Ocd symptoms toddlers
Obsessive-Compulsive Disorder (OCD) in Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is obsessive-compulsive disorder in children?
Obsessive-compulsive disorder (OCD) is a type of anxiety disorder. Obsessions are recurring thoughts. Compulsions are recurring behaviors.
A child with OCD has obsessive thoughts that are not wanted. They are linked to fears, such as touching dirty objects. He or she uses compulsive rituals to control the fears, such as excessive handwashing.
As children grow, rituals and obsessive thoughts normally happen with a purpose and focus based on age. Preschool children often have rituals and routines around meals, bathing, and bedtime. These help stabilize their expectations and view of their world. School-aged children often create group rituals as they learn to play games, take part in team sports, and recite rhymes.
Older children and teens start to collect objects and have hobbies. These rituals help children to socialize and learn to deal with anxiety.
When a child has OCD, obsessive thoughts and compulsive rituals can become very frequent and strong. They may interfere with daily living and normal development. OCD is more common in teens.
What causes OCD in a child?
The cause of OCD is not known. Research suggests it’s a brain problem. People with OCD don’t have enough of a chemical called serotonin in their brain.
OCD tends to run in families. So it may be genetic. But it may also occur without a family history of OCD. In some cases, streptococcal infections may trigger OCD or make it worse.
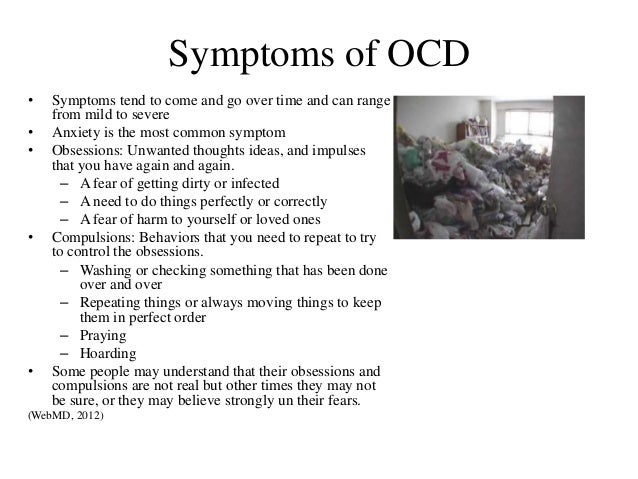
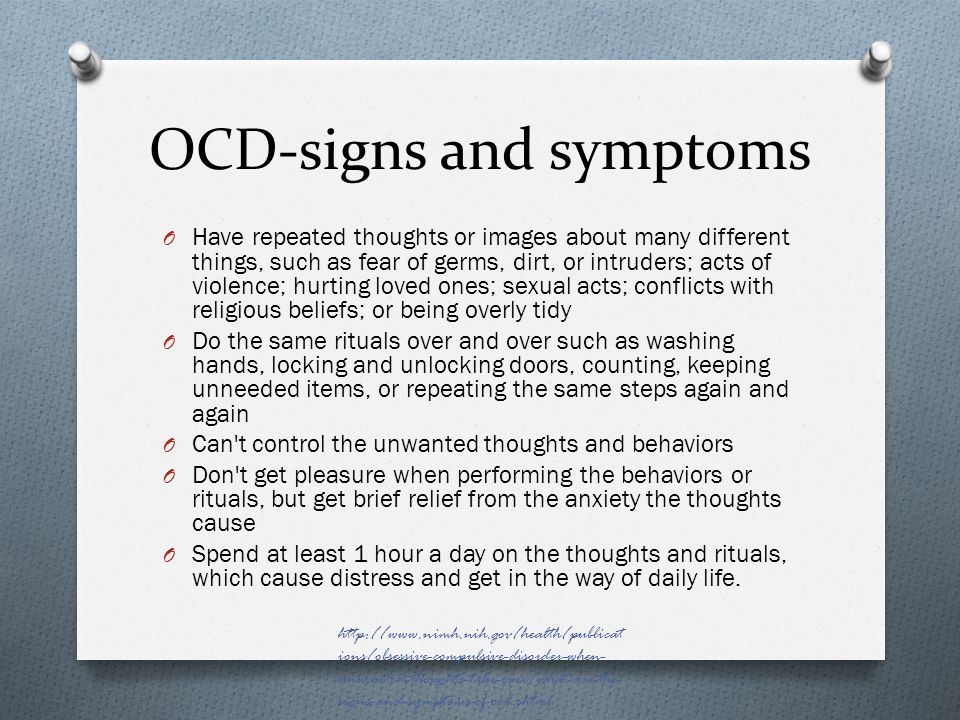
What are the symptoms of OCD in a child?
