Stimulants for ocd
Adderall And ADHD Medicines For OCD
Content
- Overview
- What is Adderall?
- Can ADHD meds help with OCD?
- Do stimulants make OCD worse?
- What about dependence or addiction?
- What is the best medication for OCD?
- The lowdown
Have you considered clinical trials for Obsessive compulsive disorder (OCD)?
We make it easy for you to participate in a clinical trial for Obsessive compulsive disorder (OCD), and get access to the latest treatments not yet widely available - and be a part of finding a cure.
Check your eligibility
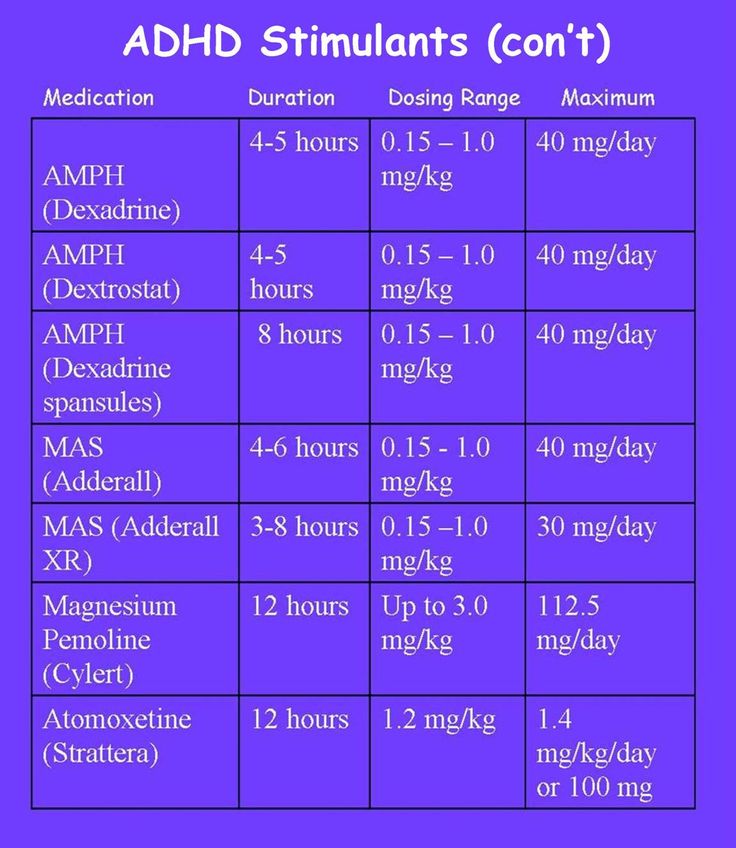
Adderall is a medication that combines amphetamine and dextroamphetamine. Doctors typically prescribe it for ADHD and use it for narcolepsy where necessary. It is a central nervous system stimulant that helps people with ADHD focus better and stays calmer.
It is one of several stimulant-type medications for ADHD. About 62% of children¹ with ADHD take medication, and many adults also use it. However, it can be habit-forming, and it is crucial to take it exactly as prescribed and not overdose.
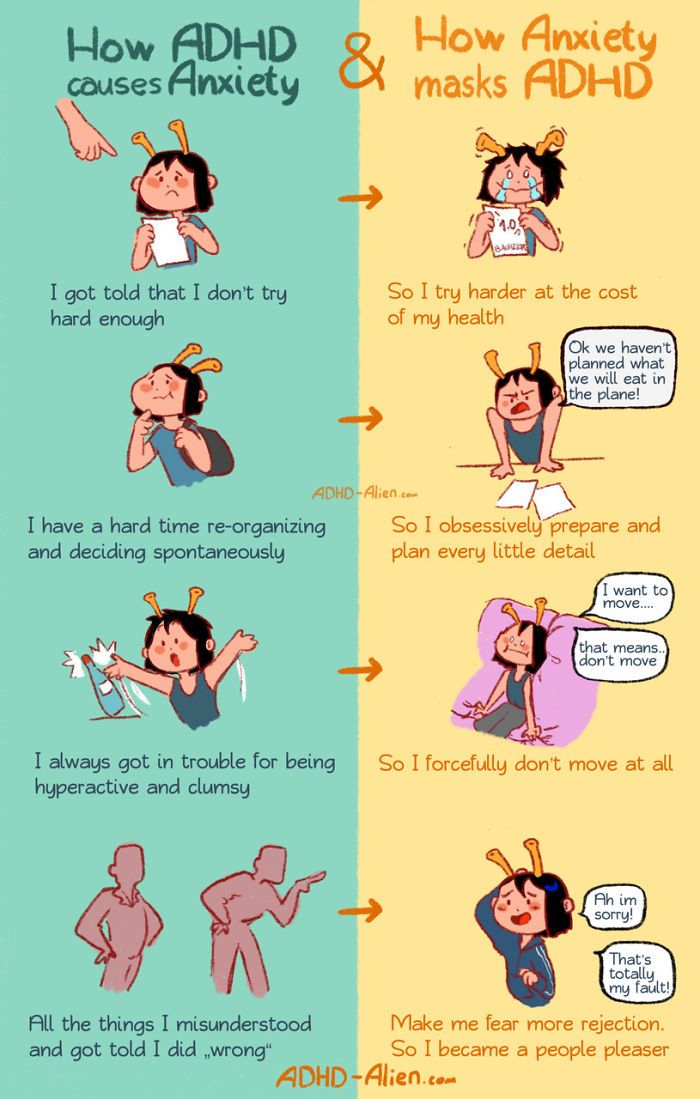
OCD and ADHD are both conditions that affect executive function and show deficits in similar parts of the brain network. So it is reasonable to think that ADHD meds may help OCD symptoms in some cases.
