Statistics on agoraphobia
Agoraphobia - StatPearls - NCBI Bookshelf
Continuing Education Activity
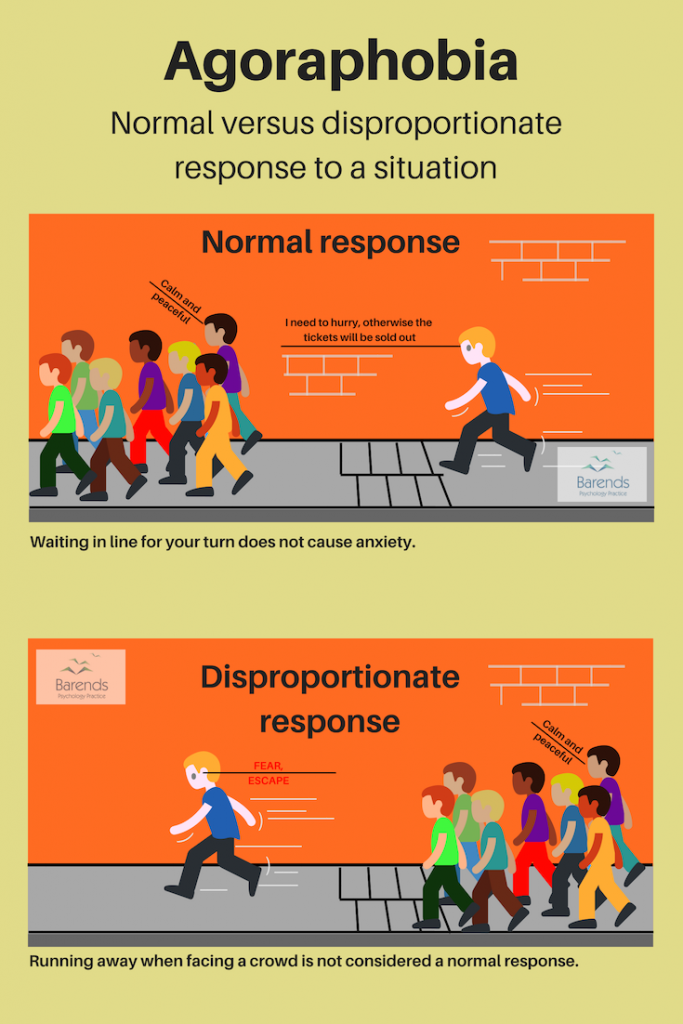
Agoraphobia is the anxiety that occurs when one is in a public or crowded place, from which a potential escape is difficult, or help may not be readily available. It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations. This activity describes the diagnostic criteria and characteristics of agoraphobia and outlines the interprofessional team's role in its evaluation and management.
Objectives:
Identify the etiology of agoraphobia.
Review the diagnostic criteria/common symptomatic presentations of agoraphobia.
Outline the options available for the management of agoraphobia.
Describe some interprofessional team strategies for improving care coordination and communication for the evaluation and management of agoraphobia.
Access free multiple choice questions on this topic.
Introduction
Agoraphobia is the anxiety that occurs when one is in a public or crowded place, from which a potential escape is difficult, or help may not be readily available. It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations.[1]
In the DSM-IV, agoraphobia was not a formal psychiatric diagnosis but was instead considered a qualifier of panic disorder. Panic disorder is characterized by recurrent or unexpected panic attacks, presenting as abrupt and intense surges of fear with various associated physical symptoms such as palpitations, shortness of breath, nausea, chest pain, dizziness, fear of dying, etc. In the currently-used DSM-5, agoraphobia is considered a distinct diagnosis that can occur independently of other diagnoses, such as generalized anxiety disorder or panic disorder. In the DSM-5, the condition is defined as “marked fear or anxiety about actual or anticipated exposure of public spaces, with the symptoms of fear or anxiety occurring most of the time in at least two of five common, different situations.” To meet the criteria for the diagnosis, an individual must both fear the exposure to public places and must also make active attempts to avoid such situations, either through behavioral or cognitive modifications. This fear or anxiety should not be in the context of a realistic threat, explained by sociocultural context, or occur in the context of substance use or withdrawal.[2] To formally diagnose a patient with agoraphobia, the diagnostic criteria must be present for greater than six months.
In the DSM-5, the condition is defined as “marked fear or anxiety about actual or anticipated exposure of public spaces, with the symptoms of fear or anxiety occurring most of the time in at least two of five common, different situations.” To meet the criteria for the diagnosis, an individual must both fear the exposure to public places and must also make active attempts to avoid such situations, either through behavioral or cognitive modifications. This fear or anxiety should not be in the context of a realistic threat, explained by sociocultural context, or occur in the context of substance use or withdrawal.[2] To formally diagnose a patient with agoraphobia, the diagnostic criteria must be present for greater than six months.
Etiology
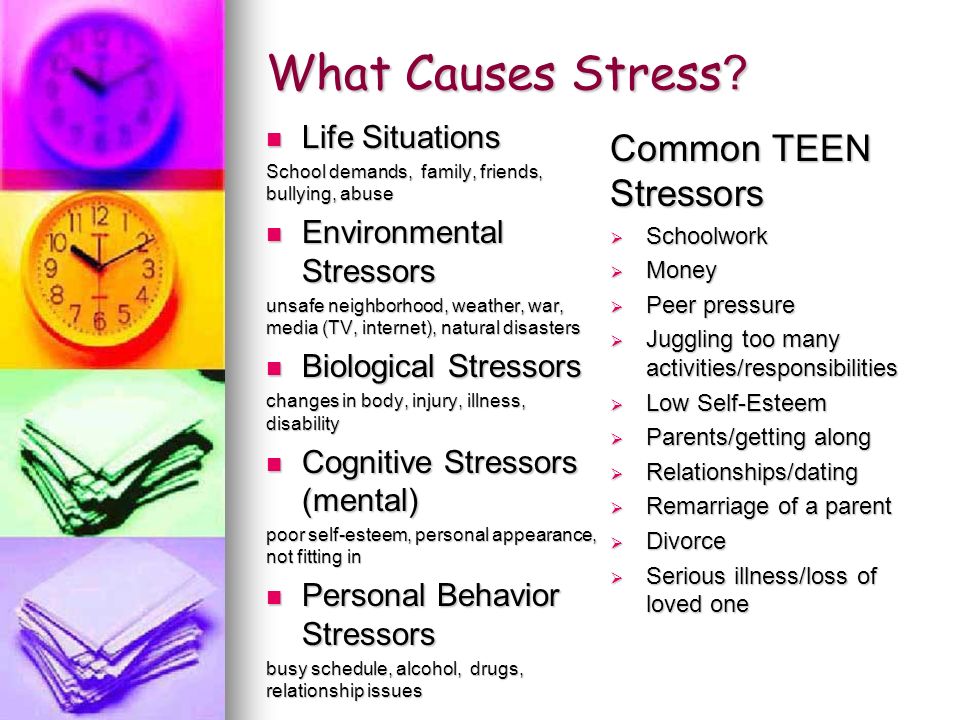
Agoraphobia is usually first identified in young adults, with the mean age of diagnosis beginning in the mid to late twenties. There is no consensus on the childhood experiences, personality characteristics, or psychosocial risk factors that lead to a diagnosis of agoraphobia. However, proposals point to several commonly occurring etiological factors. These include parental overprotectiveness, the presence of childhood fears or night terrors, experience of grief or bereavement early in life, unhappy or traumatic childhoods, or genetic predisposition. Comorbid personality types include dependent, obsessive-compulsive, or otherwise “highly-neurotic.”[3]
However, proposals point to several commonly occurring etiological factors. These include parental overprotectiveness, the presence of childhood fears or night terrors, experience of grief or bereavement early in life, unhappy or traumatic childhoods, or genetic predisposition. Comorbid personality types include dependent, obsessive-compulsive, or otherwise “highly-neurotic.”[3]
The DSM-5 further stratifies risk factors into three categories: temperamental (neuroticism, sensitivity to anxiety, and anxiety disorders), environmental (negative or traumatic events in childhood, and reduced warmth or overprotectiveness in childhood), and genetic and physiological predisposition.
Epidemiology
Anxiety disorders, encompassing generalized anxiety disorder, panic disorder, and agoraphobia, are highly prevalent in the general population.[1] There is some disparity in estimates for the prevalence of agoraphobia as it has only recently received its own diagnostic criteria rather than as a qualifier for panic disorder. According to the DSM-5, agoraphobia is present in approximately 1.7% of the general population. It further states that most cases of agoraphobia present before the age of 35. There is an increase in the risk of developing agoraphobia in late adolescence and early adulthood, with the overall average age at onset being 17 years. The National Institute of Mental Health estimates that the lifetime prevalence of agoraphobia is 1.3%, with an annual incidence rate of 0.9%. Yearly prevalence rates of agoraphobia are similar between males (0.8%) and females (0.9%).
According to the DSM-5, agoraphobia is present in approximately 1.7% of the general population. It further states that most cases of agoraphobia present before the age of 35. There is an increase in the risk of developing agoraphobia in late adolescence and early adulthood, with the overall average age at onset being 17 years. The National Institute of Mental Health estimates that the lifetime prevalence of agoraphobia is 1.3%, with an annual incidence rate of 0.9%. Yearly prevalence rates of agoraphobia are similar between males (0.8%) and females (0.9%).
History and Physical
As with all psychiatric diagnoses, an essential tool in diagnosis is the interview. There is no physical exam finding that would indicate a diagnosis of agoraphobia.
Evaluation
The DSM-5 outlines the criteria by which a diagnosis of agoraphobia is possible.[2] To definitively diagnose a patient with agoraphobia, they must have intense fear in response to or when anticipating entering into at least two of the five following situations: using public transportation (automobiles, buses, trains), being in open spaces (marketplaces, parking lots), being in enclosed spaces like theaters or malls, standing in lines or crowds, or being outside of the home alone.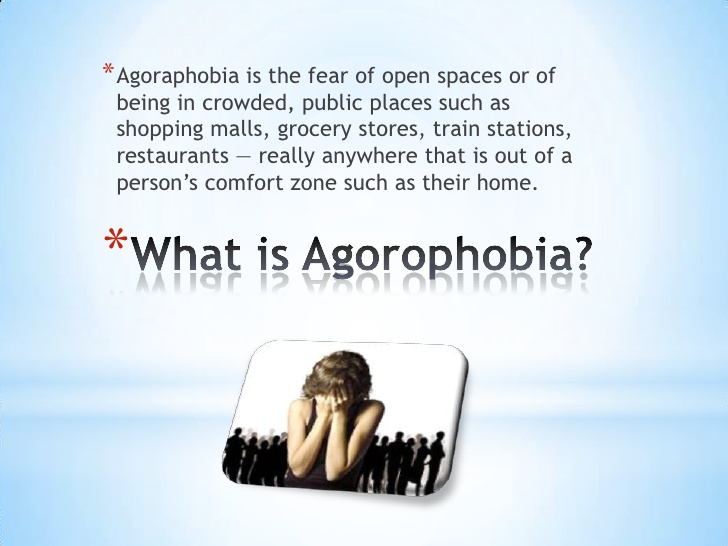 This fear, which is out of proportion to the actual stimulus, must be accompanied by behavioral or cognitive modifications to avoid placing oneself in situations where the exposure may occur. These symptoms must be present for at least six months and must cause significant distress to the patient and impairment in their lives. The symptoms also should not be better explained by another psychiatric diagnosis, be directly caused by a medical diagnosis, or occur in the context of substance use or withdrawal.
This fear, which is out of proportion to the actual stimulus, must be accompanied by behavioral or cognitive modifications to avoid placing oneself in situations where the exposure may occur. These symptoms must be present for at least six months and must cause significant distress to the patient and impairment in their lives. The symptoms also should not be better explained by another psychiatric diagnosis, be directly caused by a medical diagnosis, or occur in the context of substance use or withdrawal.
Treatment / Management
Though panic disorder and agoraphobia have been differentiated, with two different sets of diagnostic criteria, the treatment algorithms for the two remain similar. The first step is to identify the severity of the disease when the patient presents; this is often a measure of the level of impairment or distress the agoraphobia or panic disorder causes in the patient’s life.
Patients with mild or moderate panic disorder or agoraphobia can choose between psychotherapy and pharmacotherapy to achieve adequate symptom management. Studies have generally concluded that cognitive-behavioral therapy (CBT) effectively addresses and alleviates target symptoms, lessens other anxiety symptoms, and improves the patient's quality of life.[4] For patients with more severe forms of agoraphobia or for those who prefer pharmacotherapy over psychotherapy, there are several effective options for medication management. Selective serotonin receptor inhibitors (SSRIs) are generally considered first-line therapy, with therapeutic doses being the same as in depression.[5] Serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and benzodiazepines have also been effective alternatives SSRIs in the treatment of panic disorder and agoraphobia.[6][7] SSRIs are generally preferable to these other medications because of the side effect profile, affordability, availability, decreased potential for abuse, and better tolerability.[8][9][10] There is also data suggesting that the combination of CBT with pharmacotherapy may be most effective in the symptomatic management of agoraphobia and panic disorder.
