Silenor vs trazodone
A Complete Guide to Doxepin(Silenor) For Sleep
Dealing with insomnia can be a stressful, frustrating experience. Thankfully, a range of safe and effective medications are available to help you fall asleep easier, stay asleep for longer and feel better after waking.
One of these medications is doxepin. Originally developed as a treatment for major depressive disorder, doxepin (at much lower doses) is also highly effective at treating sleep disorders such as insomnia.
If you find it difficult to stay asleep, frequently wake up in the middle of the night or just don’t feel refreshed after waking up in the morning, doxepin may be able to help you maintain better sleep habits and enjoy a higher quality of life.
Below, we’ve explained what doxepin is and how it works as a medication for sleep. We’ve also looked at the science behind doxepin, as well as how it compares to other common medications prescribed to treat insomnia and other sleep issues.
What Is Doxepin?
Doxepin is a tricyclic antidepressant medication. It was first approved in the 1960s by the FDA as a treatment for depression.
After extensive scientific studies showed that it was also effective at treating sleep disorders, the FDA approved doxepin in 2010 as a treatment for insomnia.
As well as depression and insomnia, doxepin is also used to treat certain anxiety disorders and skin conditions. It’s most commonly used in tablet form, with topical doxepin cream used to treat skin rashes and disorders such as hives, atopic dermatitis and lichen simplex chronicus.
Doxepin is available as a generic medication. It’s sold under a wide range of brand names in the United States and abroad. You may have seen doxepin for sale under brand names like Silenor®, Sinequan®, Quitaxon® and Aponal®.
In the United States, Silenor is the low-dose version of doxepin that’s typically used for insomnia.
How Doxepin Works
As a tricyclic antidepressant, doxepin works by affecting the way your brain absorbs and deals with certain chemicals, such as norepinephrine and serotonin.
Doxepin induces drowsiness by affecting the body’s histamine receptors, which play a major role in managing the sleep-wake cycle.
More specifically, doxepin is an antagonist of the h2 receptor, which is responsible for mediating your feelings of wakefulness and arousal. By binding to the h2 receptor, doxepin limits the effects of histamine in the body, causing users to feel drowsy and promoting sleep.
Doxepin for Sleep: The Science
Studies of doxepin show that it can improve sleep quality in people with insomnia when taken at a low dose, with relatively few side effects compared to other sleep medications.
Several studies of doxepin show that it can increase total sleep time and reduce the risk of waking up during the night in people with insomnia.
For example, a 2013 scientific review of doxepin, which involved analysis of several large-scale studies, found that low doses of doxepin were effective at managing both chronic and transient (short-term, non-recurring) insomnia.
This review also noted that doxepin was a “safe and non-habit forming option” for treating sleep difficulties.
Another scientific review from 2014 found that 3mg and 6mg doses of doxepin helped to reduce waking after sleep onset and increase the total amount of time spent asleep in older adults with difficulty sleeping.
Another systematic review, this time from 2015, looked at nine placebo-controlled doxepin trials and concluded that that low-dose doxepin produced a small to medium effect for sleep duration and sleep maintenance when compared to a non-therapeutic placebo.
Numerous smaller studies have also found that doxepin is effective at treating insomnia. In one study from 2007, researchers found that even very small doses of doxepin (1mg, taken prior to sleep) helped to improve sleep in people with chronic insomnia.
In short, doxepin’s effectiveness as a sleep medication is backed up by a sizable body of evidence, both from large and small-scale studies.![]()
Anonymous Support Groups
Having trouble sleeping? Try a free support group session online and learn effective tools and strategies
Doxepin and Next-Day Drowsiness
Many sleeping pills, including prescription medications used to prevent insomnia, are associated with early-morning drowsiness and headaches — symptoms that are occasionally referred to as a sleeping pill “hangover.”
These side effects are common with older sleeping pills and can range from a minor annoyance to quite a serious issue.
For example, the FDA has urged health care professionals to caution people who are prescribed zolpidem (Ambien®) about the risk of next-morning impairment, which could affect activities such as driving or operating machinery.
Many benzodiazepines used to treat insomnia, such as alprazolam (Xanax®), are also linked to next-morning impairment and hangover-like side effects.
Doxepin’s effects as a sleep medication last for about seven hours, meaning you’ll feel tired and drowsy during this time after taking the medication. Because of this, you shouldn’t use doxepin if you need to wake up after less than eight hours of sleep.
Because of this, you shouldn’t use doxepin if you need to wake up after less than eight hours of sleep.
However, most studies of doxepin show that after the medication’s effective period is finished, it typically does not cause the next-morning drowsiness or other common sleeping pill “hangover” symptoms that are associated with other insomnia medications.
In the 2013 review we mentioned above, the researchers noted that doxepin “does not cause daytime sedation (no next-day sedation).” Likewise, the 2015 review concluded that there was “no significant next-day residual effect” associated with low-dose doxepin use.
The 2007 study linked above also concluded that doxepin had “no significant hangover/next-day residual effects.”
Put simply, doxepin doesn’t appear to cause significant next-day drowsiness or hangover effects that are common with older sleep medications, provided it’s used at the recommended dose and enough time is allowed to pass before waking up.
Doxepin vs. Zolpidem (Ambien)
As a popular sleeping medication, doxepin is often compared to zolpidem, the active ingredient in Ambien.
Although doxepin and zolpidem are both used to treat insomnia, there are a few key differences between these two medications, from how they work within the body to the effects they have on sleep and alertness. There’s also a significant difference in side effects.
Some of the most noticeable differences between doxepin and zolpidem are the ways in which each drug affects sleep latency, total sleep time and next-morning alertness.
Sleep Latency (Time Required to Fall Asleep)
Zolpidem works by reducing the amount of time required to fall asleep. In short, it induces sleep, allowing you to fall asleep faster. This makes it an effective treatment if you have difficulty falling asleep and often spend a long time awake in bed before dozing off.
For example, an eight-month study of people with insomnia found that zolpidem reduced sleep latency (the amount of time it takes to fall asleep). An older study from 1991 also reached the same conclusion, noting that zolpidem decreased time awake before persistent sleep.
An older study from 1991 also reached the same conclusion, noting that zolpidem decreased time awake before persistent sleep.
Because of this effect, zolpidem is a popular option for treating insomnia in people who find it difficult to fall asleep in a normal amount of time.
Doxepin, in contrast, is more effective at helping you stay asleep and sleep for longer than it is at helping you fall asleep quickly.
Most studies, including several of the reviews mentioned above, note that doxepin doesn’t have a significant effect on sleep latency. In this 2014 review, the researchers noted that doxepin did not cause any improvement in latency to persistent sleep compared to a placebo.
However, some studies have found that doxepin does improve sleep latency in people affected by insomnia. For example, this study from 2010 found that doxepin improved both sleep quality and latency to sleep onset (time to fall asleep) in older adults with chronic primary insomnia.
In short, while there’s some evidence that doxepin may reduce sleep latency, it doesn’t appear to be as effective for reducing the amount of time required to fall asleep as zolpidem.
Total Sleep Time
Zolpidem and doxepin both increase total sleep time, meaning you may sleep for longer after using either medication.
In the eight-month study listed above of zolpidem involving 91 people with insomnia, researchers found that nightly use of zolpidem resulted in an increase in overall sleep time.
Studies of doxepin have produced similar results. This 2014 review concluded that doxepin can improve sleep duration in the last third of the night, while this 2013 review concluded that even mild doses of doxepin are effective at improving total sleep time.
Put simply, zolpidem and doxepin are both effective at increasing total sleep time in people with insomnia.
Next-Day Drowsiness
As we mentioned above, studies of doxepin show that it usually doesn’t cause any noticeable next-day drowsiness. Doxepin’s effects on alertness and energy tend to last for seven to eight hours, after which the medication wears off with few or no lingering effects the next day.
