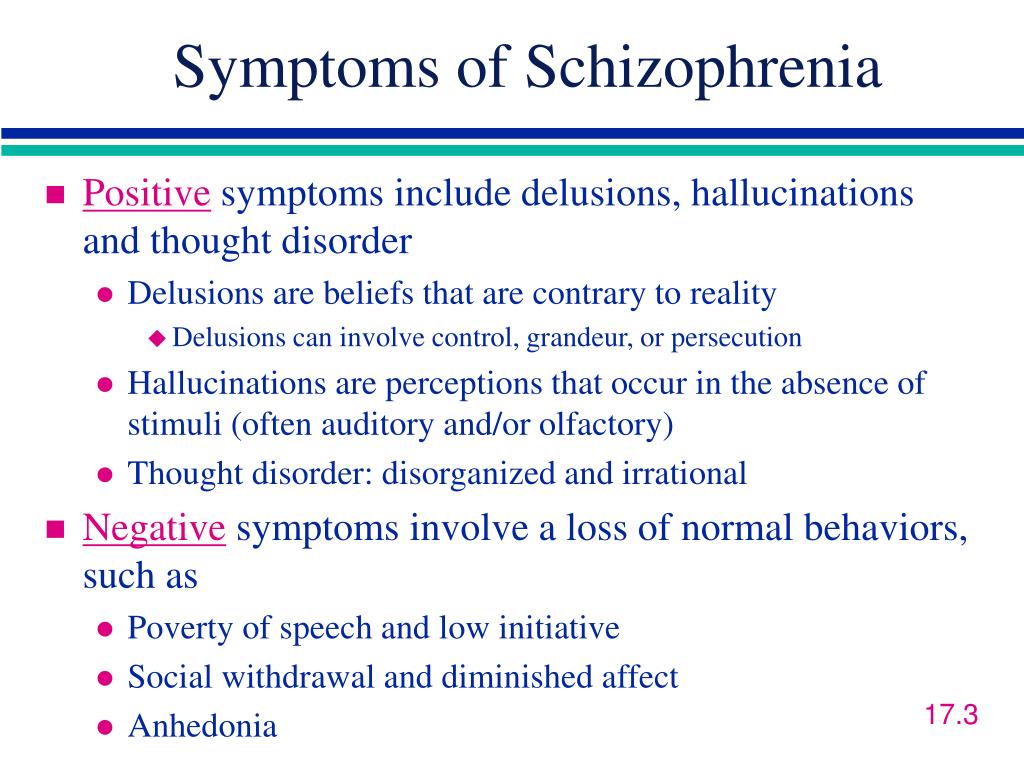
Long-acting injectable antipsychotics
Some antipsychotics may be given as an intramuscular or subcutaneous injection. They are usually given every two to four weeks, depending on the medication. Ask your doctor about more information on injectable medications. This may be an option if someone has a preference for fewer pills and may help with adherence.
Common medications that are available as an injection include:
- Aripiprazole (Abilify Maintena, Aristada)
- Fluphenazine decanoate
- Haloperidol decanoate
- Paliperidone (Invega Sustenna, Invega Trinza)
- Risperidone (Risperdal Consta, Perseris)
Psychosocial interventions
Once psychosis recedes, in addition to continuing on medication, psychological and social (psychosocial) interventions are important. These may include:
- Individual therapy. Psychotherapy may help to normalize thought patterns. Also, learning to cope with stress and identify early warning signs of relapse can help people with schizophrenia manage their illness.
- Social skills training. This focuses on improving communication and social interactions and improving the ability to participate in daily activities.
- Family therapy. This provides support and education to families dealing with schizophrenia.
- Vocational rehabilitation and supported employment. This focuses on helping people with schizophrenia prepare for, find and keep jobs.
Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups and crisis situations. A case manager or someone on the treatment team can help find resources. With appropriate treatment, most people with schizophrenia can manage their illness.
Hospitalization
During crisis periods or times of severe symptoms, hospitalization may be necessary to ensure safety, proper nutrition, adequate sleep and basic hygiene.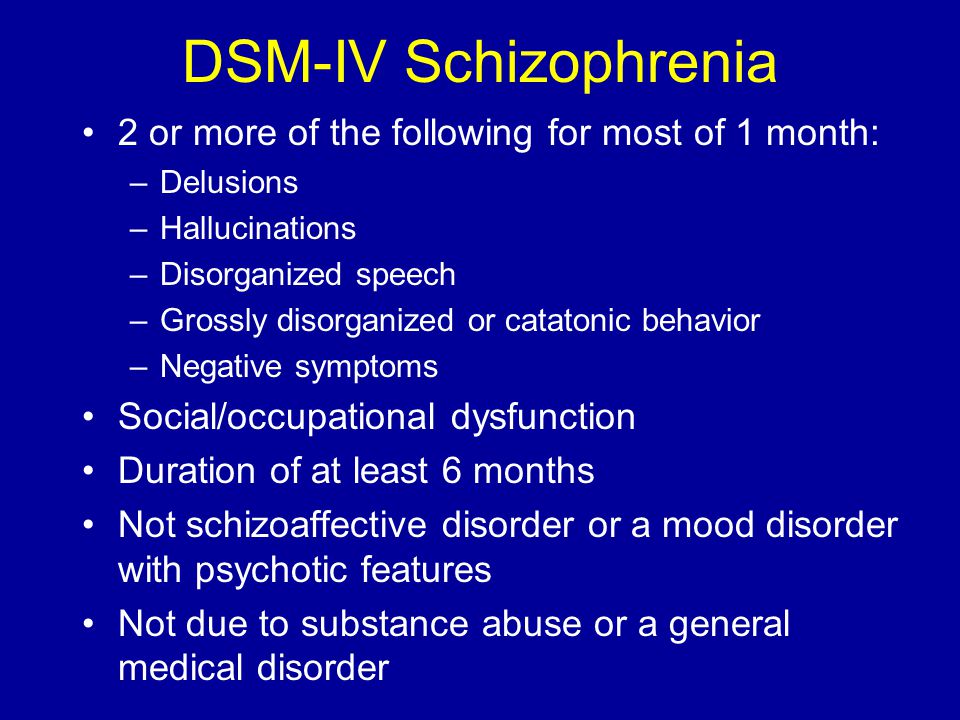
Electroconvulsive therapy
For adults with schizophrenia who do not respond to drug therapy, electroconvulsive therapy (ECT) may be considered. ECT may be helpful for someone who also has depression.
More Information
- Family therapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.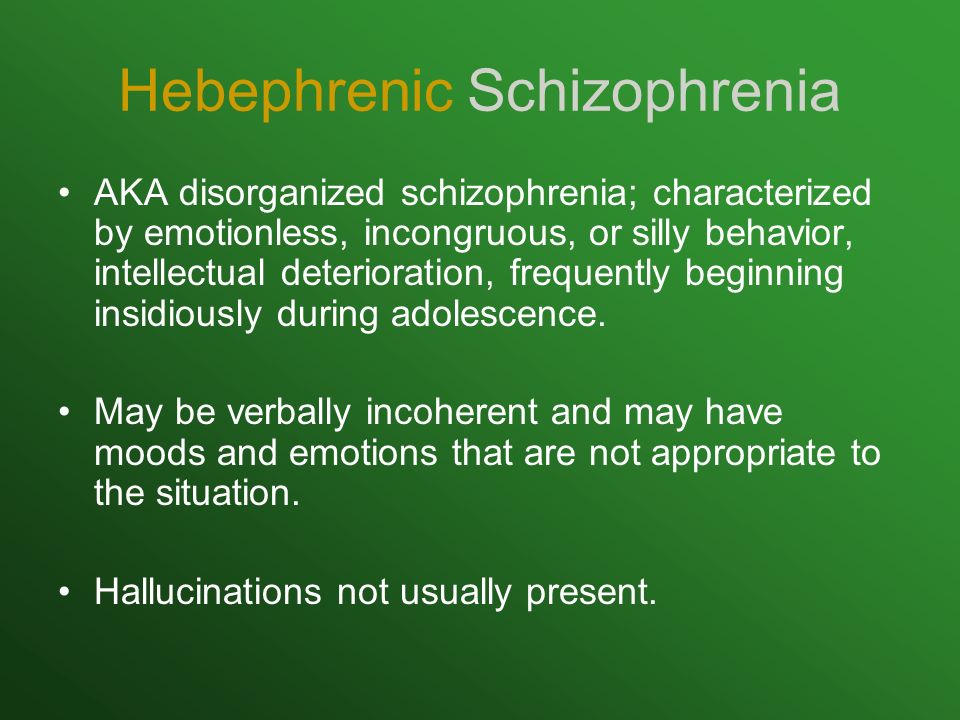 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Coping and support
Coping with a mental disorder as serious as schizophrenia can be challenging, both for the person with the condition and for friends and family. Here are some ways to cope:
- Learn about schizophrenia. Education about the disorder can help the person with schizophrenia understand the importance of sticking to the treatment plan. Education can help friends and family understand the disorder and be more compassionate with the person who has it.
- Stay focused on goals. Managing schizophrenia is an ongoing process. Keeping treatment goals in mind can help the person with schizophrenia stay motivated. Help your loved one remember to take responsibility for managing the disorder and working toward goals.
- Avoid alcohol and drug use. Using alcohol, nicotine or recreational drugs can make it difficult to treat schizophrenia.
 If your loved one is addicted, quitting can be a real challenge. Get advice from the health care team on how best to approach this issue.
If your loved one is addicted, quitting can be a real challenge. Get advice from the health care team on how best to approach this issue. - Ask about social services assistance. These services may be able to assist with affordable housing, transportation and other daily activities.
- Learn relaxation and stress management. The person with schizophrenia and loved ones may benefit from stress-reduction techniques such as meditation, yoga or tai chi.
- Join a support group. Support groups for people with schizophrenia can help them reach out to others facing similar challenges. Support groups may also help family and friends cope.
Preparing for your appointment
If you're seeking help for someone with schizophrenia, you may start by seeing his or her family doctor or health care professional. However, in some cases when you call to set up an appointment, you may be referred immediately to a psychiatrist.
What you can do
To prepare for the appointment, make a list of:
- Any symptoms your loved one is experiencing, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- Medications, vitamins, herbs and other supplements that he or she is taking, including the dosages
- Questions to ask the doctor
Go with your loved one to the appointment. Getting the information firsthand will help you know what you're facing and what you need to do for your loved one.
For schizophrenia, some basic questions to ask the doctor include:
- What's likely causing the symptoms or condition?
- What are other possible causes for the symptoms or condition?
- What kinds of tests are needed?
- Is this condition likely temporary or lifelong?
- What's the best treatment?
- What are the alternatives to the primary approach you're suggesting?
- How can I be most helpful and supportive?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
The doctor is likely to ask you a number of questions. Anticipating some of these questions can help make the discussion productive. Questions may include:
- What are your loved one's symptoms, and when did you first notice them?
- Has anyone else in your family been diagnosed with schizophrenia?
- Have symptoms been continuous or occasional?
- Has your loved one talked about suicide?
- How well does your loved one function in daily life — is he or she eating regularly, going to work or school, bathing regularly?
- Has your loved one been diagnosed with any other medical conditions?
- What medications is your loved one currently taking?
The doctor or mental health professional will ask additional questions based on responses, symptoms and needs.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Treatment - Schizophrenia - NHS
Schizophrenia is usually treated with an individually tailored combination of talking therapy and medicine.