Studies have generally concluded that cognitive-behavioral therapy (CBT) effectively addresses and alleviates target symptoms, lessens other anxiety symptoms, and improves the patient's quality of life.[4] For patients with more severe forms of agoraphobia or for those who prefer pharmacotherapy over psychotherapy, there are several effective options for medication management. Selective serotonin receptor inhibitors (SSRIs) are generally considered first-line therapy, with therapeutic doses being the same as in depression.[5] Serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and benzodiazepines have also been effective alternatives SSRIs in the treatment of panic disorder and agoraphobia.[6][7] SSRIs are generally preferable to these other medications because of the side effect profile, affordability, availability, decreased potential for abuse, and better tolerability.[8][9][10] There is also data suggesting that the combination of CBT with pharmacotherapy may be most effective in the symptomatic management of agoraphobia and panic disorder.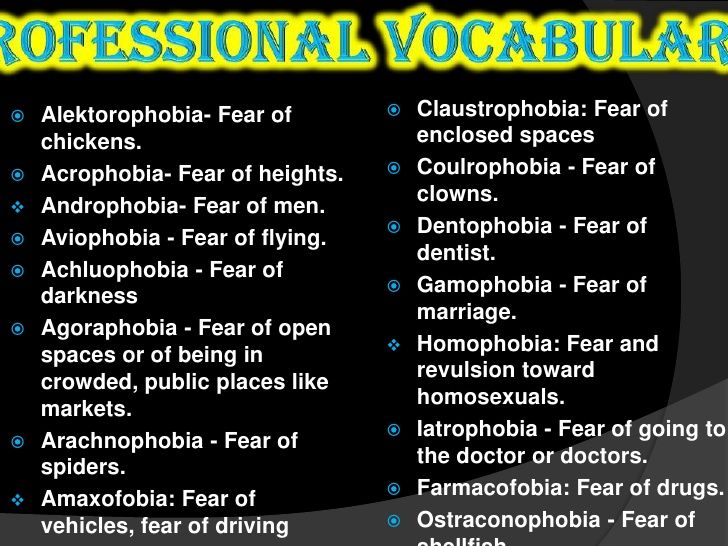 [11]
[11]
Differential Diagnosis
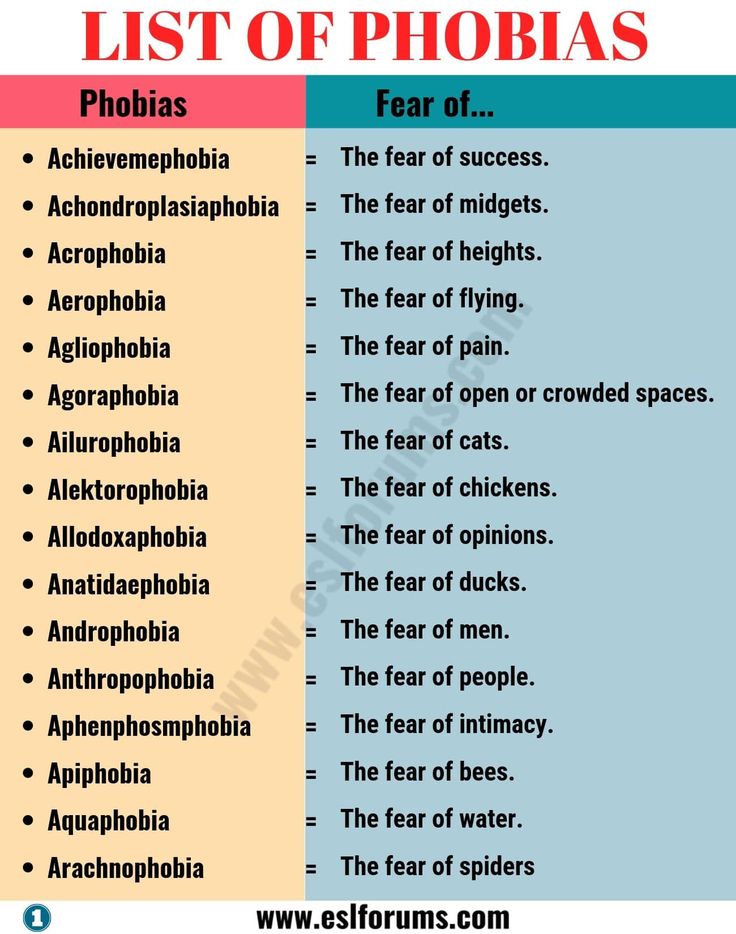
According to the DSM-5, the most common differential diagnoses for agoraphobia include specific phobia, separation anxiety disorder, social anxiety disorder, panic disorder, acute stress disorder or posttraumatic stress disorder, and major depressive disorder. Specific phobia should be diagnosed, rather than agoraphobia, if the fear, anxiety, avoidance, or behavioral modification is limited to one of the five, rather than two, of the situations in which agoraphobia can occur. Separation anxiety disorder can be differentiated from agoraphobia if the fear or anxiety arises when considering detachment from loved ones or the home environment, rather than the panic associated with being in the feared situations themselves.
Social anxiety involves fear about being negatively judged in public situations rather than, like separation anxiety disorder, being in the situations themselves. Panic disorder is the appropriate diagnosis if the panic symptoms occur in less than two of the five diagnostic agoraphobic conditions or if they occur in other non-public situations or circumstances. Acute stress disorder or posttraumatic stress disorder is the diagnosis if the fear, anxiety, or avoidance functions to avoid reminding the individual of a past traumatic event. Major depressive disorder should be the diagnosis if the patient also reports associated anhedonia, apathy, loss of energy, insomnia, or low self-esteem. Agoraphobia also cannot be diagnosed if the behavioral modifications are to avoid consequences of medical conditions, such as fears of losing consciousness in public for someone with cardiovascular pathology or developing diarrhea in someone with inflammatory bowel disease.
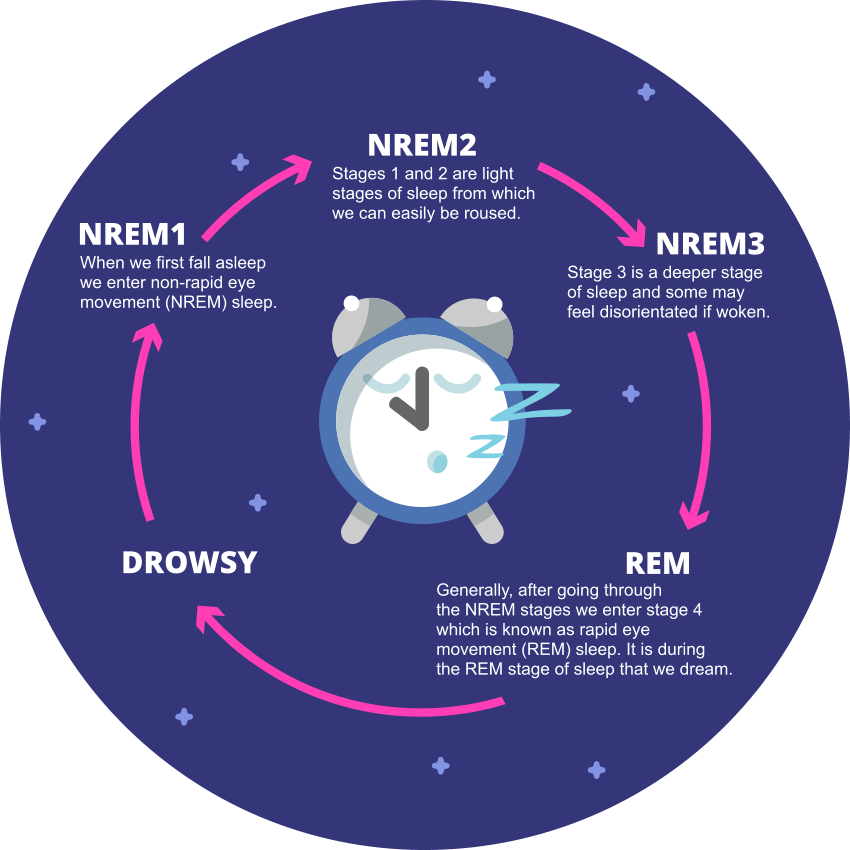
Acute stress disorder or posttraumatic stress disorder is the diagnosis if the fear, anxiety, or avoidance functions to avoid reminding the individual of a past traumatic event. Major depressive disorder should be the diagnosis if the patient also reports associated anhedonia, apathy, loss of energy, insomnia, or low self-esteem. Agoraphobia also cannot be diagnosed if the behavioral modifications are to avoid consequences of medical conditions, such as fears of losing consciousness in public for someone with cardiovascular pathology or developing diarrhea in someone with inflammatory bowel disease.
Prognosis
The DSM-5 describes the course of agoraphobia as “persistent and chronic,” with complete remission being relatively rare except with treatment or intervention.[12] Rates of remission are reduced when the severity of agoraphobia is higher. The chance of a favorable prognosis is also reduced by the presence of comorbid anxiety disorders, depression, personality disorders, or substance use disorders.
Complications
Agoraphobia itself is associated with significant distress and impairment in life. In severe cases, it can cause individuals to become completely home-bound and dependent on others for anything that requires leaving one’s home. This can lead to self-medication with non-prescription medications or other substances. The DSM-5 states that remission rates without treatment are quite low, with averages estimated at about 10%.
Agoraphobia is also associated with an increased risk of developing comorbid major depressive disorder, persistent depressive disorder (dysthymia), and substance use disorders.
Deterrence and Patient Education
The prevention of agoraphobia would involve the mediation of significant risk factors. Appropriate strategies for its management include early identification of symptoms, prompt intervention, access to resources and mental health professionals, facilitation of open discussions with patients, and effective management with psychotherapy or pharmacotherapy.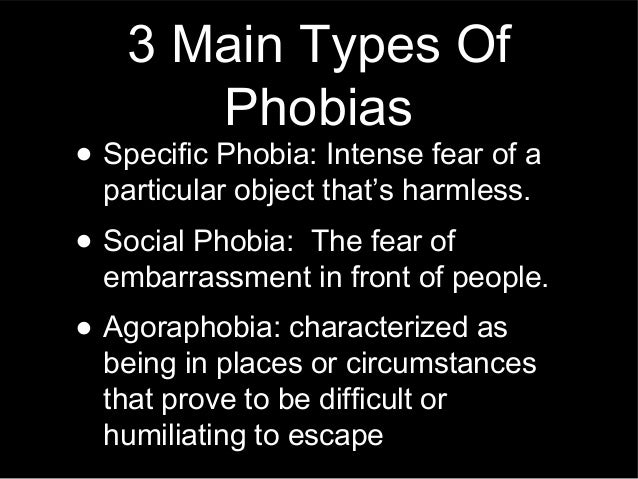
Enhancing Healthcare Team Outcomes
Agoraphobia, while only recently differentiated from panic disorder with its diagnostic criteria, is extremely prevalent in the general population. When present, it causes significant distress and potential disability in an individual’s life. Due to its “persistent and chronic” course, if left untreated, it is essential that agoraphobia is diagnosed early and intervention initiated promptly. It is critical that healthcare professionals, particularly primary care providers, be well-versed in the symptomatology of agoraphobia and proficient in diagnosing and starting any necessary treatment. Patients must have a connection to avenues to obtain adequate resources for their distress and disability, and referrals to psychology and psychiatry should take place if deemed necessary. Treatment can involve psychologists, social workers, psychiatric nurses, and nurse practitioners. They all participate in patient education and monitor patients. Nursing staff can assess compliance, answer patient questions, and watch for adverse effects from medication, alerting the prescriber promptly of any concerns. Pharmacists review prescriptions, check for interactions and inform patients about side effects. They can also provide input on which agents are best to use for a specific patient and therapy modifications if progress stalls. These interprofessional interventions can improve patient outcomes for agoraphobia patients. [Level 5]
Pharmacists review prescriptions, check for interactions and inform patients about side effects. They can also provide input on which agents are best to use for a specific patient and therapy modifications if progress stalls. These interprofessional interventions can improve patient outcomes for agoraphobia patients. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Roest AM, de Vries YA, Lim CCW, Wittchen HU, Stein DJ, Adamowski T, Al-Hamzawi A, Bromet EJ, Viana MC, de Girolamo G, Demyttenaere K, Florescu S, Gureje O, Haro JM, Hu C, Karam EG, Caldas-de-Almeida JM, Kawakami N, Lépine JP, Levinson D, Medina-Mora ME, Navarro-Mateu F, O'Neill S, Piazza M, Posada-Villa JA, Slade T, Torres Y, Kessler RC, Scott KM, de Jonge P., WHO World Mental Health Survey Collaborators. A comparison of DSM-5 and DSM-IV agoraphobia in the World Mental Health Surveys.
 Depress Anxiety. 2019 Jun;36(6):499-510. [PMC free article: PMC6548607] [PubMed: 30726581]
Depress Anxiety. 2019 Jun;36(6):499-510. [PMC free article: PMC6548607] [PubMed: 30726581]- 2.
Asmundson GJ, Taylor S, Smits JA. Panic disorder and agoraphobia: an overview and commentary on DSM-5 changes. Depress Anxiety. 2014 Jun;31(6):480-6. [PubMed: 24865357]
- 3.
Tearnan BH, Telch MJ, Keefe P. Etiology and onset of agoraphobia: a critical review. Compr Psychiatry. 1984 Jan-Feb;25(1):51-62. [PubMed: 6141894]
- 4.
Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018 Jun;35(6):502-514. [PMC free article: PMC5992015] [PubMed: 29451967]
- 5.
Otto MW, Tuby KS, Gould RA, McLean RY, Pollack MH. An effect-size analysis of the relative efficacy and tolerability of serotonin selective reuptake inhibitors for panic disorder. Am J Psychiatry. 2001 Dec;158(12):1989-92.
 [PubMed: 11729014]
[PubMed: 11729014]- 6.
Plag J, Petzold MB, Gechter J, Liebscher C, Ströhle A. Patients' characteristics and their influence on course of fear during agoraphobic symptom provocation: may SS(N)RI treatment compensate unfavorable individual preconditions? Nord J Psychiatry. 2018 Jul;72(5):325-335. [PubMed: 29644923]
- 7.
Imai H, Tajika A, Chen P, Pompoli A, Furukawa TA. Psychological therapies versus pharmacological interventions for panic disorder with or without agoraphobia in adults. Cochrane Database Syst Rev. 2016 Oct 12;10(10):CD011170. [PMC free article: PMC6457876] [PubMed: 27730622]
- 8.
