Schizophrenia genetic testing
Schizophrenia Study Suggests Advanced Genetic Scorecard Cannot Predict a Patient’s Fate | Mount Sinai
- Press Release
Mount Sinai study showed that polygenic risk scores were no better at predicting whether a patient’s symptoms worsened than written reports
Newsroom
- New York, NY
- (September 07, 2021)
With the help of cutting-edge computer programs, researchers at the Icahn School of Medicine at Mount Sinai went through the genetic and medical records of more than 8,000 schizophrenia patients. They found that a tool commonly used in research for evaluating a person’s genetic risk for a disease, called a polygenic risk score, was no better at predicting the outcome of a patient’s disease over time than written reports. The results raise important questions about the use of polygenic risk scores in real-world, clinical situations, and also suggest that a doctor’s written report may be an untapped source of predictive information.
“Treating schizophrenia patients is a heart-wrenching experience. One of the hardest parts about taking care of patients is trying to determine whether each patient’s condition will worsen or improve. If we could do that, then we might help relieve the suffering that the patients and their loved ones experience,” said Alexander W. Charney, MD, PhD, Assistant Professor in the Departments of Psychiatry and Genetics and Genomic Sciences at Icahn Mount Sinai and the senior author of the study published in Nature Medicine. “Our results show that for the mental illnesses most deeply characterized at the genetic level, the current state of genetics research cannot solve this problem just yet.”
Affecting about 20 million people worldwide, schizophrenia is a life-shortening mental disorder that alters the way a person thinks, acts, and perceives reality. Typically, symptoms appear in the late teens to early thirties and can last a lifetime. While some patients may respond well to treatment, others do not at all.
Although it is a highly inherited disease, the majority of cases cannot be linked to a single gene. Instead, scientists have found that the risk of suffering from schizophrenia is influenced by a complex combination of normal genetic variants, none of which on their own contribute a great amount to risk but together account for many cases. Currently, nearly 300 such variants have been associated with schizophrenia.
The polygenic risk score is a commonly used method for summarizing the genetic component of a person’s risk for a disease. Over the past decade, many large studies have shown that the risk scores of schizophrenia patients are significantly higher than that of healthy controls. Similar results have been seen in studies on other disorders such as hypertension and diabetes.
“The polygenic risk score basically adds up all of the traits that are associated with a complex disorder. Initially it was designed to be descriptive tool. More recently, scientists have proposed that it could be an effective tool for precision medicine wherein a person’s genetics is used to diagnose disease and predict outcomes,” said Isotta Landi, PhD, a post-doctoral fellow in Dr.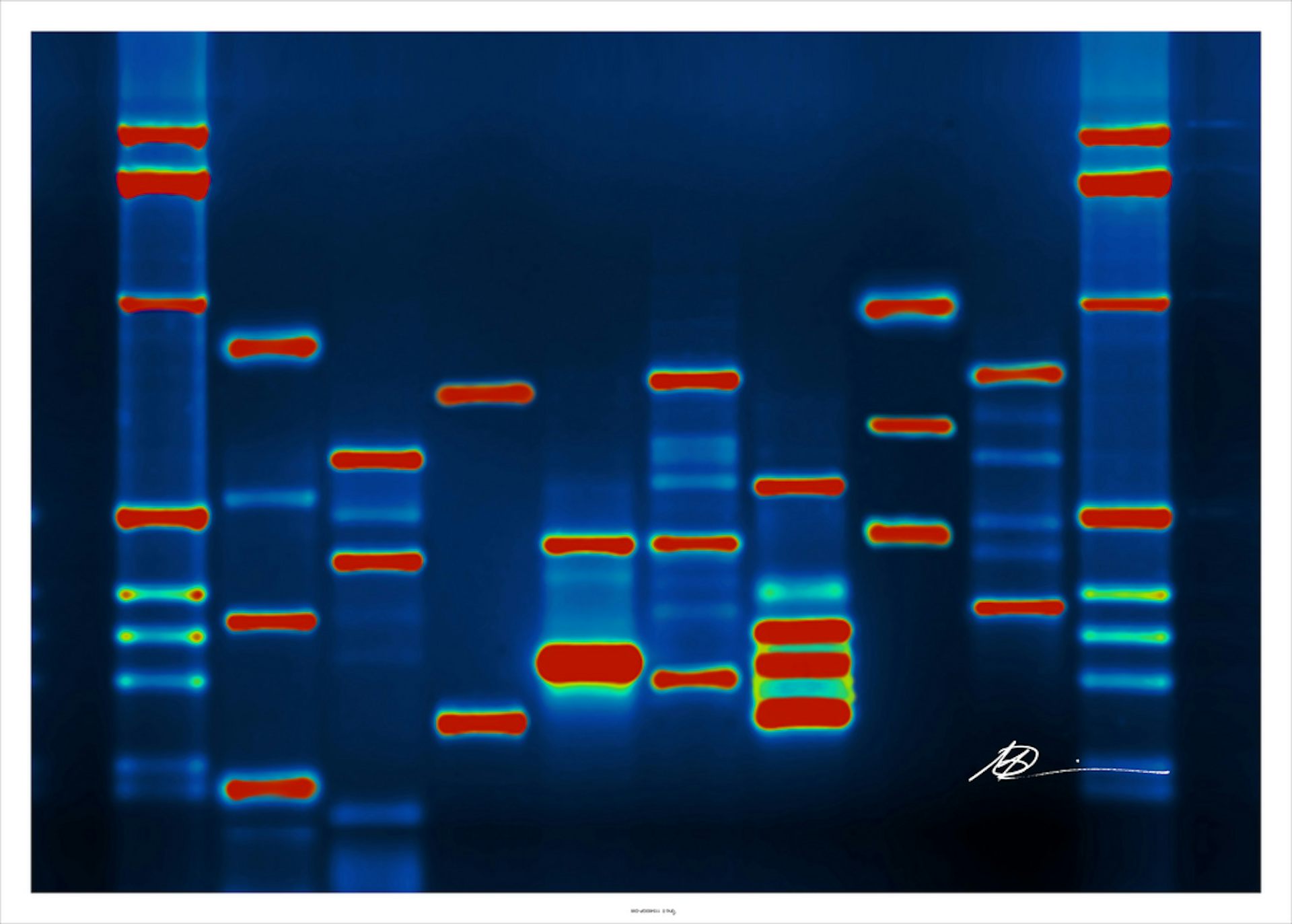 Charney’s lab and the lead author of the study. “In this study we wanted to rigorously test out whether the polygenic risk score could also be a predictive tool.”
Charney’s lab and the lead author of the study. “In this study we wanted to rigorously test out whether the polygenic risk score could also be a predictive tool.”
At first, the researchers compared the genetic and medical records of 762 schizophrenia patients stored in the Mount Sinai Health System’s BioMe™ BioBank program. Specifically, they tested whether a patient’s polygenic risk score for schizophrenia could predict six poor outcomes of each patient any better than the information derived from the medical reports written by doctors.
To do this, Dr. Landi worked with others to develop advanced computer programs that calculate polygenic risk scores from a patient’s genetic data and use natural language processing tools to extract information from written reports.
They found that two of the outcomes—aggressive behavior and the need for hospitalization—were significantly associated with higher polygenic risk scores. However, the scores were no more effective at predicting these outcomes than was the information derived from the written reports, and combining the two did not change predictability.
Follow-up experiments supported these results. For instance, the researchers saw no change in the results when they tried to predict outcomes only in people with the highest polygenic risk scores.
Finally, they saw the same trend when they analyzed genetic and medical records of 7,779 patients stored in the Genomic Psychiatry Cohort, a large National Institutes of Health-funded project. Once again, the polygenic risk scores did not improve upon the ability of clinical data to predict poor outcomes.
“Our results suggest that more work needs to be done to harness the potential that genetics has to improve the treatment of schizophrenia patients,” Dr. Charney said. “The results also suggest that the detailed medical reports that doctors write may contain much more valuable and predictive information than we originally anticipated.”
