Morning a loss
5 Stages of Grief After Facing A Loss
The five stages of grief are denial, anger, bargaining, depression, and acceptance. There’s no order to them and they serve as a reference instead of a guide on how to grieve.
Mourning is an intimate and unique experience for each of us. If you or someone you love are going through a loss, the new emotions may feel overwhelming and confusing.
There are at least five emotions associated with grief. Feeling this way is natural and even necessary.
These emotions are forward steps in the healing journey, even when it doesn’t feel like it at the moment.
Healing from a loss is possible, but it does take time and patience. Even if you’re having a particularly hard time with it, resources like counseling and support groups can help you cope when you’re going through the five stages of grief.
In an effort to better understand the grieving process, many mental health experts and researchers have dedicated years to studying loss and the emotions that come with it.
One of these experts was Elisabeth Kübler-Ross, a Swiss American psychiatrist. She created the Kübler-Ross model, the theory of the five stages of grief and loss.
In her 1969 book, “On Death and Dying,” Kübler-Ross examined the five most common emotional reactions to loss:
- denial
- anger
- bargaining
- depression
- acceptance
Originally, Kübler-Ross referred to them as the “five stages of death.” This was because she was working with terminally ill patients at the time, and these were the common emotions they had regarding their own mortality.
Years after her first book, Kübler-Ross adapted and extended her model to include other kinds of loss. The five stages of death became the five stages of grief.
This grief can come in many forms and for different reasons. Everyone, from all walks of life and across cultures, experiences loss and grief at some point.
Mourning doesn’t come only from dealing with your own death or the death of a loved one. Mourning can also come as a result of an illness, the end of a close relationship, or even the end of a project or dream.
Mourning can also come as a result of an illness, the end of a close relationship, or even the end of a project or dream.
Grief can similarly come from a perceived or real change in your life. For example, moving to a new city, school, or job, transitioning into a new age group, or staying in isolation because of a pandemic.
In other words, there’s no written-in-stone list of “valid” reasons to grieve.
What matters is how you feel. And there are no right or wrong feelings regarding a loss.
Exploring the five stages of grief and loss could help you understand and put into context where you are in your own grieving process and what you feel.
Similarly, if you’re concerned or want to understand someone else’s grieving process, remember that there’s no one way of going through it. Everyone mourns differently.
You could go through many intense emotions, or you could seemingly not react at all. Both responses are valid and not uncommon.
How much time you spend navigating the stages of grief also varies from person to person. It might take you hours, months, or longer to process a loss and heal from it.
It might take you hours, months, or longer to process a loss and heal from it.
You might not experience all these stages of grief or in the order listed above. You could go back and forth from one stage to another.
You may even skip all these emotions and process your loss differently altogether. The five stages of grief are supposed to serve you as a reference, not as a rule.
For some people, this may be the first response to loss.
Denial is a common defense mechanism. It may help you buffer the immediate shock of the hurtful situation.
As an immediate reaction, you might doubt the reality of the loss at first.
A few examples of this type of denial are:
- If you’re facing the death of a loved one, you might find yourself fantasizing someone will call to say there’s been a mistake and nothing really happened.
- If you’re dealing with a breakup, you might convince yourself your partner will soon regret leaving and come back to you.

- If you lost your job, you might feel your former boss will offer you the position back after they realize they’ve made a mistake.
After this first reaction of shock and denial, you may go numb for a while.
At some point, you could feel like nothing matters to you anymore. Life as you once knew it has changed. It might be difficult to feel you can move on.
The first stage of grief is a natural reaction that helps you process the loss in your own time. By going numb, you’re giving yourself time to explore at your own pace the changes you’re going through.
Denial is a temporary response that carries you through the first wave of pain. Eventually, when you’re ready, the feelings and emotions you have denied will resurface, and your healing journey will continue.
Sometimes pain takes other forms. According to Kübler-Ross, pain from a loss is often redirected and expressed as anger.
Feeling intensely angry might surprise you or your loved ones, but it’s not uncommon. This anger serves a purpose.
This anger serves a purpose.
It might be particularly overwhelming for some people to feel anger because, in many cultures, anger is a feared or rejected emotion. You might be more used to avoiding it than confronting it.
During the anger stage of grief, you might start asking questions like “Why me?” or “What did I do to deserve this?”
You could also feel suddenly angry at inanimate objects, strangers, friends, or family members. You might feel angry at life itself.
It’s not rare to also feel anger toward the situation or person you lost. Rationally, you might understand the person isn’t to blame. Emotionally, however, you may resent them for causing you pain or for leaving you.
At some point, you might also feel guilty for being angry. This could make you angrier.
Try reminding yourself that underneath your anger is pain. And even if it might not feel like it, this anger is necessary for healing.
Anger might also be a way to reconnect to the world after isolating yourself from it during the denial stage. When you’re numb, you disconnect from everyone. When you’re angry, you connect, even if through this emotion.
When you’re numb, you disconnect from everyone. When you’re angry, you connect, even if through this emotion.
But anger isn’t the only emotion you might experience during this stage. Irritability, bitterness, anxiety, rage, and impatience are just some other ways you might cope with your loss. It’s all part of the same process.
Bargaining is a stage of grief that helps you hold on to hope in a situation of intense pain.
You might think to yourself that you’re willing to do anything and sacrifice everything if your life is restored to how it was before the loss.
During this internal negotiation, you could find yourself thinking in terms of “what if” or “if only”: what if I did XYZ, then everything will go back to normal; if only I had done something differently to prevent the loss.
Guilt might be an accompanying emotion during this stage as you inadvertently might be trying to regain some control, even if at your own expense.
All these emotions and thoughts aren’t uncommon. As hard as it might feel, this helps you heal as you confront the reality of your loss.
As hard as it might feel, this helps you heal as you confront the reality of your loss.
Just as in all the other stages of grief, depression is experienced in different ways. There’s no right or wrong way to go about it, nor is there a deadline to overcome it.
In this instance, depression isn’t a sign of a mental health condition. Instead, it’s a natural and appropriate response to grief.
During the depression stage, you start facing your present reality and the inevitability of the loss you’ve experienced. Understandably, this realization may lead you to feel intense sadness and despair.
This intense sadness could cause you to feel different in other aspects too. You could feel:
- fatigued
- vulnerable
- confused and distracted
- not wanting to move on
- not hungry or wanting to eat
- not able or willing to get ready in the morning
- not able to enjoy what you once did
This is all typically temporary and a direct response to your grieving process.
