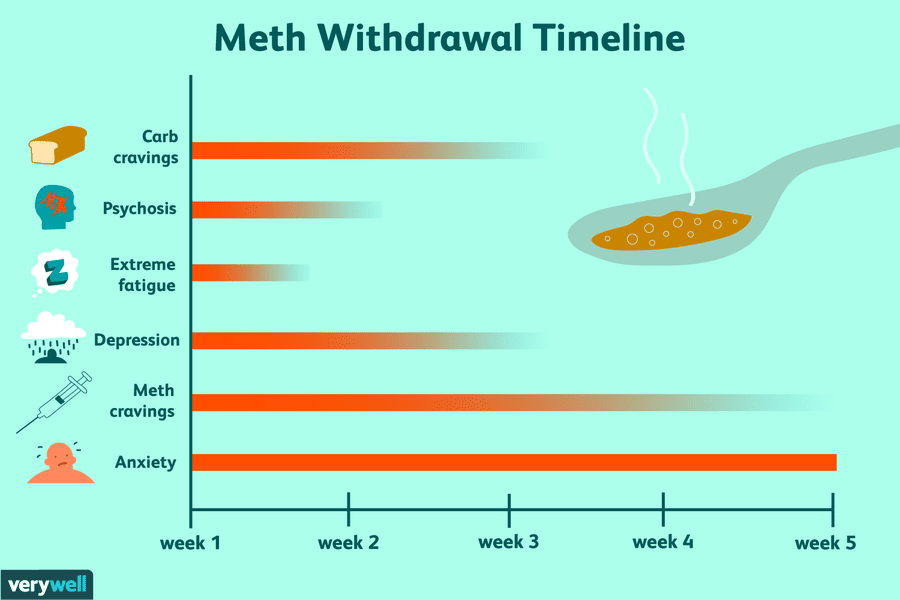
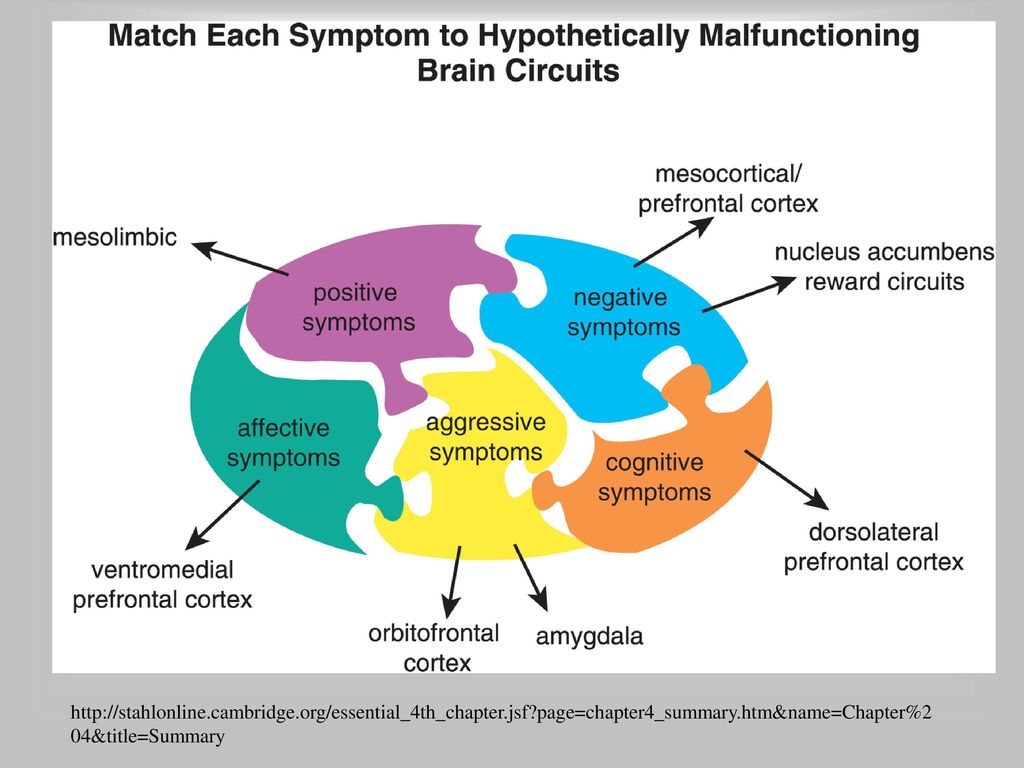
Meth psychosis symptoms
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.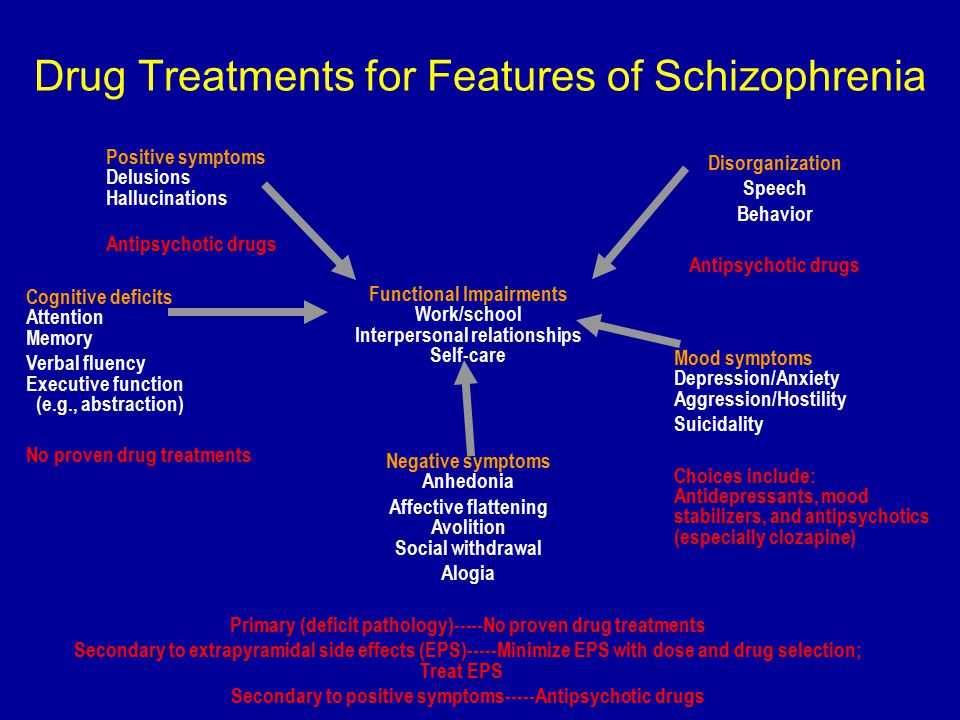 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.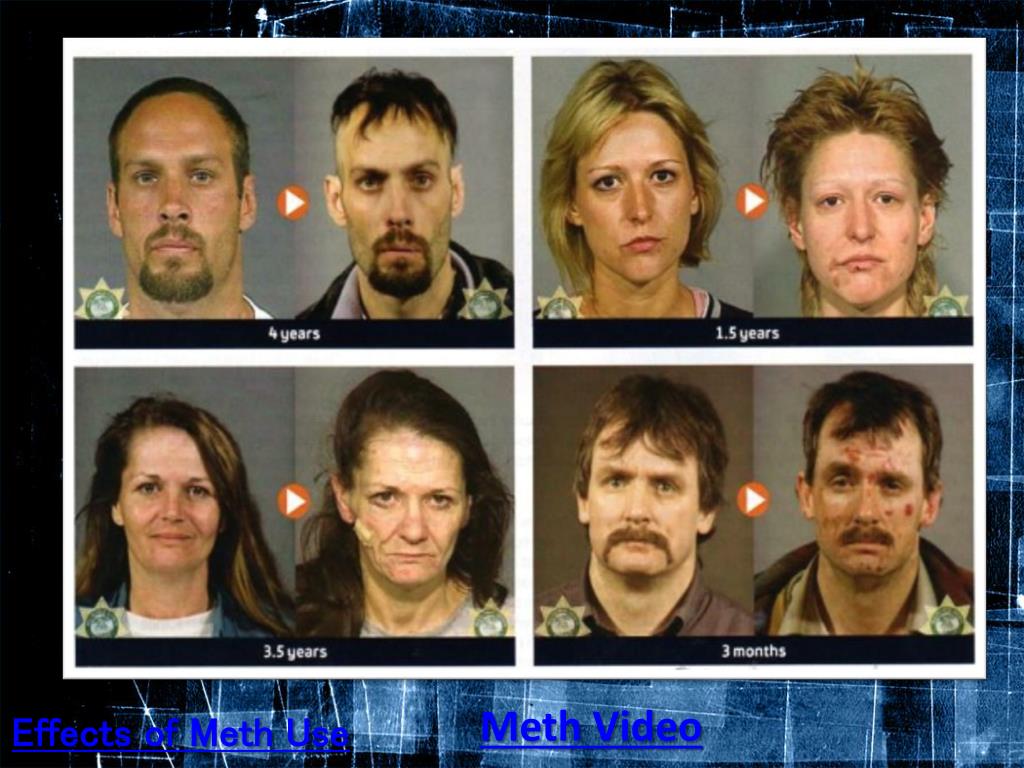 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.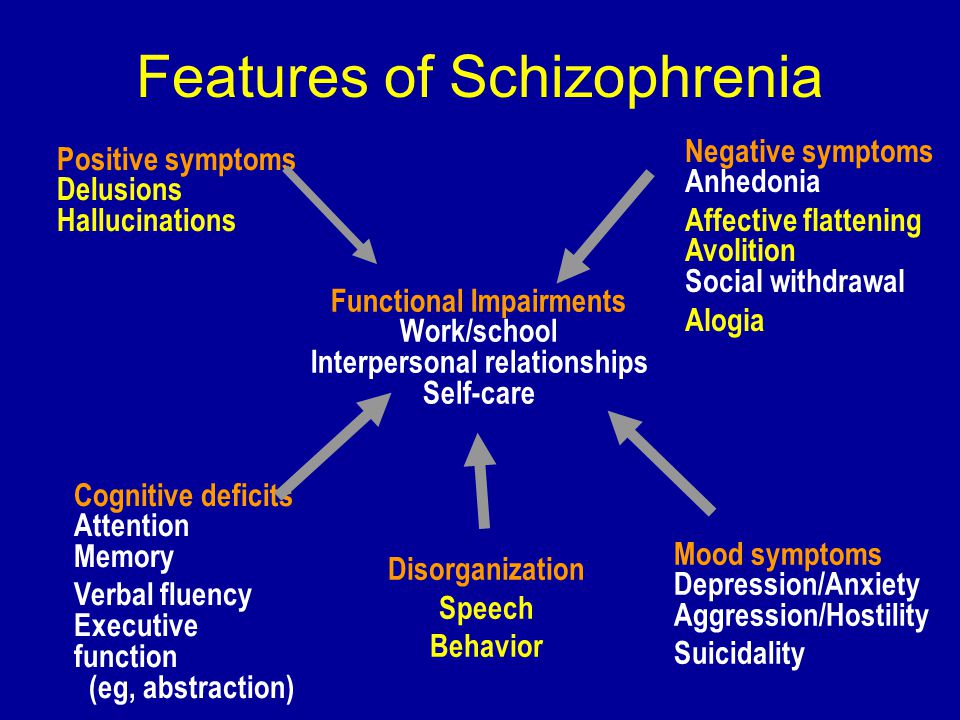
