How to control ocd thoughts
International OCD Foundation | 25 Tips for Succeeding in Your OCD Treatment
by Fred Penzel, PhD
Psychologist/Executive Director; Western Suffolk Psychological Services
IOCDF Scientific & Clinical Advisory Board Member
This article was initially published in the Summer 2014 edition of the OCD Newsletter.
I originally wrote this list for my own patients, and then I realized it would be useful to others out there who are just starting or who are currently engaged in treatment. Here are my 25 tips for succeeding in your OCD treatment.
1. Always expect the unexpected. You can have an obsessive thought at any time or any place. Don’t be surprised when old or even new ones occur. Don‘t let it throw you. Be prepared to use your therapy tools at any time, and in any place. Also, if new thoughts appear, be sure to tell your therapist so you can keep them informed.
2. Be willing to accept risk. Risk is an integral part of life, and as such it cannot be completely gotten rid of. Remember that not recovering is the biggest risk of all.
3. Never seek reassurance from yourself or others. Instead, tell yourself the worst will happen, is happening, or has already happened. Reassurance will cancel out the effects of any therapy homework you use it on and prevent you from improving. Reassurance-seeking is a compulsion, no matter how you may try to justify it.
4. Always try hard to agree with all obsessive thoughts — never analyze, question, or argue with them. The questions they raise are not real questions, and there are no real answers to them. Try not to get too detailed when agreeing — simply say the thoughts are true and real.
5. Don’t waste time trying to prevent or not think your thoughts. This will only have the opposite effect and lead to thinking more thoughts.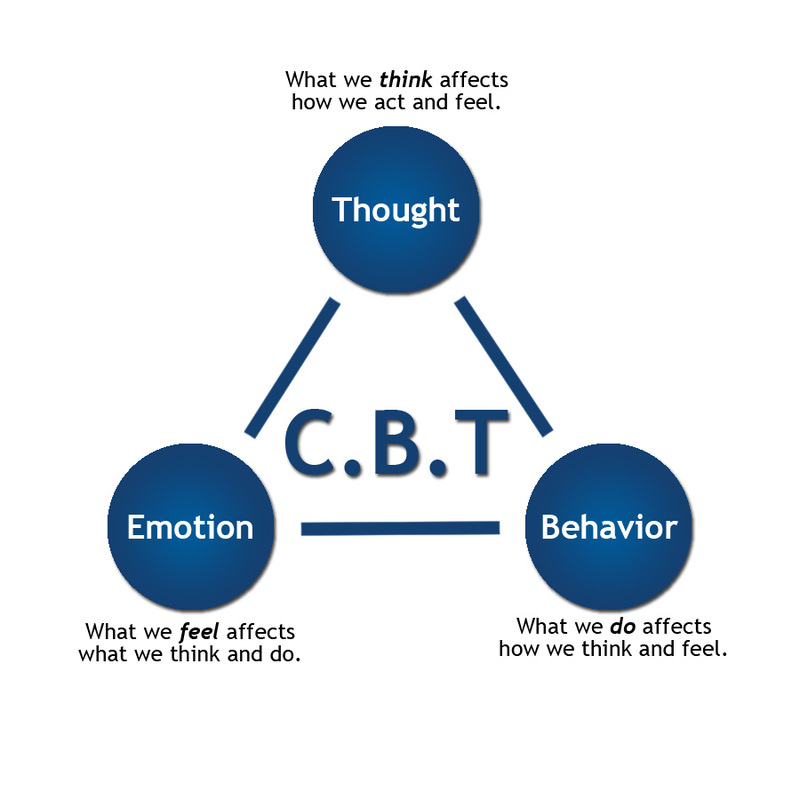 Studies have shown that you cannot effectively stop or push down particular thoughts. Your motto should be, “If you want to think about them less, think about them more.”
Studies have shown that you cannot effectively stop or push down particular thoughts. Your motto should be, “If you want to think about them less, think about them more.”
6. Try to not be a black-and-white, all-or-nothing thinker — don’t tell yourself that one slip up means you are now a total failure. If you slip and do a compulsion, you can always turn it around and do something to cancel it. The good news is that you are in this for the long haul, and you always get another chance. It is normal to make mistakes when learning new skills, especially in therapy. It happens to everyone now and then. Accept it. Even if you have a big setback, don’t let it throw you. Remember the saying, “A lapse is not a relapse.” This means that you never really go back to square one. To do that, you would have to forget everything you have learned up to that point, and that really isn’t possible. Also remember the sayings, “Never confuse a single defeat with a final defeat,” (F. Scott Fitzgerald) and as they say in AA, “You can always start your day over.”
Scott Fitzgerald) and as they say in AA, “You can always start your day over.”
7. Remember that dealing with your symptoms is your responsibility alone. Don’t involve others in your therapy homework (unless your therapist tells you to) or expect them to push you or motivate you. They won’t always be there when you need them, but YOU are always there for YOU.
8. Don’t get too impatient with your progress, or compare yourself to someone else. Everyone goes at their own pace. Instead, try to simply focus on carrying out each day’s therapy homework, one day at a time.
9. When you have a choice, always go toward the anxiety, never away from it. The only way to overcome a fear is to face it. You can’t run away from your own thoughts, so you really have no choice but to face them. If you want to recover, you will have to do this.
10. When faced with two possible choices of what to confront, choose the more difficult of the two whenever possible.
11. Review your therapy homework assignments daily, even if you think you know all of them. It is easy to overlook them — especially the ones you don’t look forward to doing.
12. If your therapist gives you an assignment you don’t feel ready to do, you can speak up and tell them so. As half of the therapist–patient team, you should be able to have a say in your own therapy. The goal is for the homework to produce some anxiety for you to get used to tolerating — not to overwhelm you with it and cause you a setback. On the other hand, don’t be afraid to stretch yourself a bit whenever you can.
13. Don’t wait for the “perfect moment” to start your therapy homework assignments. Procrastination is a feature of many people’s OCD, so start your therapy homework assignments the day you get them. The perfect moment is whenever you begin doing them.
14. Don’t be side-tracked by perfectionism. Perfectionism can be another feature of OCD.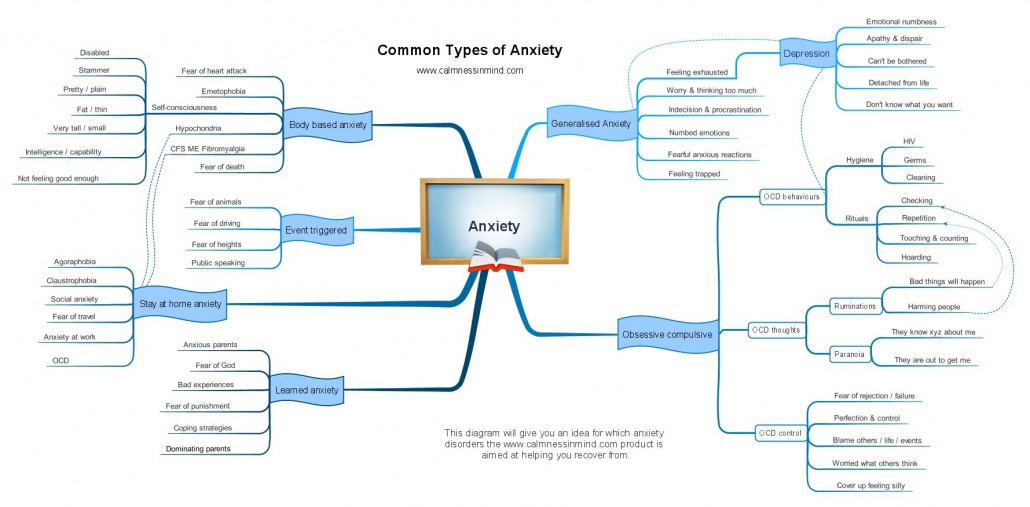 You may find your OCD telling you that if you don’t do your homework perfectly, you won’t recover. If you do find yourself obsessing about having to do your homework perfectly, you risk turning it into another compulsion. Watch out for having to do your homework according to the same rigid rules each time you do it. Also, don’t do your homework so excessively that it takes up your whole day. Remember that you still have a life to live.
You may find your OCD telling you that if you don’t do your homework perfectly, you won’t recover. If you do find yourself obsessing about having to do your homework perfectly, you risk turning it into another compulsion. Watch out for having to do your homework according to the same rigid rules each time you do it. Also, don’t do your homework so excessively that it takes up your whole day. Remember that you still have a life to live.
15. Try to read over your homework assignments at the start of each day. Don’t assume that you know them all and will not forget them.
16. When carrying out assignments, be careful to not provide yourself reassurance and undo your hard work. Telling yourself things like,“It’s only homework, and the things I’m saying and doing don’t count and aren’t real,” or “My therapist wouldn’t ask me to do something that would cause harm to me or others,” or “I’m only doing this because I was told to, so I’m not responsible for anything bad that happens,” can undermine all the work your doing.
17. Give your homework your full attention, focus on what you are doing, and let yourself feel the anxiety. Try to not let yourself tune out when doing certain assignments, so that you don’t have to feel the anxiety. People sometimes let the homework become routine and do it in a very automatic way as a kind of avoidance. Also, don’t do homework while carrying out other distracting activities. You are building tolerance to what you fear, and for that to happen you have to be in the moment with it.
18. When faced with a challenging assignment or an unexpected challenging situation, try to look at it as a positive. View it as another opportunity to get better instead of saying, “Oh, no. Why do I have to do this?” Instead tell yourself, “This will be good for me — another chance to practice and get stronger.”
19. Try to not rush through your therapy homework so that you don’t have to feel as much anxiety. Take your time, and see if you can view it in terms of all the good it will do you. Getting it over with as quickly as possible is not the goal — raising a moderate level of anxiety and staying with it is the goal.
Getting it over with as quickly as possible is not the goal — raising a moderate level of anxiety and staying with it is the goal.
20. If your homework doesn’t really give you any anxiety, tell your therapist about it. If your exposure homework doesn’t cause at least some anxiety, it isn’t going to help you that much. On the other hand, try doing all new assignments for at least a week before deciding that they don’t make you anxious. Some assignments can cause reactions later on, and it may take doing them a few times before the anxiety occurs.
21. It is sometimes possible for OCD to try to make you doubtful about your homework. It may tell you that you are not in the right treatment, that your assignments cannot possibly make you better, or that you really don’t understand what you are doing and won’t be able to make it work. Remember that OCD was known as the Doubting Disease, and it will try to cast doubt on anything that is important to you. To fight this, you may have to agree with it by saying, “Yes, that’s right. I really won’t get better.”
To fight this, you may have to agree with it by saying, “Yes, that’s right. I really won’t get better.”
22. Never forget that you have OCD. This means that you will not always be able to trust your own reactions or the things you think and feel, especially if they seem to be telling you very negative and extreme things. If you are unsure if something is really a symptom, treat it as a symptom. Better to do a bit more exposure than not enough.
23. Remember that in OCD, the problem is not the anxiety — the problem is the compulsions.
If you think the anxiety is the problem, you will only do more compulsions to get rid of it (which will only create more anxiety). If you recognize that the compulsions are the problem, stop doing them, and stay with the fearful situation, then the anxiety will eventually go away as you build up tolerance.
24. Always take a moment to be proud of your own efforts and recognize your successes. It’s a good way to help keep up your motivation.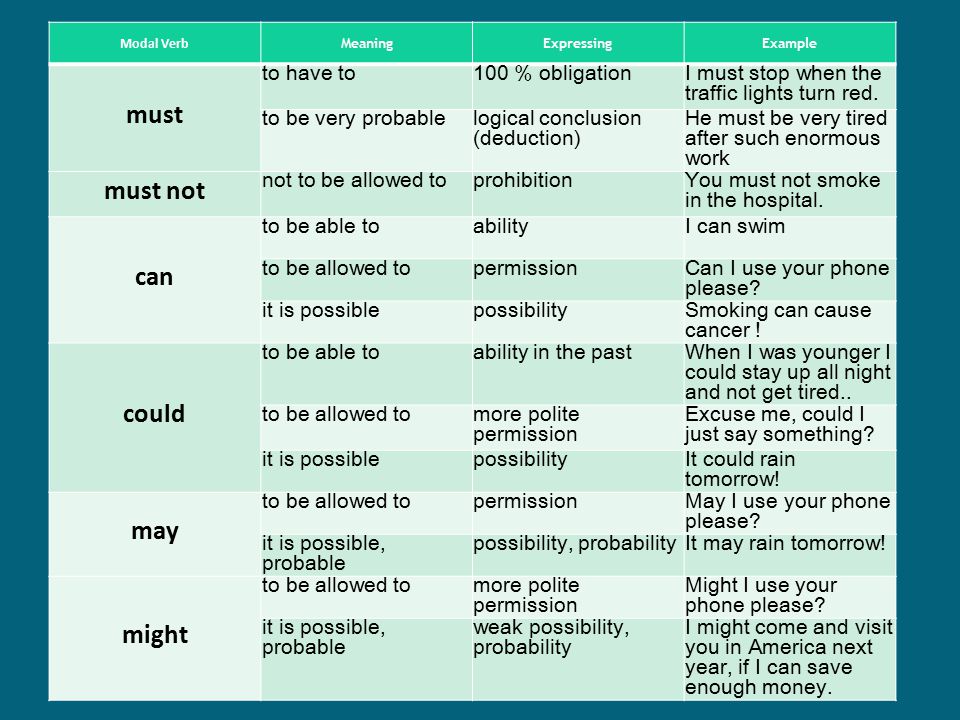 Look back at earlier assignments that are no longer challenging if you believe you aren’t making progress.
