Going off antidepressant
Going Off Antidepressants - Harvard Health Publishing
Coming off your medication can cause antidepressant withdrawal – and could set you up for a relapse of depression.
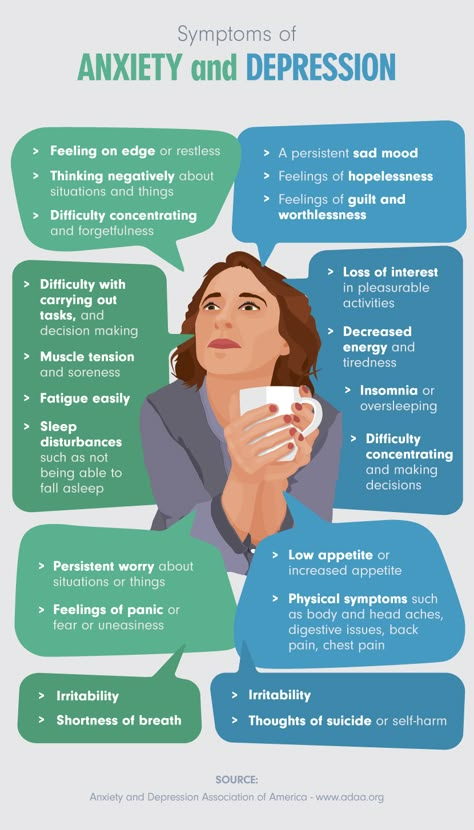
Can going off your medication cause antidepressant withdrawal symptoms (antidepressant discontinuation syndrome)? About 10% of women ages 18 and over take antidepressants. As many of us know, these medications can be a godsend when depression has robbed life of its joy and made it hard to muster the energy and concentration to complete everyday tasks. But as you begin to feel better and want to move on, how long should you keep taking the pills?
If you're doing well on antidepressants and not complaining of too many side effects, many physicians will renew the prescription indefinitely — figuring that it offers a hedge against a relapse of depression. But side effects that you may have been willing to put up with initially — sexual side effects (decreased desire and difficulty having an orgasm), headache, insomnia, drowsiness, vivid dreaming, or just not feeling like yourself — can become less acceptable over time, especially if you think you no longer need the pills.
The decision to go off antidepressants should be considered thoughtfully and made with the support of your physician or therapist to make sure you're not stopping prematurely, risking a recurrence of depression. Once you decide to quit, you and your physician should take steps to minimize or avoid the discontinuation symptoms that can occur if such medications are withdrawn too quickly.
Why antidepressant withdrawal?
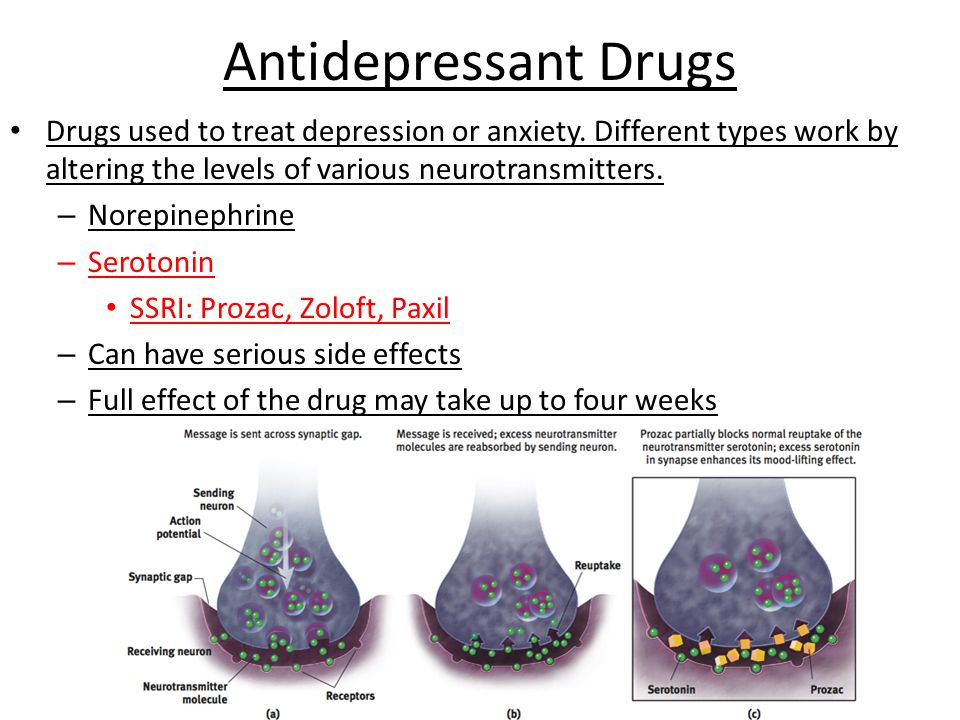
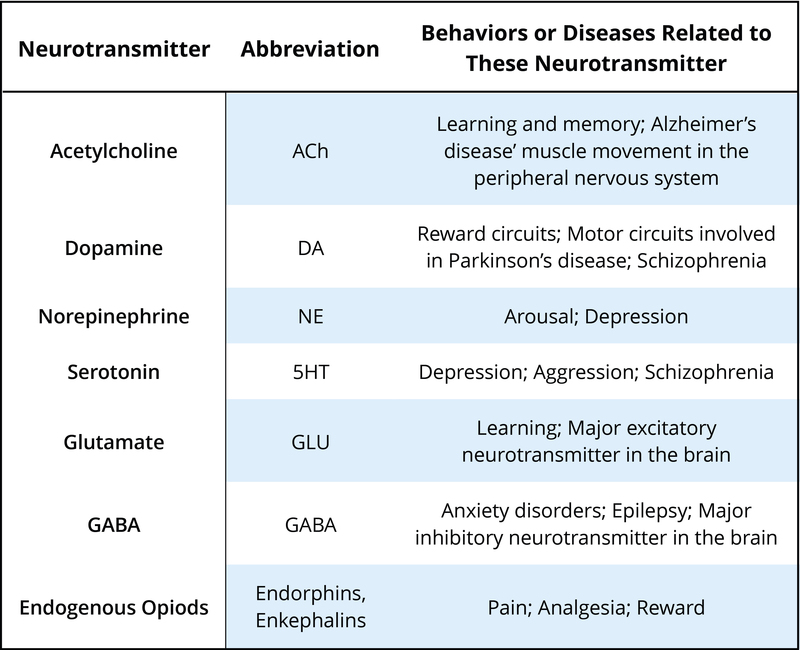
Antidepressants work by altering the levels of neurotransmitters — chemical messengers that attach to receptors on neurons (nerve cells) throughout the body and influence their activity. Neurons eventually adapt to the current level of neurotransmitters, and symptoms that range from mild to distressing may arise if the level changes too much too fast — for example, because you've suddenly stopped taking your antidepressant. They're generally not medically dangerous but may be uncomfortable.
