Ocd perfectionism treatment
Perfectionism OCD: Overview, Symptoms and Therapy Options
All types of OCD include obsessions and compulsions. Obsessions are unwanted and intrusive thoughts, feelings, urges and doubts, while compulsions are repetitive physical or mental actions performed in an attempt to relieve distress and anxiety
Perfectionism, also known as Just Right OCD, is one of the most common ways obsessive-compulsive disorder (OCD) is portrayed in movies and on television. A character with OCD is typically oversimplified and shown as constantly arranging items until they’re perfectly aligned, and may be called a “neat freak.” Outside of the media, we’ve also colloquially developed stereotypical phrasing for someone who is extraordinarily clean and organized, dubbing them “so OCD.”
These stereotypes can be harmful and misleading, potentially deterring someone with unhealthy perfectionist tendencies from receiving the help they need.
You may be asking yourself, what does unhealthy perfectionism look like? Where is the line between healthy and unhealthy? When is it considered OCD? Let’s take a closer look.
What is perfectionism?
Having a meticulously organized closet or turning in perfect assignments may seem like an ideal situation — something to strive for. Perfectionism, when healthy, is a personality trait that often leads to a life of success and excellence. In general, it may be tied to goal-oriented behavior and good organizational skills, both of which are perceived as highly desirable traits.
If you are someone who values perfectionism but does not have OCD, your perfectionist tendencies likely add to your overall life experience. You may follow rigid schedules or hold high standards for yourself and others, but you do these things out of choice — not because of anxiety — and they may genuinely increase the pleasure you get from life.
This is one of the key differences between perfectionism and perfectionism OCD. If you have OCD, your perfectionist tendencies likely are a form of compulsions, meaning you take these actions in order to relieve the distress of intrusive thoughts.
Symptoms of perfectionism OCD
Perfectionism OCD can mean you experience unwanted, intrusive thoughts and enact certain rituals to ease your anxiety. Because there are overlaps between healthy perfectionism and its unhealthy counterpart, it may be hard to identify the symptoms. If you think you may have perfectionism OCD, ask yourself if you feel in control of your thoughts and actions. If the answer is no, you likely have OCD.
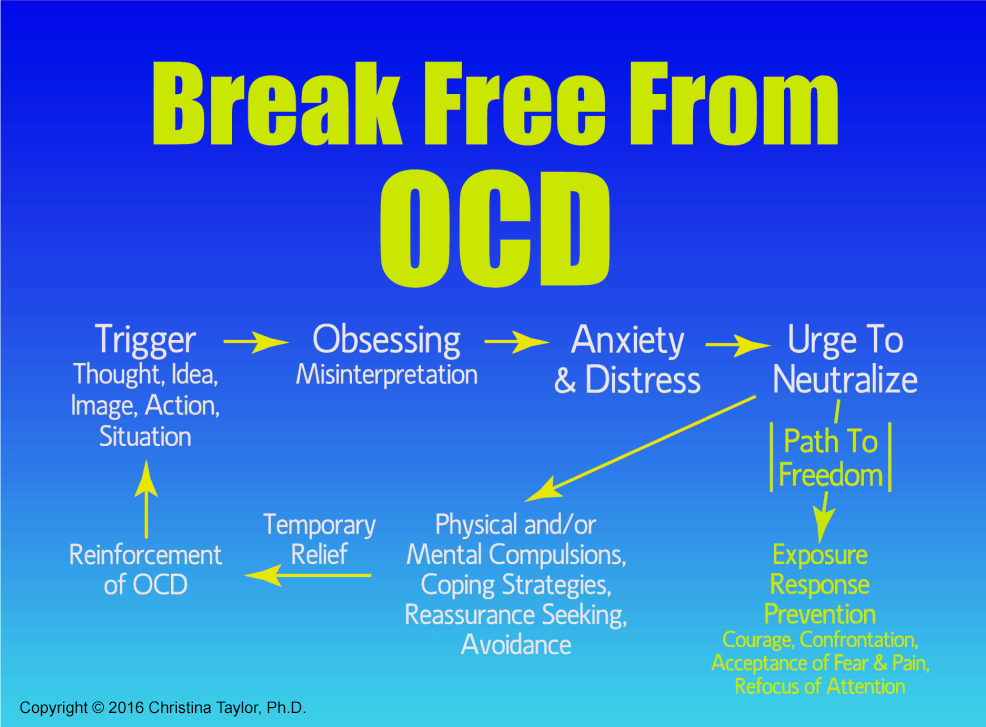
Like other subtypes, perfectionism OCD will follow the obsessive-compulsive cycle. Here are a few examples of what your obsessions may look like:
- excessively worrying about what others think of you and your work/school performance
- an intense fear that you might make a catastrophic mistake
- feeling certain something terrible will happen if you don’t enact your perfectionist tendencies
Your compulsions may look like perfectionist tendencies that, in someone without OCD, would be considered healthy. However, as mentioned before, your tendencies are likely done in an effort to stop your obsessions and the anxiety they cause. This can lead to them feeling out of your control, which may disrupt your normal routine and lead to complications at work or school or in your relationships.
This can lead to them feeling out of your control, which may disrupt your normal routine and lead to complications at work or school or in your relationships.
If you feel like your perfectionist tendencies are causing you more harm than good, treatment options are available to help you regain control of your life.
How is perfectionism OCD treated?
Realizing your perfectionism may be a form of OCD can be scary, but it is also the first step towards living a life free of your obsessive thoughts and unhealthy tendencies.
