Schizoaffective dsm 5 criteria
Schizoaffective Disorder - StatPearls - NCBI Bookshelf
Continuing Education Activity
Schizoaffective disorder is among the most frequently misdiagnosed psychiatric disorders in clinical practice. Due to concerns about the reliability and utility of the diagnostic criteria for schizoaffective disorder, some researchers have proposed revisions, while others have suggested altogether removing the diagnosis from the Diagnostic and Statistical Manual of Mental Disorders. This activity describes limitations and challenges related to the diagnostic criteria and highlights the interprofessional team's role in caring for patients with psychiatric disorders.
Objectives:
Describe the pathophysiology of schizoaffective disorder.
Outline the classic clinical presentation of a patient with schizoaffective disorder.
Summarize the treatment options for patients with schizoaffective disorder.
Describe the importance of collaboration and communication amongst the interprofessional team to improve patient compliance with treatment and thus improve outcomes for patients with schizoaffective disorder.
Access free multiple choice questions on this topic.
Introduction
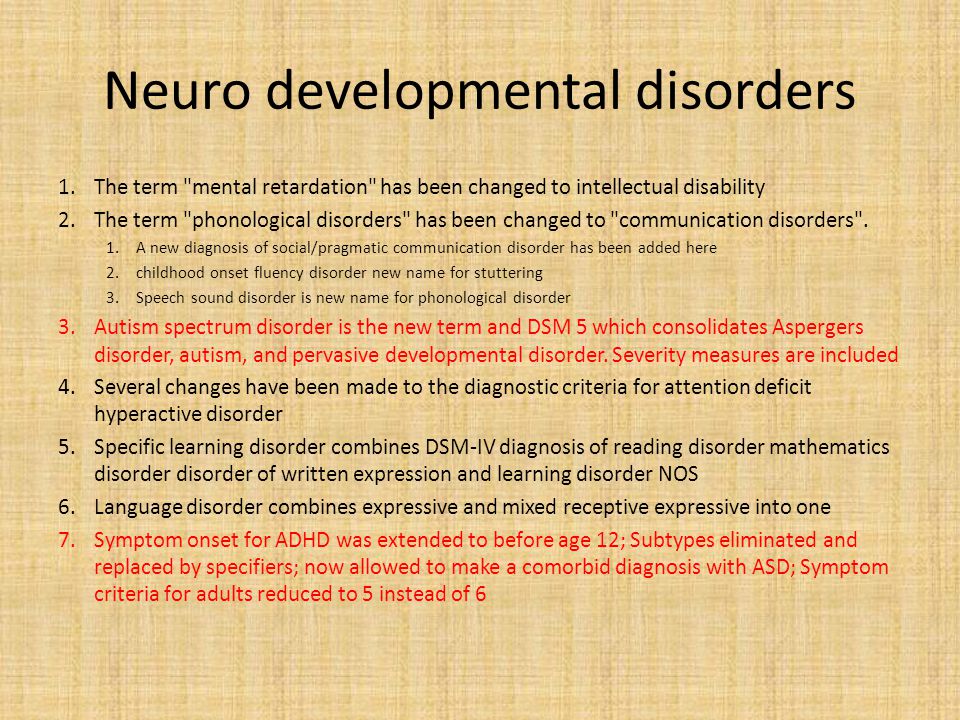
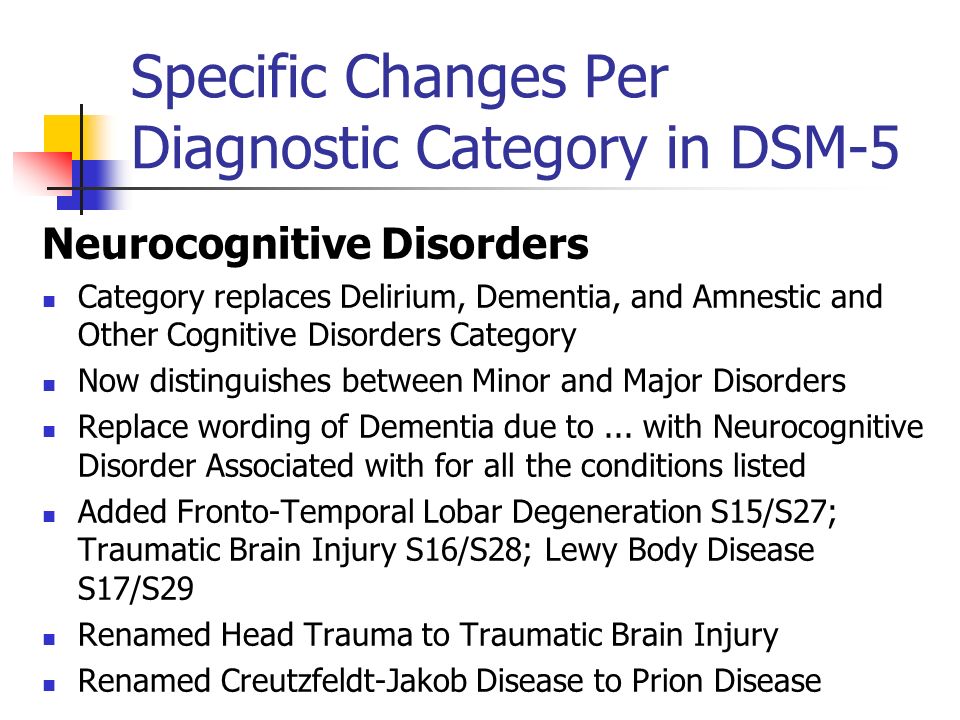
Schizoaffective disorder is one of the most misdiagnosed psychiatric disorders in clinical practice.[1] In fact, some researchers have proposed revisions to the diagnostic criteria, and others have suggested removing the diagnosis altogether from the DSM-5.[2] There were significant concerns regarding the reliability and utility of the diagnosis when it was first introduced in the DSM.[2] The challenges lie within the diagnostic criteria itself since the disorder is part of a spectrum that shares criteria with many other prominent psychiatric disorders found in clinical practice.
Etiology
The term schizoaffective disorder first appeared as a subtype of schizophrenia in the first edition of the DSM. It eventually became its own diagnosis despite a lack of evidence for unique differences in etiology or pathophysiology. Therefore, there have been no conclusive studies on the etiology of the disorder.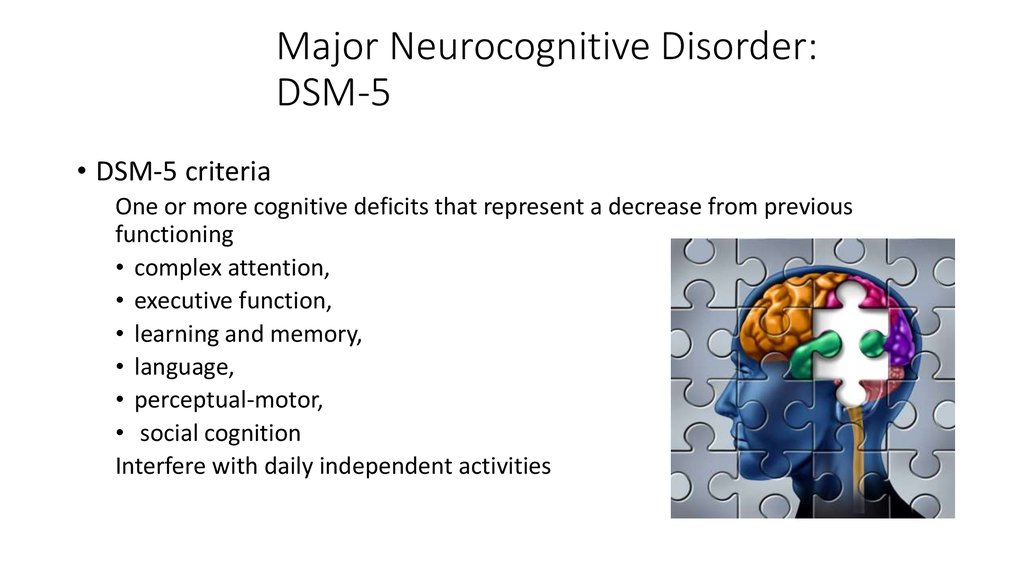 However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
Some studies show that as high as 50% of people with schizophrenia also have comorbid depression.[3] The pathogenesis of both mood disorders and schizophrenia is multifactorial and covers a range of risk factors, including genetics, social factors, trauma, and stress.[4] Among people with schizophrenia, there is a possible increased risk for first-degree relatives for schizoaffective disorder and vice-versa; there may be increased risk among individuals for schizoaffective disorder who have a first-degree relative with bipolar disorder schizophrenia, or schizoaffective disorder.[5]
Epidemiology
The diagnostic criteria for schizoaffective disorder have been reworded and addended since its inclusion in the DSM, making it difficult to subsequently conduct appropriate epidemiological studies. Thus, there have been no large-scale studies on the epidemiology, incidence, or prevalence of schizoaffective disorder.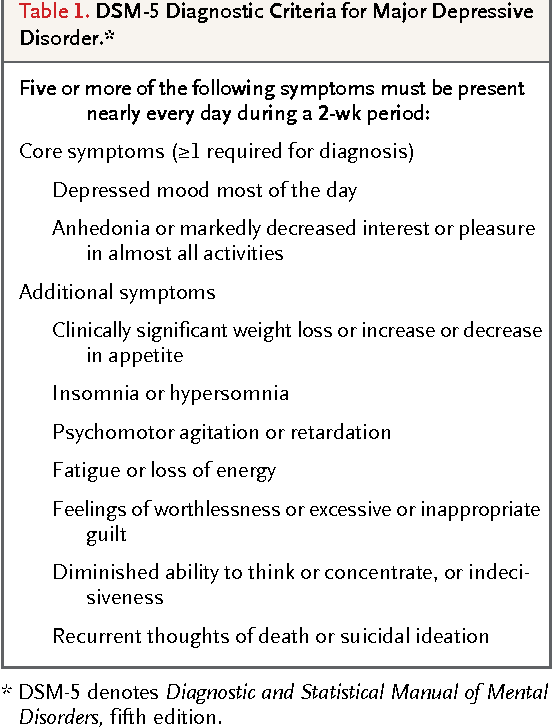 Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Pathophysiology