Each child may have different symptoms. These are the most common symptoms:
- An extreme obsession with dirt or germs
- Repeated doubts, such as whether or not the door is locked
- Interfering thoughts about violence, hurting or killing someone, or harming oneself
- Long periods of time spent touching things, counting, and thinking about numbers and sequences
- Preoccupation with order, symmetry, or exactness
- Ongoing thoughts about doing offensive sexual acts or forbidden, taboo behaviors
- Troubled by thoughts that are against personal religious beliefs
- A great need to know or remember things that may be very minor
- Too much attention to detail
- Too much worrying about something bad occurring
- Aggressive thoughts, urges, or behaviors
Compulsive behaviors are the repetitive rituals used to ease anxiety caused by the obsessions. They can be excessive, disruptive, and time-consuming. They may interfere with daily activities and relationships. They may include:
They can be excessive, disruptive, and time-consuming. They may interfere with daily activities and relationships. They may include:
- Repeated handwashing (often 100 or more times a day)
- Checking and rechecking many times, such as making sure that a door is locked
- Following firm rules of order, such as putting on clothes in the very same order each day
- Hoarding objects
- Counting and recounting a lot
- Grouping objects or putting things in a certain order
- Repeating words spoken by oneself or others
- Asking the same questions again and again
- Repeatedly using four-letter words or making rude (obscene) gestures
- Repeating sounds, words, numbers, or music to oneself
The symptoms of OCD may seem like other health problems.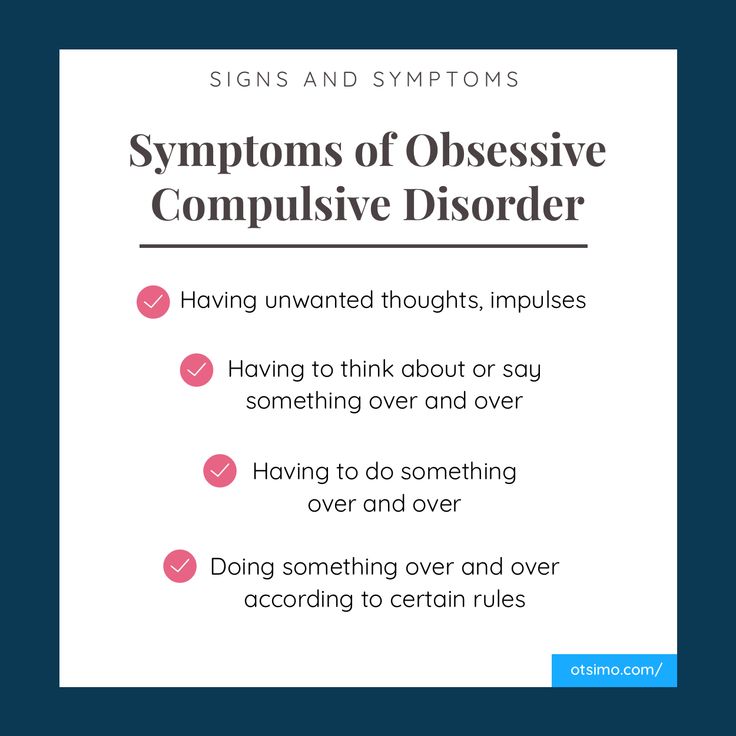 Have your child see his or her healthcare provider for a diagnosis.
Have your child see his or her healthcare provider for a diagnosis.
How is OCD diagnosed in a child?
A child psychiatrist or other mental health expert can diagnose OCD. He or she will do a mental health evaluation of your child. To be diagnosed with OCD, your child must have obsessions and compulsions that are continuous, severe, and disruptive. They must harm your child’s day-to-day living.
In most cases, the activities of OCD such as handwashing or checking the locks on doors use up more than 1 hour each day. They also cause mental health distress and affect how your child thinks. In most cases, adults realize that their actions are not normal to some degree. But often children can't see that their behavior is irrational and abnormal.