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
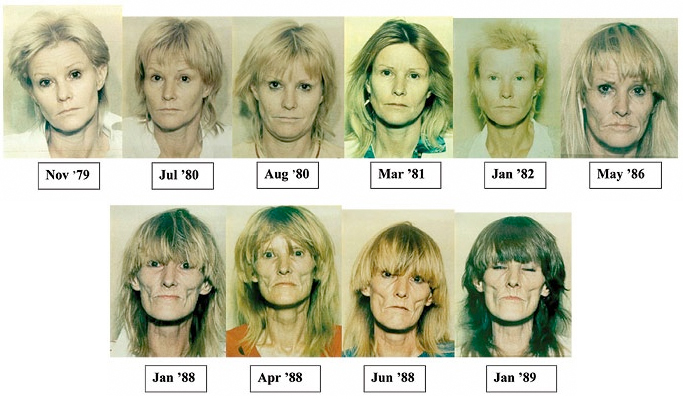
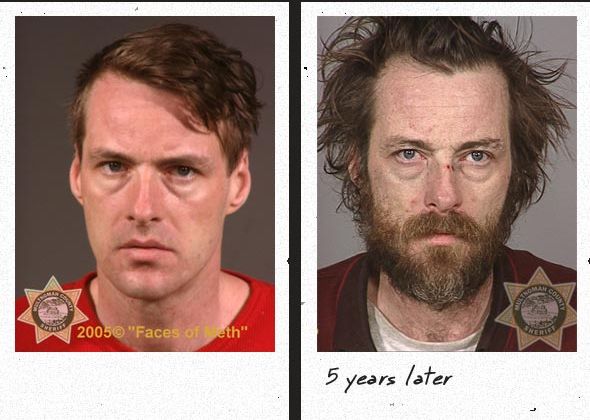
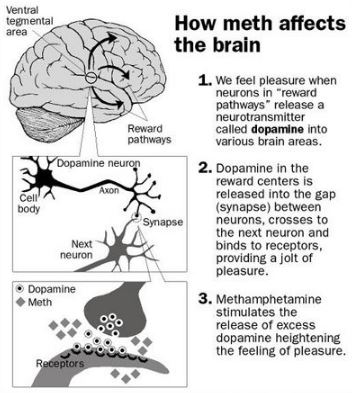
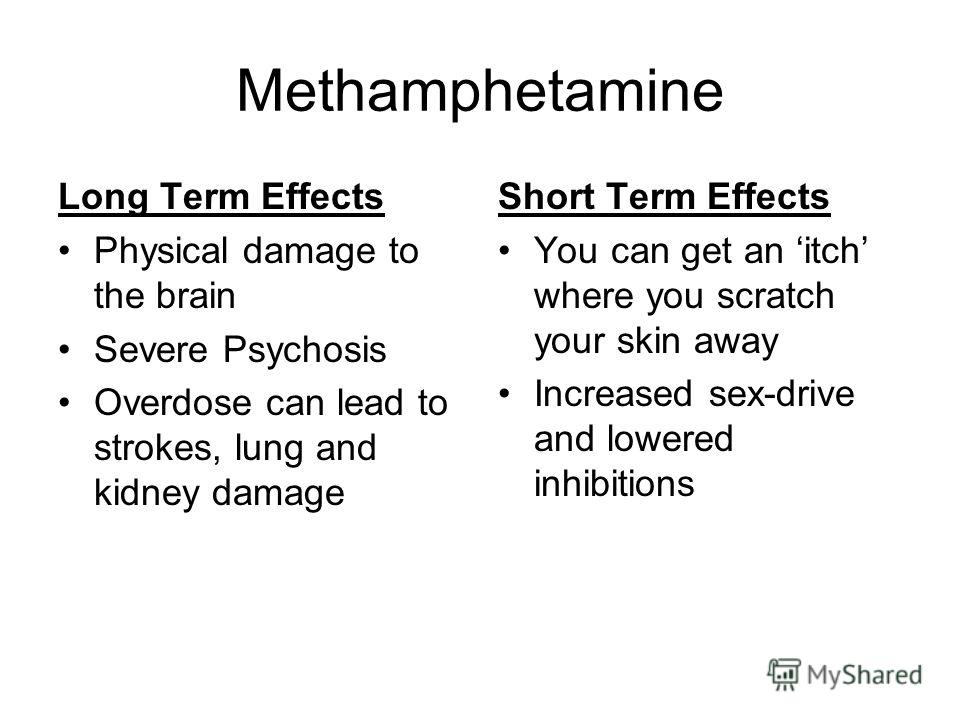
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Likelihood of developing psychosis when using psychoactive substances