Zolpidem, on the other hand, is often associated with drowsiness, tiredness and a general lack of alertness that can last into the next morning after it’s used.
The FDA label for Ambien, the most widely-used drug containing zolpidem, warns of the risk of feeling drowsy in the morning after using this medication. It also warns against driving or doing other dangerous activities after using zolpidem unless fully awake.
If you suffer from insomnia and need to be highly alert early in the morning, such as to drive to your workplace or operate machinery, doxepin (or, for mild insomnia, a non-prescription sleep aid such as melatonin) may be a more suitable treatment for you.
Late-Night Activities and Memory Loss
Several hypnotic sleep medications, including zolpidem, are associated with unusual nighttime behavior. The FDA label for Ambien also mentions that “Complex sleep behaviors including sleep-walking, sleep-driving and engaging in other activities while not fully awake may occur following use of AMBIEN”, often with the user having no memory of the activity occurring.
The label specifically mentions driving a car (“sleep-driving”), making and eating food, talking on the phone, having sex and sleep-walking as late-night activities reported by Ambien users.
If you use zolpidem for insomnia and notice any unusual nighttime behavior, you should stop the medication immediately and discuss this with your healthcare provider as soon as possible.
As a sedative, doxepin has the potential to affect your level of alertness, meaning you may not be fully aware of your behavior during the nighttime.
However, because doxepin doesn’t doesn’t affect the GABA-A receptor, it has shown no association with abuse or addiction, withdrawal, or the complex sleep behaviors as seen in medications like zolpidem.
Doxepin Side Effects
Used for sleep conditions such as insomnia at the prescribed dose, doxepin is a safe, effective medication that’s less likely to cause side effects than many other sleeping pills.
Like other medications, doxepin has the potential to cause certain side effects. It’s also possible for doxepin to interact with other medications.
It’s also possible for doxepin to interact with other medications.
Before discussing specific side effects of doxepin, it’s important to note that doxepin is available in a range of dosages to treat different conditions.
For example, doxepin is prescribed for major depressive disorder at dosages ranging from 25mg to 300mg per day. Used for insomnia and other sleep issues, it’s prescribed at a much lower dose, typically in the 3mg to 6mg range.
This means that data on side effects for high doses of doxepin prescribed for major depressive disorder, anxiety and other conditions may not be fully comparable if you use doxepin to treat insomnia.
Used for insomnia at a dose of 3 to 6mg, the most common side effects of doxepin are drowsiness and sedation, upper respiratory tract infection and nausea. In trials of doxepin, a small percentage of users reported nausea, hypertension and gastroenteritis.
Taken at a higher dosage, doxepin may cause other side effects, including several serious ones. We’ve listed these and provided more information in our complete guide to doxepin side effects.
We’ve listed these and provided more information in our complete guide to doxepin side effects.
Although abnormal nighttime behavior is not common with doxepin, hypnotic medications have the potential to lead to behaviors such as sleep-walking and “sleep-driving.” You have a higher risk of doing these activities if you drink alcohol or combine doxepin with other medications.
If you engage in any abnormal nighttime behavior while using doxepin, you should stop taking the medication immediately and contact your doctor as soon as possible.
Like other tricyclic antidepressants, it’s possible to overdose on doxepin. If you or someone you know may have taken more than the recommended dosage of doxepin, call 911 or the national toll-free Poison Help hotline (1-800-222-1222) as soon as possible.
In Conclusion
Doxepin is a safe, easy-to-use and effective medication for treating insomnia. Studies show that it can improve general sleep quality and increase the total amount of time people with insomnia spend asleep each night.
However, doxepin doesn’t appear to have such a strong effect on sleep latency, meaning it may not help you fall asleep faster if you’re prone to spending a long time awake late at night.
Unlike many other sleeping pills, doxepin doesn’t appear to cause early-morning drowsiness or any hangover-like side effects. This may make it a better option than other sleep medications if you need to be fully alert early in the morning after waking up.
Learn More About Getting Better Sleep
Considering doxepin? Our complete guide to prescription sleeping pills compared doxepin to a range of other medications prescribed to treat insomnia. You can also learn more about treating insomnia in our detailed guide to why insomnia happens and how to treat it.
Sleep Gummy Vitamins
Ward off restless nights with Melatonin Sleep Gummies.
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Top trazodone alternatives and how to switch your Rx
Trazodone doesn't work for everyone. Mirtazapine, doxepin, amitriptyline, paroxetine, and bupropion are some trazodone alternatives. Get the full list here.
Compare trazodone alternatives | Mirtazapine | Doxepin | Amitriptyline | Paroxetine | Bupropion | Natural alternatives | How to switch meds
Trazodone hydrochloride (brand names Desyrel and Oleptro) is a commonly used medication to treat major depressive disorder (MDD). It can help improve mood, increase energy level, decrease anxiety, and reduce insomnia associated with depression. Trazodone is a unique antidepressant as it is both a serotonin antagonist and reuptake inhibitor and a 5HT2 receptor antagonist.
As a drug that doesn’t belong to any of the main classes of antidepressants, trazodone may be referred to as a serotonin modulator. It works to increase the amount of serotonin, which is an important neurotransmitter (chemical messenger). Increased serotonin in the central nervous system (CNS) can stabilize mood, happiness, and overall well-being. Additionally, trazodone blocks histamine h2 receptors (similar to an antihistamine), which can be associated with enhanced sleep and potential for daytime drowsiness. These unique properties have led to many off-label uses of trazodone including sleep disorders, anxiety, Alzheimer disease, substance abuse, bulimia, and fibromyalgia.
It works to increase the amount of serotonin, which is an important neurotransmitter (chemical messenger). Increased serotonin in the central nervous system (CNS) can stabilize mood, happiness, and overall well-being. Additionally, trazodone blocks histamine h2 receptors (similar to an antihistamine), which can be associated with enhanced sleep and potential for daytime drowsiness. These unique properties have led to many off-label uses of trazodone including sleep disorders, anxiety, Alzheimer disease, substance abuse, bulimia, and fibromyalgia.
Although clinical trial data is limited, trazodone is often used at lower doses as a sedative to help with sleep in people with depression either alone or in combination with other antidepressants. Trazodone is available as a tablet and is typically taken one to three times daily for depression. Clinical studies have shown trazodone to be comparable in treating depression to other antidepressant medications including tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs). Trazodone avoids the issue of sexual dysfunction, insomnia, and anxiety that can be common with SSRI and SNRI therapy.
Trazodone avoids the issue of sexual dysfunction, insomnia, and anxiety that can be common with SSRI and SNRI therapy.
While an effective treatment for some people, trazodone may not be the best or safest option for all people managing depression. Common side effects of trazodone include sedation, dizziness, dry mouth, and nausea. Serious side effects of trazodone include priapism (painful, prolonged erection), orthostatic hypotension (sudden drop in blood pressure), heart arrhythmias, serotonin syndrome, and suicidal thoughts. Trazodone has a black box warning (highest FDA safety-related warning for serious or life-threatening adverse effects) for an increased risk of suicidal thoughts and behaviors in children and young adults.
Due to the way the liver and kidney break down trazodone, special care is necessary for people with severe liver problems and severe kidney impairment. Published literature on trazodone use in pregnant women has not found any associated risks of miscarriage, major congenital disabilities, and adverse maternal or fetal outcomes. Healthcare providers should consider the risk of untreated depression if planning to discontinue or change antidepressant treatment while a person is pregnant. In breastfeeding, caution should be used as small amounts of trazodone have been found in breast milk.
Healthcare providers should consider the risk of untreated depression if planning to discontinue or change antidepressant treatment while a person is pregnant. In breastfeeding, caution should be used as small amounts of trazodone have been found in breast milk.