As overwhelming as it may feel at this point, this stage is a necessary part of your healing journey.
Reaching acceptance isn’t necessarily about being OK with what happened. Depending on your experience, it might be understandable if you don’t ever feel this way.
Acceptance is more about how you acknowledge the losses you’ve experienced, how you learn to live with them, and how you readjust your life accordingly.
You might feel more comfortable reaching out to friends and family during this stage, but it’s also natural to feel you prefer to withdraw at times.
You may also feel like you accept the loss at times and then move to another stage of grief again. This back-and-forth between stages is natural and a part of the healing process.
In time, you may eventually find yourself stationed at this stage for long periods of time.
That doesn’t mean you’ll never feel sadness or anger again toward your loss, but your long-term perspective about it and how you live with this reality will be different.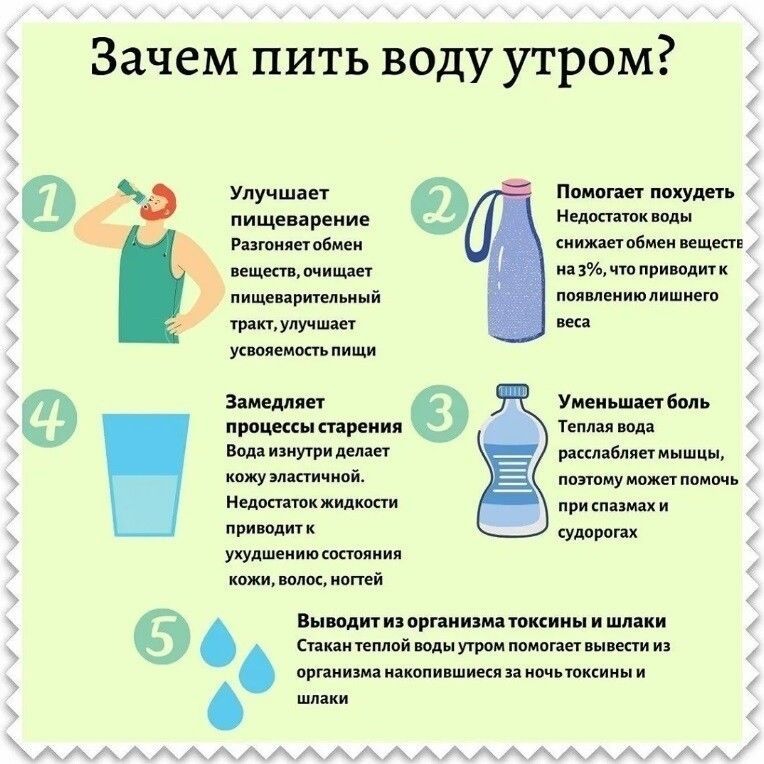
The five stages of grief proposed by Kübler-Ross have served as a framework for many mental health professionals working with the grief process.
Some of these professionals, such as British psychiatrist John Bowlby, have developed their own work around the emotional responses to loss. Others, including Kübler-Ross herself, have adapted and extended the original five-stage model.
This adaptation is usually known as the Kübler-Ross Change Curve. It extends the five core stages of grief to seven overlapping stages:
- Shock. Intense and sometimes paralyzing surprise at the loss.
- Denial. Disbelief and the need to look for evidence to confirm the loss.
- Anger and frustration. A mix between acknowledgment that some things have changed and anger toward this change.
- Depression. Lack of energy and intense sadness.
- Testing. Experimenting with the new situation to discover what it actually means in your life.
- Decision. A rising optimism about learning how to manage the new situation.
- Integration. Acceptance of the new reality, reflection on what you learned, and stepping out in the world as a renewed person.
Because everyone mourns differently and for different reasons, sometimes you might feel your own grieving process isn’t going “according to the norm.”
But remember, there’s no such thing as a right or wrong way of coping with a loss.
These might be some of the thoughts that could cross your mind when looking at your own or someone else’s way of grieving.
1. ‘I am doing it wrong’
One of the most common misconceptions about grieving is that everyone goes through it in the same way.
When it comes to healing from a loss, there’s no correct way of doing it. You might find it useful to remind yourself there’s no “I should be feeling this way.”
Grieving isn’t about going over or following a set list of steps.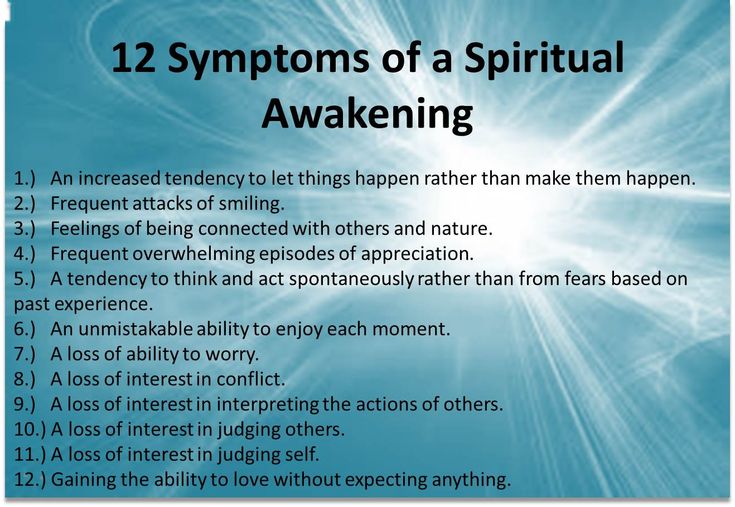 It’s a unique and multidimensional healing journey.
It’s a unique and multidimensional healing journey.
2. ‘I should be feeling…’
Not everyone experiences all the above-mentioned stages or even goes through these emotions the same way.
For example, maybe the depression stage feels more like irritability than sadness for you. And denial could be more of a sense of shock and disbelief than an actual expectation that something out of the blue will fix the loss.
The emotions used to contextualize the stages of grief aren’t the only ones you’ll experience. You might not even experience them at all, and that’s natural too.
This is no indication that your healing journey is faulty in some way. Your healing experience is unique to you and valid nonetheless.
3. ‘This goes first’
Remember, there’s no specific or linear order for the stages of grief.