Bakker A, van Balkom AJ, Spinhoven P. SSRIs vs. TCAs in the treatment of panic disorder: a meta-analysis. Acta Psychiatr Scand. 2002 Sep;106(3):163-7. [PubMed: 12197851]
- 9.
Wilkinson G, Balestrieri M, Ruggeri M, Bellantuono C. Meta-analysis of double-blind placebo-controlled trials of antidepressants and benzodiazepines for patients with panic disorders.
 Psychol Med. 1991 Nov;21(4):991-8. [PubMed: 1685792]
Psychol Med. 1991 Nov;21(4):991-8. [PubMed: 1685792]- 10.
Pollack MH, Lepola U, Koponen H, Simon NM, Worthington JJ, Emilien G, Tzanis E, Salinas E, Whitaker T, Gao B. A double-blind study of the efficacy of venlafaxine extended-release, paroxetine, and placebo in the treatment of panic disorder. Depress Anxiety. 2007;24(1):1-14. [PubMed: 16894619]
- 11.
Furukawa TA, Watanabe N, Churchill R. Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia. Cochrane Database Syst Rev. 2007 Jan 24;2007(1):CD004364. [PMC free article: PMC6823237] [PubMed: 17253502]
- 12.
Perugi G, Frare F, Toni C. Diagnosis and treatment of agoraphobia with panic disorder. CNS Drugs. 2007;21(9):741-64. [PubMed: 17696574]
Agoraphobia - StatPearls - NCBI Bookshelf
Continuing Education Activity
Agoraphobia is the anxiety that occurs when one is in a public or crowded place, from which a potential escape is difficult, or help may not be readily available.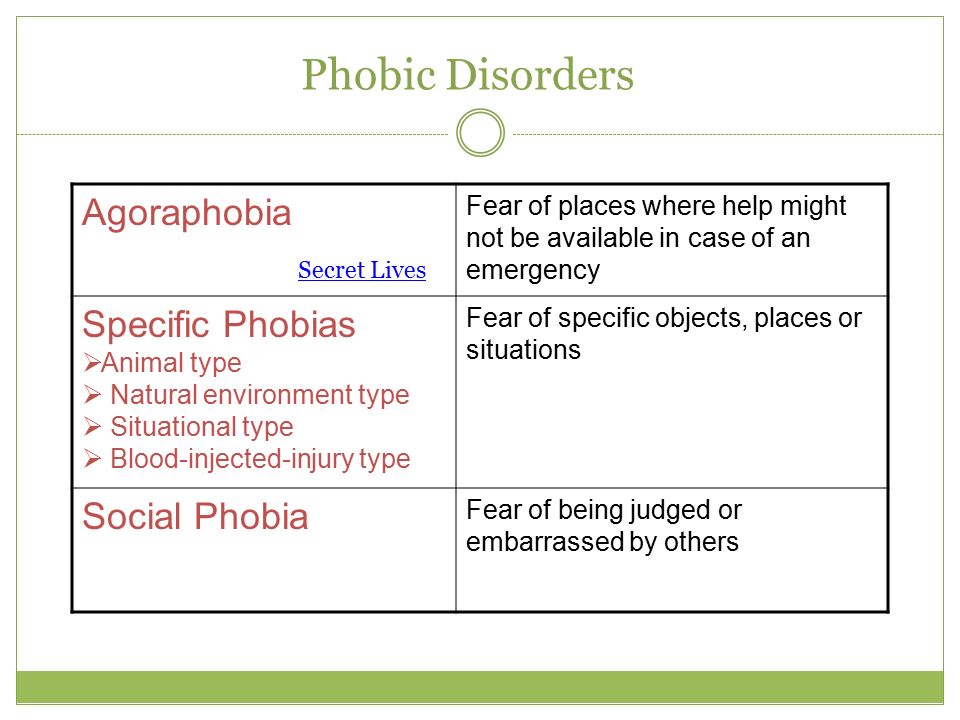 It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations. This activity describes the diagnostic criteria and characteristics of agoraphobia and outlines the interprofessional team's role in its evaluation and management.
It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations. This activity describes the diagnostic criteria and characteristics of agoraphobia and outlines the interprofessional team's role in its evaluation and management.
Objectives:
Identify the etiology of agoraphobia.
Review the diagnostic criteria/common symptomatic presentations of agoraphobia.
Outline the options available for the management of agoraphobia.
Describe some interprofessional team strategies for improving care coordination and communication for the evaluation and management of agoraphobia.
Access free multiple choice questions on this topic.
Introduction
Agoraphobia is the anxiety that occurs when one is in a public or crowded place, from which a potential escape is difficult, or help may not be readily available. It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations.[1]
It is characterized by the fear that a panic attack or panic-like symptoms may occur in these situations. Individuals with agoraphobia, therefore, strive to avoid such situations or locations.[1]
In the DSM-IV, agoraphobia was not a formal psychiatric diagnosis but was instead considered a qualifier of panic disorder. Panic disorder is characterized by recurrent or unexpected panic attacks, presenting as abrupt and intense surges of fear with various associated physical symptoms such as palpitations, shortness of breath, nausea, chest pain, dizziness, fear of dying, etc. In the currently-used DSM-5, agoraphobia is considered a distinct diagnosis that can occur independently of other diagnoses, such as generalized anxiety disorder or panic disorder. In the DSM-5, the condition is defined as “marked fear or anxiety about actual or anticipated exposure of public spaces, with the symptoms of fear or anxiety occurring most of the time in at least two of five common, different situations.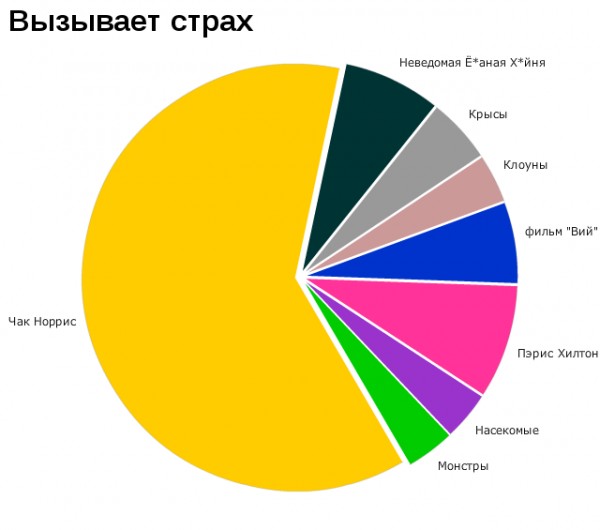 ” To meet the criteria for the diagnosis, an individual must both fear the exposure to public places and must also make active attempts to avoid such situations, either through behavioral or cognitive modifications. This fear or anxiety should not be in the context of a realistic threat, explained by sociocultural context, or occur in the context of substance use or withdrawal.[2] To formally diagnose a patient with agoraphobia, the diagnostic criteria must be present for greater than six months.
” To meet the criteria for the diagnosis, an individual must both fear the exposure to public places and must also make active attempts to avoid such situations, either through behavioral or cognitive modifications. This fear or anxiety should not be in the context of a realistic threat, explained by sociocultural context, or occur in the context of substance use or withdrawal.[2] To formally diagnose a patient with agoraphobia, the diagnostic criteria must be present for greater than six months.
Etiology
Agoraphobia is usually first identified in young adults, with the mean age of diagnosis beginning in the mid to late twenties. There is no consensus on the childhood experiences, personality characteristics, or psychosocial risk factors that lead to a diagnosis of agoraphobia. However, proposals point to several commonly occurring etiological factors. These include parental overprotectiveness, the presence of childhood fears or night terrors, experience of grief or bereavement early in life, unhappy or traumatic childhoods, or genetic predisposition. Comorbid personality types include dependent, obsessive-compulsive, or otherwise “highly-neurotic.”[3]
Comorbid personality types include dependent, obsessive-compulsive, or otherwise “highly-neurotic.”[3]
The DSM-5 further stratifies risk factors into three categories: temperamental (neuroticism, sensitivity to anxiety, and anxiety disorders), environmental (negative or traumatic events in childhood, and reduced warmth or overprotectiveness in childhood), and genetic and physiological predisposition.
Epidemiology
Anxiety disorders, encompassing generalized anxiety disorder, panic disorder, and agoraphobia, are highly prevalent in the general population.[1] There is some disparity in estimates for the prevalence of agoraphobia as it has only recently received its own diagnostic criteria rather than as a qualifier for panic disorder. According to the DSM-5, agoraphobia is present in approximately 1.7% of the general population. It further states that most cases of agoraphobia present before the age of 35. There is an increase in the risk of developing agoraphobia in late adolescence and early adulthood, with the overall average age at onset being 17 years. The National Institute of Mental Health estimates that the lifetime prevalence of agoraphobia is 1.3%, with an annual incidence rate of 0.9%. Yearly prevalence rates of agoraphobia are similar between males (0.8%) and females (0.9%).
The National Institute of Mental Health estimates that the lifetime prevalence of agoraphobia is 1.3%, with an annual incidence rate of 0.9%. Yearly prevalence rates of agoraphobia are similar between males (0.8%) and females (0.9%).
History and Physical
As with all psychiatric diagnoses, an essential tool in diagnosis is the interview. There is no physical exam finding that would indicate a diagnosis of agoraphobia.
Evaluation
The DSM-5 outlines the criteria by which a diagnosis of agoraphobia is possible.[2] To definitively diagnose a patient with agoraphobia, they must have intense fear in response to or when anticipating entering into at least two of the five following situations: using public transportation (automobiles, buses, trains), being in open spaces (marketplaces, parking lots), being in enclosed spaces like theaters or malls, standing in lines or crowds, or being outside of the home alone. This fear, which is out of proportion to the actual stimulus, must be accompanied by behavioral or cognitive modifications to avoid placing oneself in situations where the exposure may occur.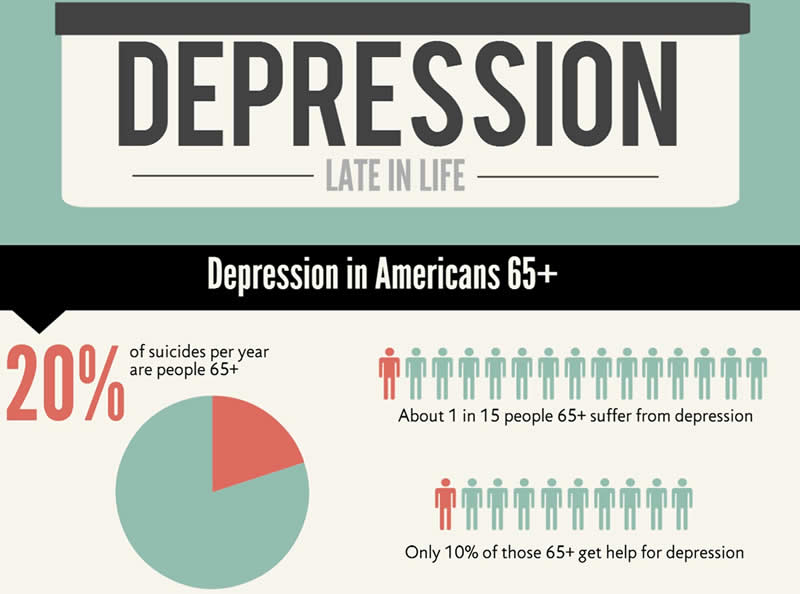 These symptoms must be present for at least six months and must cause significant distress to the patient and impairment in their lives. The symptoms also should not be better explained by another psychiatric diagnosis, be directly caused by a medical diagnosis, or occur in the context of substance use or withdrawal.
These symptoms must be present for at least six months and must cause significant distress to the patient and impairment in their lives. The symptoms also should not be better explained by another psychiatric diagnosis, be directly caused by a medical diagnosis, or occur in the context of substance use or withdrawal.
Treatment / Management
Though panic disorder and agoraphobia have been differentiated, with two different sets of diagnostic criteria, the treatment algorithms for the two remain similar. The first step is to identify the severity of the disease when the patient presents; this is often a measure of the level of impairment or distress the agoraphobia or panic disorder causes in the patient’s life.
