Psychogenic fugue state
Mental Health: Dissociative Fugue
Written by WebMD Editorial Contributors
In this Article
- What Are the Symptoms of Dissociative Fugue?
- What Causes Dissociative Fugue?
- How Common Is Dissociative Fugue?
- How Is Dissociative Fugue Diagnosed?
- How Is Dissociative Fugue Treated?
- What Is the Outlook for People With Dissociative Fugue?
- Can Dissociative Fugue Be Prevented?
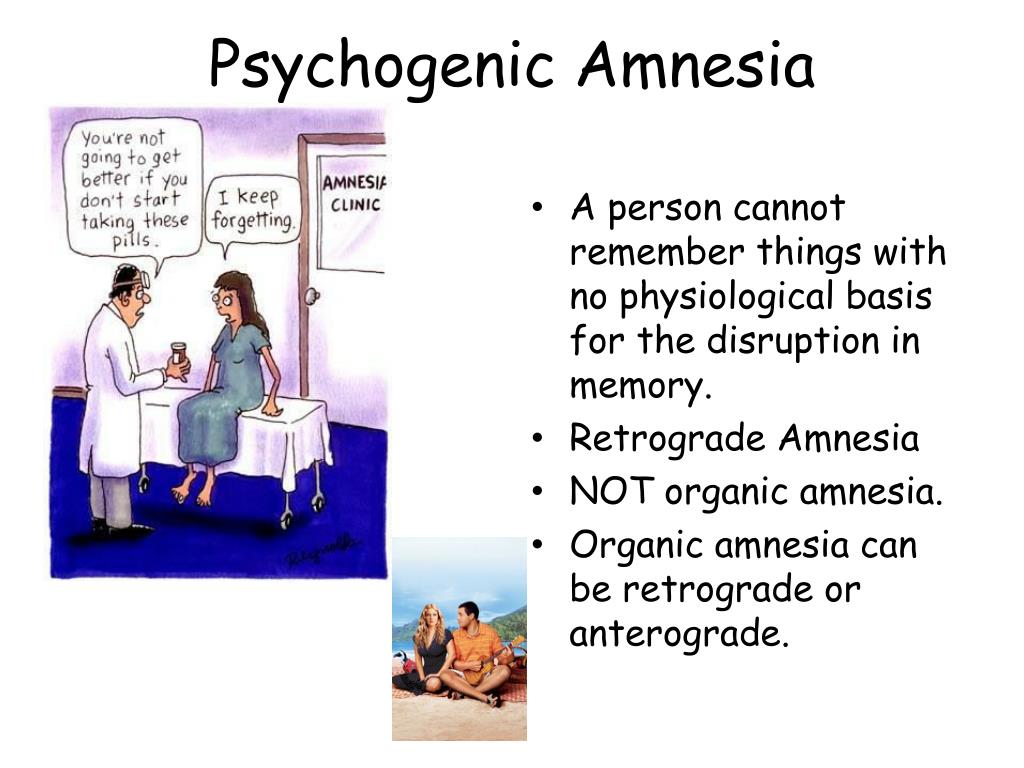
Dissociative fugue, formerly called psychogenic fugue, is one of a group of conditions called dissociative disorders. The word fugue comes from the Latin word for "flight." People with dissociative fugue temporarily lose their sense of personal identity and impulsively wander or travel away from their homes or places of work. They often become confused about who they are and might even create new identities. Outwardly, people with this disorder show no signs of illness, such as a strange appearance or odd behavior.
Dissociative disorders are mental illnesses that involve disruptions or breakdowns of memory, conscious awareness, identity, and/or perception. When one or more of these functions is disrupted, symptoms can result. These symptoms can interfere with a person's general functioning, including social and work activities, and relationships.
What Are the Symptoms of Dissociative Fugue?
A fugue in progress often is difficult for others to recognize because the person's outward behavior appears normal. Symptoms of dissociative fugue might include the following:
- Sudden and unplanned travel away from home
- Inability to recall past events or important information from the person's life
- Confusion or loss of memory about their identity, possibly assuming a new identity to make up for the loss
- Extreme distress and problems with daily functioning (due to the fugue episodes)
What Causes Dissociative Fugue?
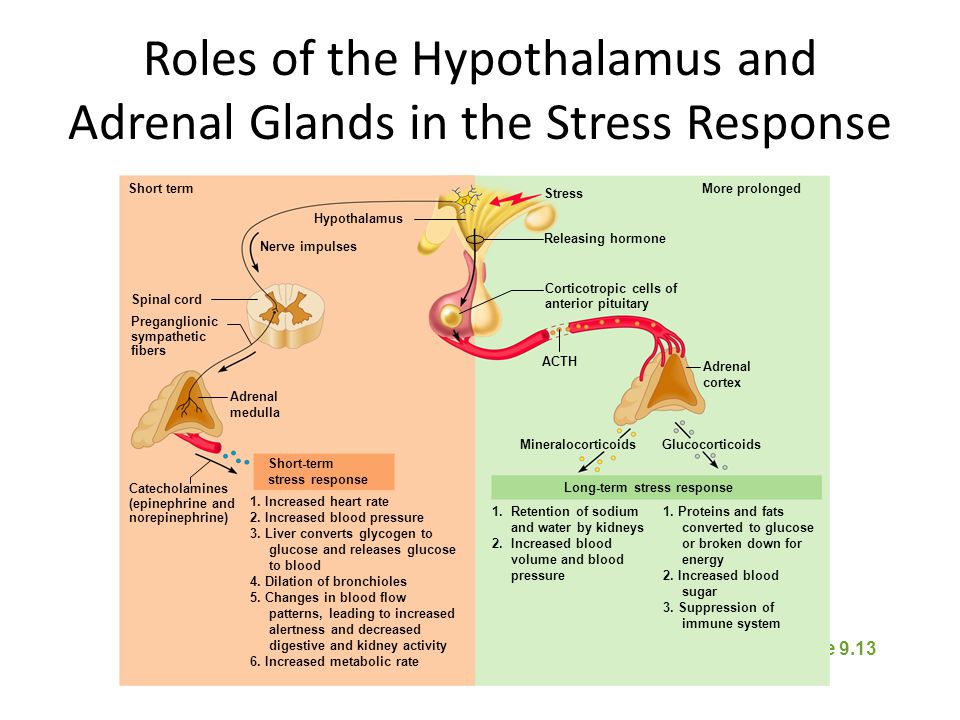
Dissociative fugue has been linked to severe stress, which might be the result of traumatic events -- such as war, abuse, accidents, disasters, or extreme violence -- that the person has experienced or witnessed. The use or abuse of alcohol and certain drugs also can cause fugue-like states, such as alcohol-induced "blackouts."