What can I take in place of trazodone?
There are other options available to treat depression that do not improve with trazodone and other options for those who have both depression and sleep problems. These alternative prescription medications include other serotonin modulators, atypical antidepressants, selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs). These options may be more suitable for certain individuals due to their different uses, side effect profiles, and dosages. If pricing is a factor in finding an alternative to trazodone, a SingleCare prescription discount card may help reduce prescription costs of up to 80% at participating pharmacies.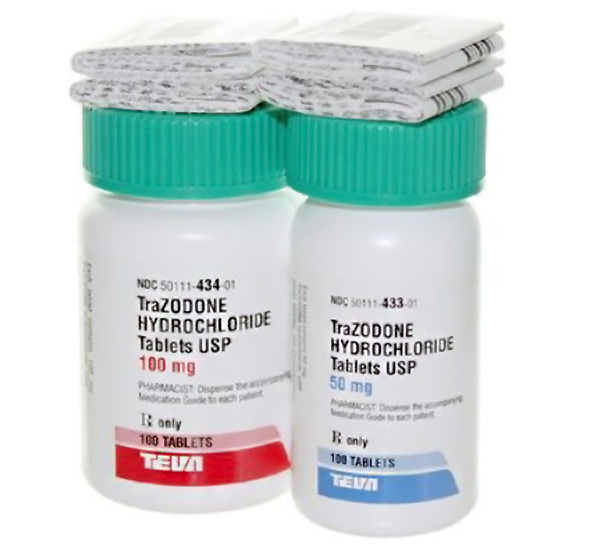 Switching from one antidepressant to another can be common in order to find the best fit for the person. A study of a claims database analysis involving 134,287 patients treated with antidepressants determined 23.2% had a treatment change including 9.5% with a switch in antidepressants and 9.1% with an addition of combination therapy.
Switching from one antidepressant to another can be common in order to find the best fit for the person. A study of a claims database analysis involving 134,287 patients treated with antidepressants determined 23.2% had a treatment change including 9.5% with a switch in antidepressants and 9.1% with an addition of combination therapy.
RELATED: What you should know before switching antidepressants
Other alternatives to trazodone:
- Desipramine
- Desvenlafaxine
- Deuloxetine
- Fluoxetine
- Fluvoxamine
- Imipramine
- Levomilnacipran
- Nortriptyline
- Phenelzine
- Tranylcypromine
RELATED: Depression Treatments and Medications
Top 5 trazodone alternatives
The following are some of the most common alternatives to trazodone.
1. Mirtazapine
Mirtazapine is an atypical antidepressant and has a unique way of working. Mirtazapine is an alpha-2 adrenergic antagonist and serotonin 5-HT2 receptor antagonist. Like trazodone, mirtazapine is used to treat major depressive disorder and can cause sedation. Due to mirtazapine’s sleep-promoting effects, it may be an alternative to trazodone for people managing both depression and sleep problems. A literature search that analyzed studies involving mirtazapine in depressed patients that specifically assessed sleep found mirtazapine produced significant improvement in sleep efficiency, total sleep time, and sleep quality. Along with sedation, common side effects of mirtazapine include increased appetite, weight gain, and dizziness. Mirtazapine has a starting dose of 15 to 45 mg tablet by mouth at bedtime.
2. Doxepin
Doxepin belongs to a group of antidepressants called tricyclic antidepressants (TCAs). Doxepin can be used for depression, anxiety, and insomnia. Due to sedating effects, TCAs like doxepin can be used in people with depression who have insomnia. However, TCAs have more side effects to be aware of including dry mouth, orthostatic hypotension, constipation, sexual dysfunction, nausea, dizziness, blurred vision, increased appetite, and weight gain. For depression or anxiety, doxepin is dosed as a 150 to 300 mg capsule by mouth at bedtime.
Due to sedating effects, TCAs like doxepin can be used in people with depression who have insomnia. However, TCAs have more side effects to be aware of including dry mouth, orthostatic hypotension, constipation, sexual dysfunction, nausea, dizziness, blurred vision, increased appetite, and weight gain. For depression or anxiety, doxepin is dosed as a 150 to 300 mg capsule by mouth at bedtime.
3. Amitriptyline
Amitriptyline belongs to a group of antidepressants called tricyclic antidepressants (TCAs). Amitriptyline can be used to treat depression, and similar to the TCA doxepin, it can be used in people with depression who have insomnia due to sedating effects. Amitriptyline, like most TCAs, produces additional side effects such as dry mouth, orthostatic hypotension, constipation, blurred vision, and nausea to name a few.. Amitriptyline is dosed as a 50 to 150 mg tablet by mouth at bedtime.
4. Paroxetine
Paroxetine belongs to a common group of antidepressants called selective serotonin reuptake inhibitors (SSRIs). Along with treating major depressive disorder, paroxetine can be used for panic disorder, social anxiety disorder, and premenstrual dysphoric disorder. SSRIs tend to have similar side effects, however nausea and sedation may be more likely to occur with paroxetine. Like trazodone, paroxetine may help with sleep along with treating depression. Other side effects of paroxetine include sexual dysfunction, weight gain, dizziness, and headache. For depression, paroxetine is dosed as either a 20 to 50 mg tablet by mouth once daily or a 25 to 62.5 mg extended-release tablet by mouth once daily.
Along with treating major depressive disorder, paroxetine can be used for panic disorder, social anxiety disorder, and premenstrual dysphoric disorder. SSRIs tend to have similar side effects, however nausea and sedation may be more likely to occur with paroxetine. Like trazodone, paroxetine may help with sleep along with treating depression. Other side effects of paroxetine include sexual dysfunction, weight gain, dizziness, and headache. For depression, paroxetine is dosed as either a 20 to 50 mg tablet by mouth once daily or a 25 to 62.5 mg extended-release tablet by mouth once daily.
5. Bupropion
Bupropion is an atypical antidepressant and has a unique way of working. Bupropion is an aminoketone antidepressant. A literature review found that bupropion has a unique sleep profile, which may be well-suited for people suffering from depression. The review found that bupropion was not associated with daytime sleepiness and that sleep disturbance occurred at a low rate compared to other modern reuptake inhibitors. Unlike other antidepressants, the review found the sleep profile for bupropion does not suppress REM sleep. Common side effects of bupropion include agitation, dry mouth, constipation, headache/migraine, nausea/vomiting, and dizziness. Bupropion does have an increased seizure risk and should be discontinued if seizures occur. Bupropion is dosed as a 100 mg tablet by mouth three times daily.
Unlike other antidepressants, the review found the sleep profile for bupropion does not suppress REM sleep. Common side effects of bupropion include agitation, dry mouth, constipation, headache/migraine, nausea/vomiting, and dizziness. Bupropion does have an increased seizure risk and should be discontinued if seizures occur. Bupropion is dosed as a 100 mg tablet by mouth three times daily.
Natural alternatives to trazodone
Alternative remedies for trazodone include certain supplements, lifestyle changes, and diet modifications to help improve mood and overall well-being. Some of these remedies include regular exercise, meditation, cognitive behavioral therapy, and the Mediterranean diet.
Both high-intensity exercise and consistent low-intensity exercise can have a positive impact on brain function improving how people feel. High-intensity exercise releases the body’s feel-good chemicals called endorphins, while low-intensity exercise promotes the release of proteins (neurotrophic or growth factors) which cause nerve cells to grow and make new connections.
RELATED: 6 health conditions that exercise prevents
Meditation can influence self-awareness and may ease depression by momentarily stopping the constant worries and fears that can fuel it. For more sudden symptoms such as anxiety, the 3-3-3- rule may be beneficial. This tactic involves looking around and naming three things one sees, naming three sounds one hears, and moving three body parts such as an ankle, finger, or arm. Cognitive behavioral therapy can be used in mental health conditions like depression, anxiety, substance use, and phobias. This form of therapy can help identify the thinking patterns that cause distress to manage overwhelming emotions and unhelpful behaviors.