Patients with mild or moderate panic disorder or agoraphobia can choose between psychotherapy and pharmacotherapy to achieve adequate symptom management. Studies have generally concluded that cognitive-behavioral therapy (CBT) effectively addresses and alleviates target symptoms, lessens other anxiety symptoms, and improves the patient's quality of life. [4] For patients with more severe forms of agoraphobia or for those who prefer pharmacotherapy over psychotherapy, there are several effective options for medication management. Selective serotonin receptor inhibitors (SSRIs) are generally considered first-line therapy, with therapeutic doses being the same as in depression.[5] Serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and benzodiazepines have also been effective alternatives SSRIs in the treatment of panic disorder and agoraphobia.[6][7] SSRIs are generally preferable to these other medications because of the side effect profile, affordability, availability, decreased potential for abuse, and better tolerability.[8][9][10] There is also data suggesting that the combination of CBT with pharmacotherapy may be most effective in the symptomatic management of agoraphobia and panic disorder.[11]
[4] For patients with more severe forms of agoraphobia or for those who prefer pharmacotherapy over psychotherapy, there are several effective options for medication management. Selective serotonin receptor inhibitors (SSRIs) are generally considered first-line therapy, with therapeutic doses being the same as in depression.[5] Serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and benzodiazepines have also been effective alternatives SSRIs in the treatment of panic disorder and agoraphobia.[6][7] SSRIs are generally preferable to these other medications because of the side effect profile, affordability, availability, decreased potential for abuse, and better tolerability.[8][9][10] There is also data suggesting that the combination of CBT with pharmacotherapy may be most effective in the symptomatic management of agoraphobia and panic disorder.[11]
Differential Diagnosis
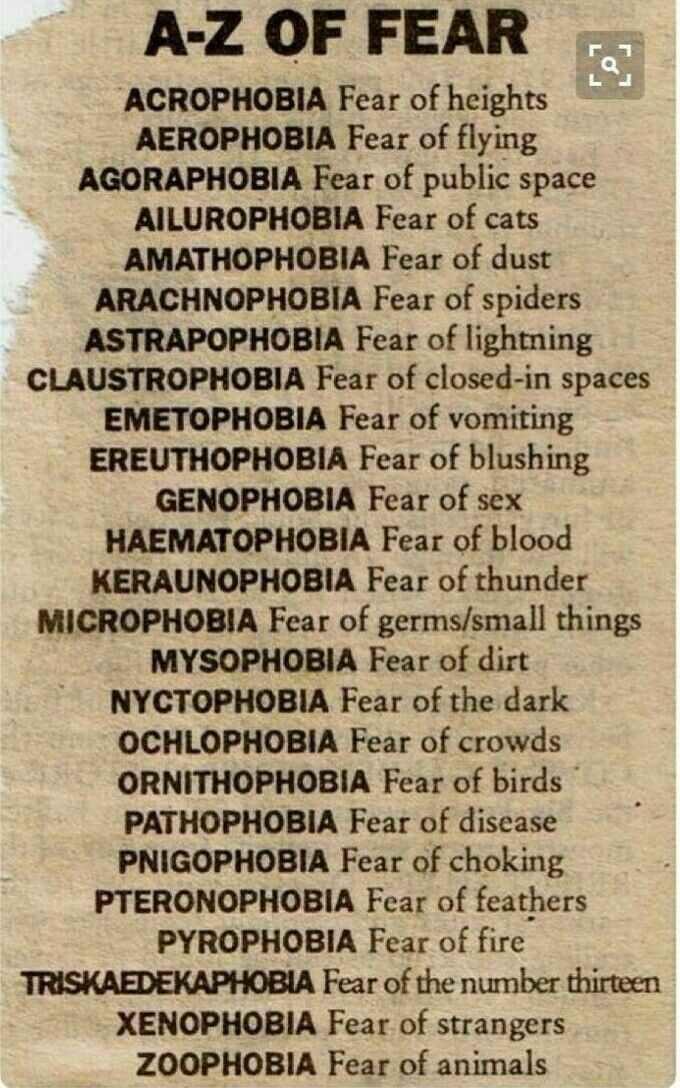
According to the DSM-5, the most common differential diagnoses for agoraphobia include specific phobia, separation anxiety disorder, social anxiety disorder, panic disorder, acute stress disorder or posttraumatic stress disorder, and major depressive disorder. Specific phobia should be diagnosed, rather than agoraphobia, if the fear, anxiety, avoidance, or behavioral modification is limited to one of the five, rather than two, of the situations in which agoraphobia can occur. Separation anxiety disorder can be differentiated from agoraphobia if the fear or anxiety arises when considering detachment from loved ones or the home environment, rather than the panic associated with being in the feared situations themselves.
Specific phobia should be diagnosed, rather than agoraphobia, if the fear, anxiety, avoidance, or behavioral modification is limited to one of the five, rather than two, of the situations in which agoraphobia can occur. Separation anxiety disorder can be differentiated from agoraphobia if the fear or anxiety arises when considering detachment from loved ones or the home environment, rather than the panic associated with being in the feared situations themselves.
Social anxiety involves fear about being negatively judged in public situations rather than, like separation anxiety disorder, being in the situations themselves. Panic disorder is the appropriate diagnosis if the panic symptoms occur in less than two of the five diagnostic agoraphobic conditions or if they occur in other non-public situations or circumstances. Acute stress disorder or posttraumatic stress disorder is the diagnosis if the fear, anxiety, or avoidance functions to avoid reminding the individual of a past traumatic event.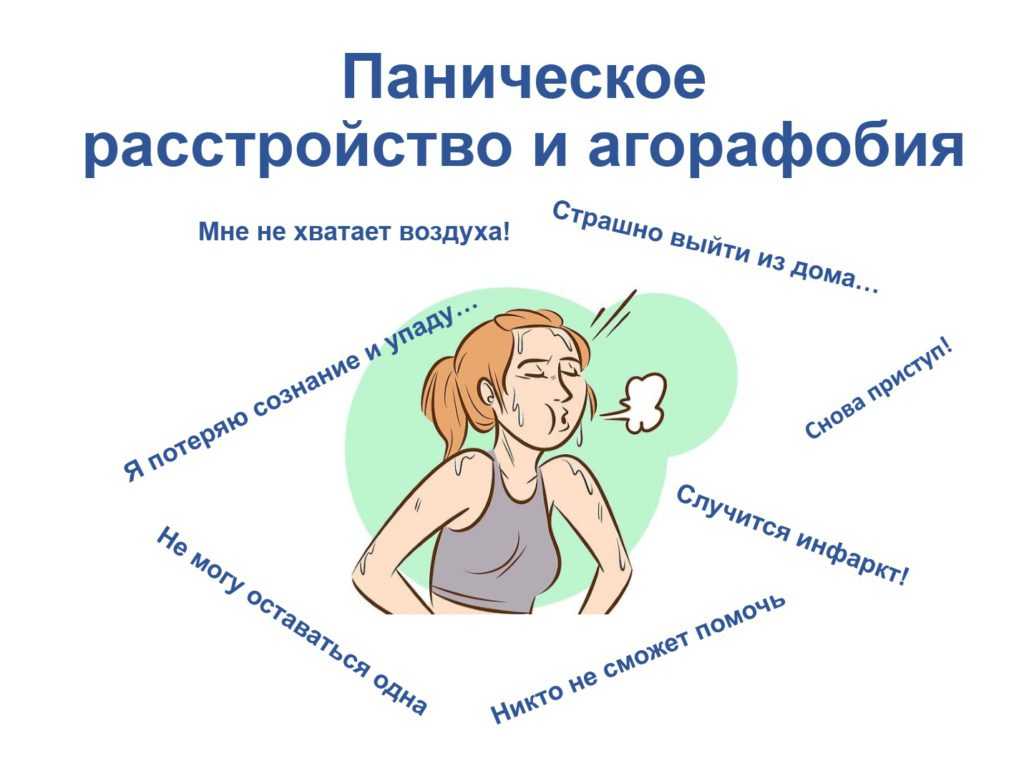 Major depressive disorder should be the diagnosis if the patient also reports associated anhedonia, apathy, loss of energy, insomnia, or low self-esteem. Agoraphobia also cannot be diagnosed if the behavioral modifications are to avoid consequences of medical conditions, such as fears of losing consciousness in public for someone with cardiovascular pathology or developing diarrhea in someone with inflammatory bowel disease.
Major depressive disorder should be the diagnosis if the patient also reports associated anhedonia, apathy, loss of energy, insomnia, or low self-esteem. Agoraphobia also cannot be diagnosed if the behavioral modifications are to avoid consequences of medical conditions, such as fears of losing consciousness in public for someone with cardiovascular pathology or developing diarrhea in someone with inflammatory bowel disease.
Prognosis
The DSM-5 describes the course of agoraphobia as “persistent and chronic,” with complete remission being relatively rare except with treatment or intervention.[12] Rates of remission are reduced when the severity of agoraphobia is higher. The chance of a favorable prognosis is also reduced by the presence of comorbid anxiety disorders, depression, personality disorders, or substance use disorders.
Complications
Agoraphobia itself is associated with significant distress and impairment in life. In severe cases, it can cause individuals to become completely home-bound and dependent on others for anything that requires leaving one’s home. This can lead to self-medication with non-prescription medications or other substances. The DSM-5 states that remission rates without treatment are quite low, with averages estimated at about 10%.
This can lead to self-medication with non-prescription medications or other substances. The DSM-5 states that remission rates without treatment are quite low, with averages estimated at about 10%.
Agoraphobia is also associated with an increased risk of developing comorbid major depressive disorder, persistent depressive disorder (dysthymia), and substance use disorders.
Deterrence and Patient Education
The prevention of agoraphobia would involve the mediation of significant risk factors. Appropriate strategies for its management include early identification of symptoms, prompt intervention, access to resources and mental health professionals, facilitation of open discussions with patients, and effective management with psychotherapy or pharmacotherapy.
Enhancing Healthcare Team Outcomes
Agoraphobia, while only recently differentiated from panic disorder with its diagnostic criteria, is extremely prevalent in the general population. When present, it causes significant distress and potential disability in an individual’s life. Due to its “persistent and chronic” course, if left untreated, it is essential that agoraphobia is diagnosed early and intervention initiated promptly. It is critical that healthcare professionals, particularly primary care providers, be well-versed in the symptomatology of agoraphobia and proficient in diagnosing and starting any necessary treatment. Patients must have a connection to avenues to obtain adequate resources for their distress and disability, and referrals to psychology and psychiatry should take place if deemed necessary. Treatment can involve psychologists, social workers, psychiatric nurses, and nurse practitioners. They all participate in patient education and monitor patients. Nursing staff can assess compliance, answer patient questions, and watch for adverse effects from medication, alerting the prescriber promptly of any concerns. Pharmacists review prescriptions, check for interactions and inform patients about side effects. They can also provide input on which agents are best to use for a specific patient and therapy modifications if progress stalls.
Due to its “persistent and chronic” course, if left untreated, it is essential that agoraphobia is diagnosed early and intervention initiated promptly. It is critical that healthcare professionals, particularly primary care providers, be well-versed in the symptomatology of agoraphobia and proficient in diagnosing and starting any necessary treatment. Patients must have a connection to avenues to obtain adequate resources for their distress and disability, and referrals to psychology and psychiatry should take place if deemed necessary. Treatment can involve psychologists, social workers, psychiatric nurses, and nurse practitioners. They all participate in patient education and monitor patients. Nursing staff can assess compliance, answer patient questions, and watch for adverse effects from medication, alerting the prescriber promptly of any concerns. Pharmacists review prescriptions, check for interactions and inform patients about side effects. They can also provide input on which agents are best to use for a specific patient and therapy modifications if progress stalls.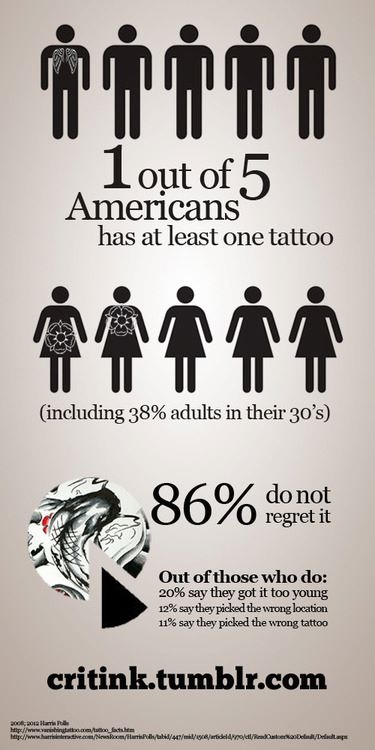 These interprofessional interventions can improve patient outcomes for agoraphobia patients. [Level 5]
These interprofessional interventions can improve patient outcomes for agoraphobia patients. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Roest AM, de Vries YA, Lim CCW, Wittchen HU, Stein DJ, Adamowski T, Al-Hamzawi A, Bromet EJ, Viana MC, de Girolamo G, Demyttenaere K, Florescu S, Gureje O, Haro JM, Hu C, Karam EG, Caldas-de-Almeida JM, Kawakami N, Lépine JP, Levinson D, Medina-Mora ME, Navarro-Mateu F, O'Neill S, Piazza M, Posada-Villa JA, Slade T, Torres Y, Kessler RC, Scott KM, de Jonge P., WHO World Mental Health Survey Collaborators. A comparison of DSM-5 and DSM-IV agoraphobia in the World Mental Health Surveys. Depress Anxiety. 2019 Jun;36(6):499-510. [PMC free article: PMC6548607] [PubMed: 30726581]
- 2.
Asmundson GJ, Taylor S, Smits JA. Panic disorder and agoraphobia: an overview and commentary on DSM-5 changes.
 Depress Anxiety. 2014 Jun;31(6):480-6. [PubMed: 24865357]
Depress Anxiety. 2014 Jun;31(6):480-6. [PubMed: 24865357]- 3.
Tearnan BH, Telch MJ, Keefe P. Etiology and onset of agoraphobia: a critical review. Compr Psychiatry. 1984 Jan-Feb;25(1):51-62. [PubMed: 6141894]
- 4.
Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018 Jun;35(6):502-514. [PMC free article: PMC5992015] [PubMed: 29451967]
- 5.
Otto MW, Tuby KS, Gould RA, McLean RY, Pollack MH. An effect-size analysis of the relative efficacy and tolerability of serotonin selective reuptake inhibitors for panic disorder. Am J Psychiatry. 2001 Dec;158(12):1989-92. [PubMed: 11729014]
- 6.
Plag J, Petzold MB, Gechter J, Liebscher C, Ströhle A. Patients' characteristics and their influence on course of fear during agoraphobic symptom provocation: may SS(N)RI treatment compensate unfavorable individual preconditions? Nord J Psychiatry.
 2018 Jul;72(5):325-335. [PubMed: 29644923]
2018 Jul;72(5):325-335. [PubMed: 29644923]- 7.
Imai H, Tajika A, Chen P, Pompoli A, Furukawa TA. Psychological therapies versus pharmacological interventions for panic disorder with or without agoraphobia in adults. Cochrane Database Syst Rev. 2016 Oct 12;10(10):CD011170. [PMC free article: PMC6457876] [PubMed: 27730622]
- 8.
Bakker A, van Balkom AJ, Spinhoven P. SSRIs vs. TCAs in the treatment of panic disorder: a meta-analysis. Acta Psychiatr Scand. 2002 Sep;106(3):163-7. [PubMed: 12197851]
- 9.
Wilkinson G, Balestrieri M, Ruggeri M, Bellantuono C. Meta-analysis of double-blind placebo-controlled trials of antidepressants and benzodiazepines for patients with panic disorders. Psychol Med. 1991 Nov;21(4):991-8. [PubMed: 1685792]
- 10.