The use or abuse of alcohol and certain drugs also can cause fugue-like states, such as alcohol-induced "blackouts."
How Common Is Dissociative Fugue?
Dissociative fugue is relatively rare. The frequency of dissociative fugue tends to increase during stressful or traumatic periods, such as during wartime or after a natural disaster.
How Is Dissociative Fugue Diagnosed?
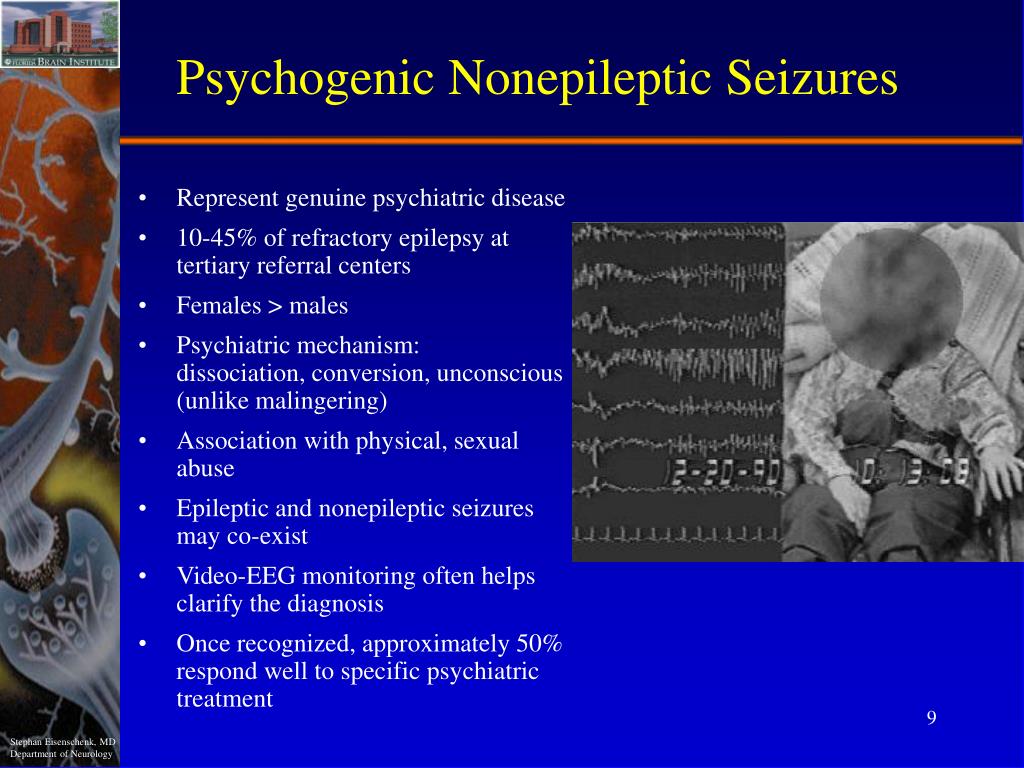
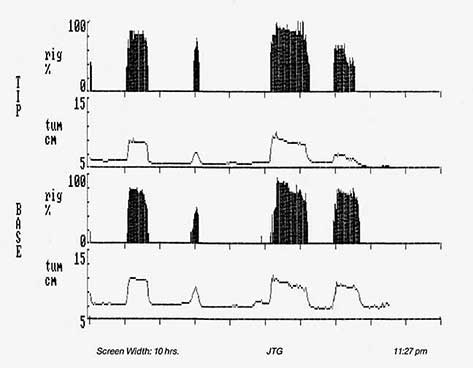
If symptoms of dissociative fugue are present, the doctor will often begin an evaluation by performing a complete medical history and physical exam. Although there are no lab tests to specifically diagnose dissociative disorders, the doctor might sometimes recommend various diagnostic tests, such as neuroimaging studies, electroencephalograms (EEGs), and blood tests, to rule out physical illness or medication side effects if these are suspected as causing the symptoms. Certain conditions -- including brain diseases (such as epilepsy), head injuries, drug and alcohol intoxication, and sleep deprivation -- can lead to symptoms similar to those of dissociative disorders, including amnesia (loss of memory).
If no physical illness is found, the person might be referred to a psychiatrist or psychologist, health care professionals who are specially trained to diagnose and treat mental illnesses. Psychiatrists and psychologists use specially designed interviews and assessment tools to evaluate a person for a dissociative disorder.
How Is Dissociative Fugue Treated?
The goal of dissociative fugue treatment is to help the person come to terms with the stress or trauma that triggered the fugue. Treatment also aims to develop new coping methods to prevent further fugue episodes. The best treatment approach depends on the individual and the severity of their symptoms, but most likely will include some combination of the following treatment methods:
- Psychotherapy: Psychotherapy, a type of counseling, is the main treatment for dissociative disorders. This treatment uses techniques designed to encourage communication of conflicts and increase insight into problems.