This study was funded by the National Institutes of Health (Mh221923). The Genomic Psychiatry Cohort was also supported by the NIH (MH085548, Mh204964, and Mh22345).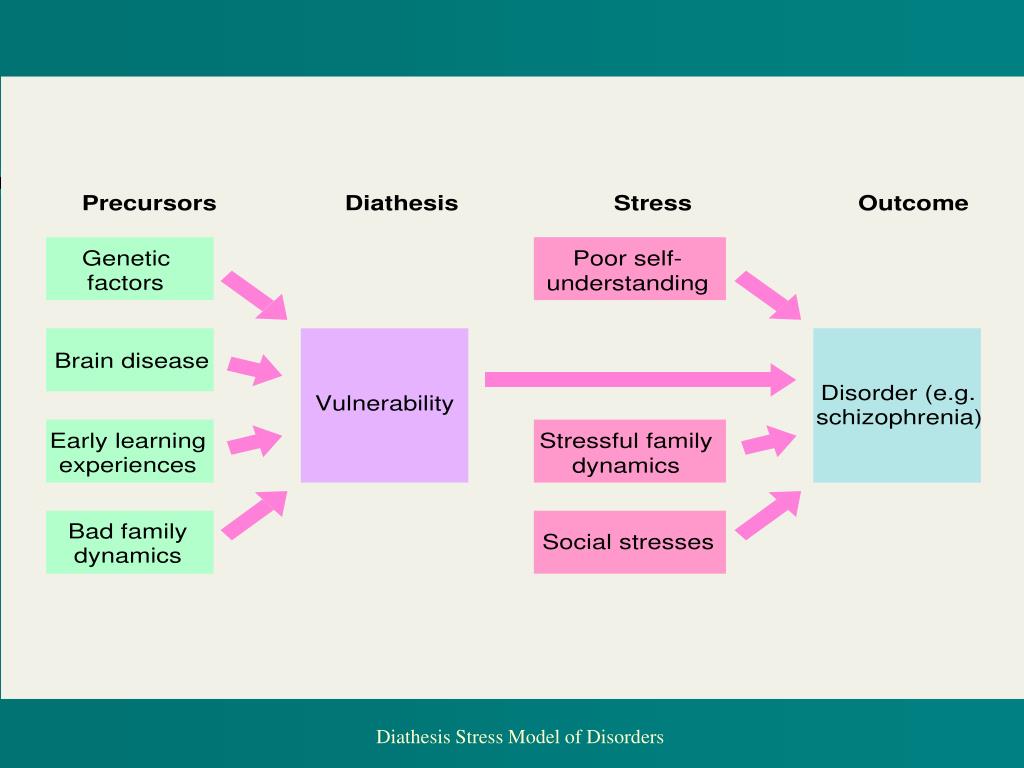
Article
Landi, I. et al., Prognostic value of polygenic risk scores for adults with psychosis. Nature Medicine, September 6, 2021, DOI: 10.1038/s41591-021-01475-7
Tags: BioMe® BioBank Program, Department of Genetics & Genomic Sciences , Icahn School of Medicine at Mount Sinai, Mount Sinai Health System, Patient Care, Psychiatry, Schizophrenia and Psychotic Disorders, Alexander Charney, MD, PhD, ISOTTA LANDI
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U. S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.
S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties. The Icahn School of Medicine at Mount Sinai is one of three medical schools that have earned distinction by multiple indicators: It is consistently ranked in the top 20 by U.S. News & World Report's "Best Medical Schools," aligned with a U.S. News & World Report "Honor Roll" Hospital, and top 20 in the nation for National Institutes of Health funding and top 5 in the nation for numerous basic and clinical research areas.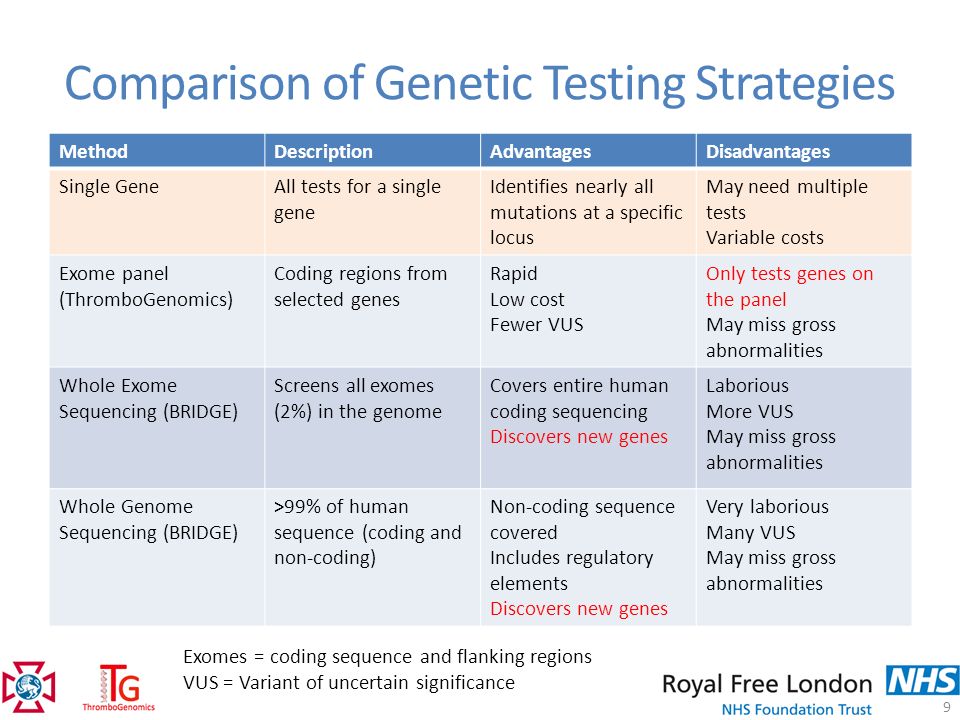 Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
Newsweek’s “The World’s Best Smart Hospitals” ranks The Mount Sinai Hospital as No. 1 in New York and in the top five globally, and Mount Sinai Morningside in the top 20 globally.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
Schizophrenia 'risk genes' aren't so risky if mother's pregnancy was healthy
Far be it from us to tell 23andMe how to run its business, but if it or any other DNA company wants to give customers a better read of disease risk, they might start asking how mom’s pregnancy went.
That’s the key message of a schizophrenia study, published Monday, which showed that 108 regions of the genome previously identified as raising the risk of schizophrenia do so only slightly if the mother experiences no complications during pregnancy — but by some twelvefold if she does.
Taking into account prenatal conditions gives a starkly different read of how risky schizophrenia risk genes are: Taken together, they raise the chance of developing the disease to 12 in 1,000 if there are no complications — or to 80 in 1,000 if there are.
advertisement
“This should be an eye-opening study, especially for anyone who thinks disease risk is all genetic,” said Janine LaSalle, of the University of California, Davis, who studies the genetics of autism and was not involved in the schizophrenia research. “Genes don’t exist in a lock-box away from everything else that happens to you.”
The idea that both genes and environment affect risk of disease is conventional scientific wisdom. But that usually means that while both genes and environment are involved, they act via separate biological pathways. BRCA mutations can raise the risk of breast cancer, for instance, and so can not bearing children, but the two don’t work by the same molecular mechanism.
