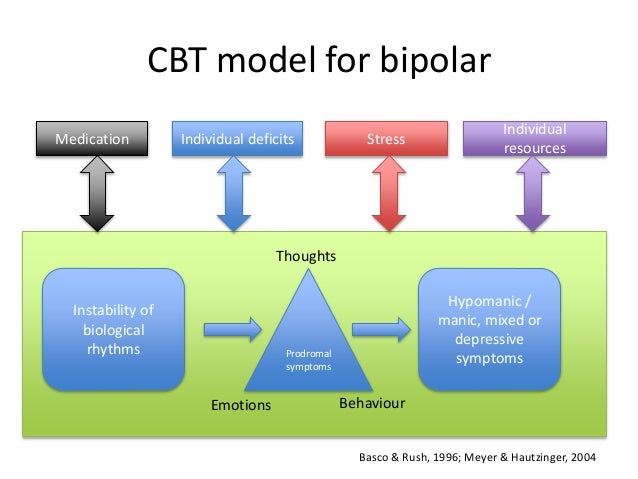
Is bipolar disorder biological or psychological
The Neurobiology of Bipolar Disorder: An Integrated Approach
1. Hirschfeld RM. Differential diagnosis of bipolar disorder and major depressive disorder. J Affect Disord. 2014;169(Suppl 1):S12–S16. [PubMed] [Google Scholar]
2. Parker G. John Cade. Am J Psychiatry. 2012;169:125–126. [PubMed] [Google Scholar]
3. Muneer A. Pharmacotherapy of bipolar disorder with quetiapine: a recent literature review and an update. Clin Psychopharmacol Neurosci. 2015;13:25–35. [PMC free article] [PubMed] [Google Scholar]
4. Pregelj P. Gene environment interactions in bipolar disorder. Psychiatr Danub. 2011;23(Suppl 1):S91–S93. [PubMed] [Google Scholar]
5. Craddock N, Sklar P. Genetics of bipolar disorder. Lancet. 2013;381:1654–1662. [PubMed] [Google Scholar]
6. Assies J, Mocking RJ, Lok A, Ruhé HG, Pouwer F, Schene AH. Effects of oxidative stress on fatty acid- and one-carbon-metabolism in psychiatric and cardiovascular disease comorbidity. Acta Psychiatr Scand. 2014;130:163–180. [PMC free article] [PubMed] [Google Scholar]
7. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858–873. [PubMed] [Google Scholar]
8. Grande I, Magalhães PV, Kunz M, Vieta E, Kapczinski F. Mediators of allostasis and systemic toxicity in bipolar disorder. Physiol Behav. 2012;106:46–50. [PubMed] [Google Scholar]
9. Gama CS, Kunz M, Magalhães PV, Kapczinski F. Staging and neuroprogression in bipolar disorder: a systematic review of the literature. Rev Bras Psiquiatr. 2013;35:70–74. [PubMed] [Google Scholar]
10. Rosa AR, Magalhães PV, Czepielewski L, Sulzbach MV, Goi PD, Vieta E, et al. Clinical staging in bipolar disorder: focus on cognition and functioning. J Clin Psychiatry. 2014;75:e450–e456. [PubMed] [Google Scholar]
11. Weinstock LM, Gaudiano BA, Epstein-Lubow G, Tezanos K, Celis-Dehoyos CE, Miller IW. Medication burden in bipolar disorder: a chart review of patients at psychiatric hospital admission.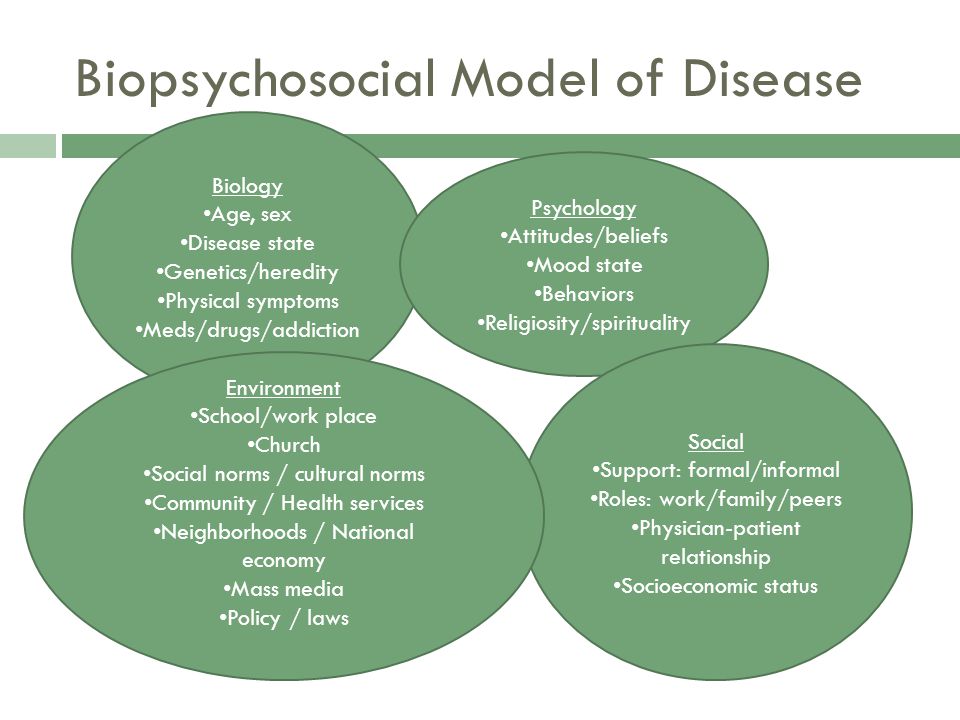 Psychiatry Res. 2014;216:24–30. [PMC free article] [PubMed] [Google Scholar]
Psychiatry Res. 2014;216:24–30. [PMC free article] [PubMed] [Google Scholar]
12. Fries GR, Pfaffenseller B, Stertz L, Paz AV, Dargél AA, Kunz M, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14:667–675. [PubMed] [Google Scholar]
13. Girshkin L, Matheson SL, Shepherd AM, Green MJ. Morning cortisol levels in schizophrenia and bipolar disorder: a metaanalysis. Psychoneuroendocrinology. 2014;49:187–206. [PubMed] [Google Scholar]
14. Watson S, Gallagher P, Ritchie JC, Ferrier IN, Young AH. Hypothalamic-pituitary-adrenal axis function in patients with bipolar disorder. Br J Psychiatry. 2004;184:496–502. [PubMed] [Google Scholar]
15. Ellenbogen MA, Santo JB, Linnen AM, Walker CD, Hodgins S. High cortisol levels in the offspring of parents with bipolar disorder during two weeks of daily sampling. Bipolar Disord. 2010;12:77–86. [PubMed] [Google Scholar]
16. Binder EB. The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders.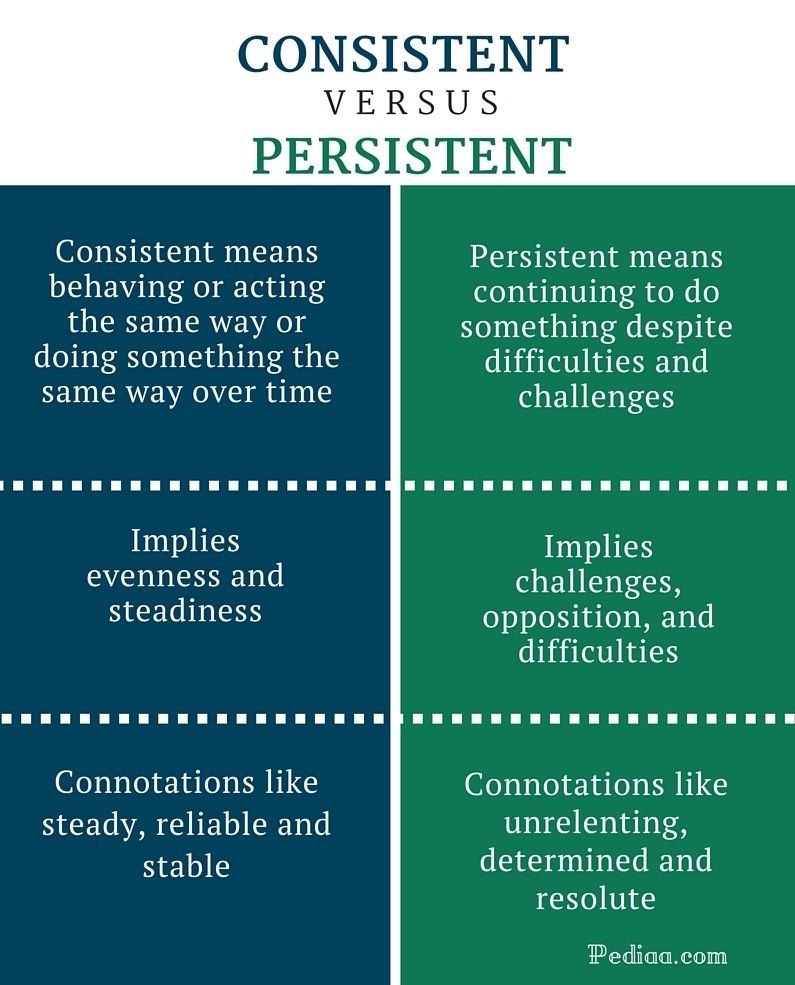 Psychoneuroendocrinology. 2009;34(Suppl 1):S186–S195. [PubMed] [Google Scholar]
Psychoneuroendocrinology. 2009;34(Suppl 1):S186–S195. [PubMed] [Google Scholar]
17. Scammell JG, Denny WB, Valentine DL, Smith DF. Overexpression of the FK506-binding immunophilin FKBP51 is the common cause of glucocorticoid resistance in three New World primates. Gen Comp Endocrinol. 2001;124:152–165. [PubMed] [Google Scholar]
18. Vermeer H, Hendriks-Stegeman BI, van der Burg B, van Buul-Offers SC, Jansen M. Glucocorticoid-induced increase in lymphocytic FKBP51 messenger ribonucleic acid expression: a potential marker for glucocorticoid sensitivity, potency, and bioavailability. J Clin Endocrinol Metab. 2003;88:277–284. [PubMed] [Google Scholar]
19. Huzayyin AA, Andreazza AC, Turecki G, Cruceanu C, Rouleau GA, Alda M, et al. Decreased global methylation in patients with bipolar disorder who respond to lithium. Int J Neuropsychopharmacol. 2014;17:561–569. [PubMed] [Google Scholar]
20. Yang X, Ewald ER, Huo Y, Tamashiro KL, Salvatori R, Sawa A, et al. Glucocorticoid-induced loss of DNA methylation in non-neuronal cells and potential involvement of DNMT1 in epigenetic regulation of Fkbp5.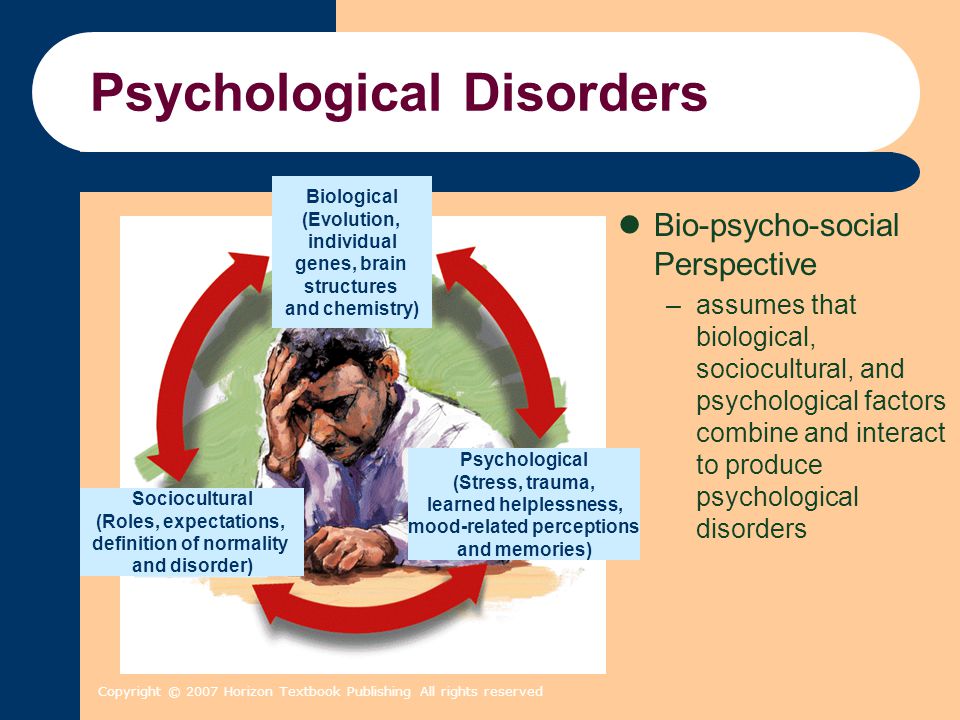 Biochem Biophys Res Commun. 2012;420:570–575. [PMC free article] [PubMed] [Google Scholar]
Biochem Biophys Res Commun. 2012;420:570–575. [PMC free article] [PubMed] [Google Scholar]
21. Fries GR, Vasconcelos-Moreno MP, Gubert C, dos Santos BT, Sartori J, Eisele B, et al. Hypothalamic-pituitary-adrenal axis dysfunction and illness progression in bipolar disorder. Int J Neuropsychopharmacol. 2014;18:pii: pyu043. [Google Scholar]
22. Uyanik V, Tuglu C, Gorgulu Y, Kunduracilar H, Uyanik MS. Assessment of cytokine levels and hs-CRP in bipolar I disorder before and after treatment. Psychiatry Res. 2015;228:386–392. [PubMed] [Google Scholar]
23. Bai YM, Su TP, Tsai SJ, Wen-Fei C, Li CT, Pei-Chi T, et al. Comparison of inflammatory cytokine levels among type I/type II and manic/hypomanic/euthymic/depressive states of bipolar disorder. J Affect Disord. 2014;166:187–192. [PubMed] [Google Scholar]
24. Leboyer M, Soreca I, Scott J, Frye M, Henry C, Tamouza R, et al. Can bipolar disorder be viewed as a multi-system inflammatory disease. J Affect Disord. 2012;141:1–10. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
25. Miller GE, Chen E, Sze J, Marin T, Arevalo JM, Doll R, et al. A functional genomic fingerprint of chronic stress in humans: blunted glucocorticoid and increased NF-kappaB signaling. Biol Psychiatry. 2008;64:266–272. [PMC free article] [PubMed] [Google Scholar]
26. Jones KA, Thomsen C. The role of the innate immune system in psychiatric disorders. Mol Cell Neurosci. 2013;53:52–62. [PubMed] [Google Scholar]
27. Barbosa IG, Bauer ME, Machado-Vieira R, Teixeira AL. Cytokines in bipolar disorder: paving the way for neuroprogression. Neural Plast. 2014;2014:360481. [PMC free article] [PubMed] [Google Scholar]
28. Brambilla P, Bellani M, Isola M, Bergami A, Marinelli V, Dusi N, et al. Increased M1/decreased M2 signature and signs of Th2/Th3 shift in chronic patients with bipolar disorder, but not in those with schizophrenia. Transl Psychiatry. 2014;4:e406. [PMC free article] [PubMed] [Google Scholar]
29. Fiedorowicz JG, Prossin AR, Johnson CP, Christensen GE, Magnotta VA, Wemmie JA.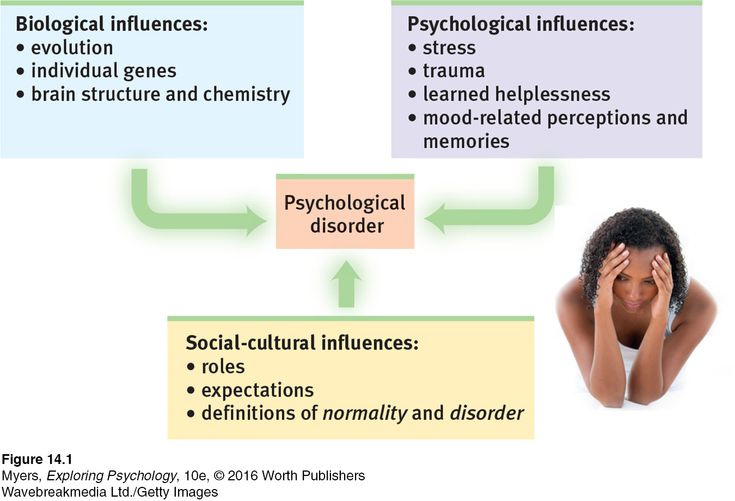 Peripheral inflammation during abnormal mood states in bipolar I disorder. J Affect Disord. 2015;187:172–178. [PMC free article] [PubMed] [Google Scholar]
Peripheral inflammation during abnormal mood states in bipolar I disorder. J Affect Disord. 2015;187:172–178. [PMC free article] [PubMed] [Google Scholar]
30. Li H, Hong W, Zhang C, Wu Z, Wang Z, Yuan C, et al. IL-23 and TGF-β1 levels as potential predictive biomarkers in treatment of bipolar I disorder with acute manic episode. J Affect Disord. 2015;174:361–366. [PubMed] [Google Scholar]
31. Wieck A, Grassi-Oliveira R, do Prado CH, Rizzo LB, de Oliveira AS, Kommers-Molina J, et al. Pro-inflammatory cytokines and soluble receptors in response to acute psychosocial stress: differential reactivity in bipolar disorder. Neurosci Lett. 2014;580:17–21. [PubMed] [Google Scholar]