The reality is more complex. First of all, it is possible to have OCD and ADHD² at the same time. This can manifest as impulsivity, making it harder to resist compulsions. Both disorders originate in the frontostriatal-insular-cerebellar regions, which play a role in self-control, foresight, and decision-making.
However, the two conditions have opposing deficits despite possibly being comorbid.
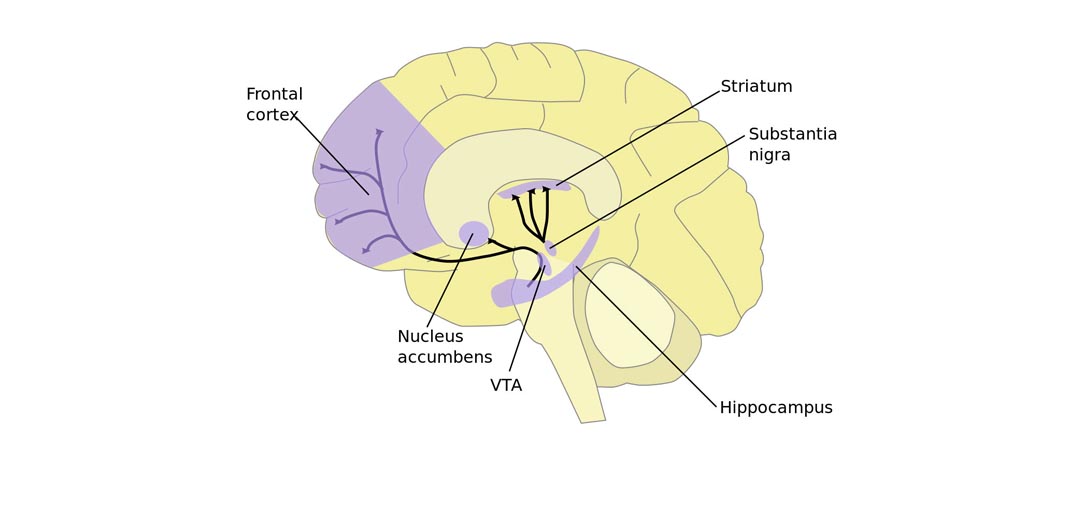
In people with OCD, the frontostriatal region is overactive. Selective serotonin reuptake inhibitors (SSRIs) dampen brain activity. In people with ADHD, the region is underactive, so stimulants increase brain activity in that area.
If you have both conditions, there is evidence that stimulant treatment improves obsessive-compulsive symptoms. It's vital to treat both, as not treating ADHD increases the risk of an OCD relapse. Despite their apparently opposing effects, your doctor may prescribe an SSRI and a stimulant.
It's vital to treat both, as not treating ADHD increases the risk of an OCD relapse. Despite their apparently opposing effects, your doctor may prescribe an SSRI and a stimulant.
However, due to anecdotal evidence that stimulants can make OCD worse and the need to isolate side effects, you will likely try SSRI first.
Some people who appear to have OCD alone also benefit from stimulants, although this might be because they have undiagnosed, milder ADHD.
While extremely rare, stimulants can sometimes cause obsessive-compulsive symptoms. If you show new compulsive behavior after starting ADHD meds, you may need your meds discontinued or changed. It could indicate that the stimulants are overcorrecting the reduced brain activity and pushing you to the other extreme.
While people commonly believe stimulants make OCD symptoms worse, there is no evidence of this.
Another reason to be careful about using ADHD meds for OCD is the risk of dependence. People with OCD are more likely to abuse substances.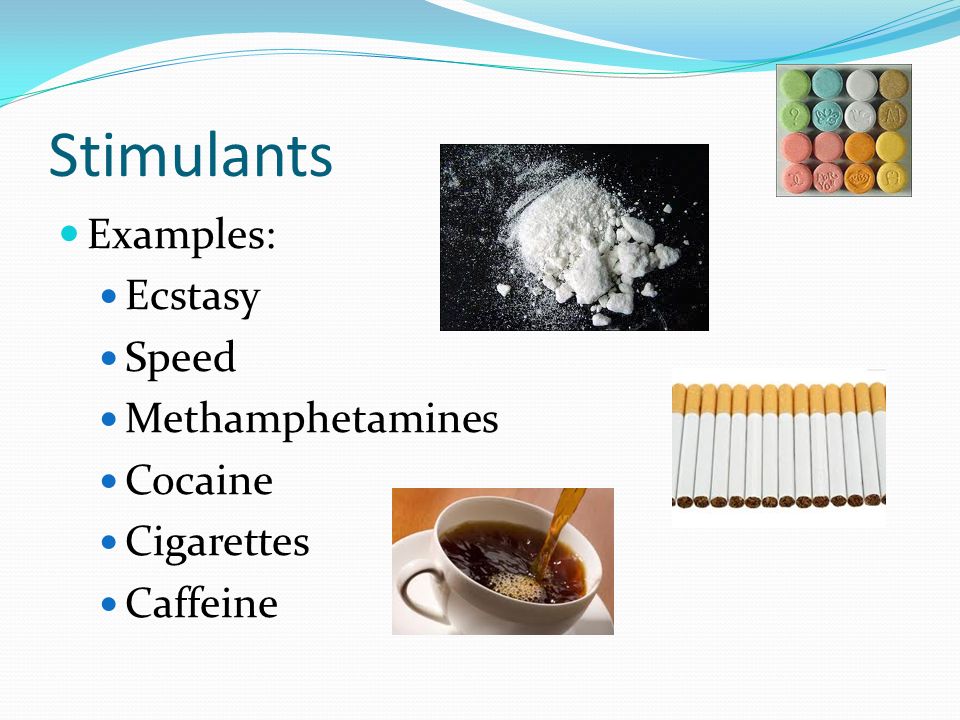 One study³ estimates that 24% of people with OCD have an alcohol use disorder and 18% have a drug use disorder. Rates are 2–6% higher than the general population.