The Mediterranean diet involves eating plenty of fruits, vegetables, bread and other grains, potatoes, beans, nuts, and seeds. This diet includes olive oil as a primary fat source and low to moderate amounts of dairy products, eggs, fish, and poultry. A study published in 2020 found that eating a Mediterranean diet along with fish oil supplementation in people self-reporting depressive symptoms showed improved mental health after 6 months. In addition, reduced depression was significantly linked with adherence to the Mediterranean diet, more consumption of nuts, and more consumption of vegetables.
In addition, reduced depression was significantly linked with adherence to the Mediterranean diet, more consumption of nuts, and more consumption of vegetables.
Since trazodone is often used to help with sleep problems in people treating depression, over-the-counter sleep aids are available as alternatives. Melatonin is a natural hormone in the body that promotes sleep that is available as a supplement in dosage forms such as tablets, gummies, and liquid.
RELATED: A melatonin dosage guide: How much do I need to sleep?
How to switch to a trazodone alternative
1. Discuss all health conditions with a healthcare provider
Before switching from trazodone to an alternative, it’s important that the prescribing doctor is aware of all medical conditions. Some alternatives should be used with caution or avoided with certain medical conditions. For example, TCAs like amitriptyline and doxepin can potentially cause damage to the heart and should be avoided in people with heart disease. Additionally, the alternative bupropion should not be used in people with seizure disorders.
Additionally, the alternative bupropion should not be used in people with seizure disorders.
2. Do not suddenly stop taking trazodone without medical advice
Only stop taking trazodone if the prescribing doctor has been consulted and decided stopping the medication is safe. If trazodone is stopped suddenly, there may be sudden withdrawal symptoms or worsening depression symptoms. It’s important for a therapy plan to be established prior to stopping trazodone suddenly. The trazodone dose should be gradually reduced rather than stopping abruptly whenever possible.
3. Discuss all prescription and over-the-counter medications with a healthcare provider
Before switching from trazodone to an alternative, it’s important that the prescribing doctor has reviewed a patient’s medication list including prescription drugs and over-the-counter meds. Some alternatives have dangerous drug interactions that must be avoided.
4. Continue to monitor depression symptoms
It’s important for people treating depression to keep track of their symptoms and behavior over time. Self-monitoring can be done with methods such as recording feelings through journaling or smartphone applications. This information can be shared with the prescribing doctor to help support and reinforce positive change in mental health and to counteract negative developments.
Self-monitoring can be done with methods such as recording feelings through journaling or smartphone applications. This information can be shared with the prescribing doctor to help support and reinforce positive change in mental health and to counteract negative developments.
Antidepressants: Methods of Use, Common Brands and Safety Information - Product Information
Home >> Product Information >> Antidepressants: Methods of Use, Common Brands, and Safety Information
Information about the drug
List of antidepressants | What are antidepressants? | How do they work | Uses | Types | Who can take antidepressants? | Security | Side effects | Expenses
Depression is a very common mood disorder that can cause severe symptoms if left untreated. There are different types of depression, but each can affect how you feel and how you relate to daily activities such as sleep, work, or food.
Depression is diagnosed when you experience certain symptoms most of the day every day for two weeks.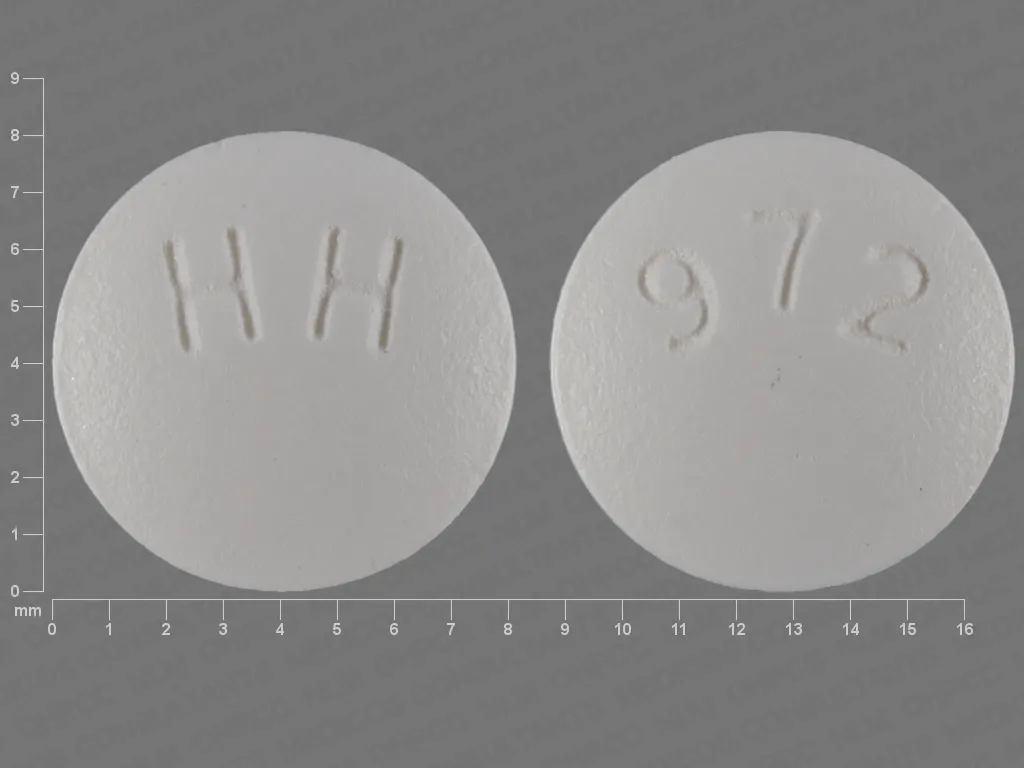 Symptoms include a persistent sad or anxious mood, feelings of hopelessness, guilt, or worthlessness, loss of interest in hobbies, or decreased energy. There are other symptoms of depression, and your doctor or psychiatrist can tell you more if they suspect you are depressed.
Symptoms include a persistent sad or anxious mood, feelings of hopelessness, guilt, or worthlessness, loss of interest in hobbies, or decreased energy. There are other symptoms of depression, and your doctor or psychiatrist can tell you more if they suspect you are depressed.
Depression is a treatable disorder. Treatment options include psychotherapy, exercise, medication, or a combination of these. In more severe cases, electroconvulsive therapy (ECT) and other types of brain stimulation may be helpful. In terms of drug treatment options, antidepressants are a general class of medications used to treat depression. There are many subtypes of antidepressants, and we will discuss their different properties, common brand names, and their safety.
 99 US dollars for 30 tablets, 5 mg
99 US dollars for 30 tablets, 5 mg  12 for 30 20mg tablets
12 for 30 20mg tablets Other antidepressants
- Azendine (Amoxapine)
- Rexulti (Brexipiprazole)
- Anatrannil (clomipromin)
- Poddazhi (dapoxetine)
- Norpramine (dezipramine)
- SPRAVATO (Esketamine)
- Varicose extensions (hepyrine)
- Tofranille (Imipramine)
- MARPARN (LEA) Metapholin (Izocarboxysid) 9020 Fetzima (levomilnacipran)
- Ludiomil (maprotiline)
- Remeron (mirtazapine)
- Serzone (nefazodone)
- Pamelor (nortriptyline)
- Zyprexa (olanzapine)
- Nardil (Fenelzin)
- Vivactil (Pritriptilin)
- Serokvel (Quetiapin)
- Eldepril (Selegilin)
- Parnat (Tranilsipromin)
- Surmontil (Trimipramine)
What is antidepressants?