Among the newer antidepressants, those that influence the serotonin system — selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) — are associated with a number of withdrawal symptoms, often called antidepressant or SSRI discontinuation syndrome. Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Having discontinuation symptoms doesn't mean you're addicted to your antidepressant. A person who is addicted craves the drug and often needs increasingly higher doses. Few people who take antidepressants develop a craving or feel a need to increase the dose. (Sometimes an SSRI will stop working — a phenomenon called "Prozac poop-out" — which may necessitate increasing the dose or adding another drug.)
Antidepressant withdrawal can look like depressionDiscontinuation symptoms can include anxiety and depression. Since these may be the reason you were prescribed antidepressants in the first place, their reappearance may suggest that you're having a relapse and need ongoing treatment.
If symptoms last more than a month and are worsening, it's worth considering whether you're having a relapse of depression. |
Antidepressant withdrawal symptoms
Neurotransmitters act throughout the body, and you may experience physical as well as mental effects when you stop taking antidepressants or lower the dose too fast.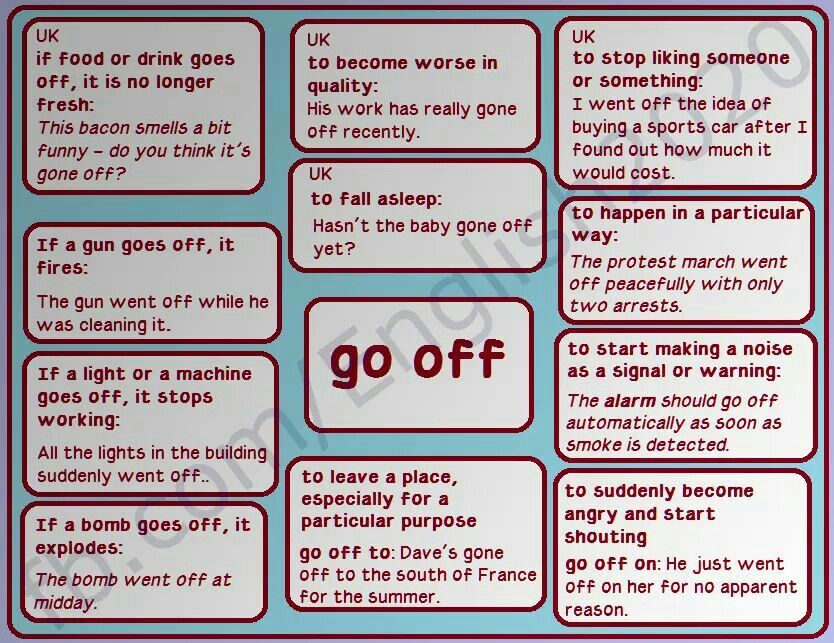 Common complaints include the following:
Common complaints include the following:
- Digestive. You may have nausea, vomiting, cramps, diarrhea, or loss of appetite.
- Blood vessel control. You may sweat excessively, flush, or find hot weather difficult to tolerate.
- Sleep changes. You may have trouble sleeping and unusual dreams or nightmares.
- Balance. You may become dizzy or lightheaded or feel like you don't quite have your "sea legs" when walking.
- Control of movements. You may experience tremors, restless legs, uneven gait, and difficulty coordinating speech and chewing movements.
- Unwanted feelings. You may have mood swings or feel agitated, anxious, manic, depressed, irritable, or confused — even paranoid or suicidal.
- Strange sensations.
You may have pain or numbness; you may become hypersensitive to sound or sense a ringing in your ears; you may experience "brain-zaps" — a feeling that resembles an electric shock to your head — or a sensation that some people describe as "brain shivers.
 "
"
As dire as some of these symptoms may sound, you shouldn't let them discourage you if you want to go off your antidepressant. Many of the symptoms of SSRI discontinuation syndrome can be minimized or prevented by gradually lowering, or tapering, the dose over weeks to months, sometimes substituting longer-acting drugs such as fluoxetine (Prozac) for shorter-acting medications. The antidepressants most likely to cause troublesome symptoms are those that have a short half-life — that is, they break down and leave the body quickly. (See the chart "Antidepressant drugs and their half-lives.") Examples include venlafaxine (Effexor), sertraline (Zoloft), paroxetine (Paxil), and citalopram (Celexa). Extended-release versions of these drugs enter the body more slowly but leave it just as fast. Antidepressants with a longer half-life, chiefly fluoxetine, cause fewer problems on discontinuation.
Besides easing the transition, tapering the dose decreases the risk that depression will recur. In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
Antidepressant drugs and their half-lives* | ||
| Drug | Half out of body in | 99% out of body in |
| Serotonin reuptake inhibitors | ||
| paroxetine (Paxil) | 24 hours | 4. |
| sertraline (Zoloft) | 26 hours | 5.4 days |
| escitalopram (Lexapro) | 27 to 32 hours | 6.1 days |
| citalopram (Celexa) | 36 hours | 7.3 days |
| fluoxetine (Prozac) | Four to six days | 25 days |
| Serotonin and norepinephrine reuptake inhibitors | ||
| venlafaxine (Effexor) | 5 hours | 1 day |
| duloxetine (Cymbalta) | 12 hours | 2. |
| desvenlafaxine (Pristiq) | 12 hours | 2.5 days |
| Dopamine and norepinephrine reuptake inhibitor | ||
| bupropion (Wellbutrin) | 21 hours | 4.4 days |
| *Discontinuation symptoms typically start when 90% or more of the drug has left your system. Source: Adapted from Joseph Glenmullen, M.D., The Antidepressant Solution: A Step-by-Step Guide to Safely Overcoming Antidepressant Withdrawal, Dependence, and "Addiction" (Free Press, 2006). | ||
How to go off antidepressants
If you're thinking about stopping antidepressants, you should go step-by-step, and consider the following:
Take your time. You may be tempted to stop taking antidepressants as soon as your symptoms ease, but depression can return if you quit too soon. Clinicians generally recommend staying on the medication for six to nine months before considering going off antidepressants. If you've had three or more recurrences of depression, make that at least two years.