You could move along the stages one by one, or you could go back and forth. Some days you might feel very sad, and the very next day you could wake up feeling hopeful. Then you could go back to feeling sad. Some days you might even feel both!
Then you could go back to feeling sad. Some days you might even feel both!
In the same way, denial isn’t necessarily the first emotion you’ll experience. Maybe your first emotional reaction is anger or depression.
This is natural and part of the healing process.
4. ‘It’s taking too long’
Coping with a loss is ultimately a deeply personal and singular experience. Many factors affect how long it takes.
Some people navigate through grief in a few days. Others take months or longer to process their loss.
You might find it useful to not set any deadlines to your process.
In grief, you’ll experience some of these emotions in waves of intensity. In time, you’ll notice this intensity decrease.
If you feel your emotions stay or increase in intensity and frequency, this might be a good time to seek professional support.
5. ‘I’m depressed’
Going through the stages of grief, particularly the depression stage, isn’t equivalent to clinical depression. There’s a distinction between having clinical depression and grieving.
There’s a distinction between having clinical depression and grieving.
This means that even though some symptoms might be similar, there are still key differences between both.
For example, in grief, the intense sadness will lessen in intensity and frequency as time goes by. You might even experience this sadness at the same time you find temporary relief in happy memories from times before the loss.
In clinical depression, on the other hand, without the proper treatment, your mood would stay negative or worsen with time. It would likely affect your self-esteem. You may rarely experience feelings of pleasure or happiness.
This doesn’t mean there isn’t a possibility you could develop clinical depression during the grieving process. If your emotions progressively increase in intensity and frequency, reach out for support.
If you’re experiencing intense grief and feel unsure about how to cope with it, reaching out for help can provide comfort and support.
Any reason that’s valid to you is a good reason for reaching out for help.
Other instances in which you might want to seek help processing your loss include the following:
- You need to go back to school or work and have a hard time going about your daily tasks. For example, you’re having trouble concentrating.
- You’re the sole or main guardian or support source for someone else. For example, you’re a single parent or someone else’s caretaker.
- You’re experiencing physical discomfort or pain.
- You’re skipping meals or medications because you don’t feel like getting up or doing anything.
- Your emotions are increasing in intensity and frequency instead of coming in waves or lessening over time.
- You’ve thought about hurting others or yourself.
If you or someone you know is considering self-harm, you’re not alone. Help is available right now:
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Text Line at 741741.
There are a few other ways to reach out for help, depending on what is available to you.
Friends and family
Talking with friends or relatives might give you a sense of relief.
Verbally expressing how you feel can sometimes release some of the inner turmoil you might be experiencing.
Sometimes you might not feel like talking but instead prefer to have silent company.
Expressing your needs to others can allow them to help you in the way you feel is best for your situation.
Support groups
Engaging in support groups can be helpful too. There are local support groups as well as online support groups.
You can connect to others in the group who have gone through or are going through similar losses. They can direct you to further resources as well.
Support groups can also become a safe space where you can express yourself without feeling judged or pressured if you feel that might be the case when talking to somebody else.
Mental health professionals
Grief counseling and therapy are two ways to work with a mental health professional who might support your own process.
If you have insurance, call your insurer to determine whether this grief counseling is covered under your policy and, if so, under which conditions.
If your insurance doesn’t cover counseling sessions, your primary care doctor might be able to offer some support or guidance.
If you don’t have health insurance or aren’t covered for this service, you could try searching for a local organization that provides grief counseling at a low or no charge.
Many national mental health organizations, like the National Alliance on Mental Illness (NAMI), have local or regional chapters. Calling them directly might give you access to some of this information and their specific grief support services.
You’ve taken the first step by just wondering how you can help your loved one.
Here are some ways you can support them now and in the future.
1. Listen
Perhaps one of the main legacies from Elisabeth Kübler-Ross and her work is the importance of listening to the grieving person.
You might have the best intentions and want to provide comforting words. But in some instances, the best support comes from just being there and making it clear that you’re available to listen to whatever — and whenever — they want to share.
It’s also important to accept it if your loved one doesn’t want to talk with you. Give them time and space.
2. Reach out
Not everyone knows how to comfort others. It might be intimidating or overwhelming seeing someone you care about have a rough time.
But don’t let these fears stop you from offering help or from being there. Lead with empathy, and the rest will follow.
3. Be practical
Look for ways to ease the weight off your loved one’s shoulders. Explore the areas they might need help managing while they process their loss.
This could mean helping with food preparation or grocery shopping, organizing their room or house, or picking up their children from school.
4. Don’t assume
You might want to verbally offer your support and be attentive to whatever they tell you might help them feel better. But avoid assuming or guessing “which step” of the process they’re going through at the moment.
But avoid assuming or guessing “which step” of the process they’re going through at the moment.
A smiley face or no tears don’t necessarily mean they’re not grieving. A change in their physical appearance doesn’t mean they’re depressed.
Wait for them to express how they feel, if they’re ready, and go from there.
5. Search for resources
You might have the clarity of mind and the energy to browse local support groups and organizations, call an insurance company, and find a mental health professional.
The decision of reaching out for this kind of help is, of course, entirely up to the grieving person. But having the information at hand might save time whenever they’re prepared or willing to take it.
Some resources you might find helpful are:
- GriefShare support groups
- The Compassionate Friends: Supporting Family After a Child Dies
- American Psychological Association: Search for a Psychologist
- Helping Kids Grieve: Toolkit
5 Stages of Grief After Facing A Loss
The five stages of grief are denial, anger, bargaining, depression, and acceptance. There’s no order to them and they serve as a reference instead of a guide on how to grieve.
There’s no order to them and they serve as a reference instead of a guide on how to grieve.
Mourning is an intimate and unique experience for each of us. If you or someone you love are going through a loss, the new emotions may feel overwhelming and confusing.
There are at least five emotions associated with grief. Feeling this way is natural and even necessary.
These emotions are forward steps in the healing journey, even when it doesn’t feel like it at the moment.
Healing from a loss is possible, but it does take time and patience. Even if you’re having a particularly hard time with it, resources like counseling and support groups can help you cope when you’re going through the five stages of grief.
In an effort to better understand the grieving process, many mental health experts and researchers have dedicated years to studying loss and the emotions that come with it.
One of these experts was Elisabeth Kübler-Ross, a Swiss American psychiatrist. She created the Kübler-Ross model, the theory of the five stages of grief and loss.