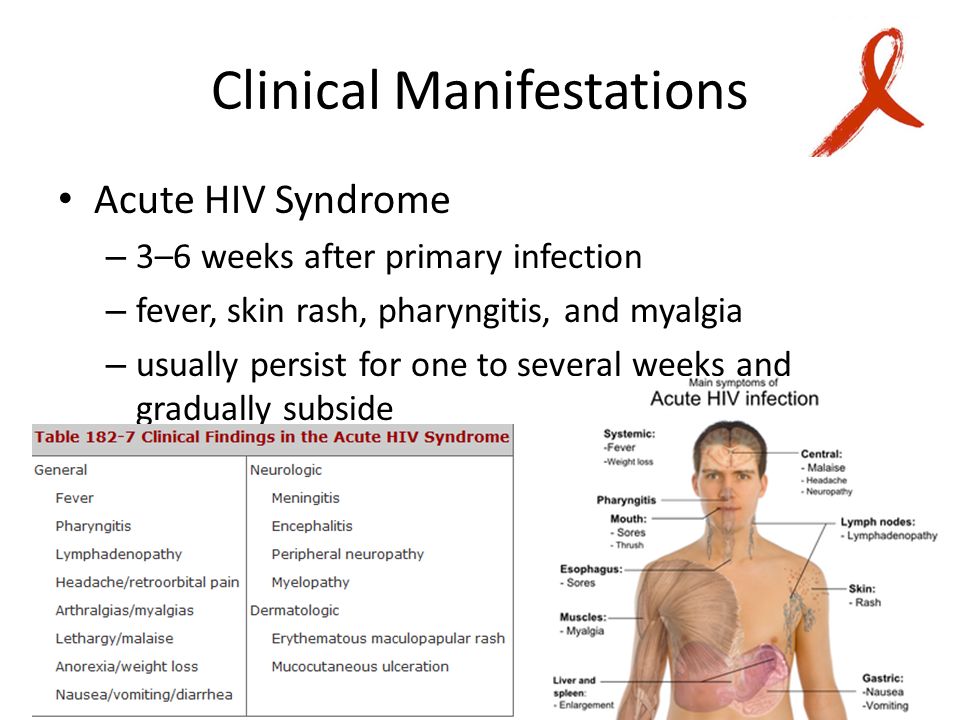
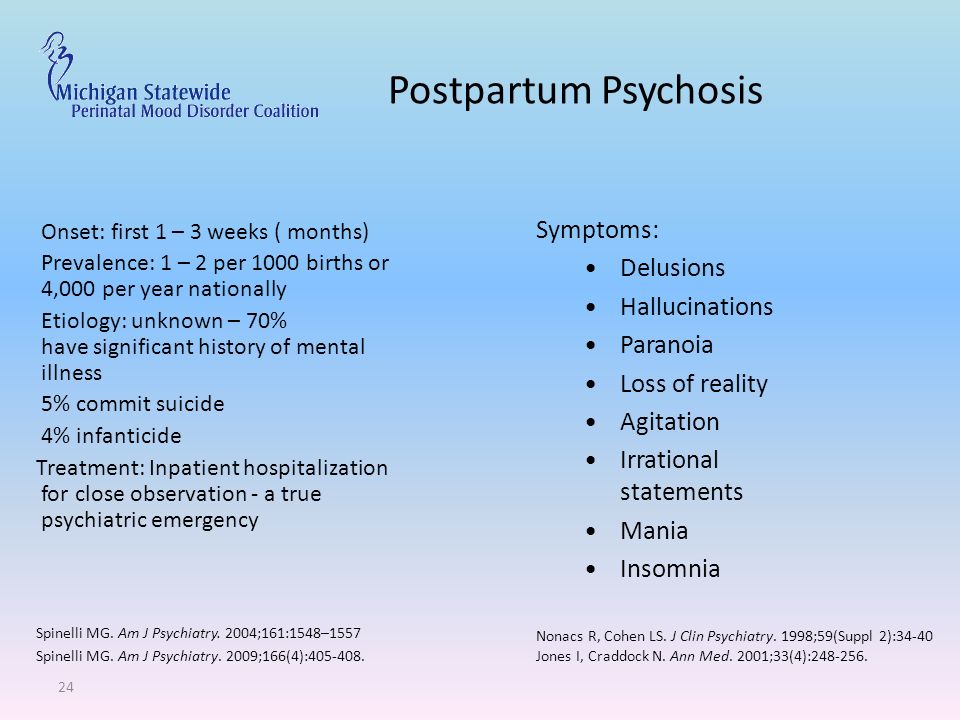
- Psychosis is a mental disorder in which the patient temporarily interprets the world around him differently than other people 1 . Psychosis may be a manifestation of severe mental illness, physical illness, or substance abuse 2 .