Pollack MH, Lepola U, Koponen H, Simon NM, Worthington JJ, Emilien G, Tzanis E, Salinas E, Whitaker T, Gao B. A double-blind study of the efficacy of venlafaxine extended-release, paroxetine, and placebo in the treatment of panic disorder.
 Depress Anxiety. 2007;24(1):1-14. [PubMed: 16894619]
Depress Anxiety. 2007;24(1):1-14. [PubMed: 16894619]- 11.
Furukawa TA, Watanabe N, Churchill R. Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia. Cochrane Database Syst Rev. 2007 Jan 24;2007(1):CD004364. [PMC free article: PMC6823237] [PubMed: 17253502]
- 12.
Perugi G, Frare F, Toni C. Diagnosis and treatment of agoraphobia with panic disorder. CNS Drugs. 2007;21(9):741-64. [PubMed: 17696574]
What is agoraphobia and how people live with it
Alena Agadzhikova has agoraphobia: she is afraid to leave her apartment and find herself in an unfamiliar place. Alena decided to conduct an experiment by placing herself in uncomfortable conditions. PR manager Dasha Tikhomirova agreed to do the same. Both girls kept diaries in the "here and now" format. Afisha publishes them along with a psychotherapist's commentary.
What is agoraphobia and where does it come from?
Agoraphobia is supposed to be the fear of open spaces. In fact, it is both the fear of not being able to immediately leave a place or situation, and the fear of being away from home. The discrepancies are due to the fact that at the time of the introduction of this term into psychiatry, there were no typical agoraphobia triggers for the modern world: public transport, passenger planes and shopping centers. Maybe in the time of Karl Westphal (a German psychiatrist and neurologist who lived in the 19th century, the author of many psychiatric terms. - Note ed. ), who first described agoraphobia, the open spaces of the piazzas were as unpleasant as our subways are now at rush hour. Agoraphobia is now commonly referred to as the fear and avoidance of independent movement outside the home (or other safe place).
In fact, it is both the fear of not being able to immediately leave a place or situation, and the fear of being away from home. The discrepancies are due to the fact that at the time of the introduction of this term into psychiatry, there were no typical agoraphobia triggers for the modern world: public transport, passenger planes and shopping centers. Maybe in the time of Karl Westphal (a German psychiatrist and neurologist who lived in the 19th century, the author of many psychiatric terms. - Note ed. ), who first described agoraphobia, the open spaces of the piazzas were as unpleasant as our subways are now at rush hour. Agoraphobia is now commonly referred to as the fear and avoidance of independent movement outside the home (or other safe place).
The disorder arises from a predisposition to anxiety and psychological factors. The latter, according to the British Ministry of Health, include: sexual abuse (especially in childhood), bereavement, divorce, job loss, anorexia or bulimia, alcohol abuse, being in an unhappy relationship or in a relationship with an over-controlling partner. In national studies of various Western countries, figures from 1.3 to 3.5% of the prevalence of agoraphobia in the population appear. Anxiety disorders are diseases in the development of which a genetic predisposition factor plays a relatively large role, so their incidence is approximately the same in different countries of the world. Based on this, it can be assumed that in Russia, about one in 50 people is also subject to agoraphobia.
In national studies of various Western countries, figures from 1.3 to 3.5% of the prevalence of agoraphobia in the population appear. Anxiety disorders are diseases in the development of which a genetic predisposition factor plays a relatively large role, so their incidence is approximately the same in different countries of the world. Based on this, it can be assumed that in Russia, about one in 50 people is also subject to agoraphobia.
Most people with agoraphobia begin with panic attacks in public places.
For many, a panic attack is one of the worst emotional experiences of a lifetime.
The strongest fear is instantly associated in the brain with the place where this event occurred. When you visit it again, the deep parts of the brain responsible for the fear reaction (in particular, the amygdala) are activated again and further strengthen this conditioned reflex connection. In the future, fear can spread to other places similar to the first in some characteristics: for example, it becomes scary to be not only in the supermarket on the minus the first floor where the first panic attack occurred, but also in all public places where you need to go down to escalator. If a person knows what kind of sensations await him in such places, he begins to avoid them. It turns out that he actually avoids not public places, but his own emotional reactions and difficult to bear bodily sensations that arise there . Sometimes a person can have both claustrophobia (fear of enclosed spaces. - ed. note ) and agoraphobia. There are no contradictions here: a common place in these states is the fear that it is impossible to instantly get out of the situation and find yourself in a “safe” place. And both the crowd on the street and the closed elevator doors can prevent this.” nine0003
If a person knows what kind of sensations await him in such places, he begins to avoid them. It turns out that he actually avoids not public places, but his own emotional reactions and difficult to bear bodily sensations that arise there . Sometimes a person can have both claustrophobia (fear of enclosed spaces. - ed. note ) and agoraphobia. There are no contradictions here: a common place in these states is the fear that it is impossible to instantly get out of the situation and find yourself in a “safe” place. And both the crowd on the street and the closed elevator doors can prevent this.” nine0003
What happens if a person with agoraphobia confronts their fear?
Situation
Plan: take the subway two stops. I definitely won't do it anymore. One is not interesting, because I want to live the moment when the train stops, the doors open, and I don’t run out and go on. The last time I was on the subway was about a year and a half ago when I was trying to get out of my comfort zone and train myself. Before that, I had not been to the subway for about two more years. Agoraphobia began in me during an exacerbation of an anxiety-depressive disorder, which I have been suffering from for several years. In general, panic attacks have been with me all my life: they appeared and left, I felt bad on the subway or on the street, but I coped without medication, because there was no choice - I hid these conditions from relatives and friends, I was ashamed. Now I have been seeing a psychiatrist for three years now, I visit a cognitive-behavioral psychotherapist once a week, I drink a “cocktail” of antidepressants and tranquilizers. nine0003
Before that, I had not been to the subway for about two more years. Agoraphobia began in me during an exacerbation of an anxiety-depressive disorder, which I have been suffering from for several years. In general, panic attacks have been with me all my life: they appeared and left, I felt bad on the subway or on the street, but I coped without medication, because there was no choice - I hid these conditions from relatives and friends, I was ashamed. Now I have been seeing a psychiatrist for three years now, I visit a cognitive-behavioral psychotherapist once a week, I drink a “cocktail” of antidepressants and tranquilizers. nine0003
Beginning
I usually become anxious about going out as soon as I know it is necessary. This may be the decision to go to a cafe with a friend, the need to go to the doctor without her husband, and anything else. Anxiety increases on the eve of the event. This manifests itself in hyperventilation (frequent shallow breathing. - Note ed. ), stomach cramps, dizziness, pain in general in all muscles of the body, tachycardia. That's what happened this time as well. nine0003
), stomach cramps, dizziness, pain in general in all muscles of the body, tachycardia. That's what happened this time as well. nine0003
When Alena invited me to participate in the experiment, I was horrified. I immediately began to choke, the muscles of my forearms cramped.
Further, as a rule, the same thought loops in the head, which is almost impossible to get rid of. Now this is a picture of how I cannot get out of a subway car during a panic attack. Such situations happened to me more than once, and they merge into one terrible scene at once. A panic attack sets in, I restrain it with all the methods known to me: I touch objects, listen to smells, count colors, stretch my feet. Fear drives me crazy and makes me depressed. It is at such moments that the desire to commit suicide escalates to a maximum. nine0003
Preparation
In order to fool my brain, I have developed a system of rituals that helps reduce anxiety to a level that allows you to even step over the threshold of the house. Here they are: wash your hair, style your hair beautifully, carefully choose clothes. Then I start putting on makeup. These are my ways of putting extra armor on my body to protect myself from the outside world. In addition, this is a rather meditative process that requires concentration. Anxiety has less space in the mind. In parallel, I think about all the options for the development of events and convince myself that none of them will lead to my death. nine0003
Here they are: wash your hair, style your hair beautifully, carefully choose clothes. Then I start putting on makeup. These are my ways of putting extra armor on my body to protect myself from the outside world. In addition, this is a rather meditative process that requires concentration. Anxiety has less space in the mind. In parallel, I think about all the options for the development of events and convince myself that none of them will lead to my death. nine0003
So, I carefully put on makeup, dressed up, admired the new coat and pink shoes, checked if clonazepam (an antiepileptic drug, used by a doctor. - Note ed. ) was in place and whether it was enough (I usually wear a minimum three tablets, although a quarter or half is enough to relieve a panic attack). She said all the options: I’m starting an attack, I’m shaking, I can’t breathe, I grab onto all the surrounding objects, everyone is staring at me, it gets dark in my eyes, my legs buckle, I dream of losing consciousness, nothing helps, the train gets stuck in the tunnel, I feel even worse, clonazepam does not help.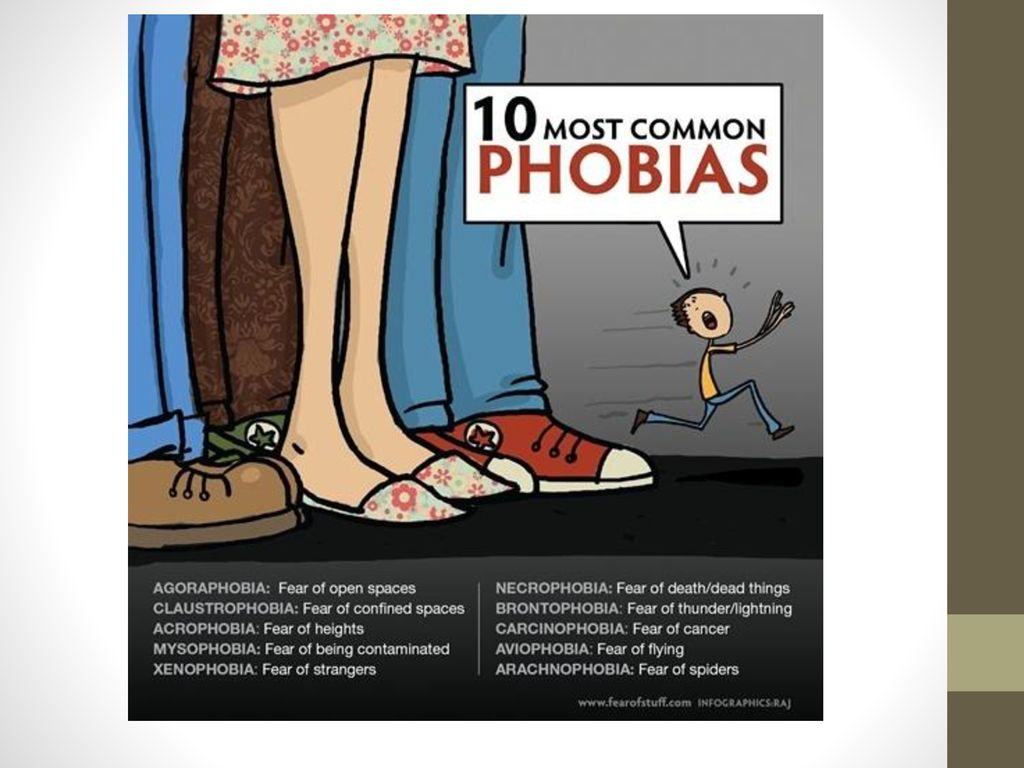 I run up to the car doors to run out, as soon as they start to open, my legs give way, I lie down and sob. I countered: “You know that you don’t die from a panic attack!” People around are not evil: they will either sympathize or not pay attention. Someone can offer help. It gets a little better. nine0003
I run up to the car doors to run out, as soon as they start to open, my legs give way, I lie down and sob. I countered: “You know that you don’t die from a panic attack!” People around are not evil: they will either sympathize or not pay attention. Someone can offer help. It gets a little better. nine0003
Climax
I alone could not decide to accomplish this little feat, I asked my husband to take part in the experiment. My husband is getting dressed, I am furious because it seems to me that he does it too slowly. When the inevitable is near, you want it to happen as soon as possible. We go out into the street, my husband tries to distract me with conversations on external topics. When he sees that it does not work, he starts asking questions so that I can express my feelings. He pronounces all the ways of salvation: we can go home at any moment, we will be very close to home, so it will not take much time. If it gets bad, bury yourself in me. We continue to walk: I am surprised how the road to the metro has changed (new paths, fences), the area in front of the metro (a mini-square with benches has been broken!), the entrance group (like fashionable). nine0003
nine0003
Coming down. I feel my leg muscles contract, it hurts to walk. I turn off consciousness, something like depersonalization sets in. It’s as if I’m watching from the side as the girl Dasha applies the ticket, stands on the platform. The train is coming. Once I enter it, it will be impossible to escape. I start crying (this is another tension-release mechanism recently discovered by accident). In front of the car doors, I say: "NO!" I take my husband by the arm, I feel that now I will collapse.
All muscles are so cramped that it is almost impossible to walk. Breathing is impossible. Hands and feet are icy, palms are shaking, sticky with sweat. nine0003
People squint, we quickly leave. I feel like I'm sweating through, right down to my beautiful blue coat. The scarf is pulled off, it is unbearable to feel something on the throat. I'm very hot, we're walking back down the street. It's cold outside, but I can't button up.