32. Bai YM, Su TP, Li CT, Tsai SJ, Chen MH, Tu PC, et al. Comparison of pro-inflammatory cytokines among patients with bipolar disorder and unipolar depression and normal controls. Bipolar Disord. 2015;17:269–277. [PubMed] [Google Scholar]
33. Barbosa IG, Morato IB, de Miranda AS, Bauer ME, Soares JC, Teixeira AL. A preliminary report of increased plasma levels of IL-33 in bipolar disorder: further evidence of pro-inflammatory status. J Affect Disord. 2014;157:41–44. [PubMed] [Google Scholar]
A preliminary report of increased plasma levels of IL-33 in bipolar disorder: further evidence of pro-inflammatory status. J Affect Disord. 2014;157:41–44. [PubMed] [Google Scholar]
34. Doganavsargil-Baysal O, Cinemre B, Aksoy UM, Akbas H, Metin O, Fettahoglu C, et al. Levels of TNF-α, soluble TNF receptors (sTNFR1, sTNFR2), and cognition in bipolar disorder. Hum Psychopharmacol. 2013;28:160–167. [PubMed] [Google Scholar]
35. Agorastos A, Hauger RL, Barkauskas DA, Moeller-Bertram T, Clopton PL, Haji U, et al. Circadian rhythmicity, variability and correlation of interleukin-6 levels in plasma and cerebrospinal fluid of healthy men. Psychoneuroendocrinology. 2014;44:71–82. [PubMed] [Google Scholar]
36. Munkholm K, Weikop P, Kessing LV, Vinberg M. Elevated levels of IL-6 and IL-18 in manic and hypomanic states in rapid cycling bipolar disorder patients. Brain Behav Immun. 2015;43:205–213. [PubMed] [Google Scholar]
37. Steiner J, Walter M, Gos T, Guillemin GJ, Bernstein HG, Sarnyai Z, et al.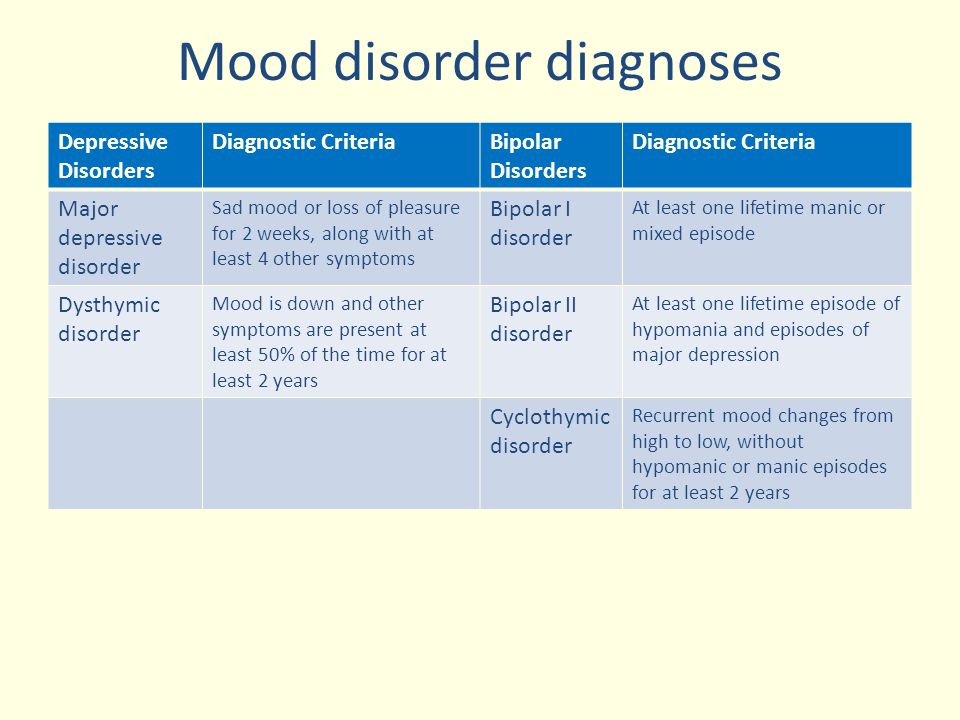 Severe depression is associated with increased microglial quinolinic acid in subregions of the anteriorcingulate gyrus: evidence for an immune-modulated glutamatergic neurotransmission. J Neuroinflammation. 2011;8:94. [PMC free article] [PubMed] [Google Scholar]
Severe depression is associated with increased microglial quinolinic acid in subregions of the anteriorcingulate gyrus: evidence for an immune-modulated glutamatergic neurotransmission. J Neuroinflammation. 2011;8:94. [PMC free article] [PubMed] [Google Scholar]
38. Mihara M, Hashizume M, Yoshida H, Suzuki M, Shiina M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci (Lond) 2012;122:143–159. [PubMed] [Google Scholar]
39. Düsterhöft S, Höbel K, Oldefest M, Lokau J, Waetzig GH, Chalaris A, et al. A disintegrin and metalloprotease 17 dynamic interaction sequence, the sweet tooth for the human interleukin 6 receptor. J Biol Chem. 2014;289:16336–16348. [PMC free article] [PubMed] [Google Scholar]
40. Rose-John S. IL-6 trans-signaling via the soluble IL-6 receptor: importance for the pro-inflammatory activities of IL-6. Int J Biol Sci. 2012;8:1237–1247. [PMC free article] [PubMed] [Google Scholar]
41. Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S.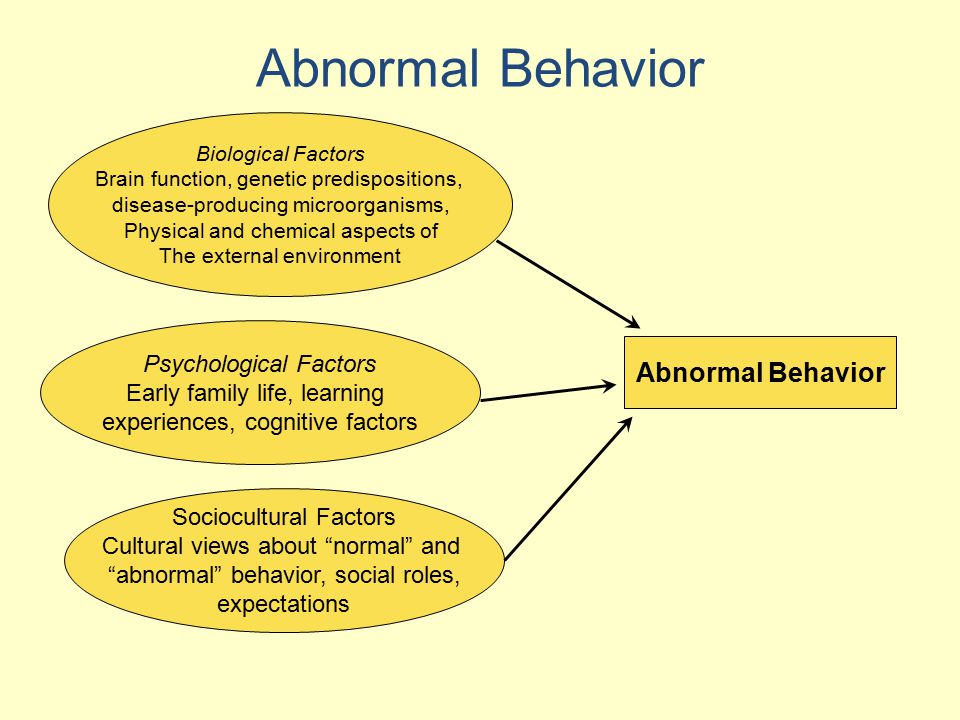 The proand anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878–888. [PubMed] [Google Scholar]
The proand anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878–888. [PubMed] [Google Scholar]
42. Chalaris A, Rabe B, Paliga K, Lange H, Laskay T, Fielding CA, et al. Apoptosis is a natural stimulus of IL6R shedding and contributes to the proinflammatory trans-signaling function of neutrophils. Blood. 2007;110:1748–1755. [PubMed] [Google Scholar]
43. Barkhausen T, Tschernig T, Rosenstiel P, van Griensven M, Vonberg RP, Dorsch M, et al. Selective blockade of interleukin-6 trans-signaling improves survival in a murine polymicrobial sepsis model. Crit Care Med. 2011;39:1407–1413. [PubMed] [Google Scholar]
44. Scheller J, Chalaris A, Garbers C, Rose-John S. ADAM17: a molecular switch to control inflammation and tissue regeneration. Trends Immunol. 2011;32:380–387. [PubMed] [Google Scholar]
45. Waetzig GH, Rose-John S. Hitting a complex target: an update on interleukin-6 trans-signalling. Expert Opin Ther Targets. 2012;16:225–236. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
46. Maes M, Anderson G, Kubera M, Berk M. Targeting classical IL-6 signalling or IL-6 trans-signalling in depression. Expert Opin Ther Targets. 2014;18:495–512. [PubMed] [Google Scholar]
47. Fonseka TM, McIntyre RS, Soczynska JK, Kennedy SH. Novel investigational drugs targeting IL-6 signaling for the treatment of depression. Expert Opin Investig Drugs. 2015;24:459–475. [PubMed] [Google Scholar]
48. Lushchak VI. Free radicals, reactive oxygen species, oxidative stress and its classification. Chem Biol Interact. 2014;224C:164–175. [PubMed] [Google Scholar]
49. Nayernia Z, Jaquet V, Krause KH. New insights on NOX enzymes in the central nervous system. Antioxid Redox Signal. 2014;20:2815–2837. [PMC free article] [PubMed] [Google Scholar]
50. Sorce S, Krause KH. NOX enzymes in the central nervous system: from signaling to disease. Antioxid Redox Signal. 2009;11:2481–2504. [PubMed] [Google Scholar]
51. Sorce S, Schiavone S, Tucci P, Colaianna M, Jaquet V, Cuomo V, et al. The NADPH oxidase NOX2 controls glutamate release: a novel mechanism involved in psychosis-like ketamine responses. J Neurosci. 2010;30:11317–11325. [PMC free article] [PubMed] [Google Scholar]
The NADPH oxidase NOX2 controls glutamate release: a novel mechanism involved in psychosis-like ketamine responses. J Neurosci. 2010;30:11317–11325. [PMC free article] [PubMed] [Google Scholar]
52. Hu X, Zhou H, Zhang D, Yang S, Qian L, Wu HM, et al. Clozapine protects dopaminergic neurons from inflammation-induced damage by inhibiting microglial overactivation. J Neuroimmune Pharmacol. 2012;7:187–201. [PMC free article] [PubMed] [Google Scholar]
53. Fatokun AA, Stone TW, Smith RA. Oxidative stress in neurodegeneration and available means of protection. Front Biosci. 2008;13:3288–3311. [PubMed] [Google Scholar]
54. Morris G, Berk M. The many roads to mitochondrial dysfunction in neuroimmune and neuropsychiatric disorders. BMC Med. 2015;13:68. [PMC free article] [PubMed] [Google Scholar]
55. Nguyen D, Alavi MV, Kim KY, Kang T, Scott RT, Noh YH, et al. A new vicious cycle involving glutamate excitotoxicity, oxidative stress and mitochondrial dynamics. Cell Death Dis. 2011;2:e240. [PMC free article] [PubMed] [Google Scholar]
2011;2:e240. [PMC free article] [PubMed] [Google Scholar]
56. Ventriglio A, Gentile A, Baldessarini RJ, Bellomo A. Early-life stress and psychiatric disorders: epidemiology, neurobiology and innovative pharmacological targets. Curr Pharm Des. 2015;21:1379–1387. [PubMed] [Google Scholar]
57. Gu Y, Dee CM, Shen J. Interaction of free radicals, matrix metalloproteinases and caveolin-1 impacts blood-brain barrier permeability. Front Biosci (Schol Ed) 2011;3:1216–1231. [PubMed] [Google Scholar]
58. Siwek M, Sowa-Kućma M, Dudek D, Styczeń K, Szewczyk B, Kotarska K, et al. Oxidative stress markers in affective disorders. Pharmacol Rep. 2013;65:1558–1571. [PubMed] [Google Scholar]
59. Bitanihirwe BK, Woo TU. Oxidative stress in schizophrenia: an integrated approach. Neurosci Biobehav Rev. 2011;35:878–893. [PMC free article] [PubMed] [Google Scholar]