One study³ estimates that 24% of people with OCD have an alcohol use disorder and 18% have a drug use disorder. Rates are 2–6% higher than the general population.
This may result from self-medication, but we need more research in this area. However, people with OCD or OCD and ADHD have to be particularly careful to avoid potential dependence on stimulant medications.
Some people take Adderall or other stimulants as "study aids."⁴ This behavior often leads to mental health problems, unusual conduct, sleep disruption, and cardiovascular side effects. You should not take these drugs unless prescribed by a doctor, as you may have underlying conditions that make stimulants dangerous.
The gold-standard medication for treating OCD remains SSRIs. These medications can relieve symptoms by normalizing activity in the brain. However, they are best in combination with exposure and prevention therapy (ERP), which trains you to stop engaging in compulsions.
Therapy has fewer side effects, and its positive effects last after discontinuing the initial treatment.
Many people with OCD will need to take SSRIs for a while. Some may also need other medication. However, Adderall and other stimulants are typically only necessary when ADHD symptoms are apparent.
Adderall and other stimulant medications are not a first-line treatment for OCD. In some anecdotal cases, they may worsen OCD symptoms. There is also a higher risk of dependency. However, doctors commonly prescribe them for people who have both OCD and ADHD.
You should not attempt to self-medicate with Adderall as it carries some nasty side effects and risks. This includes using it as a study aid.
However, there is evidence that it may be helpful for some people with OCD, especially if standard treatments are not working well. While relatively unusual, some people do find these drugs reduce their symptoms.
Co-Morbid Obsessive–Compulsive Disorder and Attention Deficit Hyperactivity Disorder: Neurobiological Commonalities and Treatment Implications
1. Sheppard B, Chavira D, Azzam A, Grados MA, Umaña P, Garrido H, et al.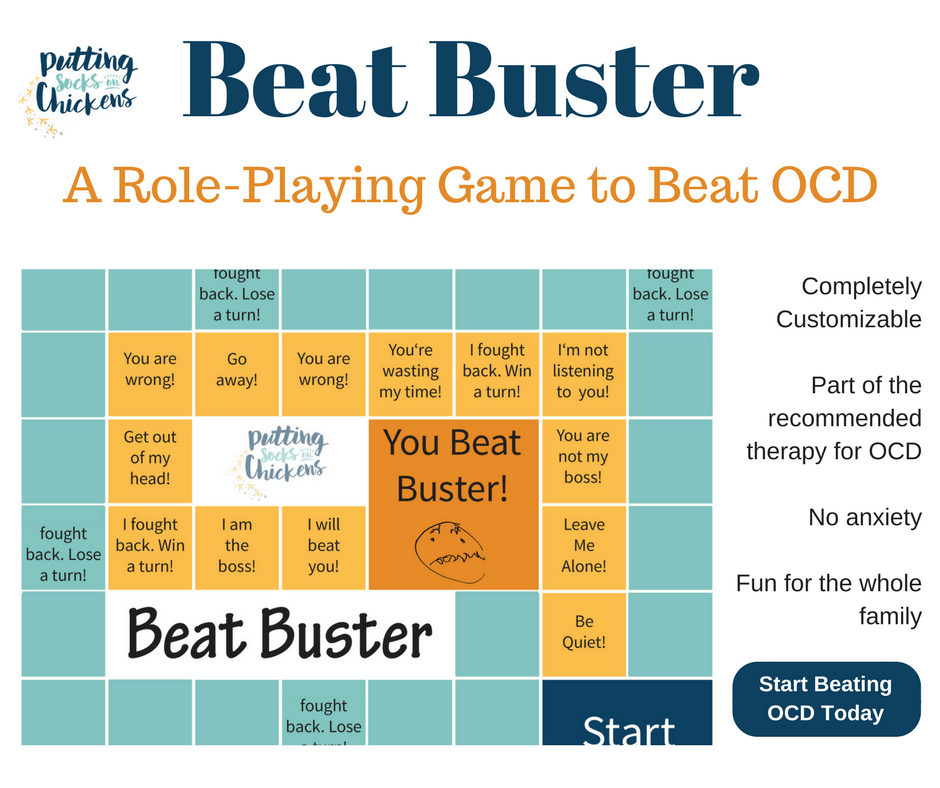 ADHD prevalence and association with hoarding behaviors in childhood-onset OCD. Depress Anxiety (2010) 27(7):667–74. 10.1002/da.20691 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
ADHD prevalence and association with hoarding behaviors in childhood-onset OCD. Depress Anxiety (2010) 27(7):667–74. 10.1002/da.20691 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, et al. A naturalistic exploratory study of the impact of demographic, phenotypic and comorbid features in pediatric obsessive–compulsive disorder. Psychopathology (2010) 43(2):69–78. 10.1159/000274175 [PubMed] [CrossRef] [Google Scholar]
3. Walitza S, Zellmann H, Irblich B, Lange KW, Tucha O, Hemminger U, et al. Children and adolescents with obsessive–compulsive disorder and comorbid attention-deficit/hyperactivity disorder: preliminary results of a prospective follow-up study. J Neural Transm (2008) 115(2):187–90. 10.1007/s00702-007-0841-2 [PubMed] [CrossRef] [Google Scholar]
4. Grados M, Riddle MA. Do all obsessive–compulsive disorder subtypes respond to medication? Int Rev Psychiatry (2008) 20(2):189–93. 10.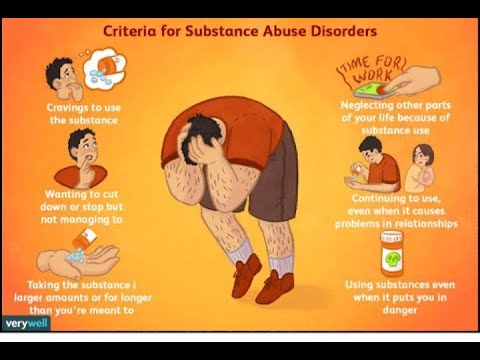 1080/09540260801889153 [PubMed] [CrossRef] [Google Scholar]