- Psychotic states may include: episodes when the patient hears or sees things that do not really exist (hallucinations), has false, often irrational beliefs for others (delusions), shows impaired memory, attention, incoherent speech, complains of deterioration sleep 3 .

In this section:
Essence of psychosis caused by substance abuse . Such addiction can cause psychotic reactions similar to those that occur in schizophrenia 5 .
Currently, the percentage of people who use psychoactive substances has increased. And most of them are teenagers. Addiction to drugs and alcohol is especially dangerous in early puberty, when the brain is still developing and can be especially sensitive to external factors 5 .
Studies have shown that the state of drug intoxication may initially lead to moderate temporary pathological effects, but gradually the negative impact on the body increases 5-7 .
Almost all psychoactive substances are capable of provoking psychosis. But its manifestations differ depending on the type of substance.
Psychotic symptoms may resolve with withdrawal of psychoactive substances or may persist for an indefinite period of time, and may be the result of withdrawal symptoms 8 .
The most common forms of psychosis due to alcohol and drug use:
1. Cannabis psychosis
Psychotic episodes are rare. Characterized by the presence of delusions, hallucinations, anxiety, the appearance of paranoid ideas 9 . Symptoms are short-term, reversible 9 .
2. Methamphetamine-induced psychosis
Psychosis is common, especially in regular methamphetamine users 9 . A predisposing factor is the formation of drug addiction at a young age 10.11 . There may be hallucinations, delusions, often frightening the patient. The psychosis continues for weeks, even after the end of drug use 10 .
Psychosis occurs 2-3 times more frequently in methamphetamine users than non-users of methamphetamine 10.11 .
3. Cocaine-induced psychosis
Cocaine use may cause transient psychotic symptoms: paranoia, hallucinations 12 . 50% of cocaine users may experience psychosis at least once 12 .
50% of cocaine users may experience psychosis at least once 12 .
A patient with severe psychosis exhibits hostility, aggression, paranoid behavior 12 .
4. Ecstasy-induced psychosis
Ecstasy and other similar substances are neurotoxic and can cause psychosis 13 . Most of the symptoms are positive, but negative symptoms are also present 13 .
Which patients are likely to develop psychosis due to substance use?
Mental disorder, as a rule, is associated with more than one-time drug use 14 .
Psychosis can be provoked either by an excessive dose of the drug, or by its long-term use - formed drug dependence 14 .
Triggers of psychosis:
Hereditary predisposition to mental illness 15
A family history of a confirmed case of mental illness is the main risk factor for psychosis when using alcohol, drugs 15 .
Other factors: place of birth, nationality, migration factors are controversial, despite the presence of an empirical base 16.17 .
There is evidence that psychosis develops more often in urban residents 18 .
Emigration to Western countries may also be correlated with a higher incidence of psychosis 19 .
An association has been established between migrant status and an increased risk of psychosis. Studies have shown that among ethnic minority groups living outside the country of birth, the prevalence of psychotic episodes is higher than among indigenous people 18-20 .
Sex and age 18-20
Most studies state that the risk of psychosis is comparable in men and women.
There is evidence that psychotic episodes occur more often in young men than in women, but a causal relationship has not yet been established. A systematic review of research done in the UK found that for the first time, psychosis was more common in boys or young men in their 20s than in girls and women 20 .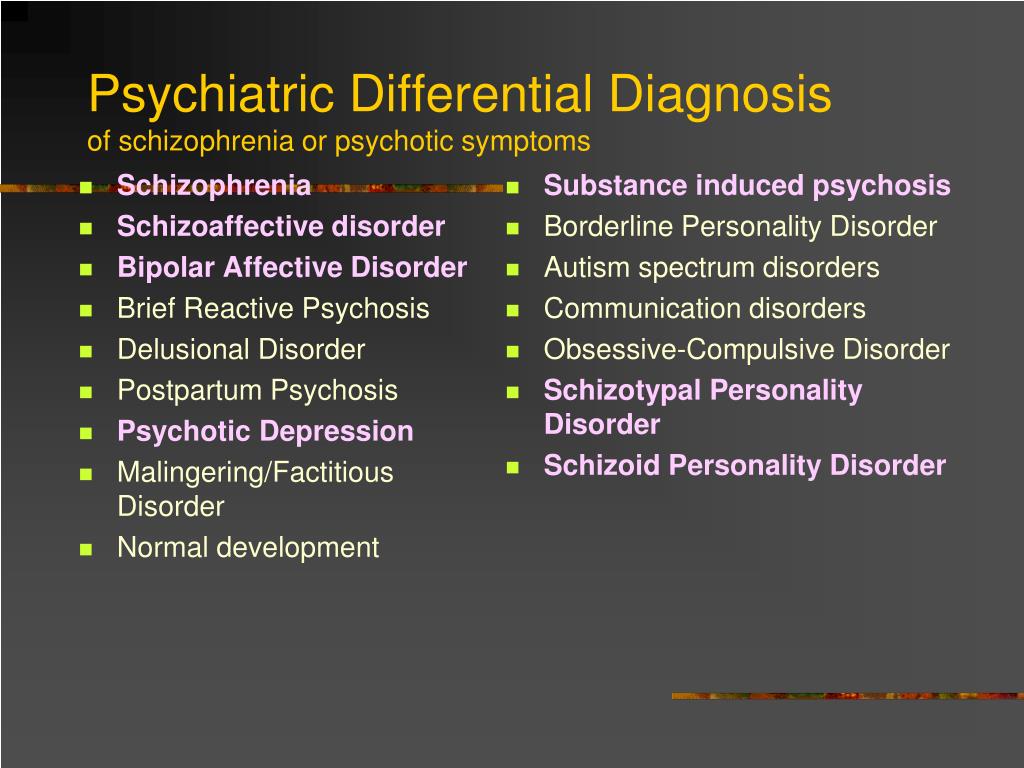
Predisposition
Several studies have concluded that there is an association between cannabis use and schizophrenia. Experience with cannabis use increases the risk of developing schizophrenia 31.32 .
In addition, patients with schizophrenia or schizophrenia-like disorders are at risk for compulsive drug use 22.23 .
Self-medication of schizophrenic patients with drugs has also been hypothesized, which may explain the increased incidence of substance abuse among patients.
Narcotic substances are mainly used to relieve the negative symptoms of the disease, as well as to reduce the discomfort associated with the side effects of taking antipsychotic drugs 23 .