60. Ramalingam M, Kim SJ. Reactive oxygen/nitrogen species and their functional correlations in neurodegenerative diseases. J Neural Transm (Vienna) 2012;119:891–910. [PubMed] [Google Scholar]
J Neural Transm (Vienna) 2012;119:891–910. [PubMed] [Google Scholar]
61. Andreazza AC, Kauer-Sant 'anna M, Frey BN, Bond DJ, Kapczinski F, Young LT, et al. Oxidative stress markers in bipolar disorder: a meta-analysis. J Affect Disord. 2008;111:135–144. [PubMed] [Google Scholar]
62. Miller E, Morel A, Saso L, Saluk J. Isoprostanes and neuroprostanes as biomarkers of oxidative stress in neurodegenerative diseases. Oxid Med Cell Longev. 2014;2014:572491. [PMC free article] [PubMed] [Google Scholar]
63. Black CN, Bot M, Scheffer PG, Cuijpers P, Penninx BW. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology. 2015;51:164–175. [PubMed] [Google Scholar]
64. Lima IM, Barros A, Rosa DV, Albuquerque M, Malloy-Diniz L, Neves FS, et al. Analysis of telomere attrition in bipolar disorder. J Affect Disord. 2014;172C:43–47. [PubMed] [Google Scholar]
65. Brown NC, Andreazza AC, Young LT. An updated meta-analysis of oxidative stress markers in bipolar disorder.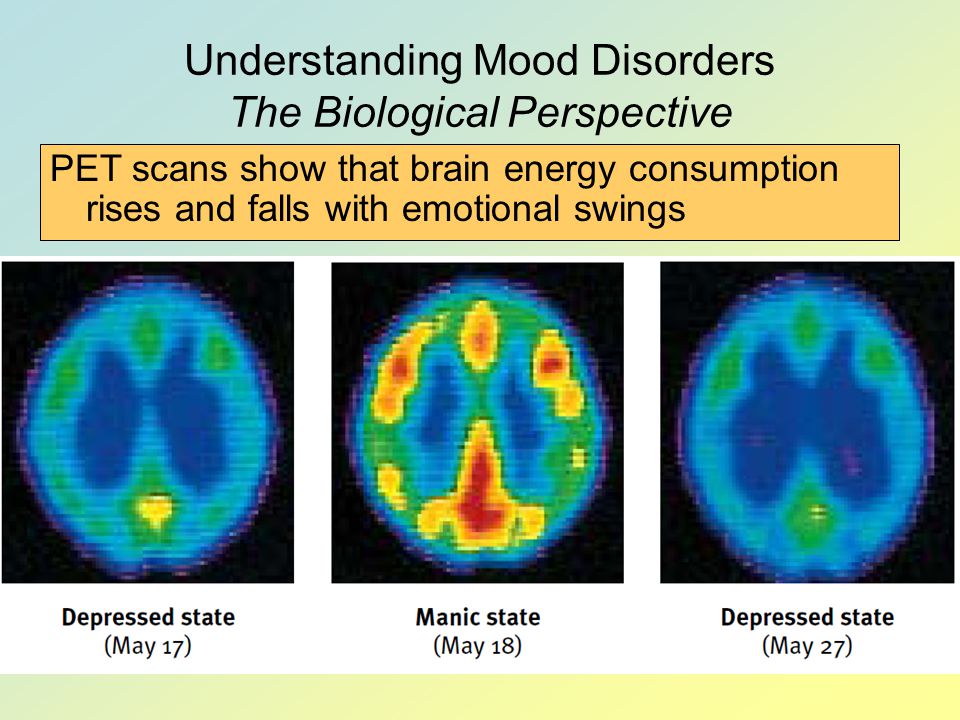 Psychiatry Res. 2014;218:61–68. [PubMed] [Google Scholar]
Psychiatry Res. 2014;218:61–68. [PubMed] [Google Scholar]
66. Joshi YB, Praticò D. Lipid peroxidation in psychiatric illness: overview of clinical evidence. Oxid Med Cell Longev. 2014;2014:828702. [PMC free article] [PubMed] [Google Scholar]
67. Schiavone S, Jaquet V, Sorce S, Dubois-Dauphin M, Hultqvist M, Bäckdahl L, et al. NADPH oxidase elevations in pyramidal neurons drive psychosocial stress-induced neuropathology. Transl Psychiatry. 2012;2:e111. [PMC free article] [PubMed] [Google Scholar]
68. Liang D, Li G, Liao X, Yu D, Wu J, Zhang M. Developmental loss of parvalbumin-positive cells in the prefrontal cortex and psychiatric anxiety after intermittent hypoxia exposures in neonatal rats might be mediated by NADPH oxidase-2. Behav Brain Res. 2016;296:134–140. [PubMed] [Google Scholar]
69. Schiavone S, Colaianna M, Curtis L. Impact of early life stress on the pathogenesis of mental disorders: relation to brain oxidative stress. Curr Pharm Des. 2015;21:1404–1412.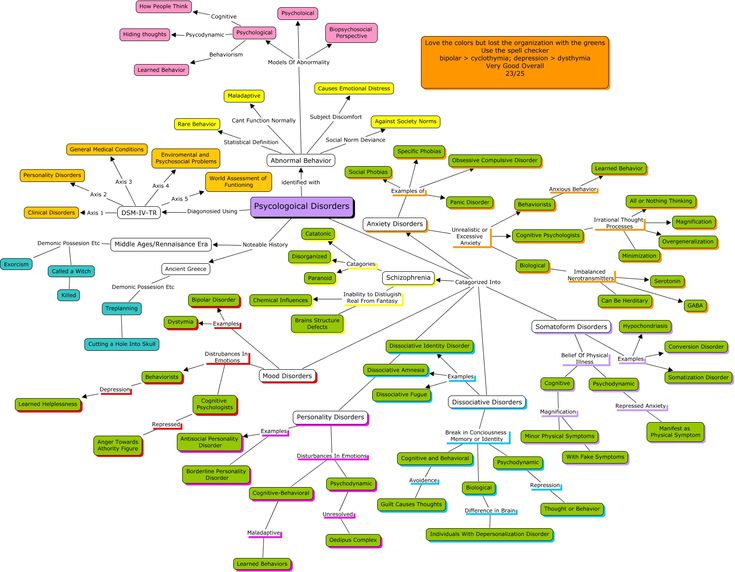 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
70. Schiavone S, Jaquet V, Trabace L, Krause KH. Severe life stress and oxidative stress in the brain: from animal models to human pathology. Antioxid Redox Signal. 2013;18:1475–1490. [PMC free article] [PubMed] [Google Scholar]
71. Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87:245–313. [PubMed] [Google Scholar]
72. Heisler JM, O'Connor JC. Indoleamine 2,3-dioxygenase-dependent neurotoxic kynurenine metabolism mediates inflammation-induced deficit in recognition memory. Brain Behav Immun. 2015;50:115–124. [PMC free article] [PubMed] [Google Scholar]
73. Müller N, Schwarz MJ. Neuroimmune-endocrine crosstalk in schizophrenia and mood disorders. Expert Rev Neurother. 2006;6:1017–1038. [PubMed] [Google Scholar]
74. Modabbernia A, Taslimi S, Brietzke E, Ashrafi M. Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry. 2013;74:15–25.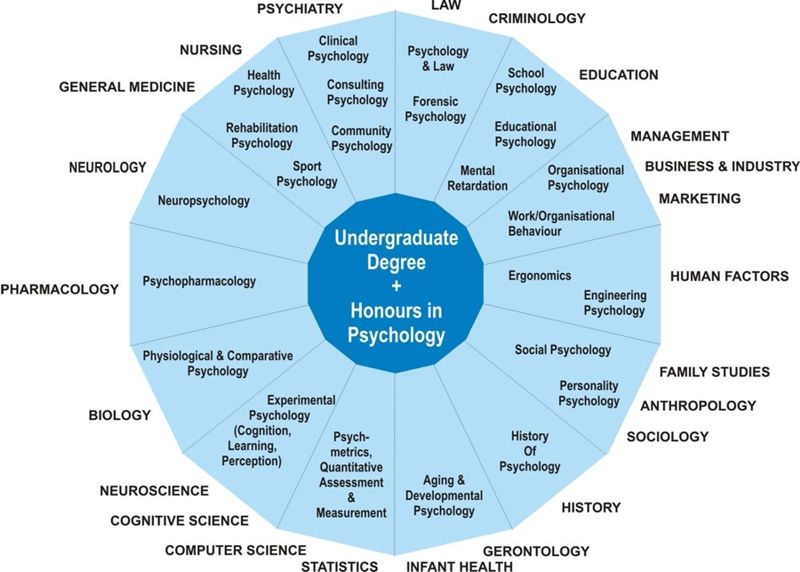 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
75. Musselman D, Royster EB, Wang M, Long Q, Trimble LM, Mann TK, et al. The impact of escitalopram on IL-2-induced neuroendocrine, immune, and behavioral changes in patients with malignant melanoma: preliminary findings. Neuropsychopharmacology. 2013;38:1921–1928. [PMC free article] [PubMed] [Google Scholar]
76. Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70:31–41. [PMC free article] [PubMed] [Google Scholar]
77. Myint AM. Kynurenines: from the perspective of major psychiatric disorders. FEBS J. 2012;279:1375–1385. [PubMed] [Google Scholar]
78. Campbell BM, Charych E, Lee AW, Möller T. Kynurenines in CNS disease: regulation by inflammatory cytokines. Front Neurosci. 2014;8:12. [PMC free article] [PubMed] [Google Scholar]
79. Schwarcz R, Bruno JP, Muchowski PJ, Wu HQ. Kynurenines in the mammalian brain: when physiology meets pathology. Nat Rev Neurosci. 2012;13:465–477. [PMC free article] [PubMed] [Google Scholar]
Schwarcz R, Bruno JP, Muchowski PJ, Wu HQ. Kynurenines in the mammalian brain: when physiology meets pathology. Nat Rev Neurosci. 2012;13:465–477. [PMC free article] [PubMed] [Google Scholar]
80. Dantzer R, Walker AK. Is there a role for glutamate-mediated excitotoxicity in inflammation-induced depression? J Neural Transm (Vienna) 2014;121:925–932. [PMC free article] [PubMed] [Google Scholar]
81. Erhardt S, Olsson SK, Engberg G. Pharmacological manipulation of kynurenic acid: potential in the treatment of psychiatric disorders. CNS Drugs. 2009;23:91–101. [PubMed] [Google Scholar]
82. Takaki J, Fujimori K, Miura M, Suzuki T, Sekino Y, Sato K. L-glutamate released from activated microglia downregulates astrocytic L-glutamate transporter expression in neuroinflammation: the 'collusion' hypothesis for increased extracellular L-glutamate concentration in neuroinflammation. J Neuroinflammation. 2012;9:275. [PMC free article] [PubMed] [Google Scholar]
83. Savitz J, Dantzer R, Wurfel BE, Victor TA, Ford BN, Bodurka J, et al. Neuroprotective kynurenine metabolite indices are abnormally reduced and positively associated with hippocampal and amygdalar volume in bipolar disorder. Psychoneuroendocrinology. 2015;52:200–211. [PMC free article] [PubMed] [Google Scholar]
Neuroprotective kynurenine metabolite indices are abnormally reduced and positively associated with hippocampal and amygdalar volume in bipolar disorder. Psychoneuroendocrinology. 2015;52:200–211. [PMC free article] [PubMed] [Google Scholar]
84. Leibowitz A, Boyko M, Shapira Y, Zlotnik A. Blood glutamate scavenging: insight into neuroprotection. Int J Mol Sci. 2012;13:10041–10066. [PMC free article] [PubMed] [Google Scholar]
85. Myint AM, Kim YK. Network beyond IDO in psychiatric disorders: revisiting neurodegeneration hypothesis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:304–313. [PubMed] [Google Scholar]
86. Milhiet V, Boudebesse C, Bellivier F, Drouot X, Henry C, Leboyer M, et al. Circadian abnormalities as markers of susceptibility in bipolar disorders. Front Biosci (Schol Ed) 2014;6:120–137. [PubMed] [Google Scholar]
87. Boudebesse C, Geoffroy PA, Bellivier F, Henry C, Folkard S, Leboyer M, et al. Correlations between objective and subjective sleep and circadian markers in remitted patients with bipolar disorder.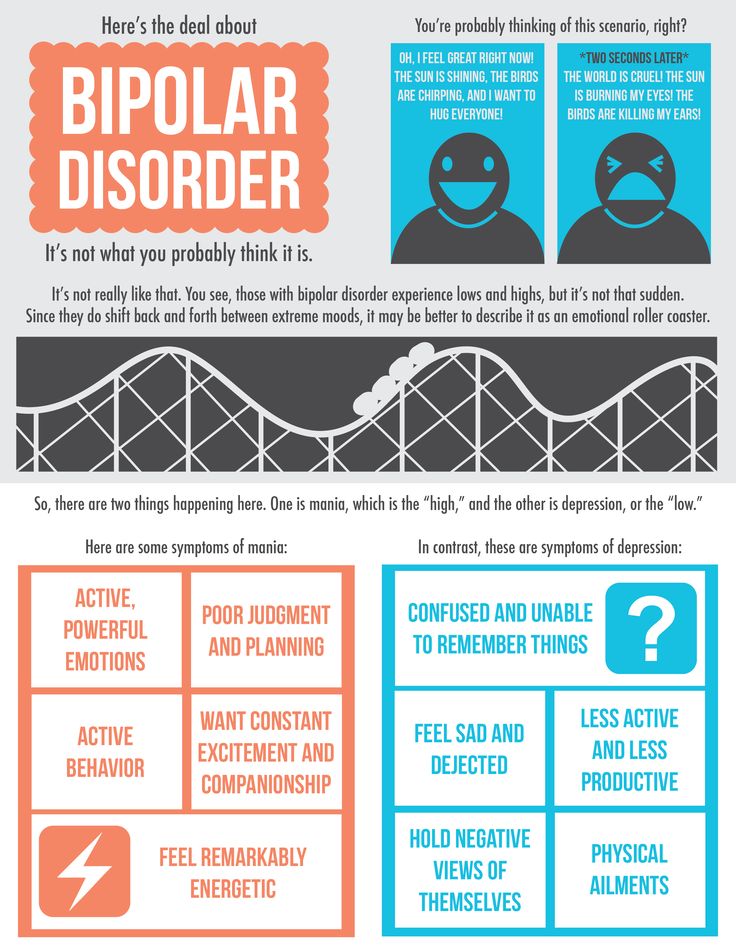 Chronobiol Int. 2014;31:698–704. [PubMed] [Google Scholar]
Chronobiol Int. 2014;31:698–704. [PubMed] [Google Scholar]
88. Gonzalez R. The relationship between bipolar disorder and biological rhythms. J Clin Psychiatry. 2014;75:e323–e331. [PubMed] [Google Scholar]
89. Abreu T, Bragança M. The bipolarity of light and dark: a review on Bipolar Disorder and circadian cycles. J Affect Disord. 2015;185:219–229. [PubMed] [Google Scholar]
90. Scott J. Clinical parameters of circadian rhythms in affective disorders. Eur Neuropsychopharmacol. 2011;21(Suppl 4):S671–S675. [PubMed] [Google Scholar]