The exact pathophysiology of schizoaffective disorder is currently unknown. Some studies have shown that abnormalities in dopamine, norepinephrine, and serotonin may play a role.[9] Also, white matter abnormalities in multiple areas of the brain, particularly the right lentiform nucleus, left temporal gyrus, and right precuneus, are associated with schizophrenia and schizoaffective disorder.[10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
History and Physical
The first step in evaluation is obtaining a complete medical history while focusing on the diagnostic criteria for schizoaffective disorder.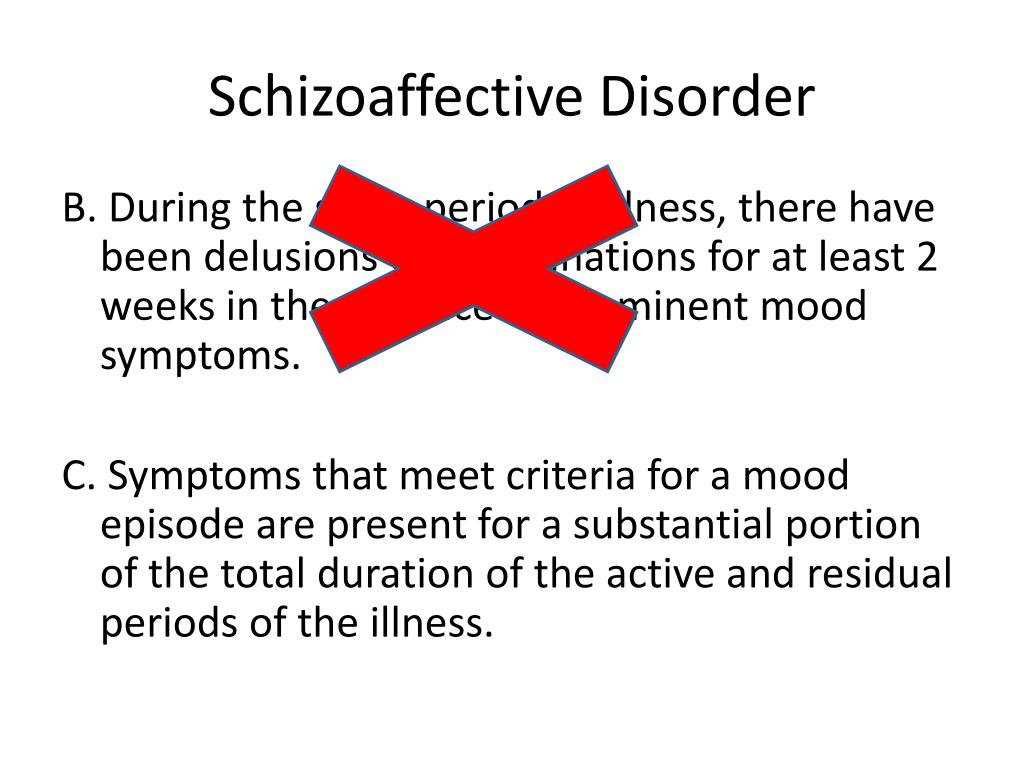
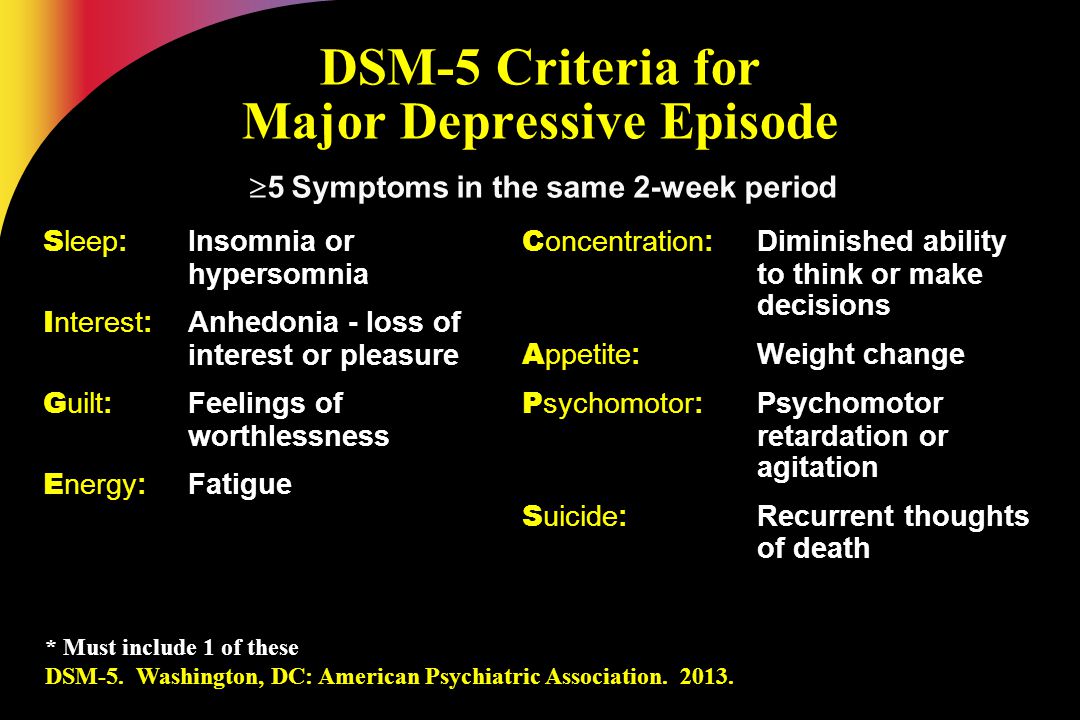
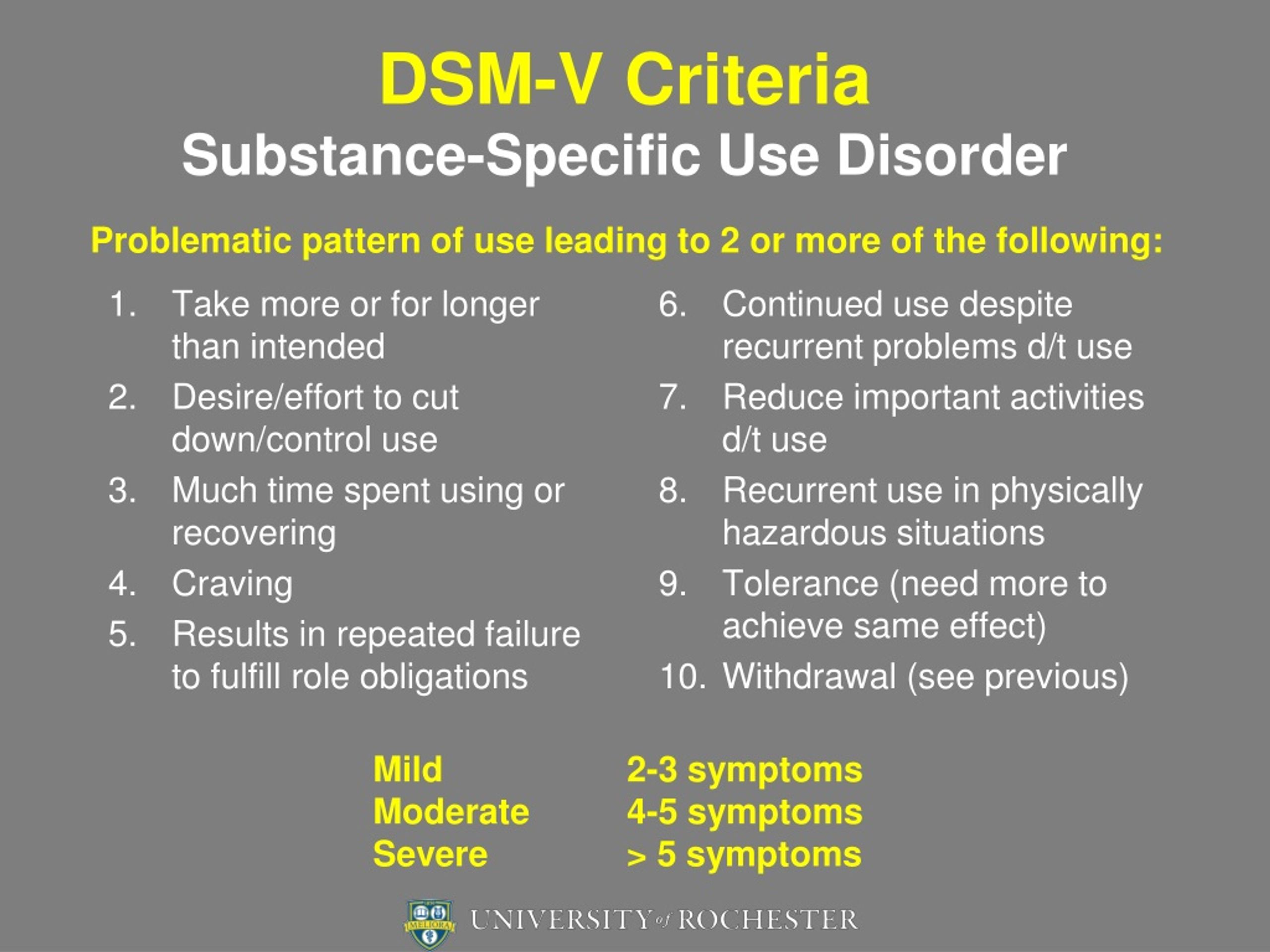
The specific DSM-5 criteria for schizoaffective disorder are as follows[1]:
A. An uninterrupted duration of illness during which there is a major mood episode (manic or depressive) in addition to criterion A for schizophrenia; the major depressive episode must include depressed mood.
Criterion A for schizophrenia is as follows[13]:
Two or more of the following presentations, each present for a significant amount of time during a 1-month period (or less if successfully treated). At least one of these must be from the first three below.
Delusions
Hallucinations
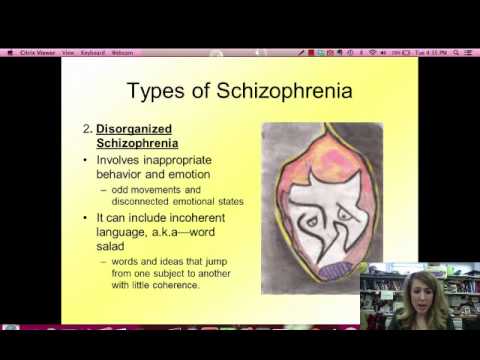
Disorganized speech (e.g., frequent derailment or incoherence).
Grossly disorganized or catatonic behavior
Negative symptoms (i.e., diminished emotional expression or avolition.)
B. Hallucinations and delusions for two or more weeks in the absence of a major mood episode (manic or depressive) during the entire lifetime duration of the illness.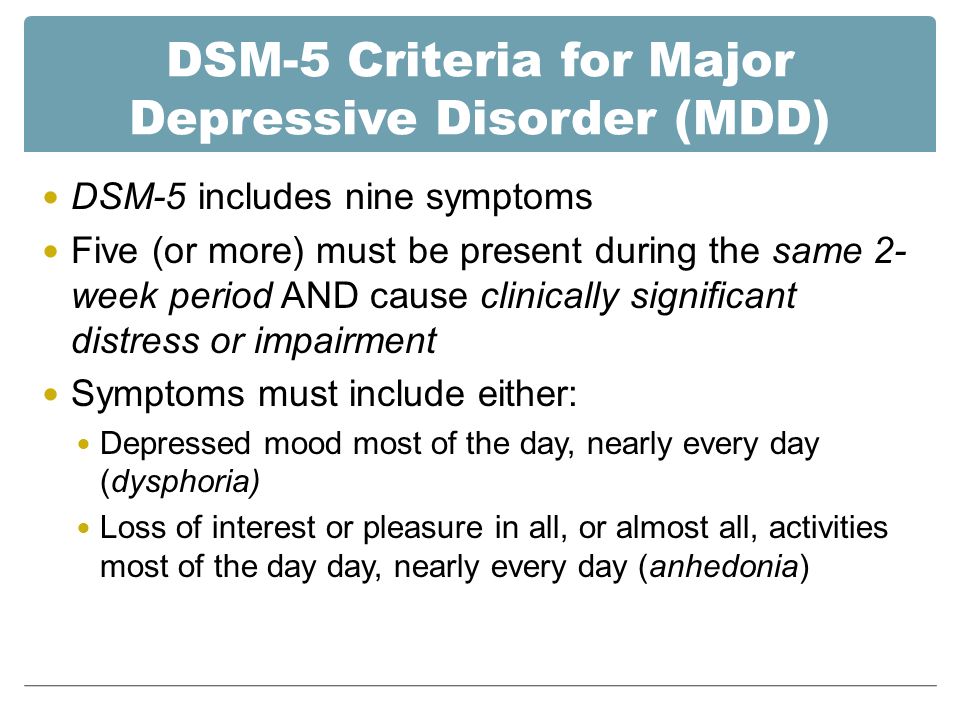
C. Symptoms that meet the criteria for a major mood episode are present for most of the total duration of both the active and residual portions of the illness.
D. The disturbance is not the result of the effects of a substance (e.g., a drug of misuse or a medication) or another underlying medical condition.
The following are specifiers based on the primary mood episode as part of the presentation.
Bipolar type: includes episodes of mania and sometimes major depression.
Depressive type: includes only major depressive episodes.
Please note the patient must meet the criteria for A-D above to be diagnosed with schizoaffective disorder. It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
The next step of evaluation is the objective and physical portion. A thorough mental status examination (MSE), physical examination, and neurologic examination should be completed to help rule out other differential diagnoses.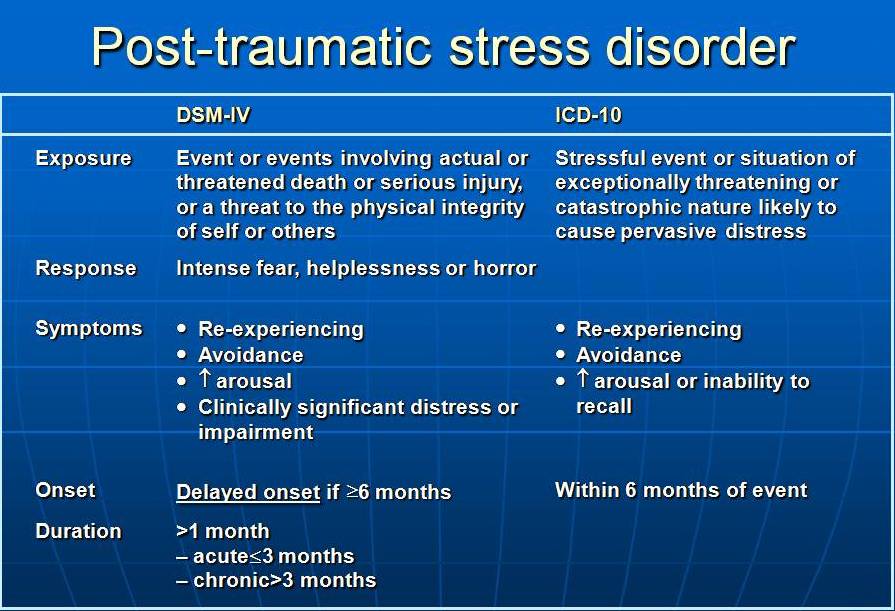
Evaluation
The following workup is optional and typically not needed to make the diagnosis. The history and physical are the mainstays of diagnosis. However, some elect to include additional tests or imaging to aid in the diagnosis, such as MRI (magnetic resonance imaging), EEG (electroencephalography), or CT (computed tomography).
Laboratory studies are tailored to the patient’s history, especially for those who have an atypical presentation.
Complete blood count (CBC)
Lipid panel
Urine drug screen
Urine pregnancy test
Urinalysis
Thyroid-stimulating hormone (TSH) level
Rapid plasma reagent
HIV test
If the patient's neurologic exam is found to be aberrant, performing a brain MRI or CT to rule out any suspected intracranial abnormalities may be considered.