 Cognitive therapy is a specific type of psychotherapy that focuses on changing dysfunctional thinking patterns and resulting feelings and behaviors.
Cognitive therapy is a specific type of psychotherapy that focuses on changing dysfunctional thinking patterns and resulting feelings and behaviors. - Medication: There is no established medication to treat the dissociative disorders themselves. However, if a person with a dissociative disorder also suffers from depression or anxiety, they might benefit from treatment with a medication such as antidepressant, anti-anxiety, or antipsychotic drugs.
- Family therapy: This helps to teach the family about the disorder and its causes, as well as to help family members recognize symptoms of a recurrence.
- Creative therapies (art therapy, music therapy): These therapies allow the patient to explore and express their thoughts and feelings in a safe and creative way.
- Clinical hypnosis: This is a treatment method that uses intense relaxation, concentration, and focused attention to achieve an altered state of consciousness (awareness), allowing people to explore thoughts, feelings, and memories they might have hidden from their conscious minds.
 The use of hypnosis for treating dissociative disorders is controversial due to the risk of creating false memories.
The use of hypnosis for treating dissociative disorders is controversial due to the risk of creating false memories.
What Is the Outlook for People With Dissociative Fugue?
Most dissociative fugues are brief, lasting from less than a day to several months. Often, the disorder goes away on its own. The outlook, therefore, is quite good. However, without treatment to work out the underlying problem, additional fugue episodes can occur.
Can Dissociative Fugue Be Prevented?
Although it might not be possible to prevent dissociative fugue, it might be helpful to begin treatment in people as soon as they begin to have symptoms. Further, quick intervention following a traumatic event or emotionally distressing experience might help reduce the risk of developing dissociative disorders.
Dissociative fugue symptoms in a 28-year-old male Nigerian medical student: a case report
- Journal List
- J Med Case Rep
- v.
 7; 2013
7; 2013 - PMC3680202
J Med Case Rep. 2013; 7: 143.
Published online 2013 May 31. doi: 10.1186/1752-1947-7-143
1
Author information Article notes Copyright and License information Disclaimer
Introduction
Dissociative fugue is a psychiatric disorder characterized by amnesia coupled with sudden unexpected travel away from the individual’s usual surroundings and denial of all memory of his or her whereabouts during the period of wandering. Dissociative fugue is a rare disorder that is infrequently reported. Before now, no case of it had been reported in a medical student.
Case presentation
This article focuses on the report of a case of dissociative fugue symptoms in a 28-year-old male Nigerian medical student.
Conclusion
The observation in this case report brings to the fore that dissociative fugue is often related to stressful life events and can comorbid with a depressive disorder.
Keywords: Dissociative, Fugue, Medical, Student
Dissociative fugue, formerly called psychogenic fugue, is one of a group of psychiatric conditions called dissociative disorders. Dissociative disorders are characterized by transient or chronic failures or disruptions of integration of consciousness, memory, perception, identity or emotion. Dissociative disorders include dissociative amnesia, fugue, depersonalization disorder, dissociative identity disorder and dissociative disorder not otherwise specified [1].
People with dissociative fugue temporarily lose their sense of personal identity and impulsively wander away from their homes or places of work [2]. They may travel far distances during the fugue, as far as several thousand miles [2,3]. They may remain in the fugue state for a couple of days, several weeks or even months [2-4]. When individuals return to their pre-dissociative states, events that occurred during the fugue are not remembered [2].
Dissociative fugue is a rare disorder and data available indicate a prevalence of 0. 2% in the general population [2,5]. The onset is often in adolescence or early adulthood [6]. Onset is usually sudden [3], and often related to traumatic or stressful life events [2,4,6]. Dissociative fugue has also been noted to be associated with a previous history of child abuse [7] and current severe distress [8]. Other factors predisposing to dissociative reactions include neuropsychological cognitive dysfunctions [9] and genetic factors [10]. Recovery is usually sudden [6] and often complete [2,6], although the fugue state may end gradually in some individuals [3]. However, following recovery there is no amnesia for earlier life events before the dissociative fugue episode [8].
2% in the general population [2,5]. The onset is often in adolescence or early adulthood [6]. Onset is usually sudden [3], and often related to traumatic or stressful life events [2,4,6]. Dissociative fugue has also been noted to be associated with a previous history of child abuse [7] and current severe distress [8]. Other factors predisposing to dissociative reactions include neuropsychological cognitive dysfunctions [9] and genetic factors [10]. Recovery is usually sudden [6] and often complete [2,6], although the fugue state may end gradually in some individuals [3]. However, following recovery there is no amnesia for earlier life events before the dissociative fugue episode [8].
Alcohol, hallucinogens, marijuana, head trauma, brain tumors, dementia, hypertension, manic episode and schizophrenia may cause effects similar to dissociative fugue [3]. It is therefore expedient that a differentiation be made between a dissociative fugue episode and dissociative fugue-like symptoms caused by a medical condition or psychological disorder. Dissociative fugue can comorbid with bipolar disorder, major depressive disorder, schizophrenia, post-traumatic stress disorder, substance-related disorders, panic disorder, anxiety disorders, eating disorders and somatoform disorders [2,3].
Dissociative fugue can comorbid with bipolar disorder, major depressive disorder, schizophrenia, post-traumatic stress disorder, substance-related disorders, panic disorder, anxiety disorders, eating disorders and somatoform disorders [2,3].
Treatment of dissociative fugue is by use of psychotherapy. Attempts are made to elicit stressors preceding the disorder [6], and psycho-education is given to both the patient and family. Efforts are made to reduce stressors that may precipitate another episode. However, if the patient is still in a fugue state, the first concern is to ensure the safety and well-being of the patient. As dissociative fugue is often comorbid with psychiatric disorders, drug treatments may be necessary for the latter.