Walking is still very painful, you have to walk slowly.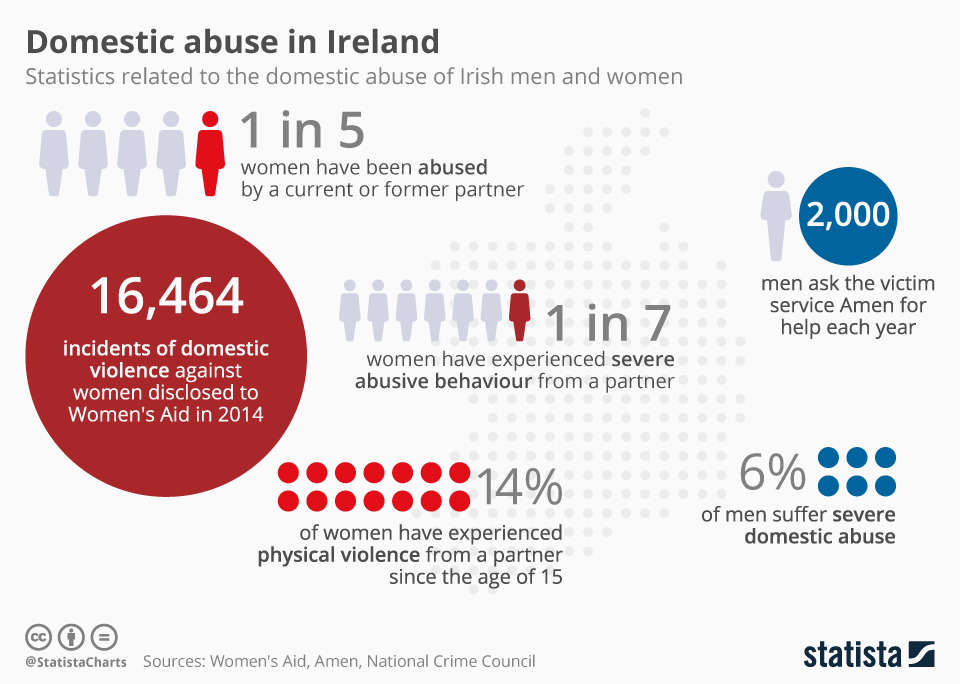 Gradually, the panic passes, and a feeling of devastation remains. I start to get cold, I wrap myself in a scarf, I overcome the rest of the way in silence, my sadness becomes somehow flat, I hate and despise myself. I try to feel sorry for myself, but it doesn't work. I feel ashamed in front of my husband. nine0003
Gradually, the panic passes, and a feeling of devastation remains. I start to get cold, I wrap myself in a scarf, I overcome the rest of the way in silence, my sadness becomes somehow flat, I hate and despise myself. I try to feel sorry for myself, but it doesn't work. I feel ashamed in front of my husband. nine0003
When I get home, I immediately take off all my clothes, wash off my make-up, and get under the covers. It’s not easy to relax, I put clonazepam under my tongue. I feel nauseous, the muscles gradually relax, but continue to whine. My head hurts. Even drawn curtains let in too much light. I wrap myself up in a blanket very tightly, put on a mask over my eyes and fall into a viscous disturbing dream. When I wake up, I continue to feel nausea, headache, dizziness, anxiety returns, but drinking clonazepam again means falling asleep again. I'm trying to disperse, eat something, breathe. I turn on the Colombo series: I know all the episodes by heart, but nothing new comes out of watching in this state. "Colombo", "Poirot" and "Harry Potter" are stored on the computer in the "Eternal" folder - I turn them on randomly in any incomprehensible situation. nine0003
"Colombo", "Poirot" and "Harry Potter" are stored on the computer in the "Eternal" folder - I turn them on randomly in any incomprehensible situation. nine0003
For the next two days I continue to experience headaches and muscle pain, it is difficult for me to concentrate, I feel moral devastation, frenzy. I cancel all the few things I do, eat, take care of myself, lie under the covers, correspond with the psychiatrist, note that this time I have gone much further than before (for example, often I just cancel the meeting after not coping with anxiety), praise myself for the fact that I learned to stop in time and decided to try it in general. I believe that everything will be fine. nine0003
Afterword
Actually, my life is not so terrible. I learned to build it by avoiding trigger situations. I almost never go to public places, but I can go to a concert or a restaurant if my husband is with me or not far away. I communicate with friends by inviting them to visit or coming to them. I go to the doctors by taxi. Previously, this was also difficult for me, but now I almost do not experience unbearable anxiety. I see progress in treatment and thank myself for every small step in overcoming myself and the disease. nine0003
I go to the doctors by taxi. Previously, this was also difficult for me, but now I almost do not experience unbearable anxiety. I see progress in treatment and thank myself for every small step in overcoming myself and the disease. nine0003
13:00. Flight from Moscow to Prague
It's so gray outside that you don't want to live. I'm going in a taxi to Sheremetyevo. I'm horrified: I'm late for the flight, and my anxiety is going through the roof. I thought that after two flights in my life, in which I was naturally delighted with air pockets and felt as safe as possible, there would be no more fear. But he is.
“What if the plane leaves and I stay at the airport? I will have a panic attack, I will lie on the ground, everything will go dark in my eyes, as it was once in the subway. Will have to call an ambulance. Don't care what people think! I don’t give a damn about the fact that at such moments my body becomes icy from the inside, and I almost can’t speak.” Great thoughts! The most it is before the flight. nine0003
nine0003
I see terminals somewhere in the distance. So maybe I won't be late. When I have such anxiety, my intestines weaken. This is probably the most socially disturbing thing for me. Lying in the middle of the crowd is still all right, but crap yourself... We are approaching. I am not late. Glory to Gagarin.
I am sitting in the airport lounge. I was not late, although I could. It seems that I need to listen to my mother more, even if she gets on my nerves with her catastrophizing. Behind the glass are airplanes. The condition, despite yesterday's gin, is quite tolerable. Probably worth saying thanks to phenazepam (drug, taken only as directed by a doctor. - Note ed. ) and herself. Two years ago, the mere thought that I would be flying in an airplane plunged me into a state of acute panic. Imagine that I am sitting here, drinking water without gas, and even one ... Show me such a photo of me before, I would definitely say that this is photoshop. And angry: "I feel so bad that I can't fly anywhere, and you're kidding!"
Beginning
It all started at 10 years old. Then I started having panic attacks. Nobody knew what was happening to me: they took me to church, to a fortune-teller, once they took me to a district psychiatrist - he refused to accept "without taking into account", requested a bribe and prescribed Novo-Passit (a sedative of plant origin. - Note ed. ) . As a child, I didn’t know what was happening to me: just one night I suddenly started shaking, and it also seemed that my head was going numb. Further - as if in a fog: unbearable horror and fear. Fear of death? No, I was not afraid to die, I knew that I was not dying. Fear of losing control? More like the truth. nine0003
Then I started having panic attacks. Nobody knew what was happening to me: they took me to church, to a fortune-teller, once they took me to a district psychiatrist - he refused to accept "without taking into account", requested a bribe and prescribed Novo-Passit (a sedative of plant origin. - Note ed. ) . As a child, I didn’t know what was happening to me: just one night I suddenly started shaking, and it also seemed that my head was going numb. Further - as if in a fog: unbearable horror and fear. Fear of death? No, I was not afraid to die, I knew that I was not dying. Fear of losing control? More like the truth. nine0003
Fear of fear, fear of this uncontrollable shaking, numb hands, growing terror? Yes.
I recently had five CBT sessions. The psychiatrist said that panic disorder develops into agoraphobia most often in those alarmists who do not have a specific phobia. In other words, the fear of death, the fear of social condemnation, the fear of a stroke are things that are less likely to lead to the fact that you will be afraid to be far from home. But the feeling of the impossibility of experiencing this difficult state, concentration on it - this is exactly that. nine0003
But the feeling of the impossibility of experiencing this difficult state, concentration on it - this is exactly that. nine0003
Panic disorder was followed by OCD (an obsessive-compulsive disorder in which a person has obsessive thoughts, memories, movements and actions, as well as various fears. - Note ed. ). For OCD - an anxiety-depressive disorder (a disease in which a person experiences both anxiety and depression without a clear dominance of one of the conditions. - Note ed. ). It's me now, examined by psychiatrists and undergoing psychotherapy, I know what's wrong with me. And then, ten years ago, information came in pieces and through the Internet. nine0003
My life underwent a major change when I suddenly became terribly afraid of being away from home. I remember at the age of 14 I stayed with my boyfriend on the other side of Moscow. It was night, neither he nor I had any money. He fell asleep, I didn't. And suddenly a familiar horror began to seize me, the back of my head began to go numb. It was cold outside, the lanterns were burning with a nasty yellow light. I became incredibly sad and scared. I thought: “What should I do if I want to go home right now? How can I get home RIGHT NOW, because the subway does not work, there are no buses, my parents will not understand me if I call and ask in a panic to pick me up. WHAT SHOULD I DO?" Panic thoughts began to come one after another. I was shaking. I was afraid to wake up the guy, because he, like me, did not know what was happening to me, so he would twist his finger at his temple. nine0003
It was cold outside, the lanterns were burning with a nasty yellow light. I became incredibly sad and scared. I thought: “What should I do if I want to go home right now? How can I get home RIGHT NOW, because the subway does not work, there are no buses, my parents will not understand me if I call and ask in a panic to pick me up. WHAT SHOULD I DO?" Panic thoughts began to come one after another. I was shaking. I was afraid to wake up the guy, because he, like me, did not know what was happening to me, so he would twist his finger at his temple. nine0003
I lay there unable to move, thinking of all sorts of crazy ways to get out of the house.
Here I imitate pain in my stomach and call an ambulance, but no, the ambulance will not take me home, but to the hospital... Here I am borrowing money from friends, but from whom? Everybody sleeps. Yes, and how to explain what urgency is? Morning has come. I didn't get any sleep. All day long she walked in a fog, periodically plunging into panic attacks and gritting her teeth.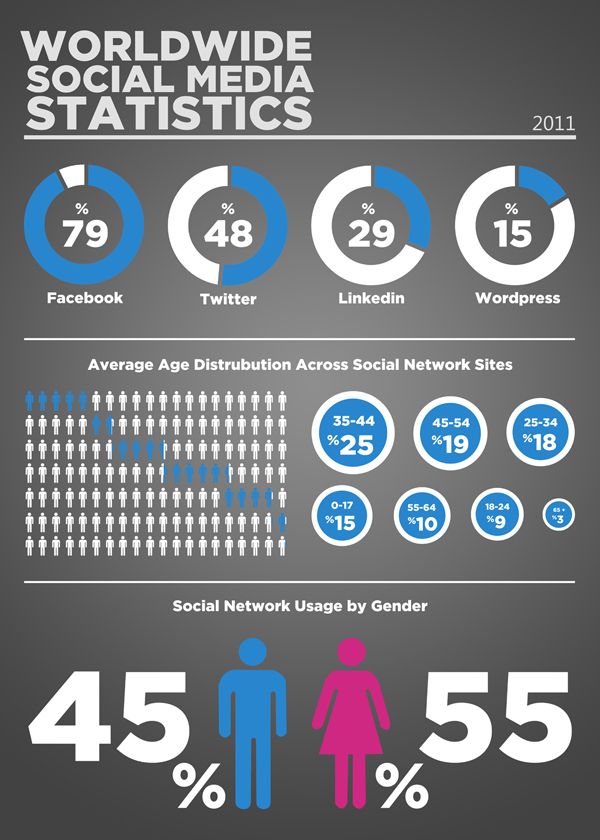
Worsening
Over time, these attacks became more frequent. It became difficult for me to travel out of town. Already on the bus, I began to think: “What if I want to get off the bus right now? I can't do that. And if I do, where should I go?" The image of me in an unfamiliar area, unable to move, firmly settled in my head. I began to avoid traveling anywhere. The next nightmare was the subway. A train stopping in a tunnel is the worst picture that has remained with me so far. nine0003
The quintessence of a situation that cannot be influenced. I was lucky to get both claustrophobia (fear of closed spaces) and agoraphobia. Every time a train gets stuck in a tunnel, I sit for three or four minutes, and then I start thrashing about. I imagine how I break the windows, how I get out. It becomes hard to breathe, there is a feeling that my own horror will eventually drive me crazy. My dream when the train stops in the tunnel is to faint and wake up when it is already at the station. nine0014 But, unfortunately, I fainted only a few times and in other circumstances.
nine0014 But, unfortunately, I fainted only a few times and in other circumstances.
At the age of 20, I started treatment - antidepressants, therapy. If I had started it earlier, at least four years, much could have been avoided. It would be easier to overcome the same agoraphobia. My social capital would be even greater, the number of accumulated impressions too. But right now it's a sin to complain.
Boarding begins.
I try to take a deep breath and realize what work has been done over all these years. nine0003
15:25. I'm on the plane
We took off. I smile and fall asleep. This is my third flight in my life and the first in the evening. It's so great that there is no light in the cabin and you can see the glow of the blue horizon of clouds - like Kuindzhi in the picture. It feels like all the problems have remained below, under the clouds, and I am cradled in a warm cradle. Something that, as it seemed to me for many years, can drive me crazy, gives a feeling of happiness and peace. I feel light and relaxed. I can not continue to write, a strong drowsiness attacked. I'll sleep. nine0003
I feel light and relaxed. I can not continue to write, a strong drowsiness attacked. I'll sleep. nine0003
Did not sleep. We are flying over Vilnius. I would like to visit Vilnius. And everywhere, since now I can fly.
How did it happen that I started flying? My beloved person moved to Prague. My best friend has been living there for the eighth year now. And so I won a grant covering flights, accommodation and study for a month in Prague. I, in fact, had no internal choice: either now or never.