Most people with schizophrenia are treated by community mental health teams (CMHTs).
The goal of the CMHT is to provide day-to-day support and treatment while ensuring you have as much independence as possible.
A CMHT can be made up of and provide access to:
- social workers
- community mental health nurses – who have specialist training in mental health conditions
- occupational therapists
- pharmacists
- counsellors and psychotherapists
- psychologists and psychiatrists – the psychiatrist is usually the senior clinician in the team
After your first episode of schizophrenia, you should initially be referred to an early intervention team.
These specialist teams provide treatment and support, and are usually made up of psychiatrists, psychologists, mental health nurses, social workers and support workers.
Care programme approach (CPA)
People with complex mental health conditions are usually entered into a treatment process known as a care programme approach (CPA). A CPA is essentially a way of ensuring you receive the right treatment for your needs.
A CPA is essentially a way of ensuring you receive the right treatment for your needs.
There are 4 stages to a CPA:
- assessment – your health and social needs are assessed
- care plan – a care plan is created to meet your health and social needs
- key worker appointed – a key worker, usually a social worker or nurse, is your first point of contact with other members of the CMHT
- reviews – your treatment will be regularly reviewed and, if needed, changes to the care plan can be agreed
Not everyone uses the CPA. Some people may be cared for by their GP, while others may be under the care of a specialist.
You'll work together with your healthcare team to develop a care plan. The care plan may involve an advance statement or crisis plan, which can be followed in an emergency.
Your care plan should include a combined healthy eating and physical activity programme and support for giving up smoking, if you smoke.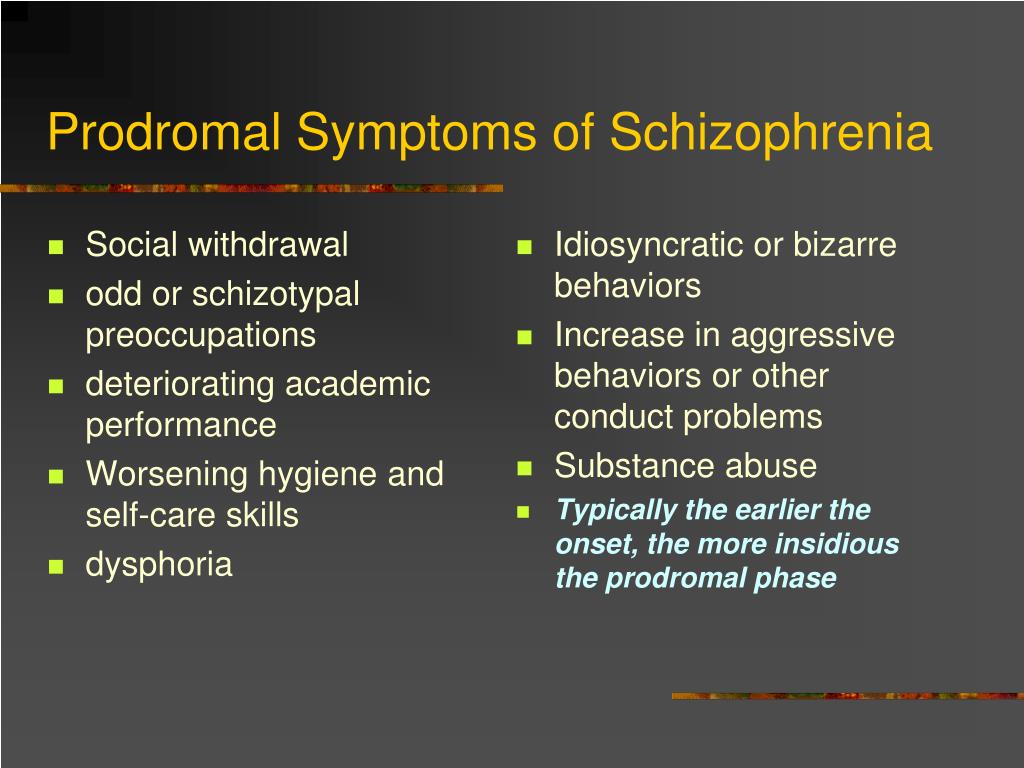
Your care co-ordinator will be responsible for making sure all members of your healthcare team, including your GP, have a copy of your care plan.
Further information
- Rethink Mental Illness: Care programme approach
Acute episodes
People who have serious psychotic symptoms as the result of an acute schizophrenic episode may require a more intensive level of care than a CMHT can provide.
These episodes are usually dealt with by antipsychotic medication and special care.
Crisis resolution teams (CRT)
A treatment option is to contact a home treatment or crisis resolution team (CRT). CRTs treat people with serious mental health conditions who are currently experiencing an acute and severe psychiatric crisis.
Without the involvement of the CRT, these people would require treatment in hospital.
The CRT aims to treat people in the least restrictive environment possible, ideally in or near their home. This can be in your own home, in a dedicated crisis residential home or hostel, or in a day care centre.
CRTs are also responsible for planning aftercare once the crisis has passed to prevent a further crisis occurring.
Your care co-ordinator should be able to provide you and your friends or family with contact information in the event of a crisis.
Voluntary and compulsory detention
More serious acute schizophrenic episodes may require admission to a psychiatric ward at a hospital or clinic. You can admit yourself voluntarily to hospital if your psychiatrist agrees it's necessary.
People can also be compulsorily detained at a hospital under the Mental Health Act (2007), but this is rare.
It's only possible for someone to be compulsorily detained at a hospital if they have a severe mental disorder and if detention is necessary:
- in the interests of the person's own health and safety
- to protect others
People with schizophrenia who are compulsorily detained may need to be kept in locked wards.
All people being treated in hospital will stay only as long as is absolutely necessary for them to receive appropriate treatment and arrange aftercare.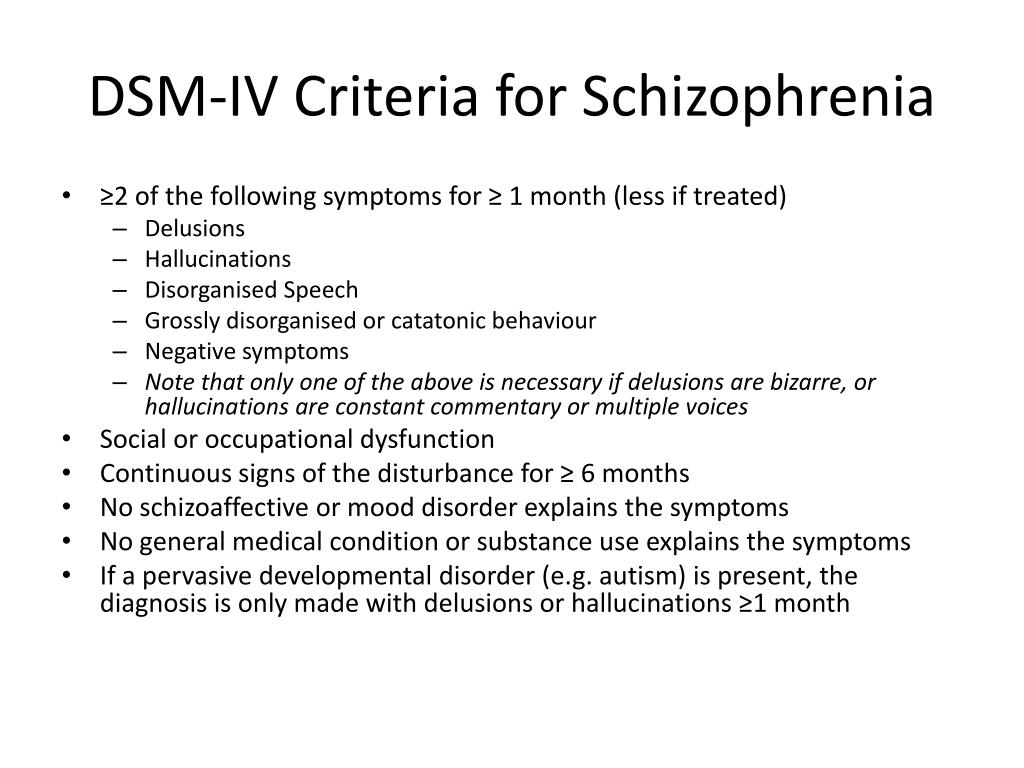
An independent panel will regularly review your case and progress. Once they feel you're no longer a danger to yourself and others, you'll be discharged from hospital. However, your care team may recommend you remain in hospital voluntarily.
Advance statements
If it's felt there's a significant risk of future acute schizophrenic episodes occurring, you may want to write an advance statement.
An advance statement is a series of written instructions about what you would like your family or friends to do in case you experience another acute schizophrenic episode. You may also want to include contact details for your care co-ordinator.
If you want to make an advance statement, talk to your care co-ordinator, psychiatrist or GP.
Further information
- Mind: Health and social care rights
Antipsychotics
Antipsychotics are usually recommended as the initial treatment for the symptoms of an acute schizophrenic episode. They work by blocking the effect of the chemical dopamine on the brain.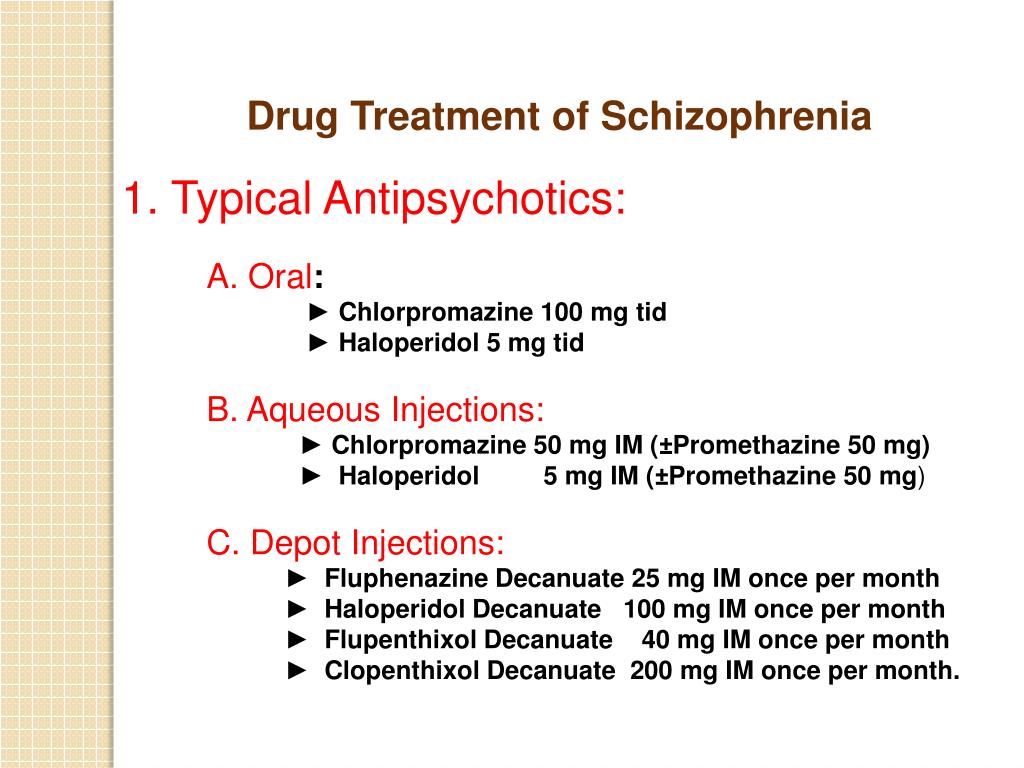
Antipsychotics can usually reduce feelings of anxiety or aggression within a few hours of use, but may take several days or weeks to reduce other symptoms, such as hallucinations or delusional thoughts.
