Obsessive compulsive personality disorder example
Obsessive-Compulsive Personality Disorder (OCPD) - HelpGuide.org
personality disorders
Know someone who fixates on small details and sets unrealistic standards for themselves and others? Or maybe that person is you? Here’s how to recognize and manage OCPD.
What is obsessive-compulsive personality disorder (OCPD)?
It's not unusual for someone to be diligent, orderly, or stubborn. In some cases, those personality traits can even come in handy. However, when those traits are taken to an extreme, they can reduce the quality of a person's physical, emotional, and social well-being.
People with obsessive-compulsive personality disorder (OCPD) have a fixation with perfection, control, and orderliness. Their preoccupation is severe enough to lead to impairment. Picture a student who is so focused on small details that they fail to complete an assignment. Or imagine someone whose moral code is so inflexible that they have trouble seeing things from another person's perspective.
A person with OCPD may not be aware of their condition or see a need for change. In fact, they may believe that other people are the ones who should change.
People with OCPD have a tendency to impose their high standards on others. For example, a husband with OCPD might refuse to let his wife help plant a garden unless the wife agrees to follow a strict methodology. If his partner deviates at all from the rules, the husband can become overly critical.
Unsurprisingly, this rigid approach to life can lead to difficulty maintaining relationships or adapting to new circumstances. Loneliness and depression may develop as relationships deteriorate. The person with OCPD may avoid or quit activities they don't immediately excel in, limiting their potential. In addition, an intense focus on perfectionism can lead to anxiety, eating disorders, and other physical and mental problems.
Do you think you recognize these symptoms in yourself or someone you love? Learn more about the specific signs of OCPD as well as self-help tips that can help manage the disorder.
Causes and symptoms of OCPD
OCPD is one of the most common personality disorders. Research indicates that somewhere between 3 to 8 percent of the population has OCPD, and it's most common in older people. This personality disorder involves a persistent pattern of behavior that often starts when the person is a teenager or young adult.
Experts haven't identified one exact cause of OCPD. However, research suggests that a person's upbringing may play a role. For example, being raised in an environment that has strict rules and harsh punishments may lead a person to obsess over doing things “the right way.” OCPD may also have a genetic component, meaning that it might be inherited.
Signs and symptoms of OCPD include:
- Perfectionism that gets in the way of finishing tasks.
- Fixation with using lists, rules, and schedules to maintain order.
- Unwillingness to delegate work to someone who may take a different approach to the task.
- Devotion to work that leads to neglect of relationships.

- Hoarding money for future disasters.
- Overly conscientious of ethics, morality, and values.
- Inability to get rid of worthless items, such as worn-out shoes, despite the lack of sentimental value.
- Overly stubborn and rigid disposition.
Diagnosis
For an OCPD diagnosis, a person must show at least four of the eight signs listed above. The symptoms must be part of a long-term pattern that was formed by early adulthood.
The diagnosis process will likely involve screening questionnaires, which allow the person to self-report on their own behavior. The screening is followed by an interview. In addition to self-reported details, information gathered from friends, family, and peers can also help a mental health expert make an accurate diagnosis.
A mental health expert will need to rule out other possible explanations for the behavior. For example, obsessive-compulsive disorder (OCD) is a separate condition that can also involve a preoccupation with orderliness and hoarding.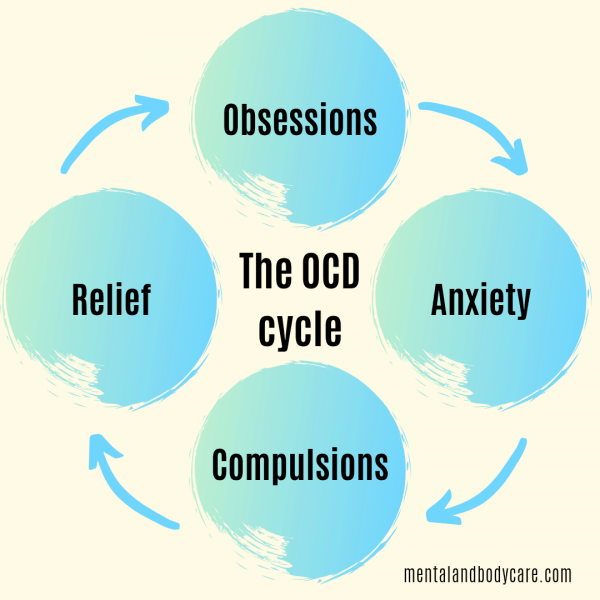
It can also be tricky to distinguish OCPD behavior from “conventional” behavior. Some questions to consider:
- Is the person overly devoted to work? Or are they just trying to earn higher pay for financial stability?
- Is the person a perfectionist? Or are they just detail-oriented and willing to cut corners when necessary?
- Is the person obsessed with control? Or do they just want a practical amount of orderliness in their home?
- Is the person having a hard time getting rid of items due to sentimental value?
If you suspect you have OCPD, you may feel hesitant to seek a diagnosis. Perhaps you feel as though your approach to life is more helpful than harmful. In many cases, people with OCPD who seek a diagnosis do so at the request of a loved one. So, if your approach to life seems to be damaging your relationships, a formal diagnosis may offer insight and a path forward.
Affordable Online Therapy for Personality Disorders
Get professional help from BetterHelp's network of licensed therapists.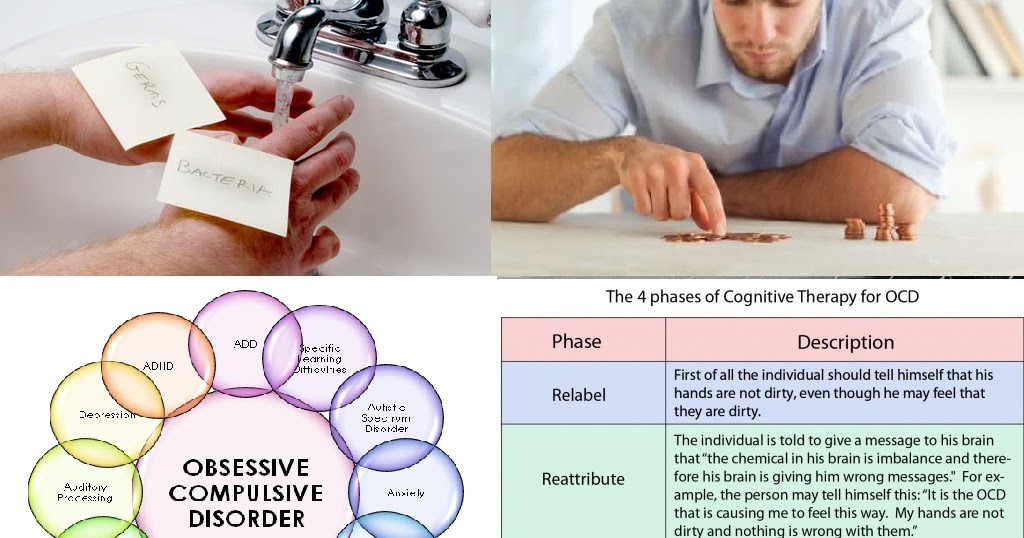
FIND A THERAPIST NOW
HelpGuide is reader supported. We may receive a commission if you sign up for BetterHelp through the provided link. Learn more.
Co-occurring disorders
People with OCPD often struggle with other physical and mental health conditions. When multiple disorders are present, it's important to address all of the issues simultaneously, as they may affect one another. Some of these co-occurring disorders include:
Eating disorders. Perfectionism can motivate people with OCPD to reach for unrealistic standards, even at the cost of their own health. That degree of perfectionism is also found in people with eating disorders, such as anorexia and bulimia nervosa, so these conditions may co-occur with OCPD.
[Read: Eating Disorder Treatment and Recovery]
Mood disorders. Research shows that OCPD is associated with mood disorders, including depression. Workplace burnout, difficulty with social interactions, and failure to live up to their own high expectations may contribute to depressive symptoms.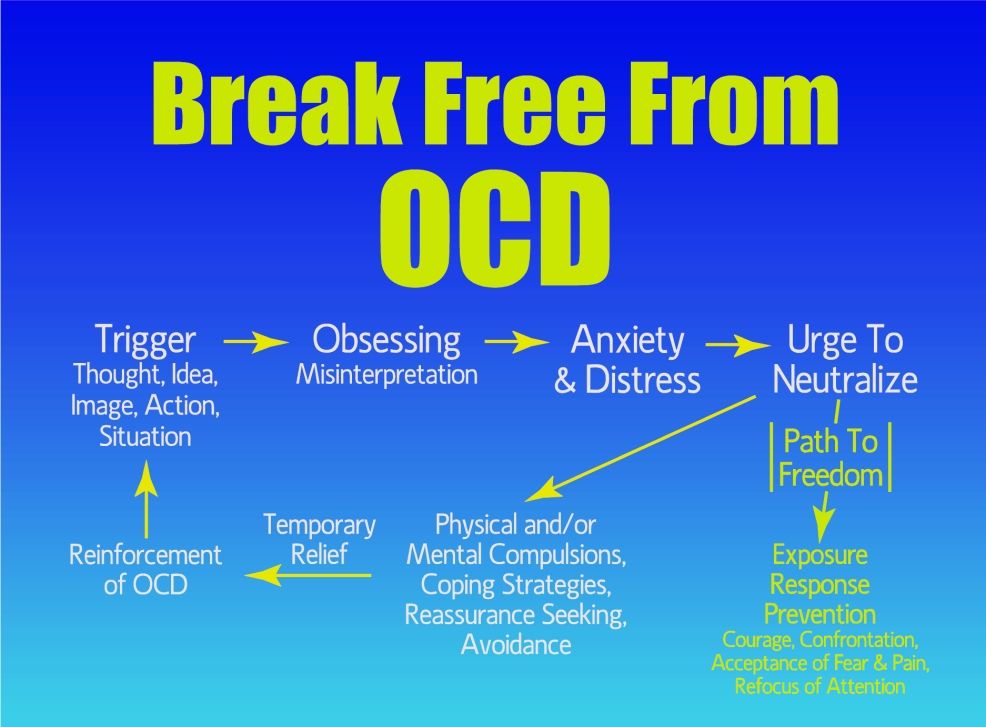 OCPD traits have also been linked to suicidal ideation.
OCPD traits have also been linked to suicidal ideation.
Physical problems. One study found that OCPD traits are linked to cardiovascular health conditions, such as hypertension. Other research seems to indicate an association between OCPD and stroke and arthritis.
Other personality disorders. A person can struggle with overlapping personality disorders. People with OCPD may also be diagnosed with dependent, histrionic, borderline, avoidant, or narcissistic personality disorders.
Anxiety disorders. As people with OCPD are striving to maintain order and achieve perfection, they may also be plagued by anxiety. Anxiety disorders, such as generalized anxiety disorder and panic disorder, may co-occur with OCPD. OCD is another anxiety disorder that may co-occur with OCPD, and the two conditions are commonly mistaken for each other.
OCPD vs. OCD
Despite similarities in their names, OCPD and obsessive-compulsive disorder (OCD) have key differences.
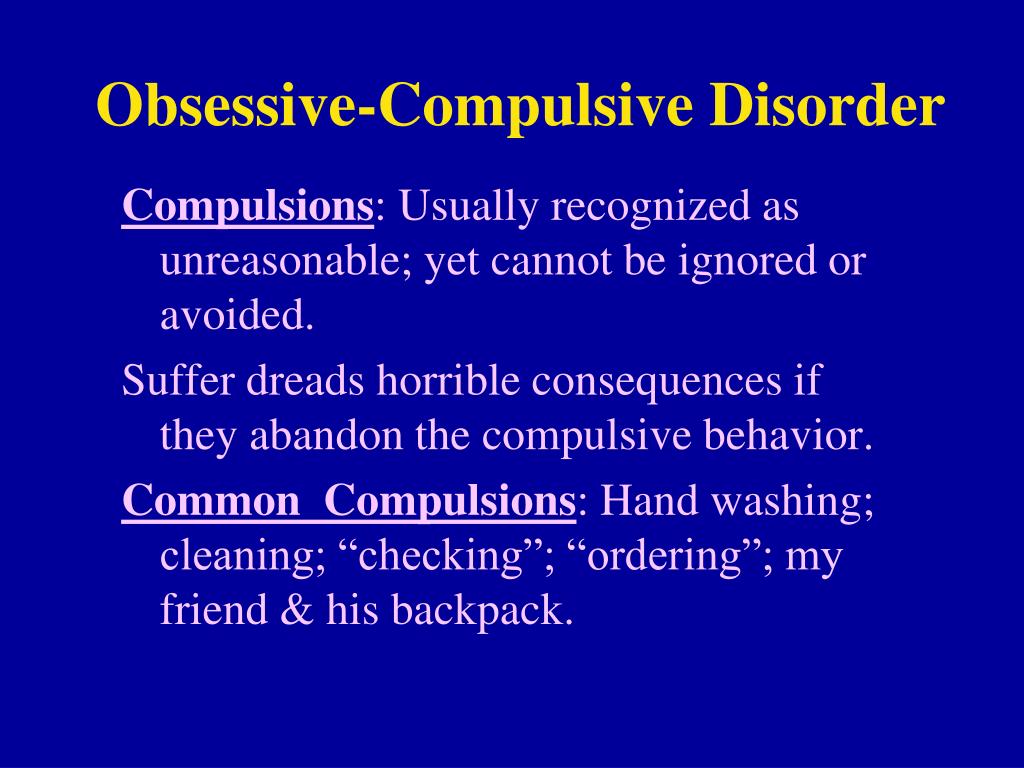
People with OCD struggle with unwanted, anxious thoughts (obsessions) and feel compelled to perform ritualized actions to reduce their anxiety. For example, a fear of germs may lead a person with OCD to continually wash their hands. The person is often aware that their fears and urges are irrational.