91. Ramanathan C, Xu H, Khan SK, Shen Y, Gitis PJ, Welsh DK, et al. Cell type-specific functions of period genes revealed by novel adipocyte and hepatocyte circadian clock models. PLoS Genet. 2014;10:e1004244. [PMC free article] [PubMed] [Google Scholar]
92. Gonzalez R, Tamminga CA, Tohen M, Suppes T. The relationship between affective state and the rhythmicity of activity in bipolar disorder. J Clin Psychiatry. 2014;75:e317–e322. [PMC free article] [PubMed] [Google Scholar]
93. Menaker M, Murphy ZC, Sellix MT. Central control of peripheral circadian oscillators. Curr Opin Neurobiol. 2013;23:741–746. [PubMed] [Google Scholar]
Menaker M, Murphy ZC, Sellix MT. Central control of peripheral circadian oscillators. Curr Opin Neurobiol. 2013;23:741–746. [PubMed] [Google Scholar]
94. Ko CH, Takahashi JS. Molecular components of the mammalian circadian clock. Hum Mol Genet. 2006 Spec No 2;15:R271–R277. [PubMed] [Google Scholar]
95. McClung CA. Circadian genes, rhythms and the biology of mood disorders. Pharmacol Ther. 2007;114:222–232. [PMC free article] [PubMed] [Google Scholar]
96. Gibbs JE, Blaikley J, Beesley S, Matthews L, Simpson KD, Boyce SH, et al. The nuclear receptor REV-ERBα mediates circadian regulation of innate immunity through selective regulation of inflammatory cytokines. Proc Natl Acad Sci U S A. 2012;109:582–587. [PMC free article] [PubMed] [Google Scholar]
97. Charmandari E, Chrousos GP, Lambrou GI, Pavlaki A, Koide H, Ng SS, et al. Peripheral CLOCK regulates target-tissue glucocorticoid receptor transcriptional activity in a circadian fashion in man. PLoS One. 2011;6:e25612.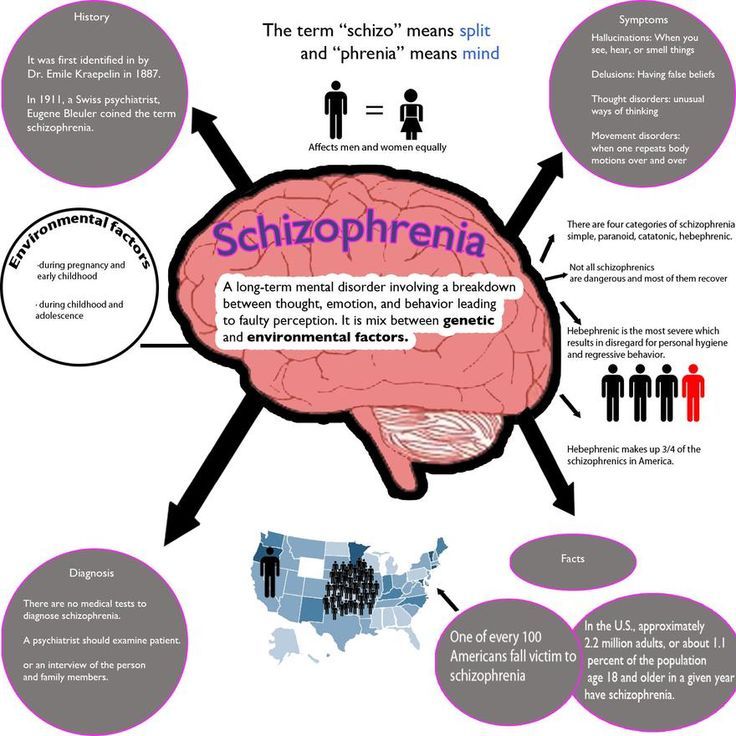 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
98. Landgraf D, McCarthy MJ, Welsh DK. Circadian clock and stress interactions in the molecular biology of psychiatric disorders. Curr Psychiatry Rep. 2014;16:483. [PubMed] [Google Scholar]
99. Cagampang FR, Bruce KD. The role of the circadian clock system in nutrition and metabolism. Br J Nutr. 2012;108:381–392. [PubMed] [Google Scholar]
100. Kim TW, Jeong JH, Hong SC. The impact of sleep and circadian disturbance on hormones and metabolism. Int J Endocrinol. 2015;2015:591729. [PMC free article] [PubMed] [Google Scholar]
101. Bellet MM, Orozco-Solis R, Sahar S, Eckel-Mahan K, Sassone-Corsi P. The time of metabolism: NAD+, SIRT1, and the circadian clock. Cold Spring Harb Symp Quant Biol. 2011;76:31–38. [PubMed] [Google Scholar]
102. Nakahata Y, Sahar S, Astarita G, Kaluzova M, Sassone-Corsi P. Circadian control of the NAD+ salvage pathway by CLOCKSIRT1. Science. 2009;324:654–657. [PMC free article] [PubMed] [Google Scholar]
103. Pinnock SB, Herbert J. Brain-derived neurotropic factor and neurogenesis in the adult rat dentate gyrus: interactions with corticosterone. Eur J Neurosci. 2008;27:2493–2500. [PMC free article] [PubMed] [Google Scholar]
Pinnock SB, Herbert J. Brain-derived neurotropic factor and neurogenesis in the adult rat dentate gyrus: interactions with corticosterone. Eur J Neurosci. 2008;27:2493–2500. [PMC free article] [PubMed] [Google Scholar]
104. AlAhmed S, Herbert J. Effect of agomelatine and its interaction with the daily corticosterone rhythm on progenitor cell proliferation in the dentate gyrus of the adult rat. Neuropharmacology. 2010;59:375–379. [PubMed] [Google Scholar]
105. Hope S, Melle I, Aukrust P, Steen NE, Birkenaes AB, Lorentzen S, et al. Similar immune profile in bipolar disorder and schizophrenia: selective increase in soluble tumor necrosis factor receptor I and von Willebrand factor. Bipolar Disord. 2009;11:726–734. [PubMed] [Google Scholar]
106. Hope S, Ueland T, Steen NE, Dieset I, Lorentzen S, Berg AO, et al. Interleukin 1 receptor antagonist and soluble tumor necrosis factor receptor 1 are associated with general severity and psychotic symptoms in schizophrenia and bipolar disorder. Schizophr Res. 2013;145:36–42. [PubMed] [Google Scholar]
Schizophr Res. 2013;145:36–42. [PubMed] [Google Scholar]
107. Sinclair D, Fillman SG, Webster MJ, Weickert CS. Dysregulation of glucocorticoid receptor co-factors FKBP5, BAG1 and PTGES3 in prefrontal cortex in psychotic illness. Sci Rep. 2013;3:3539. [PMC free article] [PubMed] [Google Scholar]
108. Wang JF, Shao L, Sun X, Young LT. Increased oxidative stress in the anterior cingulate cortex of subjects with bipolar disorder and schizophrenia. Bipolar Disord. 2009;11:523–529. [PubMed] [Google Scholar]
109. Etain B, Milhiet V, Bellivier F, Leboyer M. Genetics of circadian rhythms and mood spectrum disorders. Eur Neuropsychopharmacol. 2011;21(Suppl 4):S676–S682. [PubMed] [Google Scholar]
110. De Berardis D, Fornaro M, Serroni N, Campanella D, Rapini G, Olivieri L, et al. Agomelatine beyond borders: current evidences of its efficacy in disorders other than major depression. Int J Mol Sci. 2015;16:1111–1130. [PMC free article] [PubMed] [Google Scholar]
111. Kauer-Sant'Anna M, Kapczinski F, Andreazza AC, Bond DJ, Lam RW, Young LT, et al.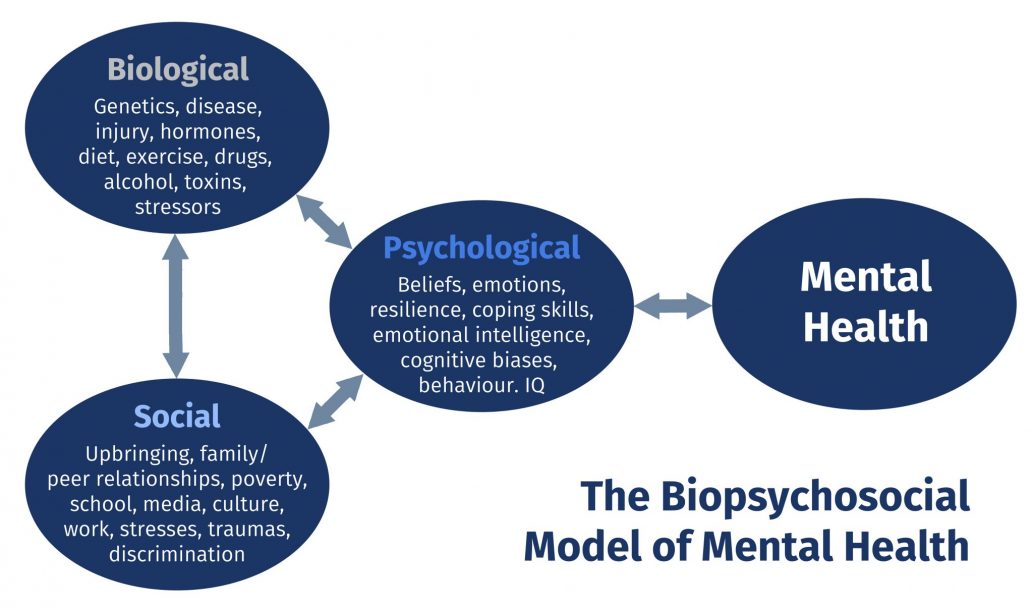 Brain-derived neurotrophic factor and inflammatory markers in patients with early- vs. late-stage bipolar disorder. Int J Neuropsychopharmacol. 2009;12:447–458. [PubMed] [Google Scholar]
Brain-derived neurotrophic factor and inflammatory markers in patients with early- vs. late-stage bipolar disorder. Int J Neuropsychopharmacol. 2009;12:447–458. [PubMed] [Google Scholar]
112. Andreazza AC, Kapczinski F, Kauer-Sant'Anna M, Walz JC, Bond DJ, Gonçalves CA, et al. 3-Nitrotyrosine and glutathione antioxidant system in patients in the early and late stages of bipolar disorder. J Psychiatry Neurosci. 2009;34:263–271. [PMC free article] [PubMed] [Google Scholar]
113. Elvsåshagen T, Vera E, Bøen E, Bratlie J, Andreassen OA, Josefsen D, et al. The load of short telomeres is increased and associated with lifetime number of depressive episodes in bipolar II disorder. J Affect Disord. 2011;135:43–50. [PubMed] [Google Scholar]
114. Strakowski SM, DelBello MP, Zimmerman ME, Getz GE, Mills NP, Ret J, et al. Ventricular and periventricular structural volumes in first- versus multiple-episode bipolar disorder. Am J Psychiatry. 2002;159:1841–1847. [PubMed] [Google Scholar]
115. Kapczinski F, Vieta E, Andreazza AC, Frey BN, Gomes FA, Tramontina J, et al. Allostatic load in bipolar disorder: implications for pathophysiology and treatment. Neurosci Biobehav Rev. 2008;32:675–692. [PubMed] [Google Scholar]
Kapczinski F, Vieta E, Andreazza AC, Frey BN, Gomes FA, Tramontina J, et al. Allostatic load in bipolar disorder: implications for pathophysiology and treatment. Neurosci Biobehav Rev. 2008;32:675–692. [PubMed] [Google Scholar]
116. Gaali S, Kirschner A, Cuboni S, Hartmann J, Kozany C, Balsevich G, et al. Selective inhibitors of the FK506-binding protein 51 by induced fit. Nat Chem Biol. 2015;11:33–37. [PubMed] [Google Scholar]
117. Dounay AB, Tuttle JB, Verhoest PR. Challenges and opportunities in the discovery of new therapeutics targeting the kynurenine pathway. J Med Chem. 2015;58:8762–8782. [PubMed] [Google Scholar]
Causes of Bipolar Disorder: Genes, Biology, and Experience
Bipolar disorder is a condition that involves extreme shifts in mood. Its causes may be complex, but bipolar disorder is very treatable.
