Treatment for disorganized schizophrenia
Disorganized Schizophrenia (Hebephrenia): Symptoms & Treatment
Schizophrenia
Disorganized schizophrenia, or hebephrenia, is one of the five subtypes of schizophrenia. Learn about the symptoms of disorganized schizophrenia and how it can be treated here
Katie Hurley, LCSW
Disorganized schizophrenia is one of the five subtypes of schizophrenia. It is characterized by disorganized behavior and speech and includes disturbance in emotional expression. Hallucinations and delusions are less pronounced with disorganized schizophrenia, though there is evidence of these symptoms occurring.
Symptoms of disorganized schizophrenia
Disorganized Speech
Schizophrenia can cause people to have difficulty concentrating and maintaining a train of thought, which manifests in the way they speak. People with disorganized speech might speak incoherently, respond to questions with unrelated answers, say illogical things, or shift topics frequently. Signs of disorganized speech involve the following:
Loose associations: Rapidly shifting between topics with no connections between topics
Perseveration: Repeating the same things over and over again
Made up words that only have meaning to the speaker
Use of rhyming words without meaning
When cognitive disorganization is severe, it can be nearly impossible to understand what the person is saying.
Disorganized Behavior Schizophrenia negatively impacts goal-directed behavior. A person with disorganized schizophrenia is likely to have difficulty beginning a specific task (ex: cooking a meal) or difficulty finishing a task. Independent functioning is exceptionally difficult due to this gross disorganization.
Disorganized behavior can manifest as the following:
A decline in overall daily functioning
Unpredictable or inappropriate emotional responses
Lack of impulse control
Behaviors that appear bizarre or lack purpose
Routine behaviors such as bathing, dressing, or brushing teeth can be severely impaired or lost.
Inappropriate Affect Affect refers to a person’s emotional responses, including the way emotions are expressed (ex: smiling when feeling happy.) People with disorganized schizophrenia exhibit flat affect, which means that they show little or no emotions in their facial expressions, voice tone, or mannerisms. At times they exhibit affect that is inappropriate to the situation, such as laughing at something sad. In addition to lack of emotional expression, people with disorganized schizophrenia are likely to experience other negative symptoms, including failing to make eye contact and blunt facial expression.
Disorganized schizophrenia is associated with early onset, between the ages of 15-25. Earlier age of onset is traditionally associated with a worse prognosis due to lower educational achievement, more prominent negative symptoms, and cognitive impairments. Early detection, diagnosis, and treatment of the disorder contributes to better outcomes.
Treatment
Beginning treatment as soon as possible is crucial to making a recovery.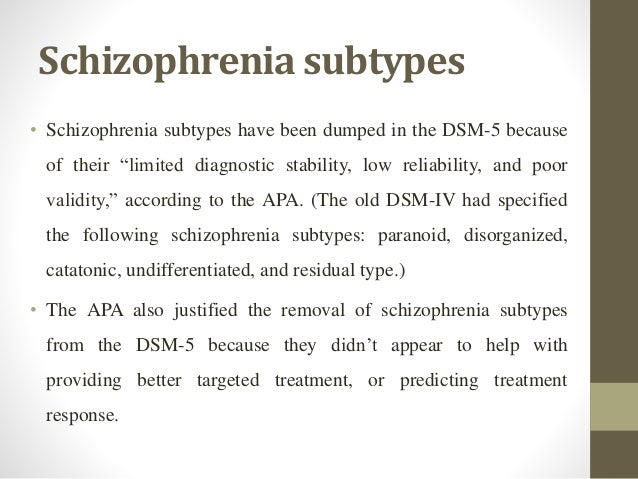 Treatment for disorganized schizophrenia involves a multimodal approach, including the following:
Treatment for disorganized schizophrenia involves a multimodal approach, including the following:
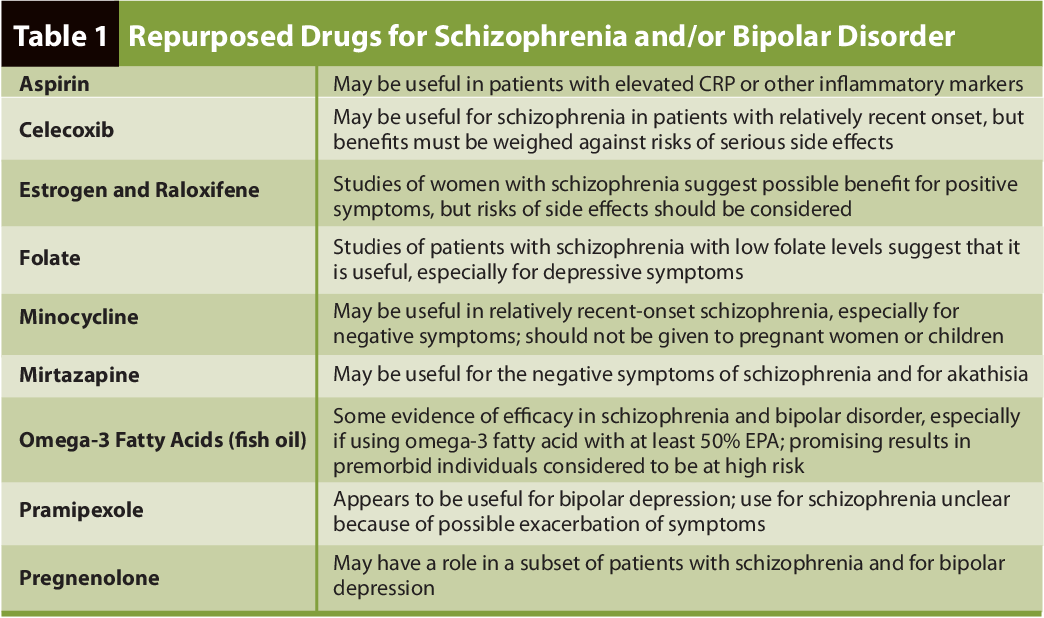
Medication management: Medication for schizophrenia can help reduce hallucinations and delusions, paranoia, and disordered thinking. Finding the right medication depends on the prominent symptoms of the disease.
Psychotherapy: Cognitive Behavioral Therapy (CBT) is recommended to reduce certain symptoms and enhance overall functioning. Through CBT, individuals identify target problems and work to develop coping strategies specific to those issues.
Life skills training: Assistance with life skills can help individuals with disorganized schizophrenia improve social interactions and increase daily living skills, with a goal of increasing independence.
Supported employment services: Individuals with disorganized schizophrenia benefit from training in the area of finding and maintaining employment.