She created the Kübler-Ross model, the theory of the five stages of grief and loss.
In her 1969 book, “On Death and Dying,” Kübler-Ross examined the five most common emotional reactions to loss:
- denial
- anger
- bargaining
- depression
- acceptance
Originally, Kübler-Ross referred to them as the “five stages of death.” This was because she was working with terminally ill patients at the time, and these were the common emotions they had regarding their own mortality.
Years after her first book, Kübler-Ross adapted and extended her model to include other kinds of loss. The five stages of death became the five stages of grief.
This grief can come in many forms and for different reasons. Everyone, from all walks of life and across cultures, experiences loss and grief at some point.
Mourning doesn’t come only from dealing with your own death or the death of a loved one. Mourning can also come as a result of an illness, the end of a close relationship, or even the end of a project or dream.
Grief can similarly come from a perceived or real change in your life. For example, moving to a new city, school, or job, transitioning into a new age group, or staying in isolation because of a pandemic.
In other words, there’s no written-in-stone list of “valid” reasons to grieve.
What matters is how you feel. And there are no right or wrong feelings regarding a loss.
Exploring the five stages of grief and loss could help you understand and put into context where you are in your own grieving process and what you feel.
Similarly, if you’re concerned or want to understand someone else’s grieving process, remember that there’s no one way of going through it. Everyone mourns differently.
You could go through many intense emotions, or you could seemingly not react at all. Both responses are valid and not uncommon.
How much time you spend navigating the stages of grief also varies from person to person. It might take you hours, months, or longer to process a loss and heal from it.
You might not experience all these stages of grief or in the order listed above. You could go back and forth from one stage to another.
You may even skip all these emotions and process your loss differently altogether. The five stages of grief are supposed to serve you as a reference, not as a rule.
For some people, this may be the first response to loss.
Denial is a common defense mechanism. It may help you buffer the immediate shock of the hurtful situation.
As an immediate reaction, you might doubt the reality of the loss at first.
A few examples of this type of denial are:
- If you’re facing the death of a loved one, you might find yourself fantasizing someone will call to say there’s been a mistake and nothing really happened.
- If you’re dealing with a breakup, you might convince yourself your partner will soon regret leaving and come back to you.
- If you lost your job, you might feel your former boss will offer you the position back after they realize they’ve made a mistake.
After this first reaction of shock and denial, you may go numb for a while.
At some point, you could feel like nothing matters to you anymore. Life as you once knew it has changed. It might be difficult to feel you can move on.
The first stage of grief is a natural reaction that helps you process the loss in your own time. By going numb, you’re giving yourself time to explore at your own pace the changes you’re going through.
Denial is a temporary response that carries you through the first wave of pain. Eventually, when you’re ready, the feelings and emotions you have denied will resurface, and your healing journey will continue.
Sometimes pain takes other forms. According to Kübler-Ross, pain from a loss is often redirected and expressed as anger.
Feeling intensely angry might surprise you or your loved ones, but it’s not uncommon. This anger serves a purpose.
It might be particularly overwhelming for some people to feel anger because, in many cultures, anger is a feared or rejected emotion. You might be more used to avoiding it than confronting it.
You might be more used to avoiding it than confronting it.
During the anger stage of grief, you might start asking questions like “Why me?” or “What did I do to deserve this?”
You could also feel suddenly angry at inanimate objects, strangers, friends, or family members. You might feel angry at life itself.
It’s not rare to also feel anger toward the situation or person you lost. Rationally, you might understand the person isn’t to blame. Emotionally, however, you may resent them for causing you pain or for leaving you.
At some point, you might also feel guilty for being angry. This could make you angrier.
Try reminding yourself that underneath your anger is pain. And even if it might not feel like it, this anger is necessary for healing.
Anger might also be a way to reconnect to the world after isolating yourself from it during the denial stage. When you’re numb, you disconnect from everyone. When you’re angry, you connect, even if through this emotion.
But anger isn’t the only emotion you might experience during this stage. Irritability, bitterness, anxiety, rage, and impatience are just some other ways you might cope with your loss. It’s all part of the same process.
Bargaining is a stage of grief that helps you hold on to hope in a situation of intense pain.
You might think to yourself that you’re willing to do anything and sacrifice everything if your life is restored to how it was before the loss.
During this internal negotiation, you could find yourself thinking in terms of “what if” or “if only”: what if I did XYZ, then everything will go back to normal; if only I had done something differently to prevent the loss.
Guilt might be an accompanying emotion during this stage as you inadvertently might be trying to regain some control, even if at your own expense.
All these emotions and thoughts aren’t uncommon. As hard as it might feel, this helps you heal as you confront the reality of your loss.
Just as in all the other stages of grief, depression is experienced in different ways. There’s no right or wrong way to go about it, nor is there a deadline to overcome it.
In this instance, depression isn’t a sign of a mental health condition. Instead, it’s a natural and appropriate response to grief.
During the depression stage, you start facing your present reality and the inevitability of the loss you’ve experienced. Understandably, this realization may lead you to feel intense sadness and despair.
This intense sadness could cause you to feel different in other aspects too. You could feel:
- fatigued
- vulnerable
- confused and distracted
- not wanting to move on
- not hungry or wanting to eat
- not able or willing to get ready in the morning
- not able to enjoy what you once did
This is all typically temporary and a direct response to your grieving process.
As overwhelming as it may feel at this point, this stage is a necessary part of your healing journey.
Reaching acceptance isn’t necessarily about being OK with what happened. Depending on your experience, it might be understandable if you don’t ever feel this way.
Acceptance is more about how you acknowledge the losses you’ve experienced, how you learn to live with them, and how you readjust your life accordingly.
You might feel more comfortable reaching out to friends and family during this stage, but it’s also natural to feel you prefer to withdraw at times.
You may also feel like you accept the loss at times and then move to another stage of grief again. This back-and-forth between stages is natural and a part of the healing process.
In time, you may eventually find yourself stationed at this stage for long periods of time.
That doesn’t mean you’ll never feel sadness or anger again toward your loss, but your long-term perspective about it and how you live with this reality will be different.
The five stages of grief proposed by Kübler-Ross have served as a framework for many mental health professionals working with the grief process.
Some of these professionals, such as British psychiatrist John Bowlby, have developed their own work around the emotional responses to loss. Others, including Kübler-Ross herself, have adapted and extended the original five-stage model.