First flight
On the eve of the first flight, I was shaken from the very morning. Parents followed. Most of all, I was afraid of waiting. The flight itself is not very good, I am not afraid of heights and death. I will die and die. Now it seems to me that death from a fall is far from the worst option. It's beautiful, and in the chest everything will go to the end. But then I was shaking because I was afraid of panic at the moment of waiting, fear of fear. A tranquilizer and awareness of what was happening helped me.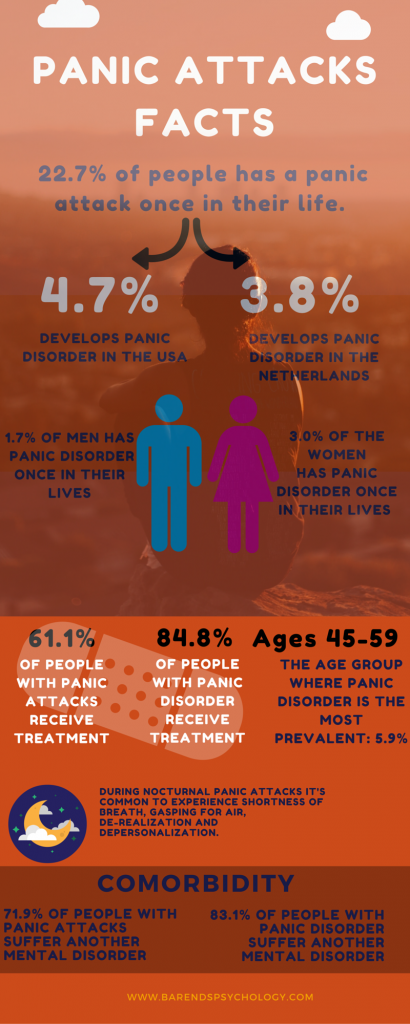 Here I am registering. Here is passport control. Here I am laying things out at customs. And here - wow - I'm in the green corridor. It made me laugh that this is technically a "nowhere" zone. I prepared myself for the worst: "Land the plane, call the paramedics" . But - as is almost always the case - my catastrophe was overdone. Yes, I was shocked, yes, I felt anxious. But all this is at the level of tolerable. I think it was largely because the people I loved met me in another country.
Here I am registering. Here is passport control. Here I am laying things out at customs. And here - wow - I'm in the green corridor. It made me laugh that this is technically a "nowhere" zone. I prepared myself for the worst: "Land the plane, call the paramedics" . But - as is almost always the case - my catastrophe was overdone. Yes, I was shocked, yes, I felt anxious. But all this is at the level of tolerable. I think it was largely because the people I loved met me in another country.
My worst recurring dream looks like this. I find myself in a foreign country where everyone speaks an incomprehensible language. I don’t know where to go, and when I try to ask passers-by, only a wheeze comes out of my mouth. Those around me shun me, and I sit down on the ground and cry as the waves of horror roll over me again and again. nine0003
In my dream I want to go home. The house is my apartment. My bed.
I remember a real incident from my childhood that reminds me of this dream. One day my mother took me to the market and quickly went ahead. I looked at the bright counters and lost sight of her. I started looking around, I felt dizzy, I wanted to call my mother, but for some reason I became afraid and ashamed to open my mouth. An unforgettable feeling in the worst sense of the word: a five-year-old child lost in the whirlwind of the market. When my mother saw me in the crowd, she pulled off her jacket by the sleeve and loudly, harshly scolded me. So she expressed fear. nine0003
One day my mother took me to the market and quickly went ahead. I looked at the bright counters and lost sight of her. I started looking around, I felt dizzy, I wanted to call my mother, but for some reason I became afraid and ashamed to open my mouth. An unforgettable feeling in the worst sense of the word: a five-year-old child lost in the whirlwind of the market. When my mother saw me in the crowd, she pulled off her jacket by the sleeve and loudly, harshly scolded me. So she expressed fear. nine0003
18:15. Prague
We sat down. I like it when people clap for the pilot, even if many people think it's ridiculous, they say, thank you for being alive. And I rejoice in this fact. Even in the cockpit it is very beautiful and the control of the aircraft seems to me some kind of impossible action. Pilots are cooler than gods - so why don't they clap?
End of the journey. Return flight
Three weeks have passed since I last opened this text. During this time, a lot has happened.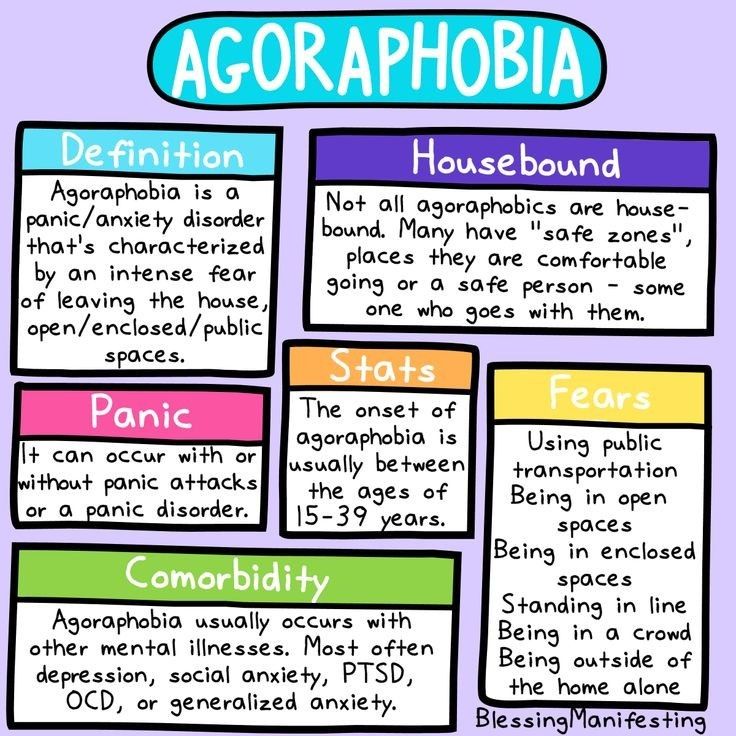 Outside the window - minus 54 degrees. I'm flying to Moscow. During takeoff, it seemed to me that something bad was going to happen. This is my fourth flight. In the past, I was very proud of the fact that I like air pockets and pitching. This time I was almost thrown into a panic because we failed in the second minute of takeoff. I felt dizzy, sweat appeared on my forehead, then the plane somehow spun and spun, and the magnificent clouds outside the window did not calm me down a bit. In one second, I imagined that I was losing control of myself: that I was starting to cry, I was hysterical, or I was silent like a fish. I'm not afraid that others will see it. This state itself is terrible: cold, I am locked in my own body and I can hardly speak. And people with their anxious faces scare even more. nine0003
Outside the window - minus 54 degrees. I'm flying to Moscow. During takeoff, it seemed to me that something bad was going to happen. This is my fourth flight. In the past, I was very proud of the fact that I like air pockets and pitching. This time I was almost thrown into a panic because we failed in the second minute of takeoff. I felt dizzy, sweat appeared on my forehead, then the plane somehow spun and spun, and the magnificent clouds outside the window did not calm me down a bit. In one second, I imagined that I was losing control of myself: that I was starting to cry, I was hysterical, or I was silent like a fish. I'm not afraid that others will see it. This state itself is terrible: cold, I am locked in my own body and I can hardly speak. And people with their anxious faces scare even more. nine0003
Do you know how I spent the last ten days? "I" is ironic. Lying at a friend's house because I broke my leg. What I feared most of all, not traveling until 25 years old, happened - I seriously injured myself in a foreign country. If my loved one and best friend were not in Prague, I don’t know what state my psyche would be in, even though I drink an antidepressant. On the seventh day I had a panic attack. Nightmares began to occur: now I can’t fly away from the country, here I am lying and silent, before my eyes there are terrible pictures, some figures with gouged out eyes. I plunge into my own panic, nothing distracts me, I feel insane and losing control. nine0013 And again this feeling of being locked in the body. Perhaps this is where agoraphobia and claustrophobia are similar: a deep-seated feeling of being unable to do anything. Moreover, the impossibility is not real, but internal, phobic.
If my loved one and best friend were not in Prague, I don’t know what state my psyche would be in, even though I drink an antidepressant. On the seventh day I had a panic attack. Nightmares began to occur: now I can’t fly away from the country, here I am lying and silent, before my eyes there are terrible pictures, some figures with gouged out eyes. I plunge into my own panic, nothing distracts me, I feel insane and losing control. nine0013 And again this feeling of being locked in the body. Perhaps this is where agoraphobia and claustrophobia are similar: a deep-seated feeling of being unable to do anything. Moreover, the impossibility is not real, but internal, phobic.
Adrian (Alyona's favorite person, to whom she flew to Prague. - Note ed. ) is sitting next to him in the plane and drawing. Outside the window is a bright sun and curly clouds. In the morning, my mother sent photos of the frozen trees of South Butovo and signed: "Beauty!" nine0003
All I dream about is to enter my clean house in the middle of an icy country, throw away my crutches, crawl under the covers and watch Homeland until I feel comfortable and at home again.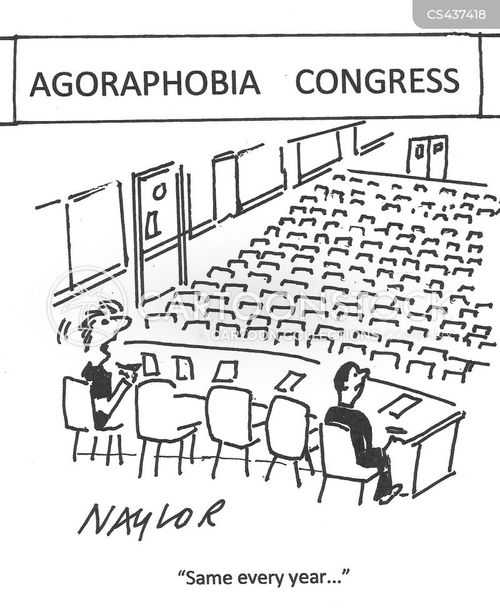
Is this progress? Definitely. Can you travel if you have agoraphobia? Of course. Whether you are 20, 30, 40 or 50 years old. It won't be easy, but the very fact that "it will be" will help to move away from the feeling of uncontrollable inevitability.
Can agoraphobia be overcome?
Agoraphobia can take on a progressive character, over time taking away more and more freedom from a person, compressing his comfort zone to the limits of an apartment. This can happen when a person unquestioningly obeys orders dictated by fear. Unfortunately, doctors' appointments in state medical institutions often have a disabling effect. The average psychoneurologist in a polyclinic or PND is most likely to prescribe phenazepam for anxiety disorder, which relieves panic attacks situationally, but in the long term causes addiction and becomes another form of avoidance. nine0003
Since agoraphobia is almost always a consequence of panic attacks and serves as a means of avoiding them, treatment should be aimed at coping with panic disorder.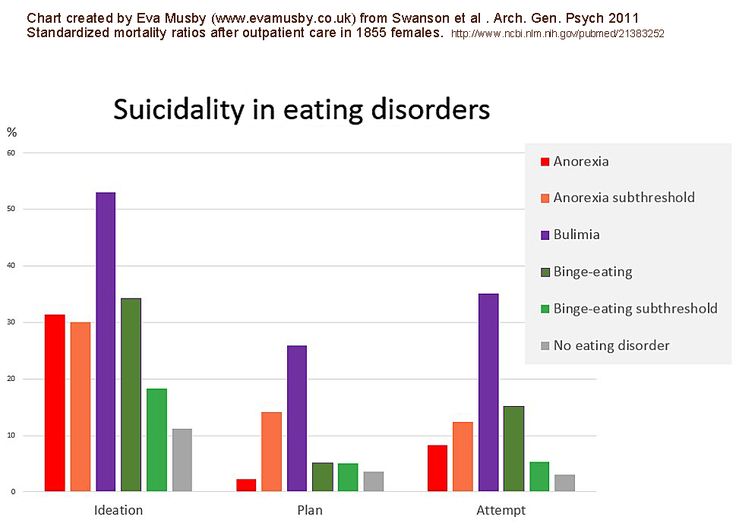 The first line of therapy, according to international recommendations (American Psychiatric Association and British National Health Service), should be one of the following methods: cognitive behavioral therapy or a course of taking an antidepressant of the SSRI group (selective serotonin reuptake inhibitors. - Note ed. ). Considering that cognitive behavioral therapy provides a more stable effect and requires only short-term work (8-12 sessions), we at the clinic recommend this option to most clients.
The first line of therapy, according to international recommendations (American Psychiatric Association and British National Health Service), should be one of the following methods: cognitive behavioral therapy or a course of taking an antidepressant of the SSRI group (selective serotonin reuptake inhibitors. - Note ed. ). Considering that cognitive behavioral therapy provides a more stable effect and requires only short-term work (8-12 sessions), we at the clinic recommend this option to most clients.
