Mental exhaustion and depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
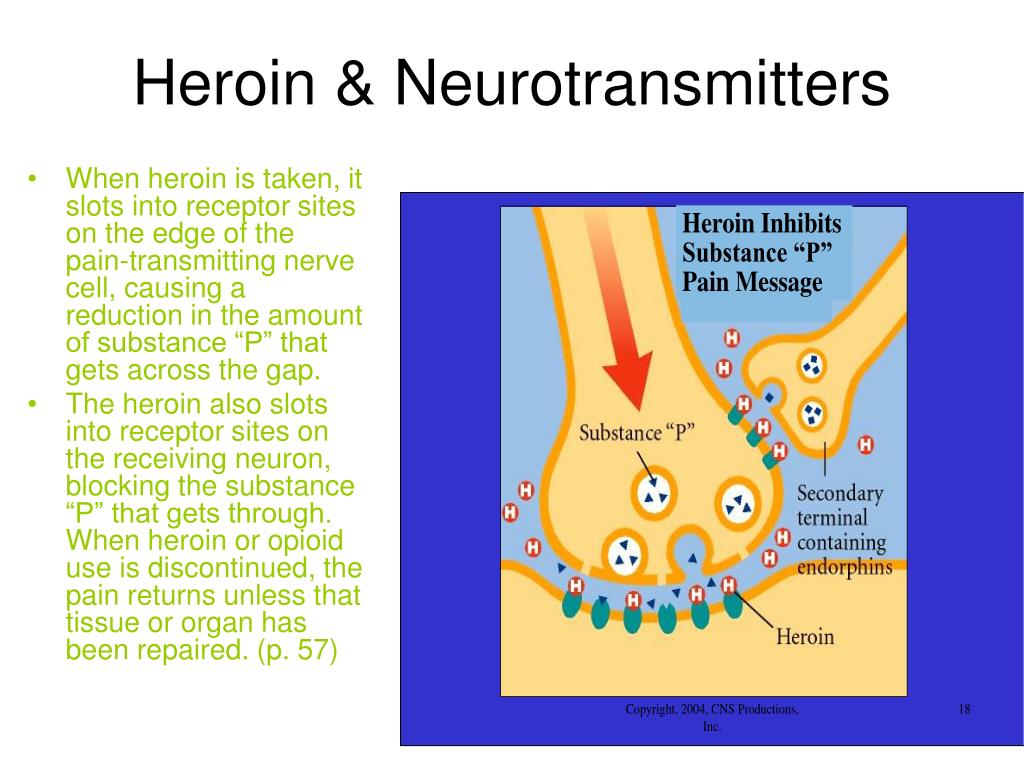
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Burnout syndrome
Burnout syndrome is a state of emotional, mental exhaustion, physical fatigue resulting from chronic stress at work. May be characterized by impaired productivity at work, fatigue, insomnia, increased susceptibility to somatic diseases, alcohol or other psychoactive substance use, and suicidal behavior.
The development of this syndrome is typical, first of all, for professions where the provision of assistance to people dominates (medical workers, teachers, psychologists, social workers, rescuers, law enforcement officers, firefighters). Work with “heavy” clients also predisposes to burnout (gerontological, oncological patients, aggressive, suicidal patients, patients with addictions. nine0003
Work with “heavy” clients also predisposes to burnout (gerontological, oncological patients, aggressive, suicidal patients, patients with addictions. nine0003
EBS is seen as the result of an unfavorable resolution of stress in the workplace.
Signs of burnout:
- Behavioral change: boredom, resistance to work, tardiness, substance use, accident susceptibility, decreased creativity.
- Change in feelings: depression, gallows humor, feelings of failure, guilt, bitterness, irritability, nit-picking. nine0016
- Changes in thinking: decreased concentration, rigidity, suspicion, incredulity, victim mentality, callousness.