[Read: Obsessive-Compulsive Disorder (OCD)]
People with OCPD are less likely to recognize their disorder than people with OCD. They typically aren’t driven by obsessive thoughts or specific repetitive actions. Instead, they have a more general desire for order and perfection, which they see as part of their own fixed values. Research also shows that people with OCPD are less impulsive and more willing to delay rewards than people OCD.
| OCD traits vs. OCPD traits | |
| OCD traits | OCPD traits |
You keep wiping down the kitchen counter because you have anxious, intrusive thoughts about food contamination. You’re aware this is a time-consuming activity, and the irrationality of it causes you distress. You’re aware this is a time-consuming activity, and the irrationality of it causes you distress. | You frequently clean the kitchen counter because you want it to look spotless. The activity is inconvenient for everyone else in your family, but you believe the kitchen needs to remain neat and orderly. |
| You keep checking and rearranging luggage items, trying to ease the fear of something being damaged, lost, or left behind. | You create a detailed list of what you want to pack and in which suitcase. You become so fixated on writing the list you no longer have time to pack. |
| You keep asking if you’ve insulted someone. You're experiencing intrusive thoughts about accidentally offending other people. | You take a long time to speak so your words avoid misinterpretation. In your mind, everyone should be this careful when speaking. |
OCPD is more common than OCD, but about 15 to 28 percent of people with OCD may also have OCPD.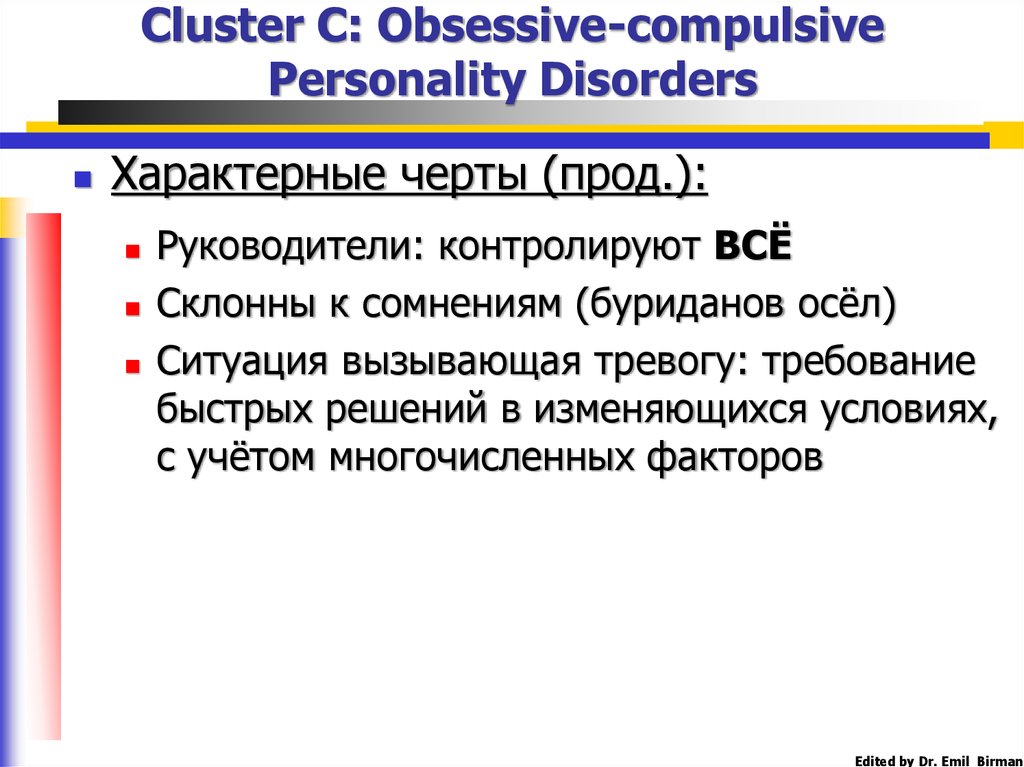 Someone with both disorders may experience more severe symptoms, as well as higher distress. Due to the stubborn nature of people with OCPD, they may be less willing to accept treatment. However, when they do accept treatment, their preoccupation with perfectionism may be beneficial. For example, they may be more thorough in following their self-help practices.
Someone with both disorders may experience more severe symptoms, as well as higher distress. Due to the stubborn nature of people with OCPD, they may be less willing to accept treatment. However, when they do accept treatment, their preoccupation with perfectionism may be beneficial. For example, they may be more thorough in following their self-help practices.
Self-help for OCPD
If you or a loved one have OCPD, there are many steps you can take to limit some of the more negative aspects of the disorder. Many of these strategies involve easing the strong desire to control every circumstance and perfect every task.
OCPD self-help tip 1: Manage stress
People with OCPD often feel they have a lot of tasks on their schedule and believe those tasks need to be done well. On top of that, crippling fear of failure can lead to procrastination. This can make for stressful days and outbursts of frustration.
Relaxation techniques can help you manage stress and improve your mood. They might also help you reflect on and accept matters that are beyond your control. Here are a few practices that may help:
They might also help you reflect on and accept matters that are beyond your control. Here are a few practices that may help:
Experiment with mindful breathing. This simple form of meditation involves focusing on your inhales and exhales. Long, deep breaths can decrease your stress response and keep you grounded in the present moment.
[Listen: Mindful Breathing Meditation]
Exercise regularly. Physical activity releases endorphins, hormones that promote a feeling of well-being. Activities such as yoga and tai chi can be especially helpful, as they combine physical activity with mindful breathing.
Get enough rest. Even if you think of yourself as a workaholic, it's important to get enough sleep every night. Lack of sleep not only raises your stress levels, it can also hinder your work performance.
Eat healthy meals. Poor eating habits can leave your body more susceptible to stress. Think of healthy meals as a high priority as you plan your daily schedule.
ADVERTISEMENT
Helping someone with OCPD manage stress
If you're living with someone with OCPD and want to encourage them to try the practices listed above, remind them that everyone can benefit from stress management. Frame it as a team activity that can improve both your lives, rather than an activity that is only meant to “fix” them. Take the time to meditate with them or join them in exercising and eating healthy.
Tip 2: Practice self-compassion
If you have OCPD, there's no doubt that you have high expectations for yourself. When those expectations aren't met, you might take your frustrations out on yourself as well as friends and family members. You might also have a tendency to overinflate the flaws you see in yourself and others.
Self-compassion starts with accepting that you (and those around you) have limits. Despite your best efforts, you'll make mistakes and overlook things. Don't think of those shortcomings as evidence that you're a failure. Look at them as opportunities to grow and remember to forgive yourself rather than allow self-hatred to build.
Look at them as opportunities to grow and remember to forgive yourself rather than allow self-hatred to build.
Adjusting self-talk
Another step toward self-compassion involves paying attention to your self-talk. When you engage in negative self-talk, you use disparaging inner monologue such as, “I'm not good enough” or “I'm such an idiot.” These kinds of thoughts can lead you to depression and warp your perception of reality.
Try to notice when you're using negative self-talk and challenge those negative statements with neutral or positive self-talk.
| Self-talk examples | |
| Negative self-talk | Neutral or positive self-talk |
| “I'm stupid for forgetting to do my taxes.” | “I forgot to do my taxes because I was busy with other things. This mistake doesn't make me a bad person.” |
“My friends secretly hate the way I act. ” ” | “I'm grateful I have supportive friends, and I can take steps to strengthen those friendships.” |
| “My relationship is falling apart, but therapy would be a waste of my time.” | “There's still time to repair my relationship. Therapy might help me grow.” |
| “I skipped my workout, which means that I'm lazy and unhealthy.” | “I didn't have the time or motivation to exercise today. I can do it some other time and let my body rest today.” |
Use self-talk to encourage yourself rather than tear yourself down. Talk to yourself as if you're trying to comfort or empower a loved one.
Helping someone with OCPD practice self-compassion
If you live with someone with OCPD, offer them praise to counter their negative self judgments. For example, if they didn't break their own jogging record, remind them that their current record is extremely impressive.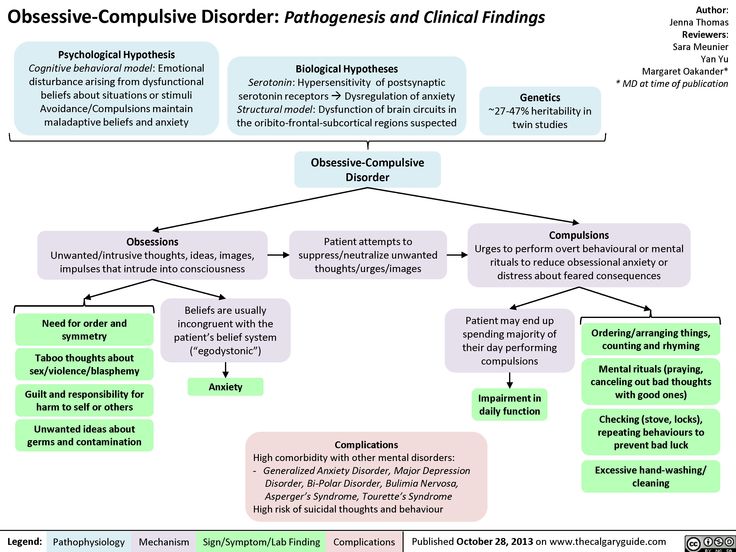 Let them know that there is always time for growth. This may help steer them away from “all or nothing” thinking and remind them to be self-compassionate.
Let them know that there is always time for growth. This may help steer them away from “all or nothing” thinking and remind them to be self-compassionate.
You can also encourage them to join you in meditation practices that focus specifically on self-kindness. Try our audio guide Being Kind to Yourself: A Meditation.
Tip 3: Manage emotions
A 2015 study that investigated emotional functioning in people with OCPD found that the disorder is associated with high levels of negative emotions, such as frustration, as well as difficulties identifying and accepting their own emotions.
So, if you have OCPD, it's not unusual to want to hide back certain emotions, especially negative ones like shame, anger, or fear. You might even feel uncomfortable when other people express those emotions. However, suppressing your emotions can also lead to issues over time, such as angry outbursts and depressive episodes. Here are a few ways to better manage your emotions:
Identify your emotions. Learn to identify your emotions instead of denying what you're feeling. You might begin by learning to notice physical signs of your emotions. Maybe when you're angry you feel your jaw tighten, or perhaps when you're sad you feel yourself droop.
Learn to identify your emotions instead of denying what you're feeling. You might begin by learning to notice physical signs of your emotions. Maybe when you're angry you feel your jaw tighten, or perhaps when you're sad you feel yourself droop.
Accept your emotions. This can be difficult, especially if you pride yourself on keeping a level head. Just know that everyone experiences a range of emotions, and it's normal to feel everything from sadness to anger to shame. Having these emotions doesn't make you a weak person.
Problem solve. Identify what's bothering you. Maybe you made a mistake at work and feel angry at yourself for overlooking details. Is there anything you can do to address the root cause of the issue? Or maybe an argument with your partner has left you feeling tired and depressed. What can be done to repair the rift between the two of you?
Reevaluate the situation. Not every problem has a solution.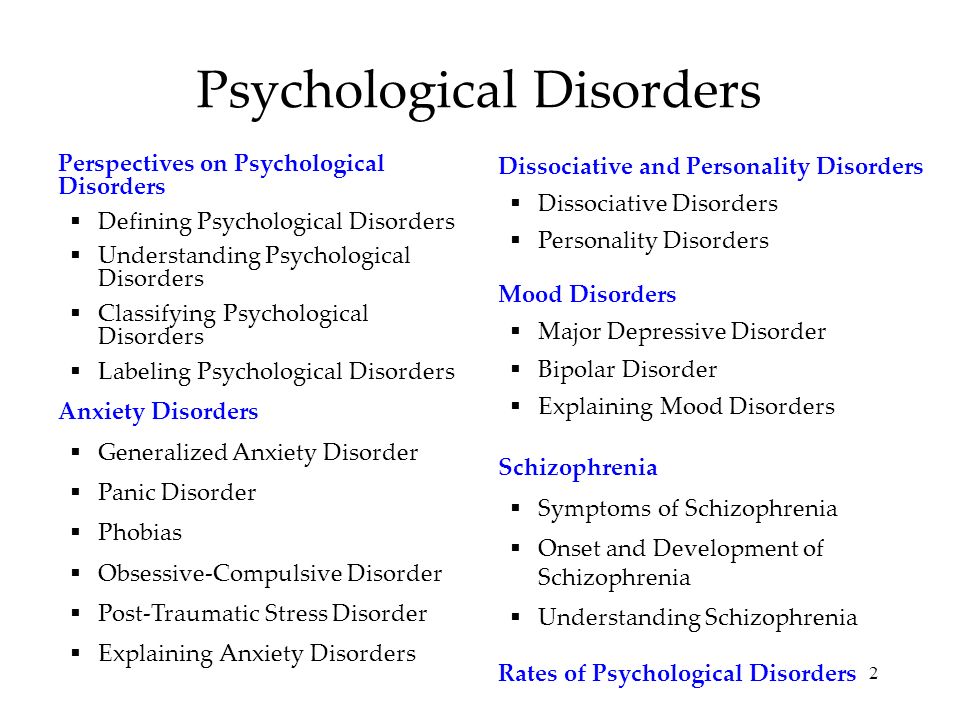 In some cases, you may simply need to accept and reevaluate the situation. Imagine that you've fallen behind schedule and now you have no time for your daily run. In the grand scheme of things, does it matter that you've missed this workout? Perhaps your body needed the rest anyway. Reappraising matters can help put them in perspective and steer you away from catastrophizing.