Likelihood of developing schizophrenia with substance use
There is evidence that substance abuse psychosis is associated with later development of schizophrenia 24 .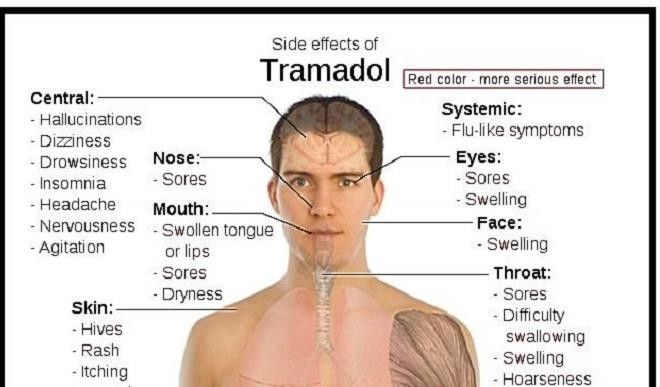
Drug dependence does not cause schizophrenia, but may trigger symptoms of schizophrenia 25 .
Use of cocaine, amphetamines and cannabis may increase the risk of or even cause symptoms of schizophrenia and/or worsen their severity 26 .
As mentioned above, individuals with psychotic disorders choose to "self-medicate" and use alcohol or other drugs to relieve symptoms of psychosis 21.22 . This tactic can bring short-term relief, but then an increase in the severity of schizophrenia symptoms follows. In addition, patients with schizophrenia are more likely to experience drug addiction, as they use drugs in high doses to reduce the symptoms of psychosis. As a result, a vicious circle is formed in which the symptoms of psychosis lead to drug use, and drugs again cause psychosis (Fig. 1) 27 .
The cycle of development of psychosis and the formation of drug dependence
Recommended treatments
The main focus of the treatment of such patients is the stabilization of psychotic symptoms, hostility and agitation 23 .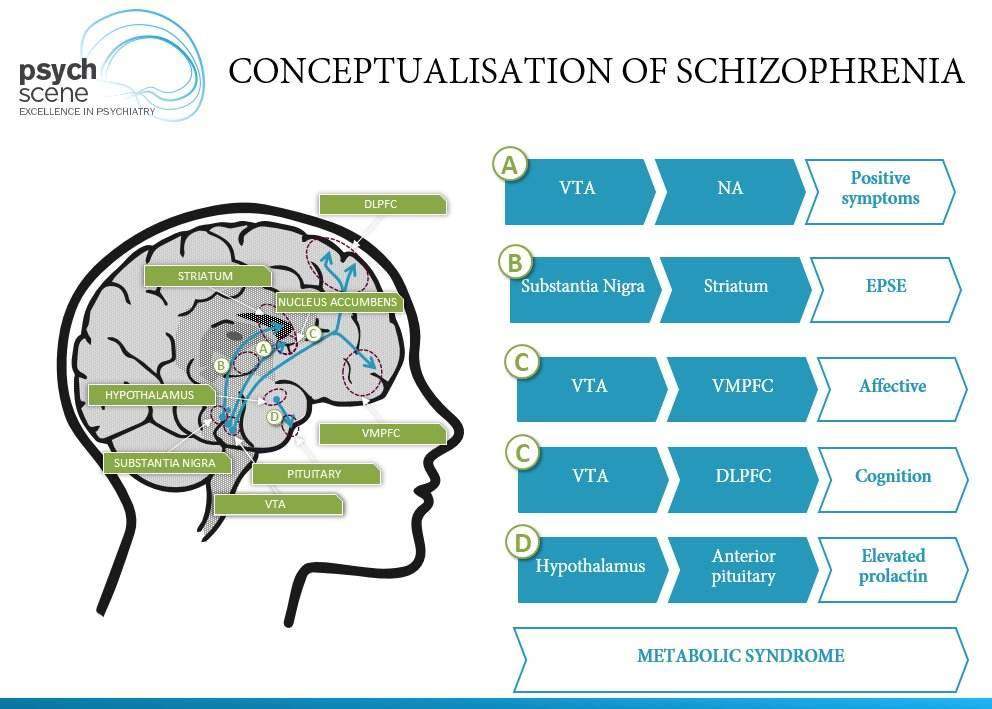
A number of new antipsychotics are being used that may be more effective than typical antipsychotics 28 .
In the early stages of treatment, patients can receive the help of a narcologist (detoxification) and a psychiatrist (hospitalization in a hospital) 29 .
The clinic provides treatment programs that help the patient achieve a more stable mental state while eliminating substance cravings 26 .
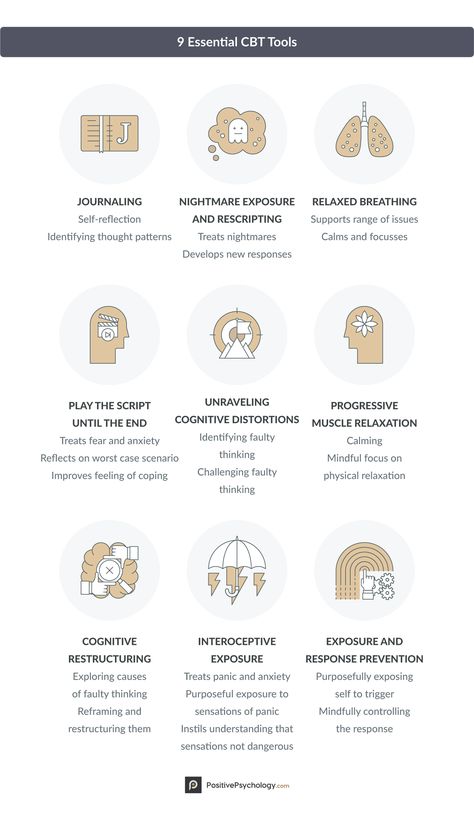
After stabilization of the condition, patients undergo outpatient treatment, which includes a rehabilitation program 28 . Psychotherapy, social learning programs and other methods may be involved, which are selected individually for each patient 30 .
In general, substance-induced psychosis is a sign of a serious mental health disorder. However, with expert support and intensive ongoing care, these patients can overcome their addiction and regain control of their lives.
Sources:
- https://www.
 nhs.uk/conditions/psychosis/ [accessed on the 17th of October 2019]
nhs.uk/conditions/psychosis/ [accessed on the 17th of October 2019] - https://www.rcpsych.ac.uk/mental-health/parents- and-young-people/young-people/psychosis—for-young-people [accessed on the 17th of October 2019]
- Wolfgang and Jürgen. Dialogues Clin Neurosci. 2015; 17(1): 9–18
- https://books.google.co.uk/books?hl=en&lr=&id=835HK7S9X1oC&oi=fnd&pg=PA317 [accessed on the 17th of October 2019]
- Mauri. Dual Diagn Open Acc 2016; 1:11.