advertisement
The schizophrenia study, in Nature Medicine, finds something more intriguing. Whether or not risk genes live up to their billing depends on what environment they find themselves in. For schizophrenia, that means the placenta: It can act like either a bump stock on a rifle, increasing the power of schizophrenia genes, or a broken firing pin, rendering the genes non-functional.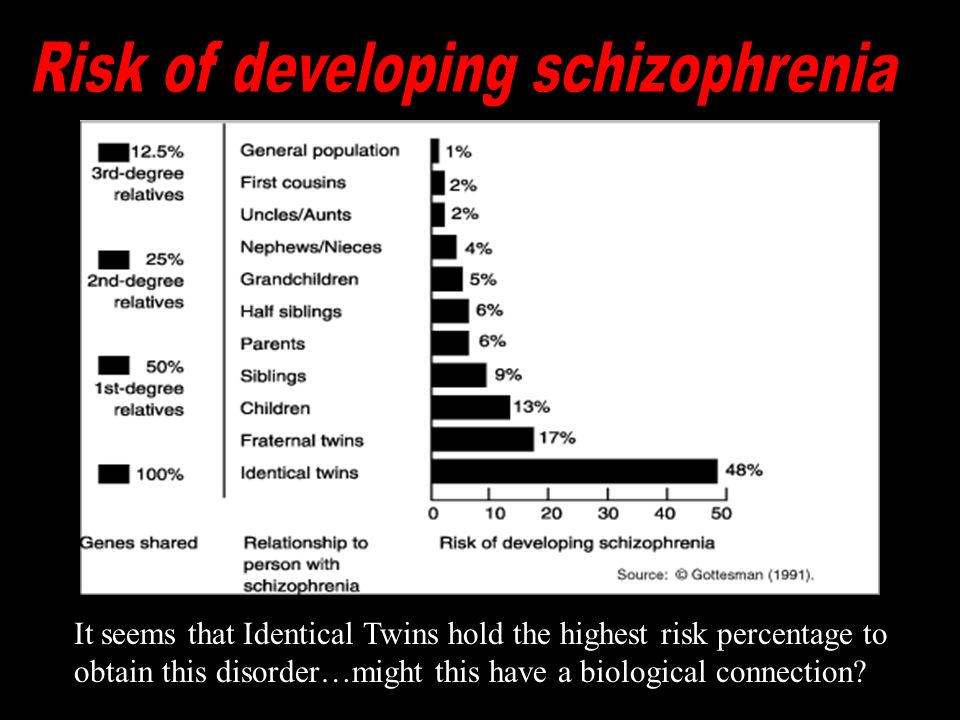
To figure this out, Dr. Daniel Weinberger of Johns Hopkins University and his colleagues started with the 108 genes linked to schizophrenia. They constructed what’s called a polygenic risk score, which calculates the extra risk of a disease from numerous genetic variants. In thousands of healthy people and people with schizophrenia, the scientists found that what is thought to be a high risk score raised the risk of schizophrenia substantially only if in utero complications such as a mother’s diabetes, obesity, pre-eclampsia, or smoking were also present.
For instance, a high score raised the risk more than 800 percent if any of these conditions was present, but just 50 percent if the pregnancy had been healthy. A 50 percent higher risk translates to 12 rather than 8 per 1,000 people developing schizophrenia.
The 108 genes that make up the risk score are expressed at particularly high levels in the placenta, the study also found, and at higher levels in the placentas of male fetuses than female ones.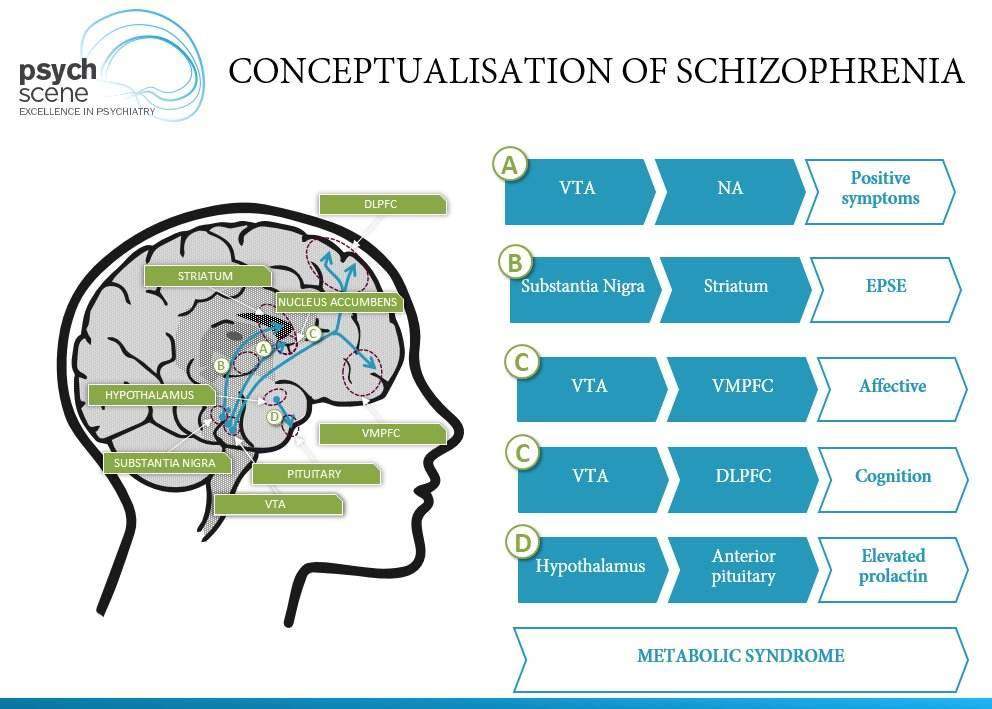 That fits with the fact that more men than women develop schizophrenia, usually in young adulthood.
That fits with the fact that more men than women develop schizophrenia, usually in young adulthood.
The activity of the schizophrenia genes is dialed up especially if the mother has pre-eclampsia or another pregnancy complication. Presumably, “this reflects the placenta’s response to stress,” Weinberger said, such that when it’s flooded with inflammatory molecules (the standard response to stress), “it turns on genes related to immune response.” Recent discoveries connect schizophrenia to the immune system.
Though specifics of how placental health and immune status affect fetal brain health are poorly understood, there is strong circumstantial evidence that it does. The chance of developing the disease is three to seven times greater in people whose mother had a respiratory infection during pregnancy, which can cause inflammation in the placenta, and up to twice as great if the mother had pre-eclampsia, a difficult delivery, or diabetes, obesity, alcohol use, vaginal bleeding, maternal smoking, or preterm birth, all of which can also affect the placenta.
“We need to create a new risk score for schizophrenia, incorporating not only genes but also placental health,” Weinberger said. “The odds of becoming schizophrenic based on your polygenic risk score is more than 10 times greater with these early-life complications than without them.” But the genes-only risk score, “in the absence of a serious complicated pregnancy, explains very little risk for schizophrenia — less that 2 percent” of the chance the individual will develop the disease.
UC Davis’ LaSalle, who studies the expression of autism-related genes in the placenta, also thinks it important to include the environment in genetic risk scores, since “if you don’t have the environmental risk you don’t have the genetic risk.” But more work needs to be done to identify which specific environmental influences on the placenta matter, she said.
23andMe doesn’t disagree. The company’s disease-risk analyses emphasize that, with the exception of single-gene disorders such as Huntington’s, you can have disease genes yet not develop the disease, or develop a disease despite not having the disease genes.
None of the analyses currently incorporate genotype-environment interactions like those found in the schizophrenia study. But at some point, said a 23andMe spokesman, if the technology and research identify more “GxE”’s for more disorders, and if the Food and Drug Administration signs off, that could well change.
About the Author Reprints
First laboratory test for objective early diagnosis of schizophrenia
Golovna > Articles > First laboratory test for objective early diagnosis of schizophrenia
Authors: A.A. Melnik, Ph.D., Kyiv
09.12.2016
PDF article.
Mental illnesses are extremely common worldwide and have serious consequences. According to WHO, more than 500 million people suffer from some kind of mental disorder.
According to WHO, more than 500 million people suffer from some kind of mental disorder.
One of the mental illnesses is schizophrenia. Schizophrenia (according to ICD-10 - F20) is a chronic progressive mental illness characterized by dissociative mental functions with a loss of unity between thinking, feelings and will, increasing mental changes in the form of emotional dullness, atactic thinking and the development of specific dementia. In schizophrenia, there is a loss of unity of mental processes with rapidly or slowly developing personality changes of a special type: autism (progressive introversion), emotional impoverishment, decreased activity (drop in energy potential) and various productive psychopathological disorders (hallucinations, delusions, affective disorders, etc.).
The prevalence of schizophrenia in the world is estimated at 0.8-1%, this figure is approximately comparable among men and women. In men, the first symptoms of schizophrenia appear, as a rule, at the age of 15-20 years, in women - after 25 years. By the age of 30, most patients have clear signs of the disease. In childhood and after 45 years, schizophrenia begins extremely rarely.
By the age of 30, most patients have clear signs of the disease. In childhood and after 45 years, schizophrenia begins extremely rarely.
To date, none of the existing theories explains the etiology of schizophrenia. There are several hypotheses regarding the nature of this pathology.