Look back at earlier assignments that are no longer challenging if you believe you aren’t making progress.
25. Overall, never forget that OCD is very paradoxical and rarely makes much sense. The things that you thought would make you better only make you worse, and the things you thought would make you worse are the very things that will make you better.
Obsessive-Compulsive Disorder (OCD) - HelpGuide.org
anxiety
Are obsessive thoughts and compulsive behaviors interfering with your daily life? Explore the symptoms, treatment, and self-help for OCD.
What is obsessive-compulsive disorder (OCD)?
It’s normal, on occasion, to go back and double-check that the iron is unplugged or worry that you might be contaminated by germs, or even have an occasional unpleasant, violent thought. But if you suffer from obsessive-compulsive disorder (OCD), obsessive thoughts and compulsive behaviors become so consuming they interfere with your daily life.
OCD is characterized by uncontrollable, unwanted thoughts and ritualized, repetitive behaviors you feel compelled to perform. If you have OCD, you probably recognize that your obsessive thoughts and compulsive behaviors are irrational—but even so, you feel unable to resist them and break free.
Like a needle getting stuck on an old record, OCD causes the brain to get stuck on a particular thought or urge. For example, you may check the stove 20 times to make sure it’s really turned off because you’re terrified of burning down your house, or wash your hands until they’re scrubbed raw for fear of germs. While you don’t derive any sense of pleasure from performing these repetitive behaviors, they may offer some passing relief for the anxiety generated by the obsessive thoughts.
You may try to avoid situations that trigger or worsen your symptoms or self-medicate with alcohol or drugs. But while it can seem like there’s no escaping your obsessions and compulsions, there are plenty of things you can do to break free of unwanted thoughts and irrational urges and regain control of your thoughts and actions.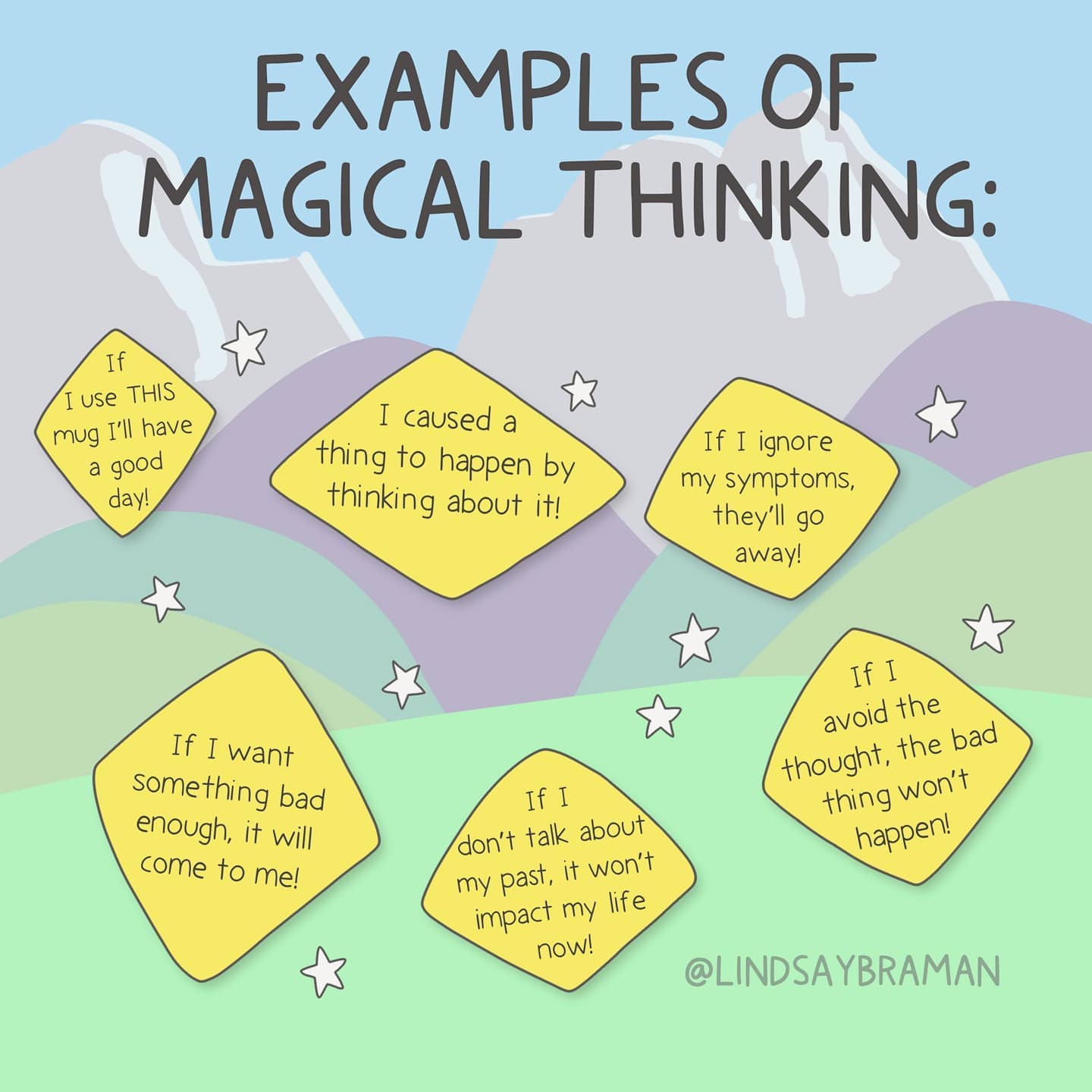
Is OCD an anxiety disorder?
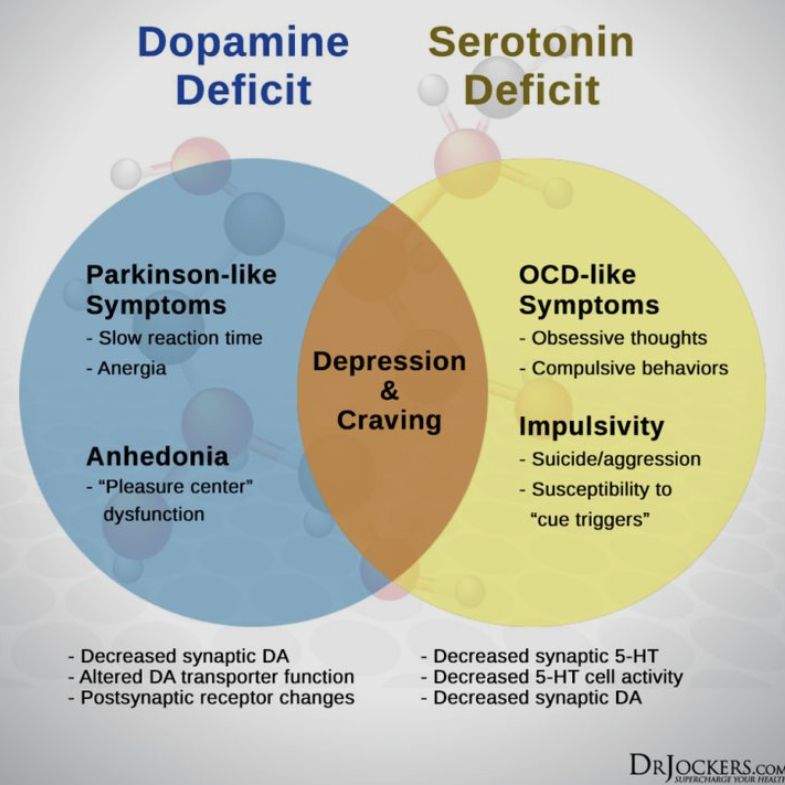
Historically, OCD was categorized as an anxiety disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM). However, in the fifth edition, the DSM separated OCD from the “Anxiety Disorders” section and created a new section called “Obsessive-Compulsive and Related Conditions.”
The change was made after researchers noted important differences between OCD and anxiety disorders. For example, with OCD you respond to unwanted thoughts with repetitive, unhelpful rituals. You may or may not realize that your thoughts and compulsions, such as excessive hand washing, are irrational. With anxiety, though, you're more likely to ruminate over real-world concerns, such as a fear of being mocked or judged. You may respond by avoiding the source of your fear, but won’t use odd rituals to ease your distress.
Certain interventions for OCD and anxiety disorders can also differ. To deal with an anxiety disorder, you might need to practice gradually facing your fears, whereas with OCD, it’s also important to address the compulsive behavior.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
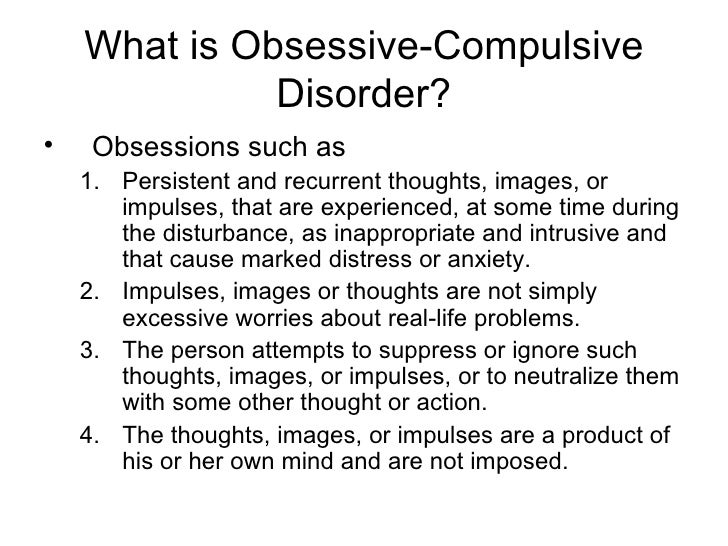
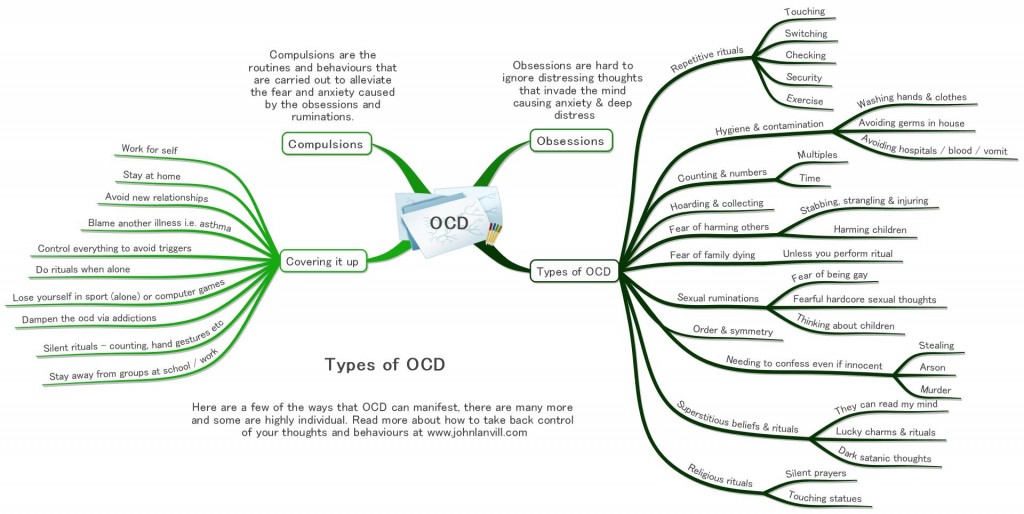
OCD obsessions and compulsions
Obsessions are involuntary thoughts, images, or impulses that occur over and over again in your mind. You don't want to have these ideas, but you can't stop them. Unfortunately, these obsessive thoughts are often disturbing and distracting.