Antidepressants are a large class of drugs prescribed to treat various types of depressive disorders. These may include major depression, persistent depressive disorder, postpartum depression, psychotic depression, seasonal affective disorder, and bipolar disorder.
These may include major depression, persistent depressive disorder, postpartum depression, psychotic depression, seasonal affective disorder, and bipolar disorder.
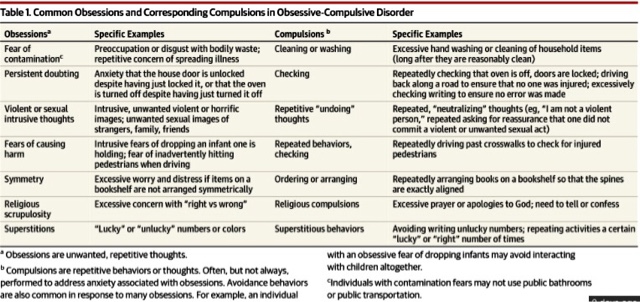
There are different types of antidepressants, and each of them alleviates the symptoms of depression in a different way. Many antidepressants have more than one approved indication, as some may help treat other disorders, including anxiety, panic disorder, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and premature ejaculation.
How do antidepressants work?
Broadly speaking, antidepressants work by changing various aspects of the neurotransmitters that affect mood. Each class of antidepressants works differently. Generally speaking, serotonin, norepinephrine, and dopamine are neurotransmitters in the central nervous system (CNS) that are associated with mood. Higher levels of these transmitters are associated with better mood and location. Each class of antidepressants uniquely increases one or more of these neurotransmitters.
Types of antidepressants
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs inhibit the reuptake of serotonin in the brain connected to the brain. This effectively leaves more free serotonin available, and this increase in free serotonin has been associated with reduced symptoms of depression and improved mood. SSRIs are considered first-choice drugs in the treatment of depression because they are effective with relatively few side effects.
Examples of SSRIs: Lexapro, Paxil, Celexa, Prozac, Zoloft
Serotonin and norepinephrine reuptake inhibitors (SNRIs)
SNRIs inhibit the reuptake of serotonin and norepinephrine at nerve synapses. These elevated free levels of both transmitters have been shown to be effective against depressive symptoms. SSRIs are just as effective as SSRIs and can be used as first-line therapy for depression.
SNRI examples: Cymbalta , Effexor, Pristiq , Fetzima
Norepinephrine and dopamine inhibitors (NDRIs)
NDRIs block the reuptake of dopamine and norepinephrine at nerve synapses by increasing the concentration of these two neurotransmitters. This class of drugs has also proven effective in smoking cessation.
Examples of NDRIs: Wellbutrin
Tricyclic antidepressants (TCAs)
Tricyclic antidepressants (TCAs) increase norepinephrine and serotonin levels and block acetylcholine and histamine, which can negatively affect mood. TCAs are the oldest class of antidepressants and are generally considered second-line drugs after SSRIs and SNRIs because they are not as easily tolerated.
Examples of TCAs: Tofranil, Pamelor, Norpramine
Monoamine oxidase inhibitors (MAOIs)
MAOIs block the action of monoamine oxidase enzymes. This increases the concentration of dopamine, norepinephrine and serotonin. MAOIs can have significant drug interactions with many other drug classes and are not considered the first choice for the treatment of depression.
MAOIs can have significant drug interactions with many other drug classes and are not considered the first choice for the treatment of depression.
MAOI examples: Marplan, Nardil, Parnat
Who can take antidepressants?
Adults
Adult men and women can take antidepressants. Caution should be used in any patient who has ever had a hypersensitivity reaction to other antidepressants. Antidepressants are associated with an increase in suicidal ideation in young people under the age of 25, and this age group should be carefully monitored for signs of suicidal ideation.
Elderly
Some types of antidepressants should be used with caution in the elderly. TCAs tend to cause severe drowsiness and may put older patients at an increased risk of falls. If liver or kidney function worsens, the doctor may start with a lower dose.
Children
Some antidepressants are approved for use in children and adolescents. However, most of them contain a strong warning against their use due to the increase in suicidal thoughts. Use in children should be limited to cases where other safer treatment options have failed and the potential benefit outweighs the risk. Children and adolescents should be closely monitored.
Use in children should be limited to cases where other safer treatment options have failed and the potential benefit outweighs the risk. Children and adolescents should be closely monitored.
Are antidepressants safe?
Serotonin syndrome may occur in patients taking drugs with serotonergic activity, especially if they take more than one. Serotonin syndrome is the result of too much free serotonin and can cause symptoms such as agitation, confusion, palpitations, profuse sweating, and diarrhea.
Some antidepressants are not recommended for patients with hepatic impairment. When discussing treatment options, make sure your doctor is aware of all of your medical conditions.
Do not stop taking antidepressants suddenly or without your doctor's consent. Withdrawal syndrome may occur.
Can antidepressants be taken while pregnant or breastfeeding?
SSRIs are generally acceptable during pregnancy and breastfeeding, with the exception of Paxil (paroxetine). This is the only SSRI that can cause harm. If you took Paxil before pregnancy, your doctor will likely recommend other options. The use of an SNRI may be acceptable after a risk-benefit analysis has been done by your doctor. Most other antidepressants should generally be avoided during pregnancy and breastfeeding.
This is the only SSRI that can cause harm. If you took Paxil before pregnancy, your doctor will likely recommend other options. The use of an SNRI may be acceptable after a risk-benefit analysis has been done by your doctor. Most other antidepressants should generally be avoided during pregnancy and breastfeeding.
Are antidepressants controlled substances?
Most antidepressants are not controlled substances because most are not habit-forming or addictive. The only exception is Spravato (esketamine), which is a Schedule III controlled substance classified by the Drug Enforcement Agency (DEA).
Common side effects of antidepressants
Antidepressants can cause many side effects. These will vary slightly depending on the type of antidepressant and are often dose dependent. This means that some side effects may be more likely with a higher dose of medication.
How much do antidepressants cost?
Virtually all classes of antidepressants are available in generic form. Thanks to the use of SingleCare coupons, many antidepressants are under $10 a month, even if you don't have insurance. There are several new drugs being used to fight depression that are not yet available in generic form. One example is Viibryd, which can cost almost $500 if you're not insured. And a coupon from SingleCare can bring Viibryd down to under $300. Trintellix is another branded antidepressant that costs over $700 on average without insurance. And the Trintellix SingleCare Coupon can bring the price down to around $360 - a significant savings.
Thanks to the use of SingleCare coupons, many antidepressants are under $10 a month, even if you don't have insurance. There are several new drugs being used to fight depression that are not yet available in generic form. One example is Viibryd, which can cost almost $500 if you're not insured. And a coupon from SingleCare can bring Viibryd down to under $300. Trintellix is another branded antidepressant that costs over $700 on average without insurance. And the Trintellix SingleCare Coupon can bring the price down to around $360 - a significant savings.
Your insurance policy may have statutory limits that require you to first be asked to try certain preferred drug regimens before they approve more expensive drugs to treat your depression. Always check with SingleCare before adding an antidepressant to make sure you are paying the best price.
All About Xyrem - Drink-Drink
For more information, see "Is Xyrem Misused?" section below.
Risk of CNS depression. Xyrem depresses (slows down) your CNS. This is called CNS depression. Even when you take Xyrem at the doses prescribed by your doctor, the drug causes this side effect. CNS depression can impair your motor skills, judgment, and thinking.
Xyrem depresses (slows down) your CNS. This is called CNS depression. Even when you take Xyrem at the doses prescribed by your doctor, the drug causes this side effect. CNS depression can impair your motor skills, judgment, and thinking.