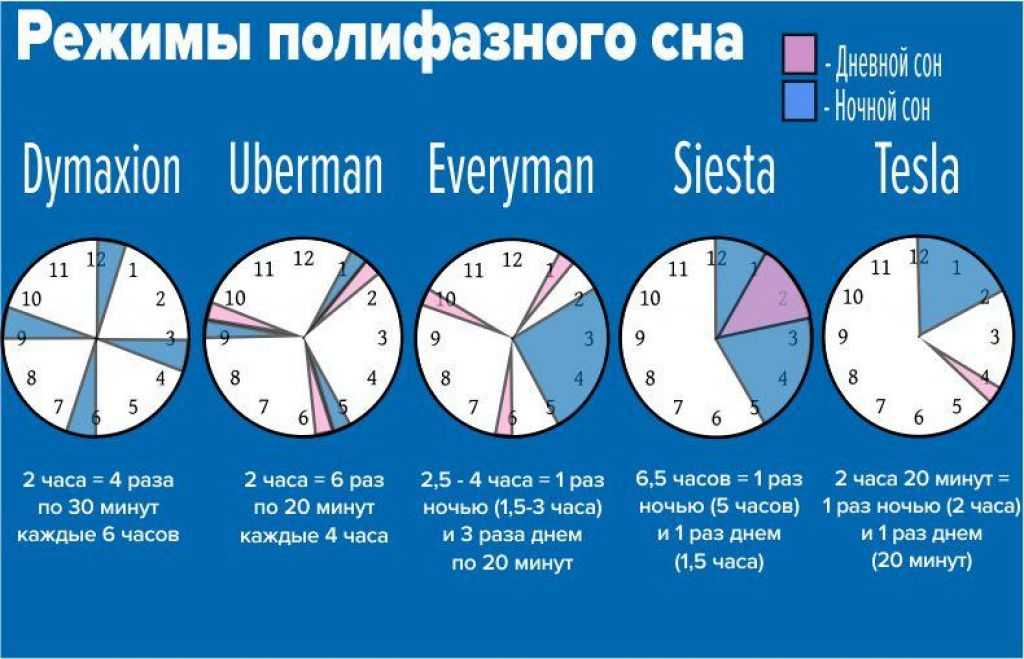
- Changes in health: sleep disturbance, fatigue, reduced immunity.
Questionnaire
Evaluation of the syndrome of emotional burnout.
Phases of development of the CMEA (according to Selye).
- I Voltage phase.
It is a harbinger and a “triggering” mechanism in the formation of emotional burnout.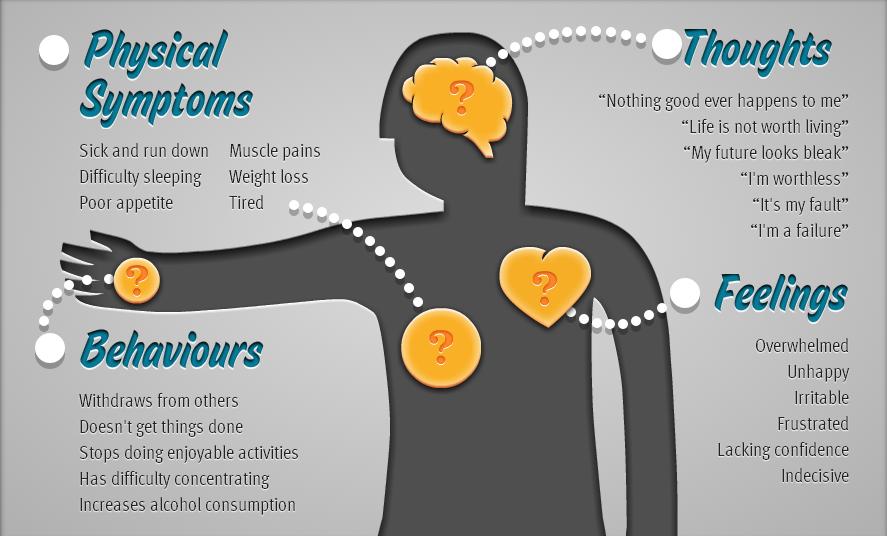 The development of CMEA is preceded by a period of increased activity, when a person is completely absorbed in work, refuses needs that are not related to it, forgets about his own needs. If these efforts of an employee are adequately assessed and supported, if a person receives a sense of the importance and significance of his work, the CMEA does not develop. If not, and there is a collapse of ideas, then the CMEA gets its development. nine0016
The development of CMEA is preceded by a period of increased activity, when a person is completely absorbed in work, refuses needs that are not related to it, forgets about his own needs. If these efforts of an employee are adequately assessed and supported, if a person receives a sense of the importance and significance of his work, the CMEA does not develop. If not, and there is a collapse of ideas, then the CMEA gets its development. nine0016 - II Phase resistance.