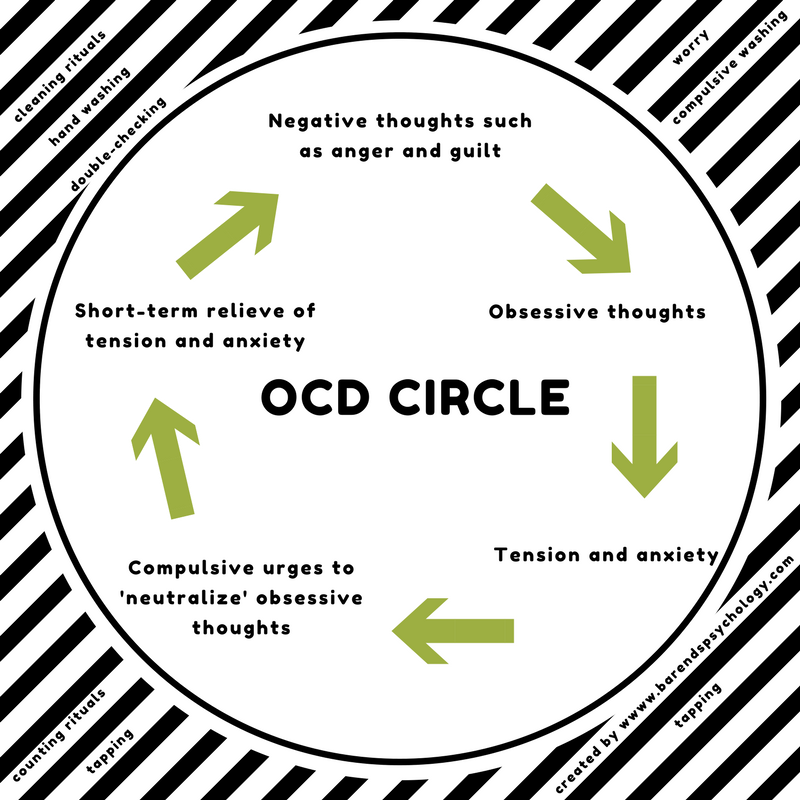
Compulsions are behaviors or rituals that you feel driven to act out again and again. Usually, compulsions are performed in an attempt to make obsessions go away. For example, if you're afraid of contamination, you might develop elaborate cleaning rituals. However, the relief never lasts. In fact, the obsessive thoughts usually come back stronger. And the compulsive rituals and behaviors often end up causing anxiety themselves as they become more demanding and time-consuming. This is the vicious cycle of OCD.
However, the relief never lasts. In fact, the obsessive thoughts usually come back stronger. And the compulsive rituals and behaviors often end up causing anxiety themselves as they become more demanding and time-consuming. This is the vicious cycle of OCD.
Most people with OCD fall into one of the following categories:
- Washers are afraid of contamination. They usually have cleaning or hand-washing compulsions.
- Checkers repeatedly check things (oven turned off, door locked, etc.) that they associate with harm or danger.
- Doubters and sinners are afraid that if everything isn't perfect or done just right something terrible will happen, or they will be punished.
- Counters and arrangers are obsessed with order and symmetry. They may have superstitions about certain numbers, colors, or arrangements.
OCD and hoarding
Hoarding used to be considered a category of OCD. While estimates suggest that up to 25 percent of people with OCD experience compulsive hoarding, it can also be a sign of a separate condition, hoarding disorder.
While estimates suggest that up to 25 percent of people with OCD experience compulsive hoarding, it can also be a sign of a separate condition, hoarding disorder.
Hoarders fear that something bad will happen if they throw anything away and hoard things that they don’t need or use. However, there are distinctions between OCD-related hoarding and hoarding disorder.
OCD-related hoarders tend not to accumulate so many possessions that their homes become unmanageable. Hoarding for them is usually unwelcome and distressing—a way to manage intrusive thoughts.
Someone with hoarding disorder, on the other hand, experiences both positive and negative emotions. Acquiring possessions provides pleasure rather than simply satisfying a compulsion and they being surrounded by their things provides comfort. The distress in hoarding disorder stems more from the consequences of hoarding—the clutter and unsafe environment—along with the anxiety of having to discard possessions.
Read: Hoarding Disorder: Help for Hoarders.
Just because you have obsessive thoughts or perform compulsive behaviors does NOT mean that you have obsessive-compulsive disorder. With OCD, these thoughts and behaviors cause tremendous distress, take up a lot of time (at least one hour per day), and interfere with your daily life and relationships.
Most people with obsessive-compulsive disorder have both obsessions and compulsions, but some people experience just one or the other.
Common obsessive thoughts in OCD include:
- Fear of being contaminated by germs or dirt or contaminating others.
- Fear of losing control and harming yourself or others.
- Intrusive sexually explicit or violent thoughts and images.
- Excessive focus on religious or moral ideas.
- Fear of losing or not having things you might need.
- Order and symmetry: the idea that everything must line up “just right”.
- Superstitions; excessive attention to something considered lucky or unlucky.
Common compulsive behaviors in OCD include:
- Excessive double-checking of things, such as locks, appliances, and switches.
- Repeatedly checking in on loved ones to make sure they're safe.
- Counting, tapping, repeating certain words, or doing other senseless things to reduce anxiety.
- Spending a lot of time washing or cleaning.
- Ordering or arranging things “just so”.
- Praying excessively or engaging in rituals triggered by religious fear.
- Accumulating “junk” such as old newspapers or empty food containers.
OCD symptoms in children
While the onset of obsessive-compulsive disorder usually occurs during adolescence or young adulthood, younger children sometimes have symptoms that look like OCD. However, the symptoms of other disorders, such as ADHD, autism, and Tourette's syndrome, can also look like obsessive-compulsive disorder, so a thorough medical and psychological exam is essential before any diagnosis is made.
The sudden development of intense OCD symptoms can also be a sign of pediatric acute-onset neuropsychiatric syndrome (PANS) or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS).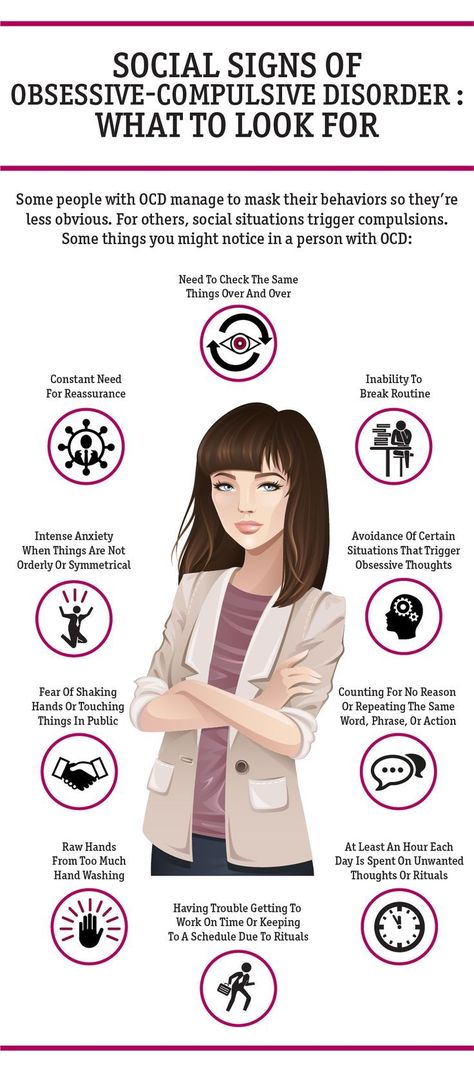
Read: PANS and PANDAS: Acute-Onset OCD in Children.
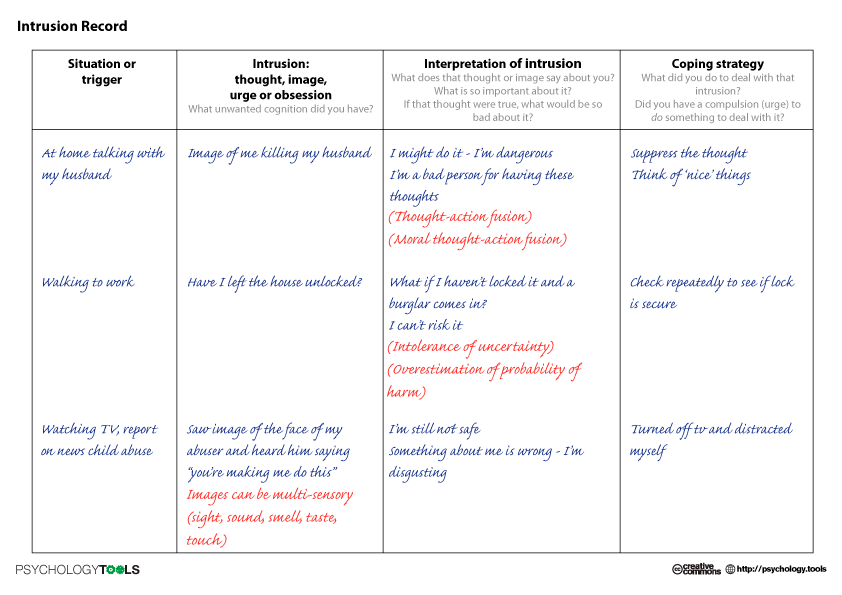
OCD self-help tip 1: Identify your triggers
The first step to managing your OCD symptoms is to recognize the triggers—the thoughts or situations—that bring on your obsessions and compulsions. Record a list of the triggers you experience each day and the obsessions they provoke. Rate the intensity of the fear or anxiety you experienced in each situation and then the compulsions or mental strategies you used to ease your anxiety. For example, if you have a fear of being contaminated by germs, touching a railing at the mall might generate a fear intensity of 3, whereas touching the restroom floor in the mall might generate a 10 and require 15 minutes of hand washing to ease your anxiety.
Keeping track of your triggers can help you anticipate your urges. And by anticipating your compulsive urges before they arise, you can help to ease them. For example, if your compulsive behavior involves checking that doors are locked, windows closed, or appliances turned off, try to lock the door or turn off the appliance with extra attention the first time.
- Create a solid mental picture and then make a mental note. Tell yourself, “The window is now closed,” or “I can see that the oven is turned off.”
- When the urge to check arises later, you will find it easier to re-label it as “just an obsessive thought.”
Identifying and recording your triggers also provides an important tool for learning to resist your OCD compulsions.
Tip 2: Learn to resist OCD compulsions
It might seem smart to avoid the situations that trigger your obsessive thoughts, but the more you avoid them, the scarier they feel. Conversely, by repeatedly exposing yourself to your OCD triggers, you can learn to resist the urge to complete your compulsive rituals. This is known as exposure and response prevention (ERP) and is a mainstay of professional therapy for OCD.
ERP requires you to repeatedly expose yourself to the source of your obsession—and then refrain from the compulsive behavior you’d usually perform to reduce your anxiety.:max_bytes(150000):strip_icc()/what-are-the-different-types-of-ocd-2510663_color3-5b3f8fda46e0fb00370d01bf.png) If you are a compulsive hand washer, for example, that could mean touching the door handle in a public restroom and then not allowing yourself to wash your hands. As you sit with the anxiety, the urge to wash your hands will gradually begin to go away on its own. In this way, you’ll learn that you don’t need the ritual to get rid of your anxiety and that you have some control over your obsessive thoughts and compulsive behaviors.
If you are a compulsive hand washer, for example, that could mean touching the door handle in a public restroom and then not allowing yourself to wash your hands. As you sit with the anxiety, the urge to wash your hands will gradually begin to go away on its own. In this way, you’ll learn that you don’t need the ritual to get rid of your anxiety and that you have some control over your obsessive thoughts and compulsive behaviors.
Tackling your biggest fears straight off might be too extreme, so ERP exercises start with you confronting lesser fears and then working your way up the “fear ladder.” Confront those situations that generate a low fear intensity and once you’re able to tolerate the anxiety you can move on to the next, more difficult exposure challenge.
Building your fear ladder
Think about your end goal (to be able to use a public restroom without fear of contamination, for example, or to drive to work without stopping to check if you’ve hit something) and then break down the steps needed to reach that goal.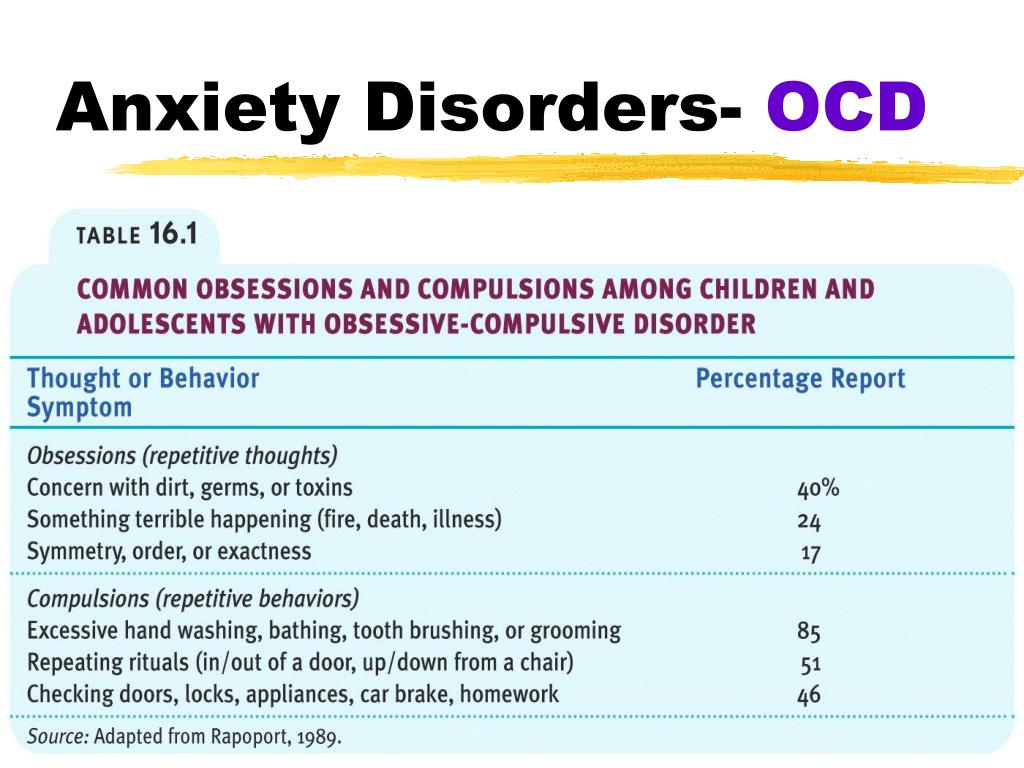 Using the information you recorded in identifying your triggers, make a list of situations from the least scary to the most scary. The first step should make you slightly anxious, but not so frightened that you’re too intimidated to try it.