In some cases, you may simply need to accept and reevaluate the situation. Imagine that you've fallen behind schedule and now you have no time for your daily run. In the grand scheme of things, does it matter that you've missed this workout? Perhaps your body needed the rest anyway. Reappraising matters can help put them in perspective and steer you away from catastrophizing.
Helping someone with OCPD manage emotions
You can encourage your loved one to use the steps above, but you can also go further and make them feel comfortable venting to you. Be an engaged listener by asking questions and empathizing with them. You shouldn't try to write off their concerns as “no big deal,” but you can gently move them along in reevaluating the situation.
Tip 4: Reach out for help
If you have OCPD, be willing to accept two potentially uncomfortable truths: You can't do everything alone and you have blind spots. Get in contact with self-help groups or online forums where people share their OCPD experiences. This can help you learn more about how the disorder affects people in different ways. You'll also learn how others cope with the negative aspects of OCPD.
This can help you learn more about how the disorder affects people in different ways. You'll also learn how others cope with the negative aspects of OCPD.
Encouraging someone with OCPD to reach out for help
If you're close to someone with OCPD, be prepared for them to push back on the idea that they need to change or improve at all. However, gently encouraging them to join OCPD self-help groups may lead them to self-reflection. They may be more willing to hear from people who have similar preoccupations with perfectionism and orderliness.
Another strategy is to point to depression, work burnout, anxiety, or irritability as a reason to seek out help rather than place the emphasis on OCPD. Appeal to the person logically, citing concrete examples of how certain traits impact your relationship.
How OCPD affects relationships
If you're in a relationship with someone with OCPD, you might struggle with your friend or partner's persistent need for control. Maybe they always insist on planning out every detail of your vacation. Or perhaps they demand that every room in the house be cleaned in a specific way and according to a specific schedule. You may have grown accustomed to walking away from arguments or feeling like their work life takes priority over you.
Or perhaps they demand that every room in the house be cleaned in a specific way and according to a specific schedule. You may have grown accustomed to walking away from arguments or feeling like their work life takes priority over you.
And if you're the one with OCPD, you might feel frustrated that the people around you have different standards. Maybe your spouse or roommate doesn't keep things as tidy as you'd like. Or perhaps they aren't as punctual or frugal as you.
Despite all of these potential frustrations, it's possible for people with OCPD to have long and healthy relationships with others. Whether you or your loved one has OCPD, use the following strategies to keep the peace:
Don't fixate on winning
This can be particularly challenging for a person with OCPD, who may feel a strong desire to be right. However, even those without OCPD may struggle with this. Do your best to put your ego aside during arguments, and look to resolve conflicts rather than “win” them.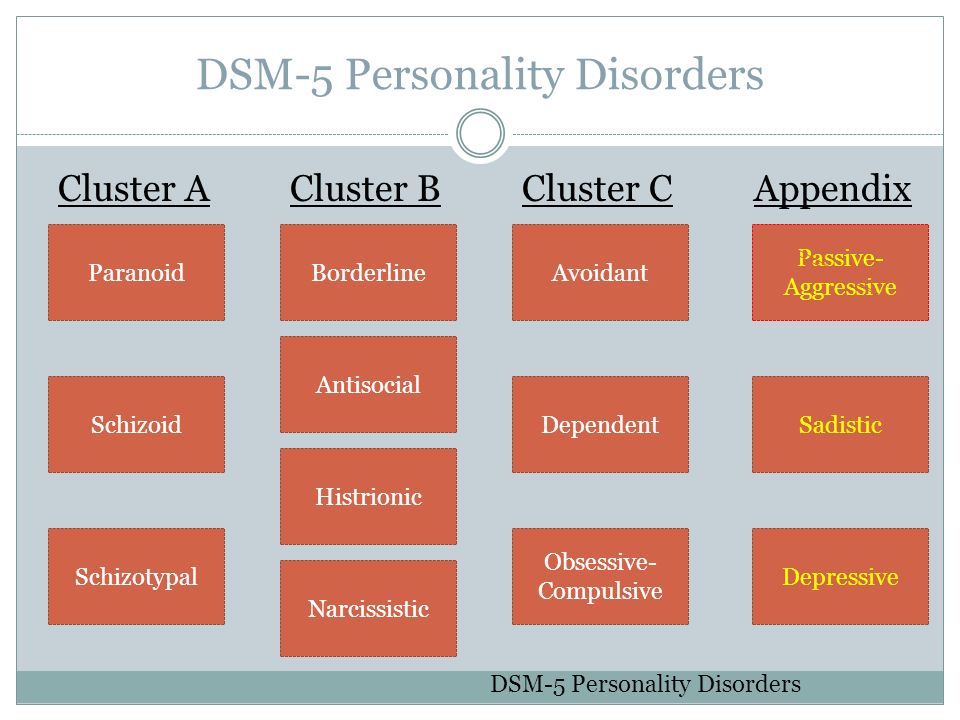
Be respectful and thoughtful in communicating, even if you both need to take an occasional pause to clear your heads. Use “I” statements to express your perspective. Avoid using “you” statements to assign blame. Don't hesitate to apologize when necessary.
Appreciate each other
Sometimes it's easy for a person with OCPD to fall into a routine of being overly critical. And the person without OCPD may fall into a similar pattern, focusing only on their friend or partner's rigidity and negative aspects.
Remember to be vocal about what traits you appreciate in each other, such as work ethic and reliability. Tell the person how they've improved your life, whether that includes their emotional support or their contributions to the household. This helps create a sense of security.
See the good in your partner
Despite a tendency to be controlling, people with OCPD often have good intentions. And when they show annoyance or frustration, they're likely grappling with feelings of anxiety or helplessness. Recognize those feelings, and ask what you can do to help.
Recognize those feelings, and ask what you can do to help.
If you have OCPD, it's also important to recognize the other person's good intentions. Their drive toward perfection may not be as strong as yours, but, in the end, neither of you can ever be flawless.
Take care of yourself
Having a relationship with someone with OCPD may require you to be more assertive. Be clear about what expectations are too high. For example, if you believe their cleanliness demands are unreasonable, let your loved one know.
Try to compromise on a solution, and don't feel the need to overextend yourself. Recognize that your way of doing things doesn't have to match their way of doing things.
If a romantic relationship isn't working, couple's therapy can be helpful. However, if your partner is abusive or unwilling to change, you may need to accept that the relationship won't work at this time.
[Read: Dealing with a Breakup or Divorce]
Professional treatment for OCPD
When self-help treatments offer little relief from negative OCPD symptoms, professional treatments are the next step.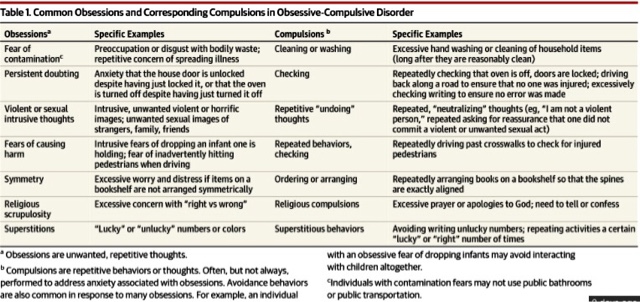 Again, many people with OCPD may not see the need to treat symptoms, much less visit a professional. You may need to be patient and present evidence that intervention is needed.
Again, many people with OCPD may not see the need to treat symptoms, much less visit a professional. You may need to be patient and present evidence that intervention is needed.
Therapy
Two common approaches to therapy for OCPD include cognitive behavioral therapy (CBT) and psychodynamic therapy.
During CBT, a therapist may draw the person's attention to how their core beliefs can be detrimental to their mental health, physical health, and relationships. For example, a therapist might challenge a person's core belief of, “I need to create lists and plan things out to feel comfortable.” CBT can also help a person find constructive ways to express emotions such as frustration.
Psychodynamic therapy helps a person with OCPD connect present-day traits with past experiences. A person with OCPD might find that their need for control and order is rooted in childhood experiences with overly critical parents.
[Read: Online Therapy: Is it Right for You?]
Other potential therapy interventions may include:
- Dialectical behavioral therapy (DBT), which may improve emotional regulation.

- Nidotherapy, which focuses on making environmental changes to improve the person's mental health.
Medication
You won't find a single type of medication for treating the entire spectrum of OCPD symptoms. However, certain medication can be prescribed to treat specific aspects of OCPD and its co-occurring disorders. A few examples include:
- Selective serotonin reuptake inhibitors (SSRIs), types of antidepressants, may be used to decrease the person's over fixation on details.
- Benzodiazepines and other anti-anxiety drugs may help a person with OCPD who is also experiencing an anxiety disorder, such as OCD.
- Anticonvulsant medications may be used to reduce irritability and stabilize mood.
Finding the right mix of medication and therapy may require some trial and error. In the meantime, a focus on accepting imperfections and managing negative emotions may lead to noticeable changes.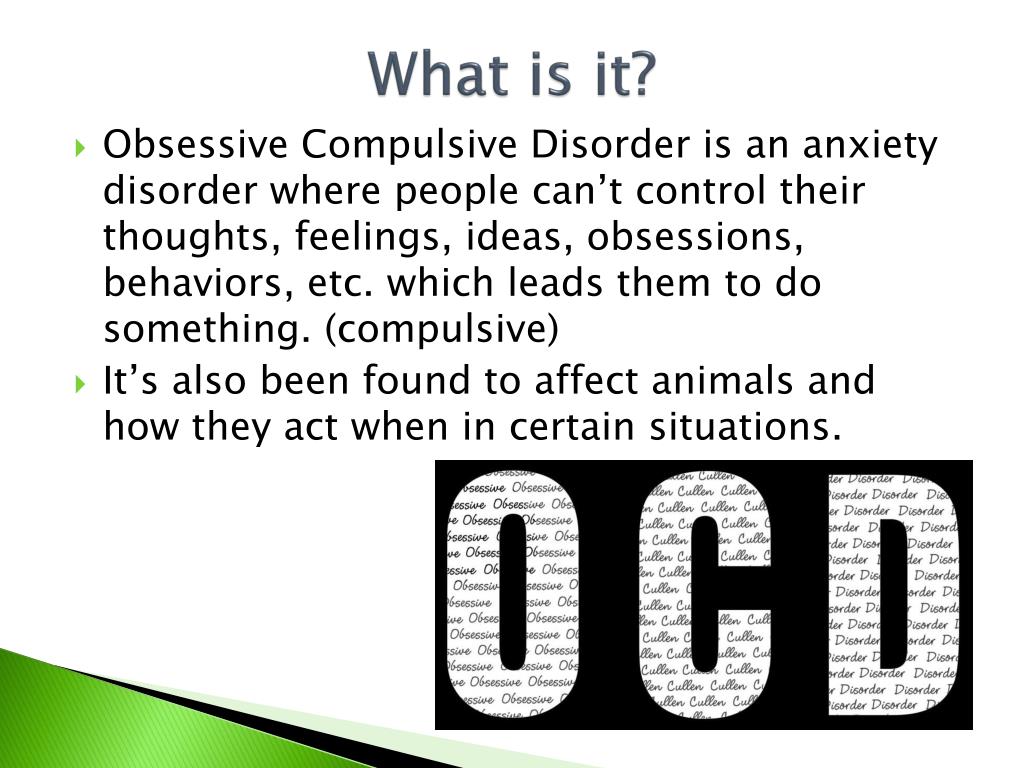
Author: Sheldon Reid.
- References
Personality Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x18_Personality_Disorders
Bowen, R., Rahman, H., Dong, L. Y., Khalaj, S., Baetz, M., Peters, E., & Balbuena, L. (2019). Suicidality in People With Obsessive-Compulsive Symptoms or Personality Traits. Frontiers in Psychiatry, 9, 747. https://doi.org/10.3389/fpsyt.2018.00747
Diedrich, A., & Voderholzer, U. (2015). Obsessive–Compulsive Personality Disorder: A Current Review. Current Psychiatry Reports, 17(2), 2. https://doi.org/10.1007/s11920-014-0547-8
Georgiadou, O., Garyfallos, G., Bozikas, V., Protogerou, C., Kosti, F., Ziliaskopoulou, D., & Adamopoulou, A. (2008). Axis I-Axis II comorbidity of Obsessive Compulsive Personality Disorder: Gender-related differences.