1080/09540260801889153 [PubMed] [CrossRef] [Google Scholar]
5. Masi G, Millepiedi S, Mucci M, Bertini N, Pfanner C, Arcangeli F. Comorbidity of obsessive–compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Compr Psychiatry (2006) 47(1):42–7. 10.1016/j.comppsych.2005.04.008 [PubMed] [CrossRef] [Google Scholar]
6. Geller DA, Coffey B, Faraone S, Hagermoser L, Zaman NK, Farrell CL, et al. Does comorbid attention-deficit/hyperactivity disorder impact the clinical expression of pediatric obsessive–compulsive disorder? CNS Spectr (2003) 8(4):259–64. 10.1017/S1092852900018472 [PubMed] [CrossRef] [Google Scholar]
7. Geller DA, Biederman J, Faraone SV, Cradock K, Hagermoser L, Zaman N, et al. Attention-deficit/hyperactivity disorder in children and adolescents with obsessive–compulsive disorder: fact or artifact? J Am Acad Child Adolesc Psychiatry (2002) 41(1):52–8. 10.1097/00004583-200201000-00011 [PubMed] [CrossRef] [Google Scholar]
8. Berlin GS, Hollander E. Compulsivity, impulsivity, and the DSM-5 process. CNS Spectr (2014) 19:62–8. 10.1017/S1092852913000722 [PubMed] [CrossRef] [Google Scholar]
Berlin GS, Hollander E. Compulsivity, impulsivity, and the DSM-5 process. CNS Spectr (2014) 19:62–8. 10.1017/S1092852913000722 [PubMed] [CrossRef] [Google Scholar]
9. Abramovitch A, Dar R, Mittelman A, Wilhelm S. Comorbidity between attention deficit/hyperactivity disorder and obsessive–compulsive disorder across the lifespan: a systematic and critical review. Harv Rev Psychiatry (2015) 23(4):245–62. 10.1097/HRP.0000000000000050 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Rubia K, Cubillo A, Woolley J, Brammer MJ, Smith A. Disorder-specific dysfunctions in patients with attention-deficit/hyperactivity disorder compared to patients with obsessive-compulsive disorder during interference inhibition and attention allocation. Hum Brain Mapp (2011) 32(4):601–11. 10.1002/hbm.21048 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Norman LJ, Carlisi CO, Christakou A, Cubillo A, Murphy CM, Chantiluke K, et al. Shared and disorder-specific task-positive and default mode network dysfunctions during sustained attention in paediatric attention-deficit/hyperactivity disorder and obsessive/compulsive disorder.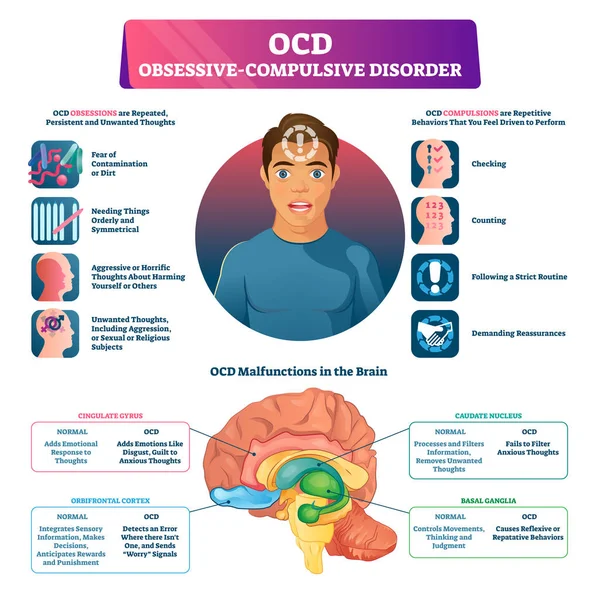 Neuroimage (2017) 15:181–93. 10.1016/j.nicl.2017.04.013 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Neuroimage (2017) 15:181–93. 10.1016/j.nicl.2017.04.013 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
12. Stahl SM, Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. New York, USA: Cambridge University Press; (2013). [Google Scholar]
13. Tripp G, Wickens JR. Neurobiology of ADHD. Neuropharmacology (2009) 57(7–8):579–89. 10.1016/j.neuropharm.2009.07.026 [PubMed] [CrossRef] [Google Scholar]