Using the information you recorded in identifying your triggers, make a list of situations from the least scary to the most scary. The first step should make you slightly anxious, but not so frightened that you’re too intimidated to try it.
Here's a sample fear ladder:
| Goal: To drive to work without stopping to check if you’ve hit something | |
| Fear intensity | Situation |
| 10 | Drive all the way to work without stopping to check if you've hit something |
| 8 | Don’t phone your spouse to check they got to work safely |
| 6 | Leave the house, lock the front door and walk away without checking |
| 4 | Turn off the stove and leave the room without checking |
| 2 | Put milk in the refrigerator without checking the top is secure |
Using your fear ladder
Work your way up the ladder.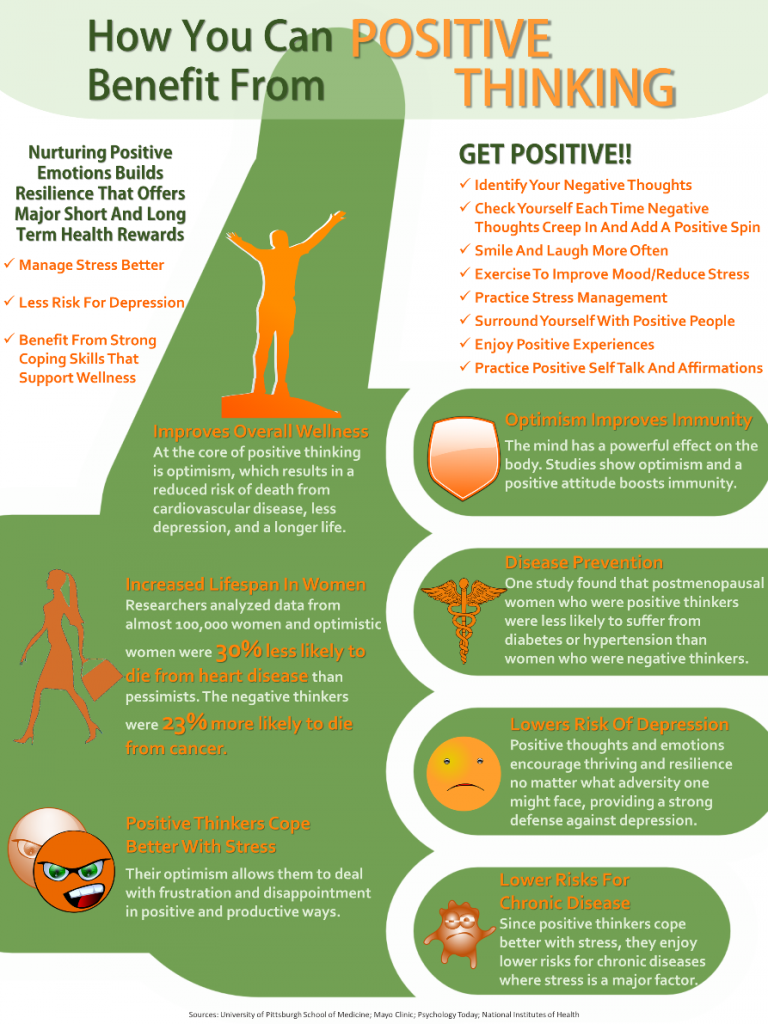 Start with the first step and don’t move on until you start to feel more comfortable doing it. If possible, stay in the situation long enough for your anxiety to decrease. The longer you expose yourself to your OCD trigger, the more you’ll get used to it and the less anxious you’ll feel when you face it the next time. Once you’ve done a step on several separate occasions without feeling too much anxiety, you can move on to the next step. If a step is too hard, break it down into smaller steps or go slower.
Start with the first step and don’t move on until you start to feel more comfortable doing it. If possible, stay in the situation long enough for your anxiety to decrease. The longer you expose yourself to your OCD trigger, the more you’ll get used to it and the less anxious you’ll feel when you face it the next time. Once you’ve done a step on several separate occasions without feeling too much anxiety, you can move on to the next step. If a step is too hard, break it down into smaller steps or go slower.
As you’re resisting your compulsions, focus on the feelings of anxiety. Instead of trying to distract yourself, allow yourself to feel anxious as you resist the urge to engage in your compulsive behavior. You may believe that the discomfort you’re feeling will continue until you engage in the compulsion. But if you stick with it, the anxiety will fade. And you’ll realize that you’re not going to “lose control” or have some kind of breakdown if you don’t perform the ritual.
Practice. The more often you practice, the quicker your progress will be. But don’t rush. Go at a pace that you can manage without feeling overwhelmed. And remember: you will feel uncomfortable and anxious as you face your fears, but the feelings are only temporary. Each time you expose yourself to your trigger, your anxiety should lessen and you’ll start to realize that you have more control (and less to fear) than you thought.
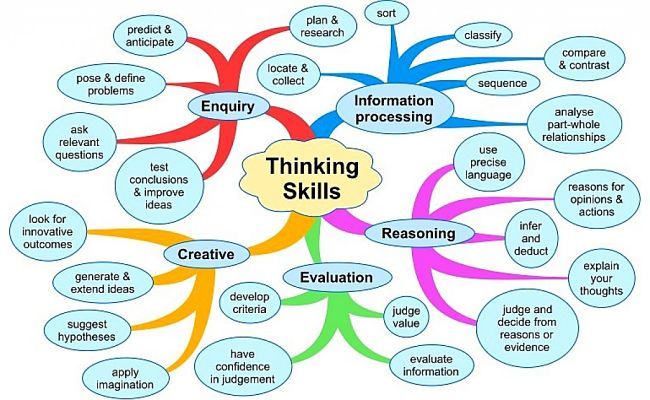
Tip 3: Challenge obsessive thoughts
Everyone has troubling thoughts or worries from time to time. But obsessive-compulsive disorder causes the brain to get stuck on a particular anxiety-provoking thought, causing it to play over and over in your head. The more unpleasant or distressing the thought, the more likely you are to try to repress it. But repressing thoughts is almost impossible and trying usually has the opposite effect, causing the unpleasant thought to resurface more frequently and become more bothersome.
As with resisting compulsions, you can overcome disturbing, obsessive thoughts by learning to tolerate them through exposure and response prevention exercises. It’s also important to remind yourself that just because you have an unpleasant thought, that doesn’t make you a bad person. Your thoughts are just thoughts. Even unwanted, intrusive, or violent thoughts are normal—it’s only the importance you attach to them that turns them into damaging obsessions.
It’s also important to remind yourself that just because you have an unpleasant thought, that doesn’t make you a bad person. Your thoughts are just thoughts. Even unwanted, intrusive, or violent thoughts are normal—it’s only the importance you attach to them that turns them into damaging obsessions.
The following strategies can help you see your thoughts for what they are and regain a sense of control over your anxious mind.
Write down your obsessive thoughts
Keep a pad and pencil on you, or type on a smartphone. When you begin to obsess, write down all your thoughts or compulsions.
- Keep writing as the OCD urges continue, aiming to record exactly what you're thinking, even if you're repeating the same phrases or the same urges over and over.
- Writing it all down will help you see just how repetitive your obsessions are.
- Writing down the same phrase or urge hundreds of times will help it lose its power.
- Writing thoughts down is much harder work than simply thinking them, so your obsessive thoughts are likely to disappear sooner.

Create an OCD worry period
Rather than trying to suppress obsessions or compulsions, develop the habit of rescheduling them.
- Choose one or two 10-minute “worry periods” each day, time you can devote to obsessing.
- During your worry period, focus only on negative thoughts or urges. Don’t try to correct them. At the end of the worry period, take a few calming breaths, let the obsessive thoughts go, and return to your normal activities. The rest of the day, however, is to be designated free of obsessions.
- When thoughts come into your head during the day, write them down and “postpone” them to your worry period.
Challenge your obsessive thoughts
Use your worry period to challenge negative or intrusive thoughts by asking yourself:
- What’s the evidence that the thought is true? That it’s not true? Have I confused a thought with a fact?
- Is there a more positive, realistic way of looking at the situation?
- What’s the probability that what I’m scared of will actually happen? If the probability is low, what are some more likely outcomes?
- Is the thought helpful? How will obsessing about it help me and how will it hurt me?
- What would I say to a friend who had this thought?
Create a tape of your OCD obsessions or intrusive thoughts
Focus on one specific thought or obsession and record it to a tape recorder or smartphone.
- Recount the obsessive phrase, sentence, or story exactly as it comes into your mind.
- Play the tape back to yourself, over and over for a 45-minute period each day, until listening to the obsession no longer causes you to feel highly distressed.
- By continuously confronting your worry or obsession you will gradually become less anxious. You can then repeat the exercise for a different obsession.
Tip 4: Reach out for support
OCD can get worse when you feel powerless and alone, so it’s important to build a strong support system. The more connected you are to other people, the less vulnerable you’ll feel. And just talking to an understanding person about your worries and urges can make them seem less threatening.
Stay connected to family and friends. Obsessions and compulsions can consume your life to the point of social isolation. In turn, social isolation will aggravate your OCD symptoms. It’s important to invest in relating to family and friends. Talking face-to-face about your worries and urges can make them feel less real and less threatening.
Talking face-to-face about your worries and urges can make them feel less real and less threatening.
Join an OCD support group. You’re not alone in your struggle with OCD, and participating in a support group can be an effective reminder of that. OCD support groups enable you to both share your own experiences and learn from others who are facing the same problems.
Tip 5: Manage stress
While stress doesn’t cause OCD, it can trigger symptoms or make them worse. Physical exercise and connecting with another person face-to-face are two very effective ways to calm your nervous system. You can also:
Quickly self-soothe and relieve anxiety symptoms by making use of one or more of your physical senses—sight, smell, hearing, touch, taste—or movement. You might try listening to a favorite piece of music, looking at a treasured photo, savoring a cup of tea, or stroking a pet.
Practice relaxation techniques. Mindful meditation, yoga, deep breathing, and other relaxation techniques can help lower your overall stress and tension levels and help you manage your urges. For best results, try practicing a relaxation technique regularly.
For best results, try practicing a relaxation technique regularly.
Tip 6: Make lifestyle changes to ease OCD
A healthy, balanced lifestyle plays a big role in easing anxiety and keeping OCD compulsions, fears, and worry at bay.
Exercise regularly. Exercise is a natural and effective anti-anxiety treatment that helps to control OCD symptoms by refocusing your mind when obsessive thoughts and compulsions arise. For maximum benefit, try to get 30 minutes or more of aerobic activity on most days. Ten minutes several times a day can be as effective as one longer period especially if you pay mindful attention to the movement process.
Get enough sleep. Not only can anxiety and worry cause insomnia, but a lack of sleep can also exacerbate anxious thoughts and feelings. When you're well rested, it's much easier to keep your emotional balance, a key factor in coping with anxiety disorders such as OCD.