Family education and support: Individuals with disorganized schizophrenia benefit from ongoing contact with family.
 Support to educate family about treatment and how to support a family member with schizophrenia is crucial. Family support increases family member’s understanding of the disorder and helps family members develop coping strategies.
Support to educate family about treatment and how to support a family member with schizophrenia is crucial. Family support increases family member’s understanding of the disorder and helps family members develop coping strategies.
Though the signs of disorganized schizophrenia tend to appear at a younger age, they can be difficult to spot. The symptoms of this subtype are often very gradual and unlikely to subside. With appropriate and ongoing treatment, however, the prognosis for disorganized schizophrenia improves. Assistance with daily living skills, educational attainment, employment services, and family support play a key role in improving the course of the disease for individuals diagnosed with disorganized schizophrenia.
- American Psychiatric Association, “Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition”, American Psychiatric Publishing, Washington, D.C., (2013): Pages 99-105.
- Shean, G., “Empirically Based Psychosocial Therapies for Schizophrenia: The Disconnection between Science and Practice”, Schizophrenia Research and Treatment, Volume 2013 (2013).
Notes: This article was originally published December 22, 2017 and most recently updated May 21, 2021.
Disorganized Symptoms and Treatment Options
Not everyone living with schizophrenia experiences it in the same way. It may depend on the subtype, and disorganized schizophrenia is one of them.
Schizophrenia is a formal mental health diagnosis. Yet, there’s more than one type of schizophrenia, and this categorization depends on the symptoms you may be living with.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) no longer subdivides schizophrenia. In other words, the schizophrenia subtypes aren’t considered separate diagnoses. However, terms for different subtypes are sometimes used in clinical and social settings.
Subtypes of schizophrenia include:
- paranoid schizophrenia: schizophrenia symptoms with intense persecutory delusions
- catatonic schizophrenia: schizophrenia symptoms with catatonia
- hebephrenic or disorganized schizophrenia: schizophrenia symptoms with disorganized features
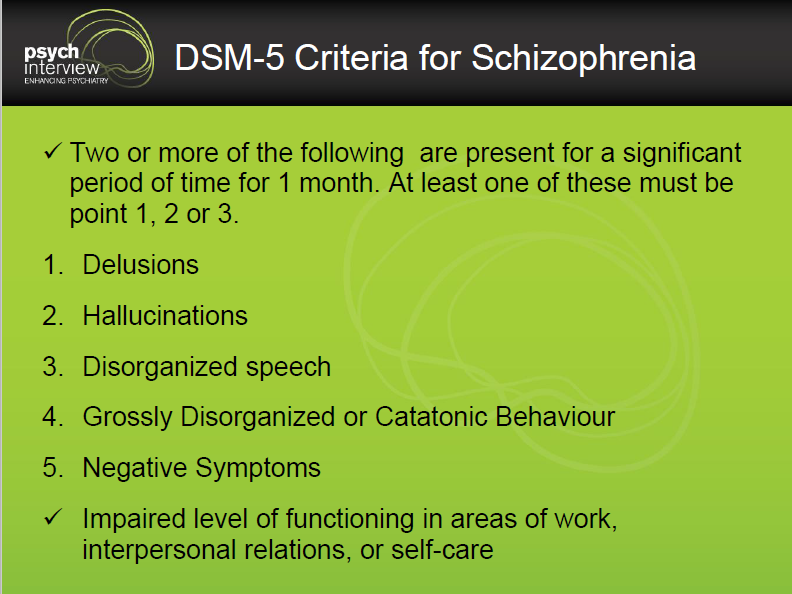
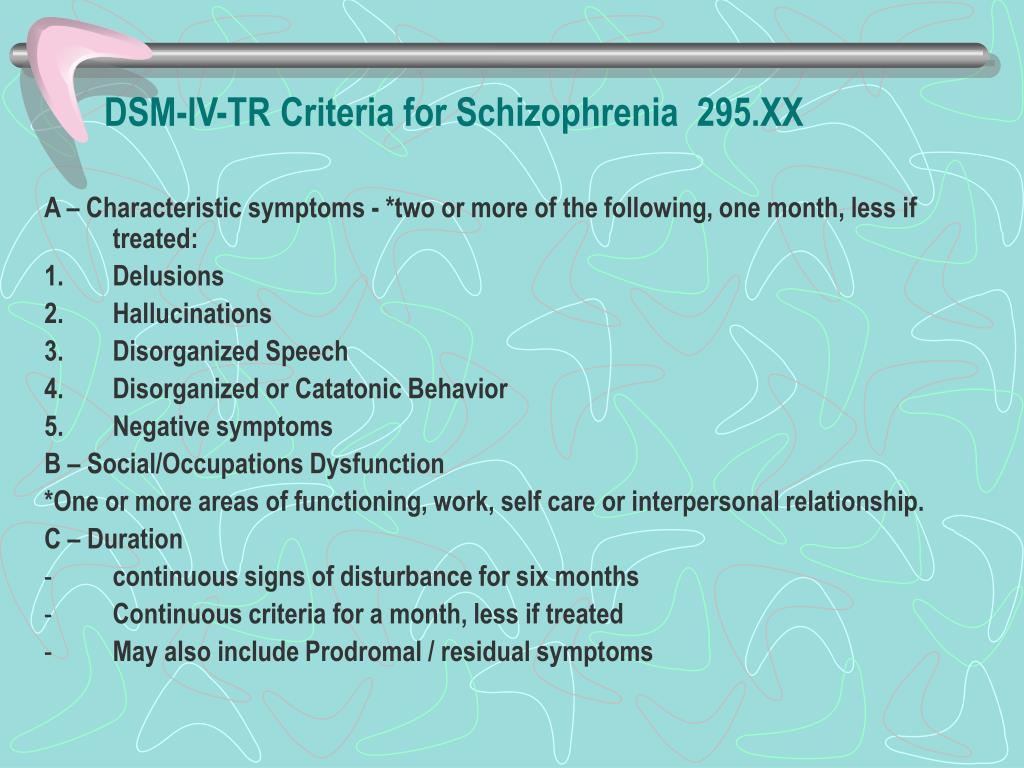
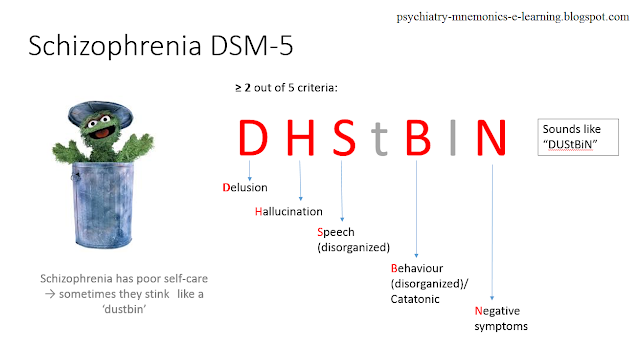
The DSM-5 establishes the formal symptoms of the condition.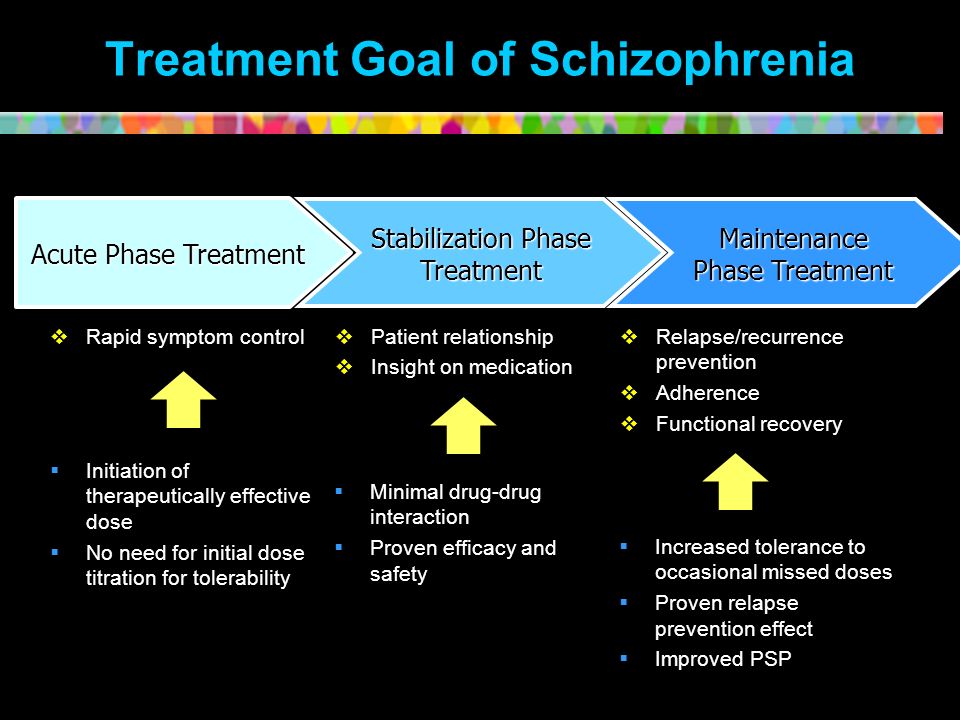 These include:
These include:
- delusions and hallucinations
- positive symptoms
- negative symptoms
Although schizophrenia can be a misunderstood and stigmatized condition, with professional support, it’s possible to manage symptoms and live a fulfilling life.
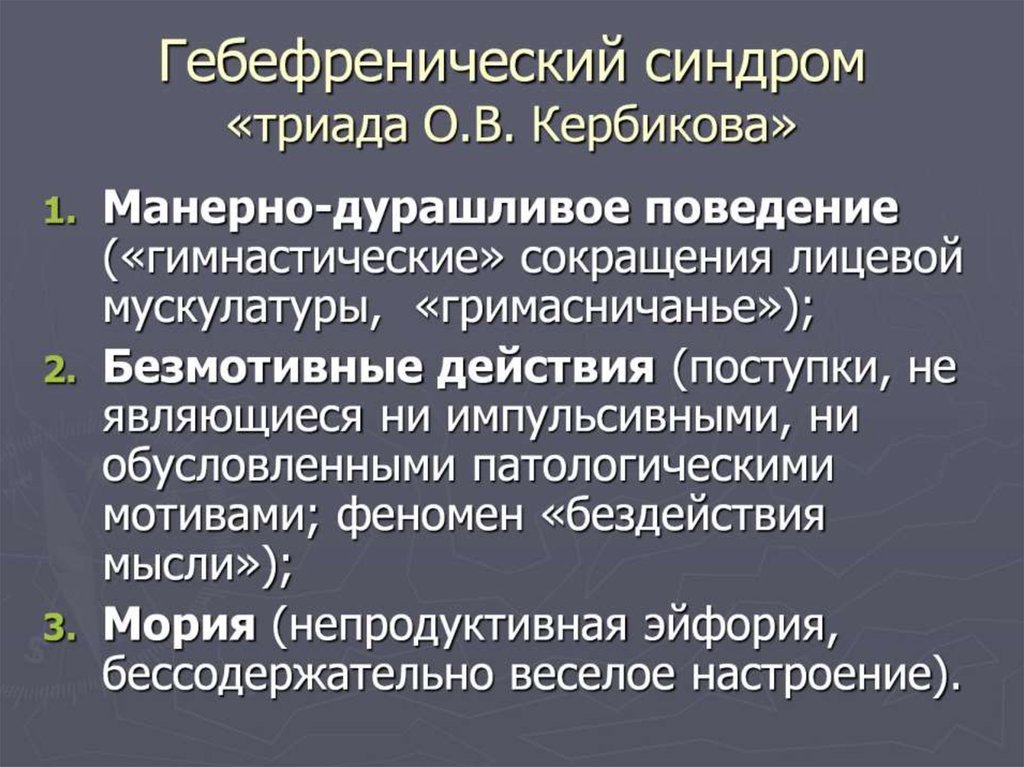
Disorganized schizophrenia is sometimes referred to as hebephrenic schizophrenia because its onset is usually between ages 15 and 25. “Hebephrenia” is rooted in the Greek word for “adolescence.”