This adaptation is usually known as the Kübler-Ross Change Curve. It extends the five core stages of grief to seven overlapping stages:
- Shock. Intense and sometimes paralyzing surprise at the loss.
- Denial. Disbelief and the need to look for evidence to confirm the loss.
- Anger and frustration. A mix between acknowledgment that some things have changed and anger toward this change.
- Depression. Lack of energy and intense sadness.
- Testing. Experimenting with the new situation to discover what it actually means in your life.
- Decision. A rising optimism about learning how to manage the new situation.
- Integration. Acceptance of the new reality, reflection on what you learned, and stepping out in the world as a renewed person.
Because everyone mourns differently and for different reasons, sometimes you might feel your own grieving process isn’t going “according to the norm.”
But remember, there’s no such thing as a right or wrong way of coping with a loss.
These might be some of the thoughts that could cross your mind when looking at your own or someone else’s way of grieving.
1. ‘I am doing it wrong’
One of the most common misconceptions about grieving is that everyone goes through it in the same way.
When it comes to healing from a loss, there’s no correct way of doing it. You might find it useful to remind yourself there’s no “I should be feeling this way.”
Grieving isn’t about going over or following a set list of steps. It’s a unique and multidimensional healing journey.
2. ‘I should be feeling…’
Not everyone experiences all the above-mentioned stages or even goes through these emotions the same way.
For example, maybe the depression stage feels more like irritability than sadness for you. And denial could be more of a sense of shock and disbelief than an actual expectation that something out of the blue will fix the loss.
The emotions used to contextualize the stages of grief aren’t the only ones you’ll experience. You might not even experience them at all, and that’s natural too.
This is no indication that your healing journey is faulty in some way. Your healing experience is unique to you and valid nonetheless.
3. ‘This goes first’
Remember, there’s no specific or linear order for the stages of grief.
You could move along the stages one by one, or you could go back and forth. Some days you might feel very sad, and the very next day you could wake up feeling hopeful. Then you could go back to feeling sad. Some days you might even feel both!
In the same way, denial isn’t necessarily the first emotion you’ll experience. Maybe your first emotional reaction is anger or depression.
This is natural and part of the healing process.
4. ‘It’s taking too long’
Coping with a loss is ultimately a deeply personal and singular experience. Many factors affect how long it takes.
Some people navigate through grief in a few days. Others take months or longer to process their loss.
You might find it useful to not set any deadlines to your process.
In grief, you’ll experience some of these emotions in waves of intensity. In time, you’ll notice this intensity decrease.
If you feel your emotions stay or increase in intensity and frequency, this might be a good time to seek professional support.
5. ‘I’m depressed’
Going through the stages of grief, particularly the depression stage, isn’t equivalent to clinical depression. There’s a distinction between having clinical depression and grieving.
This means that even though some symptoms might be similar, there are still key differences between both.
For example, in grief, the intense sadness will lessen in intensity and frequency as time goes by. You might even experience this sadness at the same time you find temporary relief in happy memories from times before the loss.
You might even experience this sadness at the same time you find temporary relief in happy memories from times before the loss.
In clinical depression, on the other hand, without the proper treatment, your mood would stay negative or worsen with time. It would likely affect your self-esteem. You may rarely experience feelings of pleasure or happiness.
This doesn’t mean there isn’t a possibility you could develop clinical depression during the grieving process. If your emotions progressively increase in intensity and frequency, reach out for support.
If you’re experiencing intense grief and feel unsure about how to cope with it, reaching out for help can provide comfort and support.
Any reason that’s valid to you is a good reason for reaching out for help.
Other instances in which you might want to seek help processing your loss include the following:
- You need to go back to school or work and have a hard time going about your daily tasks. For example, you’re having trouble concentrating.

- You’re the sole or main guardian or support source for someone else. For example, you’re a single parent or someone else’s caretaker.
- You’re experiencing physical discomfort or pain.
- You’re skipping meals or medications because you don’t feel like getting up or doing anything.
- Your emotions are increasing in intensity and frequency instead of coming in waves or lessening over time.
- You’ve thought about hurting others or yourself.
If you or someone you know is considering self-harm, you’re not alone. Help is available right now:
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Text Line at 741741.
There are a few other ways to reach out for help, depending on what is available to you.
Friends and family
Talking with friends or relatives might give you a sense of relief.
Verbally expressing how you feel can sometimes release some of the inner turmoil you might be experiencing.
Sometimes you might not feel like talking but instead prefer to have silent company.
Expressing your needs to others can allow them to help you in the way you feel is best for your situation.
Support groups
Engaging in support groups can be helpful too. There are local support groups as well as online support groups.
You can connect to others in the group who have gone through or are going through similar losses. They can direct you to further resources as well.
Support groups can also become a safe space where you can express yourself without feeling judged or pressured if you feel that might be the case when talking to somebody else.
Mental health professionals
Grief counseling and therapy are two ways to work with a mental health professional who might support your own process.
If you have insurance, call your insurer to determine whether this grief counseling is covered under your policy and, if so, under which conditions.
If your insurance doesn’t cover counseling sessions, your primary care doctor might be able to offer some support or guidance.
If you don’t have health insurance or aren’t covered for this service, you could try searching for a local organization that provides grief counseling at a low or no charge.
Many national mental health organizations, like the National Alliance on Mental Illness (NAMI), have local or regional chapters. Calling them directly might give you access to some of this information and their specific grief support services.
You’ve taken the first step by just wondering how you can help your loved one.
Here are some ways you can support them now and in the future.
1. Listen
Perhaps one of the main legacies from Elisabeth Kübler-Ross and her work is the importance of listening to the grieving person.
You might have the best intentions and want to provide comforting words. But in some instances, the best support comes from just being there and making it clear that you’re available to listen to whatever — and whenever — they want to share.
It’s also important to accept it if your loved one doesn’t want to talk with you. Give them time and space.
2. Reach out
Not everyone knows how to comfort others. It might be intimidating or overwhelming seeing someone you care about have a rough time.
But don’t let these fears stop you from offering help or from being there. Lead with empathy, and the rest will follow.
3. Be practical
Look for ways to ease the weight off your loved one’s shoulders. Explore the areas they might need help managing while they process their loss.
This could mean helping with food preparation or grocery shopping, organizing their room or house, or picking up their children from school.