The patient is a 28-year old male final year medical student from the South-Eastern region of Nigeria in sub-Saharan Africa. He was declared missing for 10 days prior to presentation because his whereabouts was unknown. He was later seen in a city in South-Western Nigeria, a distance of about 634km from South-Eastern Nigeria where he lived and schooled. Ten days before presentation, while studying in his room alone at night, the patient suddenly saw a full human skeleton reading at the same table with him, sitting at the opposite side. At the same time, the patient claimed he felt unease and quite uncomfortable. He saw the whole room turning with everything inside becoming unstable and unreal. After this he had overwhelming fears and did not know when he left the room. Two days later, he discovered he was with his younger sibling in South-Western Nigeria. The patient had no knowledge of how he made the journey that takes approximately 8 hours by road. He equally could not remember where he slept the night he left his room, how he raised money for the journey or the buses and routes he took. The patient denied all memory of events for the 2 days from when he left his room at the university to the time he suddenly realized he was at his brother’s house, 634km away. The brother, however, reported that the patient appeared unkempt, looked exhausted but was fully conscious and alert on arrival at his house without any assistance.
Ten days before presentation, while studying in his room alone at night, the patient suddenly saw a full human skeleton reading at the same table with him, sitting at the opposite side. At the same time, the patient claimed he felt unease and quite uncomfortable. He saw the whole room turning with everything inside becoming unstable and unreal. After this he had overwhelming fears and did not know when he left the room. Two days later, he discovered he was with his younger sibling in South-Western Nigeria. The patient had no knowledge of how he made the journey that takes approximately 8 hours by road. He equally could not remember where he slept the night he left his room, how he raised money for the journey or the buses and routes he took. The patient denied all memory of events for the 2 days from when he left his room at the university to the time he suddenly realized he was at his brother’s house, 634km away. The brother, however, reported that the patient appeared unkempt, looked exhausted but was fully conscious and alert on arrival at his house without any assistance.
Prior to this episode, the patient had been under severe economic and academic pressures. The younger brother who paid the patient’s bills had threatened to withdraw his sponsorship because of the patient’s prolonged stay in school beyond the stipulated duration of training occasioned by his repeats of examinations and classes. The patient had been worried that he might also fail in his final qualifying examinations scheduled to be held in 3 months. He subsequently became involved in several religious activities to obviate his perception of impending doom.
The patient admitted to having low mood, loss of interest in usually pleasurable activities and poor appetite. He had lost weight and most often preferred being alone. He had also been feeling weak especially in the morning hours but had managed to grudgingly carry on with the day’s activities. He had suicidal ideation but never attempted suicide. The patient slept poorly at night. His sleep had been marked by early morning wakefulness and waking up not feeling refreshed.
There were no symptoms suggestive of seizure, manic episode, schizophrenia, anxiety or organic disorders. He never drank alcohol or abused any psychoactive substances. The patient denied a history of head trauma or loss of consciousness in the past.
Past medical, psychiatric, family and personal histories revealed no significant findings.
Examination of his mental state revealed a young man who was clean, appropriately dressed and mildly emaciated with poor eye contact. His mood was depressed. He had preceding visual and derealization perceptual disorders. He had no thought disorders. The patient was oriented in time, place and person but had impaired attention and concentration at the time of the examination. Immediate recall, short- and long-term memory were intact. However, there was amnesia for the 2 days he wandered away from school. Judgment and insight were not impaired.
His physical examination was unremarkable. Neurological assessment and basic laboratory testing revealed no significant abnormalities.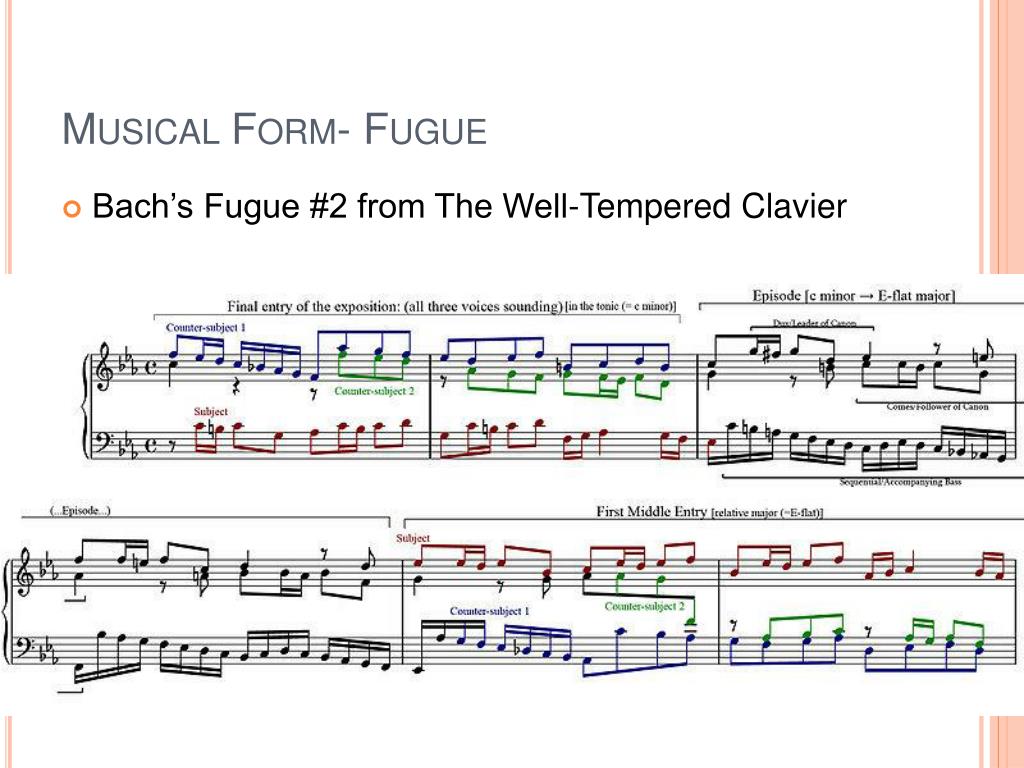
An electroencephalogram reported no seizure activity. A computed axial tomography of the brain was not done because the patient lacked resources to pay for it. Also, a test for blood alcohol level and urine drug screening were not done because the hospital had no facilities for the tests.