A person strives for psychological comfort and therefore tries to reduce the pressure of external circumstances. - III Phase of exhaustion.
It is characterized by a drop in the overall energy tone and a weakening of the nervous system. "Burnout" becomes an integral attribute of personality.
Metastases of "burnout" penetrate into the value system of the individual. There is an anti-humanistic attitude. The personality claims that working with people is not interesting, does not give satisfaction, and does not represent social value.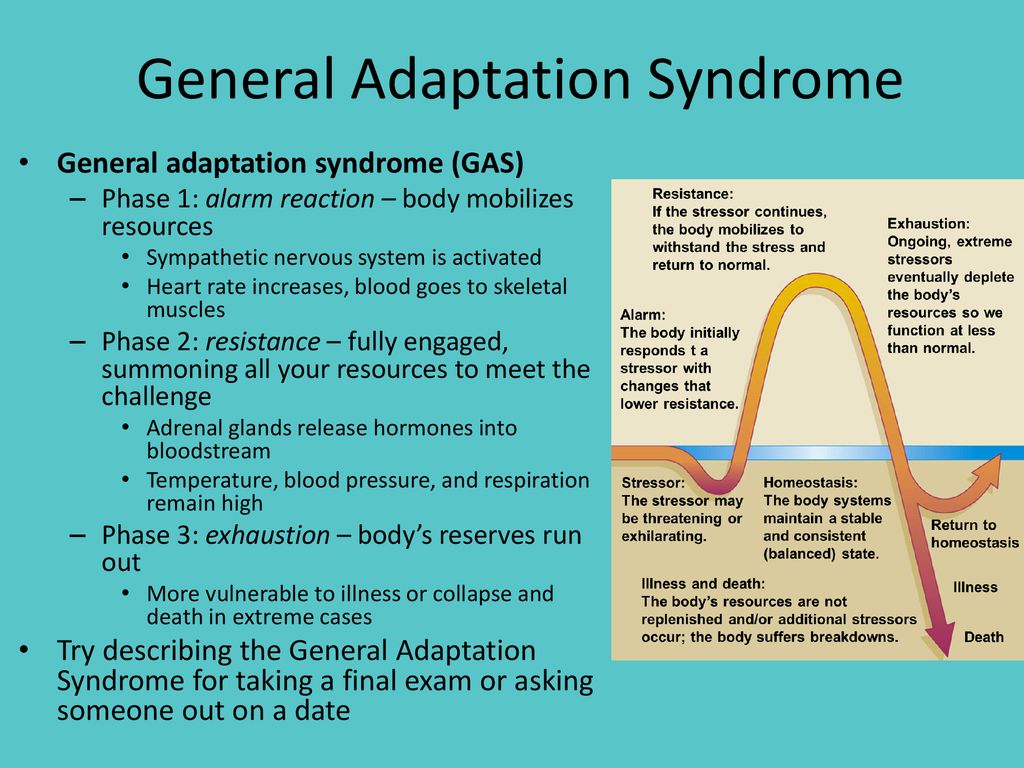 nine0003
nine0003
Prevention and treatment of burnout syndrome.
What protects against the development of EBS can also be used in the treatment of an already developed syndrome.
Two aspects can be distinguished here: individual protection and organizational approach.
Consider the qualities that help a specialist avoid professional burnout.
Firstly, these are the following individual personality traits of a person:
- Conscious, purposeful care of one's physical condition (for example, playing sports and maintaining a healthy lifestyle). nine0016
- High self-esteem and confidence in oneself, one's abilities and capabilities (working with unstable self-esteem, reading psychological literature or contacting a psychotherapist who will point out directions in this matter).
- High professional self-esteem (the need to constantly improve one's professional level).
Secondly, burnout is avoided by people who have experience of successfully overcoming professional stress; capable of constructive change under stressful conditions. nine0003
nine0003
Thirdly, an important distinguishing feature of people who are not subject to CMEA is the ability to form and maintain positive, optimistic attitudes and values in themselves, both in relation to themselves and other people and life in general. At the end of a brief review of personal protective equipment, I would like to say that "Calllessness to yourself is also a mutilation."