Due to the risk of CNS depression, Xirem should not be taken with alcohol. And you shouldn't take Xyrem with drugs called sedative-hypnotics. This is a type of medication prescribed to treat certain sleep disorders.
In addition, the combination of Xyrem with other CNS depressants can lead to serious side effects such as:
In rare cases, taking Xyrem with other CNS depressants can be fatal.
For more information about sedative-hypnotics and CNS depressants, see What to Consider Before Taking Xyrem? section below.
Due to the risk of misuse and CNS depression, only certain licensed healthcare professionals may prescribe Xyrem. And only a pharmacy with a special license can write Xyrem prescriptions.
These restrictions apply to Xyrem because the drug is prescribed through a program called a risk assessment and reduction strategy (REMS). The Food and Drug Administration (FDA) may require certain drugs to have REMS, to be prescribed only when the benefits outweigh the risks. To learn more, see Can Xyrem be misused? section below.
The Food and Drug Administration (FDA) may require certain drugs to have REMS, to be prescribed only when the benefits outweigh the risks. To learn more, see Can Xyrem be misused? section below.
Due to the CNS effects of xirem, some activities may be dangerous after a dose of this drug. You must wait at least 6 hours after taking a dose before taking part in activities that require full wakefulness. Examples include driving a car and operating machinery.
Breathing problems, including sleep apnea
Xyrem treatment may cause breathing problems, including sleep apnea. If you have trouble breathing or sleep apnea, taking Xyrem may make your condition worse.
Some people may be at higher risk of breathing problems if they take Xyrem, including:
- obese people
- males*
- women* who have gone through menopause and are not taking hormone replacement therapy
With sleep apnea, your breathing stops and resumes during sleep. This side effect has rarely been seen in Xyrem studies. But several people in these studies had to stop taking Xyrem because of this side effect.
This side effect has rarely been seen in Xyrem studies. But several people in these studies had to stop taking Xyrem because of this side effect.
Symptoms of sleep apnea may include:
- choking or choking while sleeping
- headache upon waking
- snoring
- feeling tired after sleep
If you notice sleep apnea symptoms or problems while taking Xyrem , talk to your doctor. You should also contact your doctor if you have breathing problems that get worse while you are taking Xyrem. They can best advise you if it is safe for you to continue using Xyrem. They may also recommend other treatments for your condition that may be better.
Abnormal dreams or unusual sleep behavior
Taking Xyrem may cause you to have abnormal dreams or unusual sleep behavior. These were some of the most common side effects of Xyrem in studies.
Examples of unusual sleep behavior reported by studies include:
- sleepwalking
- doing tasks such as housework while sleeping
- eating while sleeping
- talking while sleeping
For some people, this behavior has led to injury.
While you are taking Xyrem, tell your doctor right away if you notice abnormal dreams or unusual sleep behavior. They will likely want to investigate your symptoms further. Your doctor may recommend that you stop taking Xyrem and may discuss alternative treatments with you.
Allergic reaction
Some people may have an allergic reaction to Xyrem. Although no allergic reactions have been reported in studies of the drug, they have occurred in rare cases since the drug was on the market.
Symptoms of a mild allergic reaction may include:
- skin rash
- itching
- redness (temporary warmth, redness or discoloration of the skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction may include swelling under the skin, usually on the eyelids, lips, hands, or feet. They may also include swelling of the tongue, mouth, or throat, which can cause breathing problems.

Call your doctor right away if you have an allergic reaction to Xyrem. But if you think you need a medical emergency, call 911 or your local emergency number.
What are the frequently asked questions about Xyrem?
Find answers to some frequently asked questions about Xyrem.
Is Xyrem used to treat insomnia, idiopathic hypersomnia, or fibromyalgia?
Xyrem is not approved by the Food and Drug Administration (FDA) for the treatment of these conditions. Insomnia is a sleep disorder that causes difficulty falling or staying asleep. Idiopathic hypersomnia is a condition in which a person feels excessive sleepiness during the day. And fibromyalgia is a condition that causes pain and lack of energy.
But doctors may prescribe Xyrem off label to treat these conditions. Off-label use of a drug means that a drug that is approved by the FDA for one purpose is used for another purpose that has not been approved.
If you want to know more about off-label use of Xyrem, talk to your doctor or pharmacist.
Will Xyrem make you feel better? Is there a risk of addiction or withdrawal?
Xyrem is unlikely to make you feel better. Feelings of euphoria have not been reported in studies of the drug.
Xyrem does have a risk of addiction and dependence, which can lead to withdrawal. To learn more, see Can Xyrem be misused? section below.
If you have concerns about addiction and withdrawal caused by Xyrem, talk to your doctor.
What is a controlled substance and does Xyrem fall into this category?
Yes, Xyrem is a controlled substance. Certain laws control the use of Xyrem to prevent possible misuse. Abuse occurs when a person uses a drug for other purposes. Misuse of Xyrem can lead to serious side effects including breathing problems or coma. In rare cases, it can even lead to death.
Xyrem is considered a Schedule III controlled substance. This type of controlled substance is approved for medical use, but also carries the risk of misuse, addiction, and tolerance. In addiction, the body needs the drug to function properly. Tolerance means that the body gets used to the drug and needs a higher dose for the same effect.
In addiction, the body needs the drug to function properly. Tolerance means that the body gets used to the drug and needs a higher dose for the same effect.
In addition, Xyrem is only available through certain doctors and a specialized pharmacy. These restrictions apply to Xyrem because the drug is prescribed through a program called a Risk Assessment and Mitigation Strategy (REMS). The Food and Drug Administration may require certain drugs to have REMS, to be prescribed only when the benefits outweigh the risks.
To learn more about Xyrem and the risk of misuse, see the section "Can Xyrem be misused?" section below.
What is the half-life of xirem? Does this affect whether Xyrem shows up on a drug test?
The half-life of a drug is the time it takes the human body to get rid of half the dose. Xyrem has a half-life of 30 to 60 minutes. It takes about four to five times its half-life for a drug to be eliminated from the body. But that doesn't mean the drug won't show up in drug testing anymore.
Xyrem may show up on a drug test. This is because Xyrem is a form of gamma hydroxybutyrate (GHB), which is an illegal drug. Be sure to bring your prescription or doctor's note with you when you take a drug test. This may prove that you are using Xyrem under medical supervision.
Can Xyrem cause long term side effects?
It is not known if Xyrem causes long-term side effects.
Some of the side effects reported in drug studies are considered long-term if they occur in people not taking Xyrem. Examples include depression and psychosis (loss of contact with reality). But it is not known if these side effects are long term or if they will go away if you stop taking Xyrem.
Talk to your doctor or pharmacist if you want to know more about Xyrem and its long-term side effects.
Does Xirem cause weight gain?
No, Xyrem does not cause weight gain. This side effect was not reported in studies of the drug. In fact, some children who took Xyrem in these studies reported weight loss.
If you are concerned about weight changes while taking Xyrem, talk to your doctor.
Is Xyrem used for narcolepsy?
Xirem is a medicine prescribed to treat the following symptoms of narcolepsy:
- Excessive daytime sleepiness (EDS). SED is a sudden, overwhelming desire to sleep. This can make it difficult to complete activities and tasks throughout the day.
- Cataplexy. In cataplexy, the muscles may suddenly become weak or completely limp.
Xirem can be used for this purpose in adults and children 7 years of age and older.
Narcolepsy is a disorder of the nervous system that causes abnormal sleep patterns. In addition to EDS and cataplexy, people with narcolepsy sometimes have "sleep attacks" (falling asleep suddenly). This can happen at any time without warning.
How Xyrem treats narcolepsy is unknown. The drug is believed to affect certain chemicals in the brain that help improve sleep quality and treat the symptoms of narcolepsy.