The Dissociative Experiences Scale (DES) was administered to the patient and he had a score of 50%. The DES is an effective screening instrument for dissociative disorders [11,12].
A diagnosis of dissociative fugue-like syndrome was made with comorbid major depressive episode. He was engaged in psychotherapy by the departmental clinical psychologists and his depression was treated with paroxetine. He responded very well and was able to write his final qualifying examinations 3 months later. He, however, did not pass either of the two subjects examined.
At 6-month follow up, the patient could still not recall events for the 2 days from when he left school to the time he was seen in his brother’s house, 634km away.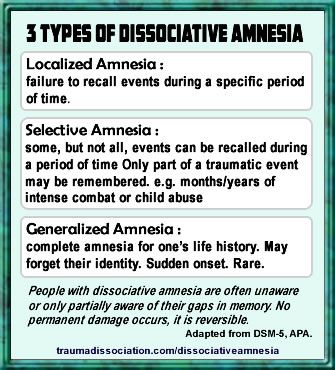 He reported no further periods of amnesia or wandering away from his place of residence.
He reported no further periods of amnesia or wandering away from his place of residence.
The observation in this case report brings to the fore that dissociative fugue is often related to stressful life events and can occur with a comorbid depressive disorder.
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The author declares that he has no competing interests.
The author thanks Dr C.G. Nwigwe, the Chairman of the Medical Advisory Committee, Federal Teaching Hospital Abakaliki, Ebonyi State Nigeria for the all-round support to the patient and the author at the early stages of caring for this patient.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, Text Revision) Washington, DC: American Psychiatric Publishing; 2000. [Google Scholar]
- Gelder M, Harrison P, Cowen P.
 Shorter Oxford Textbook of Psychiatry. 5. New York: Oxford University Press; 2006. [Google Scholar]
Shorter Oxford Textbook of Psychiatry. 5. New York: Oxford University Press; 2006. [Google Scholar] - Coons PM. Psychogenic or dissociative fugue: a clinical investigation of five cases. Psychol Rep. 1999;84:881–886. doi: 10.2466/pr0.1999.84.3.881. [PubMed] [CrossRef] [Google Scholar]
- Macleod AD. Posttraumatic stress disorder, dissociative fugue and a locator beacon. Aust N Z J Psychiatry. 1999;33:102–104. doi: 10.1046/j.1440-1614.1999.00514.x. [PubMed] [CrossRef] [Google Scholar]
- Davison GC, Neale JM. Abnormal Psychology With Cases. 8. New York: John Wiley & Sons; 2003. [Google Scholar]
- Moore DP. Handbook of Medical Psychiatry. St. Louis: Mosby-Year Book, Inc.; 1996. [Google Scholar]
- Zlotnick C, Begin A, Shea MT, Pearlstein T, Simpson E, Costello E. The relationship between characteristics of sexual abuse and dissociative experiences. Compr Psychiatry. 1994;35(6):465–470. doi: 10.1016/0010-440X(94)90230-5. [PubMed] [CrossRef] [Google Scholar]
- Ahuja N.
 A Short Textbook of Psychiatry. New Delhi: Jaypee Brothers; 2006. [Google Scholar]
A Short Textbook of Psychiatry. New Delhi: Jaypee Brothers; 2006. [Google Scholar] - MacDonald K, MacDonald T. Peas, please: a case report and neuroscientific review of dissociative amnesia and fugue. J Trauma Dissociation. 2009;10(4):420–435. doi: 10.1080/15299730903143618. [PubMed] [CrossRef] [Google Scholar]
- Amrhein C, Hengmith S, Maragkos M, Hennig-Fast K. Neuropsychological characteristics of highly dissociative healthy individuals. J Trauma Dissociation. 2008;9(4):525–542. doi: 10.1080/15299730802226332. [PubMed] [CrossRef] [Google Scholar]
- Ross CA, Norton GR, Wozney K. Multiple personality disorder: an analysis of 236 cases. Can J Psychiatry. 1989;34:413–418. [PubMed] [Google Scholar]
- Carlson EB, Putnam FW, Ross CA, Torem M, Coons P, Dill DL, Loewenstein RJ, Braun BG. Validity of the dissociative experiences scale in screening for multiple personality disorder: a multicenter study. Am J Psychiatry. 1993;150(7):1030–1036. [PubMed] [Google Scholar]
Articles from Journal of Medical Case Reports are provided here courtesy of BioMed Central
what is a dissociative fugue - T&P
In cinema, there is often a story about "a man without a past.
 " The hero suddenly finds himself in an incomprehensible place - without things, satellites and any memories of what happened to him until that moment. By the end of the film, the intrigue is usually revealed, and the memory returns. This kind of story is not a fantasy of screenwriters, but a description of a real psychiatric phenomenon - a dissociative fugue.
" The hero suddenly finds himself in an incomprehensible place - without things, satellites and any memories of what happened to him until that moment. By the end of the film, the intrigue is usually revealed, and the memory returns. This kind of story is not a fantasy of screenwriters, but a description of a real psychiatric phenomenon - a dissociative fugue. On January 17, 1887, the American priest Ansel Bourne got up early in the morning and went to the bank. There he withdrew all his savings and got on a carriage going to another city. This is the last event Bourne remembers. He did not return home that evening, and neither did he the next evening. His relatives filed a missing person's notice in the newspapers. Meanwhile, in one of the neighboring states, an unknown A. J. Brown showed up. The man rented a shop and started selling small goods.