OCD is a highly treatable disorder, and the most effective form of treatment involves exposure and response prevention (ERP) therapy, a form of cognitive behavioral therapy (CBT). ERP is the gold-standard option for OCD treatment, and it’s easy to understand why. It works by exposing you to various things that trigger your obsessions, and — in a safe and controlled environment — working through your fears, with the help of a trained therapist, to learn how to control the urge to act on them.
If you’re ready to start ERP, you can schedule a free call with the NOCD clinical team to be matched with a therapist. All NOCD therapists specialize in the treatment of OCD and receive ERP-specific training in order to offer you the best help for your symptoms.
With the right therapist, ERP can help you learn how to cope with your intrusive thoughts. Over time, you’ll gain more control over your thoughts and actions, allowing you to experience life free of your fears and compulsions. You can also join our Perfectionism OCD community and get 24/7 access to personalized self-management tools built by people who have been through OCD and successfully recovered.
Strategies for Coping with the Need to be Perfect
By Andrew M. Jacobs, Psy.D. & Martin M. Antony, Ph.D., ABPP
While perfectionism is a trait found in various forms both in the general public and across anxiety disorders (Antony, Purdon, Huta, & Swinson, 1998), it often holds a particularly focal place in the experiences of individuals with obsessive-compulsive disorder (OCD). Theory and research regarding the role of perfectionism in OCD suggest that at its core, perfectionistic thinking and behavior in OCD stem from an ongoing effort to avoid the discomfort that results from a sense of uncertainty, danger, judgment from others, or imprecision. Although it is likely that all individuals are motivated to some degree by the avoidance of these negative outcomes, several theorists have suggested that in OCD, the desire to avoid discomfort overtakes the desire to perform well or reach a specific goal (Frost, Novara, & Rhéaume, 2002). Whereas the desire to perform well might be seen as more characteristic of “healthy” perfectionism, perfectionism associated with an extreme desire to avoid discomfort can lead to the obsessive-compulsive traps all too familiar to those with OCD. Excessive perfectionism involves holding standards that are impossible to attain and experiencing negative outcomes (for example, anxiety or depression) when one’s impossibly high standards are not met.
Theory and research regarding the role of perfectionism in OCD suggest that at its core, perfectionistic thinking and behavior in OCD stem from an ongoing effort to avoid the discomfort that results from a sense of uncertainty, danger, judgment from others, or imprecision. Although it is likely that all individuals are motivated to some degree by the avoidance of these negative outcomes, several theorists have suggested that in OCD, the desire to avoid discomfort overtakes the desire to perform well or reach a specific goal (Frost, Novara, & Rhéaume, 2002). Whereas the desire to perform well might be seen as more characteristic of “healthy” perfectionism, perfectionism associated with an extreme desire to avoid discomfort can lead to the obsessive-compulsive traps all too familiar to those with OCD. Excessive perfectionism involves holding standards that are impossible to attain and experiencing negative outcomes (for example, anxiety or depression) when one’s impossibly high standards are not met.
Among the available ways to help individuals with OCD, a form of treatment called cognitive-behavioral therapy (CBT) has been consistently demonstrated as the most effective way to reduce symptoms and improve quality of life (Antony, Purdon, & Summerfeldt, 2007). In essence, the core ways CBT is used to help individuals with OCD is by helping them to identify and examine thinking styles about obsessions and compulsions that can lead to increased anxiety and worsening symptoms. Additionally, a fundamental part of CBT for OCD involves directly facing situations and triggers that are likely to cause symptoms, staying with them until anxiety has decreased, and refraining from engaging in compulsive rituals. The good news is that these strategies can also be used to specifically target perfectionistic tendencies within OCD (Antony & Swinson, 2009). This article provides suggestions for individuals with OCD for dealing effectively with perfectionism.
Perfectionistic Thinking
One of the foundations for perfectionistic tendencies in OCD is the way in which we view ourselves, the world, and our experiences. As we move through our lives, we form assumptions or “rules of thumb” that help us to make sense of our experiences and increase the chances that we will respond to situations appropriately. Quite often, our assumptions and beliefs are helpful and lead us to act in a healthy fashion – for example, if we genuinely believe that good intentions are what matters, we may be likely to interact with others in a relatively positive and cooperative fashion. Additionally, we might have more flexible standards for ourselves and others.
As we move through our lives, we form assumptions or “rules of thumb” that help us to make sense of our experiences and increase the chances that we will respond to situations appropriately. Quite often, our assumptions and beliefs are helpful and lead us to act in a healthy fashion – for example, if we genuinely believe that good intentions are what matters, we may be likely to interact with others in a relatively positive and cooperative fashion. Additionally, we might have more flexible standards for ourselves and others.
Our beliefs lead us to automatically think in particular ways, depending on the situation we are in. In CBT, these snap judgments are often called “automatic thoughts.” Automatic thoughts are informed by our general “rules of thumb” and provide us with the means to interpret what is going on in our lives. For example, the person described in the earlier example who believes that good intentions are all that matters might notice an ink smudge on a card that he or she just wrote and think “that’s not a big deal…at least my message can still be read. ” In turn, the individual’s subsequent action might be to simply send the card without trying to fix the smudge or replace the card with a new one.
” In turn, the individual’s subsequent action might be to simply send the card without trying to fix the smudge or replace the card with a new one.