4. Don’t assume
You might want to verbally offer your support and be attentive to whatever they tell you might help them feel better. But avoid assuming or guessing “which step” of the process they’re going through at the moment.
A smiley face or no tears don’t necessarily mean they’re not grieving. A change in their physical appearance doesn’t mean they’re depressed.
A change in their physical appearance doesn’t mean they’re depressed.
Wait for them to express how they feel, if they’re ready, and go from there.
5. Search for resources
You might have the clarity of mind and the energy to browse local support groups and organizations, call an insurance company, and find a mental health professional.
The decision of reaching out for this kind of help is, of course, entirely up to the grieving person. But having the information at hand might save time whenever they’re prepared or willing to take it.
Some resources you might find helpful are:
- GriefShare support groups
- The Compassionate Friends: Supporting Family After a Child Dies
- American Psychological Association: Search for a Psychologist
- Helping Kids Grieve: Toolkit
Fundamental Guide to Know
Our brains use different structures to deal with existing types of memory. There are two main types of memory: short-term memory and long-term memory. Although dysfunctions of both types of memory are possible, we will focus on Long-Term Declarative Memory.
Although dysfunctions of both types of memory are possible, we will focus on Long-Term Declarative Memory.
- Short-term memory stores a limited amount of information for a short period of time.
- Long-term memory stores a large amount of complex information for a long time. This is what is usually called "memory". In turn, there are two types of Long-term memory: Non-declarative or Implicit Memory (cycling, driving) and Declarative or Explicit memory, used to remember our personal experience or knowledge about the world (what is the name of my relative, where I left clues as to who is in charge of my country, what happened five minutes or five months ago).
What is memory loss and symptoms
When we forget something, we usually don't "lose" the memory itself, but our brain "can't find the way" to what we're trying to remember. This "pathological" loss of memory is called amnesia. Here are some symptoms of memory loss:
- Often lose personal items.

- It's hard to find the right words.
- Asking repeated questions in a conversation or telling the same story over and over.
- Forgetting whether or not you have done something, such as taking medicine.
- Become disoriented or lost in familiar places.
- Confuse year or day of the week.
- Forget about meetings or events.
- Having difficulty making decisions or following instructions.
Types of memory loss: Transient and Permanent
Memory loss can manifest itself in two forms: temporary (transient) and permanent (permanent) memory loss.
- Transient or temporary memory loss is a temporary forgetting of information that is restored in our memory after a while. If we cannot remember the name but then remember it an hour later, or if we wake up in the morning and cannot remember what happened the night before after drinking alcohol, this is considered a temporary memory loss.
- Permanent or permanent memory loss is information that we lose and cannot recover. If we fail to remember, even if we are reminded of it by the other person where we left the keys to the house, or if we forget about the meeting with the brother made the night before, we are dealing with permanent memory loss.
Causes of memory loss: medical, emotional and age-related problems
There are several factors that can lead to involuntary memory loss in both young and old age. Many of these factors are not due to poor memory performance, but due to the interference of other cognitive abilities (such as attention) or certain substances (such as drugs).
- Memory loss due to health problems which, in most cases, are treatable: side effects of certain medications, an unbalanced diet with a reduced content of vitamins B6, B9 and B12 can lead to temporary memory loss, alcohol abuse, thyroid, kidney or liver diseases, lack of oxygen in the brain (as stroke), the effects of traumatic brain injury (head trauma), cancer treatment (chemotherapy or radiation therapy), brain tumors or infections, emotional problems (such as depression), and anxiety (such as post-traumatic stress).
- Loss of memory due to stress, anxiety and other emotional problems : In addition, stress, anxiety and some of the consequences of strong emotions such as anger can cause forgetfulness. If we're in a car accident, stress can make us lose our memories of what happened that morning. But typically, these memory losses occur because we focus on threatening stimuli and remove less meaning from our surroundings. Thus, we can remember what caused us these strong emotions, but we cannot recall all the events that occurred during this time. This occurs in the case of Post Traumatic Stress Disorder and Obsessive-Compulsive Disorder. In these disorders, the person is so focused on the emotional episode or object of obsession that he ultimately does not remember anything except for this stimulus.
- Memory loss with age and normal aging : Although forgetfulness and memory disorders do not occur exclusively in older people, it is true that these people are more susceptible to such problems.
 With age, the ability to learn and the quality of memory can deteriorate even without the presence of any pathology. However, when these problems become more severe than usual, we may speak of mild cognitive impairment or, in more severe impairments, dementia.
With age, the ability to learn and the quality of memory can deteriorate even without the presence of any pathology. However, when these problems become more severe than usual, we may speak of mild cognitive impairment or, in more severe impairments, dementia. - Memory loss due to emotional problems in the elderly: It is common for older people to feel lonely when they lose loved ones or not feel useful when they retire. Given these changes, it is normal that some of the older people suffer from emotional disorders such as depression. Depressed older adults may experience feelings of memory loss more often and confuse these symptoms with Alzheimer's disease or other memory problems. Depression can cause serious memory problems in both the elderly and young people, but in the case of older patients, it is very important to conduct an appropriate differential diagnosis in order to rule out the presence of Alzheimer's disease. Although memory problems in people with depression may not be as relevant as in other pathologies, it is necessary to pay attention to the emotional problems that they suffer from.

- Mild cognitive impairment memory loss: Mild cognitive impairment is a disorder that results in memory loss but does not interfere with the person suffering from it in their daily activities. Some research indicates that mild cognitive impairment may be an early sign of Alzheimer's disease, although these impairments do not lead to Alzheimer's disease in all cases.
- Memory loss due to dementia is one of the most important health problems affecting the elderly, but it is not a normal consequence of aging. Dementia usually involves the onset of chronic cognitive problems such as problems with memory, speech, behavior, etc. There are various types of dementia, but the most common form is Alzheimer's disease.
- Memory loss caused by Alzheimer's disease In this disease, a protein called "beta-amyloid" accumulates in neurons, forming senile plaques, until these neurons lose their vitality. This leads to a gradual and severe deterioration in memory, problems with orientation (patients often do not know what day it is and where they are), difficulties in calculations and, in general, with the performance of daily tasks.