1. Genetic factors
Genetic factors and gene-environment interactions are extremely important predisposing factors in 80% of cases. The probability of developing schizophrenia in people who have first-degree relatives suffering from this pathology is 10%, while in the general population it is 1%. Schizophrenia can be inherited. At the same time, 60% of patients do not have family members with a similar disorder. In addition, people who are genetically predisposed to schizophrenia do not always develop the disease, which suggests that a genetic risk factor may remain potential. Studies show that inherited genes make a person predisposed to schizophrenia, and environmental factors, combined with a genetic combination, can provoke the disease.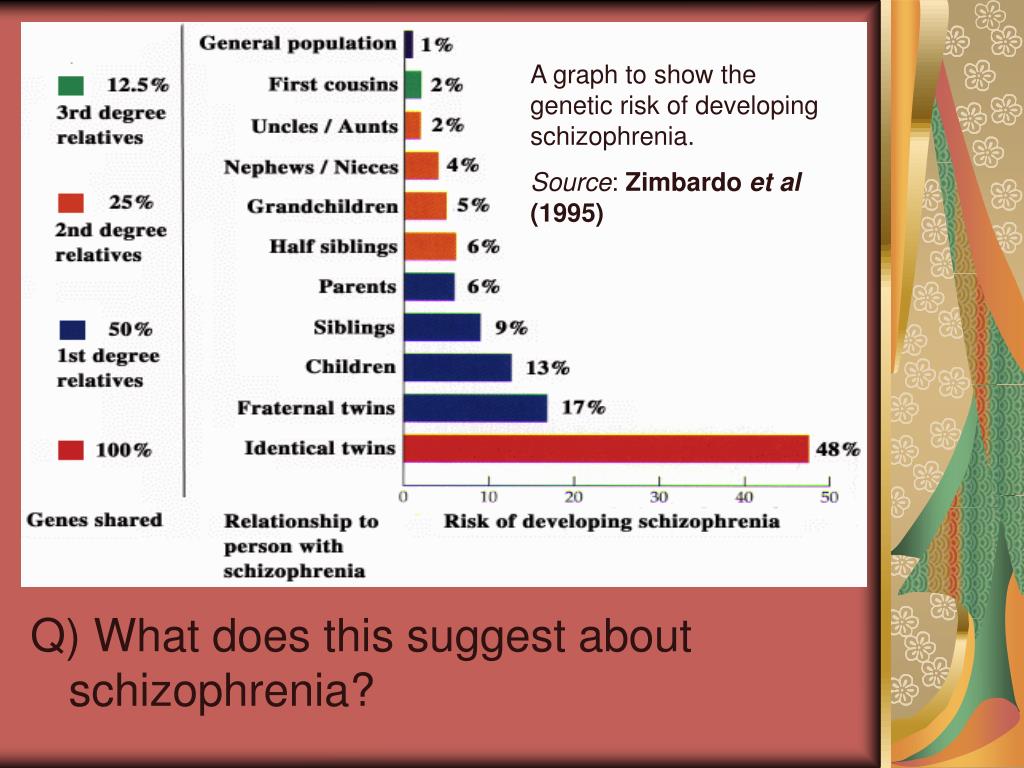 Most often, in schizophrenia, disorders are found in three chromosomal regions (22q11, 1q42 / 11q14, X-chromosome), which are considered a possible location for the localization of genes involved in the development of schizophrenia. But the total number of genes in these regions is about 4000, and specific genes have not been identified.
Most often, in schizophrenia, disorders are found in three chromosomal regions (22q11, 1q42 / 11q14, X-chromosome), which are considered a possible location for the localization of genes involved in the development of schizophrenia. But the total number of genes in these regions is about 4000, and specific genes have not been identified.
2. Infections
Numerous studies have been conducted on the role of infection in schizophrenia. Thus, scientists in the last century pointed to the causal significance of syphilitic, tuberculosis, coccal, and viral infections. Indeed, clinical experience suggests that schizophrenia often occurs after an infectious pathology. But so far, the role of the latter in the etiology of schizophrenia has not been proven.
3. Autointoxication theory
The development of autointoxication theories is associated with the discovery in the body of patients with schizophrenia of various low-molecular protein physiologically active (toxic) substances that realize neurotropic effects.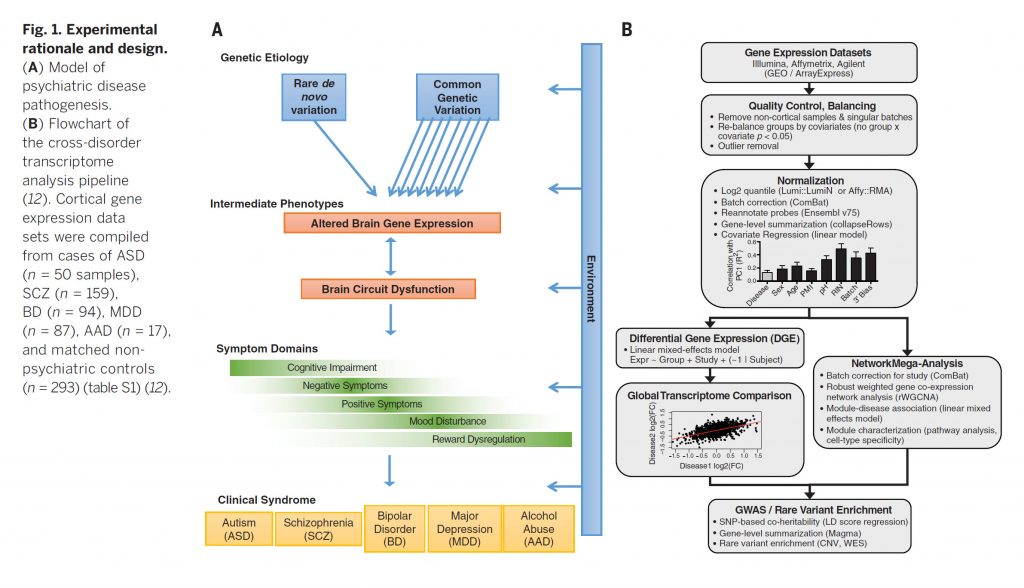 According to this theory, the source of intoxication is the products of incomplete deamination of proteins, which cause hypoxia of the central nervous system, neurodynamic disturbances in the brain and, as a result, mental disorders.
According to this theory, the source of intoxication is the products of incomplete deamination of proteins, which cause hypoxia of the central nervous system, neurodynamic disturbances in the brain and, as a result, mental disorders.
4. Biochemical hypothesis
Some hypotheses regarding the pathogenesis of schizophrenia are associated with the assumption of disorders in specific links of the body's metabolism, in particular biogenic amines. Among these biochemical hypotheses, the following can be distinguished:
1) a group of catecholamine hypotheses considering the possible role of norepinephrine and dopamine dysfunction in the mechanisms of neurobiological disorders in the brain of patients with schizophrenia; these include the 0-methylation hypothesis and the dopamine one;
2) a group of indolamine hypotheses postulating the participation of serotonin and its metabolites, as well as other indole derivatives in the mechanisms of mental activity, the disorder of which can lead to impaired mental functions, in particular to the appearance of symptoms of schizophrenia.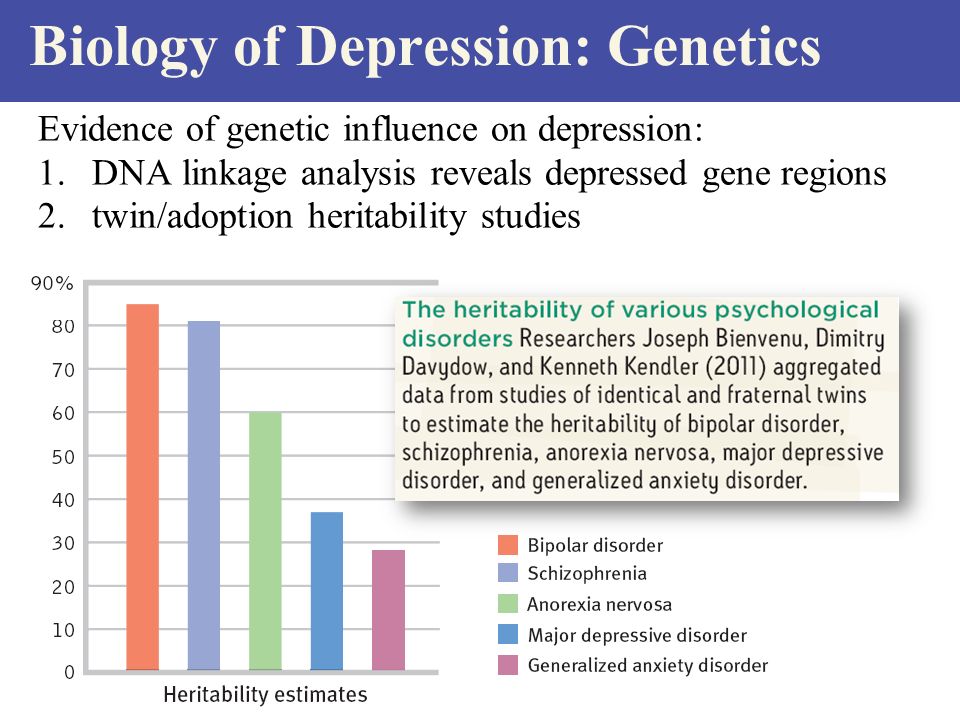 Includes concepts according to which the development of schizophrenia is associated with dysfunction of enzymatic systems involved in the exchange of biogenic amines. Enzymes such as monoamine oxidase (MAO), catechol-O-methyltransferase (COMT), dopamine-β-hydroxylase, and others attract the most attention. Numerous attempts to establish certain deviations in their content or changes in their activity in schizophrenia have led to conflicting results.