However, our assumptions can often take forms that are less helpful. To illustrate, imagine the individual who has the assumption that “it’s better to do nothing at all than to do something imperfectly,” rather than “intentions are what’s important.” The same ink smudge might now lead to thoughts such as “my friend will think I don’t care about him,” “why did I even bother” or “this card is ruined.” Our action might then be to rewrite the card until no ink smudges are present, or even to give up and send our friend nothing. As we then manage to prevent mistakes through this extreme attention to detail or avoidance of the situation altogether, we are able to escape the anxiety that would otherwise be present. Avoiding the anxiety that is triggered by making mistakes helps to keep the perfectionism alive.
Fortunately, there are several tools we can use to work with and challenge perfectionistic thinking patterns once you notice them. Below are a few ideas to begin thinking outside the “perfectionist” box:
Below are a few ideas to begin thinking outside the “perfectionist” box:
- Test your perfectionistic predictions. For example, if you assume that a typo in an e-mail to your boss might lead to ridicule or judgment, identify a timeframe when this judgment would likely come up (for example, by your next staff meeting), and then deliberately make an error in your next e-mail. Did the prediction come true? If it did, were you able to cope with the situation?
- Put your perfection into perspective. While you may find yourself thinking that “everything” must be perfect, this may not be the case. Try to think of areas where you are actually quite comfortable with imperfection. Once you’ve come up with a few ideas, ask yourself what makes these things different. Is it possible that a similar level of imperfection would be okay in the “problem areas” of your life?
- Define ‘perfect.’ Have you stopped to think what ‘perfect’ means to you? Is ‘perfect’ even a possibility? Very often, recognizing that ‘perfect’ is an exceptionally hard concept to pin down can help us understand why it’s such a challenge to strive for it.

- Try a different point of view. What would you say to a friend who was as exasperatedly aiming for “perfect” as you are? Would you think less of your friend if he or she did something imperfectly? What about your children? Not surprisingly, we often hold remarkably more rigid standards for ourselves than for others. Recognizing this tendency and putting ourselves in another’s shoes can be a very useful way to counter perfectionistic thinking.
- Do some investigating. Sometimes we might be unsure whether our standards are too perfectionistic. Do most people use spell check on every e-mail they send? Do other people need to make sure the house is spotless before they leave for the day? Think of a few people whose judgment you trust and ask whether their standards are at the same level as yours.
Facing Imperfection Directly
While aiming for perfection may cause a great deal of difficulty in the moment, it can also make it even harder to break the habit in the future. Every time we successfully make something “perfect enough” or correct a mistake, we lower the anxiety or discomfort we would have otherwise felt. This feels like quite a relief in the short term, but in the long run that feeling of relief strengthens our urge to “perfectionize” in the future. In addition, by preemptively aiming for perfection right away, we miss our chance to learn whether our need for perfection is truly warranted. In addition to the thinking patterns discussed above, this avoidance of imperfection (and the discomfort that comes with it) is another way the patterns of perfectionism are ultimately laid in place.
Every time we successfully make something “perfect enough” or correct a mistake, we lower the anxiety or discomfort we would have otherwise felt. This feels like quite a relief in the short term, but in the long run that feeling of relief strengthens our urge to “perfectionize” in the future. In addition, by preemptively aiming for perfection right away, we miss our chance to learn whether our need for perfection is truly warranted. In addition to the thinking patterns discussed above, this avoidance of imperfection (and the discomfort that comes with it) is another way the patterns of perfectionism are ultimately laid in place.
One of the most effective ways of coping with obsessive-compulsive symptoms – including perfectionism – is called exposure and response prevention. To use response prevention, a person would deliberately stop him or herself from performing rituals or other activities that he or she would normally do to work toward perfection. If you think this sounds unpleasant, you’re right – when perfectionists first stop their perfectionistic behavior, they typically feel an increase in anxiety, at first. The key to making this work is recognizing that over time, the anxiety decreases, despite the fact that something has been done imperfectly. As the person gains more and more experience with letting things remain imperfect and learns that there are no serious consequences, future encounters with imperfection become easier and easier.
The key to making this work is recognizing that over time, the anxiety decreases, despite the fact that something has been done imperfectly. As the person gains more and more experience with letting things remain imperfect and learns that there are no serious consequences, future encounters with imperfection become easier and easier.
The other component, exposure, involves deliberately doing something imperfectly and then resisting the urge to fix it. This strategy allows us to tolerate imperfections above and beyond those that occur on their own, and increases our ability to comfortably go without achieving perfection. A good idea is to start with imperfections that are not too difficult to tolerate, and then to gradually increase the difficulty until you can face some of the more challenging imperfections you’ve been avoiding or trying to prevent.
If you’d like to try exposure and response prevention, it is important to keep a number of factors in mind:
- Make sure your exposures are planned and predictable.
 As you purposely confront imperfection, it is important to plan in advance what you will be doing and when you will be doing it. It is also useful to anticipate possible outcomes. As your skill increases, you can try less predictable exercises.
As you purposely confront imperfection, it is important to plan in advance what you will be doing and when you will be doing it. It is also useful to anticipate possible outcomes. As your skill increases, you can try less predictable exercises. - Stay in the situation until your discomfort has decreased or until you learn that your feared consequences don’t occur. It is useful to “let the imperfection be” until it is no longer bothering you. If you correct the imperfection too soon, you may reinforce your initial fear and avoidance.
- Practice exposures frequently. As with any skill, you will find your exposures become easier and easier the more you practice. Practicing several times per week is better than practicing less frequently.
- Don’t take an easy way out. Be careful to notice whether you are doing anything to quickly lower your anxiety, such as trying to distract yourself, asking for reassurance from others, or checking to be sure your imperfection hasn’t caused problems.