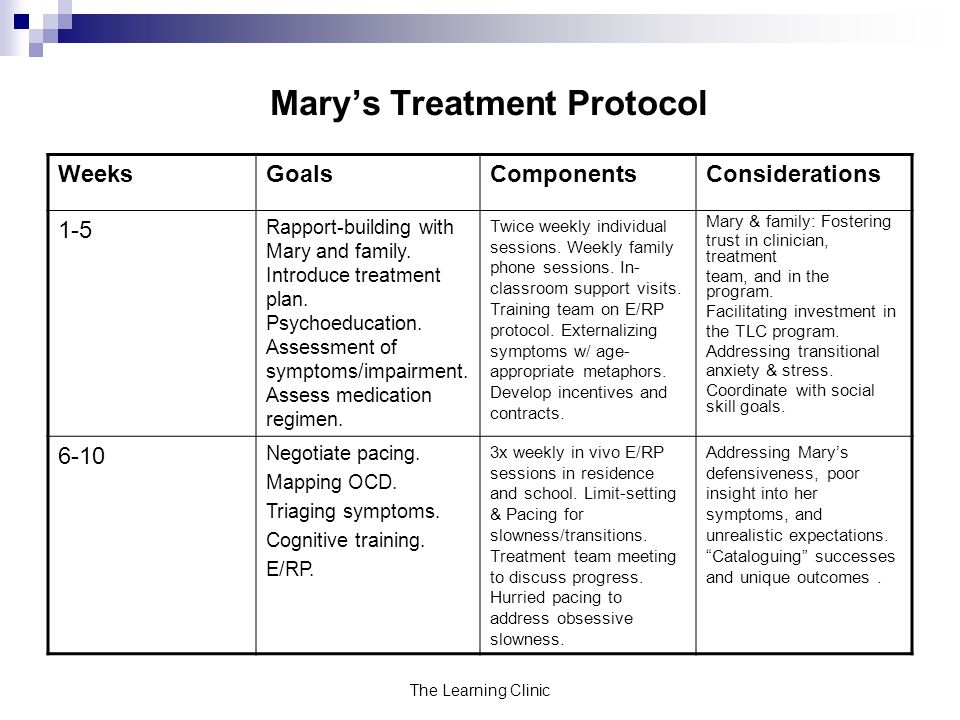
How is OCD treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment for OCD often includes a combination of the following:
- Therapy with cognitive and behavioral methods.
 Cognitive methods help a child identify and understand his or her fears. They also teach a child new ways to better resolve or reduce those fears. Behavioral methods help the child and their family make pacts or rules to limit or change behaviors. One example is setting a maximum number of times a compulsive handwasher may wash his or her hands.
Cognitive methods help a child identify and understand his or her fears. They also teach a child new ways to better resolve or reduce those fears. Behavioral methods help the child and their family make pacts or rules to limit or change behaviors. One example is setting a maximum number of times a compulsive handwasher may wash his or her hands. - Family therapy. Parents play a vital role in any treatment process. A child’s school may also be included in care.
- Selective serotonin reuptake inhibitors (SSRIs). These medicines help raise serotonin levels in the brain.
- Antibiotics. Your child may need these medicines if his or her OCD is found to be linked to a streptococcal infection.
Teens with OCD may also have one or more types of eating disorders. These will also need treatment.
These will also need treatment.
How can I help prevent OCD in my child?
Experts don’t know at this time how to prevent OCD in children and teens. But if you notice signs of OCD in your child, you can help by getting an evaluation as soon as possible. Early treatment can ease symptoms and enhance your child’s normal development. It can also improve his or her quality of life.
How can I help my child live with OCD?
OCD can be treated, often with a combination of one-on-one therapy and medicines. You play a key supportive role in your child’s treatment. Here are things you can do to help your child:
- Keep all appointments with your child’s healthcare provider.
- Talk with your child’s healthcare provider about other providers who will be included in your child’s care. Your child may get care from a team that may include counselors, therapists, social workers, psychologists, and psychiatrists.
 Your child’s care team will depend on your child’s needs and how serious the OCD is.
Your child’s care team will depend on your child’s needs and how serious the OCD is. - Keep strong and open lines of communication with your child. Children with OCD can feel embarrassed about their disorder.