 Annals of General Psychiatry, 7(S1), S227, 1744-859X-7-S1–S227. https://doi.org/10.1186/1744-859X-7-S1-S227
Annals of General Psychiatry, 7(S1), S227, 1744-859X-7-S1–S227. https://doi.org/10.1186/1744-859X-7-S1-S227Grant, J. E., Mooney, M. E., & Kushner, M. G. (2012). Prevalence, correlates, and comorbidity of DSM-IV obsessive-compulsive personality disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Psychiatric Research, 46(4), 469–475. https://doi.org/10.1016/j.jpsychires.2012.01.009
Greve, K. W., & Adams, D. (2002). Treatment of features of Obsessive-Compulsive Personality Disorder using carbamazepine. Psychiatry and Clinical Neurosciences, 56(2), 207–208. https://doi.org/10.1046/j.1440-1819.2002.00946.x
Halmi, K. A., Tozzi, F., Thornton, L. M., Crow, S., Fichter, M. M., Kaplan, A. S., Keel, P., Klump, K. L., Lilenfeld, L. R., Mitchell, J. E., Plotnicov, K. H., Pollice, C., Rotondo, A., Strober, M., Woodside, D. B., Berrettini, W. H., Kaye, W. H., & Bulik, C. M. (2005). The relation among perfectionism, obsessive-compulsive personality disorder and obsessive-compulsive disorder in individuals with eating disorders.
 International Journal of Eating Disorders, 38(4), 371–374. https://doi.org/10.1002/eat.20190
International Journal of Eating Disorders, 38(4), 371–374. https://doi.org/10.1002/eat.20190Morreale, M., Holingue, C., Samuels, J., & Nestadt, G. (2021). Long‐term physical health outcomes of obsessive‐compulsive personality disorder traits. Journal of Clinical Psychology, 77(11), 2626–2637. https://doi.org/10.1002/jclp.23207
Obsessive-Compulsive Personality Disorder & Suicide | Psychiatrist.com. (n.d.). Retrieved January 20, 2022, from https://www.psychiatrist.com/jcp/personality/obsessive-compulsive-personality-disorder-suicidal/
Obsessive-Compulsive Personality Disorder (OCPD)—Psychiatric Disorders—Merck Manuals Professional Edition. (n.d.). Retrieved January 20, 2022, from https://www.merckmanuals.com/professional/psychiatric-disorders/personality-disorders/obsessive-compulsive-personality-disorder-ocpd
Personality Disorder and Cardiovascular Disease: Results From a National Household Survey. | Psychiatrist.com.
 (n.d.). Retrieved January 20, 2022, from https://www.psychiatrist.com/jcp/personality/personality-disorder-cardiovascular-disease-results/
(n.d.). Retrieved January 20, 2022, from https://www.psychiatrist.com/jcp/personality/personality-disorder-cardiovascular-disease-results/Pinto, A., Steinglass, J. E., Greene, A. L., Weber, E. U., & Simpson, H. B. (2014). Capacity to Delay Reward Differentiates Obsessive-Compulsive Disorder and Obsessive-Compulsive Personality Disorder. Biological Psychiatry, 75(8), 653–659. https://doi.org/10.1016/j.biopsych.2013.09.007
Quirk, S. E., El-Gabalawy, R., Brennan, S. L., Bolton, J. M., Sareen, J., Berk, M., Chanen, A. M., Pasco, J. A., & Williams, L. J. (2015). Personality disorders and physical comorbidities in adults from the United States: Data from the National Epidemiologic Survey on Alcohol and Related Conditions. Social Psychiatry and Psychiatric Epidemiology, 50(5), 807–820. https://doi.org/10.1007/s00127-014-0974-1
Reddy, M. S., Vijay M., S., & Reddy, S. (2016). Obsessive-compulsive (Anankastic) Personality Disorder: A Poorly Researched Landscape with Significant Clinical Relevance.
 Indian Journal of Psychological Medicine, 38(1), 1–5. https://doi.org/10.4103/0253-7176.175085
Indian Journal of Psychological Medicine, 38(1), 1–5. https://doi.org/10.4103/0253-7176.175085Rowland, T. A., Kumar Jainer, A., & Panchal, R. (2017). Living with obsessional personality. BJPsych Bulletin, 41(6), 366–367. https://doi.org/10.1192/pb.41.6.366a
Steenkamp, M. M., Suvak, M. K., Dickstein, B. D., Shea, M. T., & Litz, B. T. (2015). Emotional Functioning in Obsessive-Compulsive Personality Disorder: Comparison to Borderline Personality Disorder and Healthy Controls. Journal of Personality Disorders, 29(6), 794–808. https://doi.org/10.1521/pedi_2014_28_174
Thamby, A., & Khanna, S. (2019). The role of personality disorders in obsessive-compulsive disorder. Indian Journal of Psychiatry, 61(7), 114. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_526_18
Obsessive Compulsive Personality Disorder (OCPD) (PDF) – Fact sheet covering symptoms, diagnosis, and treatment. (International OCD Foundation)
OCPD Online – Articles, tests, and resources. (The OCPD Foundation)
(The OCPD Foundation)
OCPD: My Life In Debris – Video content about living life with OCPD. (YouTube)
Around the web
Last updated: October 14, 2022
Obsessive-Compulsive Personality Disorder (OCPD) - Psychiatric Disorders
By
Mark Zimmerman
, MD, Rhode Island Hospital
Last full review/revision May 2021| Content last modified Sep 2022
Click here for Patient Education
Obsessive-compulsive personality disorder is characterized by a pervasive preoccupation with orderliness, perfectionism, and control (with no room for flexibility) that ultimately slows or interferes with completing a task. Diagnosis is by clinical criteria. Treatment is with psychodynamic psychotherapy, cognitive-behavioral therapy, and selective serotonin reuptake inhibitors (SSRIs).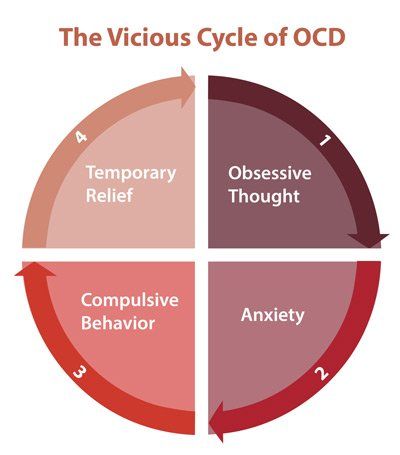
(See also Overview of Personality Disorders Overview of Personality Disorders Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more .)
Because patients with obsessive-compulsive personality disorder need to be in control, they tend to be solitary in their endeavors and to mistrust the help of others.
About 2.1 to 7.9% of the general population are estimated to have obsessive-compulsive personality disorder; it is more common among men.
Familial traits of compulsivity, restricted range of emotion, and perfectionism are thought to contribute to this disorder.
Comorbidities may be present. Patients often also have a depressive disorder Depressive Disorders Depressive disorders are characterized by sadness severe enough or persistent enough to interfere with function and often by decreased interest or pleasure in activities. Exact cause is unknown... read more (major depressive disorder or persistent depressive disorder) or an alcohol use disorder Alcohol Toxicity and Withdrawal Alcohol (ethanol) is a central nervous system depressant. Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Exact cause is unknown... read more (major depressive disorder or persistent depressive disorder) or an alcohol use disorder Alcohol Toxicity and Withdrawal Alcohol (ethanol) is a central nervous system depressant. Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Symptoms of obsessive-compulsive personality disorder may lessen even over a time period as short as 1 year, but their persistence (ie, remission and relapse rates) during the long term are less clear.
In patients with obsessive-compulsive personality disorder, preoccupation with order, perfectionism, and control of themselves and situations interferes with flexibility, effectiveness, and openness. Rigid and stubborn in their activities, these patients insist that everything be done in specific ways.
To maintain a sense of control, patients focus on rules, minute details, procedures, schedules, and lists. As a result, the main point of a project or activity is lost. These patients repeatedly check for mistakes and pay extraordinary attention to detail. They do not make good use of their time, often leaving the most important tasks until the end. Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
As a result, the main point of a project or activity is lost. These patients repeatedly check for mistakes and pay extraordinary attention to detail. They do not make good use of their time, often leaving the most important tasks until the end. Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
Because these patients want everything done in a specific way, they have difficulty delegating tasks and working with others. When working with others, they may make detailed lists about how a task should be done and become upset if a coworker suggests an alternative way. They may reject help even when they are behind schedule.
Patients with obsessive-compulsive personality disorder are excessively dedicated to work and productivity; their dedication is not motivated by financial necessity. As a result, leisure activities and relationships are neglected. They may think they have no time to relax or go out with friends; they may postpone a vacation so long that it does not happen, or they may feel they must take work with them so that they do not waste time. Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
As a result, leisure activities and relationships are neglected. They may think they have no time to relax or go out with friends; they may postpone a vacation so long that it does not happen, or they may feel they must take work with them so that they do not waste time. Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
These patients plan ahead in great detail and do not wish to consider changes. Their relentless rigidity may frustrate coworkers and friends.
Expression of affection is also tightly controlled. These patients may relate to others in a formal, stiff, or serious way. Often, they speak only after they think of the perfect thing to say. They may focus on logic and intellect and be intolerant of emotional or expressive behavior.
These patients may be overzealous, picky, and rigid about issues of morality, ethics, and values.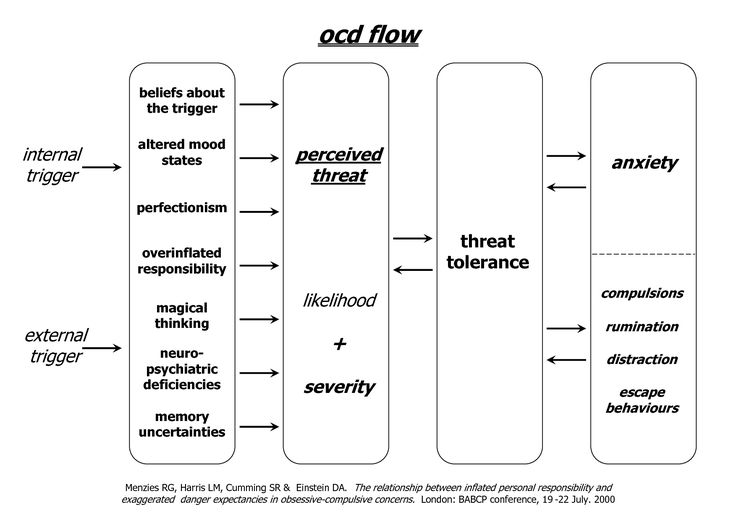 They apply rigid moral principles to themselves and to others and are harshly self-critical. They are rigidly deferential to authorities and insist on exact compliance to rules, with no exceptions for extenuating circumstances.
They apply rigid moral principles to themselves and to others and are harshly self-critical. They are rigidly deferential to authorities and insist on exact compliance to rules, with no exceptions for extenuating circumstances.
For a diagnosis of obsessive-compulsive personality disorder, patients must have
This pattern is shown by the presence of ≥ 4 of the following:
Preoccupation with details, rules, schedules, organization, and lists
A striving to do something perfectly that interferes with completion of the task
Excessive devotion to work and productivity (not due to financial necessity), resulting in neglect of leisure activities and friends
Excessive conscientiousness, fastidiousness, and inflexibility regarding ethical and moral issues and values
Unwillingness to throw out worn-out or worthless objects, even those with no sentimental value
Reluctance to delegate or work with other people unless those people agree to do things exactly as the patients want
A miserly approach to spending for themselves and others because they see money as something to be saved for future disasters
Rigidity and stubbornness
Also, symptoms must have begun by early adulthood.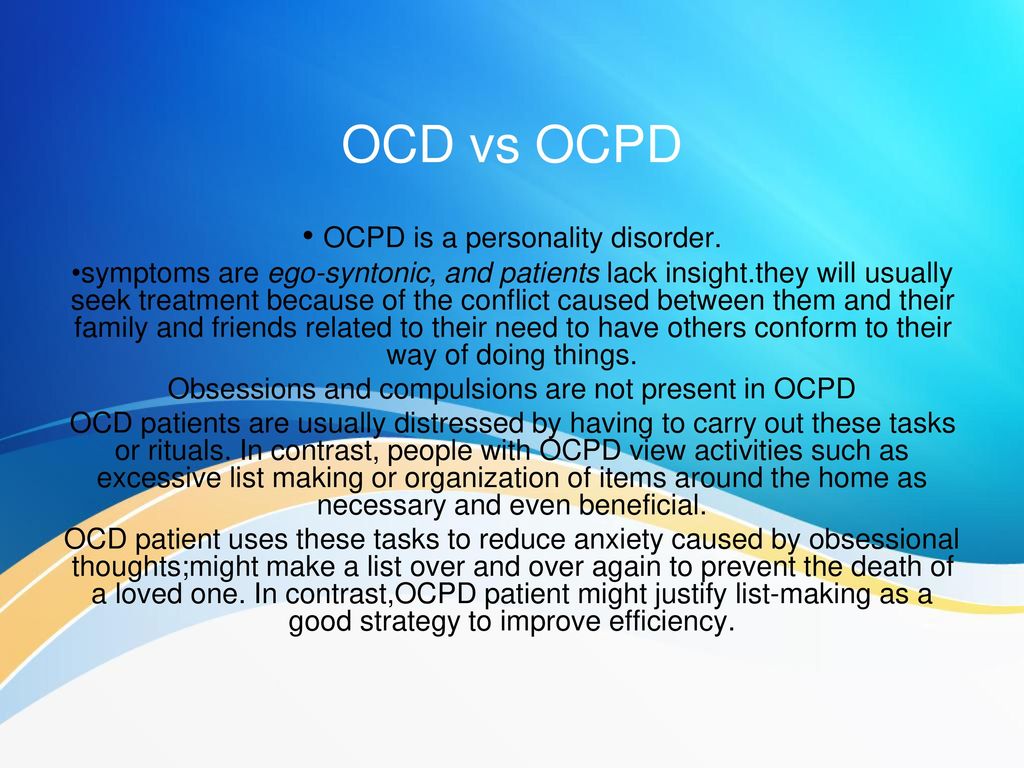
Obsessive-compulsive personality disorder should be distinguished from the following disorders:
Obsessive-compulsive disorder (OCD) Obsessive-Compulsive Disorder (OCD) Obsessive-compulsive disorder (OCD) is characterized by recurrent, persistent, unwanted, and intrusive thoughts, urges, or images (obsessions) and/or by repetitive behaviors or mental acts that... read more : Patients with OCD have true obsessions (repetitive, unwanted, intrusive thoughts that cause marked anxiety) and compulsions (ritualistic behaviors that they feel they must do to reduce their anxiety-related obsessions). Patients with OCD are often distressed by their lack of control over compulsive drives; in patients with obsessive-compulsive personality disorder, the need for control is driven by their preoccupation with order so their behavior, values, and feelings are acceptable and consistent with their sense of self.