Talk to your clinician about the benefits and risks of antidepressants in your particular situation, and work with her or him in deciding whether (and when) to stop using them. Before discontinuing, you should feel confident that you're functioning well, that your life circumstances are stable, and that you can cope with any negative thoughts that might emerge. Don't try to quit while you're under stress or undergoing a significant change in your life, such as a new job or an illness.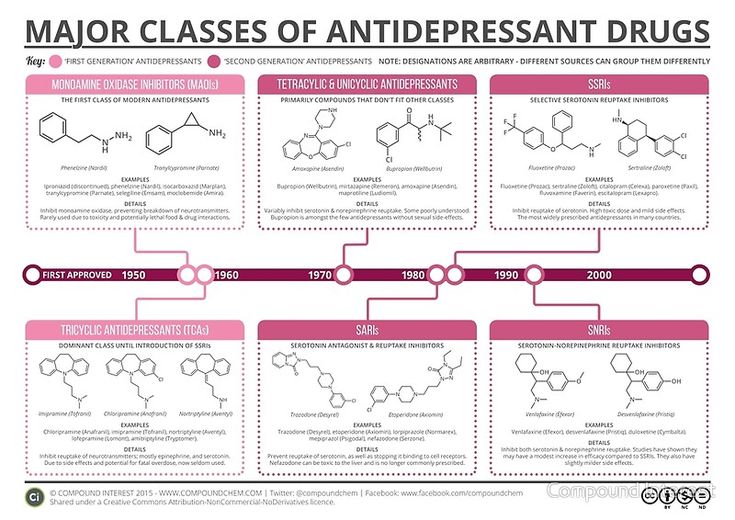
Make a plan. Going off an antidepressant usually involves reducing your dose in increments, allowing two to six weeks between dose reductions. Your clinician can instruct you in tapering your dose and prescribe the appropriate dosage pills for making the change. The schedule will depend on which antidepressant you're taking, how long you've been on it, your current dose, and any symptoms you had during previous medication changes. It's also a good idea to keep a "mood calendar" on which you record your mood (on a scale of one to 10) on a daily basis.
Consider psychotherapy. Fewer than 20% of people on antidepressants undergo psychotherapy, although it's often important in recovering from depression and avoiding recurrence. In a meta-analysis of controlled studies, investigators at Harvard Medical School and other universities found that people who undergo psychotherapy while discontinuing an antidepressant are less likely to have a relapse.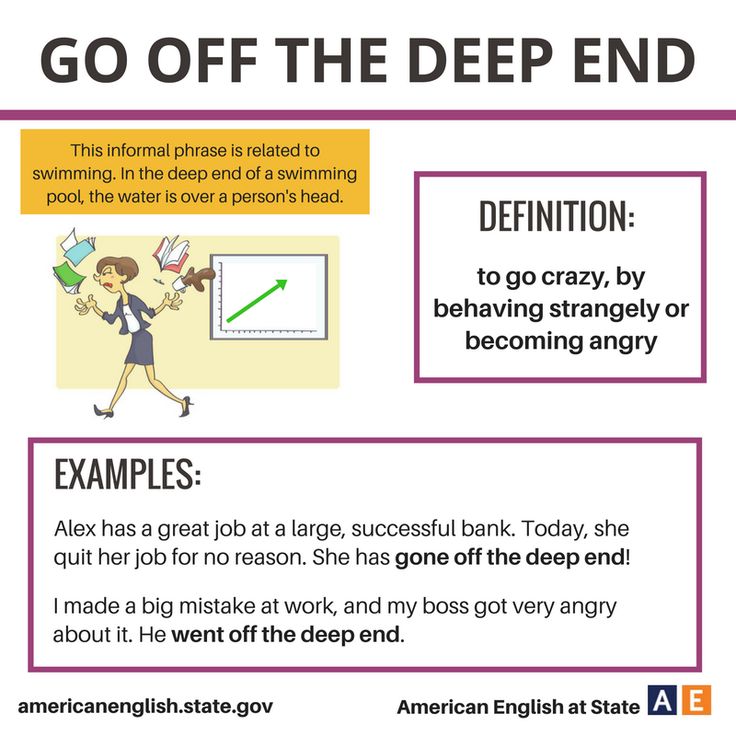
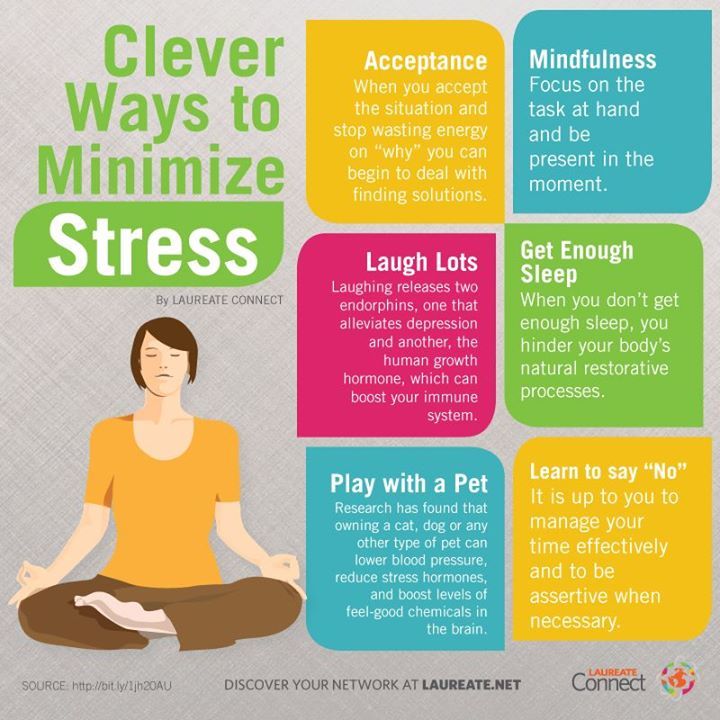
Stay active. Bolster your internal resources with good nutrition, stress-reduction techniques, regular sleep — and especially physical activity. Exercise has a powerful antidepressant effect. It's been shown that people are far less likely to relapse after recovering from depression if they exercise three times a week or more. Exercise makes serotonin more available for binding to receptor sites on nerve cells, so it can compensate for changes in serotonin levels as you taper off SSRIs and other medications that target the serotonin system.