Treatment / Management
The treatment of schizoaffective disorder typically involves both pharmacotherapy and psychotherapy.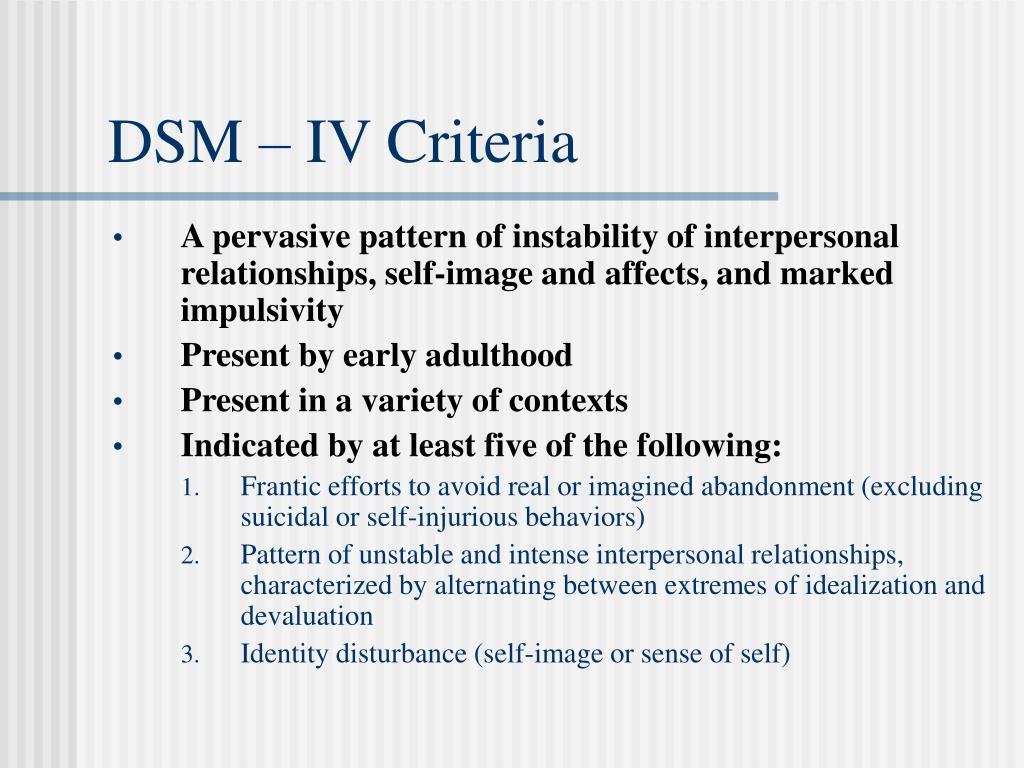 The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
Pharmacotherapy
Antipsychotics: Used to target psychosis and aggressive behavior in schizoaffective disorder. Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
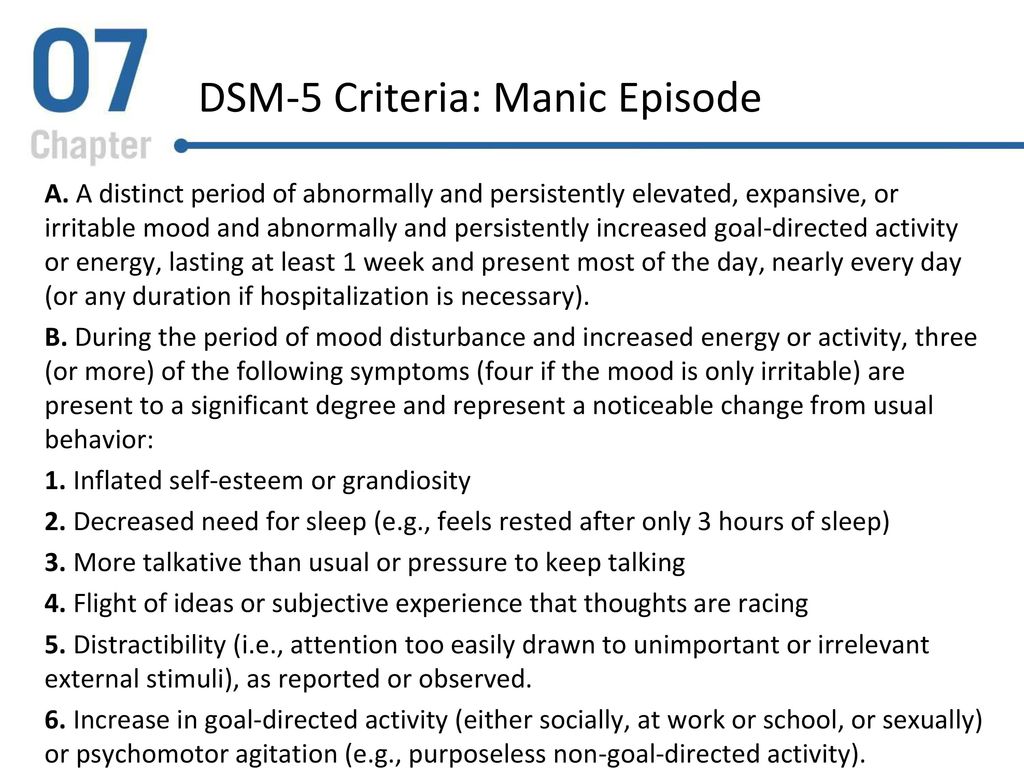
Mood-stabilizers: Patients who have periods of distractibility, indiscretion, grandiosity, a flight of ideas, increased goal-directed activity, decreased need for sleep, and who are hyper-verbal fall under the bipolar-specifier for schizoaffective disorder. Consider the use of mood-stabilizers if the patient has a history of manic or hypomanic symptoms. These include medications such as lithium, valproic acid, carbamazepine, oxcarbazepine, and lamotrigine which target mood dysregulation.[21][22][23][24]
Antidepressants: Used to target depressive symptoms in schizoaffective disorder. Selective-serotonin reuptake inhibitors (SSRIs) are preferred due to lower risk for adverse drug effects and tolerability when compared to tricyclic antidepressants and selective norepinephrine reuptake inhibitors.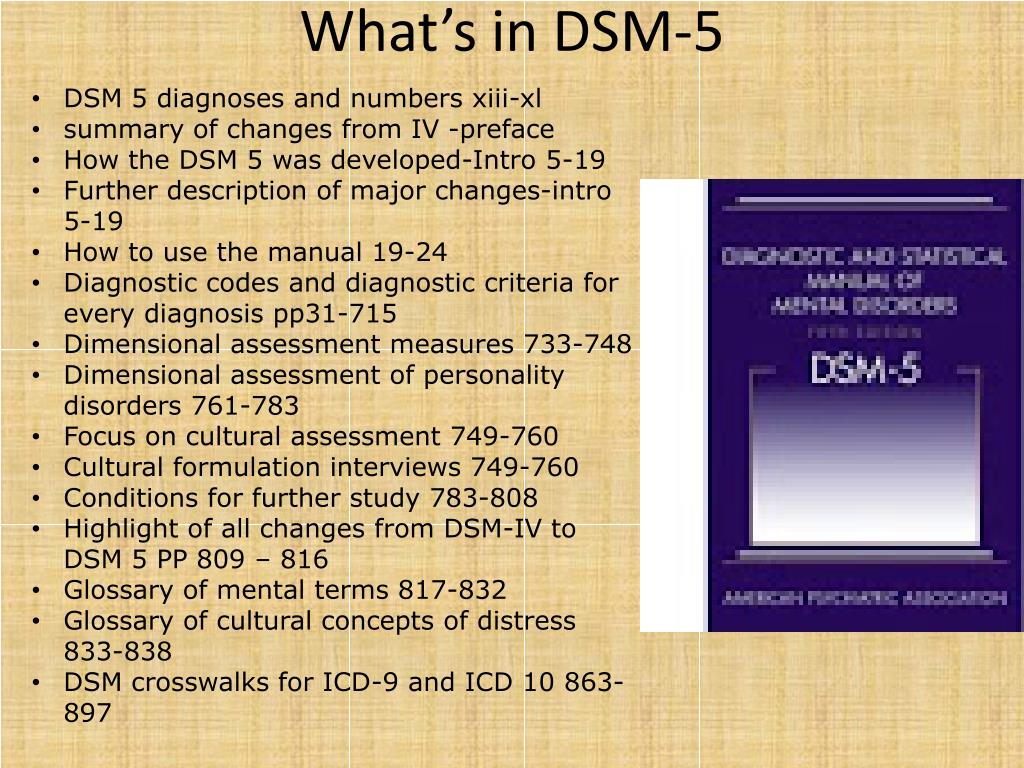 [25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
[25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
Psychotherapy
Patients who have schizoaffective disorder can benefit from psychotherapy, as is the case with most mental disorders.
Treatment plans should incorporate individual therapy, family therapy, and psychoeducational programs. The aim is to develop their social skills and improve cognitive functioning to prevent relapse and possible rehospitalization.[27] This treatment plan includes education about the disorder, etiology, and treatment.
Individual therapy: This type of treatment aims to normalize thought processes and better help the patient understand the disorder and reduce symptoms. Sessions focus on everyday goals, social interactions, and conflict; this includes social skills training and vocational training.
Family and/or group therapy: Family involvement is crucial in the treatment of this schizoaffective disorder. [28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
[28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
ECT (Electroconvulsive Therapy)
ECT is usually a last resort treatment. However, not only has it been used in urgent cases and treatment resistance, but it should also merit consideration in augmentation of current pharmacotherapy.[29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
Differential Diagnosis
Because of criteria that encompass both psychotic and mood symptoms, schizoaffective disorder is easy to mistake for other mental disorders. Disorders that must be ruled out during the workup of schizoaffective disorder include:
Schizophrenia and Schizoaffective Disorder: There has to be a definite period of at least two weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms to diagnose schizoaffective disorder. However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.
However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.
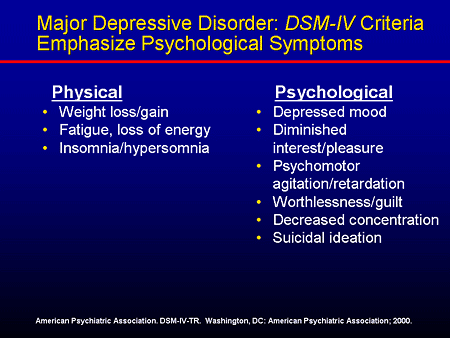
Major Depressive Disorder Psychotic Features and Schizoaffective Disorder: Patients with major depression with psychotic features (MDD with PF) only experience psychotic features during their mood episodes. In contrast, schizoaffective requires at least 2 weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms. Patients with MDD with PF do not meet criterion A of schizoaffective disorder.
Bipolar Disorder and Schizoaffective Disorder: Similar to the contrasts of MDD w/ PF, patients with bipolar disorder with psychotic features only experience psychotic features (delusions and hallucinations) during a manic episode.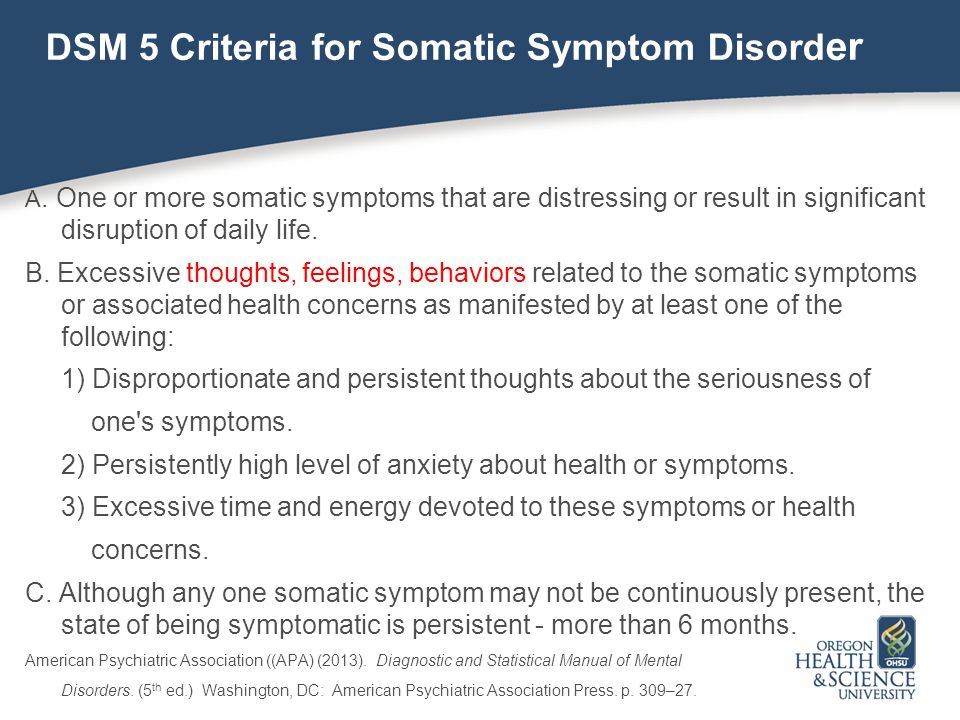 Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Prognosis
Given that the diagnostic criteria of schizoaffective disorder change periodically, prognostic studies have been challenging to conduct. However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
Complications
Left untreated, schizoaffective disorder has many ramifications in both social functioning and activities of daily living. These include unemployment, isolation, impaired ability to care for self, etc. Untreated mental disorders have more than just social and functional consequences.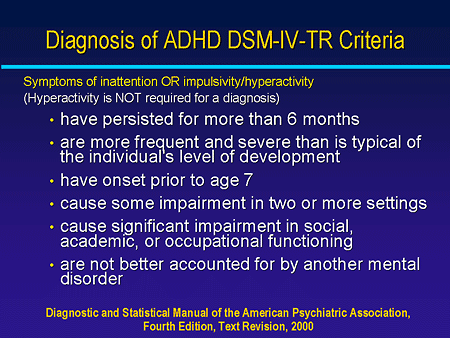 Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Deterrence and Patient Education
Patients and their families can benefit from education regarding the condition and steps to manage it.
Encourage the patient to undergo treatment and rehabilitation
Cognitive behavior therapy
Interventions for drug and alcohol misuse
Social skills training
Provide emotional and life support
Teach them skills and measures that promote self-care and independence
Supported employment
Pearls and Other Issues
Working through the differential of schizoaffective disorder is often a daunting task, and many clinicians continue to have trouble making the diagnosis.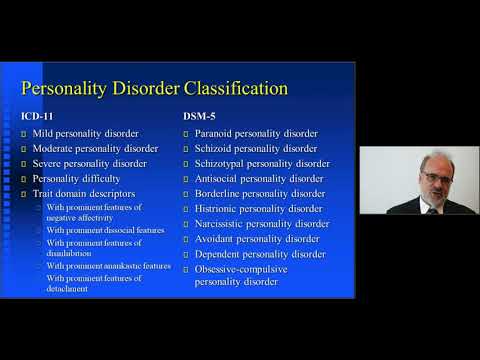 [2] A few considerations when working through the differential diagnosis include:
[2] A few considerations when working through the differential diagnosis include:
Observe the criteria for each diagnosis carefully.
Do not "fill in blanks" with preconceived notions about the patient's history. Take what the patient tells you and what family/collateral information tells you when working through a differential.
Time frames often give clues towards one specific diagnosis. Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.
Criterion B of schizoaffective disorder is key for the following reasons. One must tease out a 2 week or longer period of just psychotic symptoms in the patient's history. If one finds that the patient has always had mood symptoms during their entire illness, the diagnosis by definition is not a schizoaffective disorder.
Enhancing Healthcare Team Outcomes
As with most mental disorders, schizoaffective disorder is best managed by an interprofessional team including psychiatric specialty nurses and pharmacists, and clinicians that practice close interprofessional communication. [Level 5] Pharmacotherapy, psychotherapy, skills training, and vocational training work in tandem to create a holistic treatment plan. In addition to what the information alluded to in previous sections, psychotherapy strongly influences medication compliance.[34] An ideal treatment course to improve outcomes around patient-centered care may include:
Early detection of mental disorder in the primary care setting
Referral to a psychiatrist for further evaluation
A psychiatrist would stabilize the patient with pharmacotherapy or defer to a clinical psychologist for diagnosis or additional therapy
If the patient requires inpatient hospitalization, the nursing staff and case management become crucial in providing optimal patient care
It is critical to determine if the patient is competent to make healthcare decisions independently; otherwise, a proxy must be a consideration.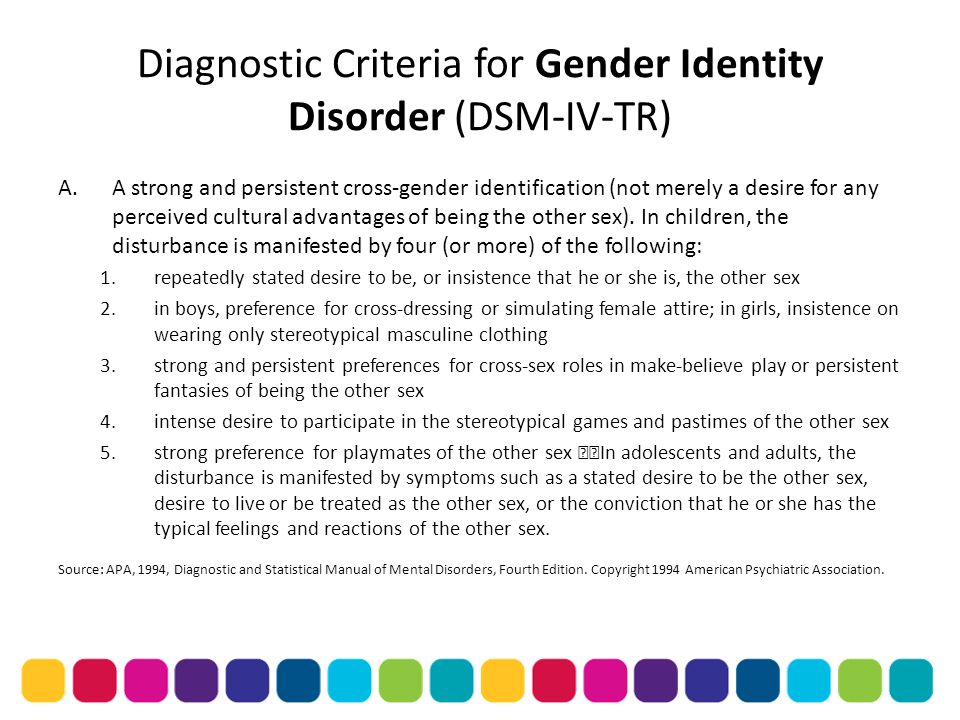
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malaspina D, Owen MJ, Heckers S, Tandon R, Bustillo J, Schultz S, Barch DM, Gaebel W, Gur RE, Tsuang M, Van Os J, Carpenter W. Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]
- 2.
Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014 Feb;264(1):29-34. [PMC free article: PMC4207055] [PubMed: 23625467]
- 3.
Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009 Mar;35(2):383-402. [PMC free article: PMC2659306] [PubMed: 19011234]
- 4.
Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry.
 2006 Jan;163(1):115-24. [PubMed: 16390898]
2006 Jan;163(1):115-24. [PubMed: 16390898]- 5.
Laursen TM, Munk-Olsen T, Nordentoft M, Bo Mortensen P. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a danish population-based cohort. J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]
- 6.
Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long-term course. Acta Psychiatr Scand. 1990 Nov;82(5):352-8. [PubMed: 2281805]
- 7.
Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008 Dec;4(6):1089-109. [PMC free article: PMC2646642] [PubMed: 19337453]
- 8.
Azorin JM, Kaladjian A, Fakra E. [Current issues on schizoaffective disorder]. Encephale.
 2005 May-Jun;31(3):359-65. [PubMed: 16142051]
2005 May-Jun;31(3):359-65. [PubMed: 16142051]- 9.
Meltzer HY, Arora RC, Metz J. Biological studies of schizoaffective disorders. Schizophr Bull. 1984;10(1):49-70. [PubMed: 6422546]
- 10.
Antonius D, Prudent V, Rebani Y, D'Angelo D, Ardekani BA, Malaspina D, Hoptman MJ. White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]
- 11.
Radonić E, Rados M, Kalember P, Bajs-Janović M, Folnegović-Smalc V, Henigsberg N. Comparison of hippocampal volumes in schizophrenia, schizoaffective and bipolar disorder. Coll Antropol. 2011 Jan;35 Suppl 1:249-52. [PubMed: 21648342]
- 12.
Smith MJ, Wang L, Cronenwett W, Mamah D, Barch DM, Csernansky JG. Thalamic morphology in schizophrenia and schizoaffective disorder. J Psychiatr Res. 2011 Mar;45(3):378-85. [PMC free article: PMC2996474] [PubMed: 20797731]
- 13.
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013 Oct;150(1):3-10. [PubMed: 23800613]
- 14.
Vieta E. Developing an individualized treatment plan for patients with schizoaffective disorder: from pharmacotherapy to psychoeducation. J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]
- 15.
Cascade E, Kalali AH, Buckley P. Treatment of schizoaffective disorder. Psychiatry (Edgmont). 2009 Mar;6(3):15-7. [PMC free article: PMC2719459] [PubMed: 19724749]
- 16.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002 Sep;63(9):763-71. [PubMed: 12363115]
- 17.
Addington DE, Pantelis C, Dineen M, Benattia I, Romano SJ.
 Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]
Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]- 18.
Ciapparelli A, Dell'Osso L, Bandettini di Poggio A, Carmassi C, Cecconi D, Fenzi M, Chiavacci MC, Bottai M, Ramacciotti CE, Cassano GB. Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]
- 19.
Ghaemi SN, Goodwin FK. Use of atypical antipsychotic agents in bipolar and schizoaffective disorders: review of the empirical literature. J Clin Psychopharmacol. 1999 Aug;19(4):354-61. [PubMed: 10440464]
- 20.
Gunasekara NS, Spencer CM, Keating GM. Spotlight on ziprasidone in schizophrenia and schizoaffective disorder.
 CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]
CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]- 21.
Baethge C, Gruschka P, Berghöfer A, Bauer M, Müller-Oerlinghausen B, Bschor T, Smolka MN. Prophylaxis of schizoaffective disorder with lithium or carbamazepine: outcome after long-term follow-up. J Affect Disord. 2004 Apr;79(1-3):43-50. [PubMed: 15023479]
- 22.
Bogan AM, Brown ES, Suppes T. Efficacy of divalproex therapy for schizoaffective disorder. J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]
- 23.
Dietrich DE, Kropp S, Emrich HM. [Oxcarbazepine in the treatment of affective and schizoaffective disorders]. Fortschr Neurol Psychiatr. 2003 May;71(5):255-64. [PubMed: 12740757]
- 24.
Leucht S, McGrath J, White P, Kissling W. Carbamazepine for schizophrenia and schizoaffective psychoses. Cochrane Database Syst Rev. 2002;(3):CD001258. [PubMed: 12137621]
- 25.
Koenig AM, Thase ME. First-line pharmacotherapies for depression - what is the best choice? Pol Arch Med Wewn.
 2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]
2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]- 26.
McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. Prim Care Companion CNS Disord. 2014;16(5) [PMC free article: PMC4321017] [PubMed: 25667812]
- 27.
Fitzgerald P, de Castella A, Arya D, Simons WR, Eggleston A, Meere S, Kulkarni J. The cost of relapse in schizophrenia and schizoaffective disorder. Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]
- 28.
Pharoah FM, Rathbone J, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2003;(4):CD000088. [PubMed: 14583908]
- 29.
Phutane VH, Thirthalli J, Kesavan M, Kumar NC, Gangadhar BN. Why do we prescribe ECT to schizophrenia patients? Indian J Psychiatry. 2011 Apr;53(2):149-51. [PMC free article: PMC3136018] [PubMed: 21772648]
- 30.
Iancu I, Pick N, Seener-Lorsh O, Dannon P. Patients with schizophrenia or schizoaffective disorder who receive multiple electroconvulsive therapy sessions: characteristics, indications, and results.
 Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]
Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]- 31.
Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, Dube KC, Ganev K, Giel R, an der Heiden W, Holmberg SK, Janca A, Lee PW, León CA, Malhotra S, Marsella AJ, Nakane Y, Sartorius N, Shen Y, Skoda C, Thara R, Tsirkin SJ, Varma VK, Walsh D, Wiersma D. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]
- 32.
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010 Nov;24(4 Suppl):81-90. [PMC free article: PMC2951591] [PubMed: 20923923]
- 33.
Suominen K, Isometsä E, Heilä H, Lönnqvist J, Henriksson M. General hospital suicides--a psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002 Nov-Dec;24(6):412-6. [PubMed: 12490343]
- 34.
Stentzel U, van den Berg N, Schulze LN, Schwaneberg T, Radicke F, Langosch JM, Freyberger HJ, Hoffmann W, Grabe HJ.
 Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
Schizoaffective Disorder - StatPearls - NCBI Bookshelf
Continuing Education Activity
Schizoaffective disorder is among the most frequently misdiagnosed psychiatric disorders in clinical practice. Due to concerns about the reliability and utility of the diagnostic criteria for schizoaffective disorder, some researchers have proposed revisions, while others have suggested altogether removing the diagnosis from the Diagnostic and Statistical Manual of Mental Disorders. This activity describes limitations and challenges related to the diagnostic criteria and highlights the interprofessional team's role in caring for patients with psychiatric disorders.
Objectives:
Describe the pathophysiology of schizoaffective disorder.
Outline the classic clinical presentation of a patient with schizoaffective disorder.
Summarize the treatment options for patients with schizoaffective disorder.
Describe the importance of collaboration and communication amongst the interprofessional team to improve patient compliance with treatment and thus improve outcomes for patients with schizoaffective disorder.
Access free multiple choice questions on this topic.
Introduction
Schizoaffective disorder is one of the most misdiagnosed psychiatric disorders in clinical practice.[1] In fact, some researchers have proposed revisions to the diagnostic criteria, and others have suggested removing the diagnosis altogether from the DSM-5.[2] There were significant concerns regarding the reliability and utility of the diagnosis when it was first introduced in the DSM.[2] The challenges lie within the diagnostic criteria itself since the disorder is part of a spectrum that shares criteria with many other prominent psychiatric disorders found in clinical practice.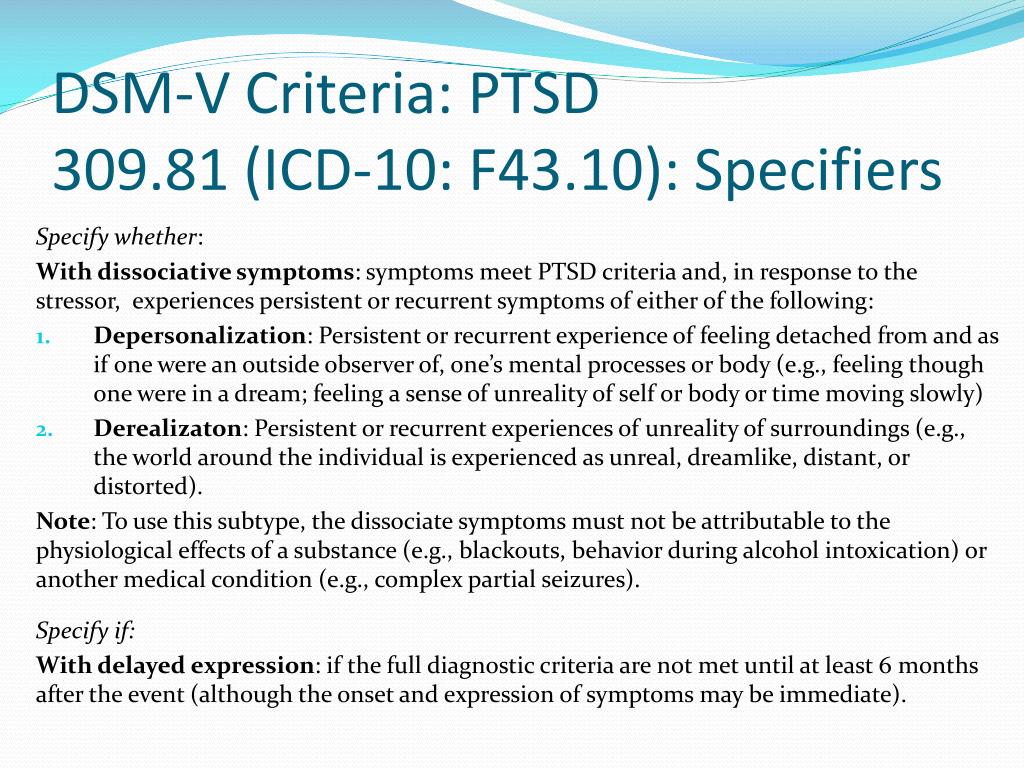
Etiology
The term schizoaffective disorder first appeared as a subtype of schizophrenia in the first edition of the DSM. It eventually became its own diagnosis despite a lack of evidence for unique differences in etiology or pathophysiology. Therefore, there have been no conclusive studies on the etiology of the disorder. However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
Some studies show that as high as 50% of people with schizophrenia also have comorbid depression.[3] The pathogenesis of both mood disorders and schizophrenia is multifactorial and covers a range of risk factors, including genetics, social factors, trauma, and stress.[4] Among people with schizophrenia, there is a possible increased risk for first-degree relatives for schizoaffective disorder and vice-versa; there may be increased risk among individuals for schizoaffective disorder who have a first-degree relative with bipolar disorder schizophrenia, or schizoaffective disorder. [5]
[5]
Epidemiology
The diagnostic criteria for schizoaffective disorder have been reworded and addended since its inclusion in the DSM, making it difficult to subsequently conduct appropriate epidemiological studies. Thus, there have been no large-scale studies on the epidemiology, incidence, or prevalence of schizoaffective disorder. Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Pathophysiology
The exact pathophysiology of schizoaffective disorder is currently unknown. Some studies have shown that abnormalities in dopamine, norepinephrine, and serotonin may play a role.[9] Also, white matter abnormalities in multiple areas of the brain, particularly the right lentiform nucleus, left temporal gyrus, and right precuneus, are associated with schizophrenia and schizoaffective disorder. [10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
[10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
History and Physical
The first step in evaluation is obtaining a complete medical history while focusing on the diagnostic criteria for schizoaffective disorder.
The specific DSM-5 criteria for schizoaffective disorder are as follows[1]:
A. An uninterrupted duration of illness during which there is a major mood episode (manic or depressive) in addition to criterion A for schizophrenia; the major depressive episode must include depressed mood.
Criterion A for schizophrenia is as follows[13]:
Two or more of the following presentations, each present for a significant amount of time during a 1-month period (or less if successfully treated). At least one of these must be from the first three below.
Delusions
Hallucinations
Disorganized speech (e.
 g., frequent derailment or incoherence).
g., frequent derailment or incoherence).Grossly disorganized or catatonic behavior
Negative symptoms (i.e., diminished emotional expression or avolition.)
B. Hallucinations and delusions for two or more weeks in the absence of a major mood episode (manic or depressive) during the entire lifetime duration of the illness.
C. Symptoms that meet the criteria for a major mood episode are present for most of the total duration of both the active and residual portions of the illness.
D. The disturbance is not the result of the effects of a substance (e.g., a drug of misuse or a medication) or another underlying medical condition.
The following are specifiers based on the primary mood episode as part of the presentation.
Bipolar type: includes episodes of mania and sometimes major depression.
Depressive type: includes only major depressive episodes.
Please note the patient must meet the criteria for A-D above to be diagnosed with schizoaffective disorder.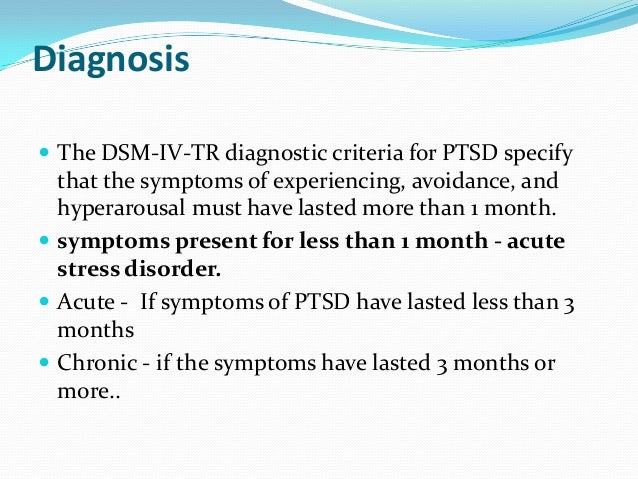 It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
The next step of evaluation is the objective and physical portion. A thorough mental status examination (MSE), physical examination, and neurologic examination should be completed to help rule out other differential diagnoses.
Evaluation
The following workup is optional and typically not needed to make the diagnosis. The history and physical are the mainstays of diagnosis. However, some elect to include additional tests or imaging to aid in the diagnosis, such as MRI (magnetic resonance imaging), EEG (electroencephalography), or CT (computed tomography).
Laboratory studies are tailored to the patient’s history, especially for those who have an atypical presentation.