It's important that your doctor gives you a thorough physical examination before you start taking antipsychotics, and that you work together to find the right one for you.
Antipsychotics can be taken orally as a pill, or be given as an injection known as a depot. Several slow-release antipsychotics are available. These require you to have one injection every 2 to 4 weeks.
You may only need antipsychotics until your acute schizophrenic episode has passed.
However, most people take medication for 1 or 2 years after their first psychotic episode to prevent further acute schizophrenic episodes occurring, and for longer if the illness is recurrent.
There are 2 main types of antipsychotics:
- typical antipsychotics – the first generation of antipsychotics developed in the 1950s
- atypical antipsychotics – newer-generation antipsychotics developed in the 1990s
The choice of antipsychotic should be made following a discussion between you and your psychiatrist about the likely benefits and side effects.
Both typical and atypical antipsychotics can cause side effects, although not everyone will experience them and the severity will differ from person to person.
The side effects of typical antipsychotics include:
- shaking
- trembling
- muscle twitches
- muscle spasms
Side effects of both typical and atypical antipsychotics include:
- drowsiness
- weight gain, particularly with some atypical antipsychotics
- blurred vision
- constipation
- lack of sex drive
- dry mouth
Tell your care co-ordinator, psychiatrist or GP if your side effects become severe. There may be an alternative antipsychotic you can take or additional medicines that will help you deal with the side effects.
If you do not benefit from your antipsychotic medicine after taking it regularly for several weeks, an alternative can be tried. It's important to work with your treatment team to find the right medicine for you.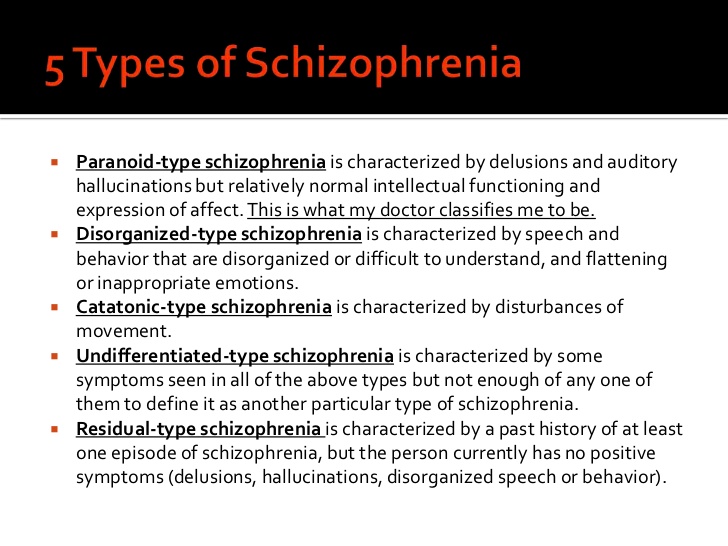
Do not stop taking your antipsychotics without first consulting your care co-ordinator, psychiatrist or GP. If you stop taking them, you could have a relapse of symptoms.
Your medicine should be reviewed at least once a year.
Further information
- Mind: Antipsychotics
- Royal College of Psychiatrists: Depot medication
Psychological treatment
Psychological treatment can help people with schizophrenia cope with the symptoms of hallucinations or delusions better.
They can also help treat some of the negative symptoms of schizophrenia, such as apathy or a lack of enjoyment and interest in things you used to enjoy.
Psychological treatments for schizophrenia work best when they're combined with antipsychotic medication.
Common psychological treatments for schizophrenia include:
- cognitive behavioural therapy (CBT)
- family therapy
- arts therapy
Cognitive behavioural therapy (CBT)
Cognitive behavioural therapy (CBT) aims to help you identify the thinking patterns that are causing you to have unwanted feelings and behaviour, and learn to change this thinking with more realistic and useful thoughts.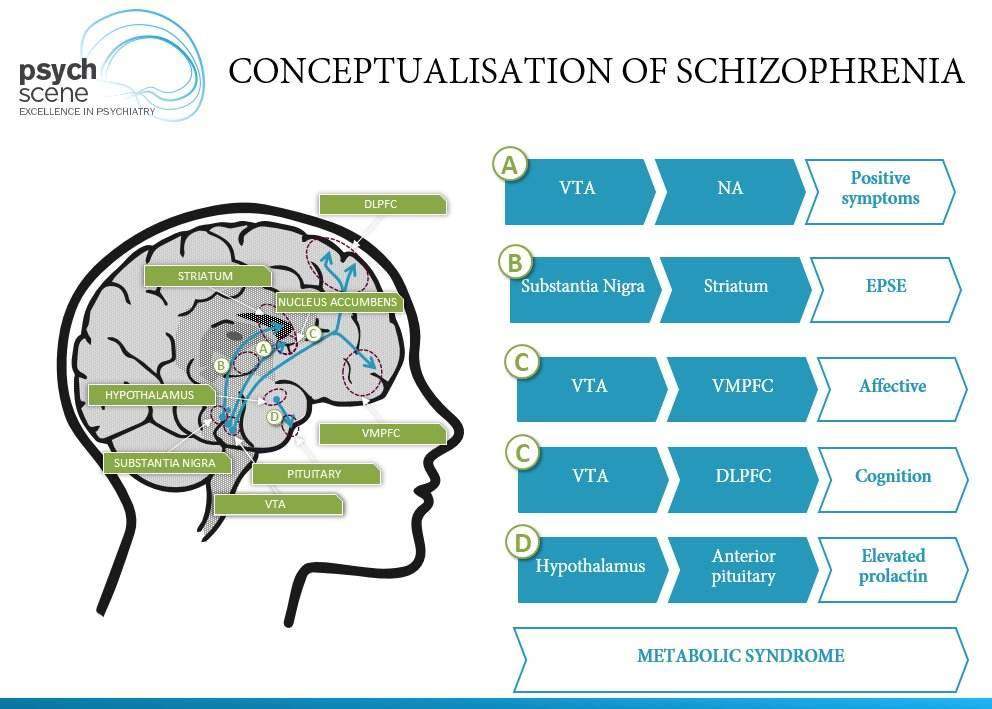
For example, you may be taught to recognise examples of delusional thinking. You may then receive help and advice about how to avoid acting on these thoughts.
Most people require a series of CBT sessions over the course of a number of months. CBT sessions usually last for about an hour.
Your GP or care co-ordinator should be able to arrange a referral to a CBT therapist.
Family therapy
Many people with schizophrenia rely on family members for their care and support. While most family members are happy to help, caring for somebody with schizophrenia can place a strain on any family.
Family therapy is a way of helping you and your family cope better with your condition. It involves a series of informal meetings over a period of around 6 months.
Meetings may include:
- discussing information about schizophrenia
- exploring ways of supporting somebody with schizophrenia
- deciding how to solve practical problems that can be caused by the symptoms of schizophrenia
If you think you and your family could benefit from family therapy, speak to your care co-ordinator or GP.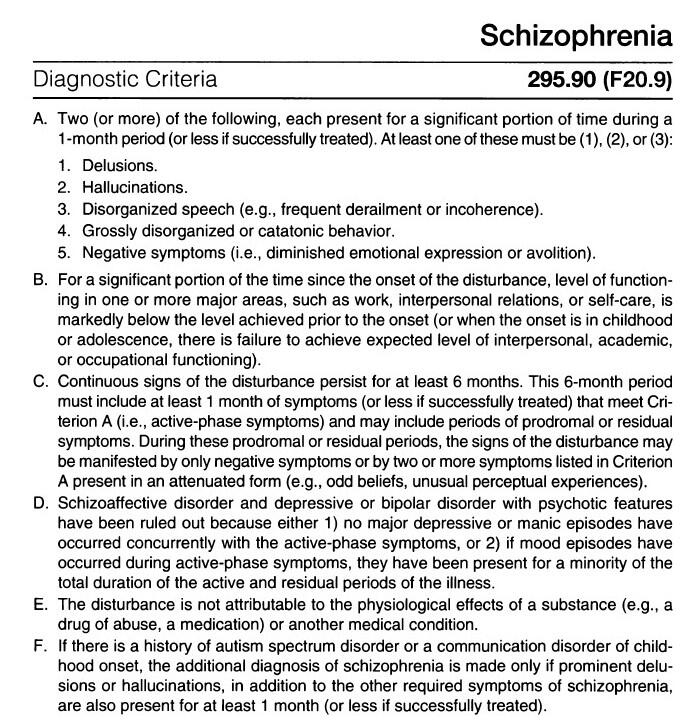
Arts therapy
Arts therapies are designed to promote creative expression. Working with an arts therapist in a small group or individually can allow you to express your experiences with schizophrenia.
Some people find expressing things in a non-verbal way through the arts can provide a new experience of schizophrenia and help them develop new ways of relating to others.
Arts therapies have been shown to alleviate the negative symptoms of schizophrenia in some people.
The National Institute for Health and Care Excellence (NICE) recommends that arts therapies are provided by an arts therapist registered with the Health and Care Professions Council who has experience of working with people with schizophrenia.
Want to know more?
- Mental Health Foundation: talking therapies
- Mind: understanding talking treatments
PKB No. 5 - Schizophrenia
Moscow State Budgetary Institution of Healthcare
Psychiatric Clinical Hospital No.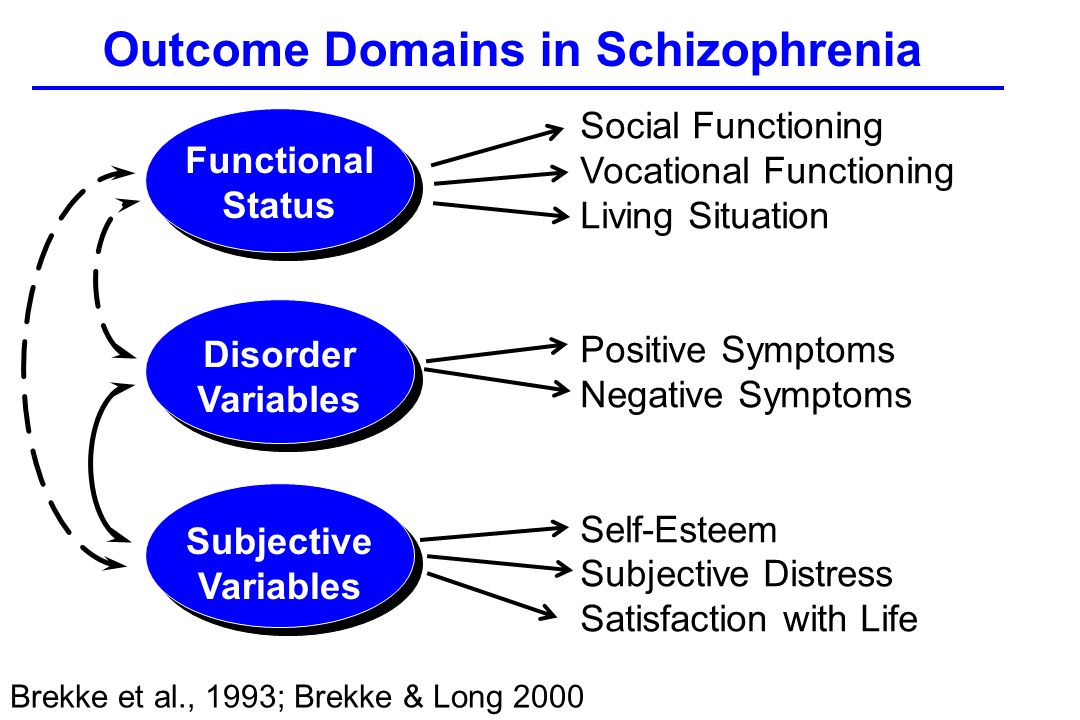 5 of the Moscow City Health Department
5 of the Moscow City Health Department
+7 (495) 445-55-25, +7 (496) 724-33 -33
Moscow region, Chekhov, s. Troitskoe, 5
Medical Tourism
Site search nine0021
Schizophrenia is a chronic mental illness, which is characterized by a violation of the unity of thought processes, with a relatively intact intellect, which is combined with significant emotional impoverishment and a decrease in will. Often hallucinatory and delusional disorders join.