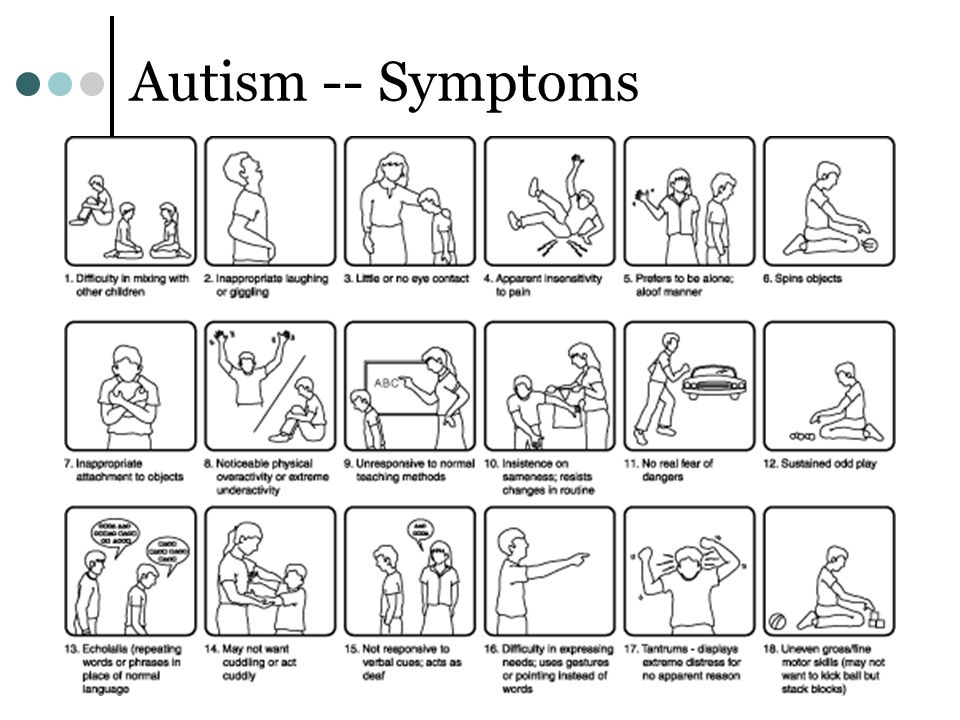
Symptoms that may be considered “disorganized” include:
- incoherent speech or speech that switches quickly from topic to topic
- flat facial expressions or those that aren’t appropriate to the situation
- showing little to no emotion in gestures and tone of voice
- unpredictable reactions (for example, laughing in a serious situation)
- disorganized thought processes and behaviors that affect work, school, hygiene, and relationships
Someone with disorganized schizophrenia might also experience delusions and hallucinations, and other symptoms of schizophrenia.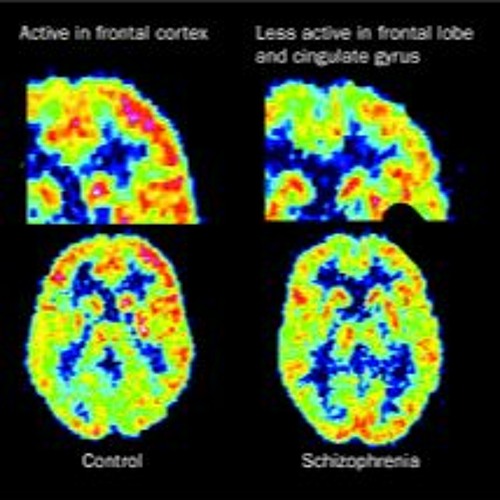
Before schizophrenia is diagnosed, a health professional may want to rule out other potential explanations for the symptoms, such as:
- substance use
- schizoaffective disorder
- bipolar disorder with psychosis
- brain injuries
Formal symptoms of schizophrenia
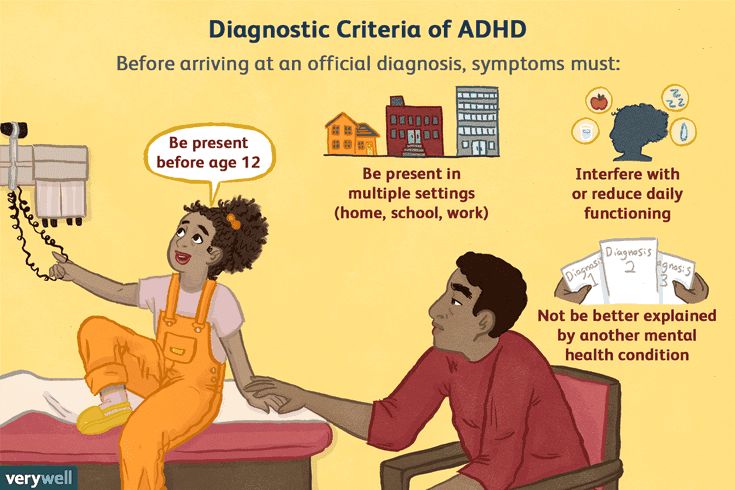
To receive a schizophrenia diagnosis, someone must persistently experience two or more of the following symptoms for at least a month:
- delusions
- hallucinations
- incoherent speech or rambling
- severely disorganized behavior in one or more aspects
- negative symptoms like avolition, lack of pleasure, blunted affect, or alogia
Clinicians also need to confirm:
- presence of one or more of the first three symptoms (delusions, hallucinations, and disorganized speech)
- these symptoms have a significant impact on one or more major areas of the person’s life (work, school, relationships)
- continuous signs of disturbance over a period of six months
People with schizophrenia are prone to disorganized speech, thinking, and behavior.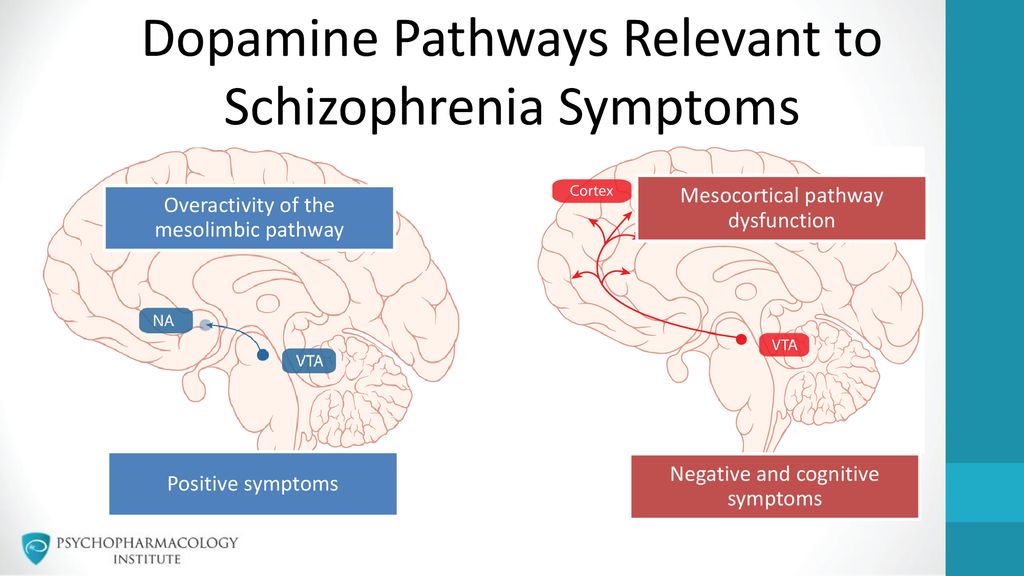 This shows up differently in different people, and not everybody with schizophrenia will behave the same.