Complete blood count (CBC)
Lipid panel
Urine drug screen
Urine pregnancy test
Urinalysis
Thyroid-stimulating hormone (TSH) level
Rapid plasma reagent
HIV test
If the patient's neurologic exam is found to be aberrant, performing a brain MRI or CT to rule out any suspected intracranial abnormalities may be considered.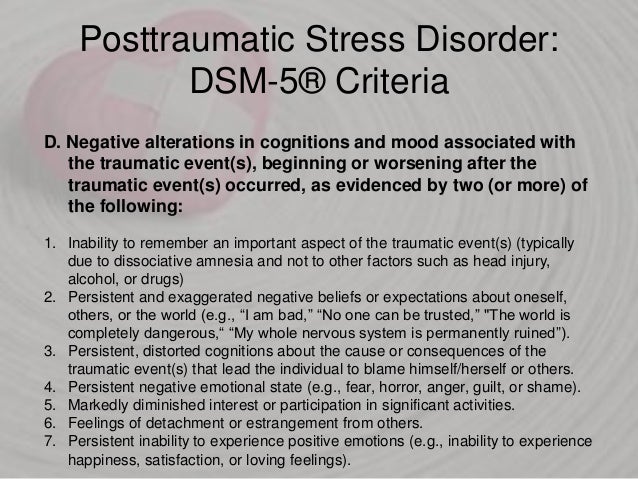
Treatment / Management
The treatment of schizoaffective disorder typically involves both pharmacotherapy and psychotherapy. The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
Pharmacotherapy
Antipsychotics: Used to target psychosis and aggressive behavior in schizoaffective disorder.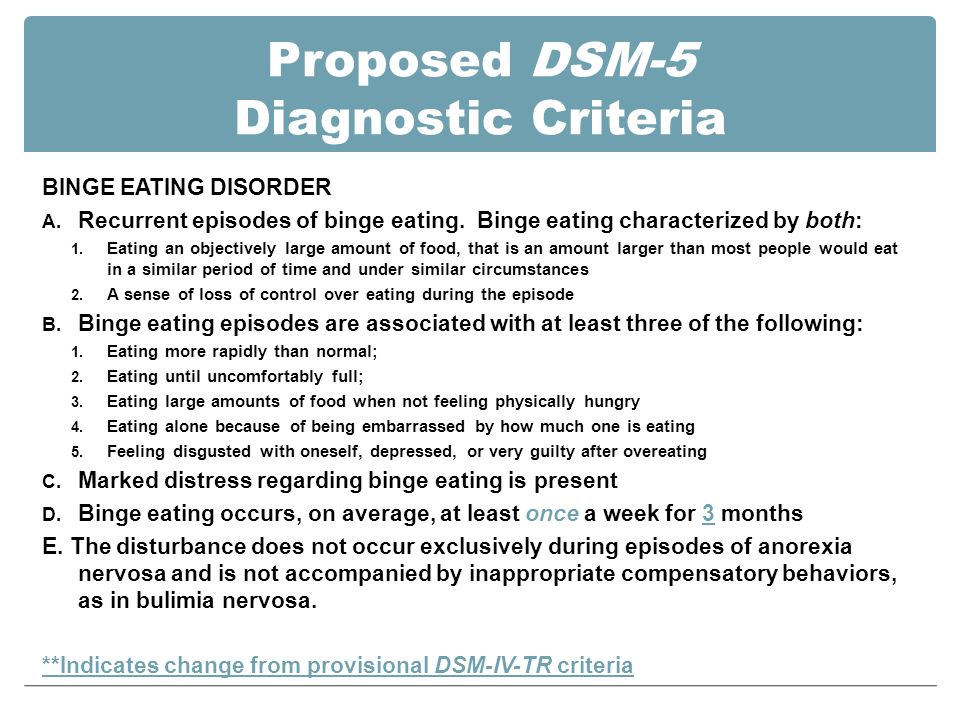 Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
Mood-stabilizers: Patients who have periods of distractibility, indiscretion, grandiosity, a flight of ideas, increased goal-directed activity, decreased need for sleep, and who are hyper-verbal fall under the bipolar-specifier for schizoaffective disorder. Consider the use of mood-stabilizers if the patient has a history of manic or hypomanic symptoms. These include medications such as lithium, valproic acid, carbamazepine, oxcarbazepine, and lamotrigine which target mood dysregulation. [21][22][23][24]
[21][22][23][24]
Antidepressants: Used to target depressive symptoms in schizoaffective disorder. Selective-serotonin reuptake inhibitors (SSRIs) are preferred due to lower risk for adverse drug effects and tolerability when compared to tricyclic antidepressants and selective norepinephrine reuptake inhibitors.[25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
Psychotherapy
Patients who have schizoaffective disorder can benefit from psychotherapy, as is the case with most mental disorders.
Treatment plans should incorporate individual therapy, family therapy, and psychoeducational programs. The aim is to develop their social skills and improve cognitive functioning to prevent relapse and possible rehospitalization.[27] This treatment plan includes education about the disorder, etiology, and treatment.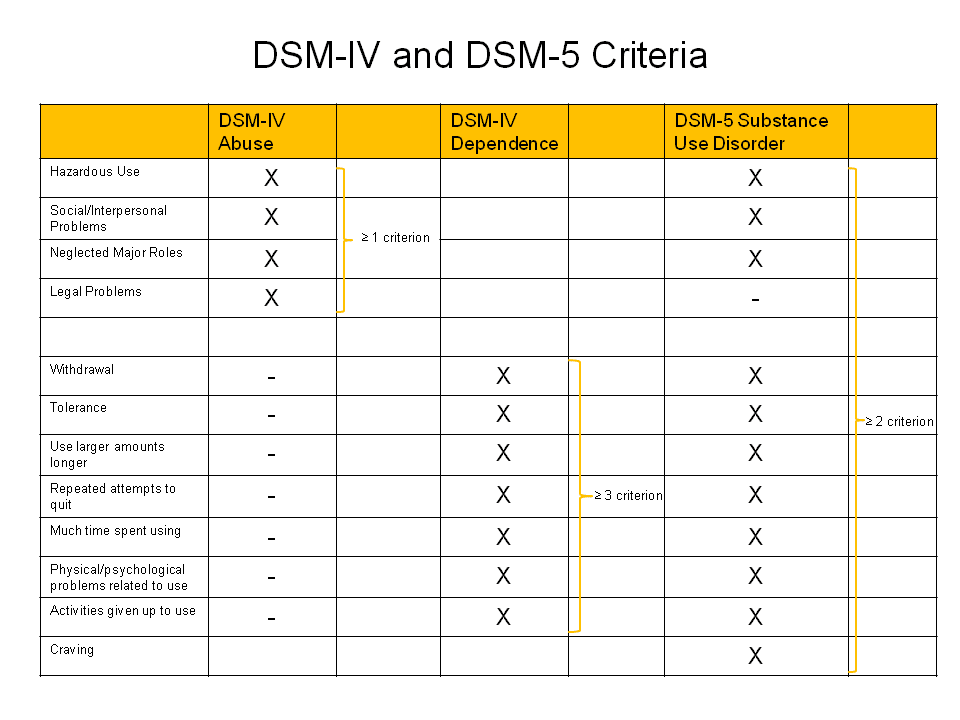
Individual therapy: This type of treatment aims to normalize thought processes and better help the patient understand the disorder and reduce symptoms. Sessions focus on everyday goals, social interactions, and conflict; this includes social skills training and vocational training.
Family and/or group therapy: Family involvement is crucial in the treatment of this schizoaffective disorder.[28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
ECT (Electroconvulsive Therapy)
ECT is usually a last resort treatment. However, not only has it been used in urgent cases and treatment resistance, but it should also merit consideration in augmentation of current pharmacotherapy. [29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
[29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
Differential Diagnosis
Because of criteria that encompass both psychotic and mood symptoms, schizoaffective disorder is easy to mistake for other mental disorders. Disorders that must be ruled out during the workup of schizoaffective disorder include:
Schizophrenia and Schizoaffective Disorder: There has to be a definite period of at least two weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms to diagnose schizoaffective disorder. However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.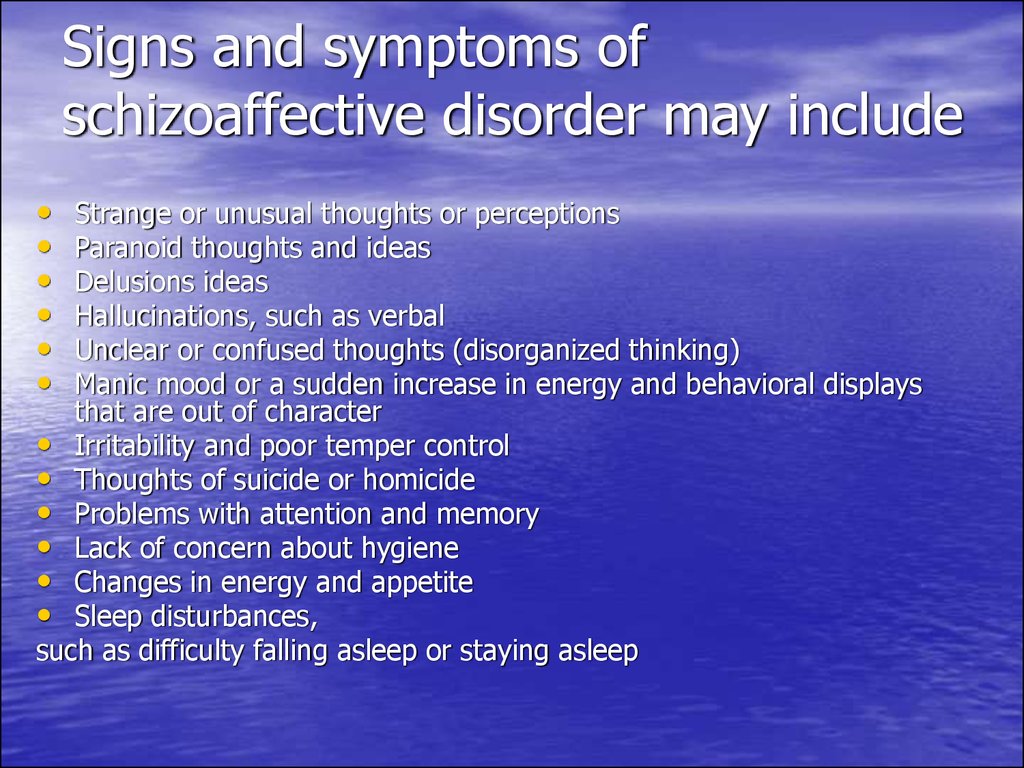
Major Depressive Disorder Psychotic Features and Schizoaffective Disorder: Patients with major depression with psychotic features (MDD with PF) only experience psychotic features during their mood episodes. In contrast, schizoaffective requires at least 2 weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms. Patients with MDD with PF do not meet criterion A of schizoaffective disorder.
Bipolar Disorder and Schizoaffective Disorder: Similar to the contrasts of MDD w/ PF, patients with bipolar disorder with psychotic features only experience psychotic features (delusions and hallucinations) during a manic episode. Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Prognosis
Given that the diagnostic criteria of schizoaffective disorder change periodically, prognostic studies have been challenging to conduct.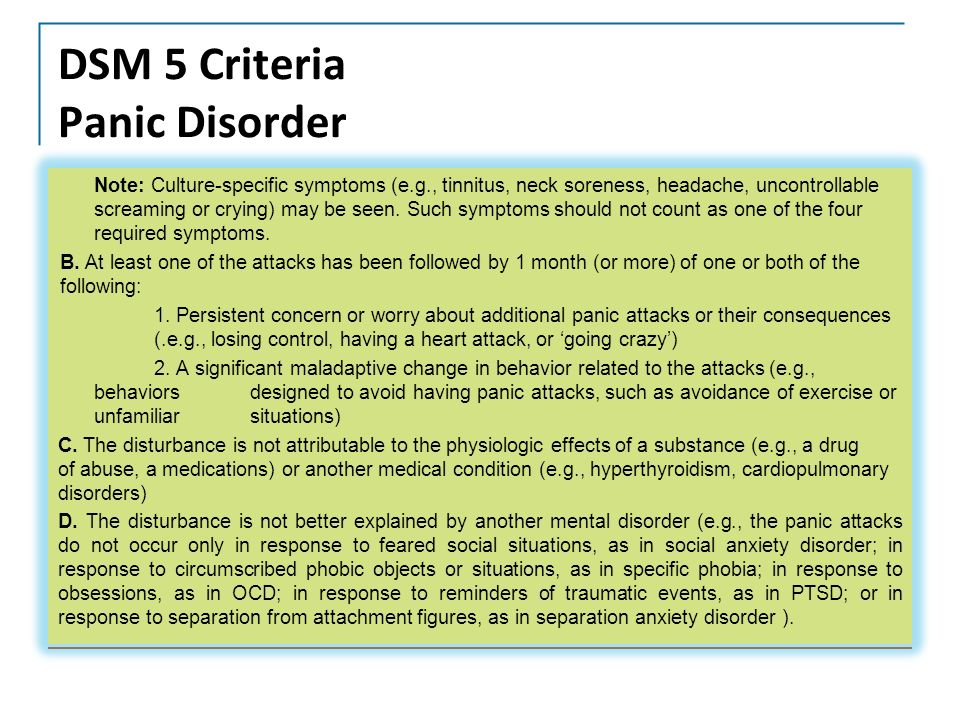 However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
Complications
Left untreated, schizoaffective disorder has many ramifications in both social functioning and activities of daily living. These include unemployment, isolation, impaired ability to care for self, etc. Untreated mental disorders have more than just social and functional consequences. Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Deterrence and Patient Education
Patients and their families can benefit from education regarding the condition and steps to manage it.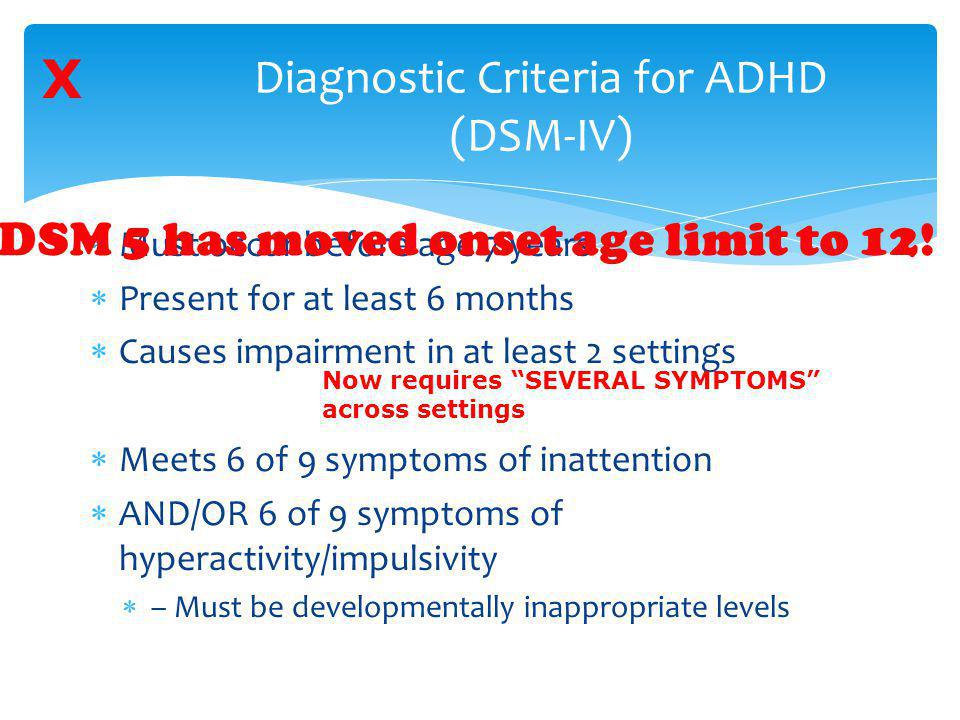
Encourage the patient to undergo treatment and rehabilitation
Cognitive behavior therapy
Interventions for drug and alcohol misuse
Social skills training
Provide emotional and life support
Teach them skills and measures that promote self-care and independence
Supported employment
Pearls and Other Issues
Working through the differential of schizoaffective disorder is often a daunting task, and many clinicians continue to have trouble making the diagnosis.[2] A few considerations when working through the differential diagnosis include:
Observe the criteria for each diagnosis carefully.