What is the dosage of Xyrem?
Your doctor will recommend the dosage of Xyrem that is right for you. The following are commonly used dosages, but always take the dosage your doctor has prescribed for .
Form
Xyrem comes as a liquid solution that you swallow.
Recommended Dosage
The recommended dosing schedule for Xyrem is as follows:
- Take one dose just before bedtime.
- Take a second dose 2.5–4 hours later.
Xyrem Dosage Questions
Below are some common Xyrem dosage questions.
- What if I miss a dose of Xyrem? If you miss a dose of Xyrem, skip the missed dose. You should never take two or more doses of Xyrem at the same time.
- Do I need to take Xyrem long term? If you and your doctor agree that Xyrem is safe and works for you, you are likely to take it for a long time.
- How long does Xyrem last? Most people fall asleep within 15 minutes of taking a dose of Xyrem.
 Some fall asleep within 5 minutes of taking a dose.
Some fall asleep within 5 minutes of taking a dose.
What should I consider before taking Xyrem?
Before you start treatment with Xyrem, it is important to discuss certain aspects of your health with your doctor. These include any medical conditions you have and any medications you are taking. This information helps them determine if Xyrem is the right treatment option for you.
interactions
Taking the medicine with some vaccines, foods and other things can affect how the medicine works. These effects are called interactions.
Be sure to tell your doctor about all medicines you are taking, including prescription and over-the-counter medicines, before taking Xyrem. Also, describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Xyrem.
Interactions with drugs or supplements
Xyrem may interact with several types of drugs. These drugs include:
- sedative sleeping pills, such as:
- Ezzopiclon (LonESTA)
- Ramelteon (Roserem)
- Zalesplon (sonata)
- certain pain relievers, including oxycodone (Oxaydo, OxyContin) and fentanyl (Actiq, Fentora)
- benzodiazepines, including alpraisals (Ksanax) and clonopine (clonopine)
- muscle relaxants, including cyclobenzaprin (Fexmides)
- antipsychotic drug clozapine (Clozaril)
- antiepileptic drug divalproex sodium (Depakote)
Due to potential interactions, your doctor will likely tell you not to take Xyrem with some of the medicines listed above.
Boxed Warnings
Xirem has boxed warnings. These are serious warnings from the Food and Drug Administration (FDA).
Xyrem box warnings include:
- Risk of misuse. Possible misuse of Xyrem. (Misuse is sometimes called abuse.) Misuse of Xyrem can lead to serious side effects, including coma or breathing problems. In rare cases, it can even lead to death. To learn more, see Can Xyrem be misused? section below.
- Risk of CNS depression. Xyrem depresses (slows down) your CNS. This effect is called CNS depression. Even when you take Xyrem at the doses prescribed by your doctor, the drug causes this side effect. CNS depression can impair your motor skills, judgment, and thinking. For more information, see "What are the side effects of Xyrem?" section above.
Other warnings
Xyrem may not be right for you if you have certain medical conditions or other factors that affect your health. Talk to your doctor about your medical history before taking Xyrem. Factors to consider include those discussed below.
Factors to consider include those discussed below.
Amber semialdehyde dehydrogenase deficiency. Having a rare brain disease called succinic semialdehyde dehydrogenase deficiency can lead to increased levels of xyrem in the body. This can lead to serious side effects. As a result, the presence of this disorder is considered a contraindication for taking Xyrem. This means that your doctor will not prescribe Xyrem if you have this condition because of the risk of harm. Instead, your doctor may suggest safer treatments for you.
Suicidal thoughts. In rare cases, Xyrem has caused suicidal thoughts or actions as a side effect. If you have or have had suicidal thoughts or behavior, talk to your doctor before you start taking Xyrem. Taking Xyrem may make these feelings worse. Your doctor can determine if it is safe for you to take Xyrem. See Suicide Prevention above for guidance on suicide prevention.
Depression. Depression or depressed mood are possible side effects of Xyrem. If you have depression, tell your doctor about it. Taking Xyrem may make your condition worse. Your doctor can determine if it is safe for you to take Xyrem.
If you have depression, tell your doctor about it. Taking Xyrem may make your condition worse. Your doctor can determine if it is safe for you to take Xyrem.
Heart failure or high blood pressure. Xyrem is high in sodium. In people with heart failure or high blood pressure, the drug may make their condition worse. For more information, see the "Ask a pharmacist" section below.
Breathing or lung problems. Xyrem may cause lung-related side effects such as decreased respiratory rate and respiratory depression. If you have lung problems, you may be at a higher risk of these side effects with Xyrem. Tell your doctor about any lung problems you have. This will help them determine if it is safe for you to take Xyrem.
Sleep apnea. Xyrem may cause sleep apnea. Taking Xyrem may make this condition worse in people who already have it. If you have sleep apnea, talk to your doctor. They can tell you if it is safe for you to take Xyrem.
Liver problems. If you have liver problems, your body may have trouble breaking down Xyrem after a dose. This can lead to a buildup of xyrem levels in the body, which can lead to serious side effects. Before starting treatment with Xyrem, tell your doctor about any liver problems you have. This will help them determine if it is safe for you to take Xyrem.
Allergic reaction. If you have had an allergic reaction to Xyrem or any of its ingredients, your doctor will likely not prescribe Xyrem. Ask them what other medicines are the best options for you.
Xyrem and alcohol
You should not take Xyrem with alcohol.
Xyrem works by depressing (slowing down) your central nervous system (CNS). This effect is called CNS depression. CNS depression can impair motor skills, thinking, and judgment.
Alcohol also depresses the central nervous system. As a result, the combination of alcohol and xirem can lead to serious side effects. These include breathing problems or coma. In rare cases, this can be fatal.
These include breathing problems or coma. In rare cases, this can be fatal.
Tell your doctor if you want to drink alcohol. They may offer treatment for your narcolepsy symptoms other than Xyrem.
Pregnancy and breastfeeding
It is not known if Xyrem is safe to take while pregnant or breastfeeding.
If you are pregnant or breastfeeding, or planning to become pregnant or breastfeeding, talk to your doctor. They will discuss safe options for treating the symptoms of narcolepsy.
What should I know about Xyrem and the alternative Provigil?
Xyrem and Provigil (modafinil) may be prescribed to treat symptoms of narcolepsy in adults. Some children may also be given Xyrem for this.
Provigil is a type of stimulant medication. It works by energizing your nervous system to release chemicals that make you feel more energized. Xyrem is not a stimulant, so it works differently.
To learn more about the two drugs, see this detailed comparison. Also, check with your doctor about which drug is right for your condition.
Also, check with your doctor about which drug is right for your condition.
What to do in case of an overdose?
Do not take more Xyrem than your doctor has told you to. Using more can lead to serious side effects.
Overdose symptoms
There have been only two reports of overdose in Xyrem studies. So it's not entirely clear what the symptoms of Xyrem overdose are.
But Xyrem's active drug, sodium oxybate, is a form of gamma hydroxybutyrate (GHB). As such, it is believed to cause overdose symptoms similar to those reported with GHB, which is an illegal drug.
Symptoms of a GHB overdose include:
- slow breathing or trouble breathing
- confusion
- seizures
- vomiting
- agitation
- blurred vision
- unconsciousness
- coma
- slow heart rate
- headache
- sweating
What to do if you have taken too much Xirem
Call your doctor if you have taken too much Xyrem You can also call 800-222-1222 to contact the American Association of Poison Control Centers or use their online resource. But if you have severe symptoms, call 9 immediately11 or your local emergency number. Or go to the nearest emergency room.
But if you have severe symptoms, call 9 immediately11 or your local emergency number. Or go to the nearest emergency room.
How is Xirem taken?