- Tell others about your child’s disorder. Work with your child’s healthcare provider and school to create a treatment plan.
- Reach out for support from local community services. Being in touch with other parents who have a child with OCD may be helpful.
Key points about OCD in children
- OCD is a type of anxiety disorder. A child with OCD has obsessive thoughts that are not wanted. They are linked to fears, such as touching dirty objects. The child uses compulsive rituals such as handwashing to control the fears. These rituals may feel rational or irrational to the person doing them.
 The child may not understand why they do these rituals. They may feel embarrassed that the behaviors occur and can't be controlled.
The child may not understand why they do these rituals. They may feel embarrassed that the behaviors occur and can't be controlled. - The exact cause of OCD is unknown. Children with OCD don’t have enough of a chemical called serotonin in their brain.
- Obsessive symptoms include repeated doubts and extreme preoccupation with dirt or germs.
- Compulsive behaviors include hoarding objects and checking things often.
- A mental health evaluation is needed to diagnose OCD.
- Treatment includes therapy and medicine.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests.
 Also write down any new instructions your provider gives you for your child.
Also write down any new instructions your provider gives you for your child. - Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Signs & Symptoms of Pediatric OCD
Obsessive compulsive disorder (OCD) is characterized by both obsessions and compulsions.
Obsessions are intrusive and unwanted thoughts, images, or urges that occur over and over again and feel outside of the child’s control. These obsessions are unpleasant for the child and typically cause a lot of worry, anxiety, and distress.
These obsessions are unpleasant for the child and typically cause a lot of worry, anxiety, and distress.
Common obsessions may include:
- Worrying about germs, getting sick, or dying.
- Extreme fears about bad things happening or doing something wrong.
- Feeling that things have to be “just right.”
- Disturbing and unwanted thoughts or images about hurting others.
- Disturbing and unwanted thoughts or images of a sexual nature.
Compulsions (also referred to as rituals) are behaviors the child feels he or she “must do” with the intention of getting rid of the upsetting feelings caused by the obsessions. A child may also believe that engaging in these compulsions will somehow prevent bad things from happening.
Common compulsions may involve:
- Excessive checking (re-checking that the door is locked, that the oven is off).
- Excessive washing and/or cleaning.
- Repeating actions until they are “just right” or starting things over again.
- Ordering or arranging things.
- Mental compulsions (excessive praying, mental reviewing).
- Frequent confessing or apologizing.
- Saying lucky words or numbers.
- Excessive reassurance seeking (e.g., always asking, “Are you sure I’m going to be okay?”).
An OCD diagnosis is warranted when these obsessions and compulsions become so time-consuming that they impair day-to-day functioning (e.g., social, school, self care, etc.). Typically, these symptoms have a gradual onset, developing over the course of several weeks or months.
OCD can start at any time from preschool to adulthood. Although OCD can occur at any age, there are generally two age ranges when OCD tends to first appears:
- Between the ages 8 and 12.
- Between the late teen years and early adulthood.
In rare cases, symptoms may develop seemingly “overnight” with a rapid change in behavior and mood and sudden appearance of severe anxiety. If this is the presentation, then consider a sub-type of pediatric OCD caused by an infection (e.g., strep throat), which confuses the child’s immune system into attacking the brain instead of the infection. This then causes the child to begin having severe symptoms of OCD, often seemingly all at once, in contrast to the gradual onset seen in most cases of pediatric OCD. The sudden appearance of symptoms is very different from general pediatric OCD, where symptoms appear more gradually.
If this is the presentation, then consider a sub-type of pediatric OCD caused by an infection (e.g., strep throat), which confuses the child’s immune system into attacking the brain instead of the infection. This then causes the child to begin having severe symptoms of OCD, often seemingly all at once, in contrast to the gradual onset seen in most cases of pediatric OCD. The sudden appearance of symptoms is very different from general pediatric OCD, where symptoms appear more gradually.
This type of OCD is called Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS) if it is a strep infection, or Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) if it is any other infection.