Avoid alcohol and nicotine.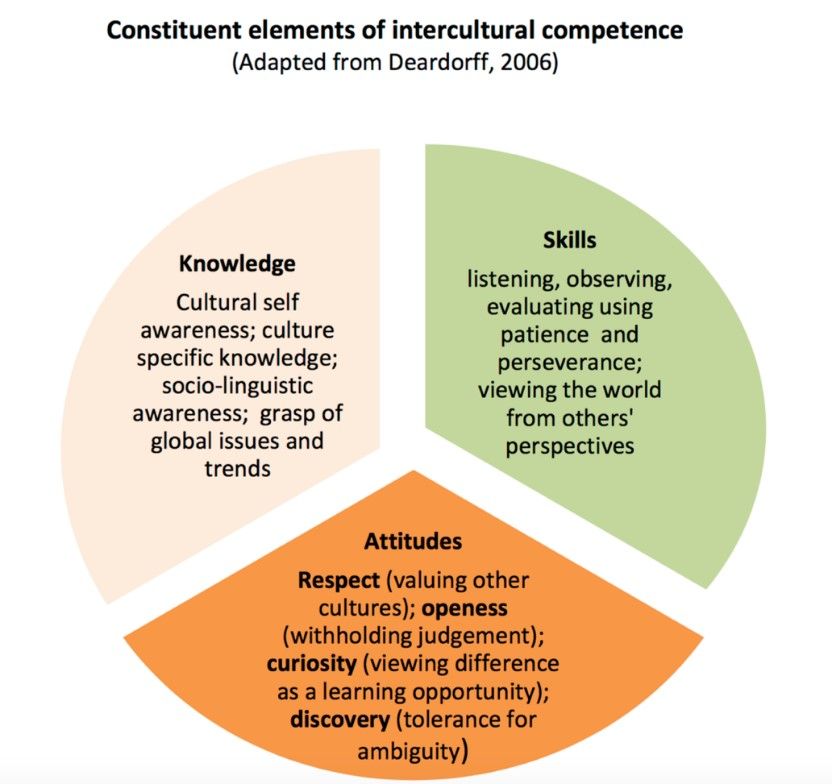 Alcohol temporarily reduces anxiety and worry, but it actually causes anxiety symptoms as it wears off. Similarly, while it may seem that cigarettes are calming, nicotine is actually a powerful stimulant. Smoking leads to higher, not lower, levels of anxiety and OCD symptoms.
Alcohol temporarily reduces anxiety and worry, but it actually causes anxiety symptoms as it wears off. Similarly, while it may seem that cigarettes are calming, nicotine is actually a powerful stimulant. Smoking leads to higher, not lower, levels of anxiety and OCD symptoms.
Treatment for OCD
Cognitive-behavioral therapy is the most effective treatment for obsessive-compulsive disorder and generally involves two components:
- Exposure and response prevention, which requires repeated exposure to the source of your obsession, as explained above.
- Cognitive therapy, which focuses on the catastrophic thoughts and exaggerated sense of responsibility you feel. A big part of cognitive therapy for OCD is teaching you healthy and effective ways of responding to obsessive thoughts, without resorting to compulsive behavior.
Other OCD treatments
In addition to cognitive-behavioral therapy, the following treatments are also used for OCD:
Medication.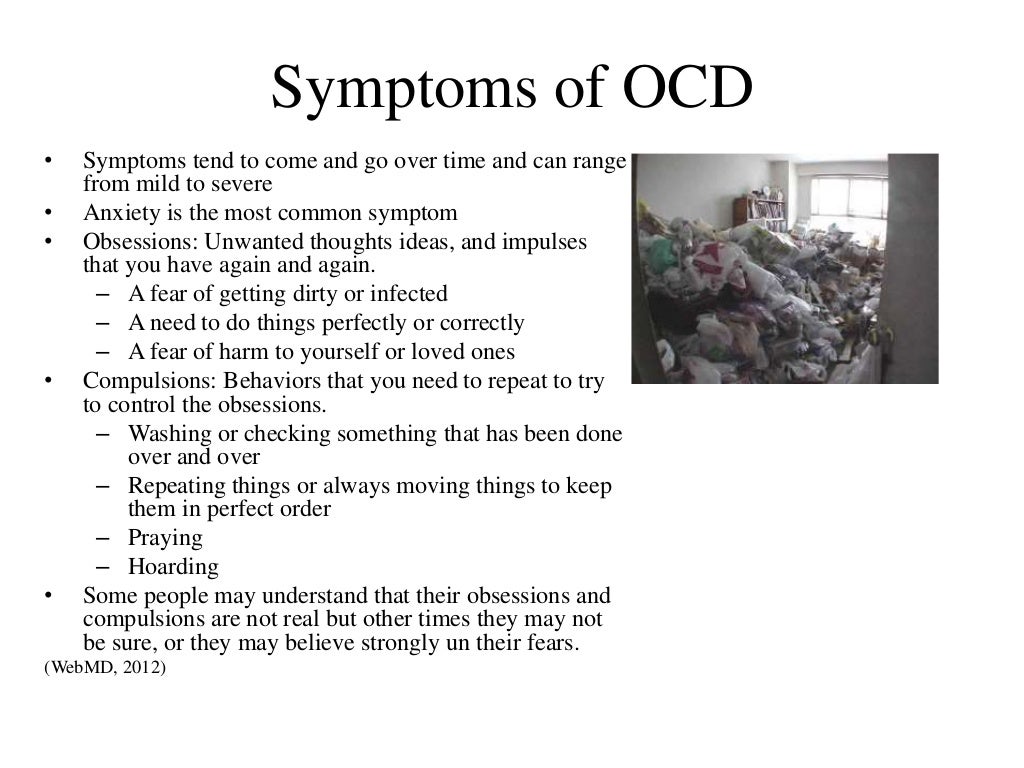 Antidepressants are sometimes used in conjunction with therapy for the treatment of obsessive-compulsive disorder. However, medication alone is rarely effective in relieving the symptoms.
Antidepressants are sometimes used in conjunction with therapy for the treatment of obsessive-compulsive disorder. However, medication alone is rarely effective in relieving the symptoms.
Family Therapy. Since OCD often causes problems in family life and social adjustment, family therapy can help promote understanding of the disorder and reduce family conflicts. It can also motivate family members and teach them how to help their loved one with OCD.
Group Therapy. Through interaction with fellow OCD sufferers, group therapy provides support and encouragement and decreases feelings of isolation.
Is unresolved trauma playing a role in your OCD?
In some people, OCD symptoms such as compulsive washing or hoarding are ways of coping with trauma. If you have post-traumatic OCD, cognitive approaches may not be effective until underlying traumatic issues are resolved.
How to help someone with OCD
The way you react to your loved one's OCD symptoms can have a big impact on their outlook and recovery. Negative comments or criticism can make OCD worse, while a calm, supportive environment can help improve the outcome of treatment.
Negative comments or criticism can make OCD worse, while a calm, supportive environment can help improve the outcome of treatment.
Avoid making personal criticisms. Remember, your loved one's OCD behaviors are symptoms, not character flaws.
Don't scold someone with OCD or tell them to stop performing rituals. They can't comply, and the pressure to stop will only make the behaviors worse.
Be as kind and patient as possible. Each sufferer needs to overcome problems at their own pace. Praise any successful attempt to resist OCD, and focus attention on positive elements in the person's life.
Do not play along with your loved one’s rituals. Going along with your loved one’s OCD “rules,” or helping with their compulsions or rituals will only reinforce the behavior. Support the person, not their compulsions.
Keep communication positive and clear. Communication is important so you can find a balance between supporting your loved one and standing up to the OCD symptoms and not further distressing your loved one.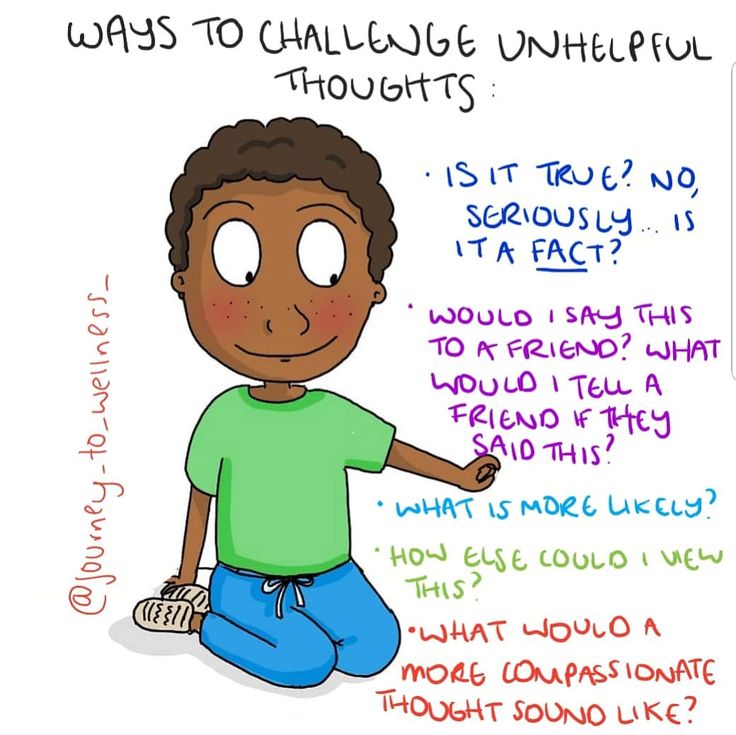
Find the humor. Laughing together over the funny side and absurdity of some OCD symptoms can help your loved one become more detached from the disorder. Just make sure your loved one feels respected and in on the joke.
Don't let OCD take over family life. Sit down as a family and decide how you will work together to tackle your loved one's symptoms. Try to keep family life as normal as possible and the home a low-stress environment.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive–compulsive disorder. Nature Reviews Disease Primers, 5(1), 1–21. https://doi.org/10.1038/s41572-019-0102-3
Fineberg, N. A., Hollander, E., Pallanti, S., Walitza, S.
 , Grünblatt, E., Dell’Osso, B. M., Albert, U., Geller, D. A., Brakoulias, V., Janardhan Reddy, Y. C., Arumugham, S. S., Shavitt, R. G., Drummond, L., Grancini, B., De Carlo, V., Cinosi, E., Chamberlain, S. R., Ioannidis, K., Rodriguez, C. I., … Menchon, J. M. (2020). Clinical advances in obsessive-compulsive disorder: A position statement by the International College of Obsessive-Compulsive Spectrum Disorders. International Clinical Psychopharmacology, 35(4), 173–193. https://doi.org/10.1097/YIC.0000000000000314
, Grünblatt, E., Dell’Osso, B. M., Albert, U., Geller, D. A., Brakoulias, V., Janardhan Reddy, Y. C., Arumugham, S. S., Shavitt, R. G., Drummond, L., Grancini, B., De Carlo, V., Cinosi, E., Chamberlain, S. R., Ioannidis, K., Rodriguez, C. I., … Menchon, J. M. (2020). Clinical advances in obsessive-compulsive disorder: A position statement by the International College of Obsessive-Compulsive Spectrum Disorders. International Clinical Psychopharmacology, 35(4), 173–193. https://doi.org/10.1097/YIC.0000000000000314Huppert, J. D. (20141222). Treating obsessive-compulsive disorder with exposure and response prevention. The Behavior Analyst Today, 4(1), 66. https://doi.org/10.1037/h0100012
Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: Systematic review and meta-analysis. BMC Psychiatry, 11(1), 200. https://doi.org/10.1186/1471-244X-11-200
Geller, D. A., & March, J. (2012). Practice Parameter for the Assessment and Treatment of Children and Adolescents With Obsessive-Compulsive Disorder.
 Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98–113. https://doi.org/10.1016/j.jaac.2011.09.019
Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98–113. https://doi.org/10.1016/j.jaac.2011.09.019Kalra, S. K., & Swedo, S. E. (2009). Children with obsessive-compulsive disorder: Are they just “little adults”? The Journal of Clinical Investigation, 119(4), 737–746. https://doi.org/10.1172/JCI37563
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience, 13(4), 413–421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3263389/
Tolin, D. F. (2010). Is cognitive–behavioral therapy more effective than other therapies?: A meta-analytic review. Clinical Psychology Review, 30(6), 710–720. https://doi.org/10.1016/j.cpr.2010.05.003
Aylett, E., Small, N., & Bower, P. (2018). Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Services Research, 18(1), 559. https://doi.org/10.1186/s12913-018-3313-5
Kandola, A.
 , Vancampfort, D., Herring, M., Rebar, A., Hallgren, M., Firth, J., & Stubbs, B. (2018). Moving to Beat Anxiety: Epidemiology and Therapeutic Issues with Physical Activity for Anxiety. Current Psychiatry Reports, 20(8), 63. https://doi.org/10.1007/s11920-018-0923-x
, Vancampfort, D., Herring, M., Rebar, A., Hallgren, M., Firth, J., & Stubbs, B. (2018). Moving to Beat Anxiety: Epidemiology and Therapeutic Issues with Physical Activity for Anxiety. Current Psychiatry Reports, 20(8), 63. https://doi.org/10.1007/s11920-018-0923-xObsessive-Compulsive and Related Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x06_Obsessive_Compulsive_and_Related_Disorders
Table 3.13, DSM-IV to DSM-5 Obsessive-Compulsive Disorder Comparison—Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health—NCBI Bookshelf. (n.d.). Retrieved November 21, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch4.t13/
Van Ameringen, M., Patterson, B., & Simpson, W. (2014). DSM-5 OBSESSIVE-COMPULSIVE AND RELATED DISORDERS: CLINICAL IMPLICATIONS OF NEW CRITERIA: Review: DSM-5 OCD and Related Disorders.