- Expect to feel uncomfortable. While it may sound counterintuitive, the more discomfort you are able to tolerate during exposure, the more imperfection you will eventually be able to face in your day-to-day life.
Virtually any area where you find yourself excessively striving for perfection is fair game for an exposure. Below are some ideas for exposure to help you get started:
- Wear mismatched socks
- Turn random books upside down on your shelf
- Place a stain or wrinkle in your clothing
- Leave an area of your floor or table uncleaned
- Deliberately include typos in an e-mail or letter
- Mispronounce words
- Purchase clothing articles discounted for manufacturing imperfections (and wear them!)
- Put your books, CDs, or DVDs in a random order
- Hang pictures slightly crooked
Other Resources
The strategies in this article, with practice, can help you make a significant difference in the way perfectionism is influencing your life. Cognitive and behavioral techniques such as those described here have been repeatedly demonstrated to be the most effective ways of combating OCD and perfectionism. To read about identifying and treating perfectionism in greater depth, we recommend the self-help book When Perfect Isn’t Good Enough: Strategies for Coping with Perfectionism by Drs. Martin M. Antony and Richard P. Swinson (2009).
Cognitive and behavioral techniques such as those described here have been repeatedly demonstrated to be the most effective ways of combating OCD and perfectionism. To read about identifying and treating perfectionism in greater depth, we recommend the self-help book When Perfect Isn’t Good Enough: Strategies for Coping with Perfectionism by Drs. Martin M. Antony and Richard P. Swinson (2009).
While many people are able to make tremendous gains with self-help treatment, it is also very common to find that perfectionism or other OCD symptoms are so firmly ingrained or overwhelming that an individual needs outside support and guidance from a professional. If you feel that you may benefit from working with a person trained to use the approaches discussed in this article, we suggest looking for a psychologist, psychiatrist, social worker, or other mental health professional who is trained in cognitive behavioral therapy. To find such therapists, you might contact your family doctor or a local department of psychology or psychiatry at a university near you. Additionally, the following websites contain names of therapists near you who may be able to help:
Additionally, the following websites contain names of therapists near you who may be able to help:
- Academy of Cognitive Therapy (http://www.academyofct.org)
- Anxiety and Depression Association of America (https://adaa.org/)
- Association for Behavioral and Cognitive Therapies (http://www.abct.org)
- Intnernational OCD Foundation (https://iocdf.org/)
References Antony, M.M., Purdon, C., & Summerfeldt, L.J. (Eds.) (2007). Psychological treatment of OCD: Fundamentals and beyond. Washington, DC: American Psychological Association. Antony, M. M., Purdon, C. L., Huta, V., & Swinson, R. P. (1998). Dimensions of perfectionism across the anxiety disorders. Behaviour Research and Therapy, 36, 1143-1154. Antony, M. M., & Swinson, R. P. (2009). When perfect isn’t good enough: Strategies for coping with perfectionism (2nd edition). Oakland, CA: New Harbinger. Frost, R. O., Novara, C., & Rhéaume, J. (2002). Perfectionism in obsessive compulsive disorder. In R. O. Frost & G. Steketee (Eds.), Cognitive approaches to obsessions and compulsions: Theory, assessment, and treatment (pp. 91-105). Amsterdam: Elsevier.
(2002). Perfectionism in obsessive compulsive disorder. In R. O. Frost & G. Steketee (Eds.), Cognitive approaches to obsessions and compulsions: Theory, assessment, and treatment (pp. 91-105). Amsterdam: Elsevier.
For more information on this topic, check out When Perfect Isn’t Good Enough: Strategies for Coping with Perfectionism, Second Edition, by Martin M. Antony, Ph.D., and Richard P. Swinson. Dr. Jacobs is a clinical psychologist in the Anxiety Treatment and Research Centre at St. Joseph’s Healthcare in Hamilton, Ontario, Canada. His professional interests focus on interpersonal and motivational factors in cognitive behavioral therapy for anxiety and mood disorders, cultural minority considerations in psychotherapy, and the dissemination of empirically-based psychological knowledge to the general public. Dr. Antony is a clinical psychologist and professor of psychology at Ryerson University in Toronto, Canada. He has authored more than 25 books on topics related to anxiety disorders, perfectionism, and cognitive behavioral therapy. Dr. Jacobs works at the Anxiety Treatment and Research Center in Hamilton, ON, Canada.
Dr. Jacobs works at the Anxiety Treatment and Research Center in Hamilton, ON, Canada.