Click here to learn more about PANDAS/PANS.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
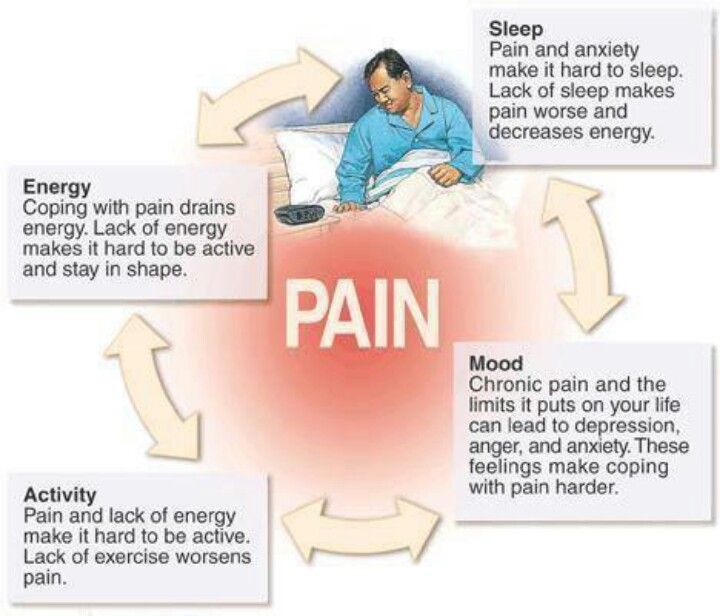
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.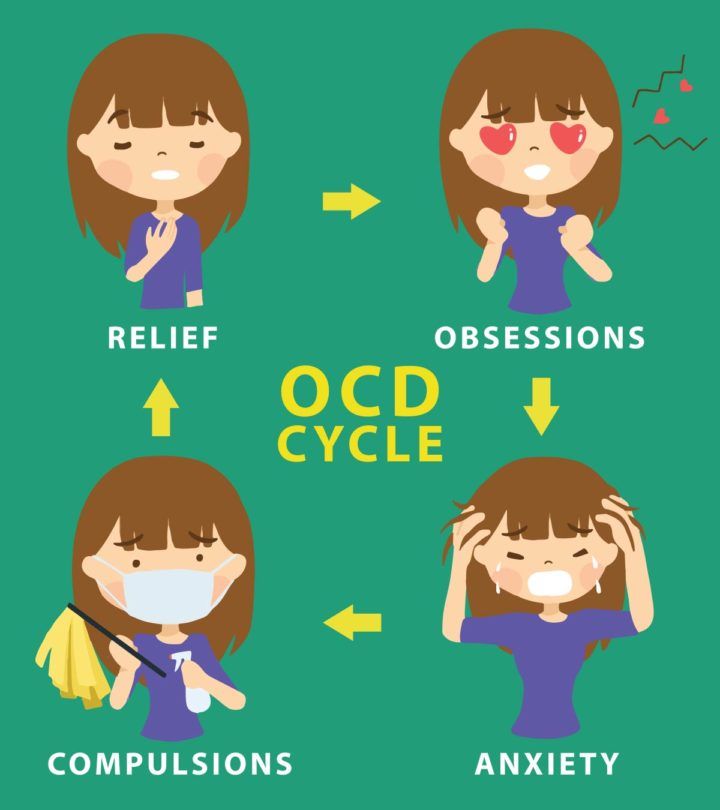
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance.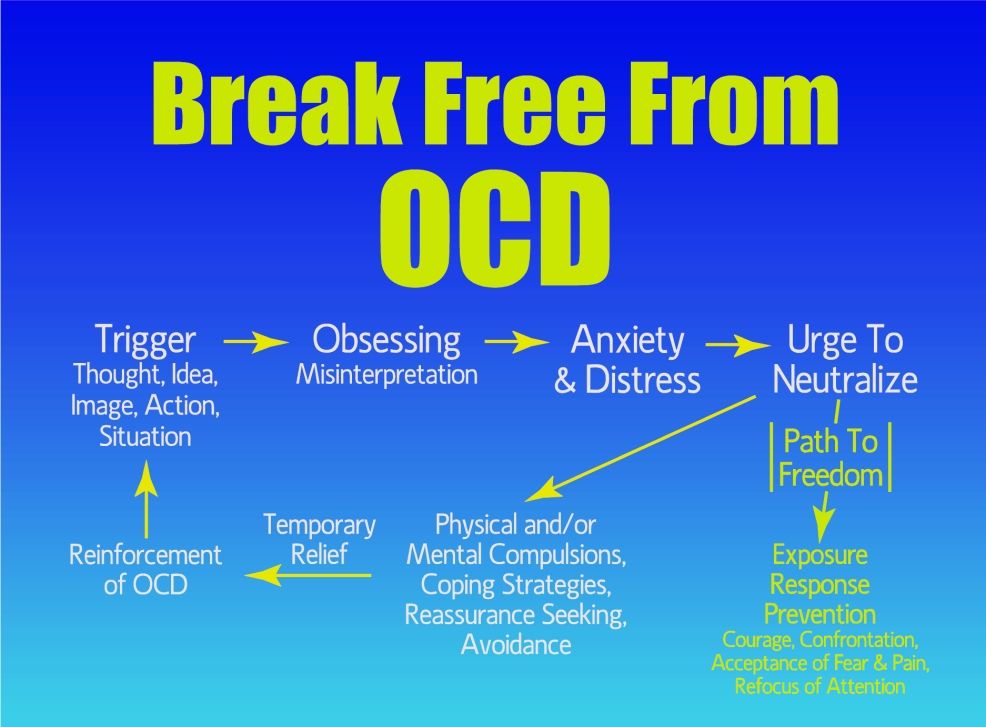 Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result.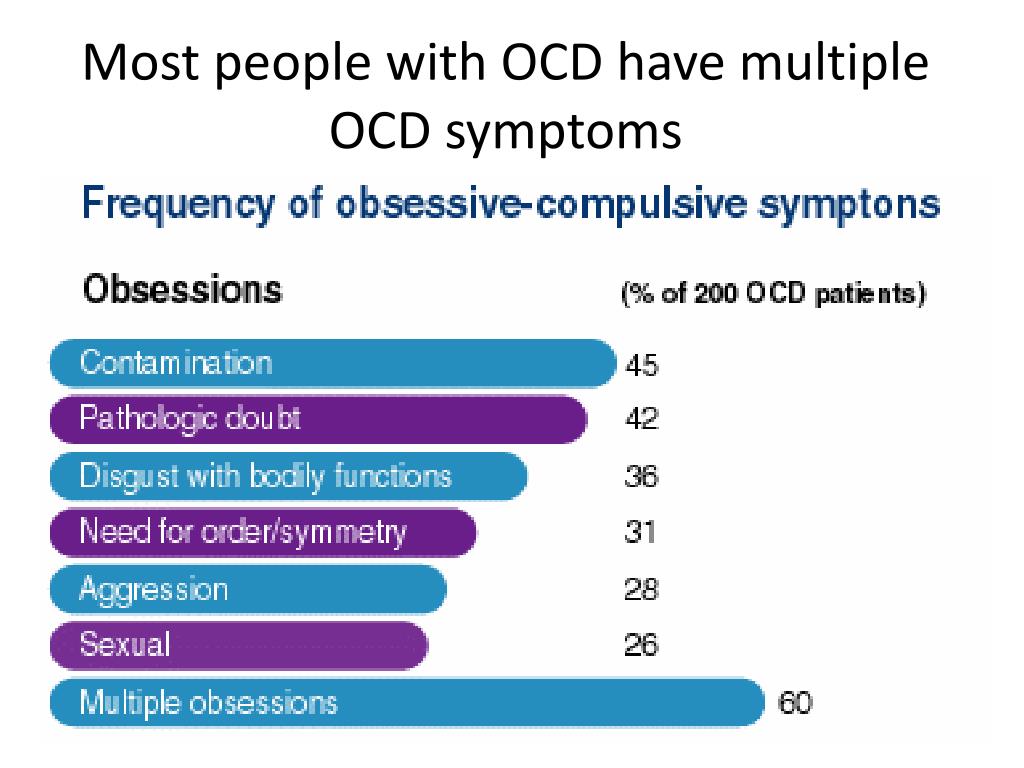 A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
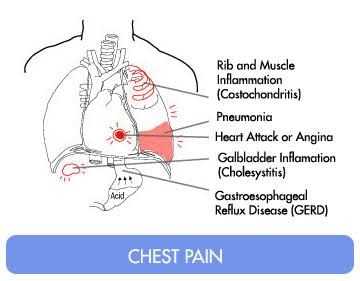
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.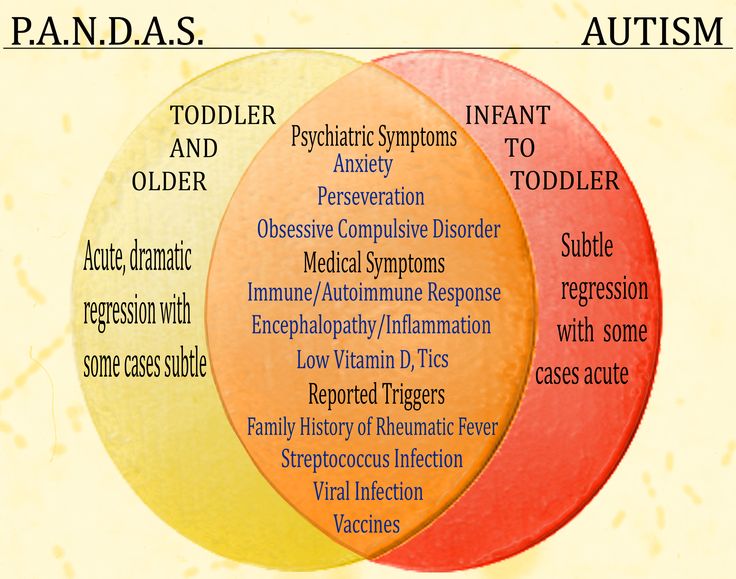 Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive-Compulsive Disorder (OCD) - key facts in English
Obsessive-Compulsive Disorder (OCD)
See our disclaimer that applies to all translations available on this site.
What is obsessive-compulsive disorder?
At times, we can all get hung up on some things, but if:
You obsessively have terrible thoughts even when you try to get rid of them,
You have to count or touch things over and over again, or repeat actions, such as washing your hands,
maybe you have obsessive-compulsive disorder (OCD).
Who gets OCD?
About 1 in 50 people will experience OCD at some point in their lives. Equally, it can be men and women. In the UK, their number is about 1 million people. OCD usually begins in adolescence or early adulthood. Symptoms of OCD may get worse or worse over time, but often people don't seek help for many years.