The term "schizophrenia" itself is made up of two Greek words - "schizo" - splitting and "freni" - mind reason.
This term was first used by the Swiss psychiatrist Eigen Bleuler in 1908y. Schizophrenia, of course, existed before, but only by the beginning of the 20th century did the idea of it as a special kind of psychosis mature.
In the mass consciousness there is an unreasonable identification of schizophrenia with a "split personality" - that is, in fact, with a very rare mental disorder in which different "I"s are alternately activated in one person.
Schizophrenia, unfortunately, is quite common. Its prevalence among the Russian population is 35 per 10,000 people, with no significant difference between the sexes. Thus, in Russia there are at least half a million patients with this serious pathology. nine0006
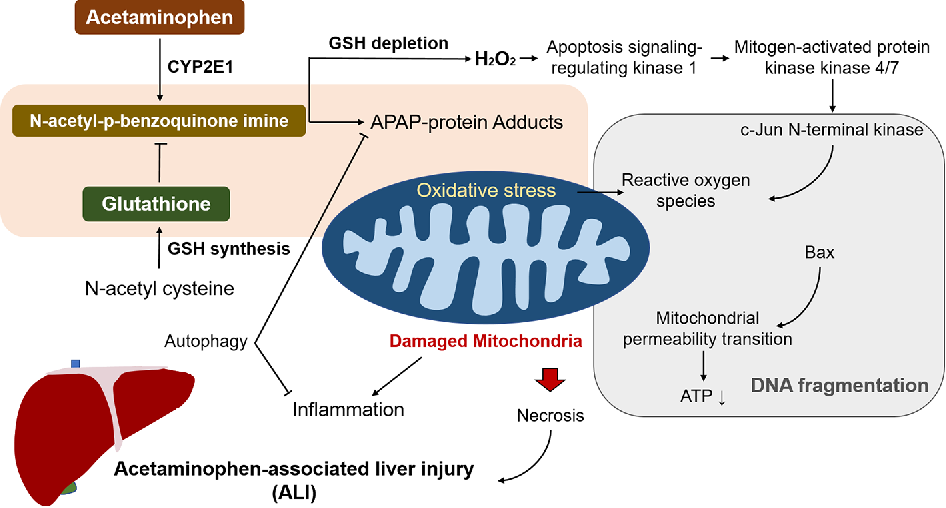
Schizophrenia refers to endogenous mental illness, which means that it is an internal breakdown of the psyche. It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.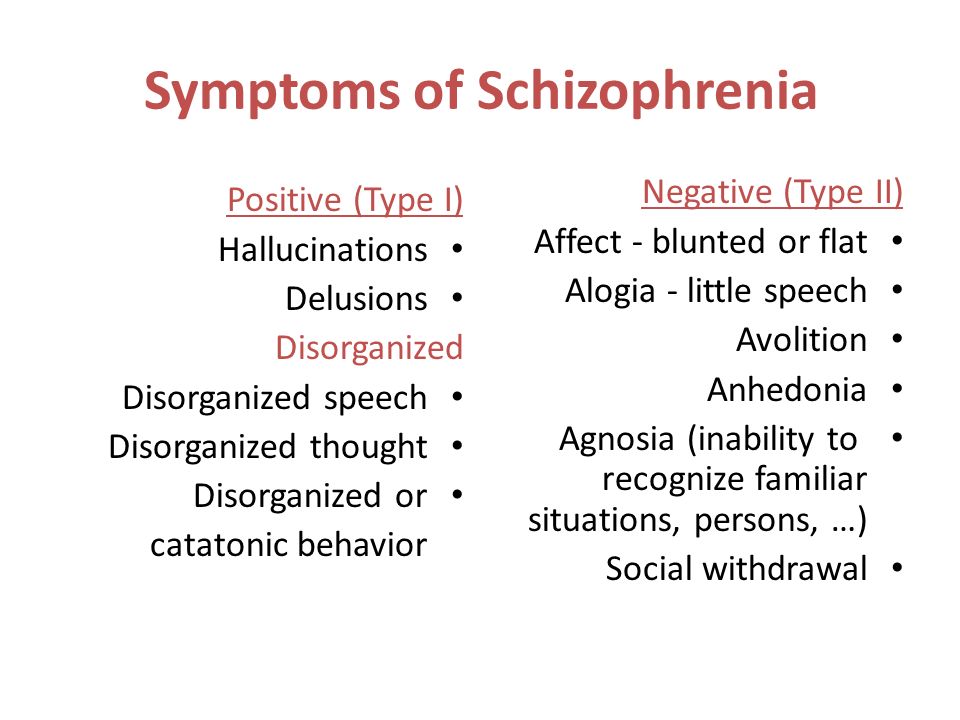 nine0006
nine0006
The role of heredity is very great. So, if one of the twins fell ill with schizophrenia, then the risk of getting sick for the other twin is 17% in a fraternal couple and 48% in an identical one. However, it is believed that in half of the cases of schizophrenia arises from a random mutation, that is, on the basis of genetic changes that were absent in the parents and appeared after conception.
Symptoms can develop at any age (possibly even in utero), but usually its onset is timed to coincide with the third pubertal crisis, that is, by the age of 12-18 years or several years later (up to about 30 years). nine0006
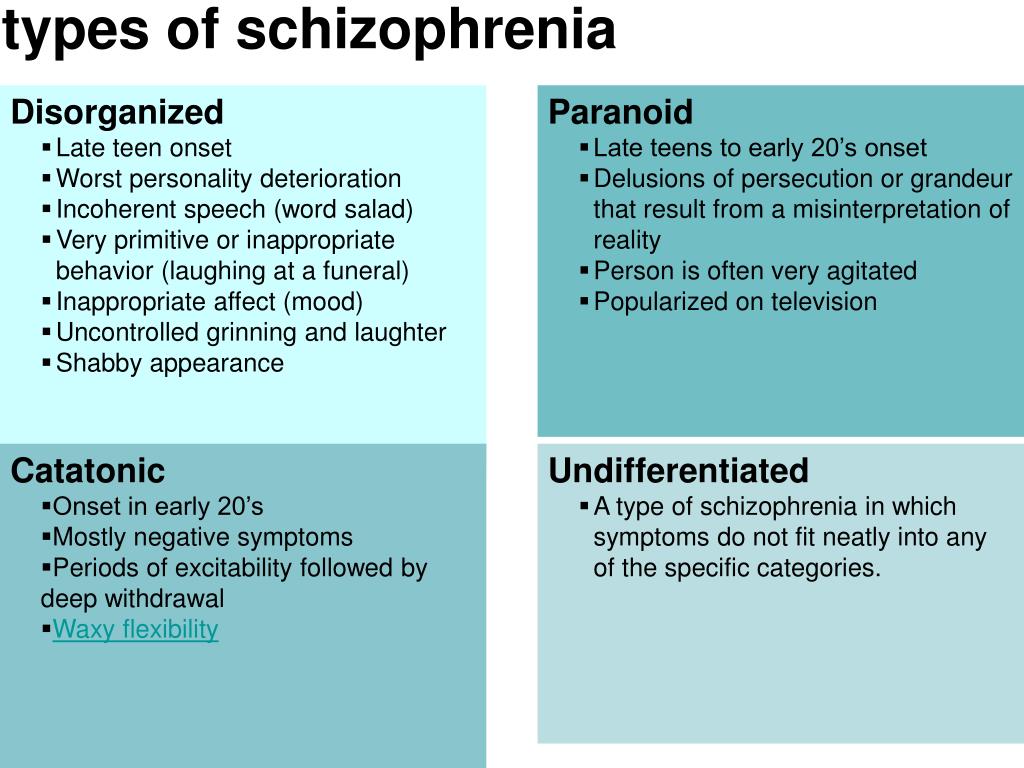
Most often, the disease begins with negative symptoms associated with the loss of normal functioning - a person changes in character for no apparent reason, becomes closed, fenced off, loses social contacts, emotional warmth in relation to relatives disappears. Former interests disappear, school or university performance drops sharply, or official duties are not fulfilled.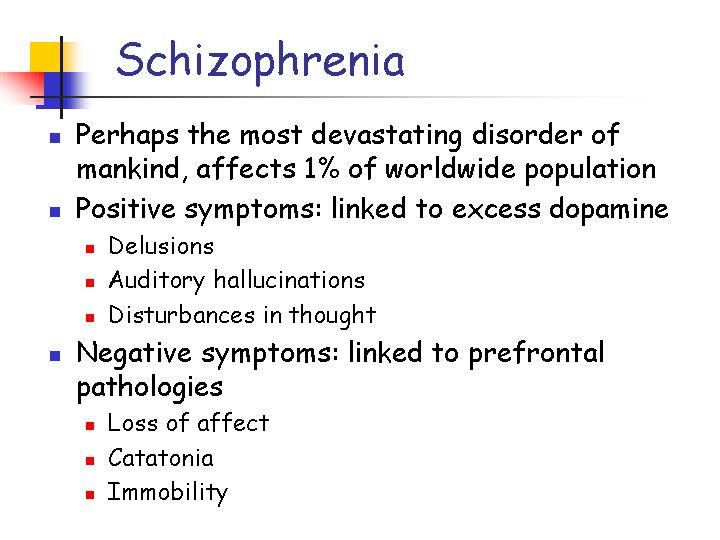 Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with. During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with. During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.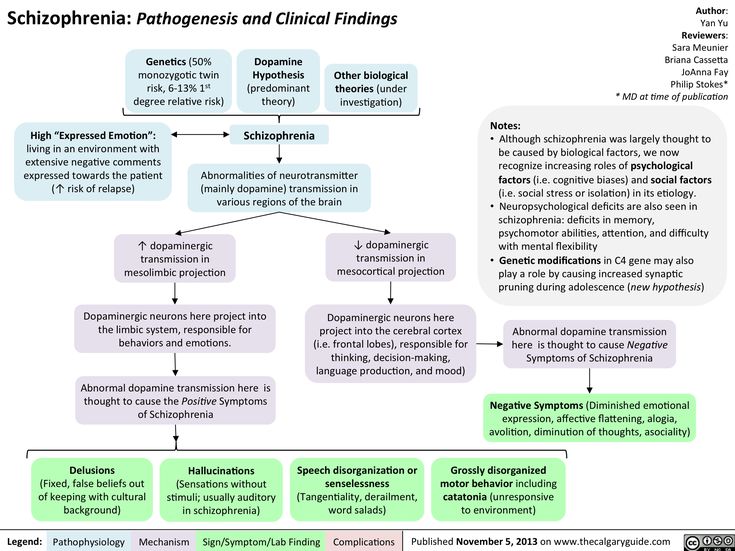 nine0006
nine0006
Patients have a painful feeling that everything around is somehow changed, devoid of naturalness, harmony (- derealization), the same feelings can arise in relation to their personality (- depersonalization). With depersonalization, the consciousness (but not the personality!) seems to split in two: one part of it looks at what is happening from the side, and the other is horrified by the realization of the loss of control over oneself.