Avoidant personality disorder Avoidant Personality Disorder (AVPD) Avoidant personality disorder is characterized by the avoidance of social situations or interactions that involve risk of rejection, criticism, or humiliation.
 Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.
Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.Schizoid personality disorder Schizoid Personality Disorder (ScPD) Schizoid personality disorder is characterized by a pervasive pattern of detachment from and general disinterest in social relationships and a limited range of emotions in interpersonal relationships... read more : Both schizoid and obsessive-compulsive personality disorders are characterized by a seeming formality in interpersonal relationships and by detachment. However, the motives are different: a basic incapability for intimacy in patients with schizoid personality disorder vs discomfort with emotions and dedication to work in patients with obsessive-compulsive personality disorder.

Psychodynamic psychotherapy
Cognitive-behavioral therapy
Selective serotonin reuptake inhibitors (SSRIs)
General treatment Treatment Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more of obsessive-compulsive personality disorder is similar to that for all personality disorders.
Information about treatment for obsessive-compulsive personality disorder is sparse. Also, treatment is complicated by the patient's rigidity, obstinacy, and need for control, which can be frustrating for therapists.
Psychodynamic therapy and cognitive-behavioral therapy can help patients with obsessive-compulsive personality disorder. Sometimes during therapy, the patient's interesting, detailed, intellectualized conversation may seem psychologically oriented, but it is void of affect and does not lead to change.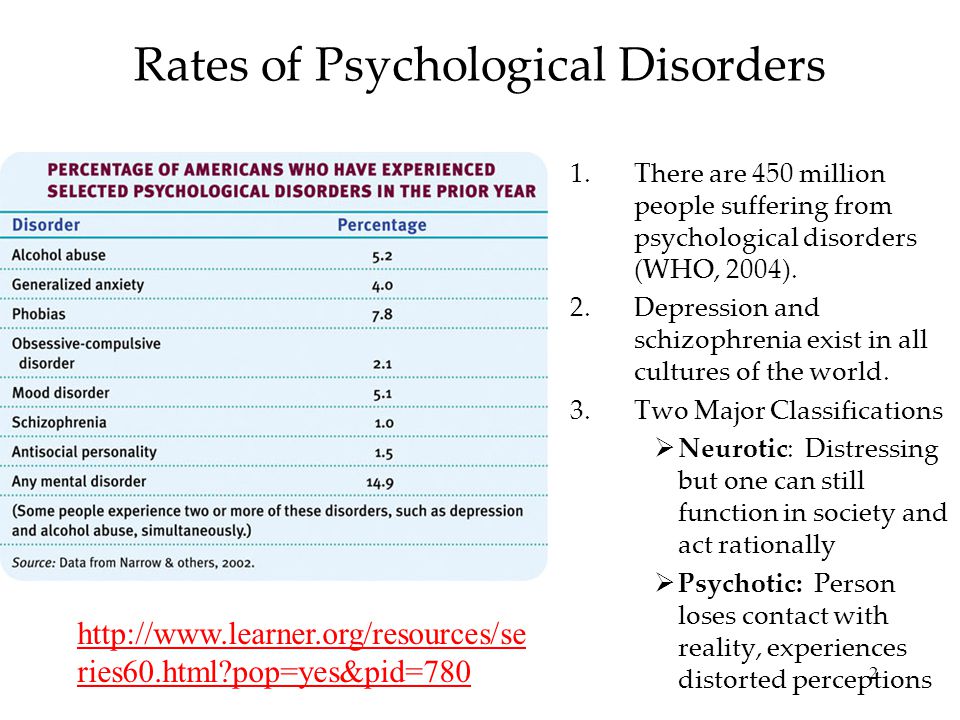
SSRIs Selective Serotonin Reuptake Inhibitors (SSRIs) Several drug classes and drugs can be used to treat depression: Selective serotonin reuptake inhibitors (SSRIs) Serotonin modulators (5-HT2 blockers) Serotonin-norepinephrine reuptake inhibitors... read more may be useful.
NOTE: This is the Professional Version. CONSUMERS: Click here for the Consumer VersionCopyright © 2022 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.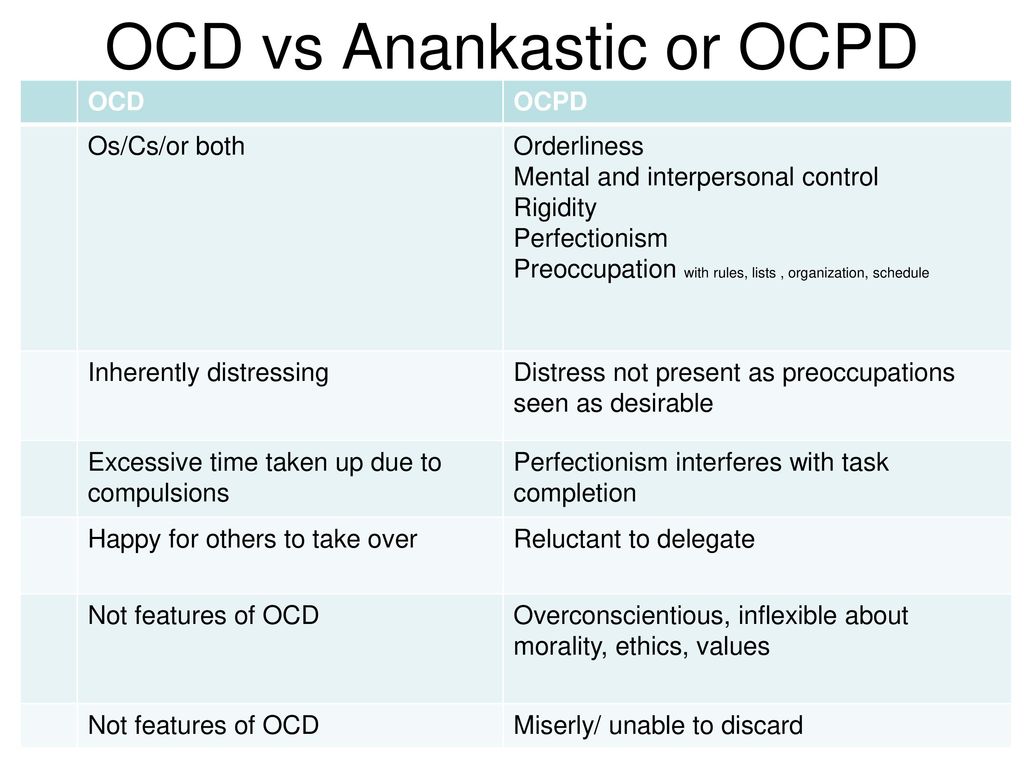
Obsession (lat. obsessio - taxation, siege, blockade).
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions). Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.
For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.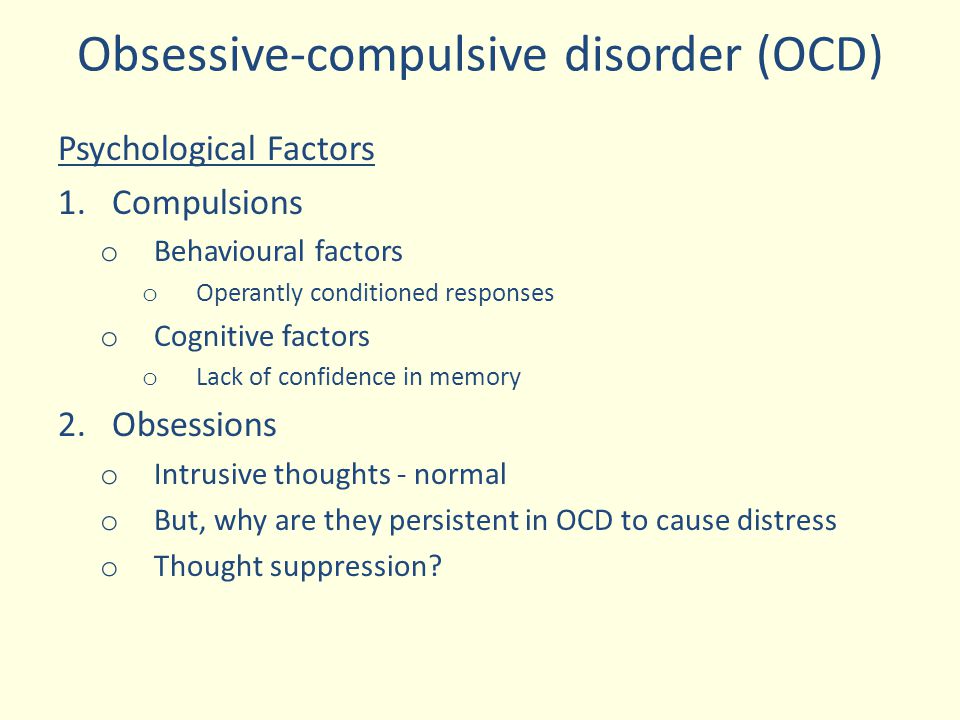 Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.
Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.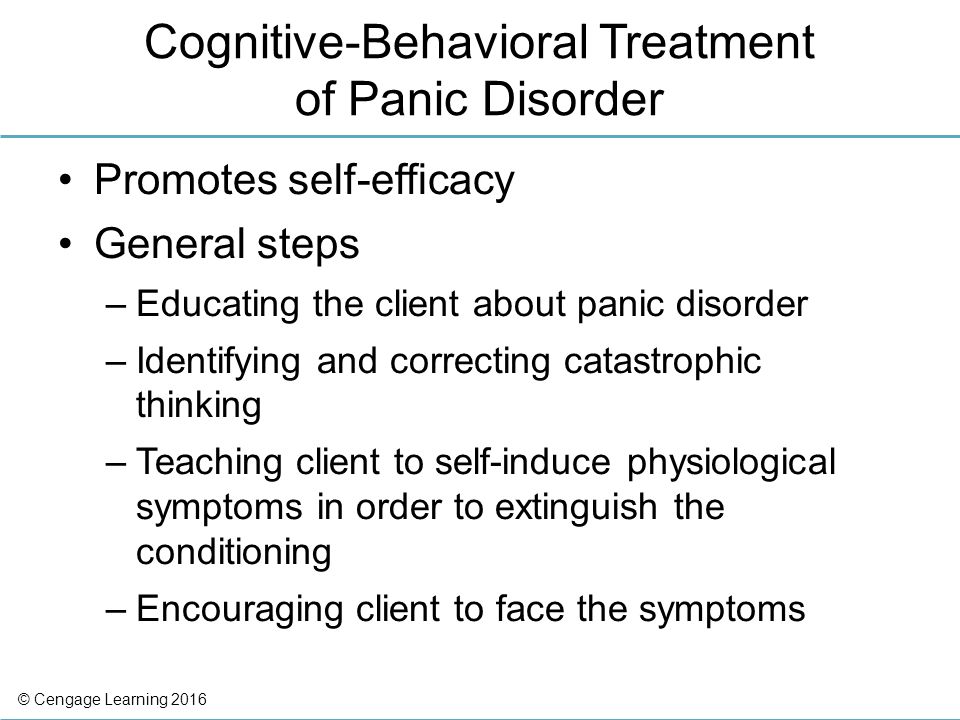 M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
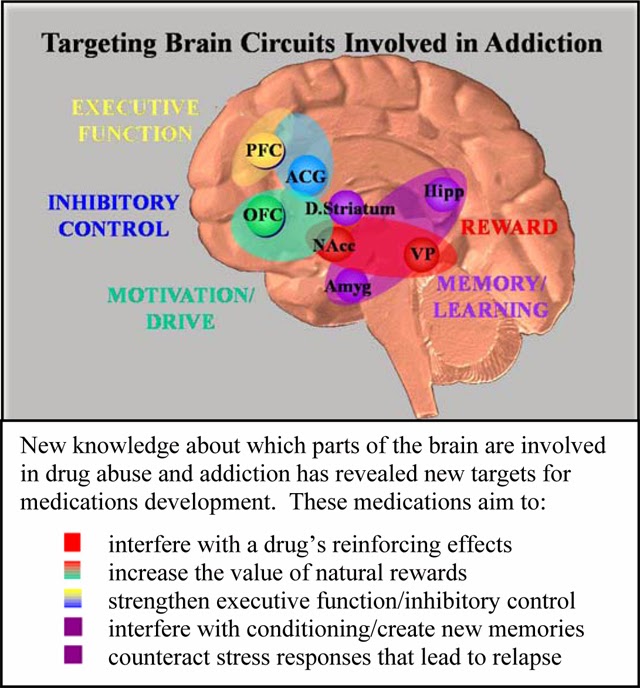
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them. Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally.