OCD usually begins in adolescence or early adulthood. Symptoms of OCD may get worse or worse over time, but often people don't seek help for many years.
What are the signs and symptoms of obsessive-compulsive disorder?
- Recurring thoughts that make you feel anxious - "obsessions" or "obsessions". It can be unpleasant words or phrases, mental pictures or doubts.
- The things you do over and over again that help you feel less anxious are 'compulsions'. You can try to correct or "neutralize" thoughts by counting over and over again, saying a special word, or performing certain rituals.
What are the causes of OCD?
Many factors can play a role in the occurrence of OCD. One or more of the following could explain why you or someone you know has OCD.
- In some cases, OCD is inherited, so sometimes the disorder can run in the family.
- Stressful life events cause OCD in about a third of cases.
- Life changes in which you have to take on more responsibility, such as puberty, the birth of a child, or a new job.
- If you have OCD and it lasts for some time, you may develop an imbalance of serotonin (also known as 5HT), a brain neurotransmitter.
- You are a neat, pedantic, methodical person - but you take it too far.
- If you have extremely high standards of morality and responsibility, you may feel especially bad about having unpleasant thoughts. To the point where you start to be wary and keep a close eye on them, which makes them even more likely to appear.
How to help yourself
- If you regularly force yourself to think the thoughts that are bothering you, you will be able to control them better. You can write them down - on a recorder or on paper, and then listen to or reread. You should do this regularly, for about half an hour every day. At the same time, try to resist compulsive behavior.
- Do not use alcohol to control your anxiety.
- If your intrusive thoughts are about your faith or religion, discuss them with your religious leader to help you understand if OCD is a problem.
- Try using a self-help book.
Professional help Various types of psychotherapy
Exposure and response prevention
Helps to stop the mutual reinforcing of compulsive behavior and anxiety.
We know that if you stay in a stressful situation long enough, you will gradually get used to it and the anxiety will go away. In this way, you gradually face the situation that you fear (exposure), but stop yourself from doing your usual compulsive rituals of checking or clearing (avoiding a response) and wait for your anxiety to go away.