- Forti et al. Lancet Psychiatry 2015; 2: 233–238
- Fattore. Biol Psychiatry 2016; 79: 539–548
- Hang et al. Medicine (Baltimore) 2017; 96(15): e6434.
- Arendt et al. BJP 2005, 187:510-515.
- McKetin et al. Drug Alcohol Rev. 2010; 29:358-63.
- Chen et al. Psychol Med. 2003; 33:1407-14.
- Roncero et al. Euro Psychiatry. 2013;28(3):141-6.
- Landabaso et al. Eur Addict Res 2002;8:133–140
- Bramness et al. B.M.C. Psychiatry. 2012; 12: 221.
- O'Donovan et al.
 Nat Genet. 2008; 40(9):1053-5.
Nat Genet. 2008; 40(9):1053-5. - Coid et al. Arch Gen Psychiatry. 2008; 65(11):1250-8.
- March et al. Epidemiol Rev. 2008; 30:84-100.
- Cheng et al. psychological medicine. 2011;41:949–958.
- Selten et al. Br J Psychiatry. 2001; 178():367-72.
- Kirkbide et al. PLOS One. 2012; 7(3): e31660.
- Ringen et al. Acta Psychiatr Scand. 2008; 118(4):297-304.
- Ringen et al. Psychol Med. 2008 Sep; 38(9):1241-9.
- Winklbaur et al. Dialogues Clin Neurosci. 2006; 8(1): 37–43.
- Schoeler et al. Lancet Psychiatry 2016; 3:215–225.
- https://www.nhs.uk/conditions/schizophrenia/causes/ [accessed on the 17th of October 2019]
- https://www.addictioncenter.com/addiction/schizophrenia/ [accessed on the 17th of October 2019]
- https://ndarc.med.unsw.edu.au/sites/default/files/ndarc/ resources/NDARC_PYCHOSIS_FINAL.pdf [accessed on the 17th of October 2019]
- Starzer et al. Am J Psychiatry. 2018; 175(4):343-350.

- Green J Subst Abuse Treat. 2008 Jan; 34(1):61-71
- Dickey et al. J Ment Health Policy Econ. 2000;3:27–33.
- Power RA, Verweij KJ, Zuhair M, Montgomery GW, Henders AK, Heath AC, Madden PA, Medland SE, Wray NR, Martin NG, Mol Psychiatry. Nov 2014; 19(11):1201-4.
- Psychol Med. 2017 Apr; 47(5):971-980. doi: 10.1017/S0033291716003172. Epub 2016 Dec 8. Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Gage Sh2, Jones HJ1, Burgess S2, Bowden J1, Davey Smith G1, Zammit S3, Munafò MR1
Login to Unlock
Suicide Prevention In particular, depression, hallucinations, delusions lead to this. Researches show that patients with schizophrenia often try to commit suicide. In particular, depression, hallucinations, delirium lead to this
More…
Login to Unlock
Drugs and difficulties in the treatment of schizophrenia… Drugs and difficulties in the treatment of schizophrenia…
Schizophrenia is a severe neuropsychiatric disorder with diverse clinical symptoms. The disease affects patients in different ways, as symptoms Schizophrenia is a severe neuropsychiatric disorder with heterogeneous clinical symptoms. The disease affects patients differently as the symptoms
The disease affects patients in different ways, as symptoms Schizophrenia is a severe neuropsychiatric disorder with heterogeneous clinical symptoms. The disease affects patients differently as the symptoms
More…
Please confirm your consent to the use of cookies
Yes, I agree
No, I refuse
Please confirm that you are a health worker
Showing 0 result(s).
Please log in to see 0 more result(s).
Stimulant psychosis | Knowledge Base
Stimulant psychosis is a psychotic disorder that occurs in some people who use psychostimulants. It most commonly occurs in users taking high doses, but, in rare cases, may occur in patients using therapeutic doses under the supervision of a physician.
Symptoms
The symptoms caused by different stimulants differ slightly, but share features with organic psychoses, such as: hallucinations, delusions, thought disturbances, and, in rare cases, catatonia.
Physical symptoms in long-term stimulant abuse or overdose are often associated with stimulant psychoses (but not organic psychoses). These additional symptoms may include aggression, arrhythmia, pupillary dilation, diarrhea, hypertension, pyrexia, nausea, shortness of breath, anxiety, seizures, sleep deprivation, tremors, and vomiting.
Psychotic stimulants
Amphetamine
Amphetamine and its derivatives (amphetamines) are known to cause psychosis when used chronically or at high doses. The word "amphetamines" means both (±)-1-phenylpropan-2-amine itself and its substituted derivatives. Examples of amphetamine derivatives: cathinone, ephedron, methamphetamine, methcathinone, methylphenidate.
Symptoms of amphetamine psychosis include auditory and visual hallucinations, delusions of persecution and delusions of attitude simultaneously with clear consciousness and extreme agitation, sometimes there may be some signs of mental automatism syndrome (Kandinsky-Clerambault syndrome).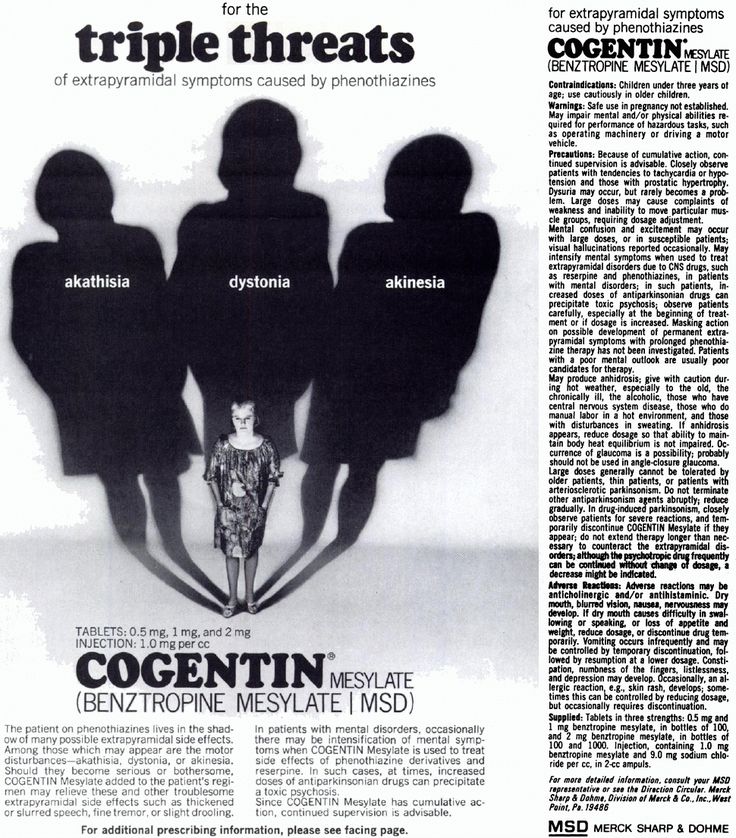 In this case, the person experiences tension and anxiety. Hallucinations are usually true, but pseudo-hallucinations can also occur.