Bipolar disorder has three main types: bipolar I, bipolar II, and cyclothymic disorder (also called cyclothymia).
The mood episodes you experience and their intensity can vary depending on which type of bipolar disorder you have.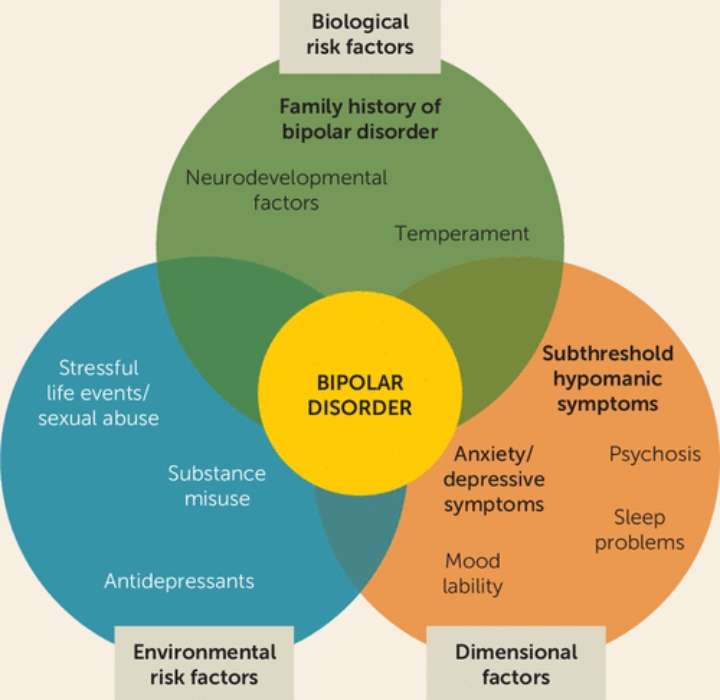
For example, you may experience mania, which is often described as an elevated, happy, and energized state. You may also experience depression that leaves you drained and disinterested in daily life.
These shifts might happen gradually, giving you time to recognize the signs of oncoming mania or depression. They can also happen swiftly, giving you little time to prepare.
If you live with bipolar disorder, you’ll already know plenty about how it makes you feel. You might know less about why you feel that way.
Hoping to learn more about its potential causes? Curious about your own chances of developing the condition? You’ve come to the right place.
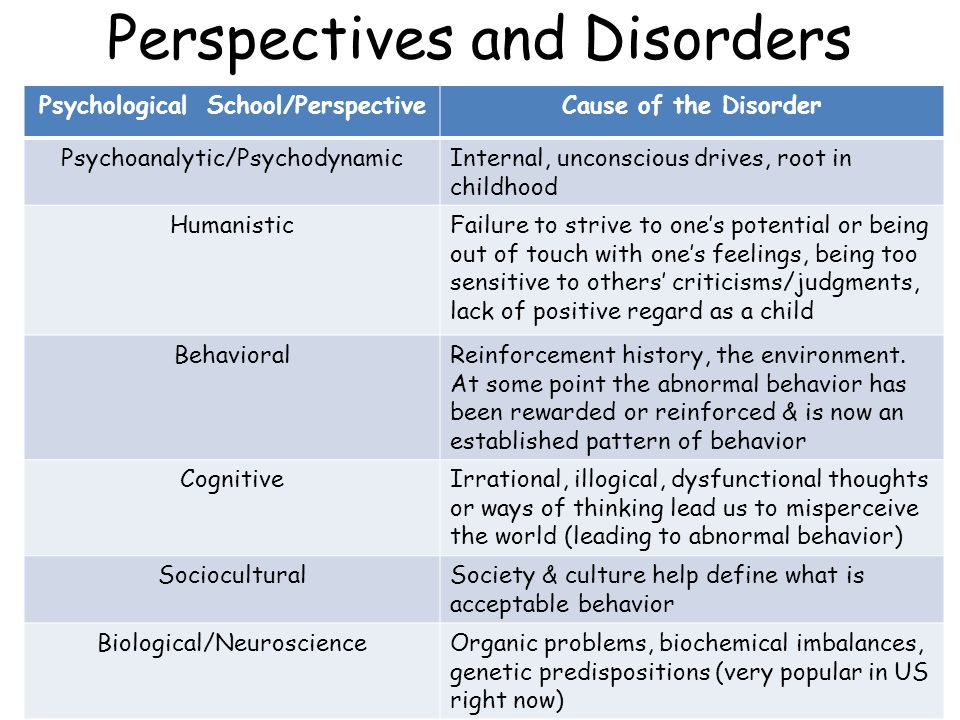
Researchers studying bipolar disorder over the past decades have several theories to explain how this condition develops. Existing evidence points to a range of possible causes rather than one specific cause.
Experts believe bipolar disorder usually develops from a combination of the following factors:
- genetics
- brain chemistry and biology
- environmental factors
If you’re noticing symptoms for the first time, you might link them to a recent source of stress, a health issue, or a new medication.
These things can absolutely trigger mood episodes, but they don’t directly cause bipolar disorder.
Bipolar disorder tends to run in families.
According to the recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), if you have an adult relative with either bipolar I or bipolar II disorder, you have an average of 10 times the chance of developing the condition yourself.
The American Psychiatric Association also reports that 80 to 90% of people with bipolar disorder have a relative living with either depression or bipolar disorder.
Related factors that influence your likelihood of developing bipolar disorder include:
- family history of depression
- family history of schizophrenia (research points to some genetic overlap between these two conditions)
- the number of family members with bipolar disorder or other mood disorders
- your relation to those family members
Generally speaking, closer kinship increases this likelihood. For example, someone whose sibling or parent has bipolar disorder has a greater chance of developing the condition than someone whose cousin or uncle has it.
For example, someone whose sibling or parent has bipolar disorder has a greater chance of developing the condition than someone whose cousin or uncle has it.
Researchers have linked two key genes, CACNA1 and ANK3, to bipolar disorder. But they note that many other genes are likely to factor in too.
What’s more, since genes make up only one part of the picture, not everyone with a family history of bipolar disorder will develop the condition.
Studies on twins support this. Evidence suggests that when one identical twin has bipolar disorder, the other has a high — but not certain — chance of the same diagnosis.
Bipolar disorder also has a neurological component.
Neurotransmitters are chemical messengers in the brain. They help relay messages between nerve cells throughout the body. These chemicals play an essential role in healthy brain function. Some of them even help regulate mood and behavior.
Older research links three main neurotransmitters to bipolar disorder:
- serotonin
- dopamine
- norepinephrine (also called noradrenaline)
Imbalances of these brain chemicals may prompt manic, depressive, or hypomanic mood episodes.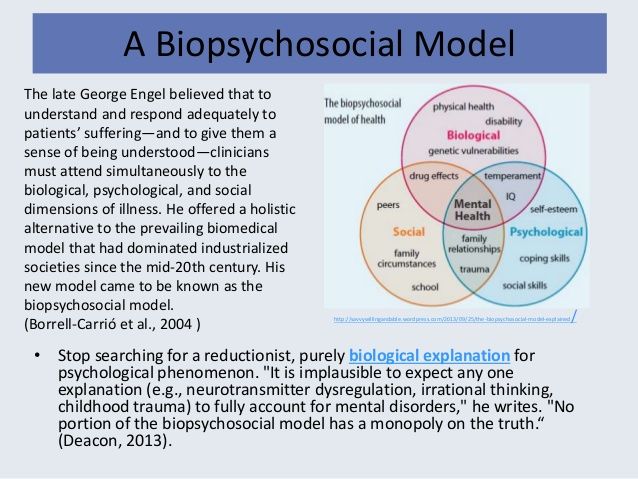 This is particularly the case when environmental triggers or other factors come into play.
This is particularly the case when environmental triggers or other factors come into play.
The role of mitochondria
Experts also believe mitochondria — which you may remember from science class as the cells that generate energy, aka “the powerhouse of the cell” — may have something to do with the development of mood disorders.
When cells don’t produce or metabolize energy as they typically would, the resulting imbalances in brain energy could lead to the changes in mood and behavior often seen with bipolar disorder.
Brain structure and gray matter
Some evidence suggests people with bipolar disorder have less gray matter in certain parts of the brain, including the temporal and frontal lobes.
These brain areas help regulate emotions and control inhibitions. A lower volume of gray matter may help explain why emotion regulation and impulse control become difficult during mood episodes.
Gray matter contains cells that help process signals and sensory information.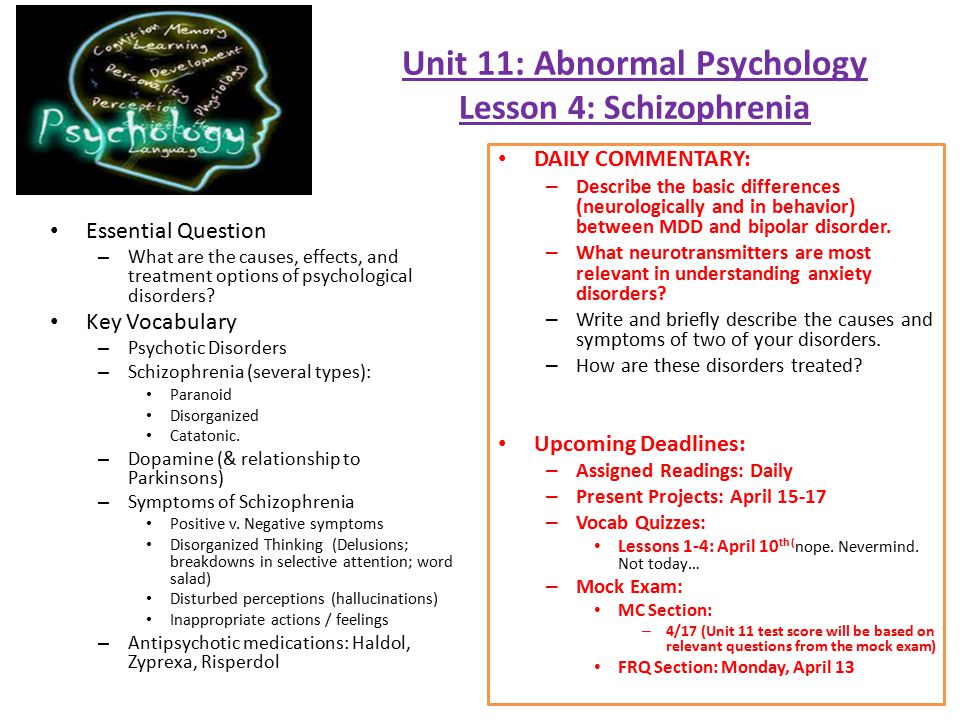
Research has also linked the hippocampus, a part of the brain implicated for learning, memory, mood, and impulse control, to mood disorders. If you have bipolar disorder, your hippocampus may have a lower total volume or a slightly altered shape.
These brain differences may not necessarily cause bipolar disorder though. Still, they offer insight on how the condition might progress and affect brain function.
Family history can certainly increase the likelihood of developing bipolar disorder, but many people with a genetic risk never develop the condition.
Various factors from your surrounding environment offer another point of connection to consider. These might include:
- personal experiences
- health and sleep
- external stress triggers
- alcohol or substance use
Research shows that childhood trauma is a risk factor for bipolar disorder, and is associated with more severe symptoms.
This is because strong emotional distress in childhood might affect your ability to regulate your emotions as an adult.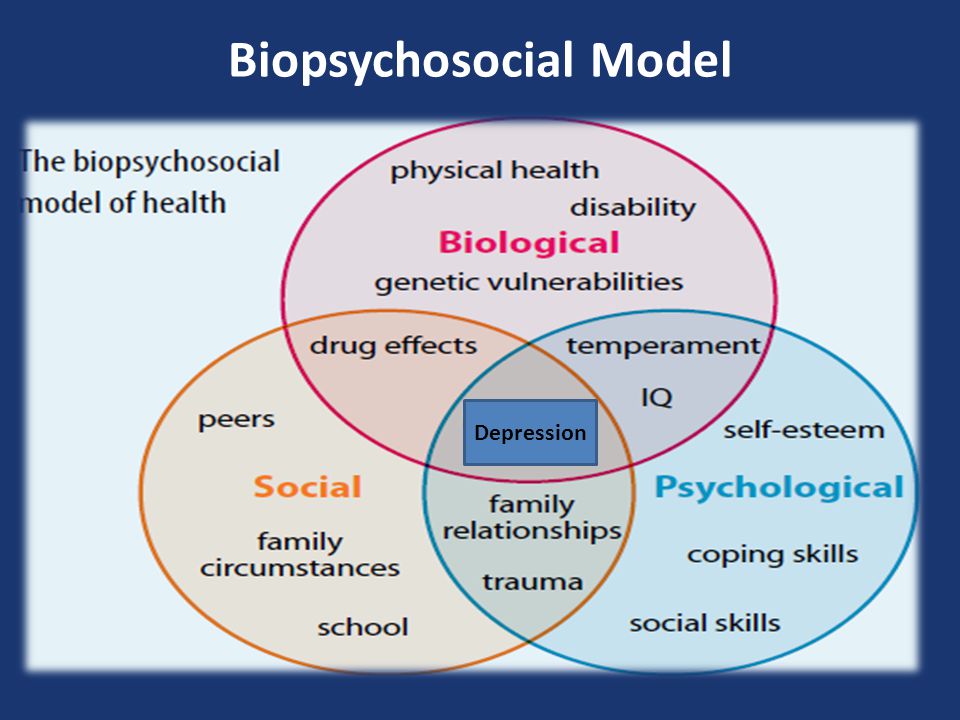 Childhood trauma can include:
Childhood trauma can include:
- sexual or physical abuse
- neglect
- traumatic events
- extreme living situations
It’s important to draw a distinction between bipolar disorder causes, such as genetics and brain chemistry, and triggers. They interact to produce mood episodes, but they aren’t entirely the same thing.