 Depression and Anxiety, 31(6), 487–493. https://doi.org/10.1002/da.22259
Depression and Anxiety, 31(6), 487–493. https://doi.org/10.1002/da.22259Goodwin, Guy M. “The Overlap between Anxiety, Depression, and Obsessive-Compulsive Disorder.” Dialogues in Clinical Neuroscience 17, no. 3 (September 2015): 249–60. https://doi.org/10.31887/DCNS.2015.17.3/ggoodwin
What You Need to Know About Obsessive Compulsive Disorder (PDF) – Including signs, symptoms, and treatment. (International OCD Foundation)
Obsessive-Compulsive Disorder in Children – Including common symptoms and behaviors. (KidsHealth)
Build a Fear Ladder – How to create and use fear ladders. (Anxiety Canada Youth)
(Video) Obsessive Compulsive Disorder – Explanatory video from Khan Academy and American Association of Colleges of Nursing. (YouTube)
Hotlines and support
In the U.S.: Call the NAMI Helpline at 1-800-950-6264. Or Find a Therapist.
UK: Call Anxiety UK at 03444 775 774.
Canada: Find services at Anxiety Canada.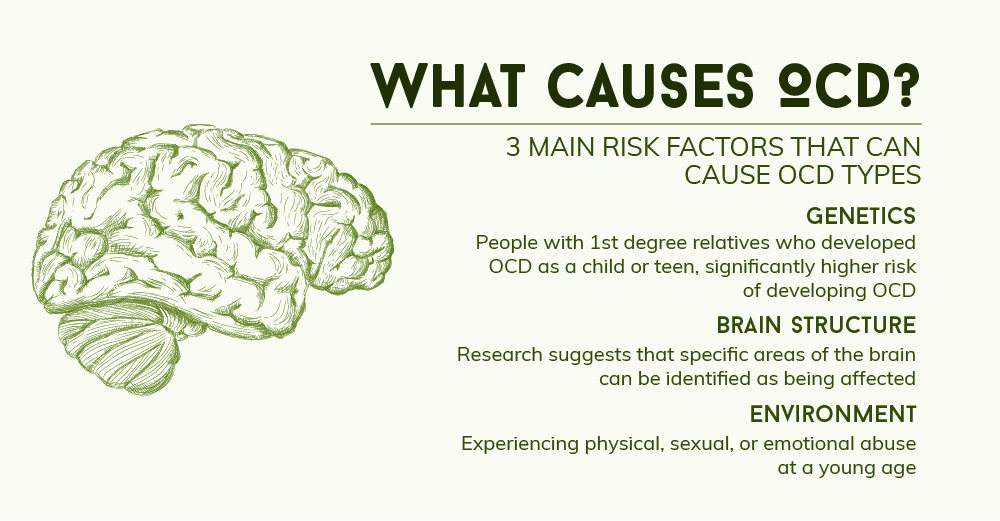
Australia: Call the SANE Help Centre at 1800 18 7263.
India: Call the Vandrevala Foundation at 1860 2662 345 or 1800 2333 330.
In other countries: Access a global database of OCD resources from the International OCD Foundation.
Last updated: December 30, 2022
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further.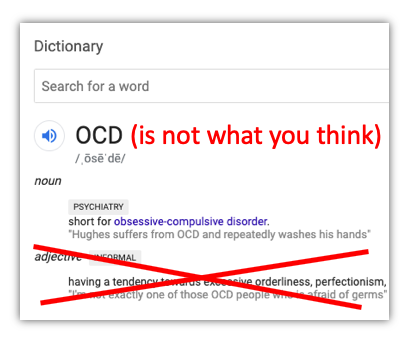 Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head. nine0003
Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head. nine0003
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you. nine0003
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last". nine0003
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row. nine0003
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed.
 Do I have OCD?
Do I have OCD? Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem. nine0003
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists. nine0050
- The thought of a person performing a compulsive action should not in itself be pleasurable.
 The fact that an action will help reduce anxiety is not considered pleasant in this sense.
The fact that an action will help reduce anxiety is not considered pleasant in this sense. - Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number. nine0003
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts.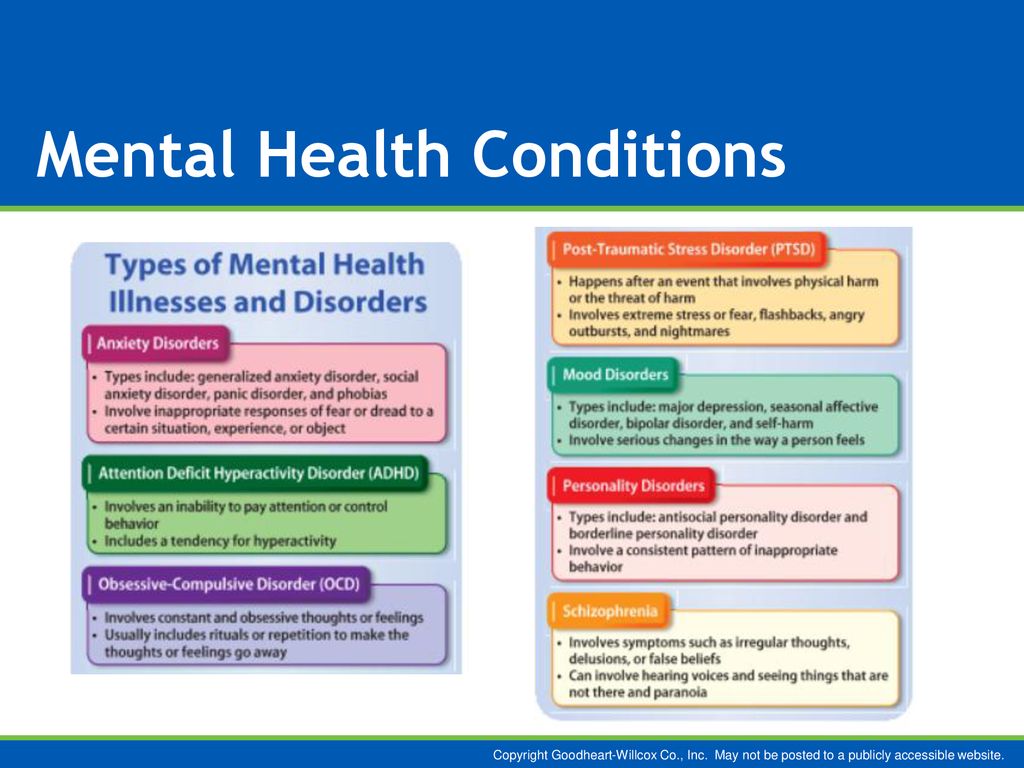 As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions. nine0003
As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions. nine0003
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away. nine0003
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist. nine0003
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help. nine0003
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons. nine0003
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared. nine0003
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
This is how a referral for hospitalization to a day hospital looks like The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital. nine0003
nine0003
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise. nine0003 During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man did not let me stop the treatment
They noticed the changes, but my young man did not let me stop the treatment
Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription. nine0003
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refusedTreatment
Second hospitalization and psychotherapy After six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital.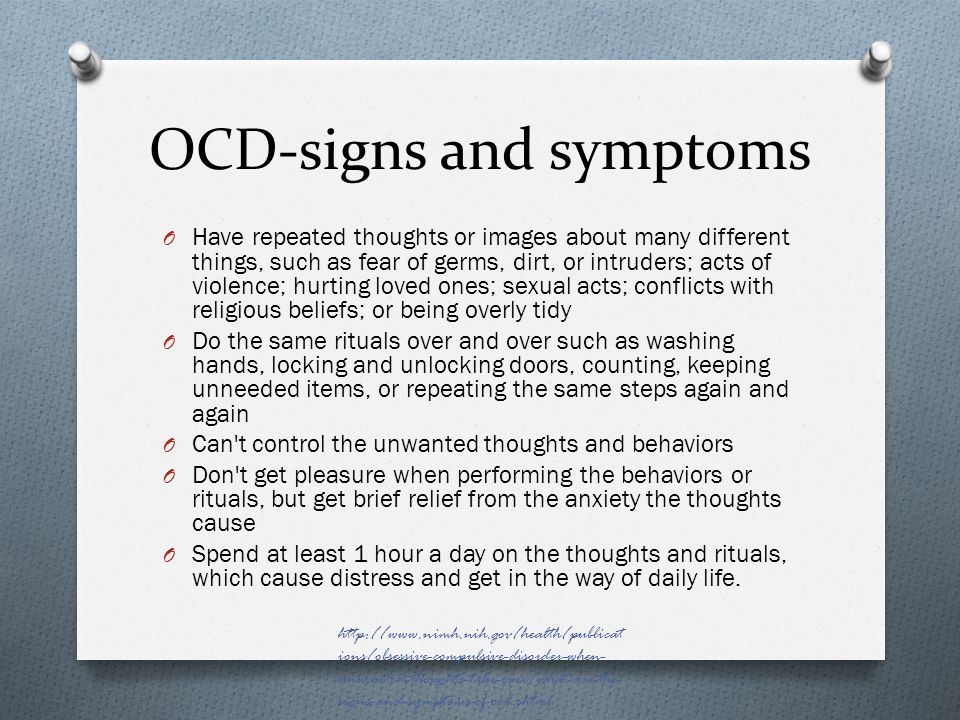 Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts. nine0003
Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts. nine0003
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression. nine0003
Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression. nine0003
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person. nine0003
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them. nine0003
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions.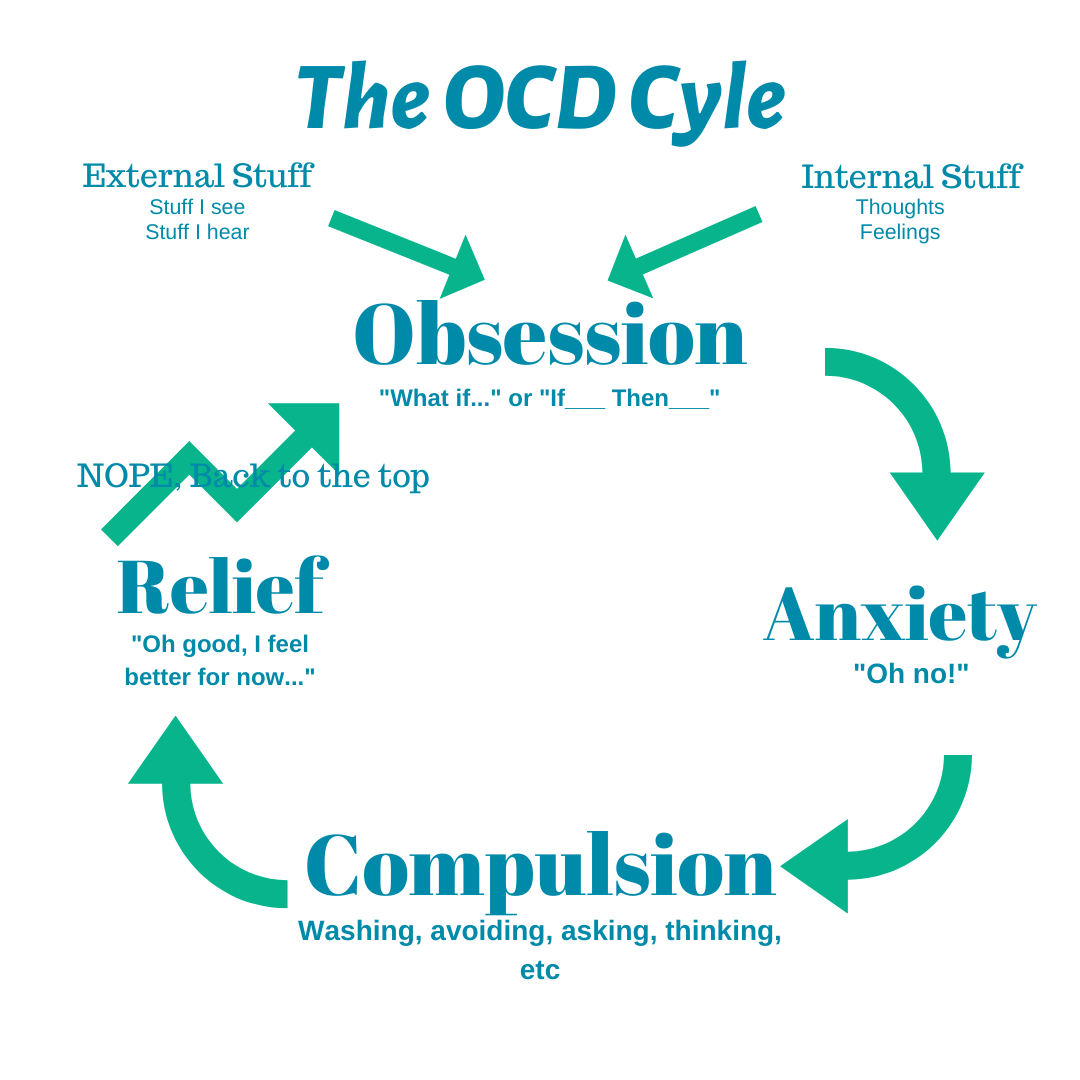 Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully. nine0003 I filled out the diary for a week, and then the psychotherapist and I analyzed the notes