In this case, the person experiences tension and anxiety. Hallucinations are usually true, but pseudo-hallucinations can also occur.
Microhallucinatory-paranoid syndrome occasionally occurs, as with cocaine use. It manifests itself in the sensations of small insects on the body, or worms, dots, threads.
In rare cases, there is a catatonic stupor or catatonic excitation, a manic state, a state of ecstasy with fussiness and brightness of perceptions, a syndrome of obsessive-compulsive disorders on the background of a depressive-dysphoric mood.
The symptoms of acute amphetamine psychosis are very similar to those of the acute phase of schizophrenia. Sometimes people in a state of amphetamine psychosis experienced sperrings (breaks in the associative process), insertion or withdrawal of thoughts, echo of thoughts (sounding of their own thoughts), reasoning, inadequacy of facial expressions.
Psychosis has only been reported with 50 mg of amphetamine, but in some cases even 650 mg did not cause psychosis. This amount of the substance was administered 8 times to a healthy person, while he experienced only euphoria, increased libido, increased mental activity and productivity. Each time after the end of the action of the substance, depression, memory impairment and a decrease in sexual desire were observed, but psychosis did not occur.
This amount of the substance was administered 8 times to a healthy person, while he experienced only euphoria, increased libido, increased mental activity and productivity. Each time after the end of the action of the substance, depression, memory impairment and a decrease in sexual desire were observed, but psychosis did not occur.
With continued use of amphetamine, psychosis increases, so treatment requires immediate withdrawal.
Single use psychoses
One patient developed convulsive seizures and further “unclear consciousness” from a single use of 140 mg of amphetamine.
A case of delirium was reported in a 7.5-year-old child who used 300 mg of amphetamine while recovering from pharyngitis. Delirium was accompanied by hallucinations, the child observed small crawling insects in the corners of the room, experienced horror and was disoriented. At the physical level, there was an increase in temperature, dilated pupils, impaired coordination. The duration of this psychosis was less than a day, and it ended in complete recovery.
The duration of this psychosis was less than a day, and it ended in complete recovery.
Duration of psychosis
The duration of psychosis as a result of acute poisoning usually lasts 1-3 days, in extremely rare cases it is extended by 1 week maximum with a large amount of the drug used.
Connell studied 30 amphetamine abusers. In 2 of them, the psychosis was gone in 5-7 weeks, in 5 people - in 2-4 weeks, in 1 - in 2 weeks, and in the majority - 15 people - the psychosis was gone in less than 1 week. The medical history of the remaining 7 is unknown.
In rare cases, psychosis may last 2–7 months or even more than 3 years after amphetamine use has been discontinued. Allier described a man who had been ill for 1.5 years with pseudo-hallucinations of a commentary nature ("voice") and a feeling of being controlled. In particular, he wrote that the patient believed that he (and other people) was being controlled by radar from the Vatican.
According to a study by Sano and Nagasaka, of 599 amphetamine abusers, 62% developed psychoses that resulted in rapid recovery. In 10% of patients, psychosis did not go away after 6 months after discontinuation of the drug.
Somatic and neurological symptoms
Acute amphetamine psychosis may be accompanied by the following somatic symptoms: tachycardia, mydriasis, tremor, revitalization of tendon reflexes, dry mouth. However, with prolonged psychosis, these symptoms may be absent.
Cocaine
Cocaine has the same potential to cause short-term psychoses. More than half of cocaine abusers reported some psychotic symptoms. Typical symptoms include paranoid delusions: people think they are being followed. Often there are hallucinations associated with delusional ideas. Delusional parasitosis with goosebumps is also a fairly common reaction.
Metcathinone (ephedron)
Metcathinone psychosis usually develops against the background of severe insomnia and general exhaustion of the body. It proceeds in the form of a rudimentary or acute paranoid with delusions of persecution, delusions of special significance, visual or verbal hallucinations. Verbal hallucinosis and delusions of jealousy are rare. The literature also describes cases of amental-like psychosis and twilight clouding of consciousness.
It proceeds in the form of a rudimentary or acute paranoid with delusions of persecution, delusions of special significance, visual or verbal hallucinations. Verbal hallucinosis and delusions of jealousy are rare. The literature also describes cases of amental-like psychosis and twilight clouding of consciousness.
Methcathinone psychosis usually lasts 3-4 hours (in some patients, the duration can be up to 1 month).
Methylphenidate
Methylphenidate, better known under the trade name Ritalin, is a central nervous system stimulant with a similar mechanism of action to cocaine. This substance, when chronically abused, can also lead to psychosis.
Methamphetamine
According to one Australian study, 18% of 309 active methamphetamine users experienced psychosis in the past year.
Symptoms of methamphetamine psychosis: auditory, visual, tactile and olfactory hallucinations, delusions of persecution and delusions of relationships (erroneous assessment by the patient of the attitude of other people towards him), compulsive behavior, stereotypes, anhedonia, depression, flattened affect. Most often, psychosis occurs in the form of a rudimentary or acute paranoid with delusions of persecution, special significance, with visual or verbal hallucinations. Like amphetamine psychosis, it is similar to the psychosis of schizophrenic patients. The literature also describes manic-delusional psychoses.
Most often, psychosis occurs in the form of a rudimentary or acute paranoid with delusions of persecution, special significance, with visual or verbal hallucinations. Like amphetamine psychosis, it is similar to the psychosis of schizophrenic patients. The literature also describes manic-delusional psychoses.
A case of twilight stupefaction in a patient who abused methamphetamine for about 2 years is described. The condition lasted 8 days, while the patient experienced visual and auditory hallucinations, heard the voice of the planet Mars, and believed that in this way this planet tried to make contact with the Earth. Tachycardia up to 120 per minute, mydriasis and arterial hypertension were also observed.
Methamphetamine psychosis usually occurs after many days of substance use, in doses of 6-11 ml intravenously per day. The duration of a psychotic disorder is usually from 8 to 10 hours, but sometimes up to 1 month.