Cognitive therapy
Instead of getting rid of your thoughts, cognitive therapy helps you change how you react to them. It specifically targets unrealistic self-critical thoughts. Useful if you have intrusive thoughts but are not performing any rituals or activities to reduce your anxiety. Can be used with Exposure and Response Prevention.
Antidepressant treatment
Even if you are not depressed, SSRI (Selective Serotonin Reuptake Inhibitor) antidepressants can help.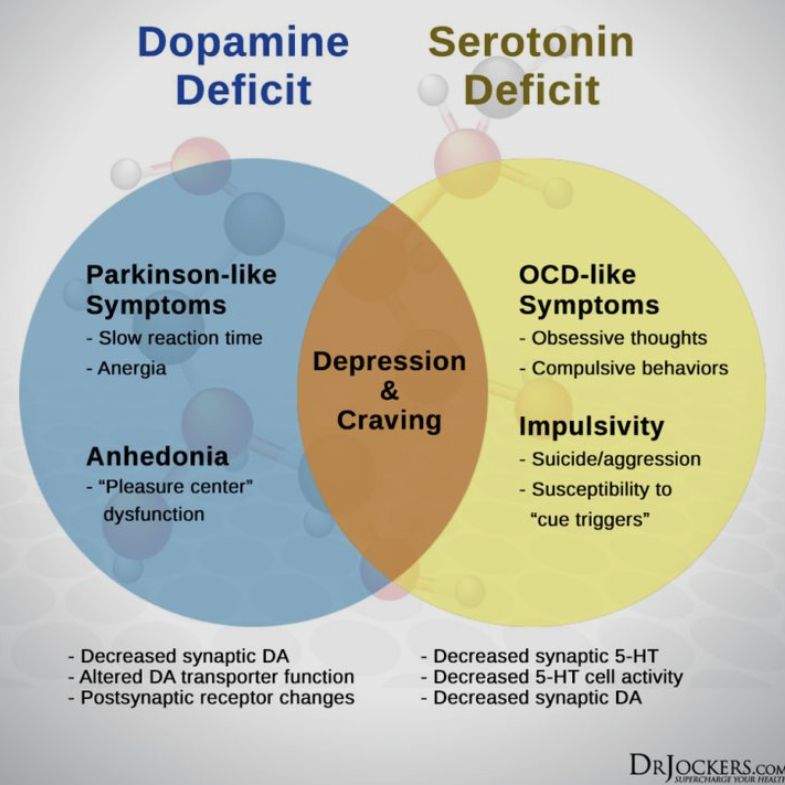 They may be used alone or with cognitive behavioral therapy for moderate to severe OCD. If the medicine doesn't help at all after three months of taking it, you can change it to another SSRI antidepressant or a medicine called Clomipramine (Anafranil).
They may be used alone or with cognitive behavioral therapy for moderate to severe OCD. If the medicine doesn't help at all after three months of taking it, you can change it to another SSRI antidepressant or a medicine called Clomipramine (Anafranil).
How effective is the treatment?
Exposure and prevention of response
About three out of four people who completed this psychotherapy did well, but one in four will return symptoms and require additional treatment. Approximately one in four people refuse to try this type of cognitive-behavioral therapy or do not complete it - they find it too hard for them.
Medications
About six people in 10 feel better with medication and their symptoms lessen by about half. Medications do help prevent OCD from returning for as long as they are taken, even years later. Unfortunately, about half of those who stop taking the drug return symptoms within a few months afterward. This is less likely when drug treatment is combined with cognitive behavioral therapy.
Which approach is best for me?
Mild OCD
Exposure and response prevention can be done without professional help. This method is effective and has no side effects, but you will feel more anxious for a while. You must be motivated and ready for hard work. Cognitive therapy and drug treatment are equally effective.
Moderate or severe OCD
- Initially, you can choose either CBT (up to 10 hours in contact with a therapist) or medication (within 12 weeks). If you do not get better, you should try both treatments together.
- If you have severe OCD, it is best to use medication and CBT together from the start.
- Taking medication alone will help you if you don't feel able to face the anxiety that Exposure and response prevention will cause, but the chances of OCD coming back are higher - about one in two compared to one in four with psychotherapy treatment. The medicine must be taken for about a year and is obviously not ideal during pregnancy or breastfeeding.