Back to article index »
Share this article:
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety. nine0003
You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety. nine0003
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions. nine0003
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.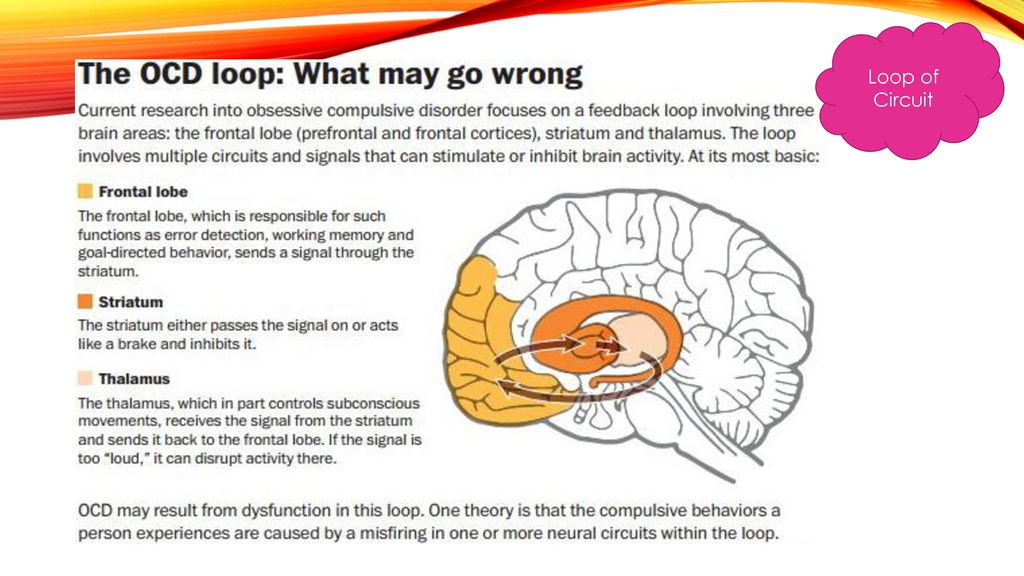 nine0003
nine0003
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions nine0007 A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community. nine0003
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result.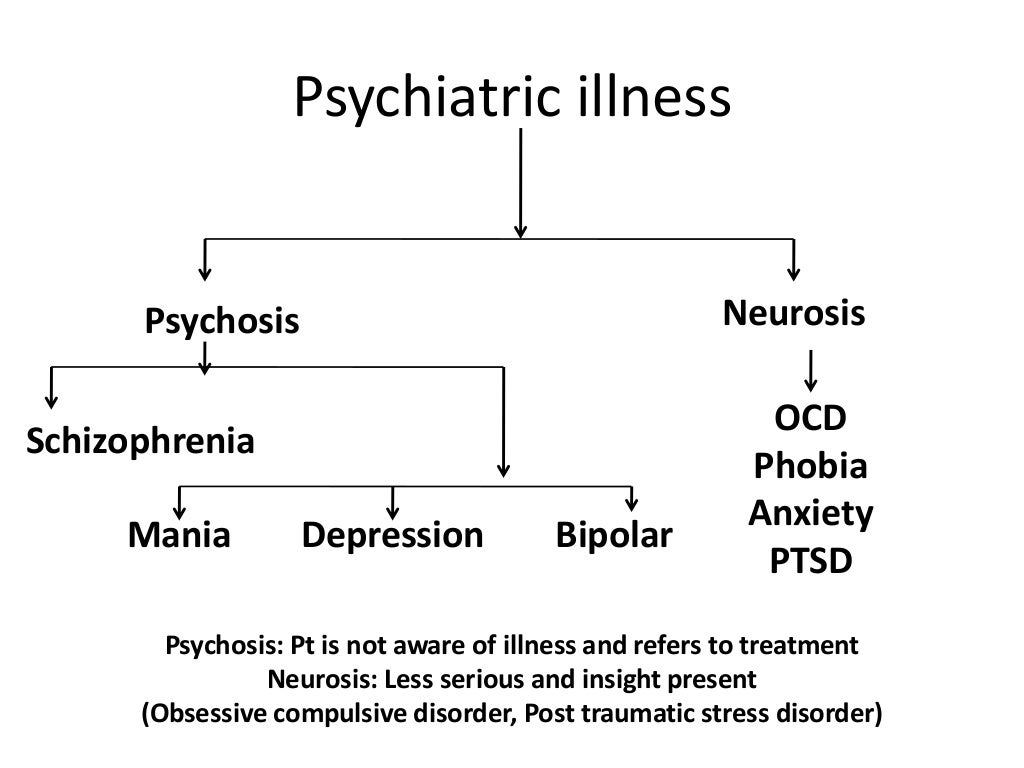 A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events. nine0003
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy. nine0007 Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Jacobson progressive muscle relaxation.
 nine0007 Traditional and modern gymnastic systems, relaxation techniques.
nine0007 Traditional and modern gymnastic systems, relaxation techniques.
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed. nine0003
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future. nine0003
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased. nine0003
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
symptoms, how to get rid of and treat
Olya Selivanova
struggling with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die. ” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die. nine0003
” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die. nine0003