Seek support. Stay in touch with your clinician as you go through the process. Let her or him know about any physical or emotional symptoms that could be related to discontinuation. If the symptoms are mild, you'll probably be reassured that they're just temporary, the result of the medication clearing your system. (A short course of a non-antidepressant medication such as an antihistamine, anti-anxiety medication, or sleeping aid can sometimes ease these symptoms. ) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
You may want to involve a relative or close friend in your planning. If people around you realize that you're discontinuing antidepressants and may occasionally be irritable or tearful, they'll be less likely to take it personally. A close friend or family member may also be able to recognize signs of recurring depression that you might not perceive.
Complete the taper. By the time you stop taking the medication, your dose will be tiny. (You may already have been cutting your pills in half or using a liquid formula to achieve progressively smaller doses.) Some psychiatrists prescribe a single 20-milligram tablet of fluoxetine the day after the last dose of a shorter-acting antidepressant in order to ease its final washout from the body, although this approach hasn't been tested in a clinical trial.
Check in with your clinician one month after you've stopped the medication altogether. At this follow-up appointment, she or he will check to make sure discontinuation symptoms have eased and there are no signs of returning depression. Ongoing monthly check-ins may be advised.
Image: AlinaTraut/Getty Images
Withdrawal From Antidepressants: Symptoms, Causes, Treatments
Written by Kelli Miller
In this Article
- What Causes Antidepressant Discontinuation Syndrome?
- Hardest-to-Stop Antidepressants
- Symptoms of Antidepressant Discontinuation
- How to Stop Antidepressants Safely
Your doctor prescribed an antidepressant to help boost your mood or ease your anxiety. But, as soon as you feel better, you might assume you no longer need the medicine. So you stop taking it.
And suddenly, you feel like you have the flu, or a stomach bug, or perhaps you find it hard to think and have disturbing thoughts.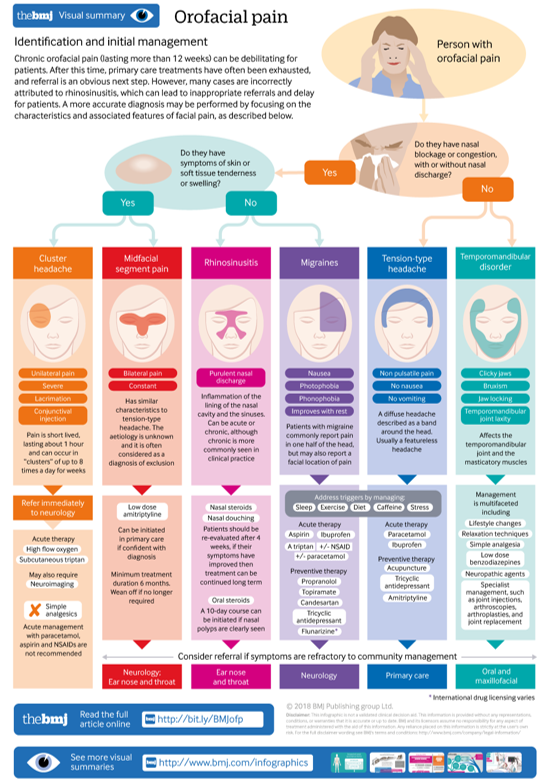
You’re probably having discontinuation symptoms.
When antidepressants that affect the brain chemical serotonin are suddenly stopped, the body may respond with physical and emotional symptoms caused by the sudden absence of increased serotonin levels that occur while taking the antidepressant. These symptoms are not technically the same thing as physical "withdrawal" from a drug. Physiological withdrawal happens when someone is taking a drug that can be addictive. This leads to craving and drug-seeking behavior. Antidepressants are not addictive or habit-forming. Unlike drug withdrawal, antidepressant discontinuation effects are not related to addiction but can reflect physiological consequences of stopping a drug, just as when someone with diabetes stops insulin. About one in five people who take an antidepressant for six or more weeks may experience discontinuation symptoms if they suddenly stop taking the medicine. Tapering down your medication gradually under the supervision of your health care provider can help avoid or minimize symptoms.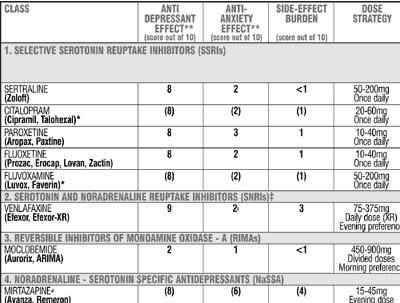 However, it is still possible in those who decrease their dose too rapidly or sometimes even slowly quit the medicine.
However, it is still possible in those who decrease their dose too rapidly or sometimes even slowly quit the medicine.
Your doctor may diagnose you with antidepressant discontinuation symptoms if:
- You suddenly develop symptoms days after stopping an antidepressant
- Symptoms rapidly go away when you start taking the antidepressant again
What Causes Antidepressant Discontinuation Syndrome?
There's no way to predict if you will have discontinuation symptoms after quitting an antidepressant. Scientists are not exactly sure why some people develop antidepressant discontinuation syndrome while others do not.
Antidepressants help restore the normal function of naturally occurring, mood-regulating substances in the brain, called neurotransmitters, including serotonin and norepinephrine. Some mental health experts theorize that abruptly stopping an antidepressant simply does not give your brain time to adjust to the rapid changes.
Hardest-to-Stop Antidepressants
All depression drugs can potentially lead to discontinuation symptoms, but some are much more likely to do so than others. In fact, antidepressant labels often warn that stopping the medication too quickly may lead to bothersome symptoms. However, discontinuation symptoms are more likely with antidepressants that stay in your body for a shorter period of time, especially those that affect both serotonin and norepinephrine, such as duloxetine (Cymbalta) and venlafaxine (Effexor). Other short-acting medications that affect mainly serotonin include:
In fact, antidepressant labels often warn that stopping the medication too quickly may lead to bothersome symptoms. However, discontinuation symptoms are more likely with antidepressants that stay in your body for a shorter period of time, especially those that affect both serotonin and norepinephrine, such as duloxetine (Cymbalta) and venlafaxine (Effexor). Other short-acting medications that affect mainly serotonin include:
- citalopram) (Celexa)
- escitalopram (Lexapro)
- paroxetine (Paxil)
- sertraline (Zoloft)
Withdrawal is less common with medications that take longer for the body to clear, such as fluoxetine (Prozac) or vortioxetine (Trintellix). However, longer-acting antidepressants can still sometimes cause discontinuation symptoms.