Be attentive to yourself. At the first manifestations of SEB, take action: take a break, meet friends, change the environment, discover your creative abilities. If improvised means do not help, seek help. This can be attending trainings (from personal growth training to creativity training), individual or group work with a psychotherapist. Remember, the CMEA will not go away on its own, you must take steps to protect yourself. If you feel that you cannot cope with the problem yourself, do not delay the trip to a specialist. nine0003
By leaving your personal data, you give your voluntary consent to the processing of your personal data. Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc.). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed "). By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data".
Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc.). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed "). By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data".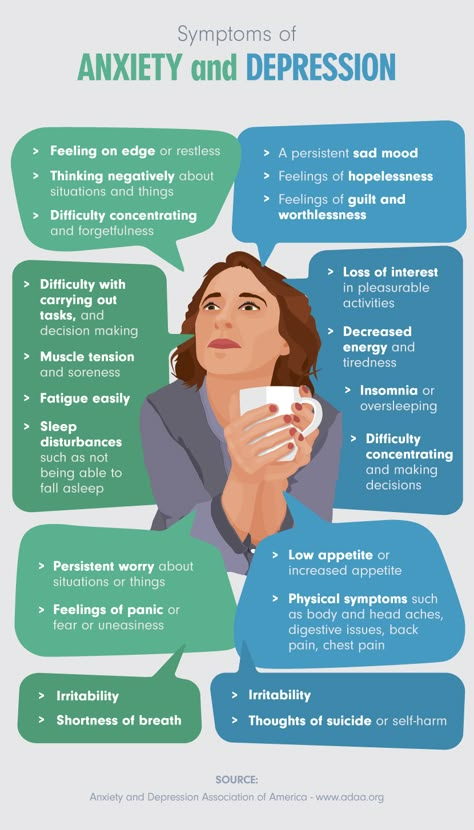 nine0003
nine0003
why exhaustion is not a personal, but an organizational problem - Career on vc.ru
And its solution is in the hands of the manager, not the employee. Reminder edition material.
25 342 views
Damir Kopezhanov / Unsplash
The problem of professional burnout has been relevant for many years, but recently it has sharply worsened. Why do we burn out more and more and how to avoid it? Gradually, experts begin to emerge the answer to this question. nine0003
Who is to blame for the fact that we burn out
The traditional answer is ourselves. They failed to balance work and rest, were not competent enough, failed to adapt, succumbed to procrastination. Explanations may vary, but the essence does not change - this is always our mistake, for which we pay with a loss of motivation and productivity.
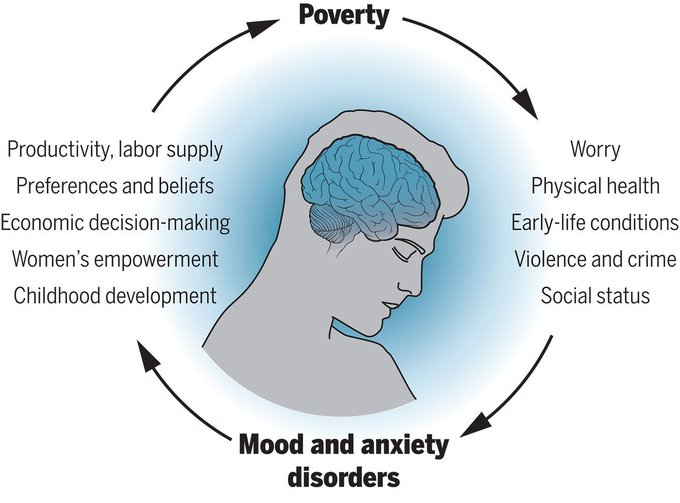
But if it's our fault, isn't it strange that the symptoms of burnout are not like frustration (disappointment over not being able to achieve what you want), but depression? And it seems so much so that some experts even consider this condition a variant of a depressive disorder. nine0003
nine0003
Psychologist Irwin Schoenfeld examined 5,000 burnt-out teachers and found that 90% had symptoms of clinical depression: apathy, depression, and a sense of helplessness. Other researchers have found that symptoms of burnout and depression tend to worsen in parallel: the worse the burnout, the deeper the depression.