14. Konrad K, Eickhoff SB. Is the ADHD brain wired differently? A review on structural and functional connectivity in attention deficit hyperactivity disorder. Hum Brain Mapp (2010) 31(6):904–16. 10.1002/hbm.21058 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Norman LJ, Carlisi CO, Christakou A, Chantiluke K, Murphy C, Simmons A, et al. Neural dysfunction during temporal discounting in paediatric attention-deficit/hyperactivity disorder and obsessive–compulsive disorder. Psychiatry Res Neuroimaging (2017) 269:97–105.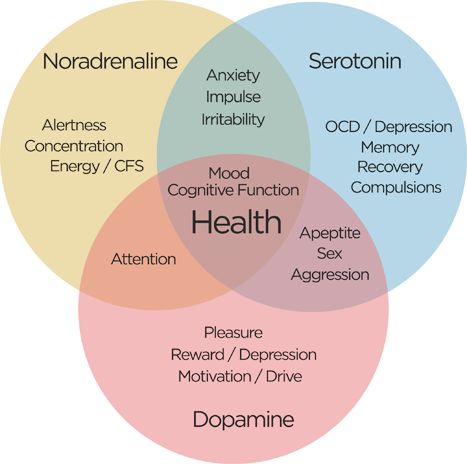 10.1016/j.pscychresns.2017.09.008 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10.1016/j.pscychresns.2017.09.008 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Norman LJ, Carlisi C, Lukito S, Hart H, Mataix-Cols D, Radua J, et al. Structural and functional brain abnormalities in attention-deficit/hyperactivity disorder and obsessive–compulsive disorder: a comparative meta-analysis. JAMA Psychiatry (2016) 73(8):815–25. 10.1001/jamapsychiatry.2016.0700 [PubMed] [CrossRef] [Google Scholar]
17. Zametkin AJ, Liebenauer LL, Fitzgerald GA, King AC, Minkunas DV, Herscovitch P, et al. Brain metabolism in teenagers with attention-deficit hyperactivity disorder. Arch Gen Psychiatry (1993) 50(5):333–40. 10.1001/archpsyc.1993.01820170011002 [PubMed] [CrossRef] [Google Scholar]
18. Zametkin AJ, Nordahl TE, Gross M, King AC, Semple WE, Rumsey J, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med (1990) 323(20):1361–6. 10.1056/NEJM199011153232001 [PubMed] [CrossRef] [Google Scholar]
19. Cubillo A, Halari R, Ecker C, Giampietro V, Taylor E, Rubia K.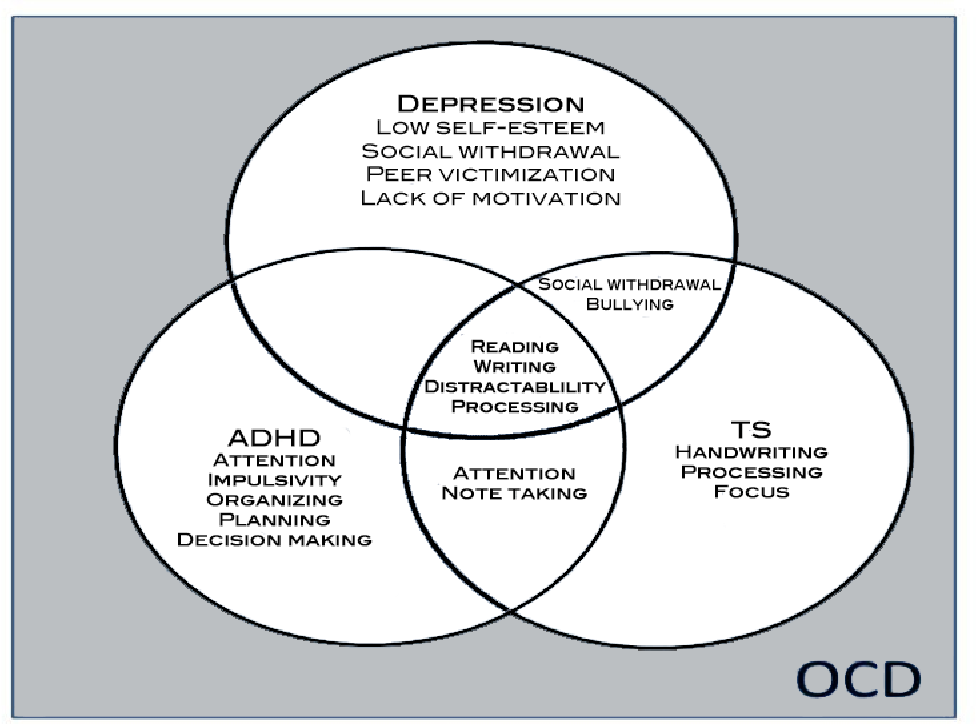 Reduced activation and inter-regional functional connectivity of fronto-striatal networks in adults with childhood attention-deficit hyperactivity disorder (ADHD) and persisting symptoms during tasks of motor inhibition and cognitive switching. J Psychiatr Res (2010) 44(10):629–39. 10.1016/j.jpsychires.2009.11.016 [PubMed] [CrossRef] [Google Scholar]
Reduced activation and inter-regional functional connectivity of fronto-striatal networks in adults with childhood attention-deficit hyperactivity disorder (ADHD) and persisting symptoms during tasks of motor inhibition and cognitive switching. J Psychiatr Res (2010) 44(10):629–39. 10.1016/j.jpsychires.2009.11.016 [PubMed] [CrossRef] [Google Scholar]
20. Wolf RC, Plichta MM, Sambataro F, Fallgatter AJ, Jacob C, Lesch KP, et al. Regional brain activation changes and abnormal functional connectivity of the ventrolateral prefrontal cortex during working memory processing in adults with attention-deficit/hyperactivity disorder. Hum Brain Mapp (2009) 30(7):2252–66. 10.1002/hbm.20665 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
21. Pujol J, Soriano-Mas C, Alonso P, Cardoner N, Menchon JM, Deus J, et al. Mapping structural brain alterations in obsessive–compulsive disorder. Arch Gen Psychiatry (2004) 61(7):720–30. 10.1001/archpsyc.61.7.720 [PubMed] [CrossRef] [Google Scholar]
22. Lacerda AL, Dalgalarrondo P, Caetano D, Haas GL, Camargo EE, Keshavan MS. Neuropsychological performance and regional cerebral blood flow in obsessive–compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry (2003) 27(4):657–65. 10.1016/S0278-5846(03)00076-9 [PubMed] [CrossRef] [Google Scholar]
Lacerda AL, Dalgalarrondo P, Caetano D, Haas GL, Camargo EE, Keshavan MS. Neuropsychological performance and regional cerebral blood flow in obsessive–compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry (2003) 27(4):657–65. 10.1016/S0278-5846(03)00076-9 [PubMed] [CrossRef] [Google Scholar]