Discontinuation symptoms have also been reported in people who stop taking older types of antidepressant medications, including tricyclics and monoamine oxidase inhibitors (MAOIs).
Symptoms of Antidepressant Discontinuation
Symptoms of antidepressant withdrawal depend on the specific medication you have been taking.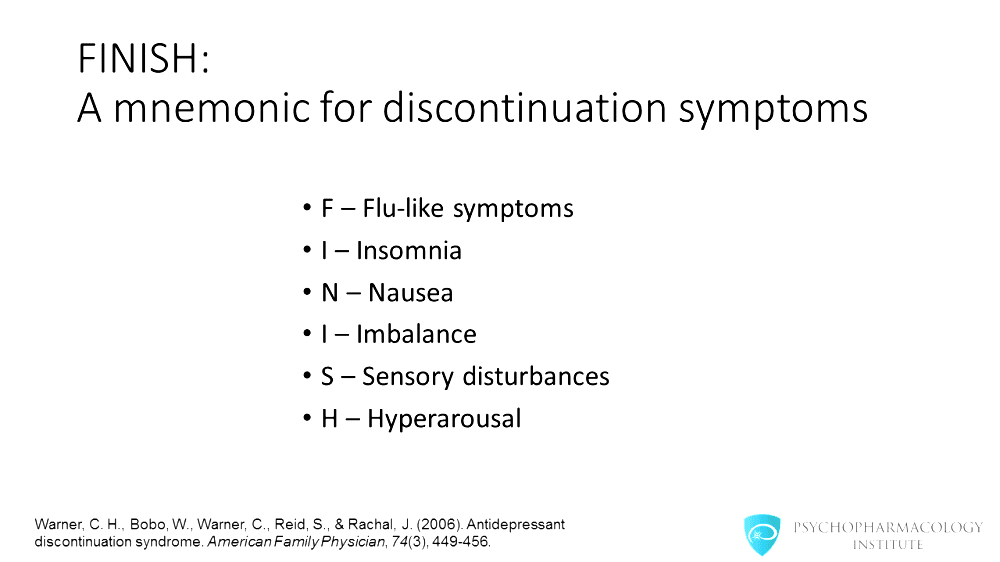
Symptoms most often occur within three days of stopping the antidepressant. TThere can be some differences in how people feel when they stop their medicine. Some people might have symptoms that are moderate to severe and may last longer than a few weeks. Symptoms can include:
- Anxiety
- Depression and mood swings
- Dizziness and balance problems, possibly vertigo
- Electric shock sensations
- Fatigue
- Flu-like symptoms
- Headache
- Loss of coordination
- Muscle spasms
- Nausea
- Nightmares
- Tremors
- Trouble sleeping
- Vomiting
In rare cases, antidepressant withdrawal may cause mania. Certain, older types of antidepressants called MAOIs can lead to confusion and psychotic symptoms.
How to Stop Antidepressants Safely
If you are thinking about stopping your antidepressant therapy, talk to your doctor to discuss the risks and benefits of discontinuing treatment. Never stop "cold turkey. " In many cases, the best way to stop taking most antidepressants is to slowly cut back your dose under the guidance of your doctor. This is called tapering. Tapering helps your brain adjust to the chemical changes and can help prevent discontinuation symptoms. Your doctor will tell you how to lower your dose over a couple of days. Never try to do this on your own.
" In many cases, the best way to stop taking most antidepressants is to slowly cut back your dose under the guidance of your doctor. This is called tapering. Tapering helps your brain adjust to the chemical changes and can help prevent discontinuation symptoms. Your doctor will tell you how to lower your dose over a couple of days. Never try to do this on your own.
Sometimes, doctors can prescribe medicines to help with discontinuation symptoms such as nausea or insomnia. They also may advise switching from a short- to a long-acting antidepressant to ease the transition off of a medicine for depression.
Discontinuation symptoms usually go away within a few weeks. But if you have extremely severe withdrawal symptoms, your doctor may recommend other medicines to relieve them.
Next Article
Depression and SuicideDepression Guide
- Overview & Causes
- Symptoms & Types
- Diagnosis & Treatment
- Recovering & Managing
- Finding Help
Long-term use of antidepressants is associated with an increased risk of coronary artery disease, cerebrovascular disease, cardiovascular and overall mortality, but a reduced risk of hypertension and diabetes mellitus: a large observational study
is 6 months, with a continuing risk of recurrence - 2 years. Very often, patients continue to take drugs for years. nine0003
Very often, patients continue to take drugs for years. nine0003 It is known that depression is associated with an increase in the frequency of CVD risk factors (smoking, obesity, physical inactivity) and so on. In this situation, it is very difficult in an observational study to assess the safety profile of antidepressants in terms of cardiovascular complications and overall mortality: it is not entirely clear which will have an adverse effect - antidepressants or depression itself. Therefore, the bulk of research on this topic, as a rule, causes a lot of comments. nine0003
The British Journal of Psychiatry Open published the results of an analysis of the UK Biobank registry, the design of which claims to account for the maximum number of associated risk factors, including behavioral and socioeconomic. This is supposed to help separate the effects of antidepressants and depression itself. The study included patients who initially did not suffer from CVD, did not take cardiometabolic drugs, and did not use antidepressants during the last 12 months before inclusion. Of the 222,121 participants included, 8% were taking antidepressants at 5 years and 6% at 10 years. Serotonin reuptake inhibitors and other antidepressants were analyzed separately (amitriptyline was excluded from the analysis as low doses are often prescribed in older patients for insomnia). nine0003
Of the 222,121 participants included, 8% were taking antidepressants at 5 years and 6% at 10 years. Serotonin reuptake inhibitors and other antidepressants were analyzed separately (amitriptyline was excluded from the analysis as low doses are often prescribed in older patients for insomnia). nine0003
Multivariate analysis taking into account a large number of risk factors showed that long-term use of serotonin reuptake inhibitors is associated with an increased risk of cerebrovascular disease (OR 1.34, 95% CI 1.02–1.77), cardiovascular mortality (OR 1.87, 95% CI 1.38–2.53) and death from all causes (OR 1.73, 1.48–2.03) after 10 years. For other antidepressants, similar patterns are revealed, but the odds ratios are higher: the OR for CHD is 1.99 (1.31–3.01), for cardiovascular death - 1.86 (1.10–3.15), for death from all causes - 2.2 (1.71–2.84). A relationship was found between doses of drugs and the risk of complications. Whether there is a causal relationship between antidepressants and increased mortality remains unclear. Of particular concern is the fact that the use of serotonin reuptake inhibitors is associated with a reduced risk of developing the main risk factors for CVD - diabetes (OR 0.68.95% CI 0.53–0.87) and hypertension (OR 0.77, 95% CI 0.66–0.89) at 10 years of follow-up. However, such a relationship is potentially possible, therefore, antidepressants should not be taken longer than necessary, it is advisable to use the minimum effective doses, and actively engage in screening and correction of other CVD risk factors in such patients.