But a couple of months later, the newly minted businessman woke up in a fright and called his housemates. He said that his name was Ansel Bourne, that he had no idea where he was and how he got here, and that just yesterday he took money from the bank, and then there was a blackout. Hearing the story about his own shop, the priest was horrified and admitted that he knew nothing about trade. Moreover, despite all the stories of witnesses, he himself did not remember his adventures.
Hearing the story about his own shop, the priest was horrified and admitted that he knew nothing about trade. Moreover, despite all the stories of witnesses, he himself did not remember his adventures.
Some people in the dissociative fugue not only forget the old life, but also create a new personality - with a different name, biography, and even with abilities atypical of the former personality.
It was not only the household that rejoiced at Burnu's return home. William James, an American philosopher and psychologist, became interested in its history. He performed a hypnotic session with the priest, and in a trance, the personality of the mythical A.J. Brown reappeared. The imaginary shopkeeper knew nothing about Bourne, but he spoke in detail about his life during those two months and trade, which he knew well. The story heard under hypnosis helped the psychologist describe this clinical case in detail in his book. It was he who later gave this phenomenon the name "dissociative fugue". Dissociation in psychiatry is a state when the patient feels like anyone but himself. He may look at himself from the outside, or simply feel like someone else. And "fugue" in Latin means "flight".
Dissociation in psychiatry is a state when the patient feels like anyone but himself. He may look at himself from the outside, or simply feel like someone else. And "fugue" in Latin means "flight".
According to medical statistics, dissociative fugue occurs in 0.2% of the population, that is, approximately two people out of 1,000. In modern psychiatry, this term is used to describe a condition when a patient suddenly and purposefully leaves or goes somewhere, completely forgetting who he is such a. In this state, a person, as a rule, retains basic knowledge such as geography and multiplication tables, but he completely forgets events from his own life, his address and even his name. Therefore, it can be difficult for relatives to find missing patients with fugue.
Something similar, for example, happened to Agatha Christie. In 1926, after her mother's death and her husband's infidelity, Christie left home. Nothing was known about her whereabouts for 11 days. The detective queen's books have already become popular, so the story has caused a lot of buzz. The English police, conducting the search, first found an abandoned car, and a couple of days later, Agatha herself. She didn't remember anything about what had happened. Having collected eyewitness accounts, the investigators learned that the writer checked into the hotel under the name of her husband's mistress, after which she read books for 11 days, underwent healing procedures and played the piano. Later, the British psychologist Andrew Norman called this case a typical example of a dissociative fugue.
The English police, conducting the search, first found an abandoned car, and a couple of days later, Agatha herself. She didn't remember anything about what had happened. Having collected eyewitness accounts, the investigators learned that the writer checked into the hotel under the name of her husband's mistress, after which she read books for 11 days, underwent healing procedures and played the piano. Later, the British psychologist Andrew Norman called this case a typical example of a dissociative fugue.
Some people in a dissociative fugue not only forget their old life, but also create a new personality — with a different name, biography, and even abilities atypical of the former personality. Quite often, "new people" find work in areas that have nothing to do with their previous field of activity.
A dissociative fugue is usually caused by a traumatic experience. A person cannot cope with it and tries to literally run away from an unpleasant situation and everything connected with it.
Psychiatrists are usually able to interview survivors of a fugue episode after the fact, after returning to the old reality, because the new person will never be able to realize that he is new until he remembers the old one. People experiencing this state are often able to clearly and joyfully tell anyone who wants to make up a biography, easily maintain secular conversation and do not have external signs of mental disorders. It is said that patients with fugue are often much more sociable during an attack than in their life before it.
However, not all stories look so literary. Some of the fugitives simply lose their memory, not replacing their identity with a new one, or confusingly tell fictional biographies in such a way that anyone will notice inconsistencies. The fugue usually lasts from a couple of hours to several months.
In May 1985, the young and ambitious American journalist Jody Roberts left home and never returned. Her parents initially decided that her daughter had gone on vacation or was conducting a journalistic investigation. But months passed, and the girl did not return. The police investigation turned up nothing and Jody was declared dead. But 12 years later, she was suddenly found living in the state of Alaska. True, she was no longer a young journalist: the woman introduced herself as Jane Dee, successfully worked as a web designer, lived with her husband and raised four children. And although there were those among the reporters who covered this story who considered Jodie an amnesia scam, psychiatrists unanimously declared that the woman had a dissociative fugue.
But months passed, and the girl did not return. The police investigation turned up nothing and Jody was declared dead. But 12 years later, she was suddenly found living in the state of Alaska. True, she was no longer a young journalist: the woman introduced herself as Jane Dee, successfully worked as a web designer, lived with her husband and raised four children. And although there were those among the reporters who covered this story who considered Jodie an amnesia scam, psychiatrists unanimously declared that the woman had a dissociative fugue.
These conditions are usually caused by a traumatic experience. A person cannot cope with it and tries to literally run away from an unpleasant situation and everything connected with it. That is why fugue cases are on the rise in places where there has been a recent natural disaster or financial crisis. It is believed that some teenagers run away from home in a state of dissociative fugue.
This state passes as suddenly as it began. A word, a proper name, a familiar place can bring back lost memories. At this moment, people often forget everything that they experienced during the fugue. A psychotherapist who knows hypnosis can help them remember the days and months they have lived. Unfortunately, psychological help for patients who have experienced a disorder is needed not only in this. After a long dissociative fugue, people actually find themselves in their future, having missed a significant piece of the life of their loved ones. And coming to terms with the changes that have taken place is sometimes not easy.