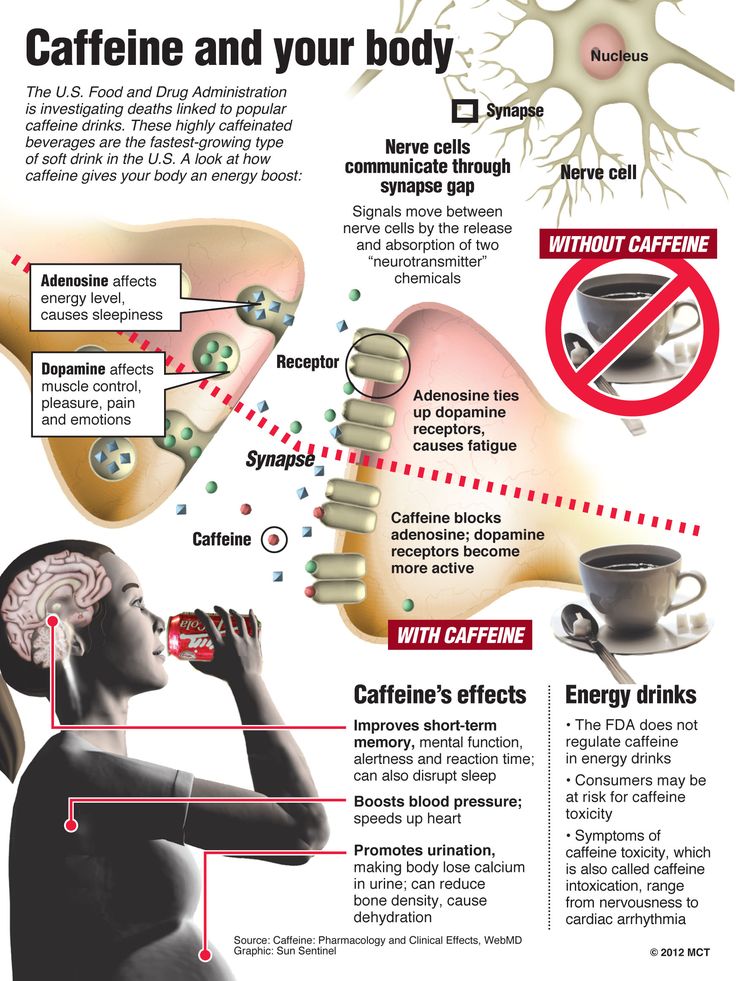
Caffeine
It has been suggested that caffeine in high doses or chronic abuse may induce psychosis in healthy individuals or exacerbate pre-existing psychosis in F20 patients. (schizophrenia).
(schizophrenia).
Chronic use of caffeine, theobromine, theophylline in high doses can lead to exhaustion of the nervous system, which can become the basis for subsequent psychosis.
The most commonly described delirium is caused by caffeine overdose. There is an influx of vivid visual hallucinations, sometimes auditory, a person loses orientation in the world around him. After removing caffeine from the body, the memory of the past is partially or completely preserved. Some patients lose the ability to judge distances correctly, and objects appear to them to be closer than they really are. Somatic disorders associated with delirium: mydriasis, hyperemia, ataxia, tachycardia, severe thirst, dry skin and mucous membranes, cyanosis of the skin, sometimes increased blood pressure and fever.
There is a case when an elderly woman who used 300 grams of coffee daily for two years experienced psychosis with disorientation in the environment, episodic visual hallucinations, euphoria, agitation, ending in death.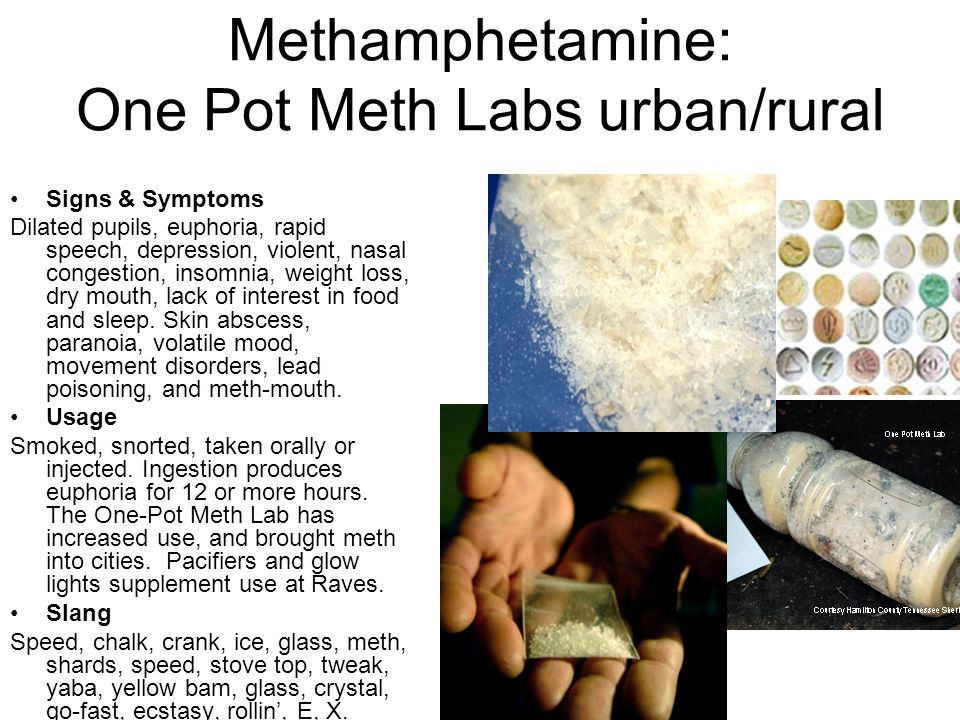
Caffeine poisoning psychosis with impaired consciousness usually lasts no more than a few days.
Designation in ICD-10
In the 10th revision of the International Classification of Diseases, psychotic disorders associated with the use of stimulants are indicated by the following codes:
- F14.50 Schizophrenia-like disorder due to cocaine use
- F14.51 Predominantly delusional disorder due to cocaine use
- F14.52 Predominantly hallucinatory disorder due to cocaine use
- F14.53 Predominantly polymorphic psychotic disorder due to cocaine use
- F14.54 Cocaine use disorder with predominantly depressive psychotic symptoms
- F14.55 Cocaine use disorder with predominantly manic psychotic symptoms
- F15.50 Schizophrenia-like disorder associated with the use of other stimulants (including caffeine)
- F15.51 Predominantly delusional disorder associated with the use of other stimulants (including caffeine)
- F15.
 52 Predominantly hallucinatory disorder associated with the use of other stimulants (including caffeine)
52 Predominantly hallucinatory disorder associated with the use of other stimulants (including caffeine) - F15.53 Predominantly polymorphic psychotic disorder associated with the use of other stimulants (including caffeine)
- F15.54 Other stimulant use disorder (including caffeine) with predominantly depressive psychotic symptoms
- F15.55 Other stimulant use disorder (including caffeine) with predominantly manic psychotic symptoms
Treatment
The treatment of stimulant psychosis is to relieve symptoms during the acute phase of intoxication: maintaining normal body temperature, blood pressure and heart rate at an acceptable level until the substance is successfully metabolized and vital body functions return to baseline. In the early stages of treatment, typical and atypical antipsychotic drugs are indicated.
In patients with arterial hypertension, it is preferable to prescribe chlorpromazine (chlorpromazine), since, in addition to dopamine receptors (D₁, D₂, D₃ and D₄), it blocks α-adrenergic receptors.