You could begin experiencing mood episodes after certain life events, like a rough breakup, job loss, or childbirth. Certain habits, like not getting enough sleep on a regular basis or drinking a lot of alcohol, can also trigger mood episodes or make them more severe.
None of this means you’re to blame, though. No one can conclusively say who will and won’t develop bipolar disorder. Its causes lie beyond your control.
Other possible environmental factors might include:
- underlying health conditions
- diet
- sudden, severe stress, such as a death or other loss
- persistent, smaller-scale stress, such as trouble at work or family problems
Between mood episodes, you might not notice any symptoms of bipolar disorder.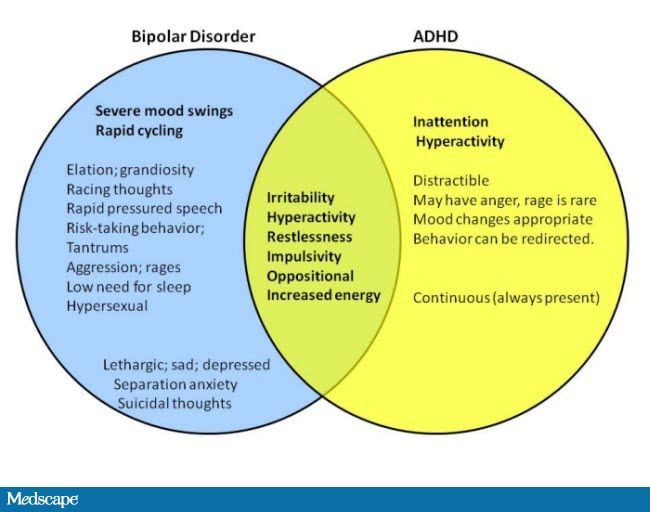 Still, it’s fairly common to have other conditions along with bipolar disorder.
Still, it’s fairly common to have other conditions along with bipolar disorder.
Conditions that often occur with bipolar disorder include:
- Anxiety. Research suggests at least half of all people with bipolar disorder will likely experience an anxiety disorder at some point in life.
- Post-traumatic stress disorder (PTSD). Bipolar disorder has been linked to childhood trauma, so it’s understandable that many people are dealing with PTSD too.
- Attention deficit hyperactivity disorder (ADHD). Bipolar disorder often occurs with ADHD, especially when mood symptoms begin before the age of 21.
- Substance use disorders. The DSM-5 notes more than half of all people who meet the criteria for a bipolar disorder diagnosis also have an alcohol use disorder or other substance use disorder.
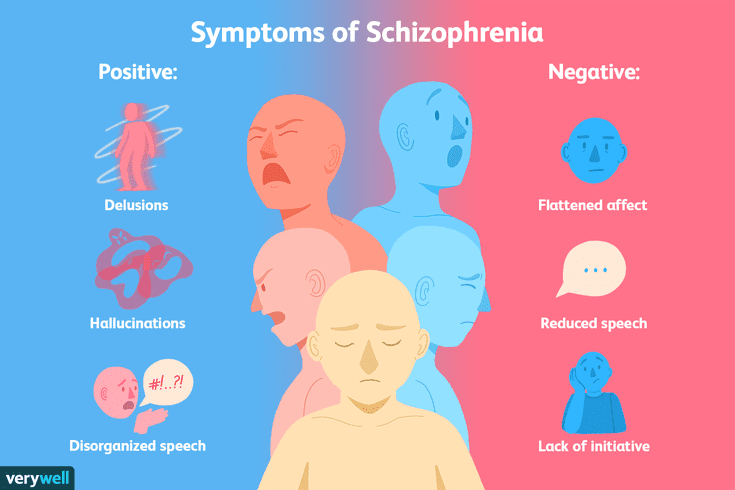
- Psychosis. Delusions, hallucinations, and other symptoms of psychosis are often symptoms of schizophrenia, but they can also happen with bipolar disorder.
- Eating disorders. Many people living with bipolar disorder also have an eating disorder. Bulimia nervosa and bipolar II disorder appear most strongly linked.
- Migraine. Research suggests people with bipolar disorder have a much higher risk for migraine.
Treating bipolar disorder with medication can be something of a delicate balance. Antidepressants that help ease depressive episodes can sometimes trigger manic episodes.
If your healthcare provider recommends medication, they might prescribe an antimanic medication such as lithium along with an antidepressant. These medications can help prevent a manic episode.
As you work to develop a treatment plan with your care provider, let them know about any medications you take. Some medications can make both depressive and manic episodes more severe.
Also tell your care provider about any substance use, including alcohol and caffeine, since they can sometimes lead to mood episodes.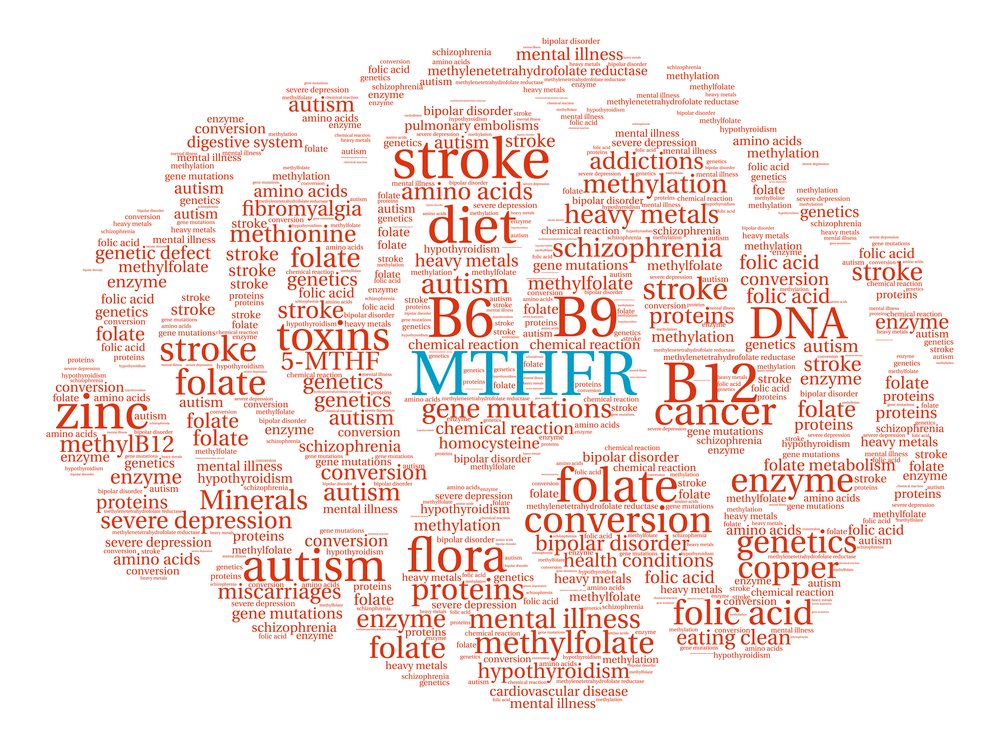
Some substances, including cocaine, ecstasy, and amphetamines, can produce a high that resembles a manic episode. Medications that might have a similar effect include:
- high doses of appetite suppressants and cold medications
- prednisone and other steroids
- thyroid medication
If you believe you’re experiencing a mood episode or other symptoms of bipolar disorder, it’s always a good idea to connect with your healthcare provider as soon as possible.
Its causes may be complex, but bipolar disorder is very treatable. While you don’t have control over whether you develop the condition, you can take steps to manage mood episodes and other symptoms.
To get started, consider talking with your care provider about a treatment plan that works well for you. Many people find medication helps stabilize mood changes, so a doctor or psychiatrist may recommend medication as a primary treatment.
Therapy and alternative treatments can also have benefit.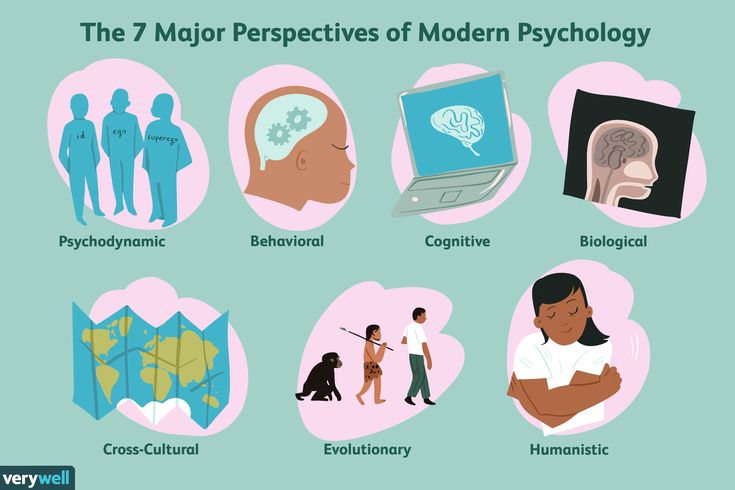 A therapist can help you address mood symptoms. And therapy in general also provides the opportunity to build healthy coping skills to manage stress and triggers on your terms.
A therapist can help you address mood symptoms. And therapy in general also provides the opportunity to build healthy coping skills to manage stress and triggers on your terms.
Looking for more treatment info? Get a deep dive on bipolar disorder treatment here.
Bipolar affective disorder, part 2. Clinical picture
© Tells Andrey Arkadyevich Shmilovich , Doctor of Medical Sciences, Doctor of the Highest Category, Head of the Department of Psychiatry and Medical Psychology of the Russian National Research Medical University. N.I. Pirogova, chief physician of the Re-Alt clinic:
– Today we will talk about the clinical picture of such a very common disease as bipolar affective disorder. This disease proceeds relatively favorably and generally has a positive prognosis if we manage to establish good compliance with the patient, that is, a good therapeutic interaction. If our patient is ready to follow the recommendations of the therapy and psychotherapy prescribed to him, visit his psychotherapist, psychologist, follow the regimen, give up some bad habits and much more.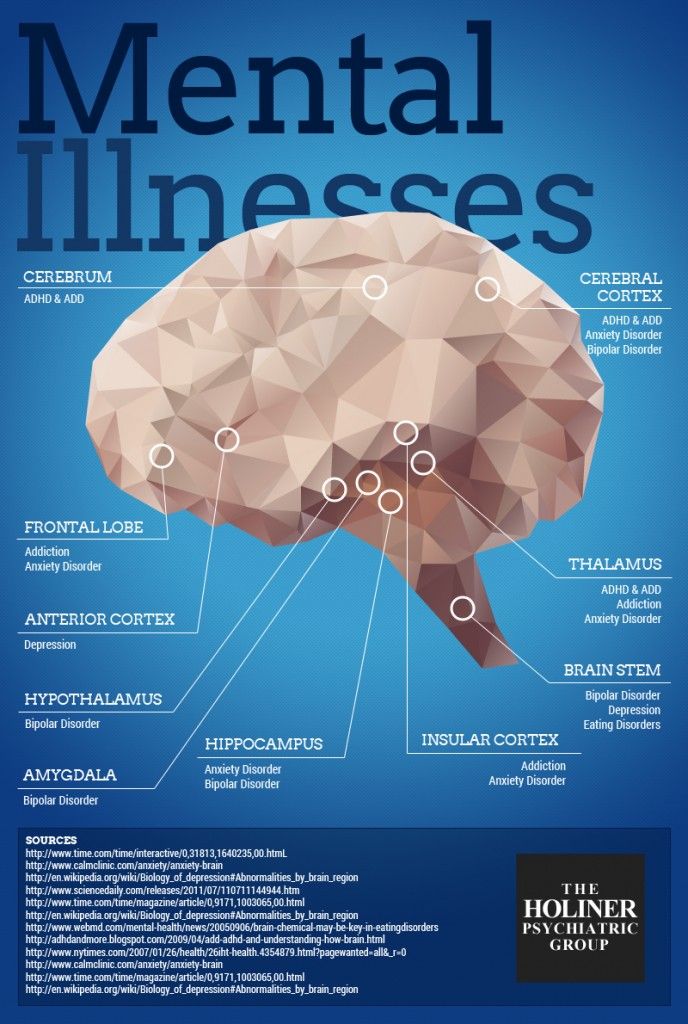 Then we can almost guarantee a relatively good forecast. nine0005
Then we can almost guarantee a relatively good forecast. nine0005
Let's talk about the clinical picture of this disease
It is conditionally possible to distinguish four main clinical states : this is a depressive syndrome, a manic syndrome, a state of so-called euthymia and a mixed affective state.
If we look at the clinical picture of this disease with a mathematical eye, we will see a sinusoid, which will, with a certain frequency, with different amplitudes, demonstrate a deviation from the normal, natural mood. In this sinusoid we can detect as manic and depressive phases - this is how the periods of exacerbation of the disease and the intervals between these phases are called, which add up to a relatively even affect, a relatively stable mood, which is commonly called euthymia.