This shows up differently in different people, and not everybody with schizophrenia will behave the same.
Disorganized means that there’s no consistent pattern or that it’s difficult for you to formulate and express ideas, or behave accordingly to the situation.
When you live with hebephrenic schizophrenia, you’re more likely to experience these disorganized symptoms.
Disorganized speech
- difficulty followiig conversations
- hard time using and ordering words correctly to form coherence sentences
- tendency to repeat words or ideas
- coming up with made-up words
- answering questions with unrelated information
- jumping from one topic to another quickly
- incoherent writing
Disorganized thinking
- difficulty understanding what others are expressing
- hard time reading or listening, or following an idea
- low ability to organize thoughts and ideas
- difficulty following and completing tasks
- forgetting and losing things
- difficulty creating and following a plan or routine
- difficulty focusing or remembering things
Disorganized behavior
- pacing or wandering around aimlessly
- difficulty following tasks like maintaining hygiene, getting dressed, or cleaning
- childlike or regressive behavior
- social withdrawal
- difficulty attending school or work
- emotionless facial expressions or mannerisms
Yes.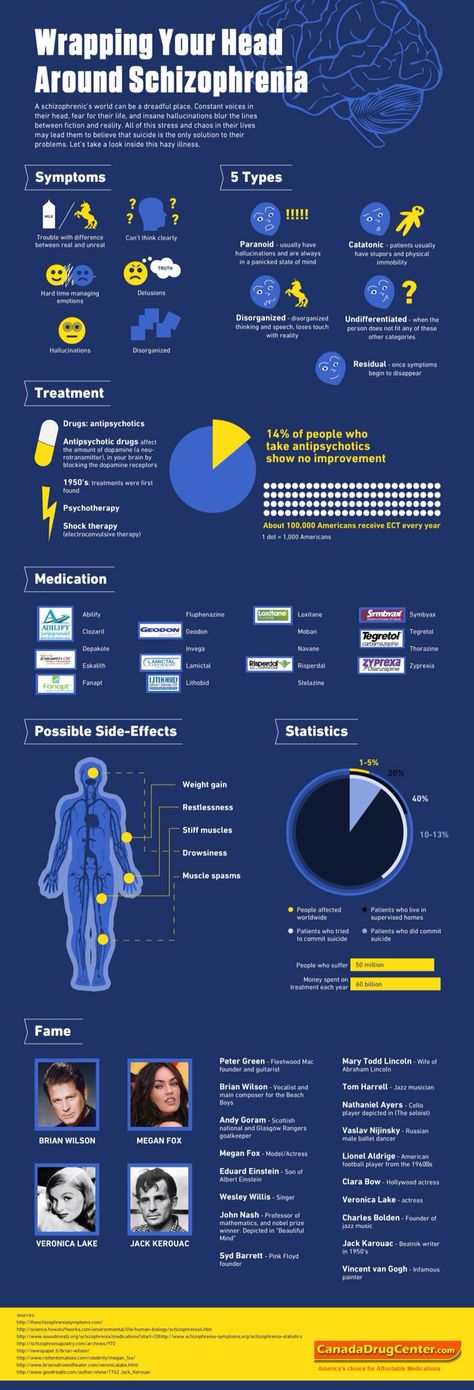 All subtypes of schizophrenia can be treated with a combination of:
All subtypes of schizophrenia can be treated with a combination of:
- medications (particularly antipsychotic medication)
- talk therapy, particularly cognitive behavioral therapy, social skills training, and social cognition training
- social support from family and community
- self-care strategies
- hospitalization (if and when needed)
The treatment plan for disorganized schizophrenia will vary from person to person depending on your specific circumstances and needs.
Although schizophrenia can’t be cured, it’s possible to live a fulfilling, happy life with the condition because symptoms can be managed with professional support.
Symptoms may re-emerge from time to time, but sticking with professional treatment can help you tremendously.
Although the DSM-5 doesn’t distinguish between different types of schizophrenia, some clinicians categorize the condition depending on the most impactful symptoms.
Disorganized schizophrenia is also called hebephrenic schizophrenia because it usually develops during the teen years.
Disorganized schizophrenia is associated with symptoms like disorganized speech, thinking, and behavior. These can make it difficult to carry out daily tasks and communicate with others.
Hebephrenic schizophrenia can also present with other symptoms like lack of motivation, no emotional expression, hallucinations, and delusions.
Disorganized schizophrenia can’t be cured, but all types of schizophrenia can be treated. This means you can manage your symptoms so they don’t affect your life.
Treatment for schizophrenia typically includes:
- talk therapy
- medications
- self-care strategies
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.
- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
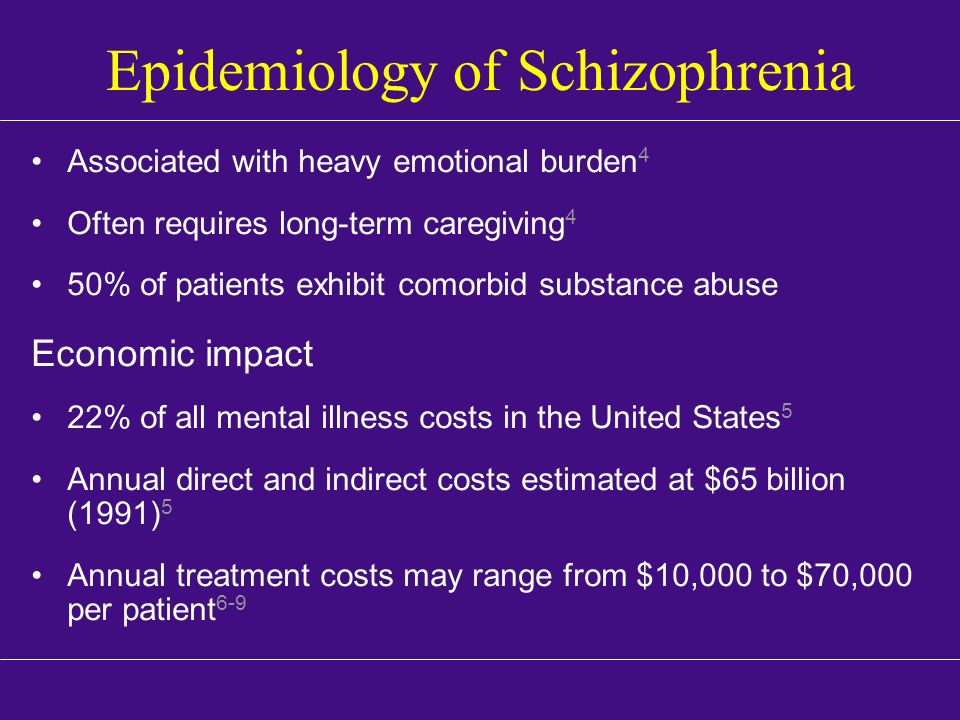
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.

- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
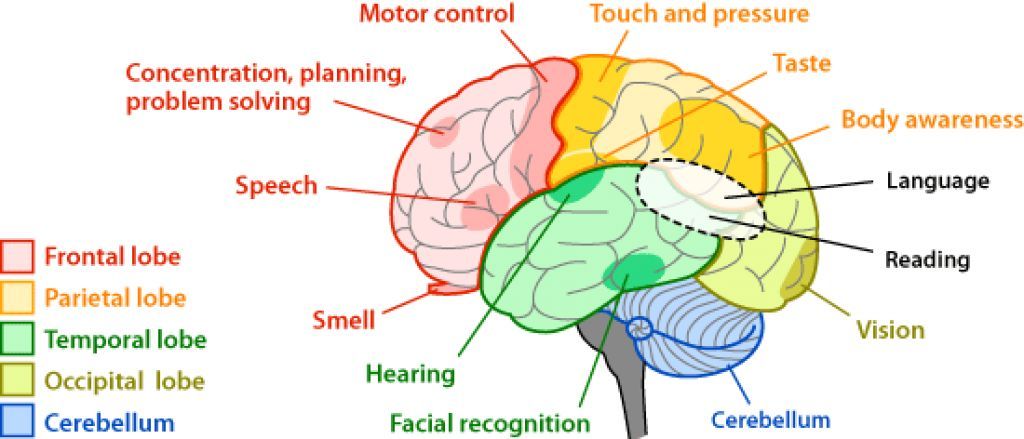
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).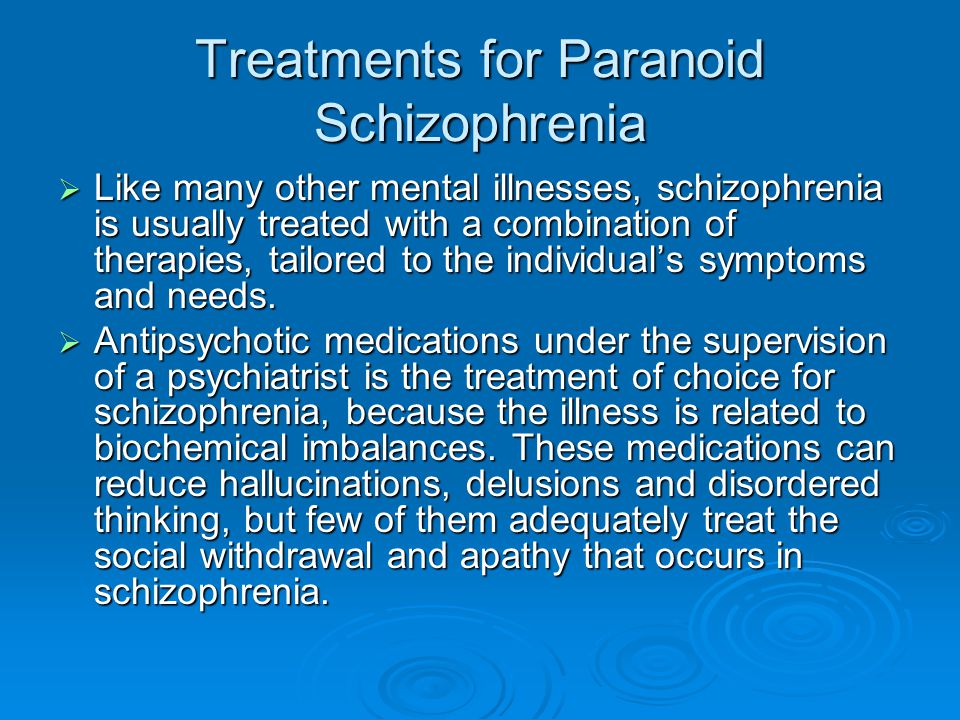 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.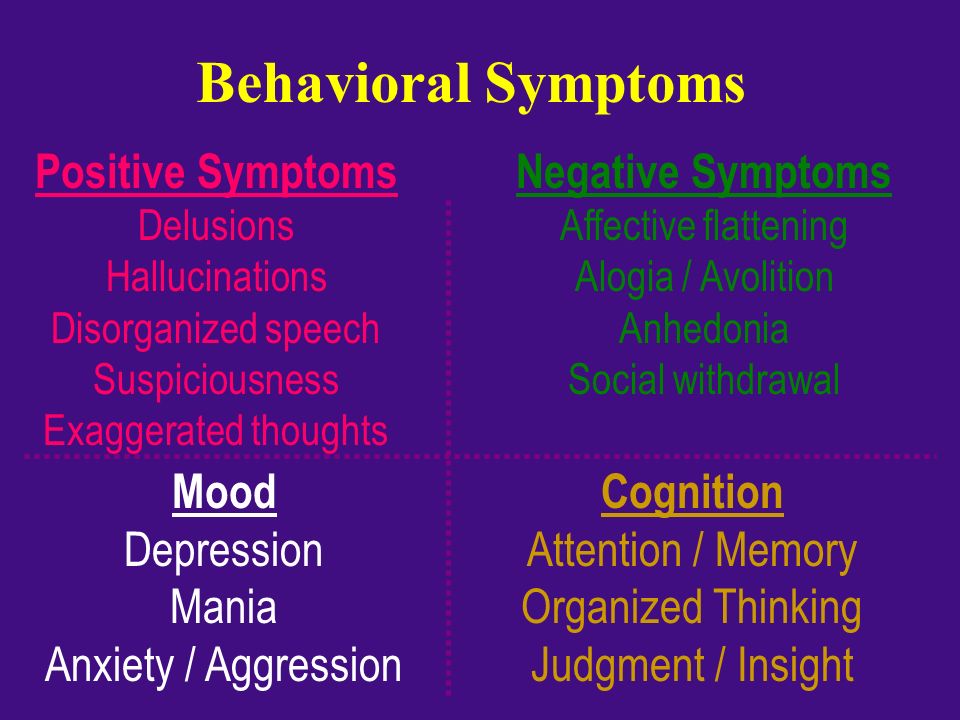
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.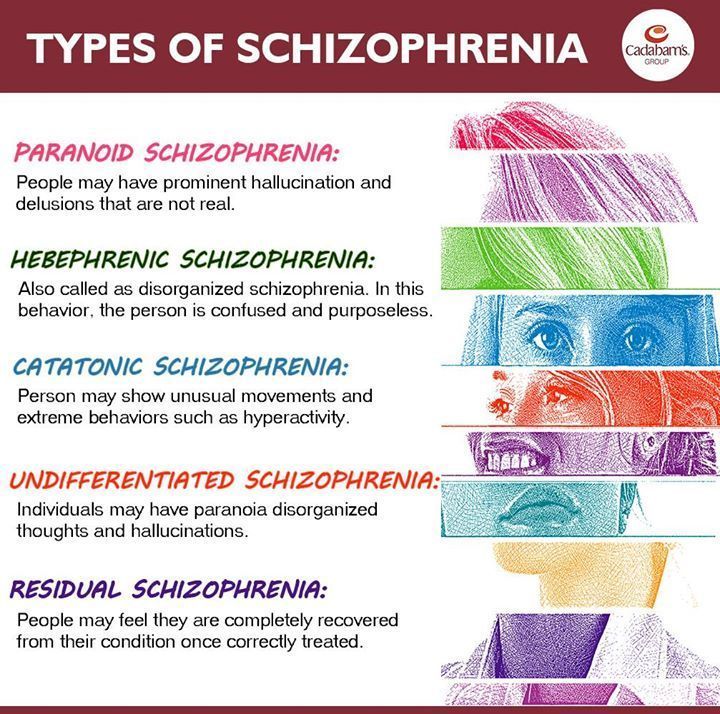 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).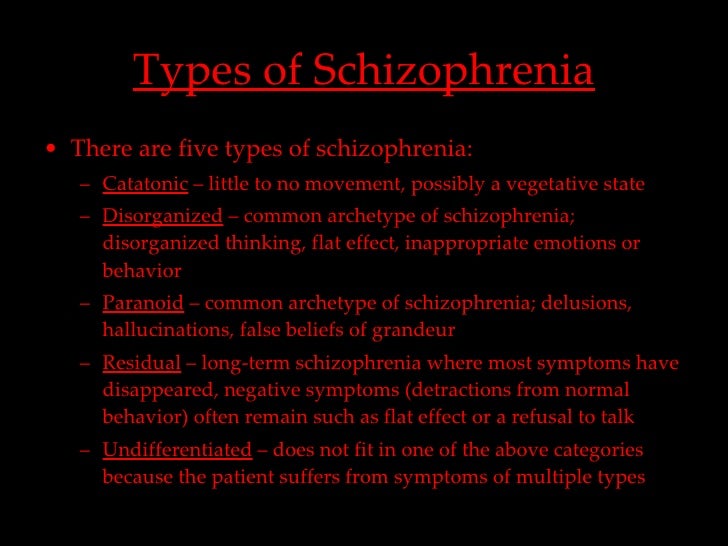 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.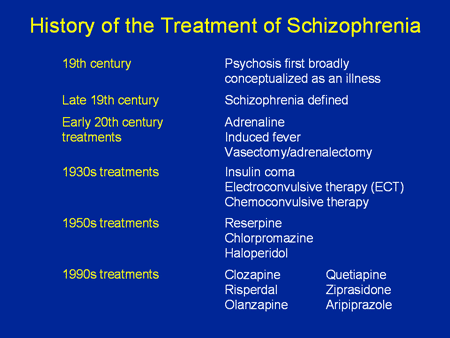 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.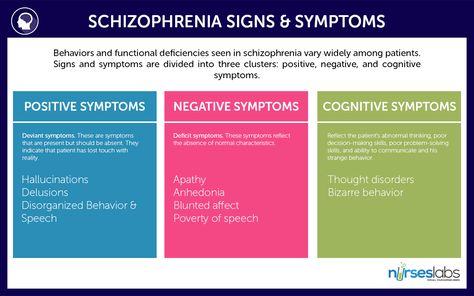 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Treatment of hebephrenic schizophrenia in St. Petersburg
- Main
- Psychiatry
- Treatment of schizophrenia
- Hebephrenic schizophrenia
We diagnose and treat hebephrenic schizophrenia in adults and adolescents (girls from 14 years of age and boys from 15–16 years of age can be hospitalized). Due to the intensification of treatment, the selection of pharmacotherapy and its correction in a hospital takes no more than 10–15 days.
Treatment of hebephrenic schizophrenia in adolescents is carried out under the supervision of Aleksey Viktorovich Bocharov, a child psychiatrist, Doctor of Medical Sciences, a recognized expert in the field of pharmacotherapy of mental disorders, associate professor of the North-Western State Medical University. I.I. Mechnikov and SPbMAPO.
I.I. Mechnikov and SPbMAPO.
In addition to the selection of pharmacotherapy in safe effective dosages, our patients receive psychotherapeutic assistance. This approach to the treatment of hebephrenic schizophrenia makes it possible to quickly achieve deep remission and correct pathological personality traits that develop against the background of the disease.
After discharge, in order to prevent the development of side effects and correct pharmacotherapy, control examinations are prescribed: in the first month after discharge - 2 times; then - once with an interval of 2-3 months for at least a year. We recommend that you do not neglect the recommendations of the attending physician on taking the prescribed medications and attend follow-up examinations in a timely manner.
Doctor's consultation on the treatment of hebephrenic schizophrenia:
+7 (812) 407-18-00
Thank you for your trust!