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century.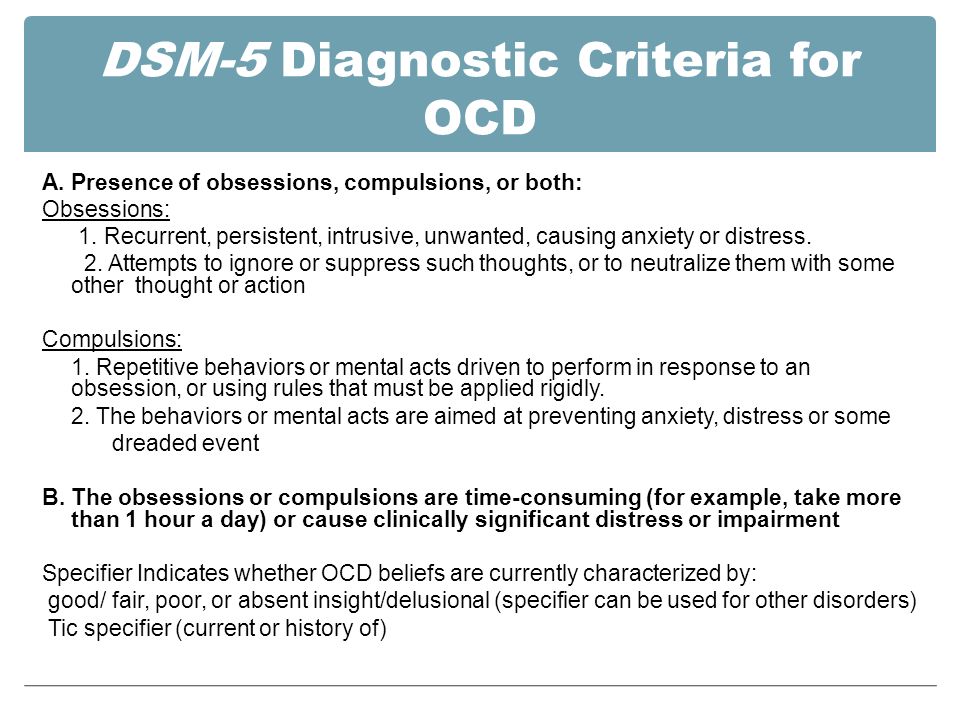 They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.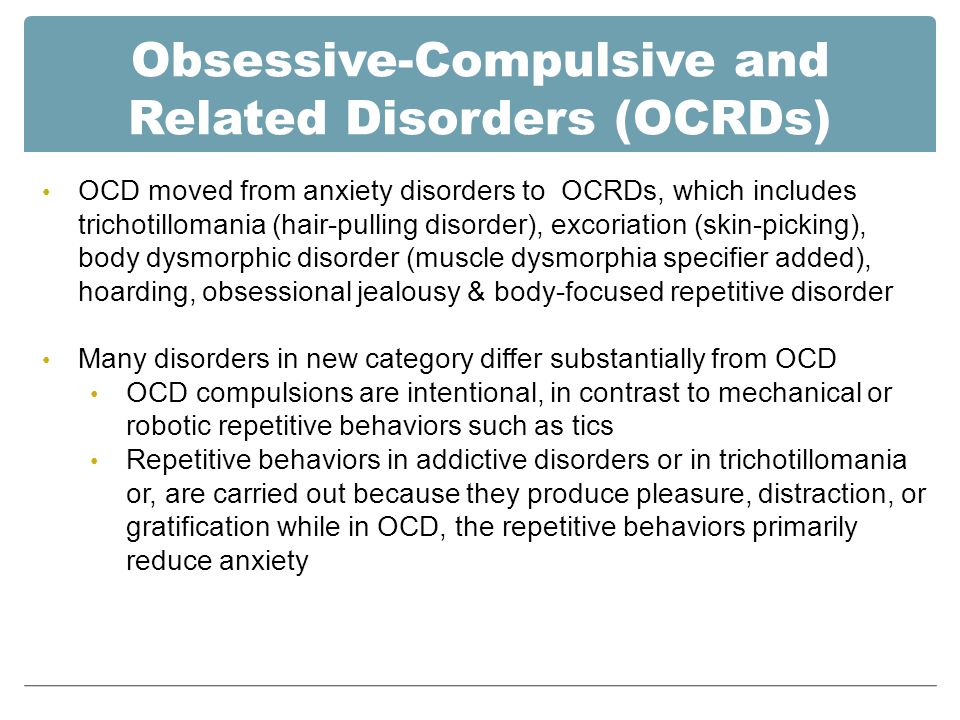
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessional thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking.
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.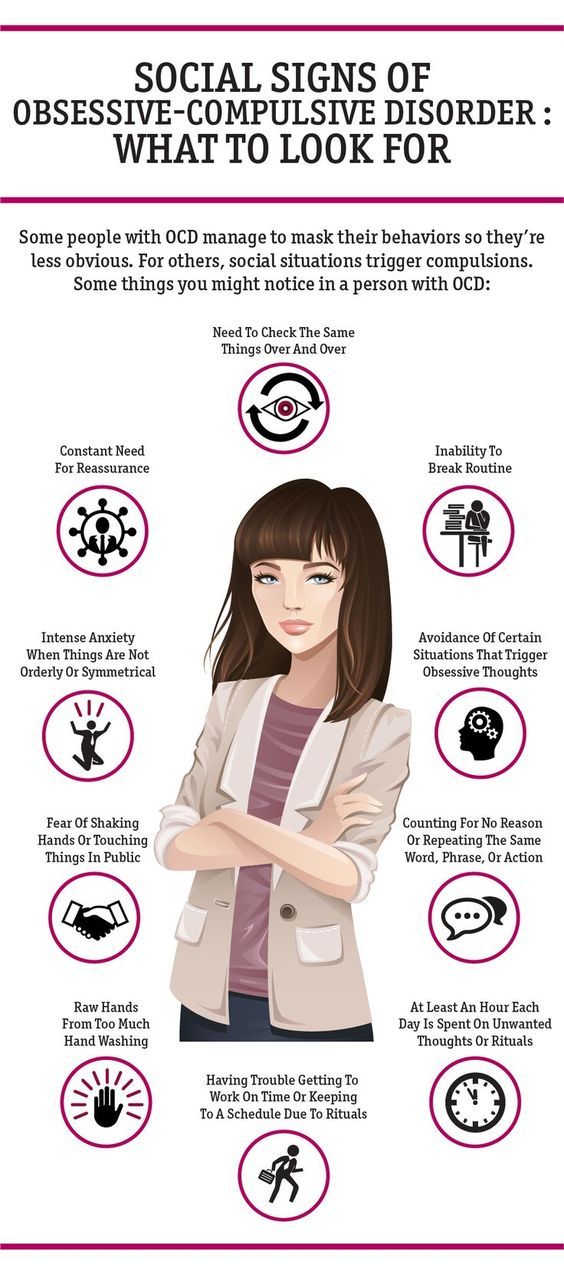
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities.
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised. Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept. Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions.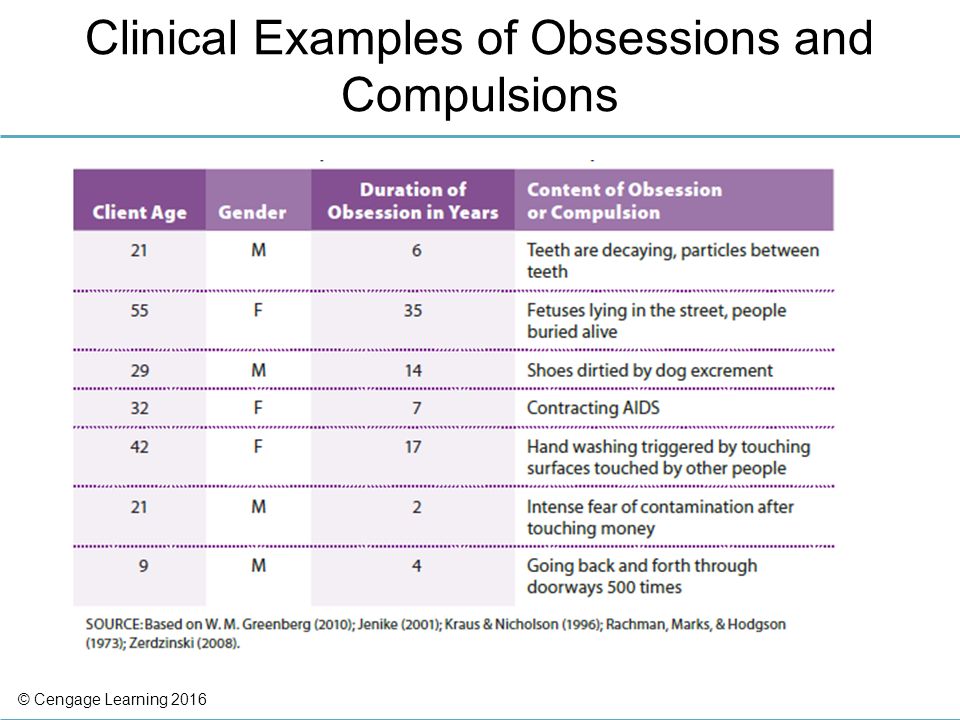 The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, remorse. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it.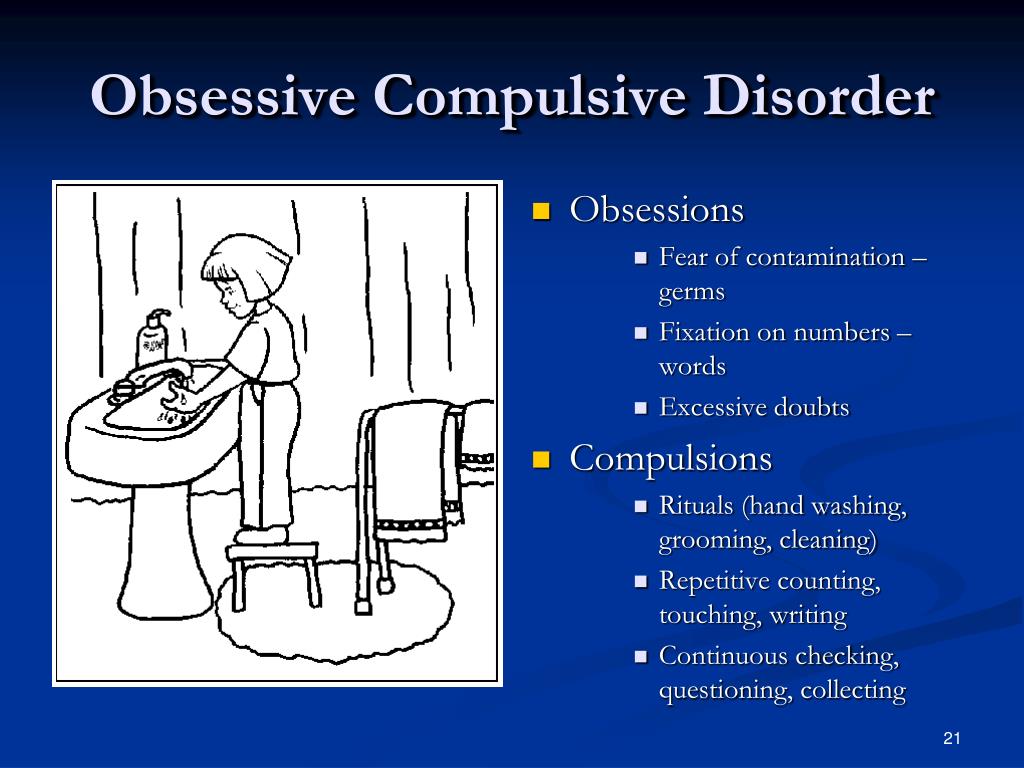 The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others.
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia). And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication.
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.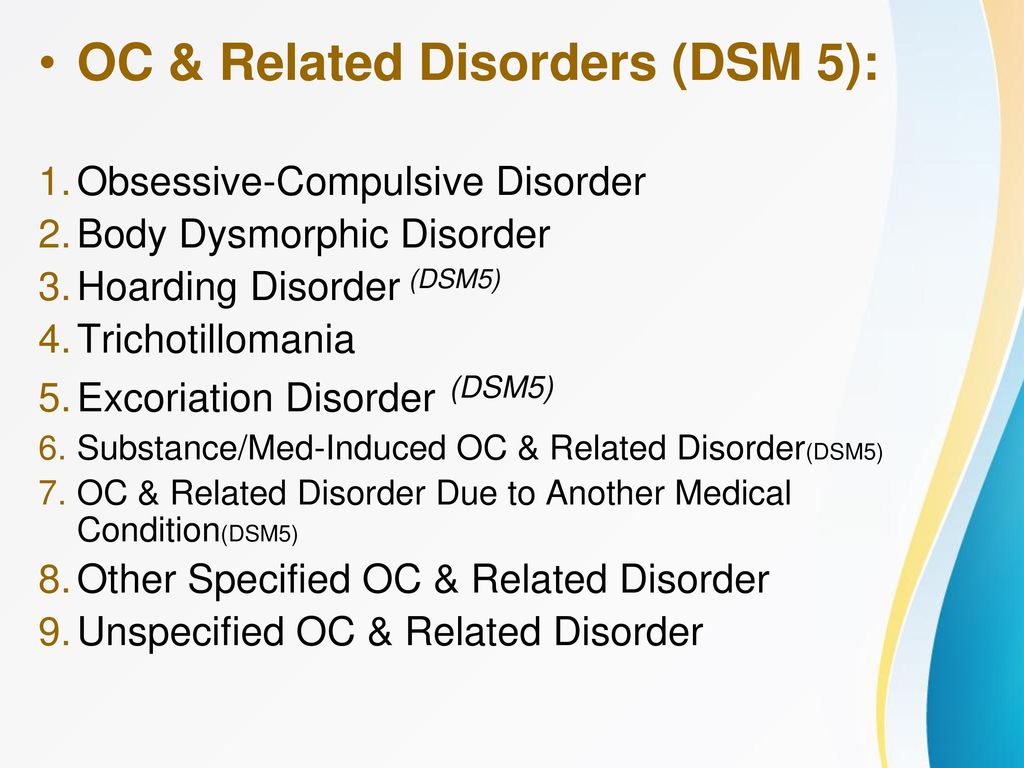
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades.