As clinical psychologist Natalie Datillo notes, burnout is often accompanied by a typically depressing sense of powerlessness: people feel that despite their best efforts, they can't change anything in their lives. nine0003
Swiss expert Renzo Bianchi even suggests this test in The Atlantic: When you face a psychological problem at work, ask yourself, can you eliminate the stressor? If the answer is “yes”, then this is not burnout yet. But if you realize that you can’t change the situation and can only passively wait for negative consequences, then you have begun to burn out.
Why do we behave in a state of burnout as if we were faced with an insurmountable external obstacle? Because that's the way it is. To see this, just look at the top six causes of burnout identified by UCLA psychology professor Christina Maslakh:
To see this, just look at the top six causes of burnout identified by UCLA psychology professor Christina Maslakh:
- Excessive workloads and tight deadlines.
- Lack of control over the work process and decision-making authority, combined with increased demands for results.
- Lack of professional recognition.
- Toxic work environment: disrespect and discrimination, conflicts in the team.
- Favoritism: undeserved privileges for individual employees. nine0016
- Monotonous and uninteresting work.
It is obvious that almost all of these factors are not associated with personal mistakes, overstated ambitions or miscalculations in time management. Reduce workloads, moderate demands, eliminate hard deadlines, avoid overtime work, allow you to change jobs, help you choose a more convenient schedule and reward for achievement and initiative - who does it depend on?
Who will stop burnout
Psychologist Adam Grant believes that there are three keys to solving the problem of burnout: adequate requirements, optimal control and the necessary support. And all three are in the hands of leaders.
And all three are in the hands of leaders.
Research also clearly shows that burnout is an organizational problem. And management is responsible for organizing the workflow. But the bosses are not the evil geniuses in this story. They may not always be able to organize work in a way that eliminates burnout. However, they may try to remedy the situation. nine0003
According to McKinsey, company executives have recently been actively implementing special programs to improve the mental health of employees, inviting coaches and psychologists, organizing yoga classes, conducting stress training, seminars on balanced nutrition and the development of positive thinking. But studies show that these measures often do not have the desired effect. And there are at least two reasons for that.
The first one is individual. Workflow experts Yu Jie Heng and Kira Shabram point out in an article in the Harvard Business Review that there are three types of burnout. And what is useful in one case may be ineffective or even harmful in another.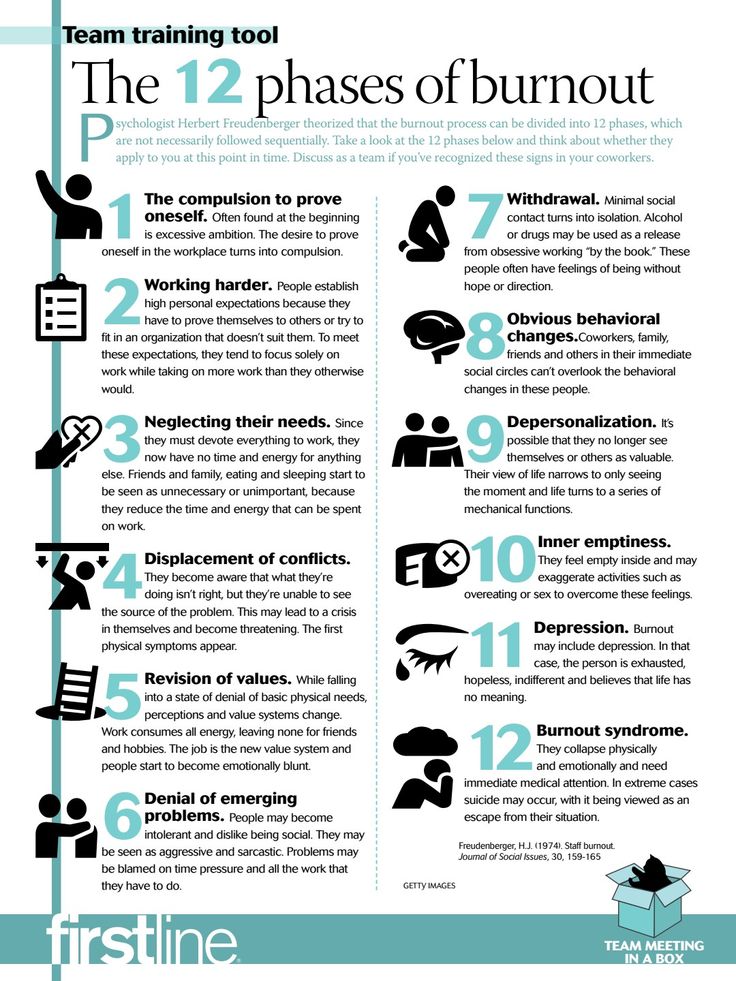 nine0003
nine0003
To cope with burnout, one must first determine which of the personal resources have been exhausted and need to be restored.