Includes concepts according to which the development of schizophrenia is associated with dysfunction of enzymatic systems involved in the exchange of biogenic amines. Enzymes such as monoamine oxidase (MAO), catechol-O-methyltransferase (COMT), dopamine-β-hydroxylase, and others attract the most attention. Numerous attempts to establish certain deviations in their content or changes in their activity in schizophrenia have led to conflicting results.
5. Psychoreactive participation
According to the old psychiatric concepts, schizophrenia is defined as independent of somatic or mental influences, that is, it occurs endogenously. However, the results of epidemiological, anamnestic, psychodynamic and follow-up studies show that psychosocial factors are also involved in the onset and course of schizophrenic psychoses. Stressful life situations (life incidents) before the onset of the disease are often not accidental. This is shown by comparative studies involving healthy people.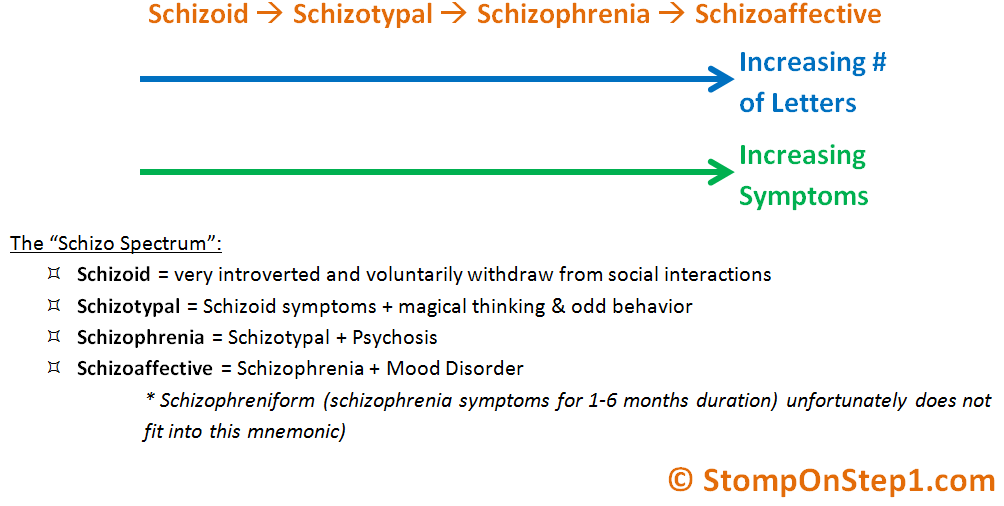 Unfortunately, it is not always possible to obtain enough information about the life of a closed and autistic patient to reliably judge the frequency and pathogenetic significance of stress loads (besides, the statistics are different).
Unfortunately, it is not always possible to obtain enough information about the life of a closed and autistic patient to reliably judge the frequency and pathogenetic significance of stress loads (besides, the statistics are different).
To date, the diagnosis of schizophrenia presents serious difficulties. From the onset of the disease to the establishment of a diagnosis, months, and sometimes even years, usually pass, which significantly complicates further treatment. In addition, the methods that are currently used are characterized by significant errors and subjectivism. Therefore, researchers dealing with this issue are faced with the task of finding a truly objective marker for the detection of schizophrenia, which would confirm this disease. The attention of scientists was focused on the search for specific blood biomarkers in schizophrenia.
History of the study of blood biomarkers in psychiatric diseases
Since ancient times, blood has been considered as a source of information about disease and health.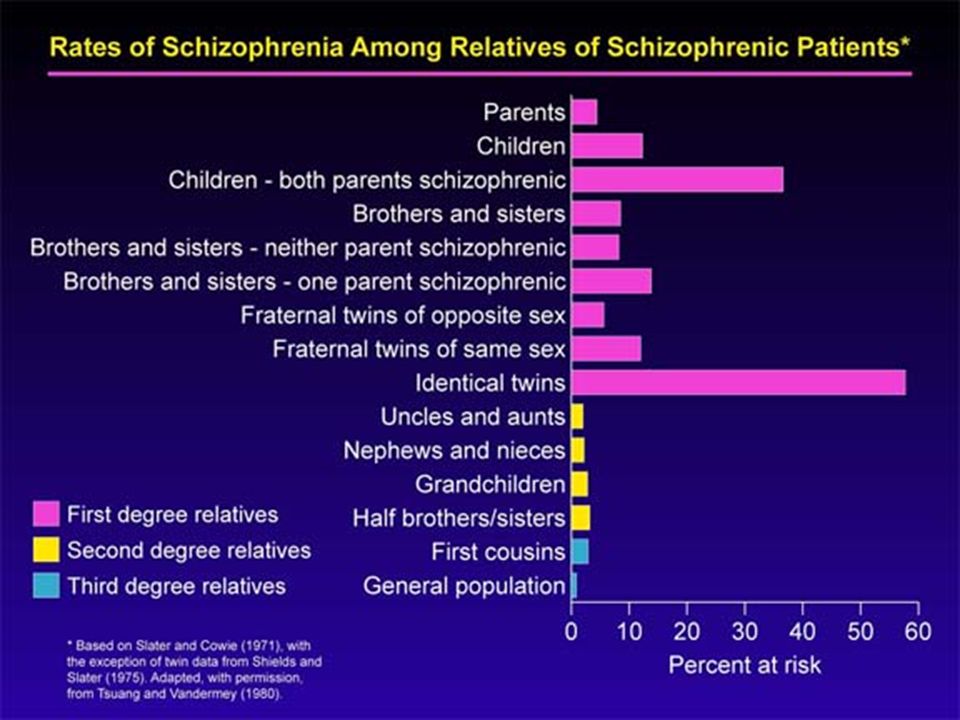 With the advent of experimental methods in medicine in the middle of the 19th century, blood tests were carried out on individuals with mental illness to identify any physical characteristics that could be used for diagnostic purposes. In the history of the development of psychiatry over the past 150 years, 4 main stages can be distinguished.
With the advent of experimental methods in medicine in the middle of the 19th century, blood tests were carried out on individuals with mental illness to identify any physical characteristics that could be used for diagnostic purposes. In the history of the development of psychiatry over the past 150 years, 4 main stages can be distinguished.