23. Maltby N, Tolin DF, Worhunsky P, O’Keefe TM, Kiehl KA. Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive–compulsive disorder: an event-related fMRI study. Neuroimage (2005) 24(2):495–503. 10.1016/j.neuroimage.2004.08.041 [PubMed] [CrossRef] [Google Scholar]
24. Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive–compulsive disorder. Arch Gen Psychiatry (2004) 61(6):564–76. 10.1001/archpsyc.61.6.564 [PubMed] [CrossRef] [Google Scholar]
25. Abramovitch A, Dar R, Hermesh H, Schweiger A. Comparative neuropsychology of adult obsessive–compulsive disorder and attention deficit/hyperactivity disorder: implications for a novel executive overload model of OCD. J Neuropsychol (2012) 6(2):161–91. 10.1111/j.1748-6653.2011.02021.x [PubMed] [CrossRef] [Google Scholar]
J Neuropsychol (2012) 6(2):161–91. 10.1111/j.1748-6653.2011.02021.x [PubMed] [CrossRef] [Google Scholar]
26. Norman LJ, Carlisi CO, Christakou A, Murphy CM, Chantiluke K, Giampietro V, et al. Frontostriatal Dysfunction During Decision Making in Attention-Deficit/Hyperactivity Disorder and Obsessive–Compulsive Disorder. Biol Psychiatry Cogn Neurosci Neuroimaging (2018) 3(8):694–703. 10.1016/j.bpsc.2018.03.009 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
27. Fineberg NA, Reghunandanan S, Brown A, Pampaloni I. Pharmacotherapy of obsessive–compulsive disorder: evidence-based treatment and beyond. Aust N Z J Psychiatry (2012) 47(2):121–41. 10.1177/0004867412461958 [PubMed] [CrossRef] [Google Scholar]
28. Bandelow B, Zohar J, Hollander E, Kasper S, Moller HJ, Zohar J, et al. World federation of societies of biological psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive–compulsive and post-traumatic stress disorders - first revision. World J Biol Psychiatry (2008) 9(4):248–312. 10.1080/15622970802465807 [PubMed] [CrossRef] [Google Scholar]
World J Biol Psychiatry (2008) 9(4):248–312. 10.1080/15622970802465807 [PubMed] [CrossRef] [Google Scholar]
29. Pittenger C, Kelmendi B, Bloch M, Krystal JH, Coric V. Clinical treatment of obsessive compulsive disorder. Psychiatry (Edgmont) (2005) 2(11):34–43. [PMC free article] [PubMed] [Google Scholar]
30. Keuneman RJ, Pokos V, Weerasundera R, Castle DJ. Antipsychotic treatment in obsessive–compulsive disorder: a literature review. Aust N Z J Psychiatry (2005) 39(5):336–43. 10.1080/j.1440-1614.2005.01591.x [PubMed] [CrossRef] [Google Scholar]
31. Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA (2016) 315(18):1997–2008. 10.1001/jama.2016.5453 [PubMed] [CrossRef] [Google Scholar]
32. Jensen CM, Amdisen BL, Jørgensen KJ, Arnfred SM. Cognitive behavioural therapy for ADHD in adults: systematic review and meta-analyses. Atten Defic Hyperact Disord (2016) 8(1):3–11. 10.1007/s12402-016-0188-3 [PubMed] [CrossRef] [Google Scholar]
33. Koizumi HM. Obsessive–compulsive symptoms following stimulants. Biol Psychiatry (1985) 20(12):1332–3. 10.1016/0006-3223(85)90120-9 [PubMed] [CrossRef] [Google Scholar]
Koizumi HM. Obsessive–compulsive symptoms following stimulants. Biol Psychiatry (1985) 20(12):1332–3. 10.1016/0006-3223(85)90120-9 [PubMed] [CrossRef] [Google Scholar]
34. Kouris S. Methylphenidate-induced obsessive–compulsiveness. J Am Acad Child Adolesc Psychiatry (1998) 37(2):135. 10.1097/00004583-199802000-00001 [PubMed] [CrossRef] [Google Scholar]