Of particular concern is the fact that the use of serotonin reuptake inhibitors is associated with a reduced risk of developing the main risk factors for CVD - diabetes (OR 0.68.95% CI 0.53–0.87) and hypertension (OR 0.77, 95% CI 0.66–0.89) at 10 years of follow-up. However, such a relationship is potentially possible, therefore, antidepressants should not be taken longer than necessary, it is advisable to use the minimum effective doses, and actively engage in screening and correction of other CVD risk factors in such patients.
Adapted from:
Bansal, N., Hudda, M., Payne, R., Smith, D., Kessler, D., & Wiles, N. (2022). Antidepressant use and risk of adverse outcomes: Population-based cohort study. BJPsych Open, 8(5), E164. doi:10.1192/bjo.2022.563
https://www.cambridge.org/
Text: Shakhmatova O.O.
I'm back on antidepressants and happy about it!
#2
No_fears
Often I hear "you have to manage on your own", learn to meditate, to relax. and so on and so forth.
and so on and so forth.
#3
#4
#5
#6
19:49
#8
#9,0003
#10
Guest
I sit on the Afobazole of the Walse forte, etc. I have a nervous life. It's probably not hell, but it's a start. I would drink something stronger, but I can’t buy it without a prescription, but I really want to live calmly and joyfully. nine0003
It's probably not hell, but it's a start. I would drink something stronger, but I can’t buy it without a prescription, but I really want to live calmly and joyfully. nine0003
#11
#12
Guest
I also want to live calmly and joyfully, and these aphobosols, Tenotenes do not help much
#13
Guest
The only thing that helped me get rid of attacks was that I began to help those in need. When I saw how lonely old people eked out an existence in shitty apartments, how animals suffer .... I will not describe all the horrors, but in short - now I am responsible for them, I just have NO TIME to relax, run around psychiatrists-psychologists-girlfriends and feel sorry for myself too once. After that, the depression, and the attacks, and the blues, and others like them, went away. nine0003
After that, the depression, and the attacks, and the blues, and others like them, went away. nine0003
#14
#15
#16
Guest
22222 Dear author, well, where do you still have children? You can’t cope with yourself, where can you raise and educate others. In addition, imagine, you become pregnant, there is a hormonal restructuring of the body. Even healthy people can hardly bear it. Hormonal restructuring + return of the state that was before the drug was discontinued + withdrawal from withdrawal. And pregnancy should be calm, then there is a chance to give birth + a chance to give birth to a healthy one. It is terrible to imagine what malformations your child may have. You at least honestly tell your soulmate about your defects. On the forums, everyone is brave, but in real life, people are then surprised. We met with a healthy, calm girl, and during pregnancy or after childbirth, the girl went nuts. nine0003
You at least honestly tell your soulmate about your defects. On the forums, everyone is brave, but in real life, people are then surprised. We met with a healthy, calm girl, and during pregnancy or after childbirth, the girl went nuts. nine0003
#17
#18
You can’t cope with yourself, where can you raise and educate others. In addition, imagine, you become pregnant, there is a hormonal restructuring of the body. Even healthy people can hardly bear it. Hormonal restructuring + return of the state that was before the drug was discontinued + withdrawal from withdrawal. And pregnancy should be calm, then there is a chance to give birth + a chance to give birth to a healthy one. It is terrible to imagine what malformations your child may have. You at least honestly tell your soulmate about your defects. On the forums, everyone is brave, but in real life, people are then surprised. We met with a healthy, calm girl, and during pregnancy or after childbirth, the girl went nuts. nine0003
On the forums, everyone is brave, but in real life, people are then surprised. We met with a healthy, calm girl, and during pregnancy or after childbirth, the girl went nuts. nine0003
#19
No_fears
I have no secrets from my husband. And what, never give birth now because of panic attacks?
#20
#21
#22
#23
Lena
Don't talk nonsense, you need to stop the drugs and then give birth well. All doctors say
All doctors say
Woman.ru experts
-
Elena Gerba
family psychologist
62 answers
-
Maxim Sorokin
Practicing psychologist
890 answers
nine0196 -
Galimov Ildar
Family psychologist
273 answers
-
Ivanova Svetlana
Coach
59 answers
nine0196 -
Osipova Ksenia Andreevna
Psychologist
34 answers
-
Anna Antonchik
Female psychologist
122 answers
nine0196 -
Vladimir Titarenko
Fitness nutritionist
52 answers
-
Maria Sinyapkina
Psychologist-Sexologist
72 answers
nine0196 -
Kremenetskaya Maria
Speech therapist - defectologist
17 answers
-
Nikitina Anna Viktorovna
Specialist of Oriental practitioners
32 answers
nine0196
#24
Guest
Don't be stupid yourself. "All doctors say" this is from the series "One grandmother said." Links to studies are great. But you can consult a gynecologist on the topic of exacerbation of chronic diseases during pregnancy, childbirth and after. And mental illness during these periods bloom in red. Today she gave birth, tomorrow she stepped out of the window due to acute depression or a panic fear of children's sores, poop, crying (underline as necessary). And this is not the worst option for a child. How do you like a woman shaking in the pantry with fear, frightened by a pediatrician ringing the doorbell, and a baby screaming before her husband arrives or faints. Or the mother was frightened by a strange sound from the street, they sit at the table for half a day and do not feed the child, not to mention the fact that the child needs to play and walk. Here you can cripple a healthy child. And there is always a risk to give birth to the same depressive everything that is afraid. Manifestations of the disease are both early and adolescent, in adulthood.