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully. nine0003 I filled out the diary for a week, and then the psychotherapist and I analyzed the notes
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary.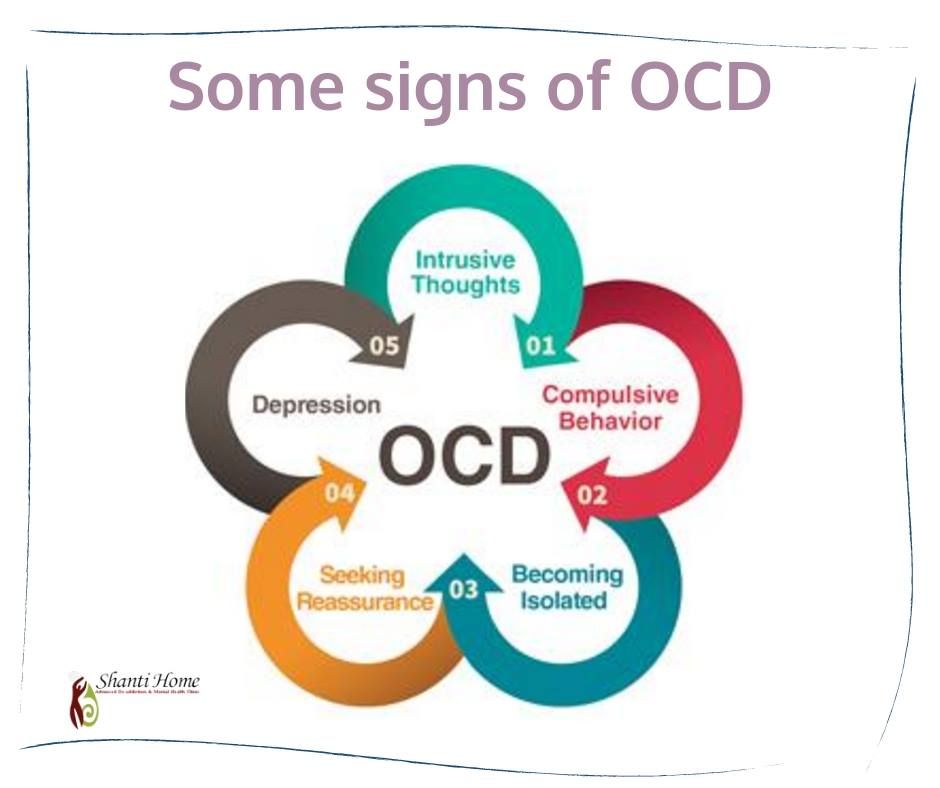 Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better. nine0003
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts.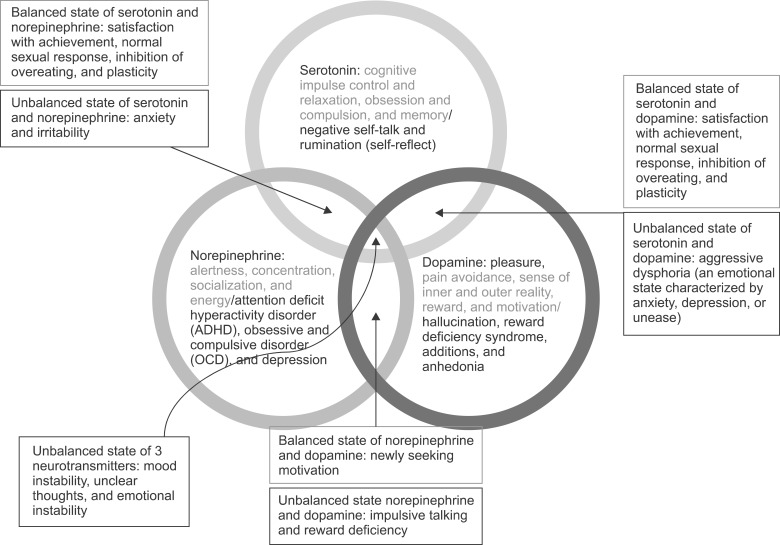 I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 P |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal. nine0003
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me.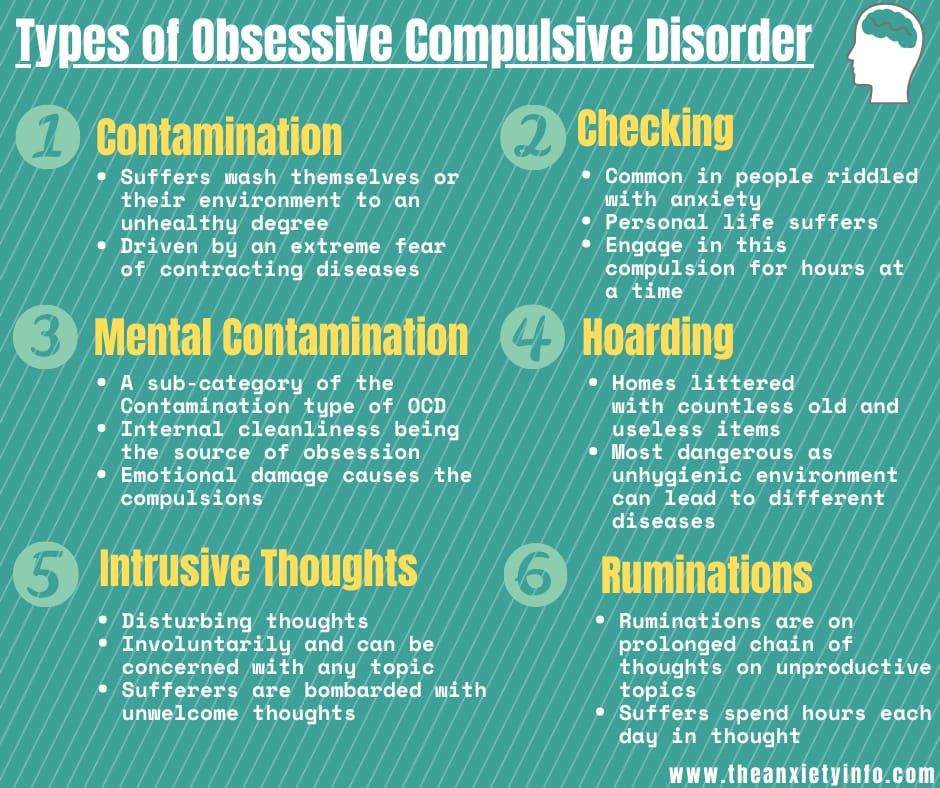 The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis. nine0003
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job. nine0050
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
Obsessive Compulsive Disorder | The CALDA Clinic
Treatment Options: Obsessive-Compulsive Disorder
Approximately 2-3 percent of all people suffer from obsessive-compulsive disorder at some time in their lives.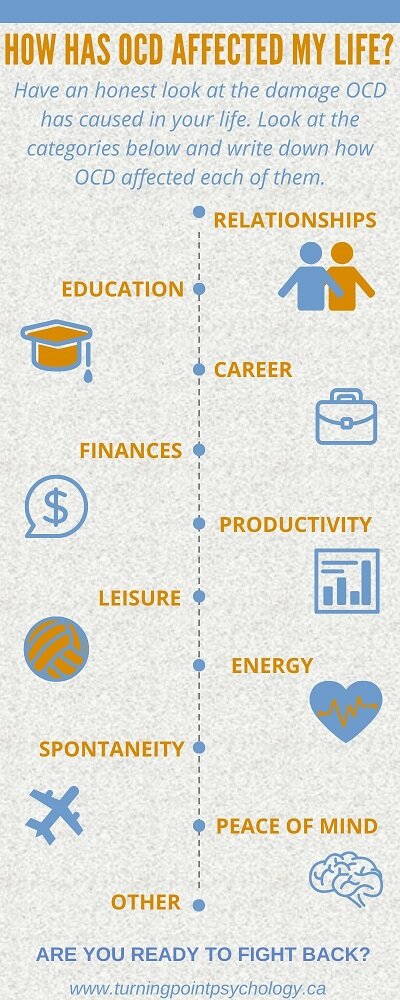 Among them are many celebrities: “When I am under stress, the same thought constantly revolves in my head, because I am afraid that otherwise something bad will happen,” singer Camila Cabello admits to Cosmopolitan magazine. The star of the musical Mamma Mia, Amanda Seyfried, also openly admits her obsessive-compulsive disorder and explains that she treated him with antidepressants for more than eleven years. nine0003
Among them are many celebrities: “When I am under stress, the same thought constantly revolves in my head, because I am afraid that otherwise something bad will happen,” singer Camila Cabello admits to Cosmopolitan magazine. The star of the musical Mamma Mia, Amanda Seyfried, also openly admits her obsessive-compulsive disorder and explains that she treated him with antidepressants for more than eleven years. nine0003
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder, formerly also called obsessive-compulsive disorder, is a serious mental illness. Patients perform repetitive unwanted actions and "rituals" accompanied by corresponding negative or dangerous thoughts. The disease usually begins around the age of 20. The first symptoms may also appear during puberty or during childhood. Even healthy people can experience temporary compulsions. For example, many people are familiar with anxious thoughts that arise after leaving the house, such as “Did I turn off the coffee maker, turn off the light, lock the door, etc.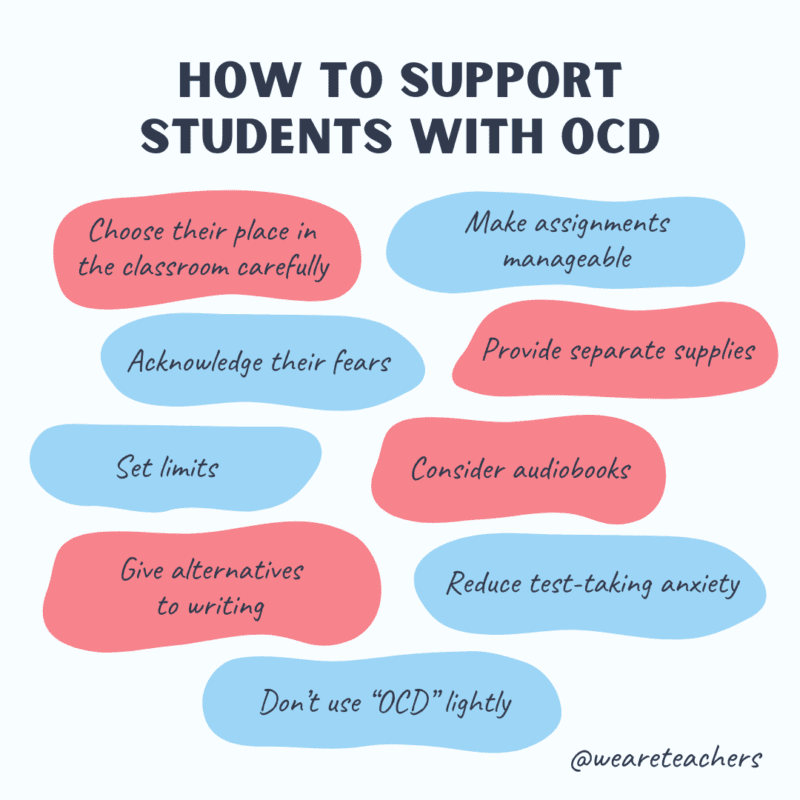 ?”. Despite the fact that a person knows for sure that everything has been done, he has a short desire to double-check again. Most people manage to calm down in such a situation, and only a few really "bother". nine0003
?”. Despite the fact that a person knows for sure that everything has been done, he has a short desire to double-check again. Most people manage to calm down in such a situation, and only a few really "bother". nine0003
More than just a fad
However, people with obsessive-compulsive disorder are usually quite aware that their obsessive thoughts are far from reality and exaggerated and that obsessive actions are useless or even harmful. However, unlike healthy people, they do not manage to reset this obsession. Patients who try to stop unwanted "rituals" experience a very strong tension that they cannot endure for a long time. Therefore, in order to reduce the internal pressure, they soon return to harmful thoughts and actions. Despite the fact that they are illogical and often quite unpleasant, the patient still returns to obsessive thoughts and compulsive actions again and again in a stereotypical manner for several days a week or even several times a day, often for hours. This creates a vicious circle that is extremely painful for the patient and greatly impairs the quality of his daily life, well-being and performance. nine0003
This creates a vicious circle that is extremely painful for the patient and greatly impairs the quality of his daily life, well-being and performance. nine0003
How does OCD manifest itself?