One's own thoughts and ideas begin to be perceived as alien. According to modern views, this is why schizophrenia has verbal hallucinations (“voices”), and it is not surprising that the sound of “voices” inside the head is typical for this disease. For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common. nine0006
Such a growing wave of unusual sensations is very painful. In many cases, internal tension is somewhat relieved by the formation of delusional ideas (quickly - like an insight - the crystallization of delirium occurs).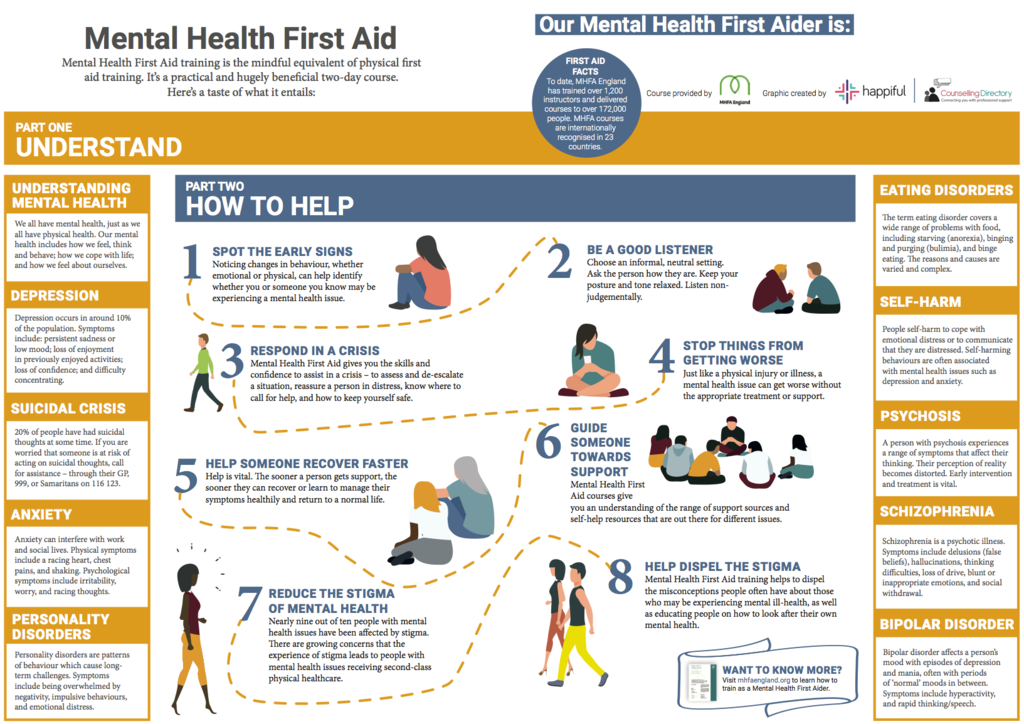 It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema. nine0006
It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema. nine0006
This whole clinical picture often develops acutely, in the form of an attack that lasts from several days to several months, and then may recur. Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness. But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more.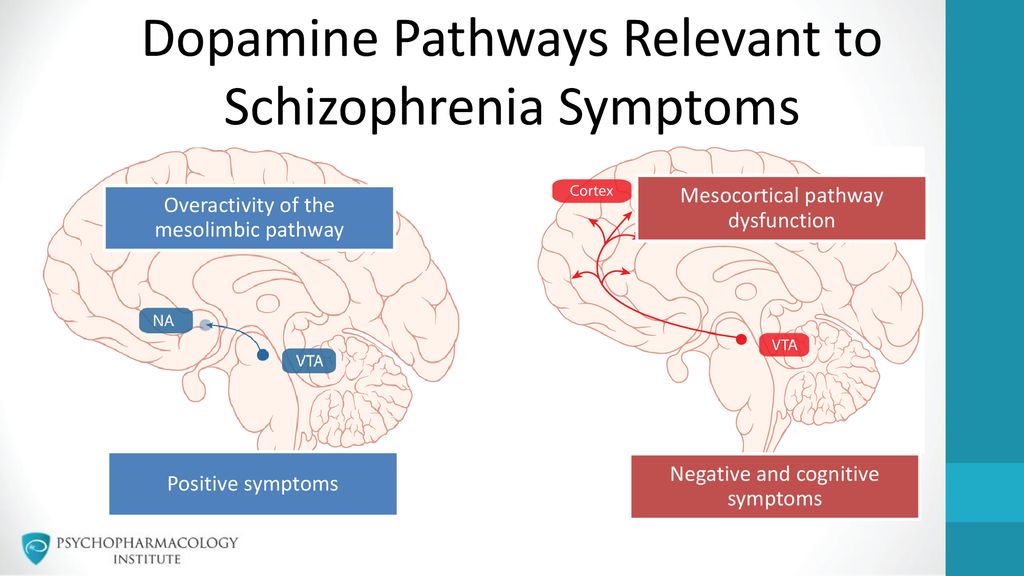 Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia. nine0006
Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia. nine0006
Patients either do not recognize themselves as ill or have conflicting thoughts about it. As a rule, they negatively meet the persuasion of relatives about the need to contact a psychiatrist. There are attempts to alleviate their condition with alcohol and drugs, which only complicates the clinical picture and leads to further social maladaptation.
Under the influence of orders "voices" and against the background of delusional experiences, the risk of socially dangerous actions of patients increases. For example, cases of attacks on imaginary "persecutors" are known. But much more often, patients with endogenous mental pathology commit OOD through other mechanisms, including when their behavior is influenced by alcohol or drug intoxication, which is superimposed on negative symptoms. nine0006
nine0006
Schizophrenia is the most common disease among patients in the Clinical Hospital No. 5 in Moscow.
Common diagnosis: Paranoid schizophrenia, episodic course with progressive defect, incomplete remission. The clinical picture with this diagnosis includes delusions and hallucinations (usually delusions of persecution and verbal hallucinations - "voices").
Treatment of schizophrenia includes antipsychotics, antidepressants, nootropics. The leading role belongs to antipsychotics, the action of which is aimed primarily at combating delusions and hallucinations. Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes. Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance.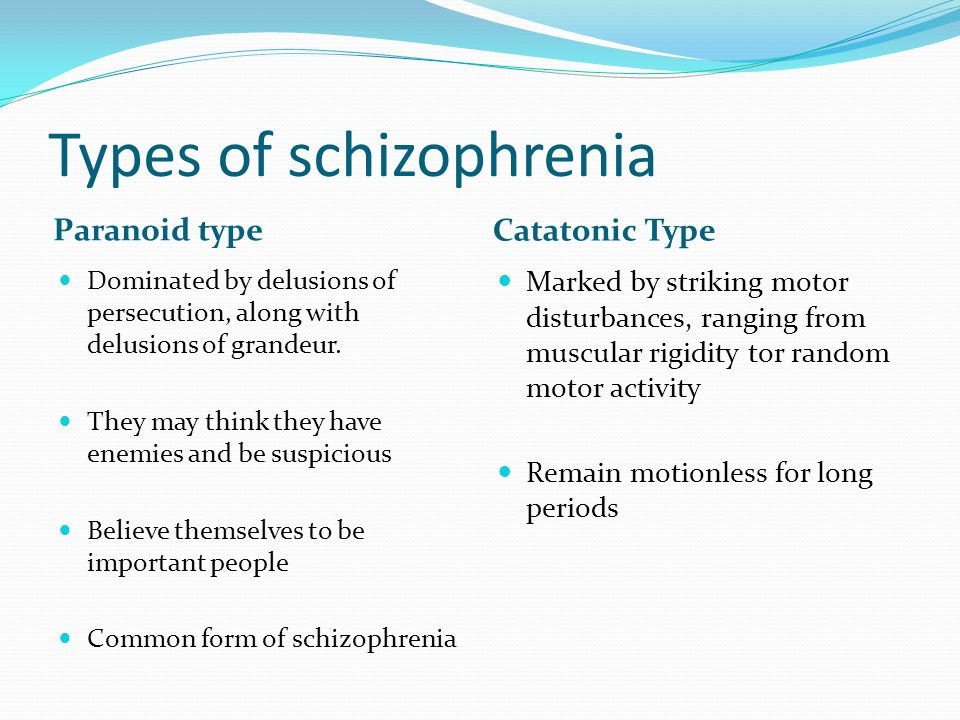 After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization. A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect. nine0006
After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization. A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect. nine0006
Although schizophrenia is a very formidable disease, it is not a death sentence. Due to the partial preservation of certain abilities (especially intellectual ones) and non-standard thinking, many of these patients have significant creative potential, which can be seen, among other things, from the works presented at the Ariadne's Thread festival of arts.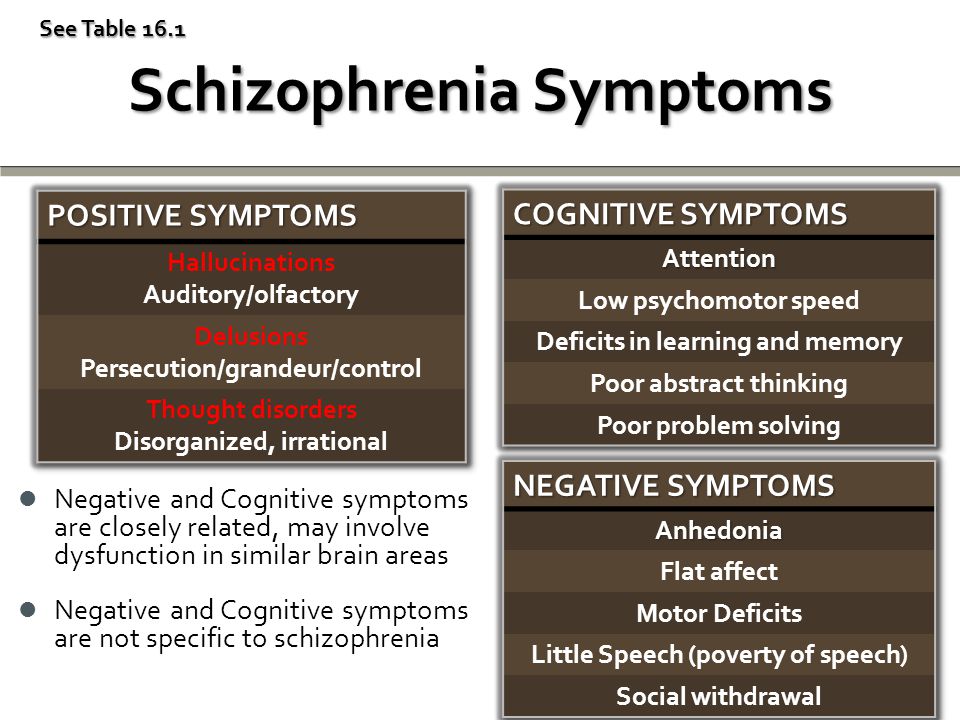
- Back
- Forward
- Are you here: nine0067
- Main page GBUZ "PKB No. 5 DZM" /
- For visitors /
- About mental disorders /
- Schizophrenia
Treatment of schizophrenia in St. Petersburg | Doctor SAN
- Home
- Psychiatry
- Treatment of schizophrenia
Schizophrenia (ICD-10 F20, ICD-11 6A20) is treated in our clinic on an outpatient or inpatient basis. We handle both the onset of schizophrenia and complex cases, including patients with resistance and drug intolerance. Hospitalization of adolescents is possible: girls - from 15 years old, boys - from 16 years old.