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, everything had come to naught, and in my teens I decided that these were just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now. nine0003
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions. nine0003
What is obsessive-compulsive disorder - Mayo Clinic
Intrusive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up. nine0003
Compulsions are difficult to resist: the anxiety will grow until the person gives up. nine0003
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch the doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person’s condition does not interfere with himself or others, then everything is in order; if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life.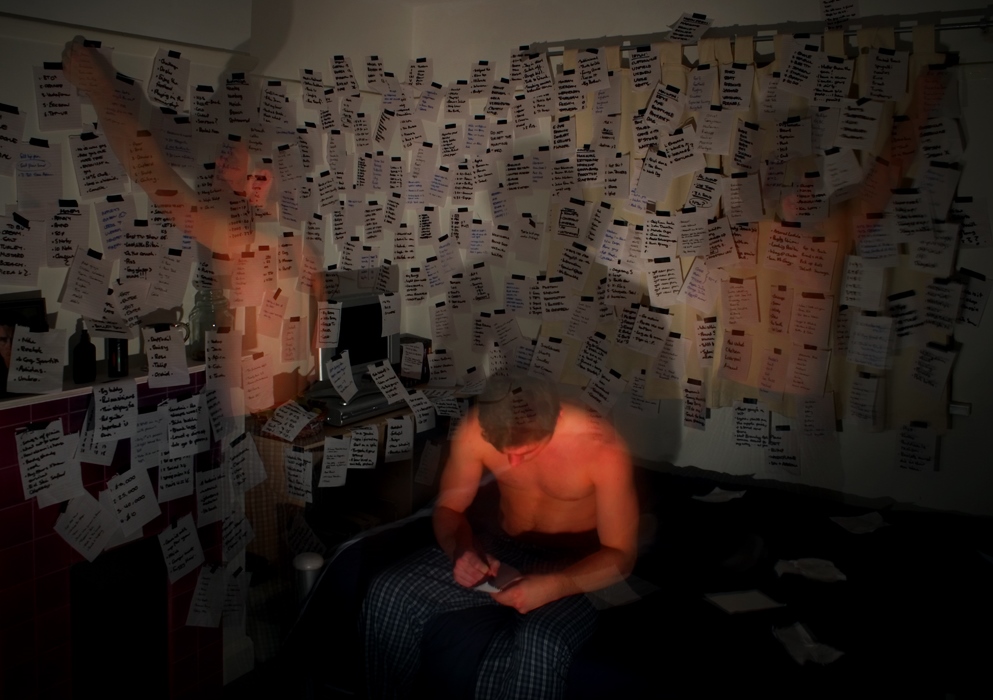 If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD. nine0003
If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD. nine0003
At the same time, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasant. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment, remission can be achieved: for a long time to get rid of obsessive thoughts and compulsive actions or reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other medications: tranquilizers, antipsychotics, or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive Behavioral Therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16.2003 No. 438 "On Psychotherapeutic Care"
OCD in Russia is treated by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn.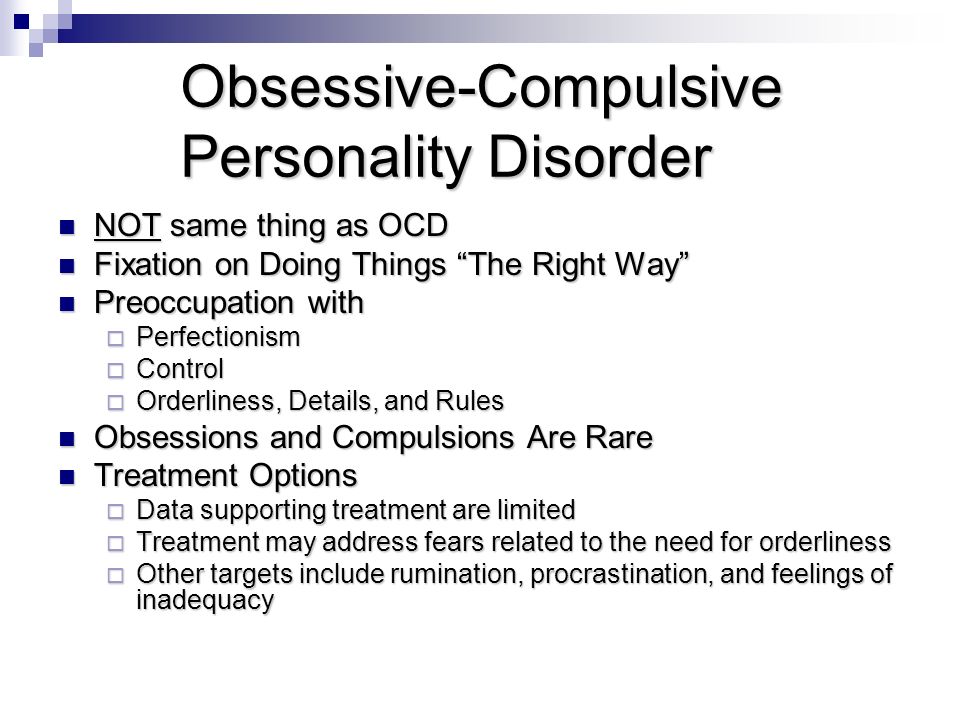 I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away. nine0003