Obsessive-compulsive disorder can manifest itself in obsessive thoughts and/or obsessive actions (compulsions). In most cases, obsessive thoughts and compulsions occur at the same time. Depending on the primary symptoms, obsessive-compulsive disorder is divided into three types:
Obsessive-compulsive disorder. Important features:
- mostly intrusive thoughts or ruminations;
- mostly compulsive actions;
- mixed obsessive thoughts and actions. Obsessive-compulsive disorder with a predominance of obsessive thoughts or reflections Intrusive thoughts are usually negative, distressing, and very disturbing to the person. They are often in the form of "mental spirals". Obsessive-compulsive thoughts are characterized by anxiety, threat, often contradiction and inconsistency with the situation in which the person actually finds himself. In particular, mental urges to act are often perceived as extremely frightening and are usually not put into practice. Typical examples of obsessive thoughts or obsessive impulses Obsessive Compulsive Disorder can also be characterized by repetitive rituals and activities that the patient cannot avoid. Typical examples: Fearing possible infections, patients wash their hands many times a day with soap, take a shower several times, rub their skin with hard brushes, constantly wash and change clothes, endlessly clean the apartment, disinfect doorknobs, work surfaces, objects, etc. Items must be arranged, arranged or assembled in a very specific order or manner. They must match a certain size, color, quantity, theme, symmetry, etc. This correspondence is regularly rechecked and infinitely corrected. The patient constantly checks to see if the door is locked, if the windows are closed, if electrical appliances are turned off, if the faucet is leaking, etc. nine0003 Because of the fear of throwing away something important, the patient accumulates everything, even unnecessary items and rubbish. If something is thrown away, there is often a strong urge to search the trash cans to make sure nothing important has been thrown away. In order to prevent imaginary dangers, catastrophes, etc. In more than 90%, that is, in the vast majority of cases, obsessive thoughts and obsessive actions occur simultaneously. This means that the majority of all patients suffer from obsessive-compulsive disorder, in which there are both painful obsessive-compulsive thoughts and stereotypical compulsive actions. Obsessive-compulsive disorder is not a quirk of some people who may appear slightly superstitious, overly clean, or especially tidy. The exact causes of OCD are not yet clearly understood. However, certain factors have been identified that are known to be particularly conducive to the development or maintenance of OCD. Research shows that heredity does play a role in the development of OCD. Although the disease is not directly transmitted, the risk of a child getting OCD has been shown to increase if one or both parents have OCD. This is also supported by the results of twin studies. Imaging studies have also shown that metabolism and brain activity in certain areas of the brain in people with obsessive-compulsive disorder are markedly increased. In particular, it was possible to detect anomalies in the basal ganglia, which, among other things, are responsible for motor processes. In addition, the balance of serotonin is disturbed. The environment in which a person grows up has a significant impact on the development of personality. A parenting style with high academic demands, strict assessment models, and perfectionist demands, as well as "fearful" parenting methods in which the child is overprotective and constantly protected from all sorts of adversity, can all contribute to the development of obsessive-compulsive disorders. nine0003 Also important risk factors for the development of obsessive-compulsive disorders are experienced trauma or mental overload. Excessively stressful events such as violence, abuse, rape, death of a loved one, etc. can unsettle a person and often cause a strong sense of insecurity and insecurity. Understandably, there is also a growing desire for control and security. The performance of "protective", "neutralizing", or "cleansing" compulsions and rituals gives the sufferer a sense of control over a situation in which they would otherwise feel helpless. Last but not least, individual personality structure also determines to some extent whether a person develops obsessive-compulsive disorder. People who are inherently fearful, vulnerable, unstable, or overly sensitive have a higher risk of developing obsessive-compulsive disorder than confident and calm individuals. Obsessive-compulsive disorders are very often diagnosed in conjunction with other psychiatric as well as dermatological diseases. The most common comorbidities associated with obsessive-compulsive disorder include: —Depressive moods and depressions —Eating disorders —Anxiety disorders —Social phobias - Post-traumatic stress disorder - Dermatillomania and trichotillomania Impulse control disorders in which the patient repeatedly scratches, squeezes and breaks the skin or pulls out hair, eyebrows or eyelashes. - Dysmorphophobic disorder distorted perception of one's own body, in which a slight "anomaly" is regarded as a completely disfiguring feature, and there is an excessive concern for an imagined flaw. nine0063  In this sense, one can speak of obsessive thoughts. Intrusive thoughts are usually perceived by people as belonging to themselves. At the same time, a person in most cases recognizes the meaninglessness and uselessness of these thoughts. But he can't get rid of them. This can lead to the impossibility of making even simple everyday decisions, since it is necessary to first weigh all possible, including completely irrational, alternatives. nine0003
In this sense, one can speak of obsessive thoughts. Intrusive thoughts are usually perceived by people as belonging to themselves. At the same time, a person in most cases recognizes the meaninglessness and uselessness of these thoughts. But he can't get rid of them. This can lead to the impossibility of making even simple everyday decisions, since it is necessary to first weigh all possible, including completely irrational, alternatives. nine0003 Symptoms. Examples of obsessive thoughts
 nine0050 №
nine0050 № Obsessive Compulsive Disorder
 nine0003
nine0003
 , the patient is forced to repeat certain actions in a certain amount and in a certain order over and over again. This should help prevent the impending "danger". For example, the patient may forbid himself from touching certain tiles, stones, patterns, and so on. or requires himself to take ten steps back fifty times, say a "special" saying seven times, and so on. nine0003
, the patient is forced to repeat certain actions in a certain amount and in a certain order over and over again. This should help prevent the impending "danger". For example, the patient may forbid himself from touching certain tiles, stones, patterns, and so on. or requires himself to take ten steps back fifty times, say a "special" saying seven times, and so on. nine0003 Obsessive-compulsive disorder with obsessive thoughts and actions
Obsessive-compulsive disorder: impact on daily life
 This is a serious disease in which people cease to control their thoughts and actions, even if they really want to, and because of which they suffer painfully. It is not uncommon for sufferers to waste several hours a day performing compulsive acts and tormenting themselves with intrusive thoughts. This not only burdens daily life and reduces the patient's ability to work, but also has a huge impact on his social environment, i.e. parents, partners, children, etc. Normal life becomes impossible for long periods of time, causing close family members to leave at some point and marriages to fall apart. In addition to serious psychological and social consequences, there are usually complaints about the physical condition. Serious skin diseases can occur, especially when the disease is accompanied by an obsessive desire to wash and clean. nine0003
This is a serious disease in which people cease to control their thoughts and actions, even if they really want to, and because of which they suffer painfully. It is not uncommon for sufferers to waste several hours a day performing compulsive acts and tormenting themselves with intrusive thoughts. This not only burdens daily life and reduces the patient's ability to work, but also has a huge impact on his social environment, i.e. parents, partners, children, etc. Normal life becomes impossible for long periods of time, causing close family members to leave at some point and marriages to fall apart. In addition to serious psychological and social consequences, there are usually complaints about the physical condition. Serious skin diseases can occur, especially when the disease is accompanied by an obsessive desire to wash and clean. nine0003 Causes of OCD
 As a rule, the development of OKR requires the combination of several factors. The importance of individual factors for each individual patient is individual. The most important risk factors for developing obsessive-compulsive disorder are:
As a rule, the development of OKR requires the combination of several factors. The importance of individual factors for each individual patient is individual. The most important risk factors for developing obsessive-compulsive disorder are:
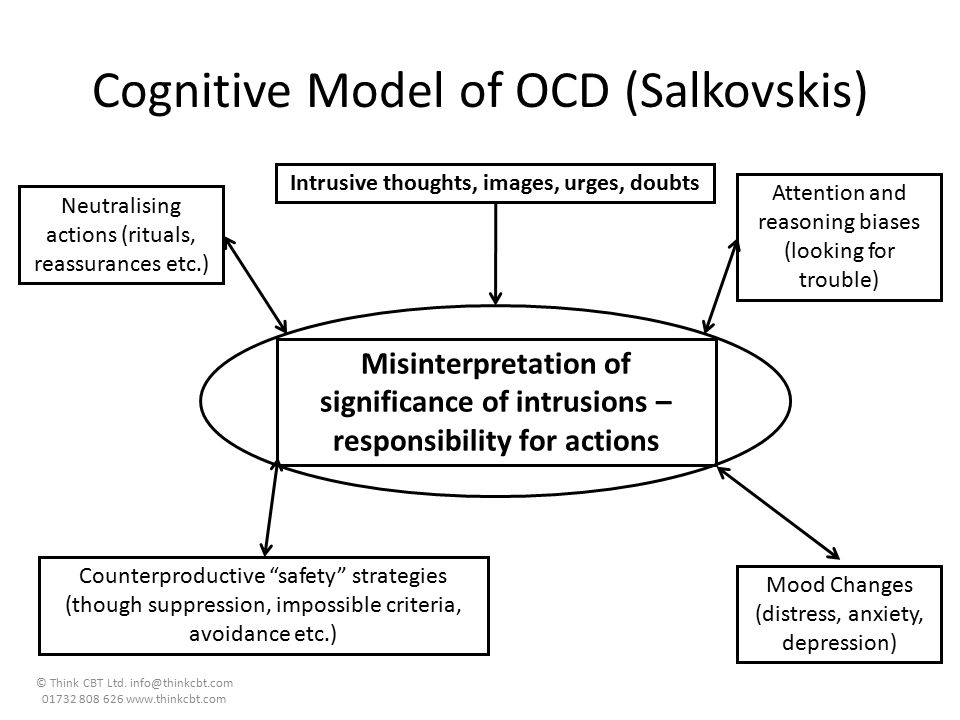 nine0003
nine0003
Common comorbidities of obsessive-compulsive disorder

- Atopic dermatitis and other skin diseases
eczema occurs mainly in compulsive washing syndrome due to persistent excessive irritation of the skin.
What are the treatments for OCD?
People with OCD know that their thoughts, actions, and rituals are irrational, but are unable to deal with them on their own. As a rule, they are very ashamed of this and try their best to hide their suffering from others. Therefore, obsessive-compulsive disorders are often diagnosed very late. On average, it takes 10 years for patients to seek professional help, but periods of 20 to 30 years are also not uncommon. Often patients are forced to see a doctor not even by the obsessive-compulsive disorder itself, but by a concomitant disease, such as severe dermatitis.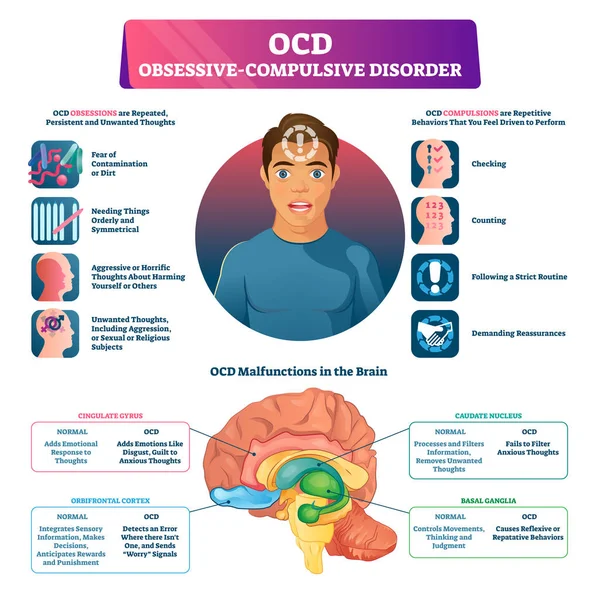 At this stage, the disease has usually already taken root, and the symptoms have greatly increased both in number and severity. nine0003
At this stage, the disease has usually already taken root, and the symptoms have greatly increased both in number and severity. nine0003
Complex causes require complex treatment at multiple levels
As with most diseases, it is best to start treatment as early as possible if you have OCD. However, even at an extended stage, very good therapeutic results can still be achieved. The multimodal approach, combining a variety of proven therapeutic options, has proven to be particularly effective. It allows you to accurately recognize many different individual causes of the disease and provide optimal treatment for the patient at every stage and at different levels. In addition, this technique allows you to recognize and effectively eliminate any individually caused physical problems and imbalances and professionally treat all associated diseases. nine0003
Modern treatments for obsessive-compulsive disorder have so far mainly involved the use of psychotherapy and psychotropic drugs.
Everything is different with us!
The CALDA concept: Let us help you!
As a client of the CALDA clinic, you are assigned a 1:1 individual therapy based on the CALDA concept, which is tailored specifically to your needs. It is a personalized, highly effective, holistically oriented, ultra-precise therapy: scientifically based methods of classical medicine are combined with specially approved therapies of complementary, traditional Chinese (TCM) and orthomolecular medicine. nine0003
Your advantage: Treatment with the CALDA concept works very effectively at different levels of the body and is problem oriented. As a result, amazing results can be achieved in a short time - and often without the use of psychotropic drugs!
CALDA concept
Our motto and guarantee:
we treat the causes, not the symptoms!
If possible, we work without psychotropic drugs! nine0003
Our time and all our know-how is an exclusive service for a specific client.