Do not "fill in blanks" with preconceived notions about the patient's history. Take what the patient tells you and what family/collateral information tells you when working through a differential.
Time frames often give clues towards one specific diagnosis.
 Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.
Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.Criterion B of schizoaffective disorder is key for the following reasons. One must tease out a 2 week or longer period of just psychotic symptoms in the patient's history. If one finds that the patient has always had mood symptoms during their entire illness, the diagnosis by definition is not a schizoaffective disorder.
Enhancing Healthcare Team Outcomes
As with most mental disorders, schizoaffective disorder is best managed by an interprofessional team including psychiatric specialty nurses and pharmacists, and clinicians that practice close interprofessional communication. [Level 5] Pharmacotherapy, psychotherapy, skills training, and vocational training work in tandem to create a holistic treatment plan. In addition to what the information alluded to in previous sections, psychotherapy strongly influences medication compliance. [34] An ideal treatment course to improve outcomes around patient-centered care may include:
[34] An ideal treatment course to improve outcomes around patient-centered care may include:
Early detection of mental disorder in the primary care setting
Referral to a psychiatrist for further evaluation
A psychiatrist would stabilize the patient with pharmacotherapy or defer to a clinical psychologist for diagnosis or additional therapy
If the patient requires inpatient hospitalization, the nursing staff and case management become crucial in providing optimal patient care
It is critical to determine if the patient is competent to make healthcare decisions independently; otherwise, a proxy must be a consideration.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malaspina D, Owen MJ, Heckers S, Tandon R, Bustillo J, Schultz S, Barch DM, Gaebel W, Gur RE, Tsuang M, Van Os J, Carpenter W.
 Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]
Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]- 2.
Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014 Feb;264(1):29-34. [PMC free article: PMC4207055] [PubMed: 23625467]
- 3.
Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009 Mar;35(2):383-402. [PMC free article: PMC2659306] [PubMed: 19011234]
- 4.
Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry. 2006 Jan;163(1):115-24. [PubMed: 16390898]
- 5.
Laursen TM, Munk-Olsen T, Nordentoft M, Bo Mortensen P. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a danish population-based cohort.
 J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]
J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]- 6.
Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long-term course. Acta Psychiatr Scand. 1990 Nov;82(5):352-8. [PubMed: 2281805]
- 7.
Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008 Dec;4(6):1089-109. [PMC free article: PMC2646642] [PubMed: 19337453]
- 8.
Azorin JM, Kaladjian A, Fakra E. [Current issues on schizoaffective disorder]. Encephale. 2005 May-Jun;31(3):359-65. [PubMed: 16142051]
- 9.
Meltzer HY, Arora RC, Metz J. Biological studies of schizoaffective disorders. Schizophr Bull. 1984;10(1):49-70. [PubMed: 6422546]
- 10.
Antonius D, Prudent V, Rebani Y, D'Angelo D, Ardekani BA, Malaspina D, Hoptman MJ.
 White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]
White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]- 11.
Radonić E, Rados M, Kalember P, Bajs-Janović M, Folnegović-Smalc V, Henigsberg N. Comparison of hippocampal volumes in schizophrenia, schizoaffective and bipolar disorder. Coll Antropol. 2011 Jan;35 Suppl 1:249-52. [PubMed: 21648342]
- 12.
Smith MJ, Wang L, Cronenwett W, Mamah D, Barch DM, Csernansky JG. Thalamic morphology in schizophrenia and schizoaffective disorder. J Psychiatr Res. 2011 Mar;45(3):378-85. [PMC free article: PMC2996474] [PubMed: 20797731]
- 13.
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013 Oct;150(1):3-10. [PubMed: 23800613]
- 14.
Vieta E. Developing an individualized treatment plan for patients with schizoaffective disorder: from pharmacotherapy to psychoeducation.
 J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]
J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]- 15.
Cascade E, Kalali AH, Buckley P. Treatment of schizoaffective disorder. Psychiatry (Edgmont). 2009 Mar;6(3):15-7. [PMC free article: PMC2719459] [PubMed: 19724749]
- 16.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002 Sep;63(9):763-71. [PubMed: 12363115]
- 17.
Addington DE, Pantelis C, Dineen M, Benattia I, Romano SJ. Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]
- 18.
Ciapparelli A, Dell'Osso L, Bandettini di Poggio A, Carmassi C, Cecconi D, Fenzi M, Chiavacci MC, Bottai M, Ramacciotti CE, Cassano GB.
 Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]
Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]- 19.
Ghaemi SN, Goodwin FK. Use of atypical antipsychotic agents in bipolar and schizoaffective disorders: review of the empirical literature. J Clin Psychopharmacol. 1999 Aug;19(4):354-61. [PubMed: 10440464]
- 20.
Gunasekara NS, Spencer CM, Keating GM. Spotlight on ziprasidone in schizophrenia and schizoaffective disorder. CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]
- 21.
Baethge C, Gruschka P, Berghöfer A, Bauer M, Müller-Oerlinghausen B, Bschor T, Smolka MN. Prophylaxis of schizoaffective disorder with lithium or carbamazepine: outcome after long-term follow-up. J Affect Disord. 2004 Apr;79(1-3):43-50. [PubMed: 15023479]
- 22.
Bogan AM, Brown ES, Suppes T. Efficacy of divalproex therapy for schizoaffective disorder.
 J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]
J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]- 23.
Dietrich DE, Kropp S, Emrich HM. [Oxcarbazepine in the treatment of affective and schizoaffective disorders]. Fortschr Neurol Psychiatr. 2003 May;71(5):255-64. [PubMed: 12740757]
- 24.
Leucht S, McGrath J, White P, Kissling W. Carbamazepine for schizophrenia and schizoaffective psychoses. Cochrane Database Syst Rev. 2002;(3):CD001258. [PubMed: 12137621]
- 25.
Koenig AM, Thase ME. First-line pharmacotherapies for depression - what is the best choice? Pol Arch Med Wewn. 2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]
- 26.
McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. Prim Care Companion CNS Disord. 2014;16(5) [PMC free article: PMC4321017] [PubMed: 25667812]
- 27.
Fitzgerald P, de Castella A, Arya D, Simons WR, Eggleston A, Meere S, Kulkarni J. The cost of relapse in schizophrenia and schizoaffective disorder.
 Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]
Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]- 28.
Pharoah FM, Rathbone J, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2003;(4):CD000088. [PubMed: 14583908]
- 29.
Phutane VH, Thirthalli J, Kesavan M, Kumar NC, Gangadhar BN. Why do we prescribe ECT to schizophrenia patients? Indian J Psychiatry. 2011 Apr;53(2):149-51. [PMC free article: PMC3136018] [PubMed: 21772648]
- 30.
Iancu I, Pick N, Seener-Lorsh O, Dannon P. Patients with schizophrenia or schizoaffective disorder who receive multiple electroconvulsive therapy sessions: characteristics, indications, and results. Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]
- 31.
Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, Dube KC, Ganev K, Giel R, an der Heiden W, Holmberg SK, Janca A, Lee PW, León CA, Malhotra S, Marsella AJ, Nakane Y, Sartorius N, Shen Y, Skoda C, Thara R, Tsirkin SJ, Varma VK, Walsh D, Wiersma D.
 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]- 32.
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010 Nov;24(4 Suppl):81-90. [PMC free article: PMC2951591] [PubMed: 20923923]
- 33.
Suominen K, Isometsä E, Heilä H, Lönnqvist J, Henriksson M. General hospital suicides--a psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002 Nov-Dec;24(6):412-6. [PubMed: 12490343]
- 34.
Stentzel U, van den Berg N, Schulze LN, Schwaneberg T, Radicke F, Langosch JM, Freyberger HJ, Hoffmann W, Grabe HJ. Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
How to diagnose schizoaffective disorder according to ICD-11 or DSM-5?
In this section
Panellists, which took place live at the 29th Virtual Congress of the European Psychiatric Association (EPA) 2021, discussed in detail the question of whether to diagnose schizoaffective disorder at the moment ( ICD-11) instead of diagnosing in dynamics (DSM-5).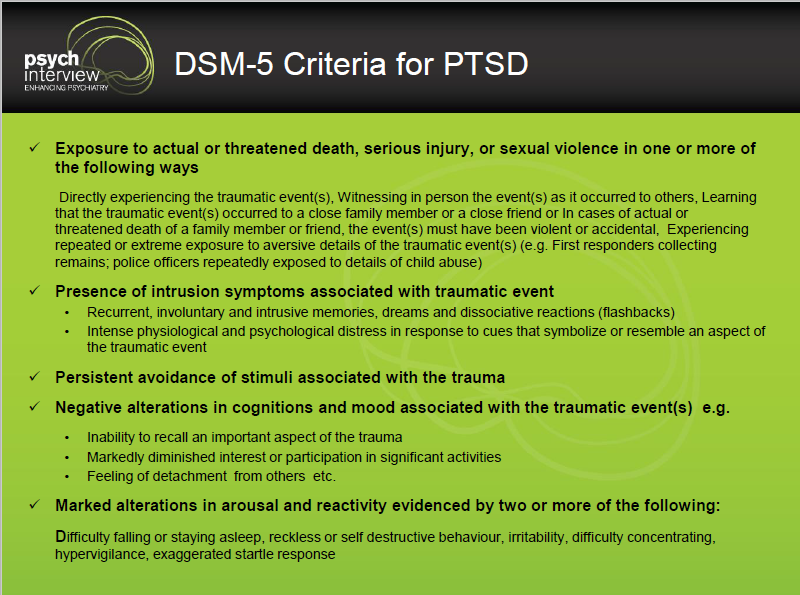 Professor Peter Falkai argued in favor of this approach, while Professor Ingrid Melle spoke out against it. The discussion was led by Professor of the Department of Psychiatry of the Campania University. Luigi Vanvitelli Silvana Galderisi.
Professor Peter Falkai argued in favor of this approach, while Professor Ingrid Melle spoke out against it. The discussion was led by Professor of the Department of Psychiatry of the Campania University. Luigi Vanvitelli Silvana Galderisi.
In a survey conducted at the beginning of the debate, 64% of participants indicated that schizoaffective disorder should be diagnosed in the dynamics, while 21% of specialists supported the diagnosis at the moment, and 14% answered that they were not sure.
Diagnosis of schizoaffective disorder should be carried out in the current state (ICD-11), and not in dynamics (DSM-5)
President of the University of Psychiatry and Psychotherapy Munich and newly elected member of the Department of Psychiatry and Psychotherapy Prof. Peter Falkay supported this approach.
Peter Falkay supported this approach.
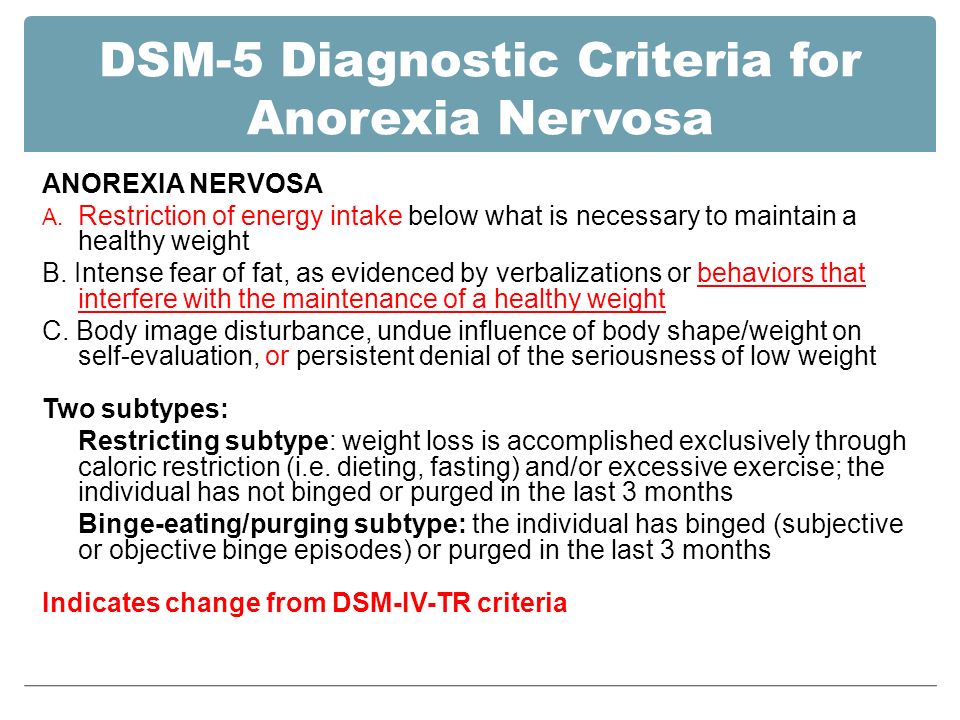
He began his speech by describing the diagnostic criteria for schizoaffective disorder; According to the provisions of the International Classification of Diseases, 11th Revision (ICD-11), a diagnosis can only be established if the symptoms of schizophrenia and a moderate or severe affective episode are observed simultaneously or with an interval of several days 1 . Moreover, the total duration of the symptoms of schizophrenia and the affective episode must be one month 1 .