35. Serby M. Methylphenidate-induced obsessive–compulsive symptoms in an elderly man. CNS Spectr (2003) 8(8):612–3. 10.1017/S1092852900018885 [PubMed] [CrossRef] [Google Scholar]
36. Woolley JB, Heyman I. Dexamphetamine for obsessive–compulsive disorder. Am J Psychiatry (2003) 160(1):183. 10.1176/appi.ajp.160.1.183 [PubMed] [CrossRef] [Google Scholar]
37. Jhanda S, Singla N, Grover S. Methylphenidate-induced obsessive–compulsive symptoms: a case report and review of literature. J Pediatr Neurosci (2016) 11(4):316–8. 10.4103/1817-1745.199461 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Guzick AG, McNamara JPH, Reid AM, Balkhi AM, Storch EA, Murphy TK, et al. The link between ADHD-like inattention and obsessions and compulsions during treatment of youth with OCD. J Obsessive Compuls Relat Disord (2017) 12:1–8. 10.1016/j.jocrd.2016.11.004 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Guzick AG, McNamara JPH, Reid AM, Balkhi AM, Storch EA, Murphy TK, et al. The link between ADHD-like inattention and obsessions and compulsions during treatment of youth with OCD. J Obsessive Compuls Relat Disord (2017) 12:1–8. 10.1016/j.jocrd.2016.11.004 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
39. Hall D, Dhilla A, Charalambous A, Gogos JA, Karayiorgou M. Sequence variants of the brain-derived neurotrophic factor (BDNF) gene are strongly associated with obsessive–compulsive disorder. Am J Hum Genet (2003) 73(2):370–6. 10.1086/377003 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Cunha C, Brambilla R, Thomas KL. A simple role for BDNF in learning and memory? Front Mol Neurosci (2010) 3:1. 10.3389/neuro.02.001.2010 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Björkholm C, Monteggia LM. BDNF — a key transducer of antidepressant effects. Neuropharmacology (2015) 102:72–9. 10.1016/j.neuropharm.2015.10.034 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, et al. Pharmacotherapy in paediatric obsessive–compulsive disorder: a naturalistic, retrospective study. CNS Drugs (2009) 23(3):241–52. 10.2165/00023210-200923030-00005 [PubMed] [CrossRef] [Google Scholar]
Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, et al. Pharmacotherapy in paediatric obsessive–compulsive disorder: a naturalistic, retrospective study. CNS Drugs (2009) 23(3):241–52. 10.2165/00023210-200923030-00005 [PubMed] [CrossRef] [Google Scholar]
43. King J, Dowling N, Leow F. Methylphenidate in the treatment of an adolescent female with obsessive–compulsive disorder and attention deficit hyperactivity disorder: a case report. Australas Psychiatry (2016) 25(2):178–80. 10.1177/1039856216671664 [PubMed] [CrossRef] [Google Scholar]
44. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL. The Yale-Brown obsessive compulsive scale. I. development, use, and reliability. Arch Gen Psychiatry (1989) 46(11):1006–11. 10.1001/archpsyc.1989.01810110048007 [PubMed] [CrossRef] [Google Scholar]
45. Ramsay JR. Assessment and monitoring of treatment response in adult ADHD patients: current perspectives. Neuropsychiatr Dis Treat (2017) 13:221–32.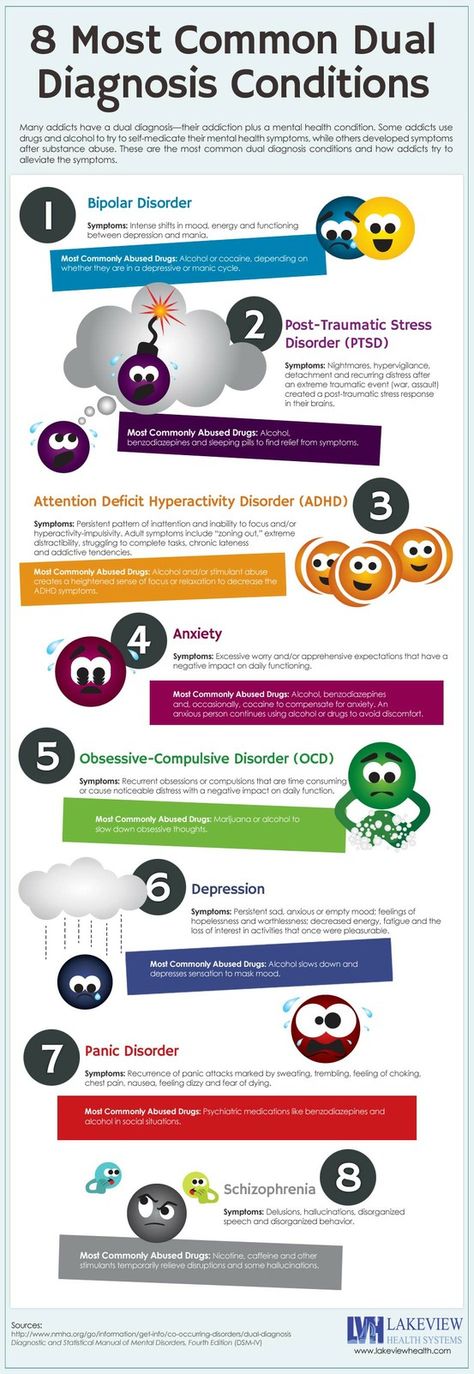 10.2147/NDT.S104706 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10.2147/NDT.S104706 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