I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away. nine0003
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist. nine0003
My young man, seeing all this, insisted that we try to see a psychologist. nine0003
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help. nine0003
The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help. nine0003
How a visit to a psycho-neurological dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons. nine0003
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalization My condition worsened, I tried to ignore obsessive thoughts.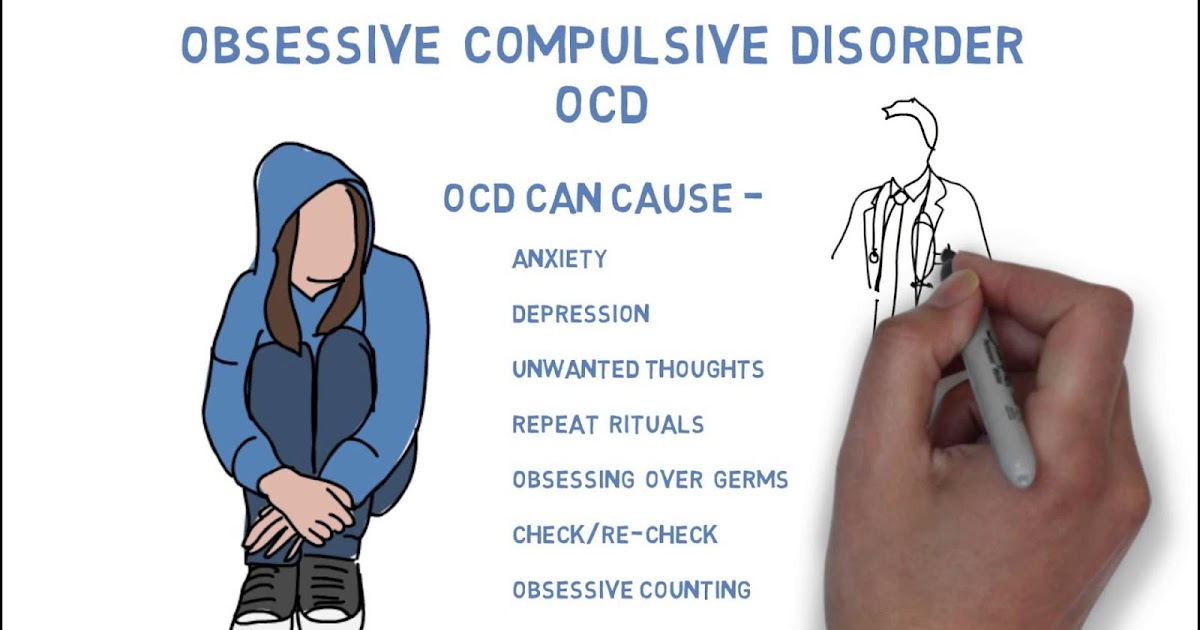 But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared. nine0003
But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared. nine0003
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine at the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital. nine0003
These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital. nine0003
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.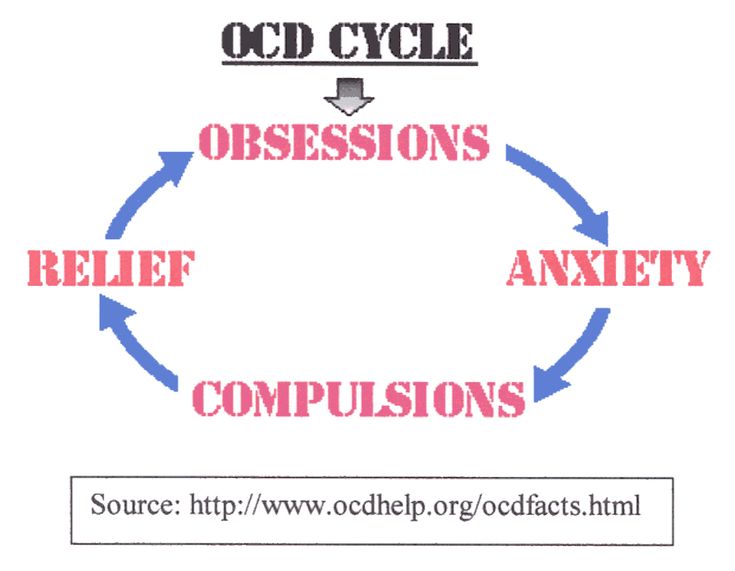 nine0003 During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man didn't let me stop the treatment
nine0003 During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man didn't let me stop the treatment
Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription. nine0003
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them.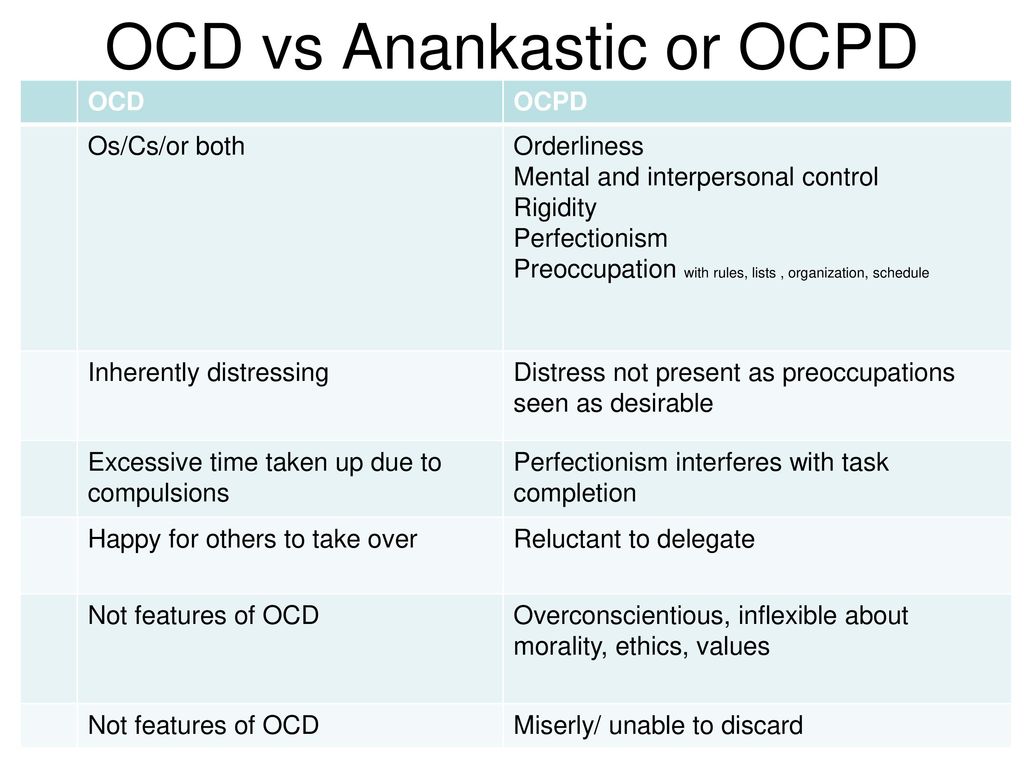 Usually the registrar complied with my request.
Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 R |
| Antipsychotics | 419 R |
| Tranquilizers | 104 R |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused
When I wanted to buy one more to have a supply, the pharmacist refused Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the local psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts. nine0003
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression. nine0003
We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression. nine0003
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive actions to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person. nine0003
nine0003
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them. nine0003
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully. nine0003 I filled out the diary for a week, and then the psychotherapist and I analyzed the notes
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
 Before treatment, there was no point in monitoring my mood: it always turned out to be bad or indifferent On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring my mood: it always turned out to be bad or indifferent On antidepressants, I began to make entries in a diary every day and could track what affects my mood I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better. nine0003
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me.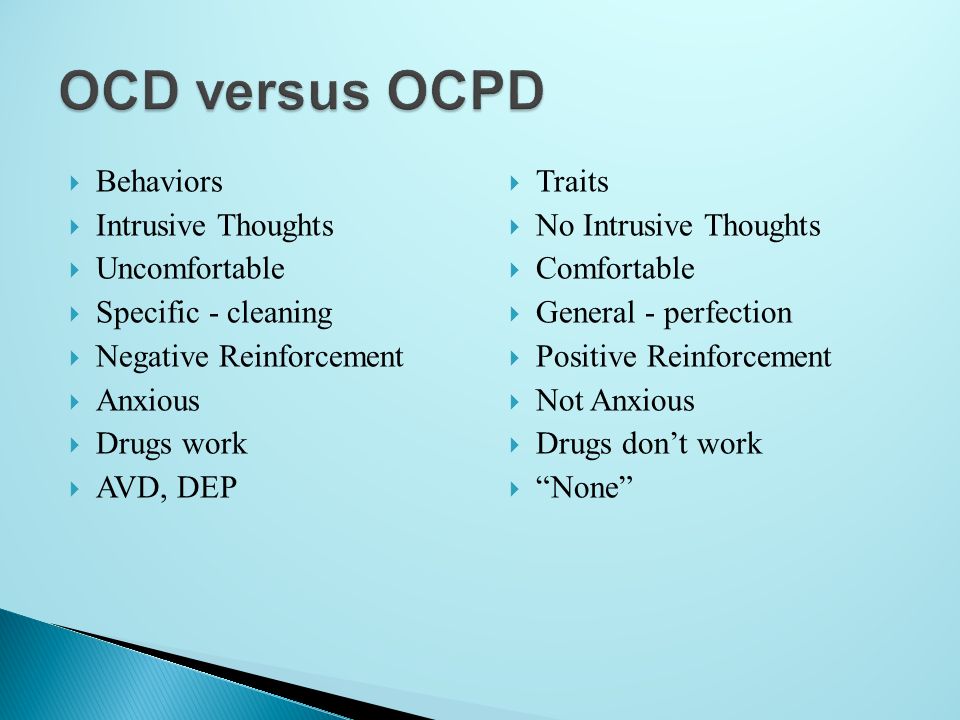 I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 P |
| Transport | 780 P |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge. I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.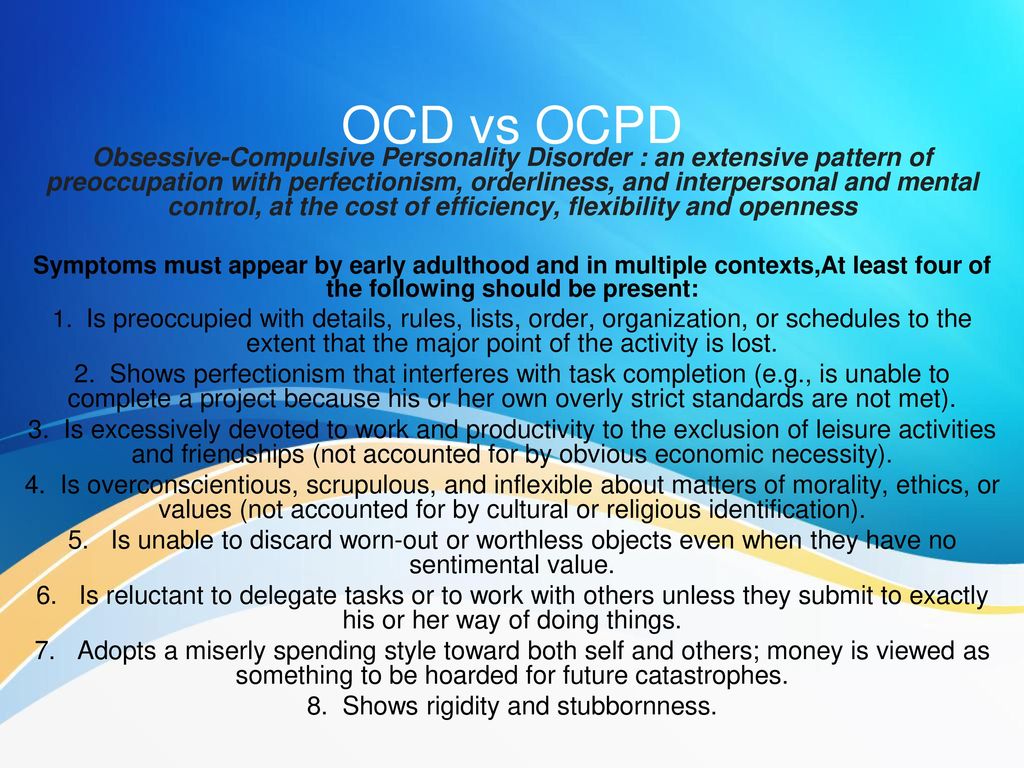 nine0003
nine0003
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis. nine0003
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenses | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 R |
| Antipsychotics | 419 R |
| Tranquilizers | 104 R |
| Transport during hospitalization | 1380 R |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.