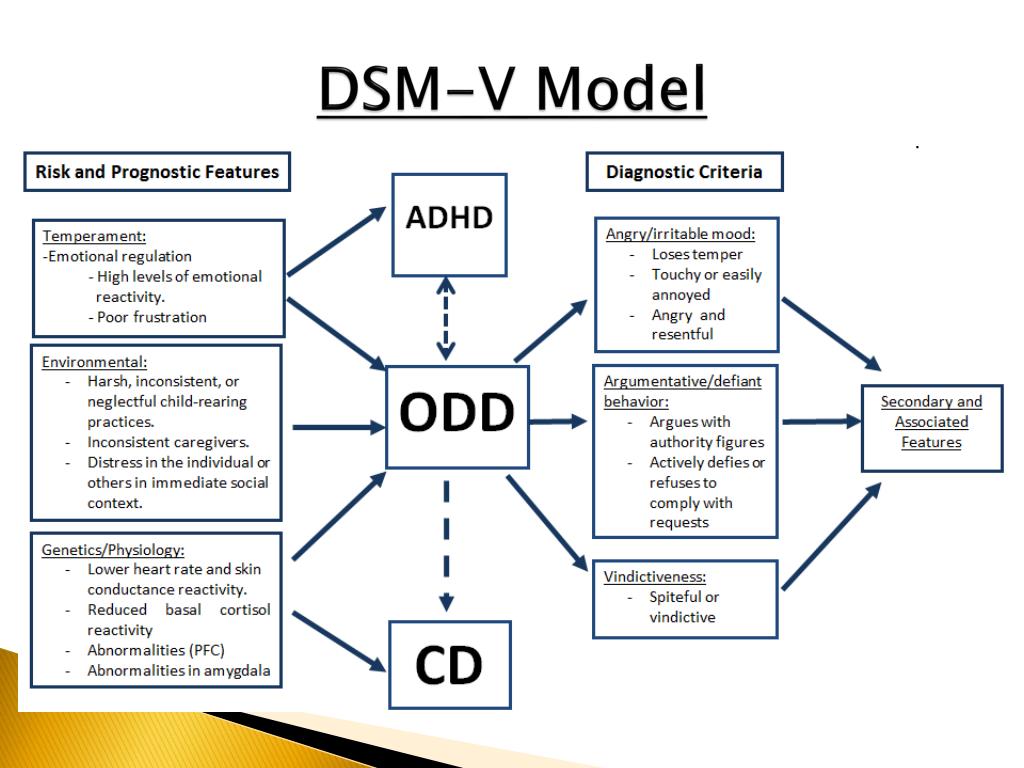
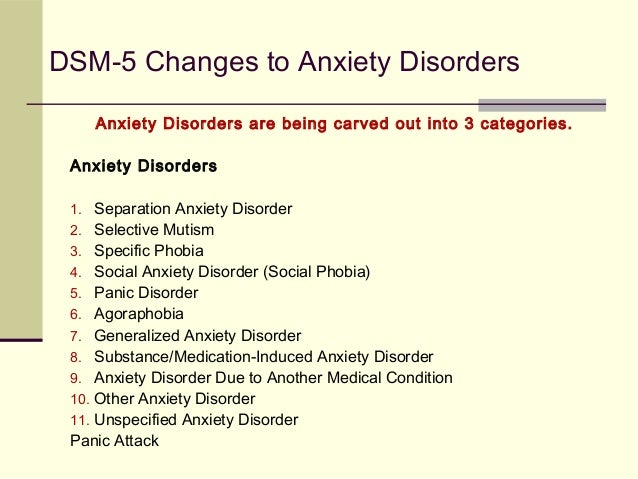
In contrast, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), confirmation of schizoaffective disorder requires a continuous period of illness with an obvious affective episode and symptoms of schizophrenia that meet criterion A, which include delusions, hallucinations, and negative symptoms 2 . In the absence of overt affective episodes, positive symptoms must be observed for two or more weeks during the entire duration of the illness, and these symptoms must not be associated with the use of any substances or other diseases 2 .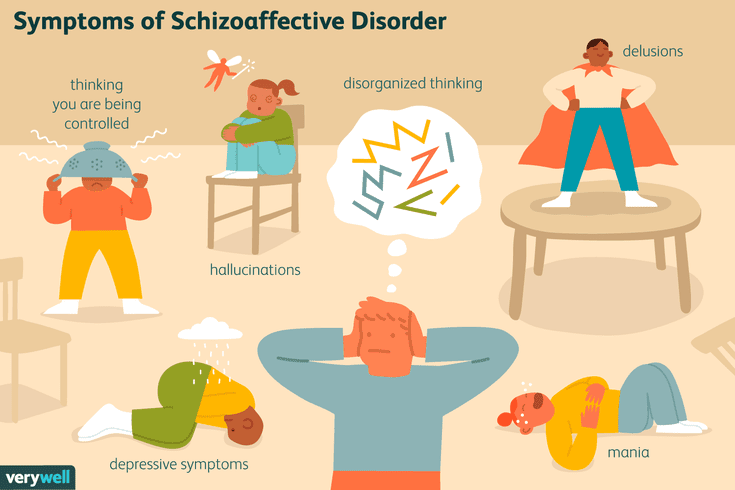
Professor Falcay noted that the main difference between the diagnostic criteria for schizoaffective disorder according to ICD-11 and DSM-5 is how episodes are considered - at the same time the relevant symptoms are detected or during the entire duration of the illness 1.2 . This is important because some patients with schizophrenia may have only one episode, while others have multiple episodes with asymptomatic intervals of several decades 2 .
Professor Falcay went on to highlight the significant differences between the ICD-11 and the DSM-5 in the conceptualization of schizoaffective disorder. According to the ICD-11, diagnostic criteria must be met simultaneously for affective episodes lasting one month and psychotic symptoms occurring at about the same time 1 . This definition focuses on the presence of symptoms during a single episode rather than a lifetime. In contrast, the DSM-5 criteria require a retrospective assessment of the relationship of psychotic and affective symptoms throughout the duration of the disease, and it is much more difficult to restore an accurate clinical picture in this case 2 .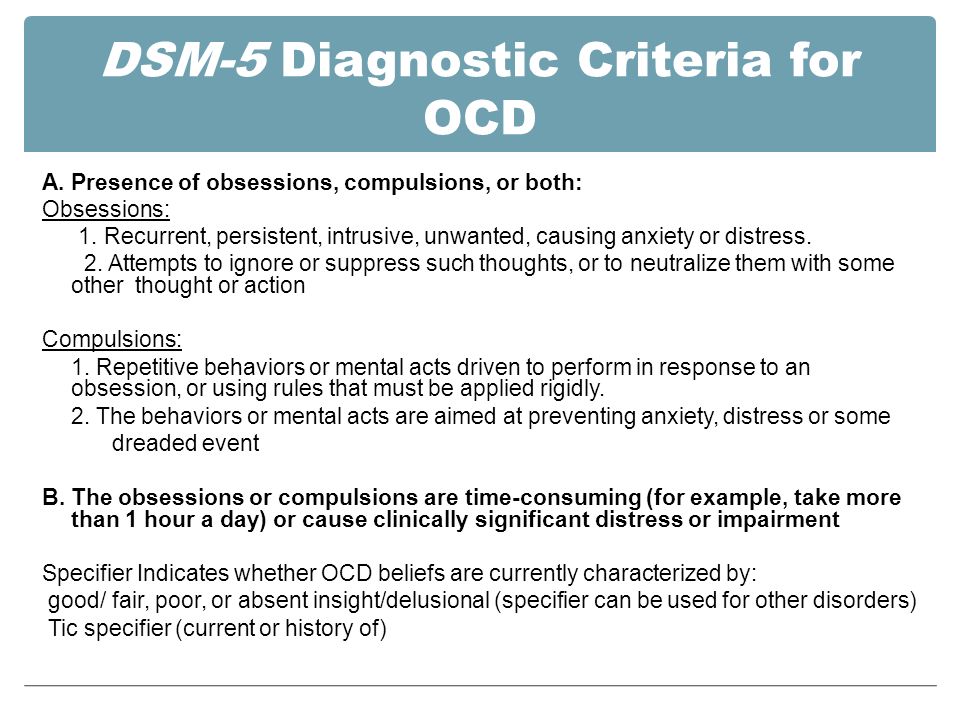
According to Prof. Falkay, these differences in diagnostic approaches partly reflect trade-offs between diagnostic stability and feasibility, which greatly affect reliability. Because the DSM-5 diagnostic criteria involve evaluation of symptoms throughout the duration of the illness, they are relatively stable. However, the high diagnostic reliability of this approach can be called into question. Indeed, Prof. Falcay stressed that the issue of reliability has long been noted in the diagnosis of schizoaffective disorder according to the DSM criteria. On the other hand, the approach proposed in the ICD-11 reflects the changing nature of the clinical picture of many psychotic disorders over time.
The results of studies conducted in a clinical setting may support this argument. Professor Falcay noted that they proved the high reliability of the ICD-11 diagnostic criteria for schizoaffective disorder, along with ease of use and clarity. For example, data from a meta-analysis of 42 studies indicated high prospective stability in the diagnosis of schizophrenic and affective spectrum psychoses, as well as the absence of statistically significant differences when using ICD and DSM 9 criteria. 0023 3 .
0023 3 .
In addition, it has become apparent that schizoaffective disorder has long had various definitions, ranging from the position that it is a separate nosological form, to the assertion that schizophrenia and a mood disorder coexist. However, it has been recognized that there are strong clinical reasons for maintaining such a diagnosis, and the DSM-5 criteria have clear limitations, both theoretical and practical, and therefore should be simplified.
Professor Falcay concluded by stating that he supported the current method of diagnosing schizoaffective disorder as described in ICD-11. This is mainly due to the fact that this method is more applicable in clinical practice than the dynamic assessment recommended in DSM-5. Moreover, considering diagnostic stability for at least 4.5 years 3 , ICD-11 provides a rational way to define and diagnose this elusive disorder.
Diagnosis of schizoaffective disorder should not be carried out at the current moment (ICD-11), but in dynamics (DSM-5)
of Medicine at the University of Oslo defended the opposite view, according to which schizoaffective disorder should be diagnosed not as of the current moment, but in dynamics, as proposed in the DSM-5.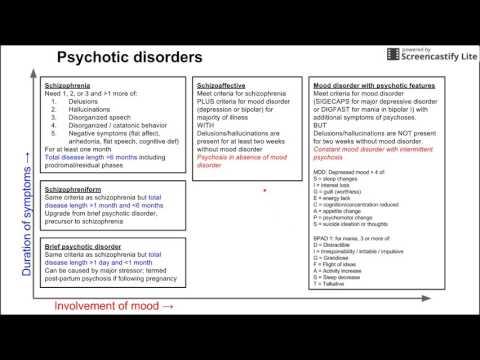
Professor Melle began her presentation by mentioning a series of clinical cases. In 1939, Kasanin first described a number of "rather atypical" cases, the clinical picture of which could indicate both schizophrenia spectrum disorders and affective disorders. This led to a whole series of questions about whether schizoaffective disorder is schizophrenia, manic-depressive psychosis, something in between, or a separate illness.
According to Professor Melle, schizoaffective disorder may include more asymptomatic periods than schizophrenia, and therefore the diagnosis of schizoaffective disorder is considered a viable concept, as it allows better prediction of patient outcomes and increases the likelihood of correct and timely treatment.
However, schizoaffective disorder should not be considered as a separate disorder, but rather as part of a broad spectrum of psychotic and affective disorders that are intermediate between schizophrenia and bipolar disorder. From the time the DSM was first drafted in 1952 to the present, clinical views on schizoaffective disorder have changed, and in reality there was not much in common between the DSM-IV and the ICD-10.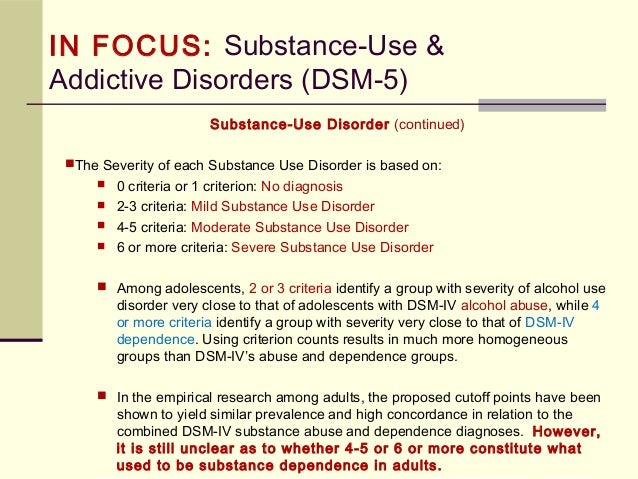
Today, DSM-5 diagnostic criteria require a continuous period of illness during which there is an apparent affective episode and symptoms of schizophrenia that meet criterion A2. However, the ICD-11 defines schizoaffective disorder as having all the symptoms of schizophrenia that occur around the same time as affective episode 9.0023 1 .
Significantly, the DSM-5 recommends that affective symptoms be assessed throughout the duration of a psychotic illness, whereas the ICD-11 suggests that they be analyzed only at the time of the current episode. Professor Melle further emphasized that the results of empirical studies indicated differences in clinical symptoms between episodes, therefore, within the framework of ICD-11, the diagnosis can change from one episode to another. This significantly affects the reliability of the diagnosis. When using the time course recommended in DSM-5, the entire medical history is considered as a whole, which reduces the risk of making a diagnosis based on an atypical episode.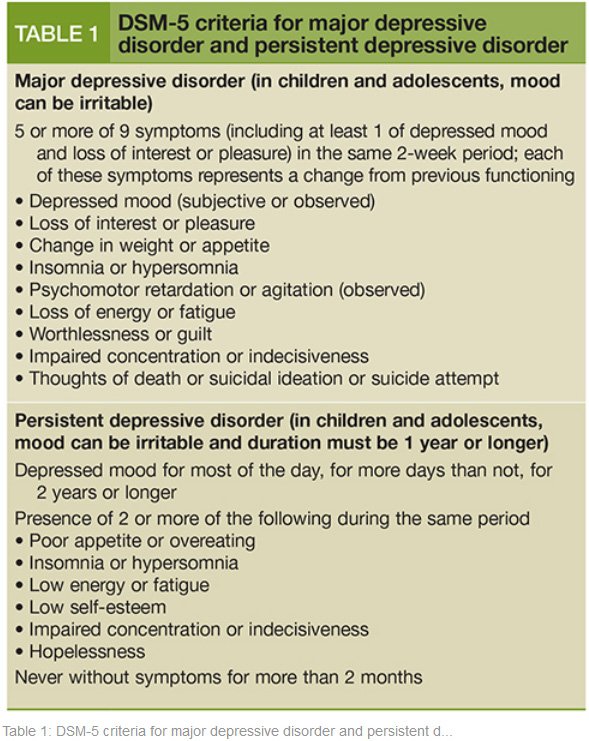
Professor Melle took her position and presented clinical data that support the effectiveness of certain drug combinations in the treatment of patients with schizoaffective disorder. From her point of view, the assessment over time offered by the DSM-5, although somewhat less practical, provides a more complete picture of the life course of schizoaffective disorder and allows patients to expect more effective treatment.
Sources:
- International Classification of Diseases 11th Revision (ICD-11). Available at: https://icd.who.int/en
- Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Available at: https://www.psychiatry.org/psychiatrists/practice/dsm.