Mixed affective state , which I already mentioned, occurs when one affective phase passes into another, and the patient for some time finds himself, as it were, simultaneously in two polar states, when there are still “tails” of a depressive disorder, but in the psyche the first symptoms of a manic state came.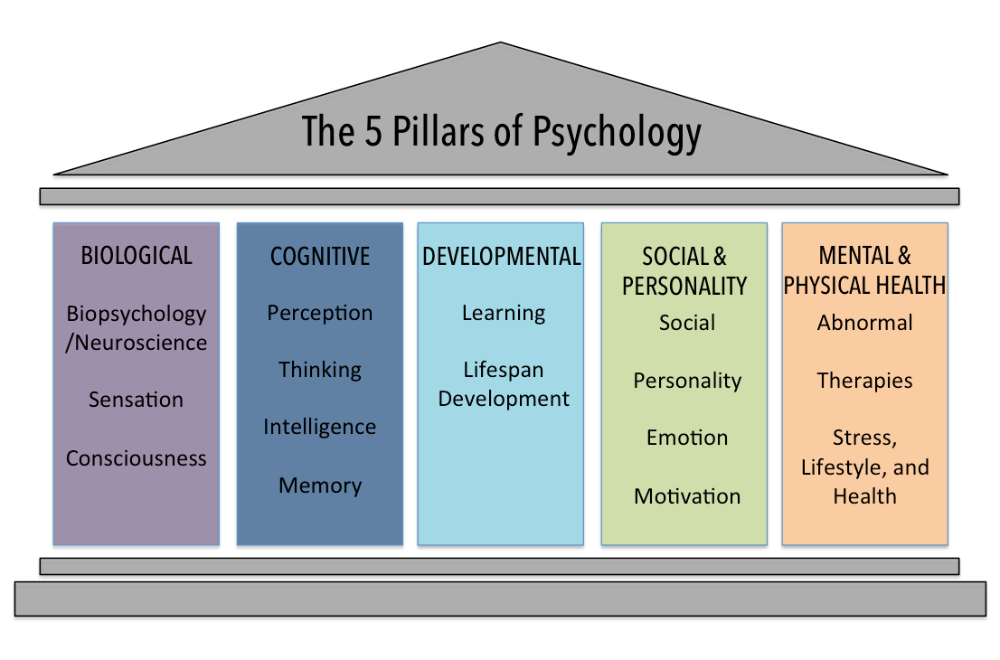 It is worth noting that this period is one of the most dangerous, in terms of suicidal risk or some anti-vital actions. But more on that later. nine0005
It is worth noting that this period is one of the most dangerous, in terms of suicidal risk or some anti-vital actions. But more on that later. nine0005
Biological nature of disease
First of all, let's talk about the fact that bipolar affective disorder has a biological nature. This disease is certainly genetically determined. We know many cases of inheritance of such a disease as bipolar affective disorder.
There is a lot of evidence that this disease is related to other biological factors: immunology, neurophysiology, endocrinology. We are also talking about psychological triggers, some kind of triggering environmental influences, psychosocial, toxic triggers - I mean the use of psychoactive substances, alcohol and much more. nine0033 We must treat this disease as a disease that comes without warning of its arrival. This disease does not knock on the door before entering.
What is a depressive disorder or bipolar depression?
This is the part of the disease that often leads patients to a state of despair, a catastrophe in which there is no other way out for the patient but to go to the next world.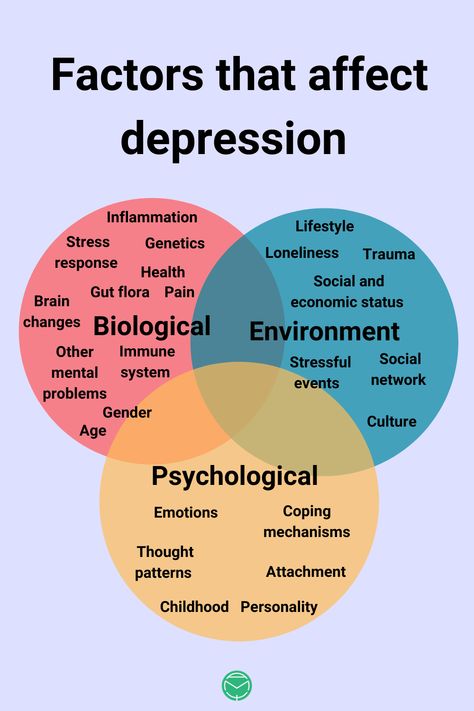 This is a very severe melancholy, this is a deep longing in the chest, this is a feeling of intense mental pain, which is literally localized in the body in the chest area. nine0033
This is a very severe melancholy, this is a deep longing in the chest, this is a feeling of intense mental pain, which is literally localized in the body in the chest area. nine0033
This is a state of utter despair, hopelessness, a state of catastrophic moment. This is a state in which the patient sees no way out, and any attempts on the part of the environment to cheer him up, set him up in an optimistic mood are perceived by him extremely negatively. In this state, the patient seeks to retire away from such advisers, he wants to hide in a corner, turn his back to the wall and remain in this state for an indefinitely long time.
There are very few thoughts in the head at this time, they move slowly, lazily, they are very monosyllabic, they do not have any perspective. As a rule, they are looped, as a symptom of a broken record or mental chewing gum - this is the so-called melancholic logic. In this state, the patient has absolutely no physical potency, he has no strength, he cannot get out of bed, he cannot perform the most elementary actions: tie his shoelaces, brush his teeth.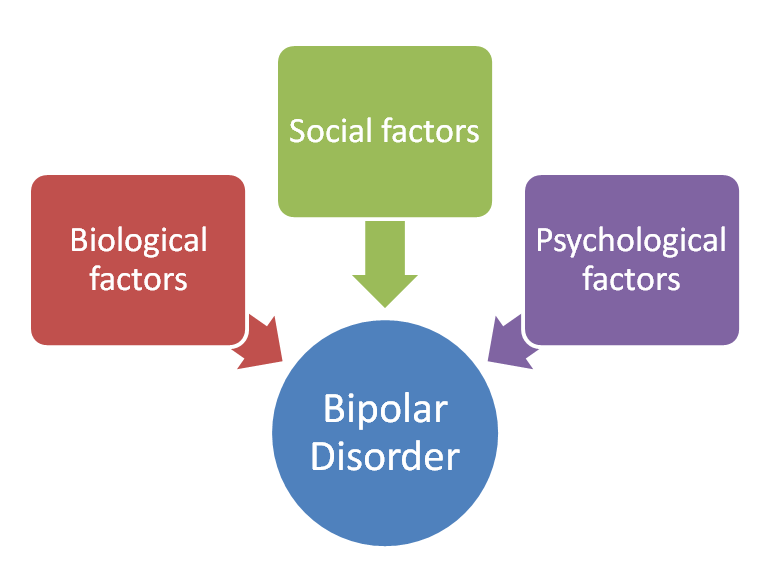 In this state, there are no desires, no aspirations, no need to enjoy, there is no food, no sex, no life desire. nine0005
In this state, there are no desires, no aspirations, no need to enjoy, there is no food, no sex, no life desire. nine0005
Suicidal thoughts
When we talk about lack of desire for life, we are talking about suicidal tendencies. Suicidal thoughts can be passive: “It would be nice if I got hit by a car, or if there was an earthquake right now and our house collapsed.” And they can be active when the patient builds clear plans, makes specific decisions, begins to prepare for the commission of one or another suicidal act.
nine0009 Depression in bipolar disorder
They can last quite a long time - from 1 to 3 - 6 months, but there are times when depression lasts either very little or very long. I have seen a case of depression in bipolar disorder lasting over a year. It’s hard to be in such a painful state, you won’t wish the enemy. When we see a patient in a state of bipolar depression, we understand that every such day is a colossal torment for him, so it is necessary to help him as soon as possible.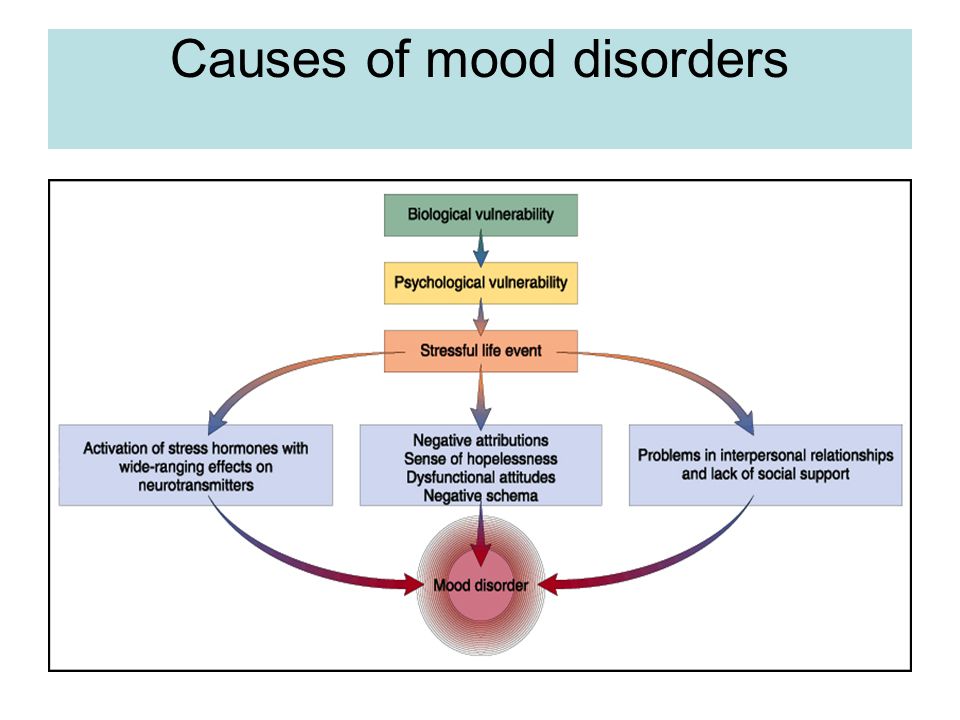 nine0005
nine0005
This state can change at any moment, it can happen absolutely autochthonously, that is, autonomously, without any external factors, or maybe after some kind of provocation. This phenomenon of changing from a depressed state to a manic state is called affect inversion.
We suddenly see a completely different person who suddenly, for no reason at all, goes into some incredible euphoric mood. He has a carelessness, he becomes very mobile, active and energetic. His brain produces a huge number of ideas, thoughts, all this is very superficial, his speech becomes machine-gun, accelerated, it is almost impossible to follow his thought, which is jumping. There is even such a phenomenon as “leaps of ideas”. nine0033
This patient is disinhibited, his sexual and food desire is disinhibited, he develops an alcoholic and narcotic excess. He becomes very risky, is not afraid of anything, commits a huge number of clearly erroneous actions, not paying attention to the fact that these actions can negatively affect his fate and those around him.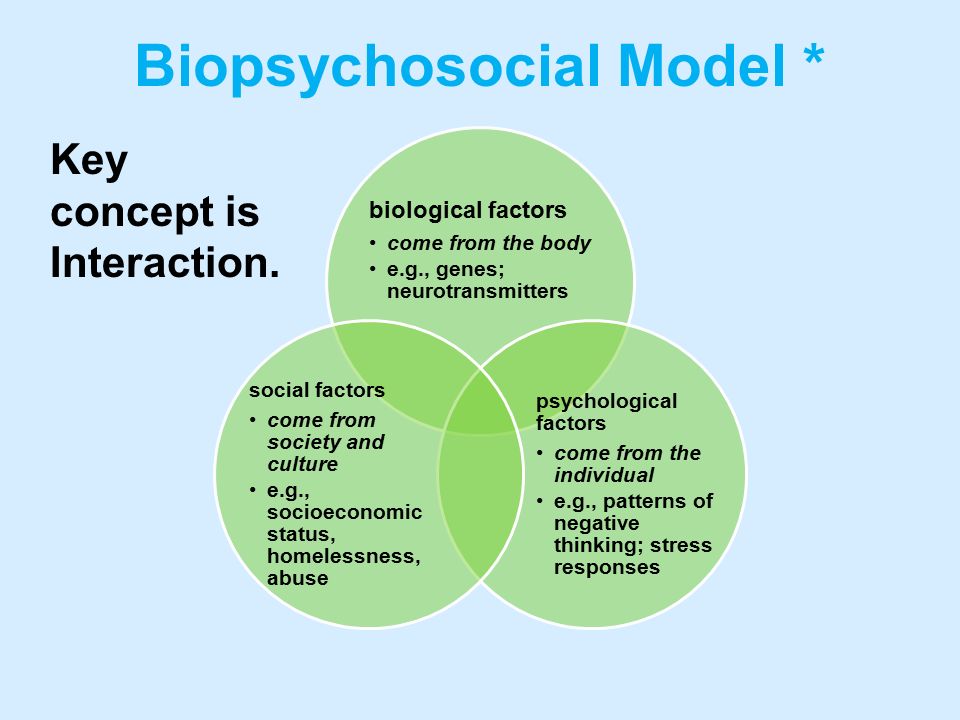 In this state, he can also stay for quite a long time - from several weeks to several months. Then this state can again change to depressive. nine0005
In this state, he can also stay for quite a long time - from several weeks to several months. Then this state can again change to depressive. nine0005
A euthymic state is a state of remission in which we do not observe either depressive or manic symptoms. In this state, the patient returns to his usual normal. Here you need to understand that the usual norm is that personality, that character with its own nuances, which was before the illness.