The first stage of (1854) was presented as a corpuscular paradigm (from the Greek paradeigma - an example, a sample - a set of scientific achievements recognized by the entire scientific community in a given period of time and serving as the basis and model for new scientific research) . So, in Scotland, in one of the psychiatric hospitals, Dr. W. Lauder Lindsey conducted a study of the morphology of blood cells under a microscope in patients with mental disorders. Using a then low-power microscope, he studied and counted the number of different blood corpuscles in the samples of his patients and staff. As a result of this work, it was concluded that "the various types and phases of insanity are not characteristic of a particular pathological condition of the blood.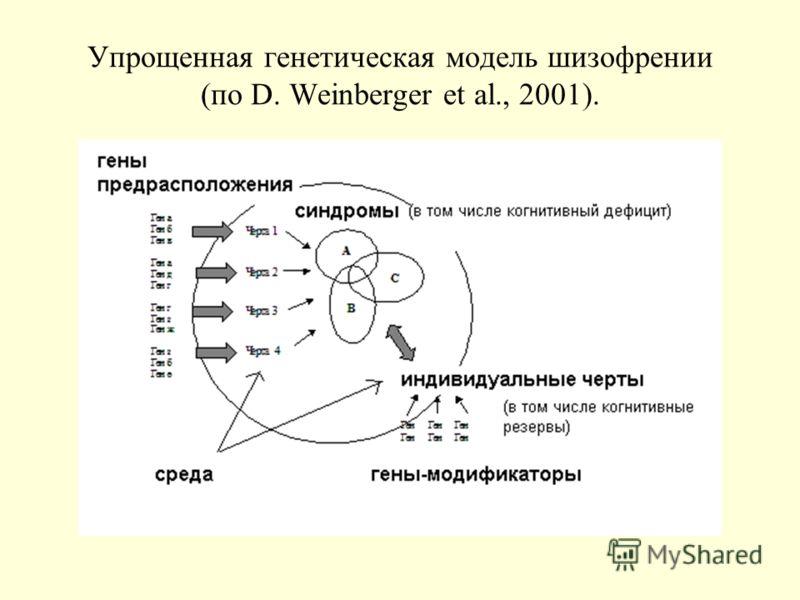 " In 1884, S. Rutherford MacPhail continued his work in this direction and found that in the early stages of mental disorders there is a shortage of blood corpuscles.
" In 1884, S. Rutherford MacPhail continued his work in this direction and found that in the early stages of mental disorders there is a shortage of blood corpuscles.
The second stage (1895) was called the metabolic paradigm. In this phase, the blood was used to determine the content of substances produced by the endocrine glands (thyroid gland, adrenal glands, pituitary gland) and known after 1905 as hormones (from Greek ορμα - stimulus).
This new paradigm was immediately taken up by psychiatrists. Hormone deficiency or overproduction was thought to be associated with psychiatric disorders in the same way as diabetes, which is caused by a deficiency of internal secretion (identified as the hormone insulin in 1921g.). The German psychiatrist E. Kraepelin in 1896 claimed that dementia praecox - "premature dementia" - is the result of an ongoing systemic metabolic disease affecting the cerebral cortex. In 1908 the Swiss psychiatrist E. Bleuer (1857-1939) proposed a more extended concept of schizophrenia.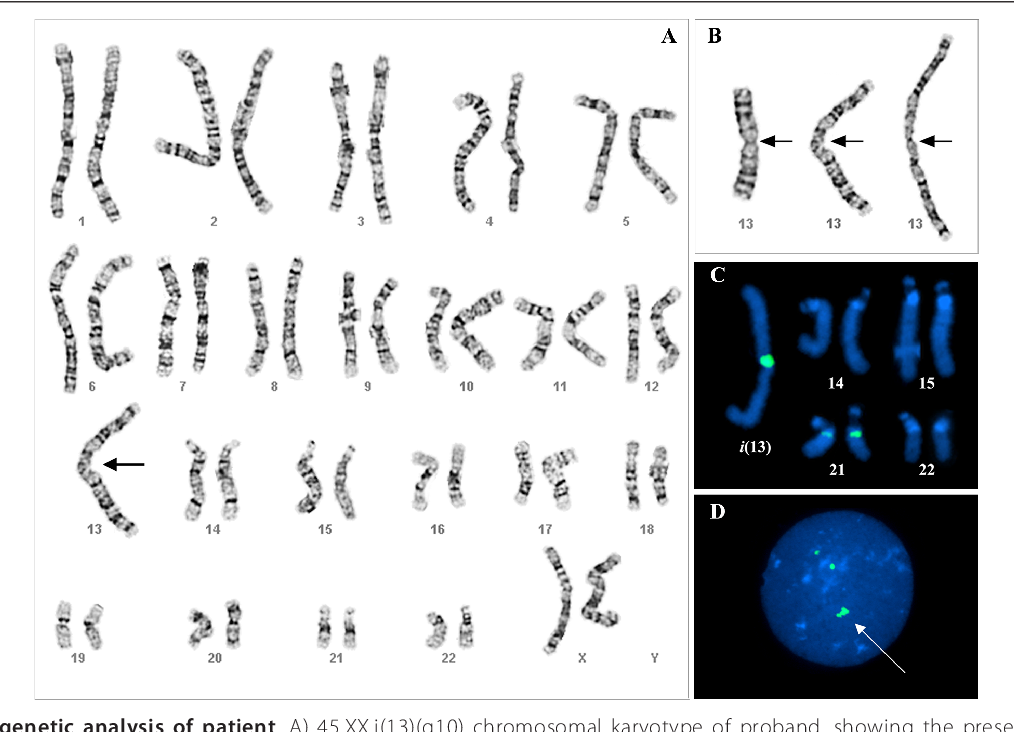 He discovered changes in the function of the pituitary gland and traced their connection with hormonal disorders in various mental disorders, including schizophrenia.
He discovered changes in the function of the pituitary gland and traced their connection with hormonal disorders in various mental disorders, including schizophrenia.
Third stage (1906) was called the immunoserodiagnostic paradigm. The development of a test (Wassermann reaction) for diagnosing neurosyphilis was the first breakthrough in biological psychiatry. The Wasserman reaction is considered the first diagnostic blood test for a discrete form of mental disorder.
There is evidence that in 1909 two German psychiatrists administered cobra venom to patients with dementia praecox and manic-depressive psychosis. It was noted that these individuals had reactions to the toxin, while healthy people did not. These data could not be reproduced in the future, they were later refuted. A much more revealing test was developed by the eminent Swiss biochemist Emil Abderhalden (1877-19fifty). In 1940 he opened the so-called. the Abdergalden reaction, the essence of which is the discovery of the so-called.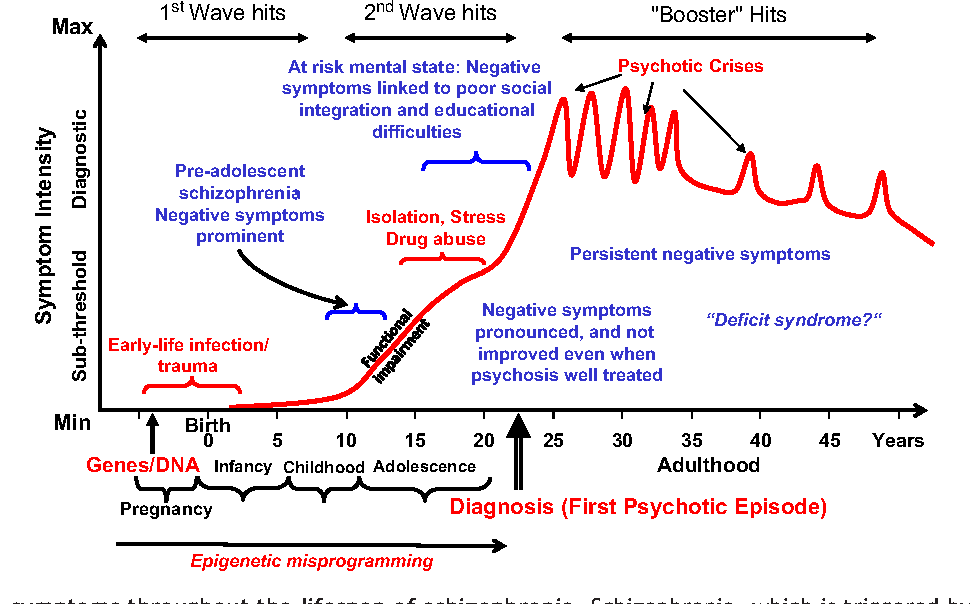 defensive enzymes produced, according to his theory, by the body when substances enter the bloodstream that are not normally found in it. Thus, by the appearance in the blood of enzymes that break down the tissue of a certain organ, it would be possible to judge the violation of its function and establish the localization of the disease process. In addition, the enzymatic defense reaction was used by the German psychiatrist August Fauser (1856-1938), who differentiated dementia praecox from manic-depressive psychosis and normal mental state in a series of studies. During 1912-1920. many scientists believed that the decoding of a blood test in patients with mental disorders had been completed. However, in a number of studies, the presence of defensive enzymes was not confirmed, and the test was recognized as doubtful.
defensive enzymes produced, according to his theory, by the body when substances enter the bloodstream that are not normally found in it. Thus, by the appearance in the blood of enzymes that break down the tissue of a certain organ, it would be possible to judge the violation of its function and establish the localization of the disease process. In addition, the enzymatic defense reaction was used by the German psychiatrist August Fauser (1856-1938), who differentiated dementia praecox from manic-depressive psychosis and normal mental state in a series of studies. During 1912-1920. many scientists believed that the decoding of a blood test in patients with mental disorders had been completed. However, in a number of studies, the presence of defensive enzymes was not confirmed, and the test was recognized as doubtful.