- Mental and emotional exhaustion. In this case, programs and courses on self-optimization can only increase tension and guilt. Helpful recommendations are often perceived as an additional burden and confirmation that you could not cope with the problem on your own. To restore internal resources, experts advise to slow down and take care of yourself. Short breaks in the working day will help here - for meditation, a walk, a snack or a dream. nine0016
- Social exclusion at work. In this case, meditation and other self-centered activities can only aggravate the condition. Therefore, just collective courses are useful, in which you can get closer to colleagues. When a person suffering from emotional alienation switches to solving other people's problems (even just spending a few minutes a day discussing other people's concerns and wishes), burnout levels decrease.
 nine0016
nine0016 - Loss of faith in one's own effectiveness. In this case, classes are needed to help restore self-esteem. Workplace positivity expert Mandy O'Neill suggests trying to start a new project that has nothing to do with work. For example, take up photography or develop the habit of running in the morning. The main thing is to feel like the master of the situation again.
The second problem is systemic. The WHO defines burnout as the result of prolonged stress in the workplace. But what creates it? When at 19The term “burnout” itself appeared for the first time in the 70s, it was believed that it was mainly doctors, psychologists, teachers and social workers who were subject to it, that is, people who, on duty, often face human problems and suffering. Then it became clear that you can burn out in any profession.
Recently, the drastic transition to remote work and the resulting disruption of the usual work and rest routine are often blamed for increased stress. Two-thirds of Amazon, Microsoft, Google and Facebook employees said in a survey that they feel more exhausted due to the need to adapt to a new work rhythm. 42% of Russians also complain about emotional exhaustion. But the burnout epidemic began long before the coronavirus pandemic. Already in 2018, 23% of American workers suffered from it. nine0003
Two-thirds of Amazon, Microsoft, Google and Facebook employees said in a survey that they feel more exhausted due to the need to adapt to a new work rhythm. 42% of Russians also complain about emotional exhaustion. But the burnout epidemic began long before the coronavirus pandemic. Already in 2018, 23% of American workers suffered from it. nine0003
Burnout is not really a curse of certain professions or the result of external circumstances, according to BuzzFeed News contributor Ann Helen Petersen. It is a natural product of the modern recycling culture that has become the norm in all industries around the world. All of us, employees and managers, have become hostages of this efficiency model.
Workers find it natural to take on excessive workloads. And managers find it natural to overload them with work. Because of this, sooner or later, each of us develops what Petersen calls "paralysis of everyday affairs." nine0003
We simply cannot cope with all these tasks at the same time, even if we are able to solve each separately. Their number paralyzes us. This is where the feeling of impotence, helplessness and apathy comes from. Of course, we can take a vacation or a day off. We can take a break for yoga or get emotional support from friends at lunchtime. But this is a temporary compromise.
Their number paralyzes us. This is where the feeling of impotence, helplessness and apathy comes from. Of course, we can take a vacation or a day off. We can take a break for yoga or get emotional support from friends at lunchtime. But this is a temporary compromise.
To truly address burnout, we all need to realize that work stress is more than just a necessary evil. It has become something of a performance indicator for us. And while it seems to us that burning ourselves at work means being effective, we will burn out. nine0003
The article was prepared by the online publication Reminder, which is dedicated to health, psychology and practical philosophy. More useful information can be found on our Facebook pages, Telegram or mailing list.
More on Reminder:
- Falling Arrow Technique: How to stop worrying about nonsense.
- Why you should monitor your heart rate at rest. Studies show that it is an important predictor of heart disease.