Character and personality do not change
In bipolar affective disorder, unlike many other disorders, character and personality do not change. It cannot be said that the norm is when there are no emotions at all, of course, there are emotions, and there are mood swings, and there should be, every person has them, and every person has a certain corridor in which these emotions change in amplitude, and the amplitude each person has his own. There are boundaries of this corridor, its size and width are different.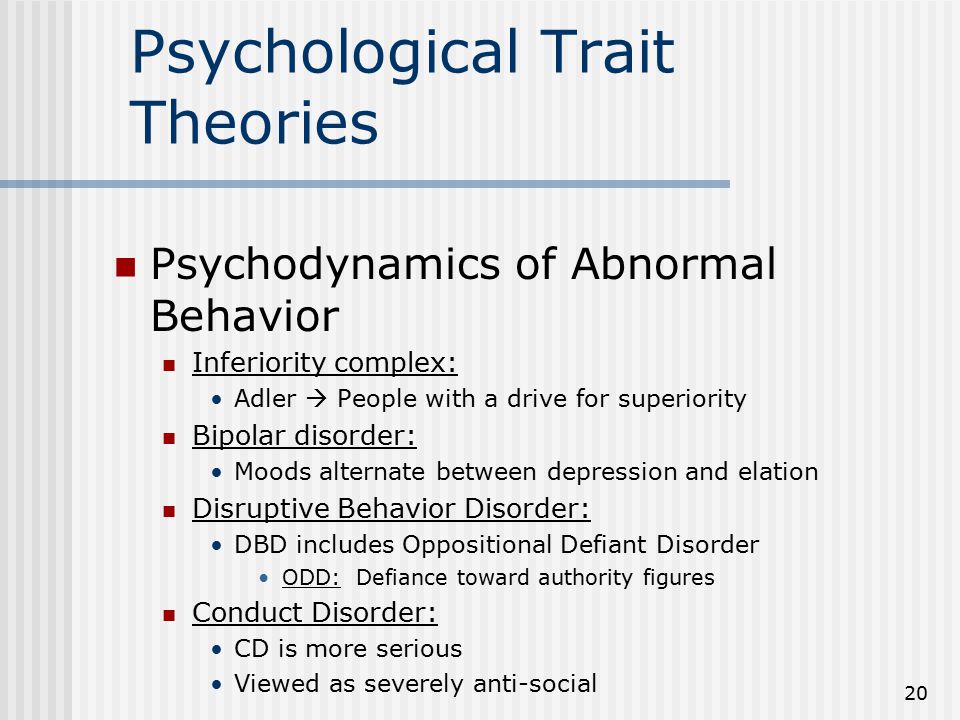 Euthymia is a return to the corridor of your emotions. When a patient in a euthymic state experiences, for example, some kind of grief associated with a real situation, with the loss of a loved one. Or a person in this euthymic state is happy that he managed to conclude a successful contract, or a child was born, or something else. These are normal, natural, human emotions. Even knowing that this person has bipolar disorder, even if he once experienced depressive and manic states, we treat this as normal, natural emotions. nine0005
Euthymia is a return to the corridor of your emotions. When a patient in a euthymic state experiences, for example, some kind of grief associated with a real situation, with the loss of a loved one. Or a person in this euthymic state is happy that he managed to conclude a successful contract, or a child was born, or something else. These are normal, natural, human emotions. Even knowing that this person has bipolar disorder, even if he once experienced depressive and manic states, we treat this as normal, natural emotions. nine0005
Mixed affective state
In the soul of such patients, a vinaigrette of feelings, mixed with each other, actually sets in. When, with cheerful intonations in his voice, a person begins to emotionally, energetically tell that his soul hurts, that he wants to go to the next world, that is, depressive complaints with a high mood. Or when complacency, ease of communication is suddenly combined with irritability, anger, rejection, pugnacity or suspicion at the same time.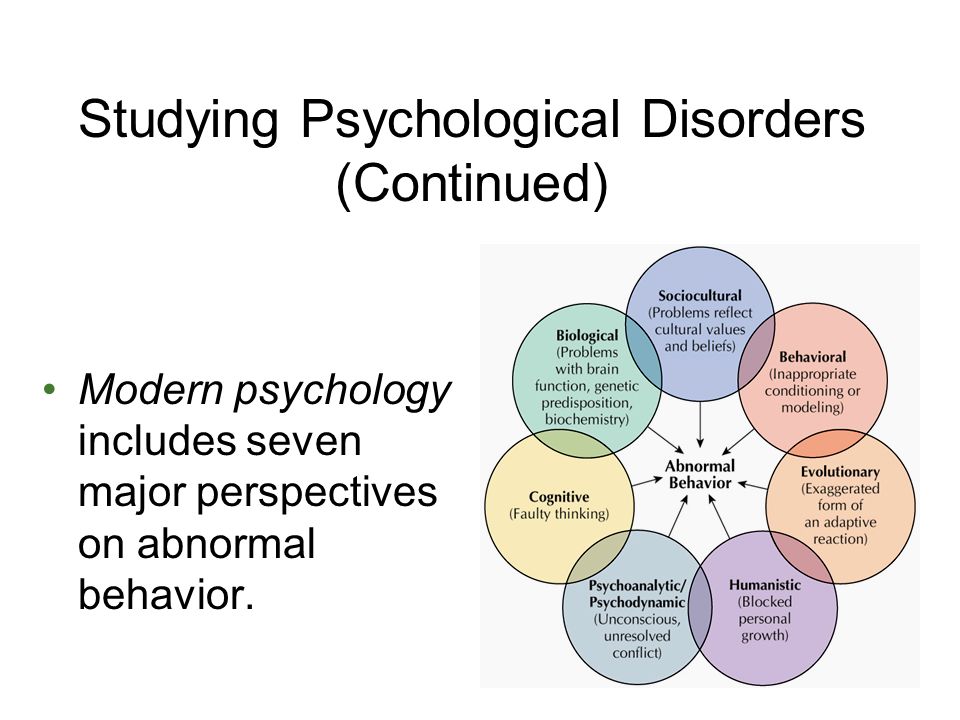 nine0005
nine0005
In such mixed affective states, it is very difficult to determine how to communicate with a person, because you do not keep up with these differences, changes, and it can be very difficult to establish some kind of productive dialogue with him. However, we are well aware that we are also talking about a painful condition that needs to be treated. Fortunately, we have such remedies, I will talk about them later, with which we can treat such mixed affective states.
Once again I want to remind you once again that it is in these mixed affective states that the probability of suicidal risk is especially high. We can also talk about varying degrees of severity of affective disorders. There are mild variants of bipolar affective disorder. One of them is called cyclothymia, when the amplitude of these fluctuations is higher than normal, but not so much as to seriously maladjust a person in his life. nine0005
There are conditions in which the amplitude of both depressive and manic syndromes is so high that at the peak of emotional disorders, other mental disorders appear, in particular, delusional states.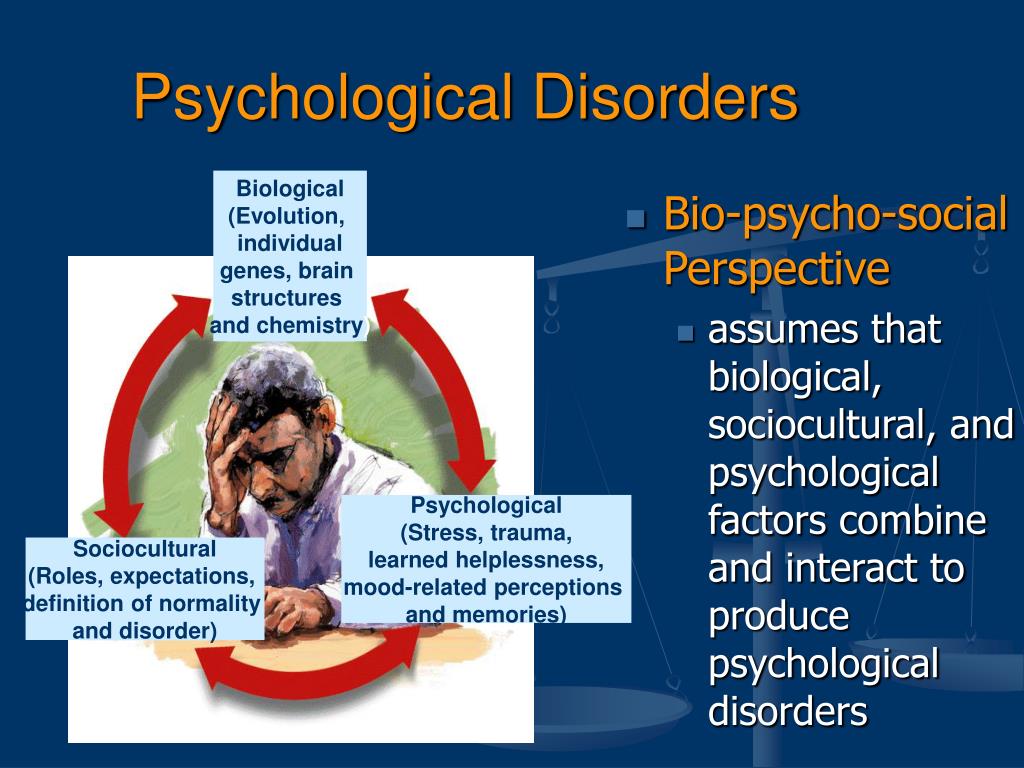 The manic patient becomes convinced of his exclusivity, his greatness, wealth, high origin. A depressed patient has thoughts of evil power, sinfulness, self-abasement.
The manic patient becomes convinced of his exclusivity, his greatness, wealth, high origin. A depressed patient has thoughts of evil power, sinfulness, self-abasement.
When we talk about such severe forms of bipolar affective disorder, we strive to do everything to place the patient in a psychiatric hospital under medical supervision as soon as possible, because otherwise this person, being in such a state, can do so many troubles, for which will then be very difficult to pay off. nine0005
Various clinical forms of bipolar affective disorder
This is a question that continues to be studied by psychiatrists, clinicians, scientists to this day, since there are many more varieties of bipolar disorder than indicated in manuals and books. In principle, there are much more varieties of mental disorders than the classifications that we know, since each person has his own nuance, his own specificity. There are no two identical patients, therefore, it is by no means possible to relate to the diagnosis of such conditions, and even more so to therapy, in a mechanistic way.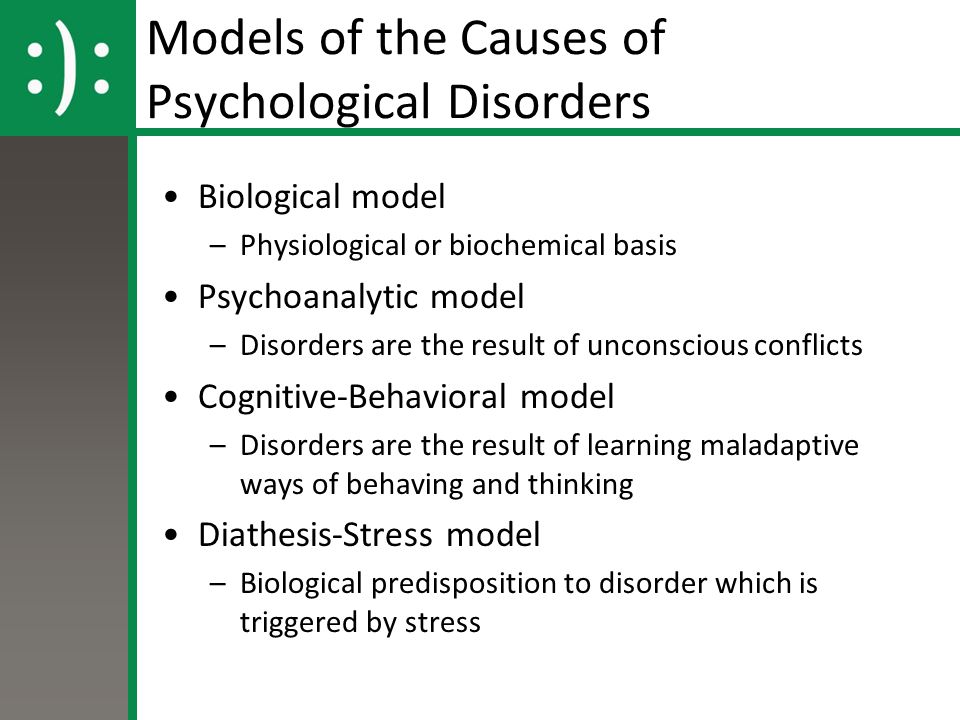 It is impossible to treat strictly according to instructions, according to standards, according to some protocols. Treatment should be based on face-to-face communication and contacts between the doctor and the patient. The doctor should use his specific tactics and strategy with each patient, from the most elementary, psychotherapeutic techniques to prescribing certain drugs. nine0005
It is impossible to treat strictly according to instructions, according to standards, according to some protocols. Treatment should be based on face-to-face communication and contacts between the doctor and the patient. The doctor should use his specific tactics and strategy with each patient, from the most elementary, psychotherapeutic techniques to prescribing certain drugs. nine0005
Self-medication is not allowed
If you or your relatives and friends, God forbid, develop a mental disorder, in particular, such as bipolar affective disorder, in no case should you rely on the Internet, books or advice from loved ones. Don't heal yourself. Believe me, this disease does not forgive mistakes. Seek help from doctors. We are ready to help you. We are nearby.
Bipolar personality disorder - treatment, causes and symptoms
Bipolar disorder is a complex psychological illness, accompanied by a sharp change in depressive, manic, mixed states or alternation of depression and euphoria.
People suffering from manic-depressive syndrome experience severe mood swings that differ significantly from the generally accepted social norm. The problem can be observed irregularly, between exacerbations, a person can lead an absolutely normal life, after which an exacerbation occurs again. nine0005
Content
Main causes of bipolar disorder
Ivan Vladimirovich Brednev
Psychiatrist - narcologist
Consultation
Experts agree that there is no single cause of manic-depressive disorder. Factors such as chemical imbalances in the brain, hormonal imbalances, genetic and biological factors, and external psychological influences can contribute to the development of the disease. nine0005
Given the high complexity of the course of bipolar disorder, treatment should be carried out only with the involvement of highly qualified specialists with successful practical experience and the necessary conditions for complex therapy.
The main symptoms of bipolar disorder
Given the complexity of the manic-depressive syndrome, the symptoms can vary significantly, and depend on the current psychological state of the patient, his mood and environmental factors. nine0005
Start treatment today
+38 (067) 426 04 04
+38 (067) 426 04 04
Feedback
Send
Some people may experience marked regular mood swings with symptoms of depression and mania. These periods can last from several days to several months, periodically the condition returns to normal. Some patients may experience euphoria or depression for several years without interruption, as well as a mixed state, accompanied by regular mood swings. nine0005
The main symptoms of bipolar disorder include:
- Pathologically high sociability, sometimes flowing into increased aggressiveness without obvious provoking reasons;
- Excessive senseless activity, absenteeism from school or work without a good reason, apathy for various activities;
Alexander Vyacheslavovich Marchenko
Psychiatrist
Consultation
- Euphoric exciting feelings, raising one's own "I" above other members of society, as well as excessive self-confidence, an inflated sense of self-esteem; nine0149
- Use of drugs, drugs and alcohol to combat insomnia;
- Provocative behavior and other symptoms associated with increased or decreased psychological activity of a person.