A word, a proper name, a familiar place can bring back lost memories. At this moment, people often forget everything that they experienced during the fugue. A psychotherapist who knows hypnosis can help them remember the days and months they have lived. Unfortunately, psychological help for patients who have experienced a disorder is needed not only in this. After a long dissociative fugue, people actually find themselves in their future, having missed a significant piece of the life of their loved ones. And coming to terms with the changes that have taken place is sometimes not easy.
As a rule, dissociative fugue occurs only once in a lifetime. However, in people with multiple personality disorder, it can also be repeated. Each of the alternative personalities may have their own goals and interests, and it is impossible to predict where they will lead the "owner of the body" in the future.
Planet Ka-Pax
In the first half of the film, the protagonist is trying to cure a patient who came to him, convinced of his alien origin, from a dissociative fugue.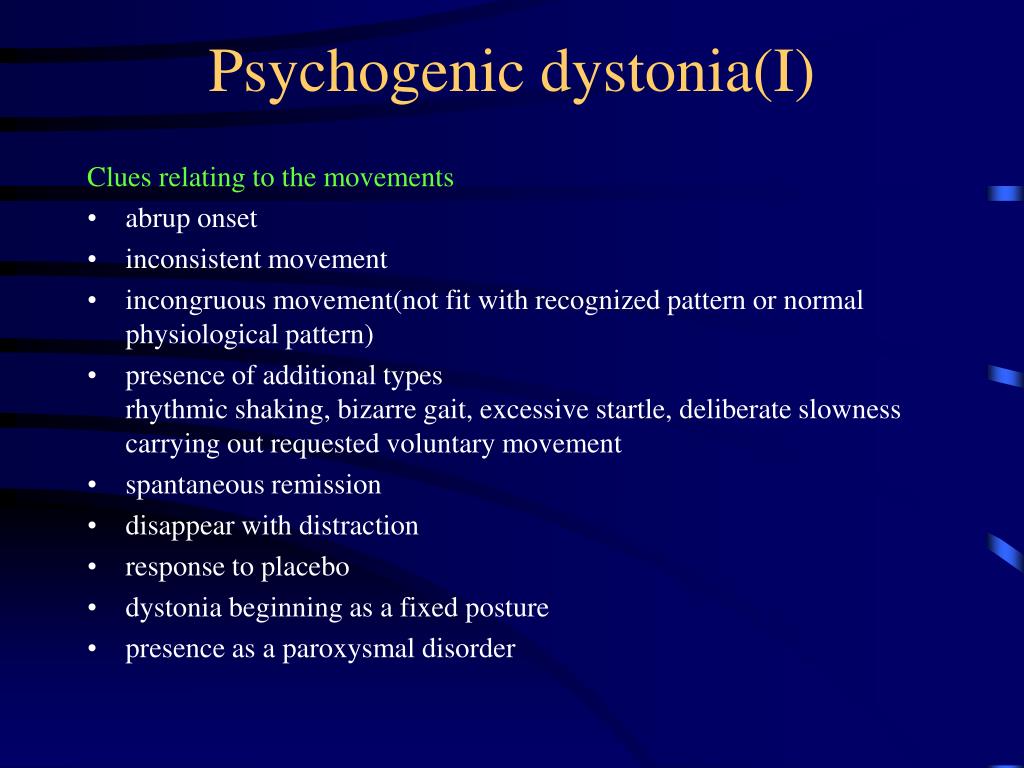 And the other half is tormented by doubts whether he is definitely sick or whether Ka-Pex is really his home.
And the other half is tormented by doubts whether he is definitely sick or whether Ka-Pex is really his home.
Highway to nowhere
Saxophonist Fred is imprisoned on suspicion of murdering his wife, but behind bars he turns into another man with a new biography - Pete Dayton. Pete does not remember how he ended up in prison, but after a series of strange adventures and symbolic events, he becomes Fred again. The Highway to Nowhere script originally contained no hints of a dissociative fugue. They say that this idea was thrown to Lynch already on the set, and she completely changed the interpretation of the film.
House of Dreams
In this film, the director creatively interprets the dissociative fugue, and the hero, experiencing this disorder, takes on his own personality, simply from a different period of life.
United States of Tara
In the TV series about a versatile woman named Tara, they show what a dissociative fugue looks like in people with multiple personality disorder: four different people “live” in the main character at once.
Dissociative fugue - causes, symptoms, diagnosis and treatment
Dissociative fugue is an acute mental disorder in which the patient, under the influence of traumatic events, suddenly leaves his place of residence, completely losing memories of his own personality. During the fugue period, the patient can invent a new personality and start a new life. The condition lasts from several hours to several months (in some cases - years) and just as suddenly ends with a return to the former personality. Memories of life during the fugue are lost. The diagnosis is exposed on the basis of the anamnesis. Psychotherapeutic treatment - assistance in eliminating a traumatic situation or correcting attitudes towards this situation.
General information
Dissociative fugue - a mental disorder accompanied by a sudden move and a complete loss of memory of one's own personality. Information of a general nature remains in the patient's memory, the intellect does not suffer, there are no disturbances of consciousness. After some time, patients return to their former personality, completely losing their memories of the events that occurred during the fugue period. The disorder occurs in 0.2% of the population.
After some time, patients return to their former personality, completely losing their memories of the events that occurred during the fugue period. The disorder occurs in 0.2% of the population.
This pathology is well known to the general public and is one of the popular plots of American action films and psychological thrillers (the most famous example is The Long Kiss Goodnight). It is assumed that in reality this disorder occurred in Agatha Christie during her famous 11-day absence. In the specialized literature, descriptions of this pathology appeared in the 19th century, the most famous example is the case of the priest Ansel Bourne, recorded by the American psychologist William James in 1890 year. Treatment is carried out by specialists in the field of psychiatry, psychotherapy and clinical psychology.