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others.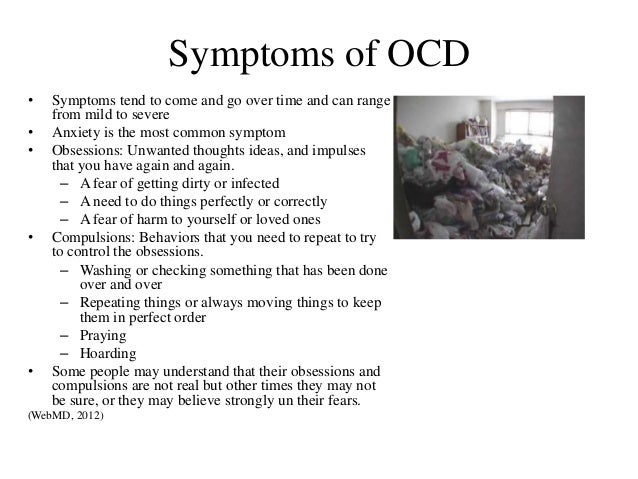 Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc. ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust). Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.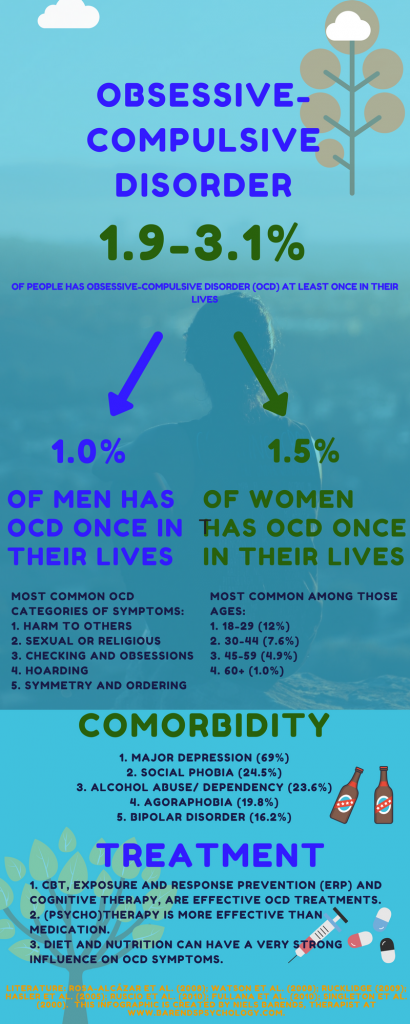 In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful. Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people.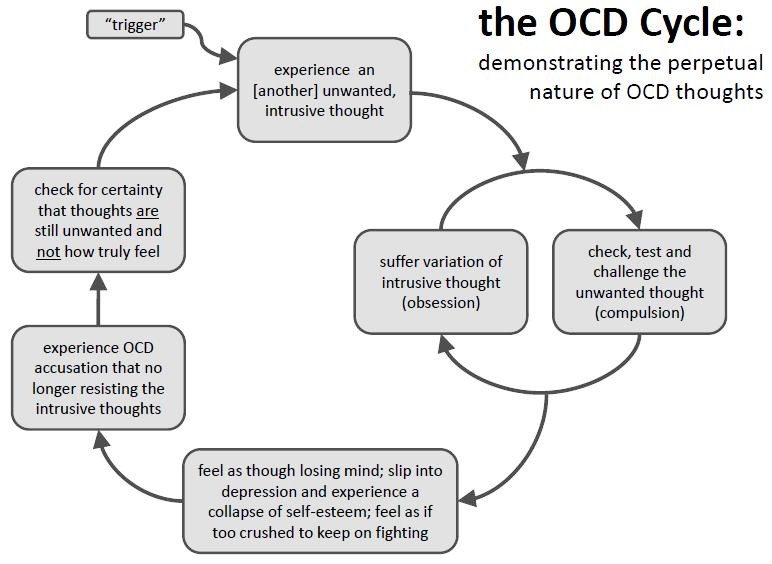 In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations. Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation. In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life. Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment. At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms.
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions). Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam).
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives.
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient. It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.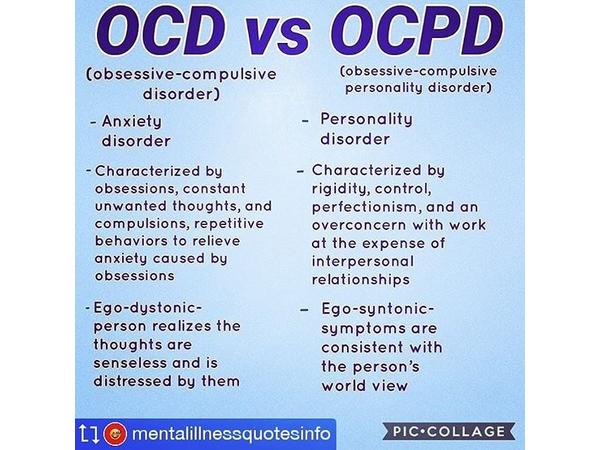 In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships. If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.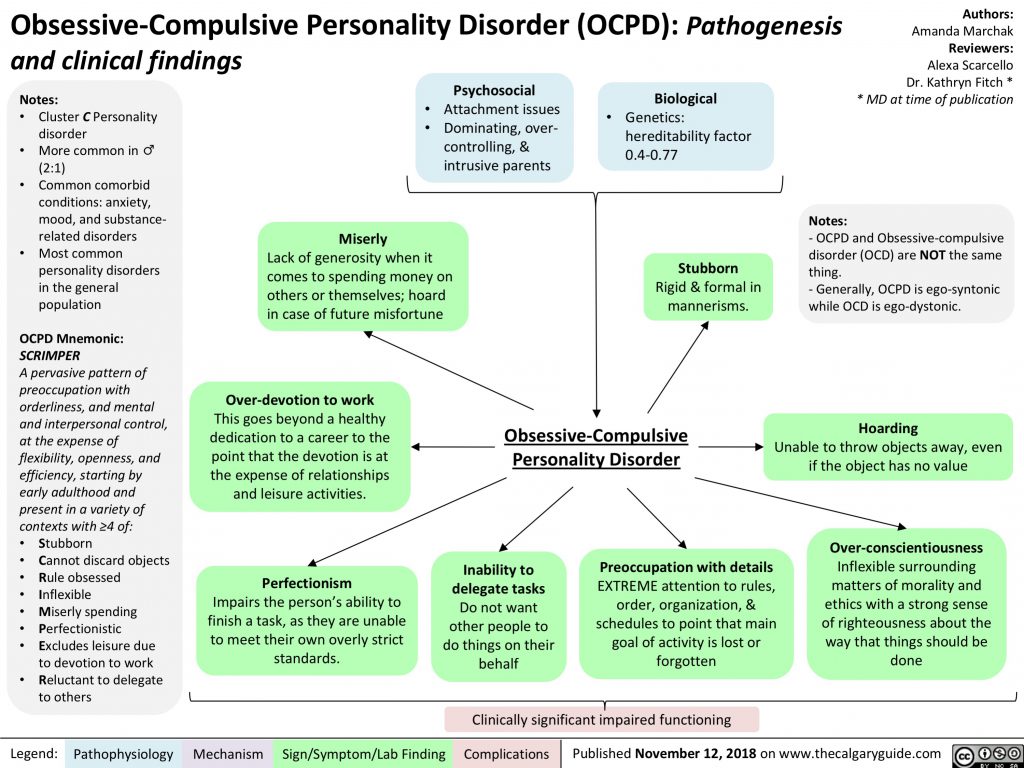
All of these methods, when used judiciously, can increase the effectiveness of drug therapy, but are not capable of completely replacing drugs. It should be noted that explanatory psychotherapy does not always help, and some patients with OCD even worsen because such procedures encourage them to think painfully and unproductively about the subjects discussed in the course of treatment. Unfortunately, science still does not know how to cure mental illness once and for all. OCD often has a tendency to recur, which requires long-term prophylactic medication.
How to recognize obsessive-compulsive disorder - Lifehacker
March 7, 2021LikbezZdorovye
There is a line after which the desire to put everything on the shelves turns into a neurosis.
Share
0You can not only read this article, but also listen to it. If it's more convenient for you, turn on the podcast.
Being a control freak is sometimes good.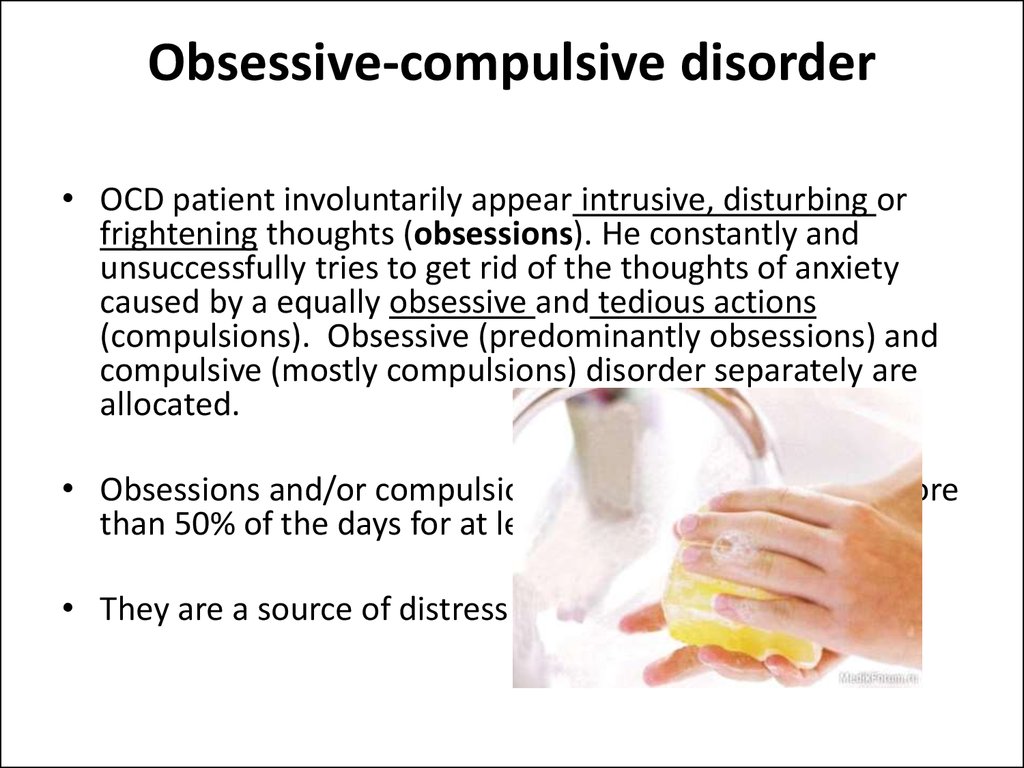 It is better to make sure five times that you definitely put your air tickets and passports in your bag than to find out later at the airport that the necessary documents are missing.
It is better to make sure five times that you definitely put your air tickets and passports in your bag than to find out later at the airport that the necessary documents are missing.
But for some, the desire to control and double-check becomes obsessive. And so much so that it seriously spoils life. A person is literally obsessed with certain things. For example, he cannot leave the house until he has made sure that the iron is turned off 20 times. Or he won't wash his hands 10 times. Or, let's say, does not bring the hallway to a shine.
This behavior is called obsessive-compulsive disorder or obsessive-compulsive disorder (OCD). With this disorder, a person is regularly visited by obsessive disturbing thoughts (obsessions), which he tries to get rid of with the help of equally obsessive rituals (compulsions).
According to the US National Institute of Mental Health's Obsessive‑Compulsive Disorder, OCD affects 1 to 2 people out of every 100.
In the US alone, the problem affects over two million people.
It is rather difficult to recognize the line where healthy forethought or love of cleanliness begins to turn into a mental disorder. But still it is possible - if you do not miss some characteristic symptoms.
How to recognize obsessive-compulsive disorder
All people are, of course, different. But obsessions most often develop along several similar scenarios Obsessive‑compulsive Disorder. Here they are.
1. Fear of germs or dirt
An uncontrollable passion for hygiene is one of the most common symptoms of OCD.