Consultations on the examination and treatment of children and adolescents are provided by a psychiatrist, an expert in the field of pharmacotherapy of mental disorders, Ph.D. I.I. Mechnikov, Alexey Viktorovich Bocharov. nine0006
Usually the treatment of the first episode and relapses of the disease is carried out in the clinic's hospital. As a rule, 2–4 weeks are enough to relieve an acute condition, to select the necessary therapy for schizophrenia. In the treatment of schizophrenia in a hospital, clinical psychologists and psychotherapists work with patients.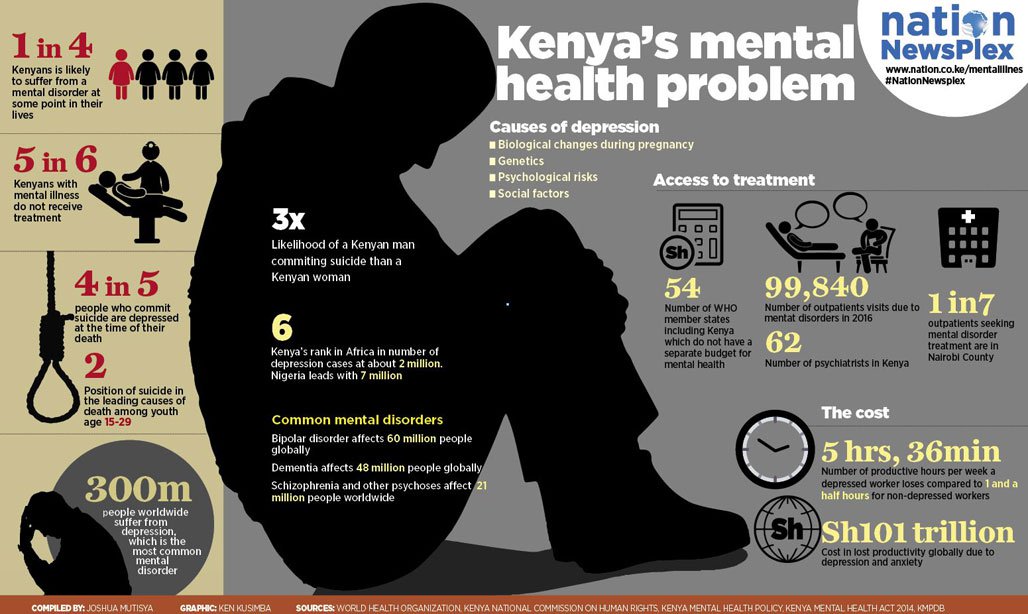 With mild psychotic symptoms, outpatient treatment is possible.
With mild psychotic symptoms, outpatient treatment is possible.
The experience of our doctors allows us to carry out intensified treatment (reduces the length of the patient's stay in the hospital), to select antipsychotic drugs with an improved therapeutic efficacy profile in the minimum effective dosages. In addition, we manage patients after discharge, provide specialized psychotherapeutic assistance in the framework of individual, family and group sessions. nine0006
Schizophrenia doctor's consultation:
+7 (812) 407-18-00
Thank you for your trust!
- Anonymous treatment without registration
- Intensive Care Hospital
- Re-episode prevention
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A.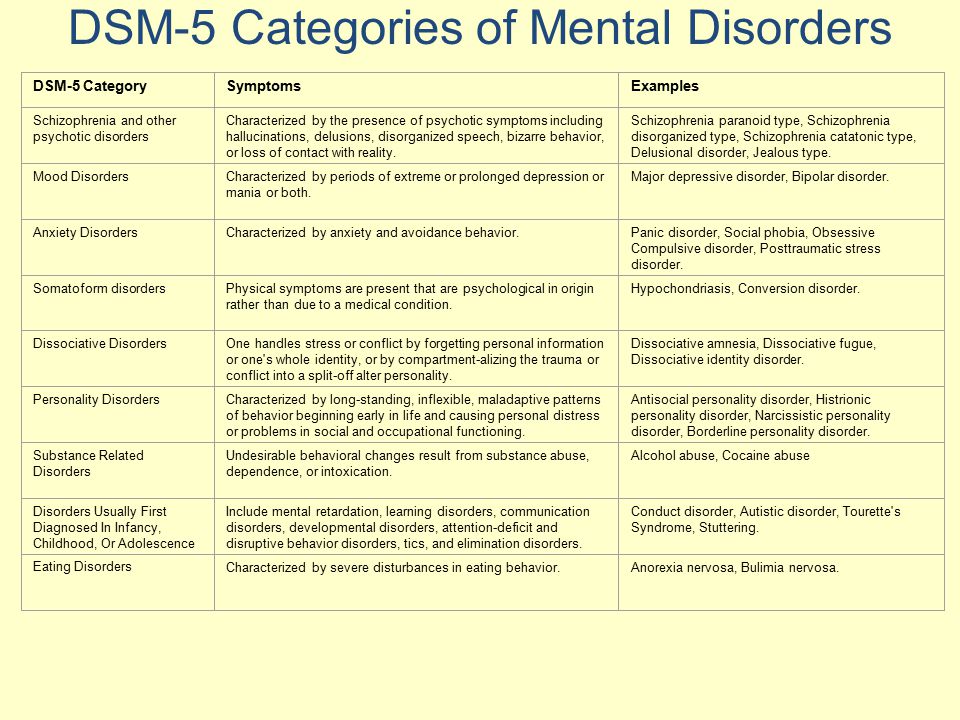 V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free nine0129 | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | nine0132 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Signs of the onset of schizophrenia
Symptoms of schizophrenia
Diagnosis of schizophrenia
Diagnosis of schizophrenia begins with an initial examination by a psychiatrist.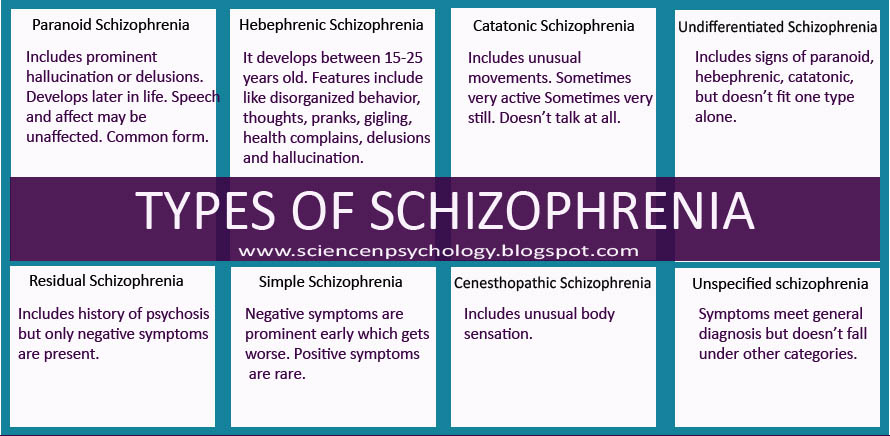 At the same time, it is important to understand that for an accurate diagnosis, observation is required for a long time - as a rule, from 1 year. Such observation makes it possible to determine the form and type of the course of the disease.
At the same time, it is important to understand that for an accurate diagnosis, observation is required for a long time - as a rule, from 1 year. Such observation makes it possible to determine the form and type of the course of the disease.
Initial examination by a psychiatrist
Initial examination by a psychiatrist includes a conversation with the patient, and, if possible, with his close relatives. Anamnesis allows you to collect information that will later allow you to choose the best diagnostic strategy. In particular, in such a conversation, the doctor clarifies the following questions:
- hereditary burden;
- premorbid personality traits;
- prodromal events;
- mental status at the time of examination;
- features of the course of the disease.
The conversation allows the doctor to get an idea about the patient - to identify accentuations of the character and features of the mental status of the individual; obtain information about development in childhood and adolescence; understand the peculiarities of relationships in the circle of close people and outside it. This information is necessary to differentiate the patient's personality and symptoms of schizophrenia. nine0006
This information is necessary to differentiate the patient's personality and symptoms of schizophrenia. nine0006
Standardized psycho-experimental testing of the patient by a clinical psychologist complements the information obtained during the collection of anamnesis about the patient, allowing a more accurate picture of the mental status, emotional and cognitive disorders.
Differential diagnosis
Differential diagnosis is necessary to rule out a somatic, neurological, organic and intoxicating nature of a mental disorder that may be the cause of a psychotic state with symptoms of schizophrenia. The following doctors are examining this patient:
- therapist;
- neurologist;
- cardiologist;
- gastroenterologist;
- narcologist.
In order to clarify the somatic status, in addition to consultation with doctors, the differential diagnosis of schizophrenia may include: general and biochemical blood tests, toxicological tests, urinalysis, ECG, EEG, MRI.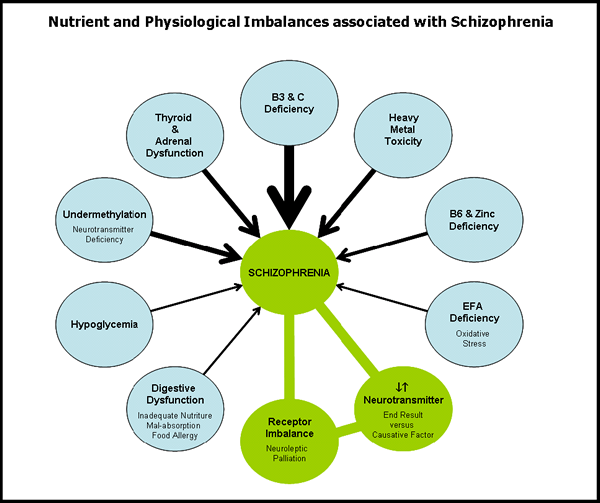
Treatment of schizophrenia in our clinic
Syndromes before and after treatment of schizophrenia
The treatment of schizophrenia consists of a combination of biological therapy and psychotherapy, including family sessions and social rehabilitation sessions, for example, in the form of group psychotherapy. Such an approach to treatment makes it possible to achieve stable long-term remission, restore relationships disturbed by the disease in the circle of close people, and adapt to life in society.
Treatment of schizophrenia in our clinic includes:
- examination;
- differential diagnosis;
- relief of a psychotic state;
- selection of psychopharmacotherapy;
- psychotherapeutic treatment;
- management of the patient after discharge.
Our doctors prefer antipsychotics with an improved therapeutic efficacy profile. In particular, we take on complex cases, cases with individual drug intolerance and resistance. Also in our clinic there is the possibility of non-drug treatment of schizophrenia using modern modified electroconvulsive therapy (ECT). nine0006
In particular, we take on complex cases, cases with individual drug intolerance and resistance. Also in our clinic there is the possibility of non-drug treatment of schizophrenia using modern modified electroconvulsive therapy (ECT). nine0006
Particular attention in the treatment of schizophrenia in the clinic is given to the psycho-emotional state of patients. Our clinical psychologists and psychotherapists conduct daily group sessions where patients work through experiences, fears, learn to understand the features of their condition and control it.