Your doctor will tell you how to take Xyrem. They will also explain how much to take and how often. Be sure to follow your doctor's instructions for administering this drug.
Taking Xyrem
Xyrem comes as a liquid solution that you swallow.
Taking Xirem with other drugs
Your doctor may suggest using Xyrem with other drugs to treat excessive daytime sleepiness caused by narcolepsy. Examples include:
- amphetamine and dextratamine (Adderall)
- Modafinil (Provigil)
- Armodafinil (nuvigil)
- methylphenidate (Ritalin, concert)
If you have questions about taking other drugs for treating symptoms , talk to your doctor.
Should I take Xyrem with food?
No, you should not take Xyrem with food. You must wait at least 2 hours after a meal before taking a dose of Xyrem.
Questions to ask your doctor
You may have questions about Xyrem and your treatment plan. It is important to discuss all your concerns with your doctor.
Here are some tips to help you talk:
- Before the meeting, write down questions such as:
- How will Xyrem affect my body, mood, or lifestyle?
- Take someone with you to the meeting if it makes you feel more comfortable.
- If you do not understand something about your condition or treatment, ask your doctor to explain it to you.
Remember that your doctor and other healthcare professionals are always available to help you. And they want you to get the best possible care. So don't be afraid to ask questions or leave feedback about your treatment.
How much does Xirem cost?
The cost of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use. For current Xyrem prices in your area, visit WellRx.com.
For current Xyrem prices in your area, visit WellRx.com.
If you have questions about how to pay for a prescription, talk to your doctor or pharmacist. You can also visit the Xyrem manufacturer's website to see if they have support options.
And to learn more about saving money on prescriptions, check out this article.
Can Xyrem be abused?
Xirem has a warning in the box about the risk of misuse.* The warnings in the boxes are serious Food and Drug Administration (FDA) warnings.
When misused, a person uses the drug in a way that is not prescribed. This may include taking more of the drug than the doctor instructed, or taking the drug prescribed to someone else. Misuse of Xyrem can lead to serious side effects. This may include coma or breathing problems. In rare cases, this can be fatal.
Xyrem is considered a Schedule III controlled substance. This type of controlled substance is approved for medical use, but also carries the risk of misuse, addiction, and tolerance. In addiction, the body needs the drug to function properly. Tolerance means that the body gets used to the drug and needs a higher dose for the same effect.
In addiction, the body needs the drug to function properly. Tolerance means that the body gets used to the drug and needs a higher dose for the same effect.
Before starting treatment with Xyrem, tell your doctor if you have a history of a substance use disorder. You may be at a higher risk of dependence on Xyrem, which may increase your risk of misuse.
About the Xyrem Program REMS
Because of the risk of misuse of Xyrem, only certain health professionals with special certifications may prescribe Xyrem. And only a pharmacy with a special license can write Xyrem prescriptions. You will not be able to buy Xyrem at your local pharmacy.
These restrictions apply to Xyrem because the drug is prescribed through a program called a risk assessment and mitigation strategy (REMS). The Food and Drug Administration may require certain drugs to have REMS, to be prescribed only when the benefits outweigh the risks.
Before your doctor can prescribe Xyrem, you must enroll in the Xyrem REMS program. You will need to complete documentation that you are using the drug safely and only as directed by your doctor.
You will need to complete documentation that you are using the drug safely and only as directed by your doctor.
If you want to know more about the Xyrem REMS program, talk to your doctor or pharmacist. You can also get information about the program by visiting the Xyrem REMS website or by calling 866-997-3688.
What to ask the doctor
If you are considering treatment with Xyrem, ask your doctor about taking this drug. More information about Xyrem will help you feel comfortable about the risks and benefits of this medication. Here are a few to help you get started:
- What should I know about treatments for narcolepsy other than Xyrem?
- Do I need to limit my salt intake while taking Xyrem?
- How do I know if it's safe for me to drive while using Xyrem?
- My job requires regular drug screening. Will Xyrem show up on a drug test?
You may also be interested in learning more about:
- Narcolepsy Treatment Options
- Cataplexy Treatment Options
Ask a Pharmacist
Q:
What Should I Take Xyrem?
Anonymous
A:
It is important to note that Xyrem has a high salt content.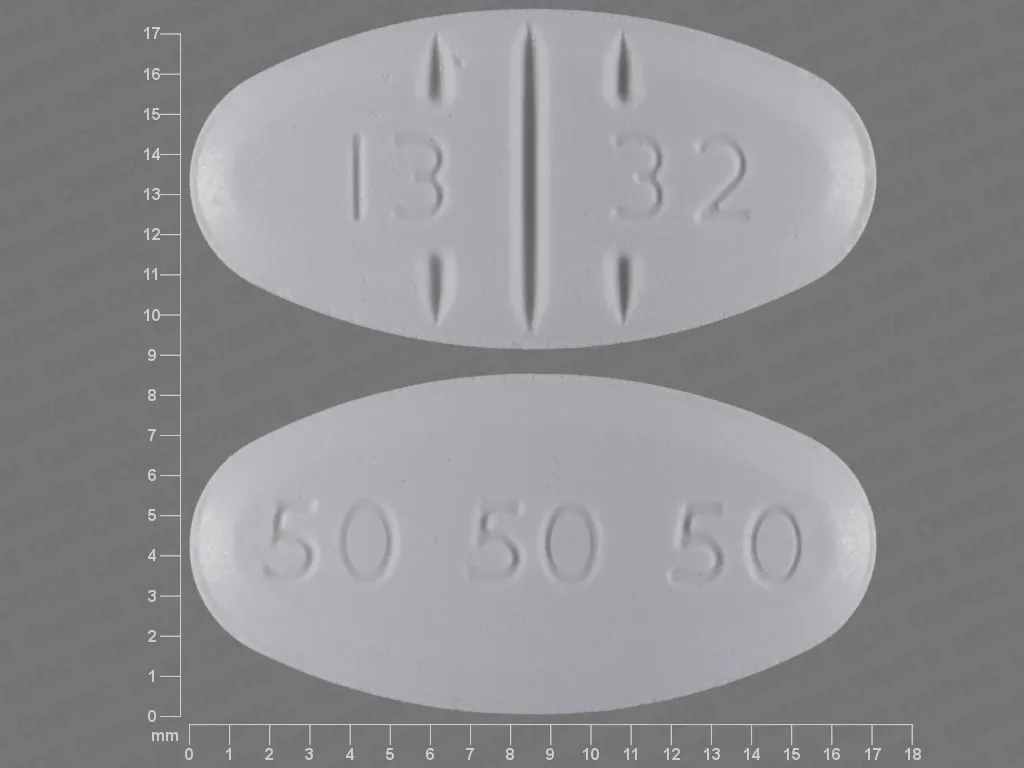 If you have heart failure, your doctor may suggest limiting your daily salt intake. It may help with symptoms of heart failure, including water retention. It may also help lower blood pressure.
If you have heart failure, your doctor may suggest limiting your daily salt intake. It may help with symptoms of heart failure, including water retention. It may also help lower blood pressure.
Below is how much salt is in certain doses of Xyrem.
- Xyrem 3 grams (g) contains 550 milligrams (mg) of salt.
- Xyrem 4.5 g contains 820 mg of salt.
- Xyrem 6 g contains 1,100 mg of salt.
- Xyrem 7.5 g contains 1,400 mg of salt.
- Xyrem 9 g contains 1.640 mg of salt.
If you are concerned about your salt intake, your doctor may suggest Xywav (calcium, magnesium, potassium, and sodium oxybates) to treat the symptoms of narcolepsy. This drug works similarly to Xyrem but contains less salt per dose.
For more information about heart failure and Xyrem, talk to your doctor.
Beverage Pharmacy Team Answers represent the opinions of our medical experts. All content is for informational purposes only and should not be considered medical advice.