 The severity of the disease varies depending on the stage at which the patient is. In the mild stage, a person with Alzheimer's disease may show significant memory loss, become lost in a familiar place, withdraw from routine activities and conversations, forget dates, and exhibit symptoms of depression and hostility. In the moderate stage, cases of memory loss are most prominent, sufferers may forget names or things that happened a few minutes ago, have difficulty shopping or preparing food, may neglect personal hygiene, have speech problems or show aggression, tend to forget their way, and eventually, their daily life becomes impossible without outside help. In the advanced stage, patients may have problems with eating or understanding simple information, they do not recognize relatives and friends, and behave inappropriately in public. At this stage, the person becomes completely dependent.
The severity of the disease varies depending on the stage at which the patient is. In the mild stage, a person with Alzheimer's disease may show significant memory loss, become lost in a familiar place, withdraw from routine activities and conversations, forget dates, and exhibit symptoms of depression and hostility. In the moderate stage, cases of memory loss are most prominent, sufferers may forget names or things that happened a few minutes ago, have difficulty shopping or preparing food, may neglect personal hygiene, have speech problems or show aggression, tend to forget their way, and eventually, their daily life becomes impossible without outside help. In the advanced stage, patients may have problems with eating or understanding simple information, they do not recognize relatives and friends, and behave inappropriately in public. At this stage, the person becomes completely dependent.
Prevention of memory loss
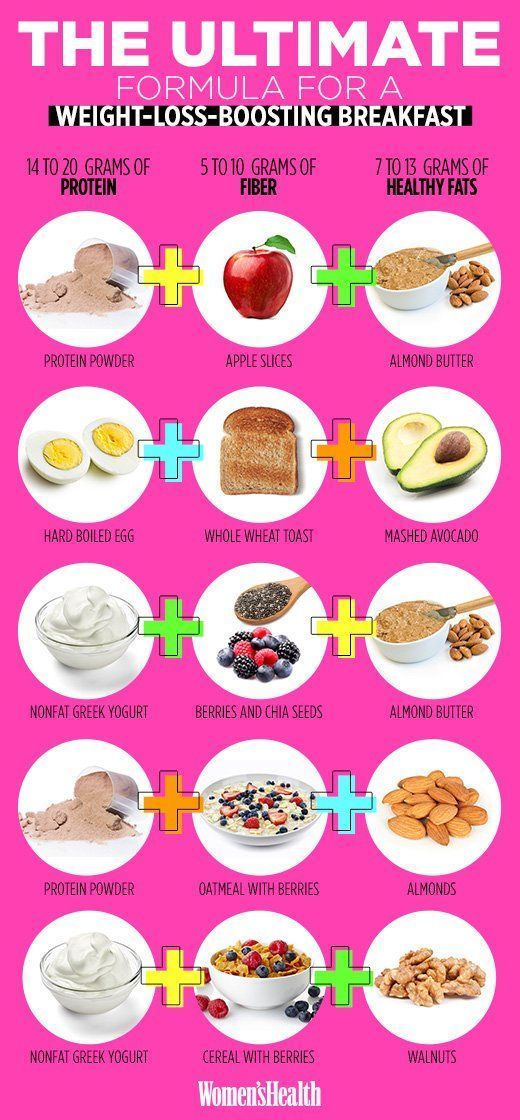
How to prevent memory loss? Factors that have been shown to be most effective in preventing or slowing the progress of Alzheimer's and other memory problems are healthy sleep , proper nutrition , exercise , an active social life and cognitive activity . Our brain functions like a muscle: the more actively we use it, the better its condition will be. Conversely, if our brain is not getting enough nutrition and oxygen through exercise, and if we do not apply our social and cognitive abilities, there will be a tendency to atrophy. For this reason, an active and healthy lifestyle can be very beneficial for our memory. CogniFit offers a wide range of scientifically proven exercises to keep your brain active and improve your cognitive abilities. In addition, cognitive activity not only strengthens memory in adults and the elderly, but can also contribute to the development of intellectual abilities in children and young people.
Our brain functions like a muscle: the more actively we use it, the better its condition will be. Conversely, if our brain is not getting enough nutrition and oxygen through exercise, and if we do not apply our social and cognitive abilities, there will be a tendency to atrophy. For this reason, an active and healthy lifestyle can be very beneficial for our memory. CogniFit offers a wide range of scientifically proven exercises to keep your brain active and improve your cognitive abilities. In addition, cognitive activity not only strengthens memory in adults and the elderly, but can also contribute to the development of intellectual abilities in children and young people.
Cognitive Stimulation allows you to stimulate, train and strengthen various cognitive abilities such as attention, perception, memory, speech and executive functions. These are precisely the abilities that can be impaired in dementia and other diseases associated with memory loss. By doing exercises that involve various cognitive abilities, we help the brain to strengthen neural connections, preventing damage to it. However, cognitive stimulation cannot be random, it needs to be applied with reliable techniques and detailed organization, according to the needs of each patient. CogniFit focuses on personalizing your exercise program to maximize your workouts and help prevent cognitive problems.
By doing exercises that involve various cognitive abilities, we help the brain to strengthen neural connections, preventing damage to it. However, cognitive stimulation cannot be random, it needs to be applied with reliable techniques and detailed organization, according to the needs of each patient. CogniFit focuses on personalizing your exercise program to maximize your workouts and help prevent cognitive problems.
In addition, proper sleep patterns and frequent reading help keep your memory in good condition. Of course, it is necessary to give up bad habits associated with the use of alcohol, tobacco or other drugs - this will help strengthen both memory and overall health.
When should you seek help? Detect and evaluate memory problems
It is very common for people with memory problems to be unaware of their existence, so these problems are usually first discovered by their relatives.
On the other hand, people prone to anxiety and depression can dwell on their mistakes. Often they overestimate their forgetfulness, thinking that they have memory problems, but this is far from always the case. If we sometimes suddenly forget the name of an object or the name of a person with whom we usually communicate a lot, or forget why we went to the room or where we left the keys, or forget to take lunch to work - this is not a cause for concern.
Often they overestimate their forgetfulness, thinking that they have memory problems, but this is far from always the case. If we sometimes suddenly forget the name of an object or the name of a person with whom we usually communicate a lot, or forget why we went to the room or where we left the keys, or forget to take lunch to work - this is not a cause for concern.
However, if the person is having trouble doing daily tasks, or if they seem confused and disoriented, it is time to see a doctor. It is recommended to write down all the information about the course of the impairment: when did the memory problems start, what kind of deterioration was observed, what type of information is forgotten, how it affects daily, social and work life. The attending physician must make an accurate diagnosis and determine whether the patient has memory problems, and if so, what kind of problems they are. When in doubt, it is always best to consult a specialist.