Selection of psychopharmacotherapy
Depending on the case, the relief of an acute condition and the selection of psychopharmacotherapy can be carried out on an outpatient basis or in a hospital. For example, if a patient is critical of his condition, understands the need for treatment and is ready to follow the doctor's recommendations, an outpatient selection of biological therapy is possible. Treatment of schizophrenia in a hospital is necessary in cases where the removal of an acute condition and the rapid selection of psychopharmacotherapy are required.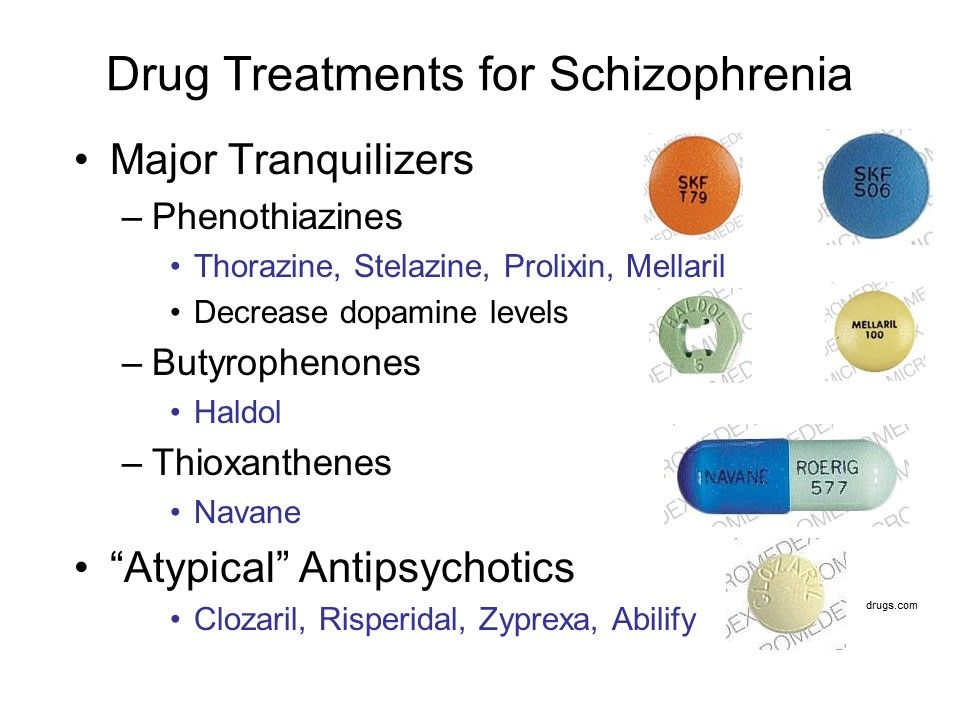 nine0006
nine0006
As a rule, it takes 2–4 weeks to select psychopharmacotherapy in a hospital setting. Outside the hospital, this period can range from 6–8 weeks to several months. Therefore, when choosing a treatment option for schizophrenia, one should take into account the severity of the psychotic state - the presence and severity of signs of psychosis, which include:
- behavioral disorders;
- aggression;
- suicidal tendencies;
- psychomotor agitation; nine0066 anxiety, fear;
- ecstasy;
- depression;
- hallucinations;
- delirium;
- sleep disorders;
- negativism;
- disorders of consciousness.
Quite often patients with schizophrenia suffer from depression. In the presence of these symptoms, we select an antidepressant that is compatible with the treatment of schizophrenia.
Stabilization of remission
Success in the selection of psychopharmacotherapy consists in achieving remission with a complete or significant reduction in productive symptoms, as well as with a favorable effect on the negative.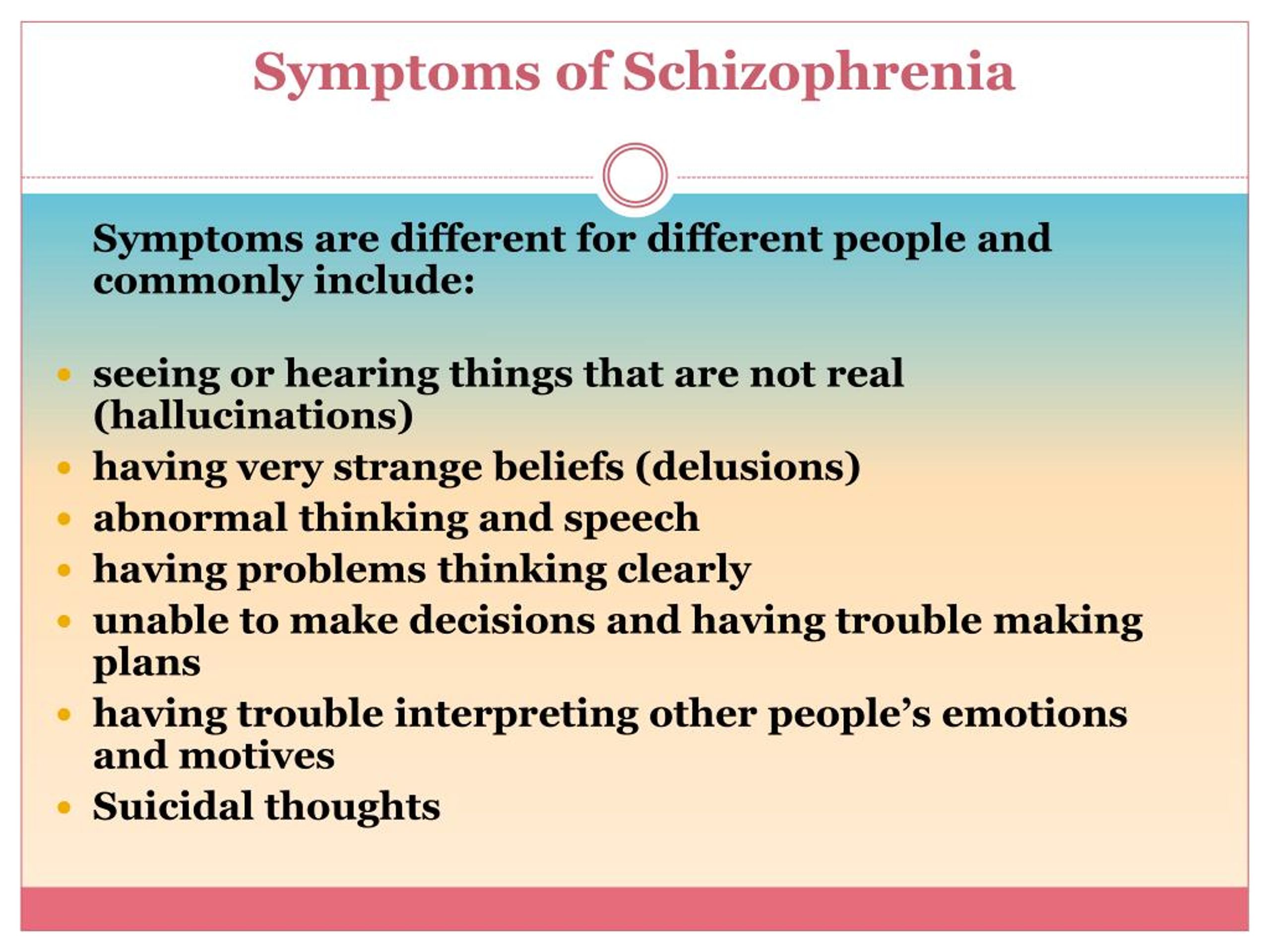 As a rule, it takes 3 to 9 days to stabilize remission.months. At this stage of drug treatment of schizophrenia, there is a gradual decrease in the dosage of the antipsychotic or a change in the drug, a modification of the selected psychopharmacotherapy.
As a rule, it takes 3 to 9 days to stabilize remission.months. At this stage of drug treatment of schizophrenia, there is a gradual decrease in the dosage of the antipsychotic or a change in the drug, a modification of the selected psychopharmacotherapy.
At a distance of stabilization of remission, both the patient and his relatives should pay special attention to the current state of health in order to avoid a relapse of the disease, contact the attending physician in time (at the first sign of deterioration of the condition) and promptly correct the drug treatment, anticipating a detailed picture of psychosis. nine0006
Anti-relapse therapy
Long-term outpatient or anti-relapse therapy is carried out at a distance of 1–2 years. At this stage in the treatment of schizophrenia, the effectiveness of biological therapy aimed at maintaining remission, preventing new psychotic episodes and slowing down the course of the disease is evaluated. In addition, at this stage, an assessment is made of the reduction of negative and cognitive disorders, the level of the patient's social functioning.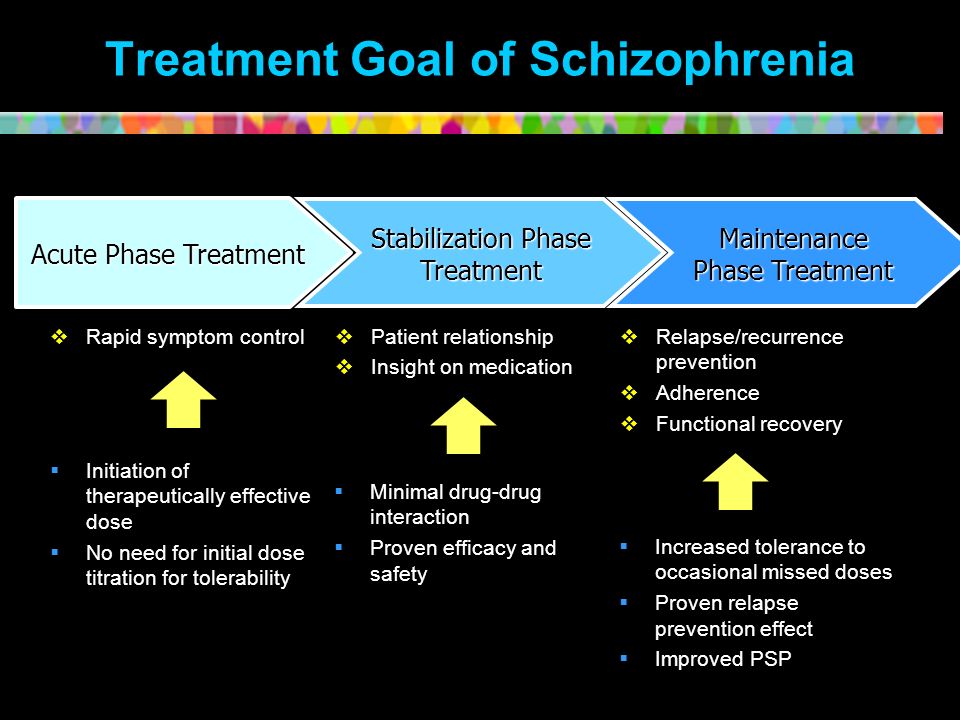
Unfortunately, after feeling better, some patients stop taking their prescribed medications. Discontinuation of treatment leads to an exacerbation of the disease and requires the selection of anti-relapse antipsychotic maintenance therapy. nine0006
During the period of long-term outpatient therapy, follow-up visits to the attending physician should not be neglected. Such visits can prevent an exacerbation of the disease - to carry out early treatment on an outpatient basis or as part of a short hospitalization in order to relieve a developing acute condition.