People with this disorder are desperately afraid that disease-causing microbes will settle on their hands or body. So they wash their hands five times in a row. And repeat the procedure every time you have to touch the doorknob or handset of the office phone. Well, the need to shake hands with a colleague, hug a friend at a meeting, or, let's say, grab a handrail in public transport, becomes their personal nightmare.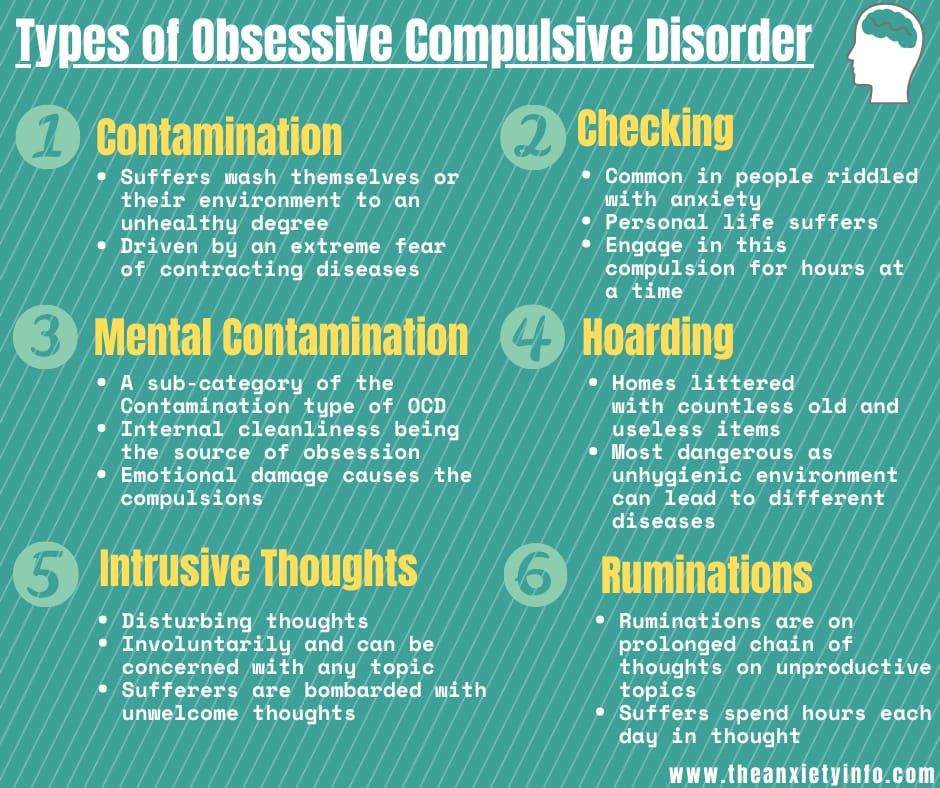
2. Unhealthy passion for cleaning
There are people whose houses literally shine. These are neat people. But if everything is clean and guests walk around the apartment like in a museum, but you are still unhappy and have an irresistible desire to rub mirrors and polish the floor in the hallway again and again, we can talk about it - obsessive-compulsive disorder.
3. The need to have everything in order (literally)
A cup left on the table instead of taking its place on the kitchen shelf can cause a natural tantrum in a person with OCD. He is enraged by any things that, in his opinion, are not where they should be. Slippers must be placed on a shoe rack, a program must be under the TV, and even a cat must sit in its basket. A person can be nervous even if the thing is located at the wrong angle.
Some might call this behavior a perfectionistic passion for order. But no - this is also a sign of obsessive-compulsive disorder.
4. Excessive self-doubt
Many people worry about how they look, whether they are doing the right thing and what others will think of them.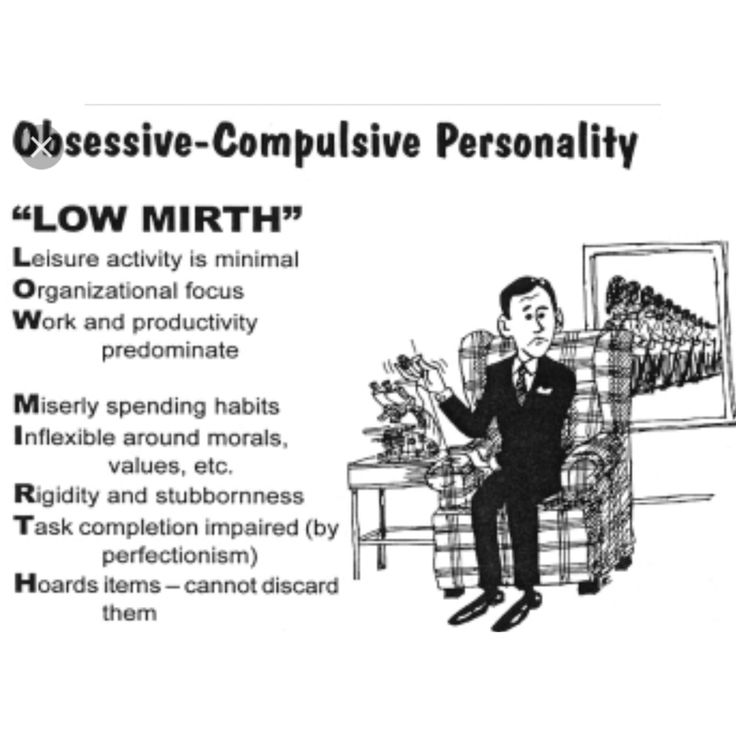 This is not a problem (more precisely, not the worst of them).
This is not a problem (more precisely, not the worst of them).
Such experiences become a problem when a person cannot keep them inside.
He wonders endlessly: do these jeans really suit him? Is the mascara smudged? Doesn't he look too fat in this dress? Is he doing the right thing? And now? And now? And here he is also not mistaken?
The neurotic physically needs constant encouragement or reassurance from others that he is all right. This is what obsessive-compulsive disorder is.
5. The need to constantly double-check everything
Standard examples are the supposedly left iron or the light on, for which a person can return home two or three times. This also includes the need to pull the door handle a dozen times, even if you just locked the door with a lock and bolt. Or, for example, regularly double-check whether the e-mail has exactly gone to the addressee.
6. Obsessive counting
Trying to focus on something, many count to themselves.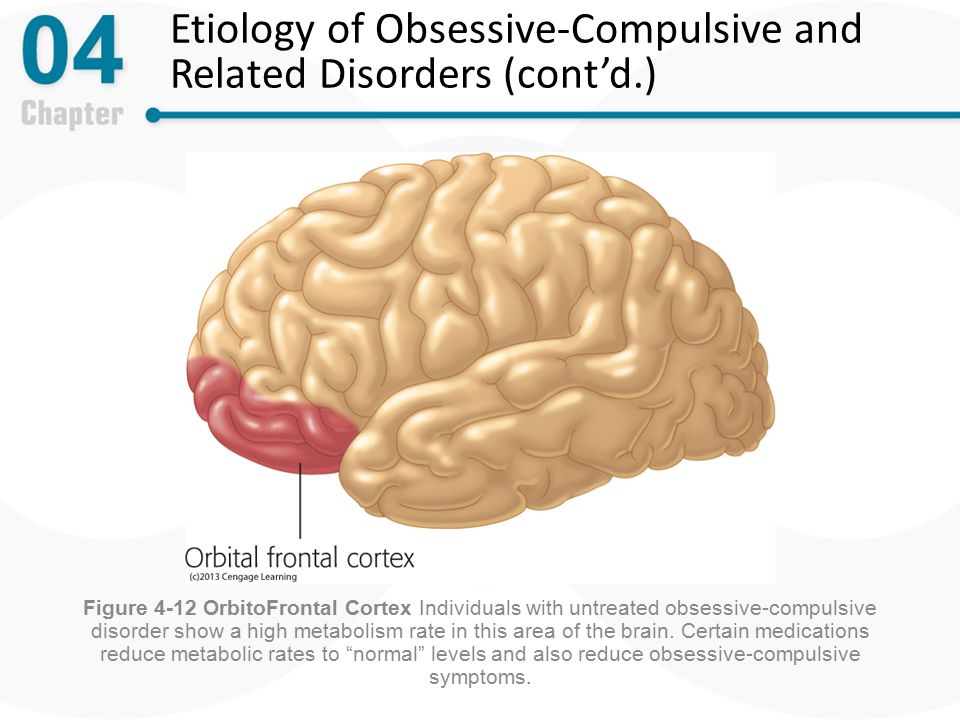 For example, they whisper: "One, two, three - let's go." This is fine.
For example, they whisper: "One, two, three - let's go." This is fine.
But if a person counts the most unexpected things - let's say, the number of trees a tram passes by, or the number of green peas in a brought salad, this is already a reason to be wary. Even worse, if the results of the calculations are disturbing (“There are 13 peas in the salad, the waiter obviously wants to spoil me!”) And they force you to perform some actions (for example, take one pea out of the salad and throw it away). This behavior is already a little beyond normal, yes.
7. Aligning life according to clear rituals
Maybe you arrange your socks in a drawer strictly in the order of the colors of the rainbow. Or at lunch, eat foods in alphabetical order: first drink broth from the soup (the letter “B”), then eat noodles (L), meat (M) and only after that - a boiled egg (I is the last letter of the alphabet). Or go to work the only, strictly defined route. A step to the left, a step to the right - and you already have a panic in half with the certainty that the day will go “wrong”.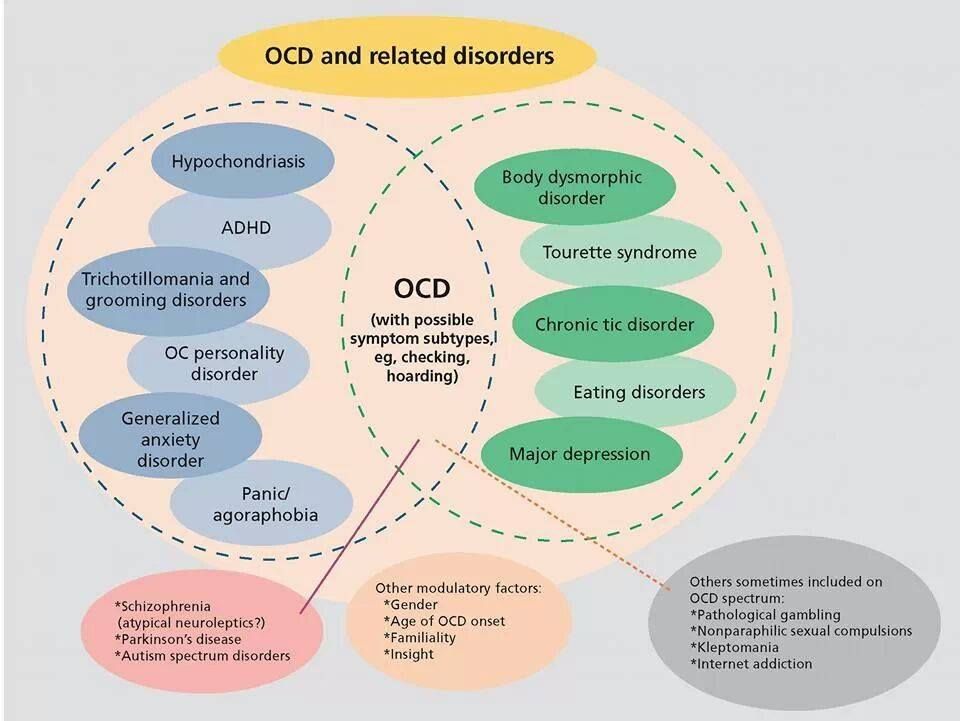
If there is any, even the most harmless ritual in your life, the deviation from which causes anxiety, this may be a sign of OCD.
8. Accumulation of things
Healthy behavior is to get rid of clothes, furniture or appliances that have become obviously unusable.
It is unhealthy to think: “Yes, let it lie down (stay), and suddenly one day it will come in handy.” And do this 100 times, or even 200 times, until the house turns into a warehouse of old things. Uncomfortable, but calm. And it fits perfectly with the symptoms of OCD.
9. Obsession with relationships
Parting with a loved one, quarrel with a friend, conflict with superiors. These are unpleasant, but quite common situations. Everyone has to worry, try to understand what exactly led to the breakup or scandal, everyone has to draw conclusions. But if experiences and self-criticism last for years, you should seek help.
What to do if you suspect obsessive-compulsive disorder
The best option is to see a psychotherapist. The specialist will help you figure out if we are really talking about OCD. Perhaps he will suggest that you take a blood test: sometimes excessive anxiety is a symptom of thyroid disorders, and then you will need to consult an endocrinologist.
The specialist will help you figure out if we are really talking about OCD. Perhaps he will suggest that you take a blood test: sometimes excessive anxiety is a symptom of thyroid disorders, and then you will need to consult an endocrinologist.
Obsessive-compulsive disorder, if confirmed, corrected with psychotherapy. Your doctor may also prescribe antidepressants. All this will help reduce the level of anxiety and get rid of obsessive thoughts and actions.
But one cannot hope for “it will pass by itself”. The fact is that mental disorders tend to increase, worsen with age. And this can lead to very unpleasant consequences. Experts from the American research organization Mayo Clinic name among them:
- contact dermatitis due to excessive handwashing;
- anxiety inability to go to work or other public places;
- difficulties in personal relationships, inability to create or maintain a family;
- general decline in quality of life;
- craving for suicide.

Learn more