The fourth stage (2005-2010) was a reflection of the medical genomics paradigm. At this stage, the blood was analyzed for the presence of the target gene. However, attempts to confirm most diseases, including mental disorders, at the genome level have been ineffective. Despite 20 years of intensive research, no single gene or combination of genes has been found to significantly increase the likelihood of developing schizophrenia. In 20093 articles were published in the journal Nature presenting the results of the largest trials using the Genome-Wide Association Studies (GWAS) method. According to the data obtained, no genetic marker was identified that was significantly associated with schizophrenia.
However, attempts to confirm most diseases, including mental disorders, at the genome level have been ineffective. Despite 20 years of intensive research, no single gene or combination of genes has been found to significantly increase the likelihood of developing schizophrenia. In 20093 articles were published in the journal Nature presenting the results of the largest trials using the Genome-Wide Association Studies (GWAS) method. According to the data obtained, no genetic marker was identified that was significantly associated with schizophrenia.
To be continued.
02.10.2022 Psychiatry Troubled discord in the practice of a family doctor: how can you safely repair it?
Scientific and practical conference “Until the Day of the Medical Practitioner (19. 06.2022). International Conference on Advances in Health and Medical Science 2022 practitioners in various specialties for the development of topical nutrition and medical assistance to patients of a therapeutic profile. As part of the call, the professor of the Department of Internal Medicine of the Kharkiv National University named after I. V.N. Karazina, Doctor of Medical Sciences Marini Mykolaivna Kochueva "Anxious patient at the reception of a family doctor: how to recognize her safely repair?"....
06.2022). International Conference on Advances in Health and Medical Science 2022 practitioners in various specialties for the development of topical nutrition and medical assistance to patients of a therapeutic profile. As part of the call, the professor of the Department of Internal Medicine of the Kharkiv National University named after I. V.N. Karazina, Doctor of Medical Sciences Marini Mykolaivna Kochueva "Anxious patient at the reception of a family doctor: how to recognize her safely repair?"....
09/25/2022 Psychiatry-innovations in the treatment of post-traumatic stress disorder
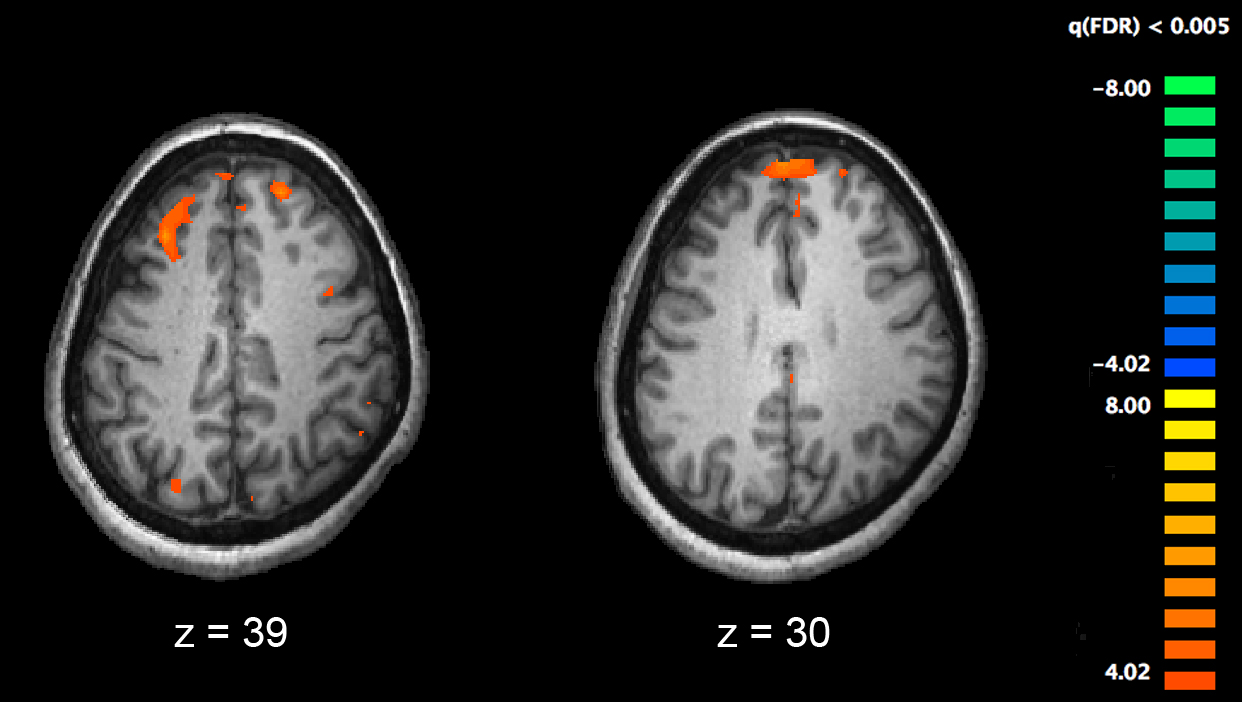
The first hour or after a traumatic experience of a person fears. Dihanna and heart beats up, blood circulation to the organs increases, mucus strains - in this way the body prepares itself to the point of insecurity. From the causes of the stressful man, there are clearly signs of, however, for the sing of the environment, it seems to be fearful for a long period of time after the stressful period. Tsey camp is called post-traumatic stress disorder (PTSD), and in the minds of the military camp, I become guilty of supralingual expansion, like the middle of the civilian population, and the middle of the military. For the preservation of the mental health of the population, it is important for the doctor to understand the principles of the development of this method in the case of an exuberant discord. About the influence of psychological trauma on the function of the brain and the specificity of the therapeutic strategy for the pathology of the disease Javanbakht Arash, psychiatrist, neurophysiologist, adjunct professor of psychiatry at Wayne University (M. Detroit, USA), director Clinics for stress, trauma and anxiety....
From the causes of the stressful man, there are clearly signs of, however, for the sing of the environment, it seems to be fearful for a long period of time after the stressful period. Tsey camp is called post-traumatic stress disorder (PTSD), and in the minds of the military camp, I become guilty of supralingual expansion, like the middle of the civilian population, and the middle of the military. For the preservation of the mental health of the population, it is important for the doctor to understand the principles of the development of this method in the case of an exuberant discord. About the influence of psychological trauma on the function of the brain and the specificity of the therapeutic strategy for the pathology of the disease Javanbakht Arash, psychiatrist, neurophysiologist, adjunct professor of psychiatry at Wayne University (M. Detroit, USA), director Clinics for stress, trauma and anxiety....
09/25/2022 PsychiatryTrivoga under the hour of war and її nasledki
A full-scale war, as if it was already over the fate, and the great trials for the Ukrainian people. Vaughn so chi іnakshe vplila on the psychological state of the skin people, including on the silence of our fellow countrymen, who hovered over the borders of Ukraine. Under the hour of large-scale military anxiety and stress, all members of the suspіlstva are experiencing it independently, because of the fact that they stink with uninterrupted reports of their podіy, that they know about the atrocities of the aggressor's army from the help of mass information. It is clear that the poor people of similar and industrial regions of Ukraine suffer the most, in which often the level of anxiety and stress “goes off the charts”. In the world in the distance, in the form of hot spots, the manifestation of things is changing. ...