Dissociative fugue
Causes of dissociative fugue
Experts believe that dissociative fugue is a protective mental mechanism designed to protect patients from unbearable experiences and extreme stress.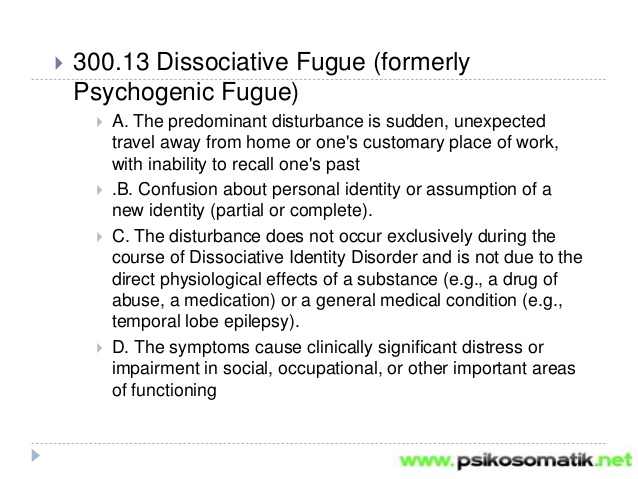 Patients literally feel the need to escape from the current situation, and the psyche realizes this need in a way that is accessible to it. Most often, the disorder occurs when there is an immediate threat to physical existence or the loss of important close relationships: when participating in hostilities, staying in a territory where hostilities are taking place, natural and man-made disasters, or multiple deaths of loved ones.
Patients literally feel the need to escape from the current situation, and the psyche realizes this need in a way that is accessible to it. Most often, the disorder occurs when there is an immediate threat to physical existence or the loss of important close relationships: when participating in hostilities, staying in a territory where hostilities are taking place, natural and man-made disasters, or multiple deaths of loved ones.
Less commonly, less global experiences become the impetus for the development of the disease: severe financial problems, conflicts in the family, dismissal, professional collapse, personal insults, etc. In all cases, the disorder is based on a powerful intrapersonal conflict, inability to accept reality and desire in any way avoid emotionally traumatic situations. The likelihood of developing this condition increases with chronic alcoholism, increased anxiety, phobias, hysteroid personality type and violent choleric temperament. In individuals with multiple personality disorder, fugue may occur repeatedly. In other cases, this condition does not recur.
In other cases, this condition does not recur.
Symptoms of dissociative fugue
Dissociative fugue begins suddenly, usually after a night's sleep. The patient wakes up, performs purposeful activities to prepare for departure (gets dressed, packs a suitcase, buys a ticket), and then leaves. There are cases in the literature when people withdrew large sums of money from the bank before leaving. As a rule, all these actions go unnoticed by relatives, from their point of view, the situation looks like “the person left and did not return.”
The patient behaves calmly and adequately, often in a new place, people around do not even suspect that something is wrong. With a prolonged fugue (lasting up to several months or more), some patients create a new identity, get a job, enter into new close relationships, and even have children. In doing so, they usually choose a different field of activity and become more sociable than before the start of the fugue. Memories of a general nature (geographical information, multiplication table) are fully preserved. The degree of plausibility of a new personality can vary - from a holistic, consistent picture to fragmentary information.
Memories of a general nature (geographical information, multiplication table) are fully preserved. The degree of plausibility of a new personality can vary - from a holistic, consistent picture to fragmentary information.
Sometimes a discrepancy between the patient's personality and his stories is discovered when trying to get a loan from a bank, after criminal incidents, traffic accidents and other situations related to checking documents. In other cases, the patient lives for some time safely in a new reality and a new personality. Separate memories of life before the dissociative fugue may appear as dreams or be perceived as plots of books once read.
The return to the old personality usually occurs suddenly, after a night's sleep. The patient wakes up in a state of severe anxiety, realizing himself as a former person. He is disoriented, does not understand where he is, and does not know what is happening. Memories of life during the period of the fugue are usually completely lost, less often separate fragments of events that took place during the period of disorder emerge in memory. After that, the patient returns to his former life. At the same time, it can be difficult for him to adapt to the changes that have occurred during his absence.
After that, the patient returns to his former life. At the same time, it can be difficult for him to adapt to the changes that have occurred during his absence.
With prolonged fugues, there is sometimes a gradual transition to the former personality. At first, the patient begins to feel inner anxiety, he does not leave the feeling that something is wrong, that he has lost something important. Then episodes from his past life gradually emerge in his memory. The main personality "manifests" and takes its rightful place, displacing the old one. The last stage may be accompanied by severe anxiety, decreased mood, vague fears, and social disorientation.
With short fugues (lasting from several hours to several days), large-scale changes, as a rule, do not have time to occur. The patient leaves somewhere, and then comes to his senses in a new place, also completely losing his memories of the period of illness. Intellectual abilities, professional knowledge and character traits are fully preserved regardless of the duration of the disorder. Organic brain damage is absent.
Organic brain damage is absent.
Diagnosis and treatment of dissociative fugue
Psychiatrists and psychotherapists rarely have to work with patients who are in a state of dissociative fugue, because they do not present any complaints and do not seek medical help. The diagnosis can usually be established only after the fact, after returning to the previous personality. There are two mandatory criteria by which dissociative fugue is differentiated from other dissociative disorders. The first is the obligatory departure from home at the beginning of the fugue. The second is the complete or partial loss of memories of the first person during the fugue period and of the second person (if any) after leaving the pathological state, combined with the preservation of all universal knowledge and skills.
The main task of psychiatrists and psychotherapists is to help and support in processing a stressful situation and changing the patient's attitude to the events that caused the development of dissociative fugue.