- Post-discharge care
- Prevention of relapses
- Anonymous, without registration
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A. V. (associate professor, Ph.D.) V. (associate professor, Ph.D.) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | Is free | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | Is free | |
Signs of hebephrenic schizophrenia
Treatment of hebephrenic schizophrenia in our clinic
Pharmacotherapy is the main treatment for hebephrenic schizophrenia.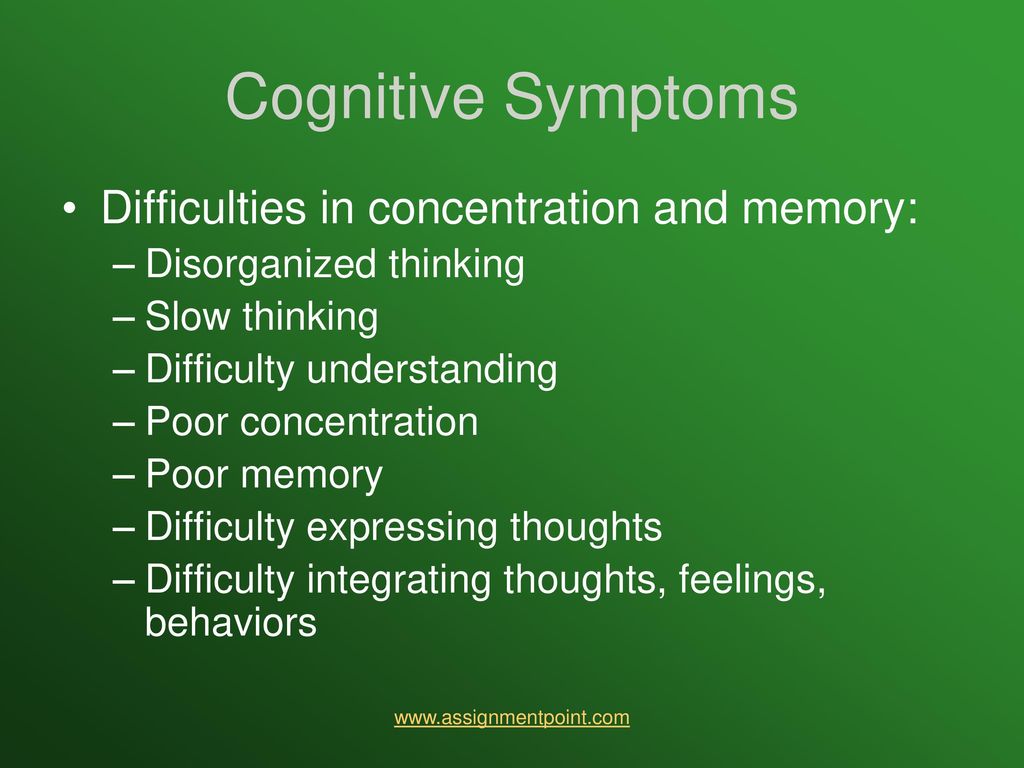 For differential diagnosis, removal of an acute condition and rapid selection of drug therapy, hospitalization is necessary.
For differential diagnosis, removal of an acute condition and rapid selection of drug therapy, hospitalization is necessary.
Differential diagnostics
Differential diagnostics in our clinic includes examination by doctors of narrow specializations (gastroenterologist, cardiologist, neuropsychiatrist), clinical-psychopathological, psychometric and psychological testing, advanced laboratory tests, EEG, MRI and (or) CT.
A differential examination is necessary to confirm the diagnosis and to rule out certain somatic and viral diseases, as well as brain tumors, which can cause symptoms similar to hebephrenic schizophrenia.
Selection of pharmacotherapy
In our clinic, it is possible to quickly select pharmacotherapy through the use of infusion therapy and plasmapheresis (the so-called intensification of the treatment of hebephrenic schizophrenia). Correction of the prescribed treatment with access to psychotherapy requires about 2-3 weeks, after which the patient can be discharged.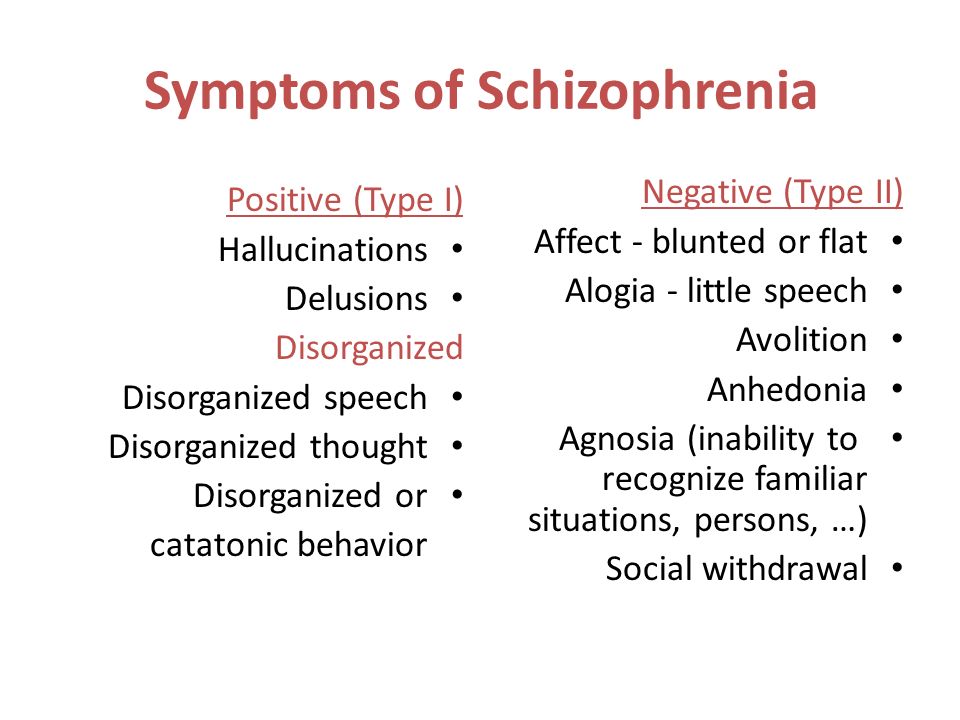
Psychotherapy
All of our patients attend group psychotherapy sessions. Psychotherapy allows you to speed up the process of treatment of hebephrenic schizophrenia and begin to work out addictive attitudes that have formed during the course of the disease (for example, fears, phobias, pathological behaviors).
Post discharge management
Resources
Nursing process/nursing of schizophrenic patients with hebephrenic schizophrenia — https://pubmed.ncbi.nlm.nih.gov
Modern antipsychotic pharmacotherapy of schizophrenia — https://www.rmj.ru
Hebephrenia - a viable psychopathological construct? — https://pubmed.ncbi.nlm.nih.gov
Update date: 11/30/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
December 02
Tomorrow
December 03
Sunday
December 04
Monday
December 05
Tuesday
December 06
Wednesday
December 07
Thursday
December 08
Friday
December 09
Saturday
December 10
Sunday
December 11
Monday
December 12
Tuesday
December 13
Wednesday
December 14
Thursday
December 15
Friday
December 16
Saturday
December 17
Sunday
December 18
Monday
December 19
Tuesday
December 20
Wednesday
December 21
Thursday
December 22
Friday
December 23
Saturday
December 24
Sunday
December 25
Monday
December 26
Tuesday
December 27
Wednesday
December 28
Thursday
December 29
Friday
December 30
Saturday
December 31
Hebephrenic schizophrenia is treated on
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Work experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Work experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Work experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.