Vaughn so chi іnakshe vplila on the psychological state of the skin people, including on the silence of our fellow countrymen, who hovered over the borders of Ukraine. Under the hour of large-scale military anxiety and stress, all members of the suspіlstva are experiencing it independently, because of the fact that they stink with uninterrupted reports of their podіy, that they know about the atrocities of the aggressor's army from the help of mass information. It is clear that the poor people of similar and industrial regions of Ukraine suffer the most, in which often the level of anxiety and stress “goes off the charts”. In the world in the distance, in the form of hot spots, the manifestation of things is changing. ...
09/24/2022 Diagnosis Algorithms for laboratory diagnostics of damage to the hemostasis system
The hemostasis system is a biological system that protects, on one side, saving a rare amount of circulating blood, and in the other - preventing that bleeding. The process of blood pharynx belongs to the category of the most complicated biological systems of the body and can be 3 different stages (platelet-judicial, coagulation, fibrinolysis), closely related to one by one. In clinical practice, there is a wide range of vision in the functioning of the hemostasis system, which suggests hemorrhagic thromboembolic complications. With such episodes in practice, doctors of practically all specialties can rightly be right (Table 1)....
The process of blood pharynx belongs to the category of the most complicated biological systems of the body and can be 3 different stages (platelet-judicial, coagulation, fibrinolysis), closely related to one by one. In clinical practice, there is a wide range of vision in the functioning of the hemostasis system, which suggests hemorrhagic thromboembolic complications. With such episodes in practice, doctors of practically all specialties can rightly be right (Table 1)....
Schizophrenia biomarkers found
- INVITRO
- Library
- Useful articles
- Biomarkers found.
 ..
..
7537 24 April
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
California scientists have been able to identify neurophysiological and neurocognitive biomarkers that can more accurately diagnose schizophrenia.
According to research team leader psychiatrist Gregory A. Light, the current diagnosis of schizophrenia is based on the physician's often subjective judgment. "Even the best of psychiatrists face problems in diagnosis due to the unclear clinical picture and the incomplete information they receive from the patient," Light is quoted by ScienceDaily. “Many people with schizophrenia simply cannot adequately convey what is happening to them. ” That is why, Light emphasized, the need for a diagnostic device that gives an unbiased assessment of the patient's condition is extremely high.
” That is why, Light emphasized, the need for a diagnostic device that gives an unbiased assessment of the patient's condition is extremely high.
The markers known as endophenotypes may ultimately be a boon for both clinicians and those who are diagnosed only on the subjective feelings of doctors.
Light's group involved more than five hundred people for research. Comparative analysis was carried out on the basis of the results of testing 341 patients with schizophrenia and 205 healthy people from the control group. The study identified a number of features that the authors claim are reliable, accurate, consistent, and long-term indicators of a person having schizophrenia. Moreover, regardless of the severity of the symptoms of the disease.
Biomarkers were selected based on a series of neurophysiological and neurocognitive tests. Attention and memory, brain response to external stimuli, basic perception processes, and much more were assessed. After the processing of the results revealed the characteristic features inherent in patients with schizophrenia, the experiment was repeated a year later on a narrower group of participants.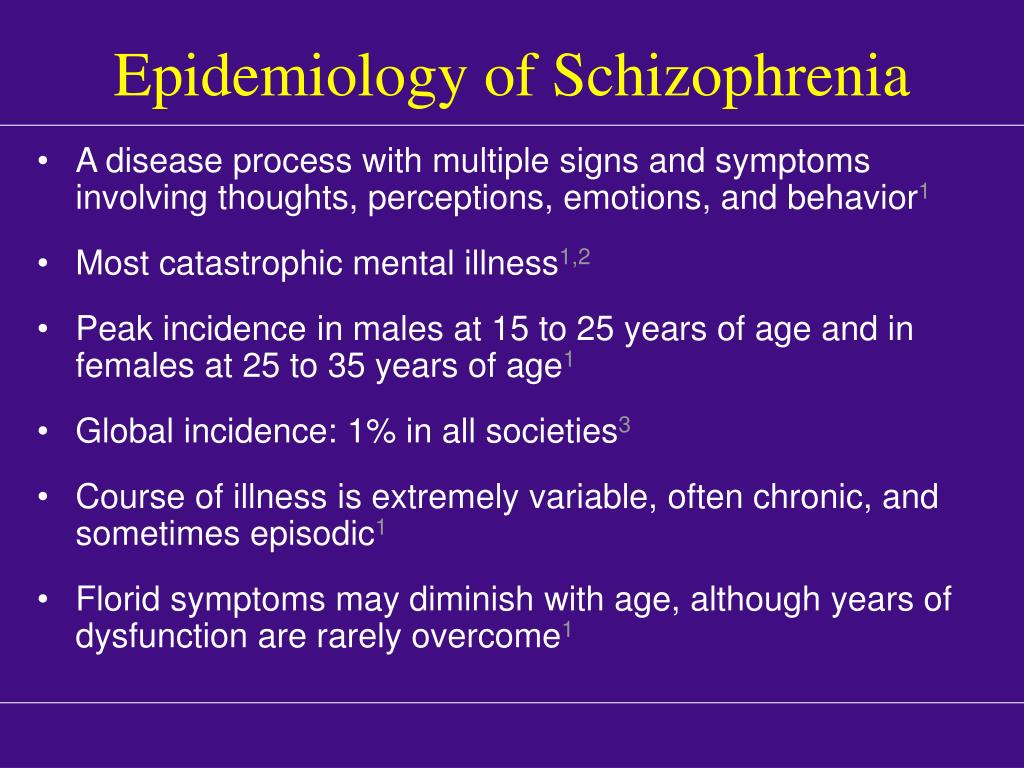 He showed that the absolute majority of previously detected abnormal characteristics, their corresponding indicators and ratios, did not change over time, despite fluctuations in the clinical picture of the patients' disease.
He showed that the absolute majority of previously detected abnormal characteristics, their corresponding indicators and ratios, did not change over time, despite fluctuations in the clinical picture of the patients' disease.
On this basis, the authors believe that the biomarkers they have selected can be considered as endophenotypes of schizophrenia in the course of further clinical and genomic studies of this disease.
Endophenotype is an intermediate link that reflects the relationship between genetic prerequisites and clinical manifestations of the disease.
Schizophrenia is a polymorphic mental illness characterized by the disintegration of thought processes and emotional reactions. The most common manifestations of the disease are auditory hallucinations, paranoid or fantastic delusions, disorganized speech and thinking against the background of impaired performance. The reason for the development of schizophrenia has not yet been identified, but it is noted that the disease is characterized by a pronounced genetic component - this disease often manifests itself in members of the same family.
| Drawings of psychiatric patients | ||
Based on UC San Diego.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Recommendations
-
Infectious disease doctor: the acute phase of the pandemic has passed, but the virus has not gone away
13472 16 March
-
Infectionist notes
13264 08 October
-
Infectionist notes
18002 July, 12
Show more
Objectively about pseudoscientific. Yogurt as a biological weapon: Is it necessary to treat dysbacteriosis?
Yogurt as a biological weapon: Is it necessary to treat dysbacteriosis?
Recently, advertising often scares us with a diagnosis of "dysbacteriosis". This is the name of the violation of the microflora, which we are called upon to urgently treat with Eubiotics, Probiotics, Symbiotics and Live Yoghurts, in which hardworking Bifido- and Lactobacilli swarm, looking forward to getting into our inner world in order to create and create there, in the dark and warm, good ... In fact, most of this information is pure myth.
More
Exhaust gases cause thrombosis
American scientists have found that air pollution with exhaust gases increases the risk of thrombosis.
More
Fourth trimester: how to plan life after pregnancy?
National survey conducted in March 2019 by a research company on behalf of the Florida Hospitals Network shows that many women are ill-prepared for the physical and emotional changes postpartum
More
Smoking, diabetes and high blood pressure can negatively affect the brain
A number of factors such as smoking and high blood pressure can negatively affect the brain.