"All doctors say" this is from the series "One grandmother said." Links to studies are great. But you can consult a gynecologist on the topic of exacerbation of chronic diseases during pregnancy, childbirth and after. And mental illness during these periods bloom in red. Today she gave birth, tomorrow she stepped out of the window due to acute depression or a panic fear of children's sores, poop, crying (underline as necessary). And this is not the worst option for a child. How do you like a woman shaking in the pantry with fear, frightened by a pediatrician ringing the doorbell, and a baby screaming before her husband arrives or faints. Or the mother was frightened by a strange sound from the street, they sit at the table for half a day and do not feed the child, not to mention the fact that the child needs to play and walk. Here you can cripple a healthy child. And there is always a risk to give birth to the same depressive everything that is afraid. Manifestations of the disease are both early and adolescent, in adulthood.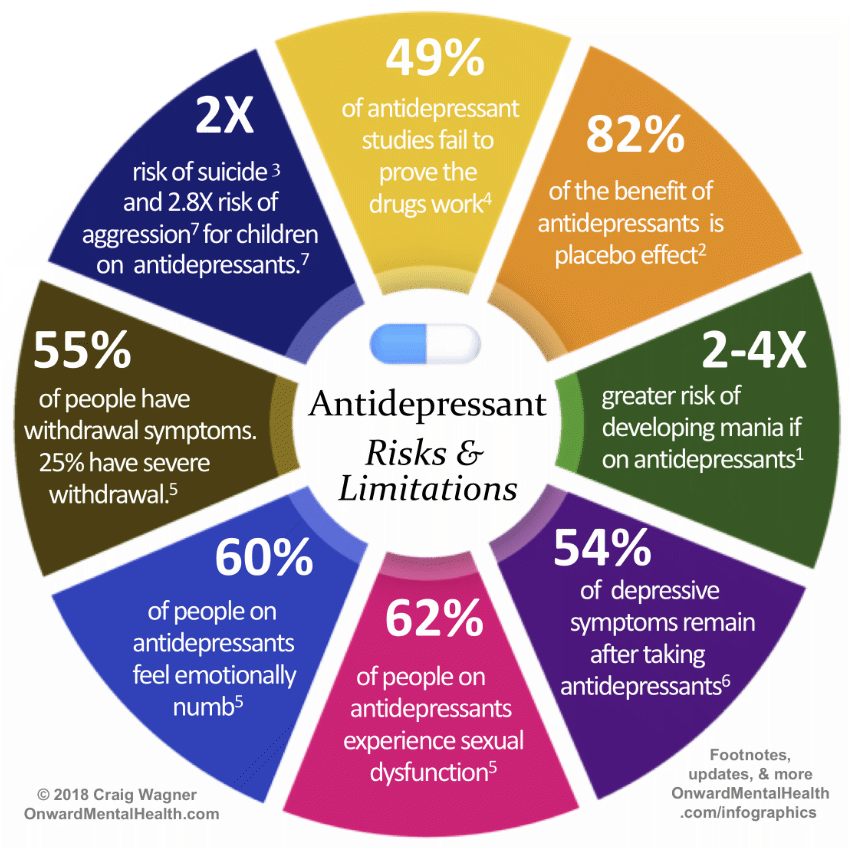 Give birth to torment? But in any case, this is the choice of the author and her problems. I can only advise to go through as many different doctors as possible and collect opinions. And if it's scary to go to the doctors, then why have a child. You can't give birth on antidepressants. nine0003
Give birth to torment? But in any case, this is the choice of the author and her problems. I can only advise to go through as many different doctors as possible and collect opinions. And if it's scary to go to the doctors, then why have a child. You can't give birth on antidepressants. nine0003
#25
Guest
I am sitting on afobazole motherwort-forte, etc. I have a nervous life. It's probably not hell, but it's a start. I would drink something stronger, but I can’t buy it without a prescription, but I really want to live calmly and joyfully.
#26
No_fears
It's just that sometimes I start to twitch like that, my heart beats and my mood is completely zero, that it's easier for me to live on a small dose of medicine. until I decide to have children, I'm going to drink hell. Because only they really help, and not all these psychotechnics and psychotherapists, whom I have replaced more than ten in 10 years. nine0003
Because only they really help, and not all these psychotechnics and psychotherapists, whom I have replaced more than ten in 10 years. nine0003
#27
Unreliable stories
-
I am infuriated with my children and grandchildren ...
1 002 Answer
-
Men Immediately warned. that all property is registered to children
818 answers
-
Such a salary - I don’t want to work
557 answers
-
2 years long lie. How to destroy? nine0312
822 answers
-
Husband left, 2 months of depression... How will you cope if you are left all alone?
184 answers
#28
Faith
My mom has been taking hell since she was 30.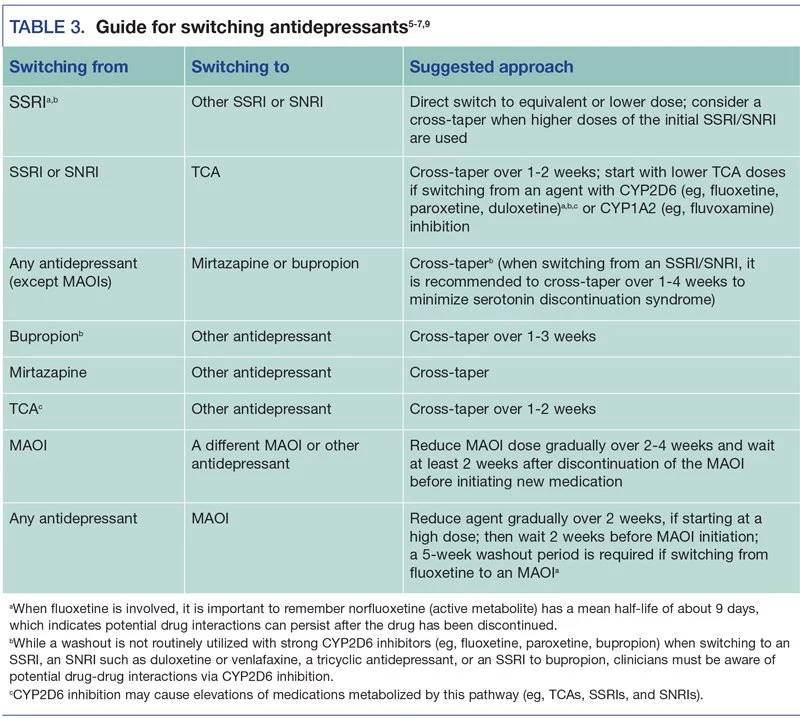 Now she is 56, looks great, is actively involved in sports, very cheerful. But when she did not take them, it was a nightmare for her and for my dad and I, I was a child at that time and I still remember those terrible panic attacks. It is clear that constant medication is bad, but without it it is even worse. nine0003
Now she is 56, looks great, is actively involved in sports, very cheerful. But when she did not take them, it was a nightmare for her and for my dad and I, I was a child at that time and I still remember those terrible panic attacks. It is clear that constant medication is bad, but without it it is even worse. nine0003
#29
Guest
Please write the name of the drug!