Let me tell you a little about the content of psychotherapy. Cognitive theory considers a panic attack primarily as a consequence of an incorrect assessment of bodily symptoms: "If my pulse is more than 130, then something is wrong with the heart"; “I feel dizzy, so I can lose consciousness”, “The world around me looks strange - I must be going crazy”, etc. At the first stage of work, we identify these erroneous interpretations and replace them with more rational ones, teaching the client basics of normal physiology.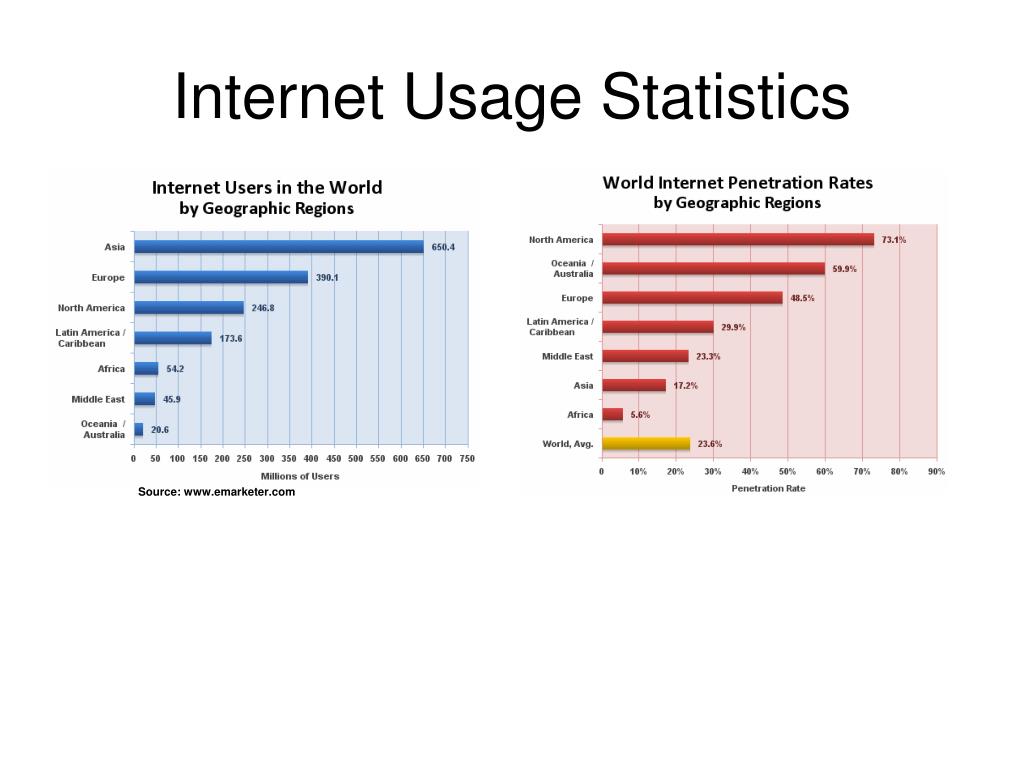 This allows you to neutralize a significant part of the experiences. nine0003
This allows you to neutralize a significant part of the experiences. nine0003
After some time, we encourage client to deliberately evoke fear and experience it in the safe environment of a therapy session. This is the key moment of treatment. A person who decides on exposure (intentional immersion in fear) forever changes his attitude towards panic attacks. He learns new knowledge: that unpleasant bodily symptoms are not a threat, that a panic attack should not be fought in any way, it does not need to be saved from it, because it passes by itself. And after that, we actually work with agoraphobia. After going through the first exposures, the client already understands that the panic attack is actually not as bad as it seemed before; at this stage, he is already ready to conduct sessions outside the office, in public places that frighten him - first accompanied by a therapist, then on his own. nine0003
I metaphorically imagine agoraphobia as some kind of evil entity that tries to stay in the host organism as long as possible with the help of threats and cunning like a parasite.
Since lies and manipulation are her main weapons, it is unlikely that she will be able to outmaneuver her with the help of any tricks: she reads your intentions three steps ahead. Only one remedy is effective: stubborn, systematic disobedience to her demands. You can make this task easier for yourself: find, for example, through some forum on anxiety disorders, a person in your city with a similar problem and train in independent exposure together. You can challenge each other with visiting various public places. Mutual face-to-face support from someone who knows firsthand about your difficulties is powerful medicine. nine0003
A loved one with agoraphobia needs to find a certain balance: on the one hand, give him enough emotional care, on the other hand, try to less indulge his avoidance. The gradual, jointly planned rejection of ubiquitous accompaniment and the transition to independent travel outside the home is an essential component of psychotherapy.
Agoraphobia and Panic Attack Test - Take it Online - How to Get Rid of Fear
Please answer the following questions:
Agoraphobia
1. Do you experience fear in one or more of the following situations, avoid them / or can you endure only with great effort, while experiencing intense fear:
Do you experience fear in one or more of the following situations, avoid them / or can you endure only with great effort, while experiencing intense fear:
be in a group of people
Yes Not
stand in line
Yes Not nine0003
be in public places, use public transport together with other people
Yes Not
visit cinemas, concerts
Yes Not
visit shopping centers, restaurants, hairdresser, doctor
Yes Not nine0003
leave the house or be outside the house alone
Yes Not
travel alone, e.g. by train, car, plane, public transport
Yes Not
2. Do you experience at least two of the following symptoms in the above situations:
palpitations, sensation of increased heart beat
Yes Not
increased perspiration
Yes Not
Yes Not
trembling of the whole body and/or limbs
Yes Not
dry mouth
Yes Not
Feeling short of breath or feeling of stopping breathing
Yes Not
chest compression
Yes Not nine0003
abdominal pain
Yes Not
nausea or vomiting
Yes Not
dizziness, feeling of weakness in the whole body
Yes Not
feeling of unreality of what is happening
Yes Not
feeling of "goosebumps" in the whole body or loss of sensation
Yes Not
3. Are you afraid:
Are you afraid:
loss of control over oneself and the situation
Yes Not nine0003
become insane/insane
Yes Not
die
Yes Not
suffocate
Yes Not
lose consciousness
Yes Not nine0003
internal "explode"
Yes Not
that you may lose control of your bowels, bladder, gag reflex
Yes Not
to be helpless?
Yes Not
nine0002 4. If you have to attend a restaurant, lecture, meeting, etc. Are you always looking for ways to escape from the premises?Yes Not
5. Do you get the impression that you are avoiding the situations described above more often?
Yes Not
6. Do you get the impression that because of your fears you are not all right with your psyche? nine0003
Yes Not
7. Does fear limit your private and public life?
Yes Not
8. Do you take medication, alcohol or anything else to get rid of your fears?
Yes Not
nine0002 9.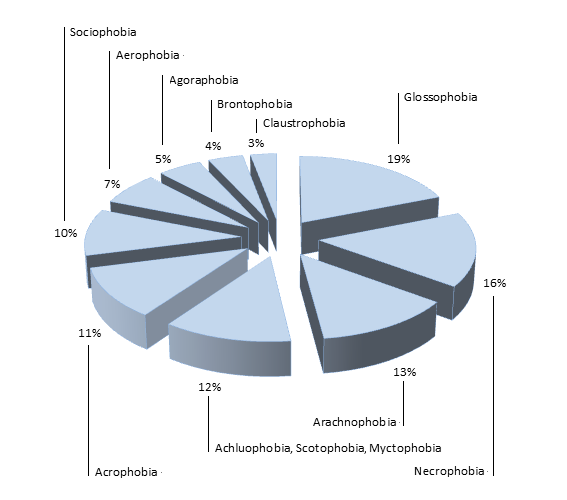 Does fear burden your life?
Does fear burden your life? Yes Not
10. Do you need to be accompanied by friends, relatives in the situations described above?
Yes Not
11. Do you often visit doctors in vain due to the physical symptoms described above?
Yes Not nine0003
12. Do you notice in yourself a craving for seclusion?
Yes Not
Transition to treatment
What is a panic attack? Why is it worth taking the panic attack test ?
Panic attacks are the sudden onset of a feeling of dread, to the point of terror, accompanied by intense physical sensations.
When panicking, they can have different manifestations and mimic severe somatic diseases:
-
- freezing flushes of cold and waves of heat;
- fear of death;
- suffocation;
- heartbeat
- feeling of unreality of what is happening;
- numbness of hands and feet;
- burning in the chest and sensation of a lump in the throat;
- profuse sweating;
- dizziness;
- vomiting, nausea, upset stomach;
- strong fluctuations in blood pressure.

Panic attack, test , which can be taken online below, often begins with a rapid heartbeat and a feeling of fear of death. At first, a person believes that he has a dangerous somatic disease, for example, myocardial infarction, as well as a suspicion that something irreparable has happened to the psyche, that the person has gone crazy, and can break right on the spot screaming and will be immediately hospitalized in a psychiatric hospital .Then the patient is examined by a cardiologist, pulmonologist, neuropathologist, gastroenterologist, family doctor. With luck, the diagnosis will be made immediately after the first panic attack. If you are not lucky, then the person will receive a diagnosis of some kind of vegetovascular dystonia, suspiciousness, chronic fatigue. nine0003
By taking the Panic Disorder and Agoraphobia Test, you will be able to immediately recognize the symptoms, you will be able to get rid of the unknown right now and find out what your disorder is called and how it is properly treated.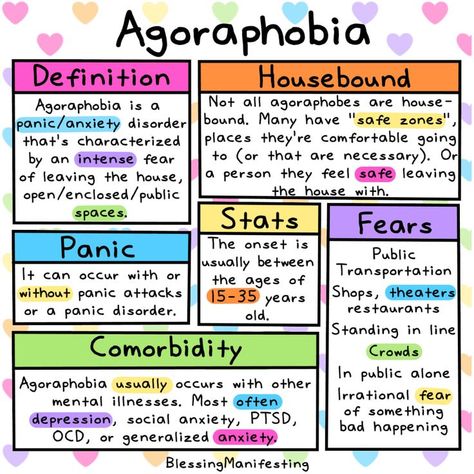
Today, psychologists compare the experience of a panic attack as a severe traumatization of the level of post-traumatic stress, even the very memory of which causes fear. This is due to the power of horror that accompanies a panic attack, a person literally survived a meeting with death. nine0003
In all cases it is difficult for the patient to believe that he has a fear disorder and that his life is safe. And the nightmare that he experienced did not and will not cause him any harm in the future.
After a powerful stress, the body is in constant expectation of a repetition of this horror, and the expectation itself causes small releases of stress mediators - the hormones adrenaline, norepinephrine, cortisol. A so-called vicious circle is formed - the fear of waiting for a panic attack makes the body live in a mode of high alert, eternal anxiety. A small load is enough to cause a panic attack as a form of protection. nine0381 Test for detecting panic attacks will help you identify your anxiety manifestations and distinguish a panic attack from other anxiety conditions, decide on treatment and get started with the first free lesson on Psycholounge. net, where you will learn everything about fears and immediately alleviate your condition.
net, where you will learn everything about fears and immediately alleviate your condition.
What is agoraphobia : test and features of the disorder
Panic attacks can occur at any time of the day, after sleepless nights and overload at work, as well as in a state of complete rest. They also tend to be combined with visual objects, such as closed and open spaces filled with people and completely empty. This disorder is called agoraphobia with panic attacks. Less common are "pure" agoraphobia, but the principle of treatment of these two forms is the same. You will see their diversity in online test for agoraphobia.
What happens in agoraphobia? The sensors of the limbic system—sight, hearing, smell, touch, and internal controllers—at some point override the precise defense system, perceiving, for example, a slight change in breathing in a store as an alarm. Since the limbic system has its own logic, it remembers the situation in an enclosed space filled with people as life-threatening.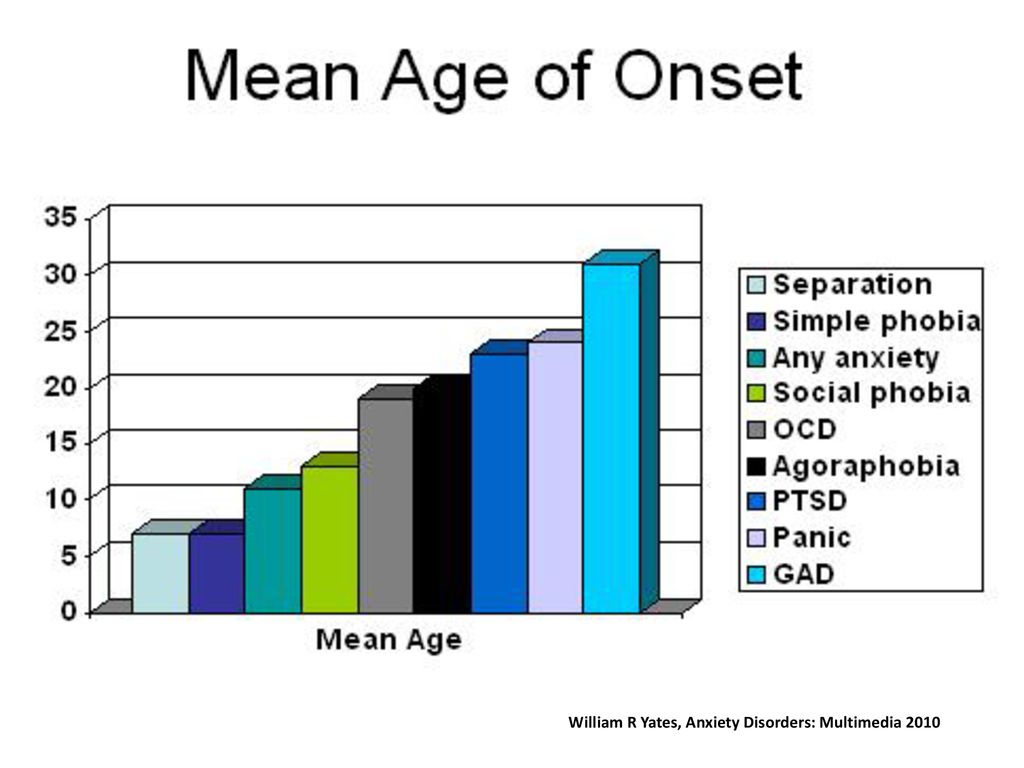 Further, agoraphobia spreads to all kinds of closed spaces - cinemas, auditoriums, elevators, transport, bazaars, then just to spaces and just to crowds of people. nine0003
Further, agoraphobia spreads to all kinds of closed spaces - cinemas, auditoriums, elevators, transport, bazaars, then just to spaces and just to crowds of people. nine0003
According to statistics, five out of a hundred people suffer from complex forms of this disorder, while at the same time, every eighth suffers from a mild form. The agoraphobia test will help you identify your symptoms. The reaction of fear spreads in waves, capturing more and more new areas of the brain, reinforcing new knowledge about danger, practically cementing them.
Fighting and defeating agoraphobia is not difficult, you will see for yourself by completing the first lesson and properly preparing in the cycle “ Treatment of agoraphobia with and without panic attacks to fear exposure. From the very first free lesson, you will understand how you can retrain your defense system, explaining to it that you are completely safe and do not need its increased care.
The symptoms of agoraphobia are no different from the physical manifestations of other forms of fear:
-
- occurrence of an attack of fear in a certain place;
- in order not to experience the horror of fear, a person begins to avoid the place where it arises; nine0392
- people exclude shops, transport, visits to the doctor, school, university, hiking in the mountains, independent travel and so on from their lives;
- as a result, life becomes complex and loses its quality;
- people delegate their daily tasks to loved ones who also become victims of agoraphobia.