46. Rubio B, Boes AD, Laganiere S, Rotenberg A, Jeurissen D, Pascual-Leone A. Noninvasive brain stimulation in pediatric attention-deficit hyperactivity disorder (ADHD): a review. J Child Neurol (2015) 31(6):784–96. 10.1177/0883073815615672 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Rubia K. Cognitive neuroscience of attention deficit hyperactivity disorder (ADHD) and its clinical translation. Front Hum Neurosci (2018) 12:100. 10.3389/fnhum.2018.00100 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
48. Paz Y, Friedwald K, Levkovitz Y, Zangen A, Alyagon U, Nitzan U, et al. Deep rTMS for ADHD. Brain Stimul (2017) 10(2):413. 10.1016/j.brs.2017.01.224 [CrossRef] [Google Scholar]
49. Cocchi L, Zalesky A, Nott Z, Whybird G, Fitzgerald PB, Breakspear M. Transcranial magnetic stimulation in obsessive–compulsive disorder: a focus on network mechanisms and state dependence.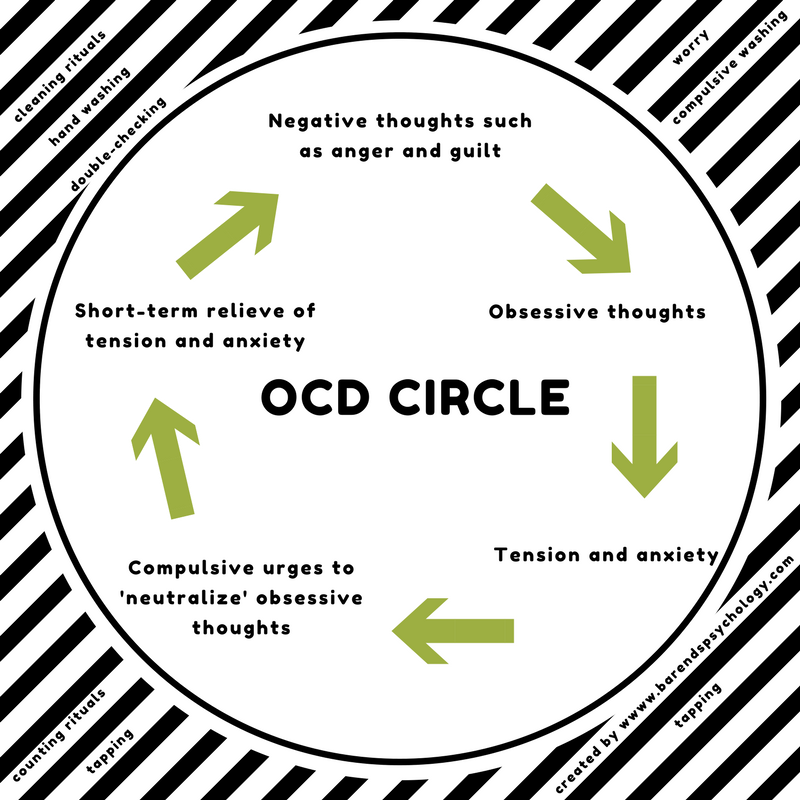 Neuroimage Clin (2018) 19:661–74. 10.1016/j.nicl.2018.05.029 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Neuroimage Clin (2018) 19:661–74. 10.1016/j.nicl.2018.05.029 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
50. Carmi L, Alyagon U, Barnea-Ygael N, Zohar J, Dar R, Zangen A. Clinical and electrophysiological outcomes of deep TMS over the medial prefrontal and anterior cingulate cortices in OCD patients. Brain Stimul (2018) 11(1):158–65. 10.1016/j.brs.2017.09.004 [PubMed] [CrossRef] [Google Scholar]
51. Dowling N, Thomas N, Blair-West S, Bousman C, Yap K, Smith DJ, et al. Intensive residential treatment for obsessive–compulsive disorder: outcomes and predictors of patient adherence to cognitive-behavioural therapy. J Obsessive Compuls Relat Disord (2016) 9:82–9. 10.1016/j.jocrd.2016.04.006 [CrossRef] [Google Scholar]
52. Taurines R, Schmitt J, Renner T, Conner AC, Warnke A, Romanos M. Developmental comorbidity in attention-deficit/hyperactivity disorder. Defic Hyperact Disord (2010) 2(4):267–89. 10.1007/s12402-010-0040-0 [PubMed] [CrossRef] [Google Scholar]
Not Found (#404)
hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
- nine0009
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.
 A. Kramar
A. Kramar -
Screening, diagnosis and treatment of diabetic sensorimotor polyneuropathy: consensus recommendations
-
Influx of mass information on delinquent behavior
R. І. Isakov
-
Stopping programs for rukhovo's rehabilitation for the normalization of the psychoemotional sphere of patients with Parkinson's disease
N.P. Voloshin, I.V. Bogdanova, I.K. Voloshin-Gaponov, S.V. Fedosiev, L.P. Tereshchenko, T.V. Bogdanova
-
Trauma management algorithm
-
Type of neuropathic pain according to the International classification of orofacial pain
-
Management of patients with dementia: key provisions for diagnosis, examination and observation for example of life
-
Significant Pre-Raphaelism: John Ruskin and Effi Gray
5-6 (135)
3-4 (134)
2 (133)
1 (132)
Other projects of the Health of Ukraine publishing house
Specialization medical portal
nine0009 Child doctorMedical aspects of women's health
Clinical Immunology, Allergology, Infectology
Rational pharmacotherapy
nine0000 Not Found (#404)hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
- nine0009
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.