#30
#31
#32 9000 9000
#33
#34
#35
kicks
When you stop taking them, the roof can go very hard. This is the biggest danger of drugs such as hell, you must say with a doctor
This is the biggest danger of drugs such as hell, you must say with a doctor
#36
#37
Gost
not you want to work on yourself)) it's hard, it's much easier to take a pill)) In this case, even a first-class psychotherapist will not help. From a long problem hell and neuroleptics such side effects, even endure the saints 9
#38
Faith
My mom has been taking hell since she was 30. Now she is 56, looks great, is actively involved in sports, very cheerful. But when she did not take them, it was a nightmare for her and for my dad and I, I was a child at that time and I still remember those terrible panic attacks. It is clear that constant medication is bad, but without it it is even worse.
It is clear that constant medication is bad, but without it it is even worse.
#39
Guest
my co-worker drank a lot of drugs and his kidneys failed. author, do not get carried away with chemistry, the kidneys and liver will fail!
#40
Guest
my co-worker drank a lot of drugs and his kidneys failed. author, do not get carried away with chemistry, the kidneys and liver will fail! March 22, 2016 nine0003
#42
Guest
This aunt is sick, but wants to be fruitful. No need to spray your genes.
#43
No_fears
I only drink paxil at the minimum dosage. March 22, 2016, 11:58
March 22, 2016, 11:58
#44
#45
Why did you decide to write here Guest
You don't need to prove anything. People who have not encountered such a state simply do not know how hard it is for you, but they always want to be smart. Don't listen to those. Do as you see fit. Just be careful and see what side effects can be from long-term use of drugs. nineonly So you say that paroxetine is a vitamin. What dosage do you drink? How long have you been drinking? Have you tried to get off it?Attention
#48
Guest
Author, why did you decide to write here? You don't need to prove anything. People who have not encountered such a state simply do not know how hard it is for you, but they always want to be smart.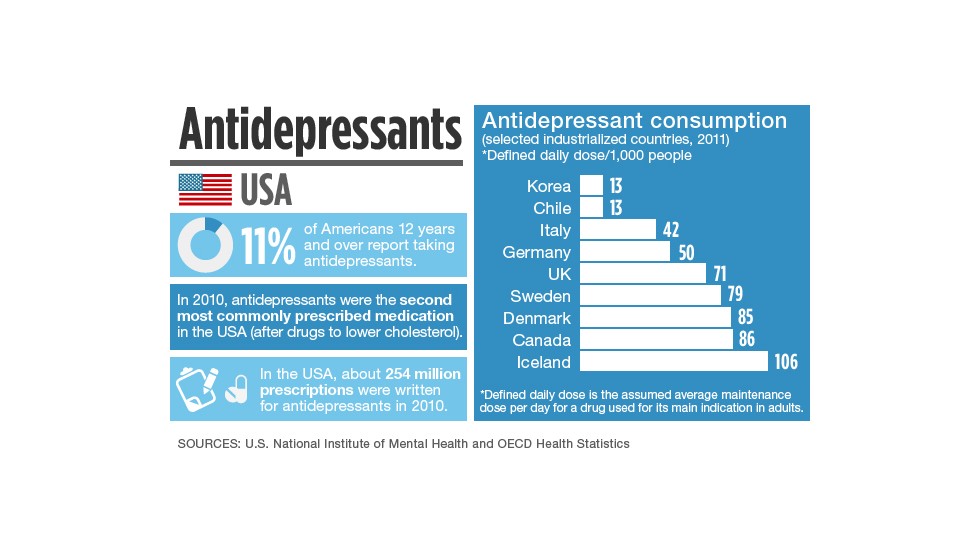
 Here's how to distinguish discontinuation symptoms from relapse:
Here's how to distinguish discontinuation symptoms from relapse: 4 days
4 days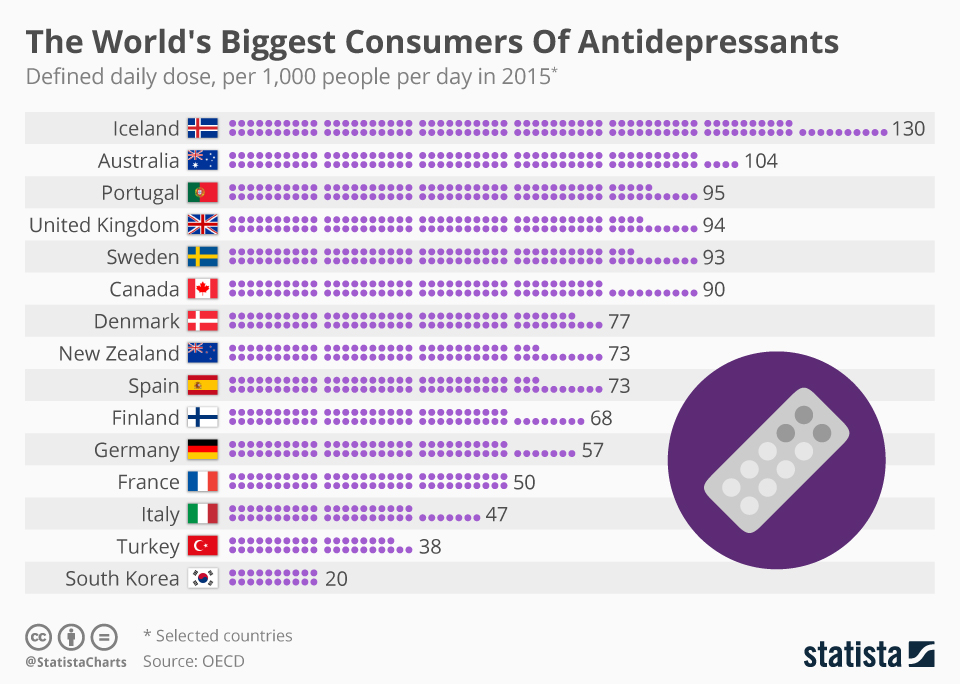 5 days
5 days