Depending on the type of disease course, maintenance therapy for the treatment of schizophrenia may be reasonable (defined by a paroxysmal course of the disease, precedes an expected exacerbation), long-term (for example, for 2-5 years) or permanent (with a continuous course of the disease). The timing of anti-relapse therapy is also affected by the individual characteristics of the patient, his motivation, psychosocial situation, and other indirect factors that can provoke a relapse of the disease.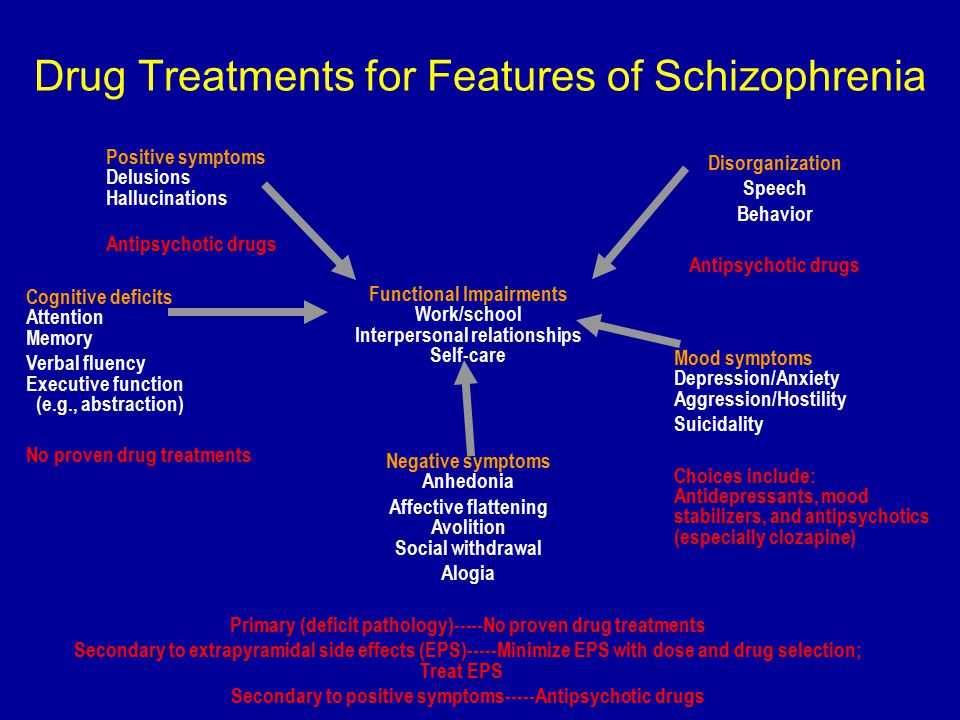 nine0006
nine0006
After discharge
Psychosocial rehabilitation
Biopsychosocial model for the development of psychosis
Psychosocial therapy is carried out in parallel with drug treatment. As a rule, it begins after the relief of an acute condition. Our clinic has a powerful psychotherapeutic support for patients. Individual sessions with a psychotherapist help the patient relieve stress, begin to work through strong inner feelings and fears, group sessions allow the patient to restore and develop the skills necessary to return to the family and society. nine0006
Individual psychotherapy
Psychosocial therapy is carried out in parallel with drug treatment. As a rule, it begins after the relief of an acute condition. Our clinic has a powerful psychotherapeutic support for patients. Individual sessions with a psychotherapist help the patient relieve stress, begin to work through strong inner feelings and fears.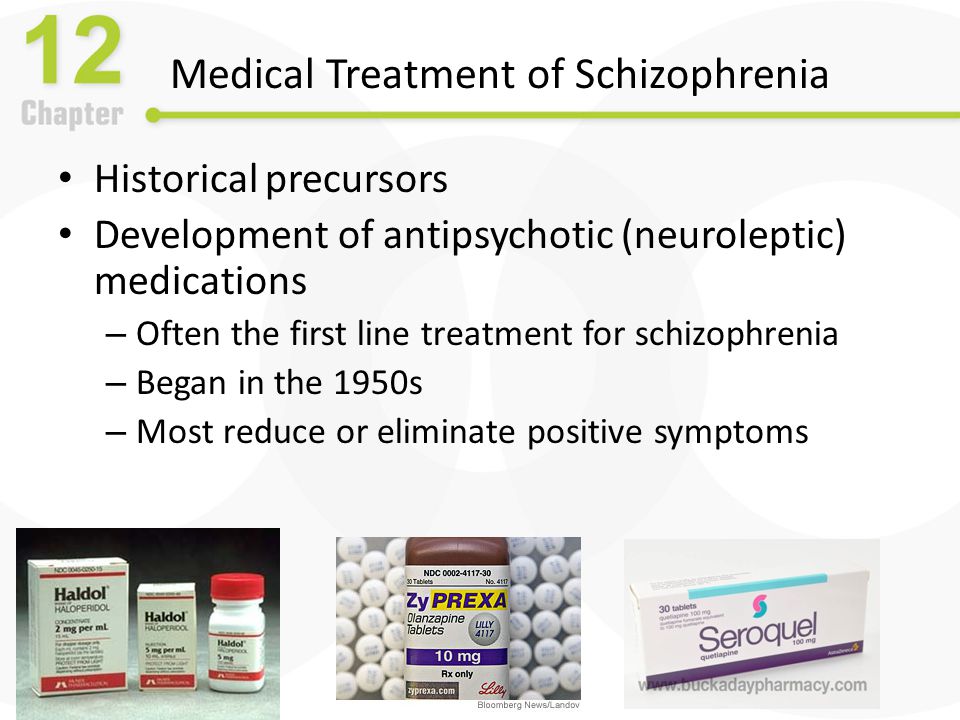
As part of individual psychotherapy for the treatment of schizophrenia it is possible to complete specialized modules, for example:
- social skills;
- communication skills;
- skills of confident behavior;
- independent living skills;
- coping skills for residual psychotic disorders;
- cognitive training.
In other words, individual sessions with a psychotherapist involve work to restore a person's cognitive, motivational and emotional resources, as well as the skills, knowledge and skills necessary for a full life in the family and society. nine0006
Group psychotherapy
In addition, we have open and closed psychotherapy groups. Working in a psychotherapeutic group allows, in conditions comfortable for the patient and under the supervision of leading psychotherapists, to adapt to life in society, overcome difficulties in communicating with other people, receive feedback and support from the participants.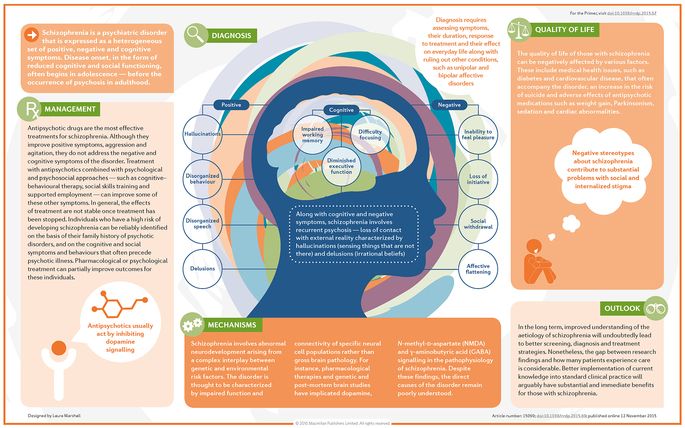 The group format is well suited for developing and consolidating social skills and role functions in order to achieve a full-fledged position in society. nine0006
The group format is well suited for developing and consolidating social skills and role functions in order to achieve a full-fledged position in society. nine0006
Family psychotherapy
Family therapy is necessary for the closest people to learn about the peculiarities of the course of the disease, to learn the correct behavior with the patient (they could control medication, recognize the first signs of a relapse). The result of such work will be to strengthen trust between family members by reducing stress levels and getting rid of false fears and concerns.
The treatment of schizophrenia should not be limited to the removal of an acute condition and the selection of pharmacotherapy. The duration and quality of remission largely depend on the patient's willpower, partnerships with the attending physician and a favorable atmosphere in the family. nine0006
References
Schizophrenia - https://apps.who.int
Schizophrenia Treatment: Types of Therapies and Medication - https://www.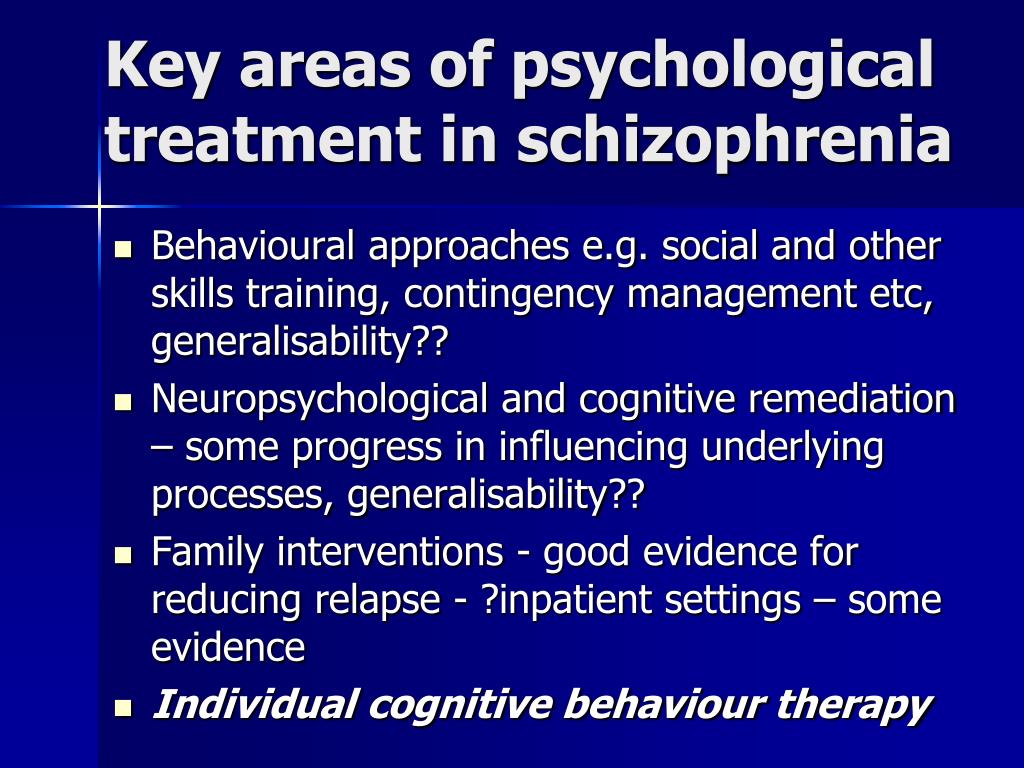 webmd.com
webmd.com
World Health Organization. Schizophrenia – https://www.who.int
Update date: 11/30/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set) nine0006
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
January 10
Tomorrow
January 11
Thursday
January 12
Friday
January 13
Saturday
January 14
Sunday
January 15
Monday
January 16
Tuesday
January 17
Wednesday
January 18
Thursday
January 19
Friday
January 20
Saturday
January 21
Sunday
January 22
Monday
January 23
Tuesday
January 24
Wednesday
January 25
Thursday
January 26
Friday
January 27
Saturday
January 28
Sunday
January 29
Monday
January 30
Tuesday
January 31
Schizophrenia is being treated
nine0002 Bocharov AlexeyViktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
nine0002 Sinenchenko AndreyGeorgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
nine0002 Zun SergeyAndreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Head of amb.