However, short-term episodes of memory loss do not mean that we are talking about serious memory problems, not to mention Alzheimer's disease. We all forget something from time to time, and this is normal (mild memory loss). Our brain has to forget something in order to process new information correctly.
We all forget something from time to time, and this is normal (mild memory loss). Our brain has to forget something in order to process new information correctly.
How to treat or reduce memory loss?
Treatment of dementia should be carried out from a multidisciplinary point of view. Depending on 9 the type of disease, the phase in which the patient is, and the specific characteristics of the patient, the involvement of a neurologist, family doctor, internist, geriatrician, psychologist, neuropsychologist, speech therapist, physiotherapist, occupational therapist and nursing staff may be required .
In the case of Alzheimer's disease, the attending physician must develop an appropriate diagnosis and treatment. In addition, exercises for cognitive stimulation of the brain of patients with Alzheimer's disease at an early stage can be included in the treatment program. In more advanced stages, as a rule, other types of treatment are used, including medication. Despite the fact that Alzheimer's disease is currently considered incurable, these drugs are aimed at maintaining the patient's impaired abilities and behavioral problems associated with this disease.
In more advanced stages, as a rule, other types of treatment are used, including medication. Despite the fact that Alzheimer's disease is currently considered incurable, these drugs are aimed at maintaining the patient's impaired abilities and behavioral problems associated with this disease.
In addition, taking preventive measures can help slow the progression of dementia once the diagnosis is made. Combining drug treatment with proper diet, exercise, social life and cognitive stimulation helps to minimize the effects of dementia in the patient's daily life.
What if a family member has memory loss?
In case of undiagnosed memory problems with a friend of yours, you should recommend 0006 contact specialist . It is normal to receive a rejection of offered care, as many patients are not aware of their problems. Therefore, one should approach this issue with patience and caution .
Once the doctor has made a diagnosis, follow his instructions. If this is a mild stage of the disease, we should help this person to carry out daily tasks both at home and socially. One of the main problems of Alzheimer's disease is temporary disorientation, so it is important to place clocks and calendars in the patient's field of vision. Despite the fact that the disease interferes with the learning process, it is strongly recommended to accustom the patient to use a diary and not reduce the usual volume of tasks. Close people should help him follow the doctor's recommendations, take the pills correctly and carry out the activities associated with the treatment. It can be very difficult for a patient to accept their diagnosis. Therefore, it is very important to him emotional support for loved ones, so that the situation is not perceived so painfully. If symptoms of depression are found, a doctor or psychologist should be informed as soon as possible.
In conclusion:
- Forgetfulness does not mean the presence of memory problems.
- It is important to be able to distinguish between the signs of Mild Cognitive Impairment and dementia, such as in Alzheimer's disease, in order to detect them as soon as possible and seek professional help. However, not all memory problems are associated with these disorders, however, they also require medical attention.
- The impact of Mild Cognitive Impairment and dementia can be reduced through proper nutrition, exercise, adequate rest, socialization and cognitive stimulation.
Fainting, sudden loss of consciousness, syncope - causes, examination and treatment in Astrakhan| Symptoms
Heart valve disease and cardiomyopathy (aortic stenosis, mitral stenosis or prosthetic valve dysfunction, hypertrophic cardiomyopathy)
Signs: Fainting during or after exercise and then rapid recovery. In young or old people. Often in patients with known heart murmurs.
In young or old people. Often in patients with known heart murmurs.
Irregular heart rhythm (slow or fast)
Signs: Fainting without warning and then recovering immediately after waking up can occur in any position. Sometimes in patients taking certain medications, especially heart medications (antiarrhythmic drugs).
Pulmonary embolism (blood clot block)
Signs: Often sharp pain when breathing, shortness of breath, rapid breathing and rapid heartbeat. Sometimes a slight fever, coughing up blood, or shock. More likely in patients with risk factors for pulmonary embolism (history of blood clots, recent surgery, leg surgery, prolonged bed rest, leg cast or splint, older age, smoking, or cancer).
Myocardial infarction
Signs: Usually in the elderly. Sometimes chest discomfort, heartburn, shortness of breath, or nausea.
Severe allergic reaction (anaphylactic shock)
Signs: Fainting during or shortly after exposure to an allergen, such as after taking a medication or being bitten by an insect. Excessive sweating and pale skin color. In patients with or without a history of allergies. Usually urticaria, shortness of breath, or localized edema (angioneurotic edema).
Excessive sweating and pale skin color. In patients with or without a history of allergies. Usually urticaria, shortness of breath, or localized edema (angioneurotic edema).
Low blood sugar (hypoglycemia)
Signs: Fainting after other symptoms develop, such as confusion, trembling, and sweating. Lack of response or confusion that does not resolve until specific treatment is given. Almost always in people with diabetes.
Increased chest pressure (due to coughing or straining to urinate or defecate)
Signs: Fainting during activities that increase chest pressure. Predictive symptoms (dizziness, nausea, or sweating). Recovery is quick, but the person may feel unwell for several hours).
Strong emotion (pain, fear or stress from the sight of blood)
Signs: Fainting at the peak of strong emotions. Predictive symptoms (dizziness, nausea, or sweating). Recovery is quick and the cause is usually obvious.
Migraine
Signs: Fainting is sometimes preceded by disturbances in sensation, vision or other functions (aura), increased sensitivity to light.
Standing for long periods of time
Signs: Cause evident from history. No other symptoms.
Pregnancy
Signs: In healthy women of childbearing age. No other symptoms. Usually in women with early pregnancy or unrecognized pregnancy.
Hyperventilation
Signs: Frequent tingling around the mouth or in the fingers to the point of fainting. Usually during or in response to a situation of emotional stress. Rapid breathing, which may go unnoticed by the patient or others. Usually in younger people.
Blood pressure medications
Signs: Dizziness and then fainting after a few minutes of sitting or standing. The drop in blood pressure in the standing position, revealed during the examination.
Drugs that may cause irregular or accelerated heart rhythm
Signs: Sometimes palpitations and fainting. Sudden loss of consciousness.
Dysfunction of the autonomic nervous system
Signs: Dizziness and then fainting after a few minutes of sitting or standing.