- Fusar-Poli P, Cappucciati M, Rutigliano G, et al. Diagnostic Stability of ICD/DSM First Episode Psychosis Diagnoses: Meta-analysis. Schizophr Bull. 2016 Nov;42(6):1395-1406.
Please confirm your consent to the use of cookies
Yes, I agree
No, I refuse
Please confirm that you are a healthcare worker
Showing 0 result(s).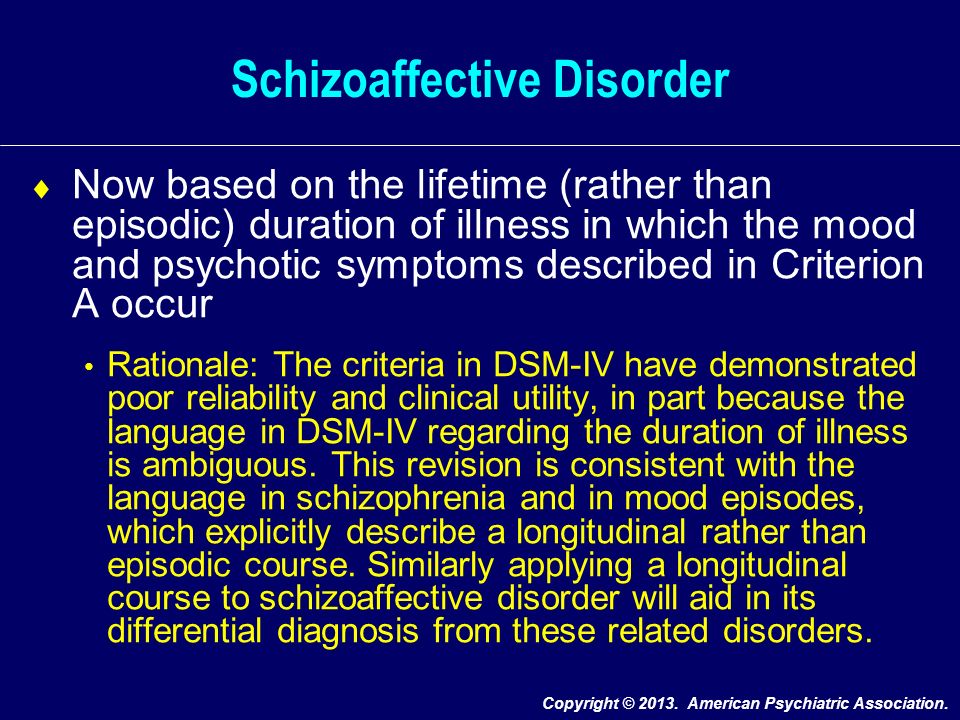
Please log in to see 0 more result(s).
FGBNU NTsPZ. ‹‹Endogenous mental illness››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
Schizoaffective psychosis — is a non-progredient endogenous mental illness with a relatively favorable prognosis, recurrent seizures, in the picture and dynamics of which circular affective disorders (depressive, manic, mixed) of an endogenous nature simultaneously coexist or sequentially develop 1 and psychotic symptoms characteristic of schizophrenia (delusional, hallucinatory) that are not derived from affect.
At the present level of psychiatric knowledge, the content of any definition of schizoaffective psychosis as an independent endogenous psychosis is conditional and debatable. To date, there are no generally accepted definitions that characterize the clinical essence of this disease.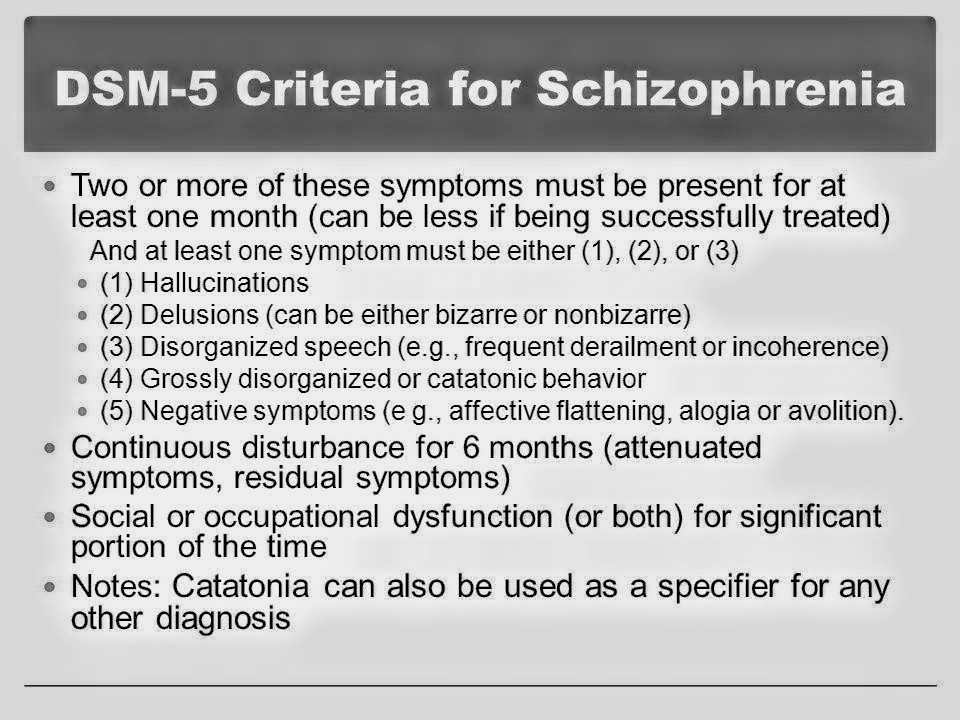 The reference to the fact that schizoaffective psychoses combine the signs of two diseases - schizophrenia and affective psychoses, is defined. regardless of external circumstances and psychotic experiences; in schizoaffective psychosis, the differentiation of circular and delusional affect is of great diagnostic importance, which allows only their assignment to the group of endogenous psychoses, but not their position in the systematics of endogenous mental illness.
The reference to the fact that schizoaffective psychoses combine the signs of two diseases - schizophrenia and affective psychoses, is defined. regardless of external circumstances and psychotic experiences; in schizoaffective psychosis, the differentiation of circular and delusional affect is of great diagnostic importance, which allows only their assignment to the group of endogenous psychoses, but not their position in the systematics of endogenous mental illness.
The criteria on which the allocation of schizoaffective psychosis is based are most fully formulated in the ICD-10. According to the latter, schizoaffective psychosis is considered not as a "disease", but as "episodic (paroxysmal) disorders" (i.e., conditions) in which both affective and schizophrenic symptoms are present, listed in the diagnostic guidelines for F20 (schizophrenia), observed simultaneously or consecutively over several days, during the same attack, when the picture of the attack meets neither the criteria for schizophrenia nor the criteria for a manic-depressive episode.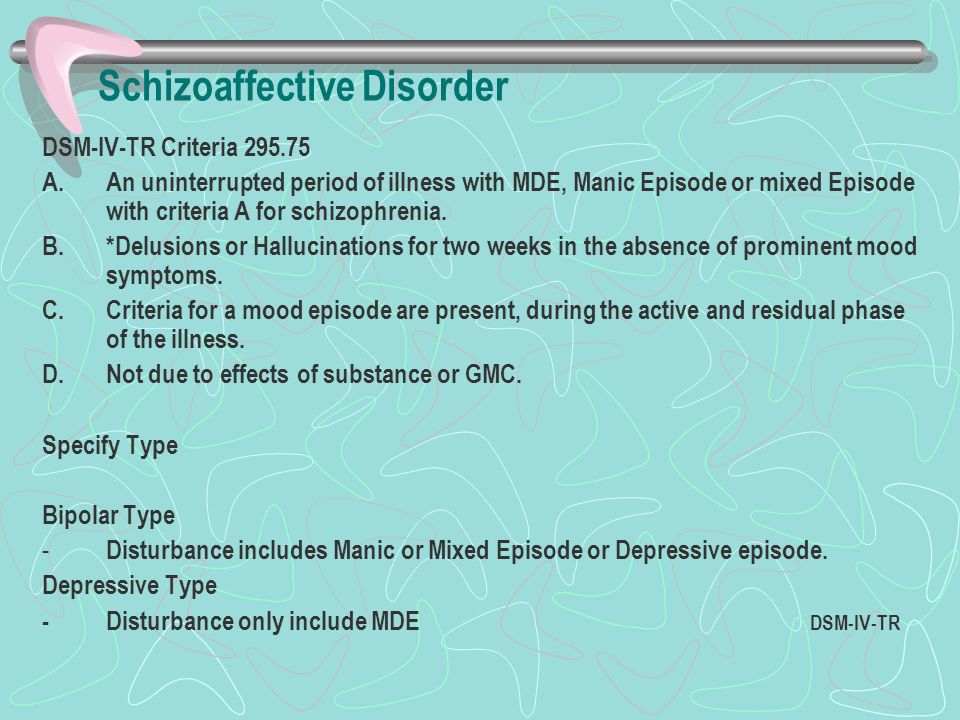
In one of the authoritative studies of the last decade, conducted by A. Marneros (1989), the concept of schizoaffective psychosis is also equated with the concept of schizoaffective disorders and is defined as a psychopathological syndrome, in the constellation of symptoms of which both schizophrenic and melancholic or manic signs are simultaneously or sequentially observed.
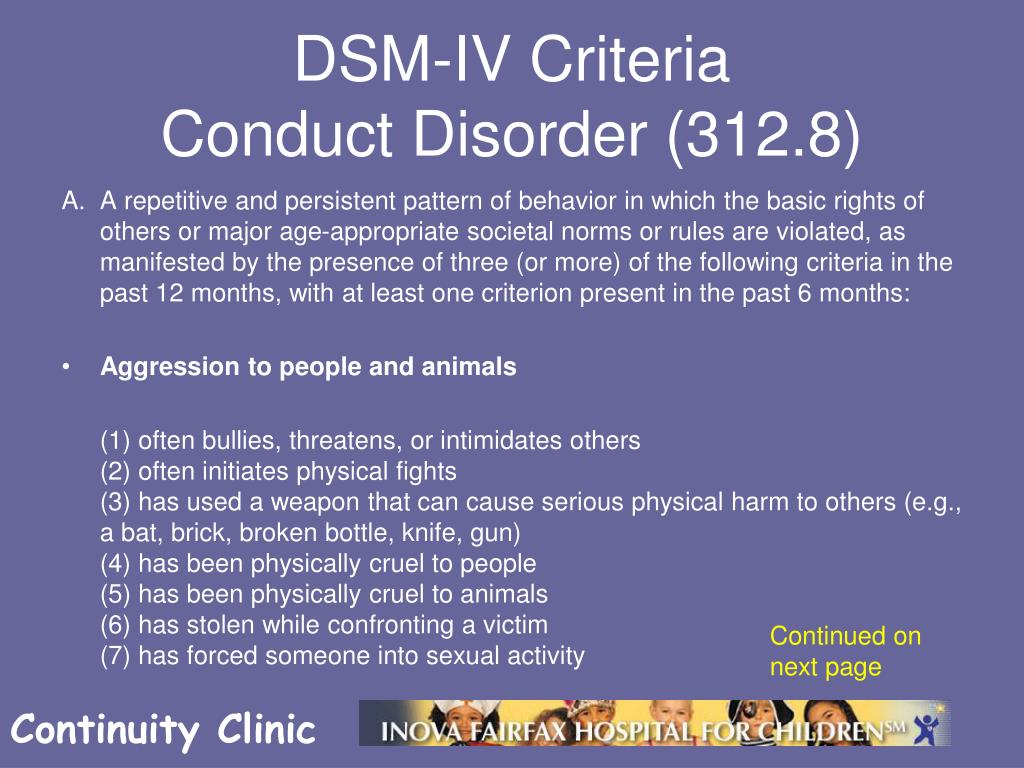
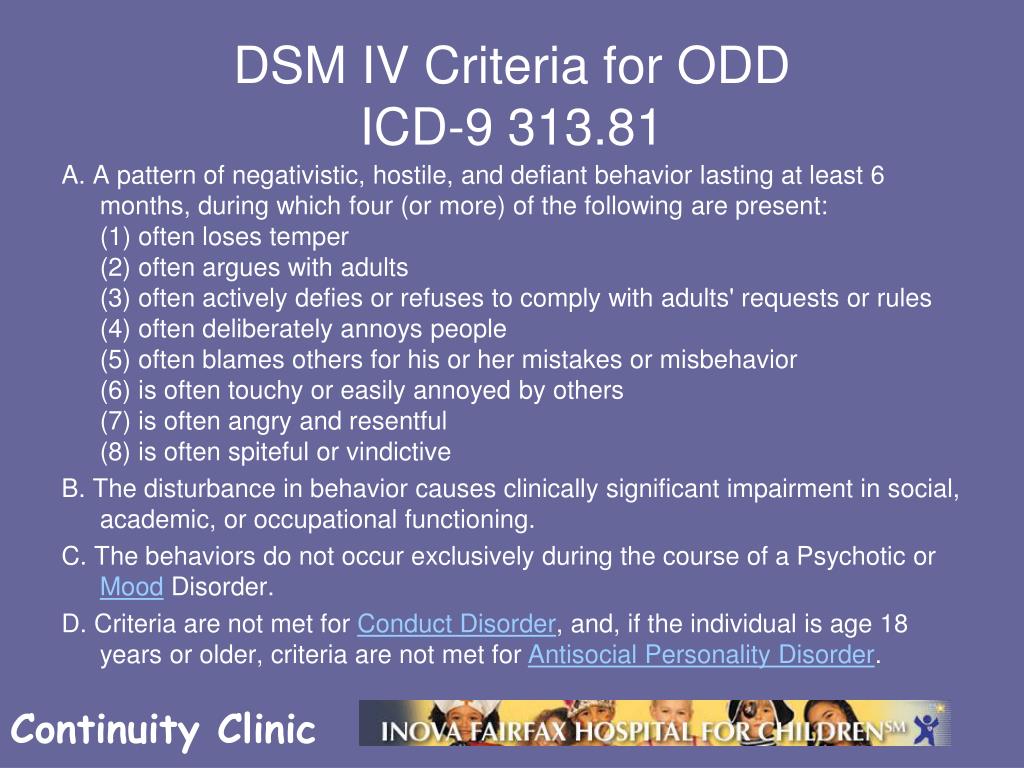
In DSM-IV, for the diagnosis of schizoaffective disorder, additional clarifying parameters have been introduced, allowing to attribute to schizoaffective psychosis only those manifestations in which: a) during a long period of the disease, distinct affective disorders (depressive, manic, mixed) and psychopathological symptoms, mandatory for the diagnosis of schizophrenia; b) delusions or hallucinations typical of schizophrenia in its pure form (i.e., without the presence of pronounced affective disorders), lasting at least 2 weeks, should determine the patient's condition; c) the symptoms of affective disorders should take a significant period of time in the total duration of schizoaffective psychosis, in its active and residual stages; d) these psychopathological phenomena should not be the result of exposure to any toxic substances and drugs or somatoorganic diseases.