Excessive worrying ocd
Is Your Chronic Worrying a Sign of Obsessive Compulsive Disorder?
Everybody worries from time to time, but some people seem to have a Ph.D. in worrying. Are you one of them? Do you spend your days (and nights) ruminating over every little thing you might have done wrong or that might go wrong in the future? Worried about the germs on every surface you touch? Worried that you should have changed that one PowerPoint slide on that big project at work? Worried that your child might get sick? Or even worse, worried that you might in some way put your child in harm’s way?
Ruminating about things you can’t control or fixating on fears of what might happen isn’t healthy. But is it normal? When worrying becomes chronic and intrusive thoughts become distressing, it can be a sign of a mental health condition that is often underrecognized and undertreated—obsessive compulsive disorder (OCD).
Why OCD is So MisunderstoodMany people know that OCD can involve repetitive rituals, such as excessive hand washing, checking and re-checking that the door is locked, or extreme cleaning. What people don’t understand is that these compulsions are typically a way for people to deal with unwanted thoughts and worries that loop in the brain. And you don’t have to have physical rituals to have OCD. Some people with the condition develop mental rituals—such as praying, counting, or saying words silently to oneself—to cope with their worries.
If you’re one of the 1 in 40 adults affected by OCD or if your child is one of the 1 in 200 kids who have it, you may have repetitive thoughts and worries about:
- Germs
- Contamination
- Disease
- Fear of making mistakes
- Fear of making the wrong decision
- Forbidden sexuality
- Harming someone
- Losing control
- Religion
- A need for symmetry
- A need for things to be “perfect”
- Superstitions or fears about “bad” numbers or colors
These unwanted worries can trigger distressing feelings of anxiety or disgust. People with OCD often make a great effort to suppress or resist these intrusive thoughts and worries, but the more a person tries to control them, the more powerful they become.
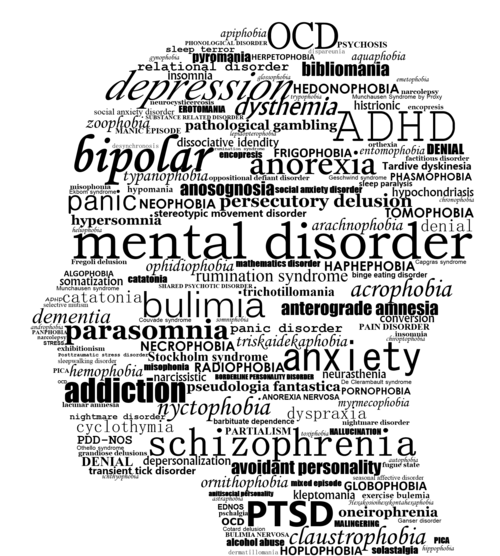
Many mental health conditions can be misdiagnosed, but OCD is one of the most likely to be mistaken for other conditions because it involves so many overlapping symptoms. In fact, a 2015 study among primary care physicians found that half of OCD cases were misdiagnosed. And other research on the diagnosis and management of OCD reported that it takes an average of 11 years to receive treatment after meeting the diagnostic criteria for OCD.
OCD can be misdiagnosed as:
ADD/ADHD: People with ADD/ADHD tend to struggle focus and attention and often don’t complete tasks. People with OCD may also have trouble finishing projects, but it’s due to a need for everything to be perfect, and if things aren’t just right they don’t complete it.
Anxiety: Like people with OCD, those with anxiety may be filled with anxious thoughts and worries. The difference is that people with anxiety tend to worry about real-life concerns while those with OCD may have irrational thoughts and worries.
Autism spectrum disorder (ASD): People with autism may display repetitive behaviors, which can mimic some of the ritualistic patterns seen in people with OCD.
Mood disorders: In depression, people have many negative thought patterns that are also common in those with OCD.
Posttraumatic stress disorder (PTSD): People with PTSD often make an effort to avoid places that bring up memories of traumatic events, while those with OCD may use avoidance to minimize the risk of triggering unwanted worries.
Psychosis or schizophrenia: These disorders are characterized by delusions. People with OCD may have irrational fears that can be mistaken for delusions. The difference is that people with OCD typically recognize that their worries are unfounded but are unable to control them, whereas those with psychosis or schizophrenia believe their delusions.
Tourette syndrome: Involuntary vocal or motor tics are the hallmarks of this condition. Some of the repetitive rituals common in people with OCD may be mistaken for Tourette.
Brain imaging studies show that the chronic worrying associated with OCD isn’t a mental health problem, but rather a brain health issue. Brain scans using SPECT imaging technology reveal abnormalities in the brains of people with OCD. In particular, SPECT scans show increased blood flow in two regions of the brain—the basal ganglia and anterior cingulate gyrus.
- Basal ganglia: This region helps set the body’s anxiety level and is involved in forming habits. When there is too much activity in the basal ganglia, it is associated with increased anxiety and heightened fear.
- Anterior cingulate gyrus (ACG): This area is involved in allowing people to shift attention from subject to subject. When the ACG is overactive, people tend to get “stuck” on the same thought or behavior.
- Low serotonin:
Low levels of the neurotransmitter serotonin are often seen in people with an overactive ACG and in people with OCD.
You can overcome chronic worrying and OCD. It starts by calming the areas of the brain that are overactive. To see some strategies you can use, read this blog on 5 simple things you can do if you have OCD.
At Amen Clinics, we take a whole-body approach to helping people overcome symptoms of chronic worrying and OCD. We perform comprehensive evaluations that include brain SPECT imaging to make an accurate diagnosis so you can get the right treatment plan for your needs. We believe in using the least toxic, most effective solutions, including helpful forms of therapy, nutritional supplements, and lifestyle changes, as well as medications when necessary.
If you want to join the tens of thousands of people who have already enhanced their brain health, overcome their symptoms, and improved their quality of life at Amen Clinics, speak to a specialist today at 888-288-9834. If all our specialists are busy helping others, you can also schedule a time to talk.
GAD or OCD What Do I Have & What's The Difference? NOCD
Anxiety is worry, nervousness or unease about something that’s on your mind. Everyone worries or feels anxiety at some point in their lives — students on exam day, brides on their wedding day or professionals who sit for a coveted job interview. These temporary anxieties are a usual part of life.
Usual vs. Unusual WorryBut not all anxieties are created equal. Sometimes usual worry becomes unusual, or unmanageable. When the worry you experience is excessive, results in behaviors designed to control anxiety or is irrational, it might be that you are coping with an anxiety disorder. Anxiety disorders are the most diagnosed mental health condition in the United States and affect 18% of adults in America each year. One such anxiety-related condition is generalized anxiety disorder, or GAD for short.
What Is
Generalized Anxiety Disorder?Generalized anxiety disorder is excessive worry about multiple life-events or activities that is hard to manage and results in physical symptoms.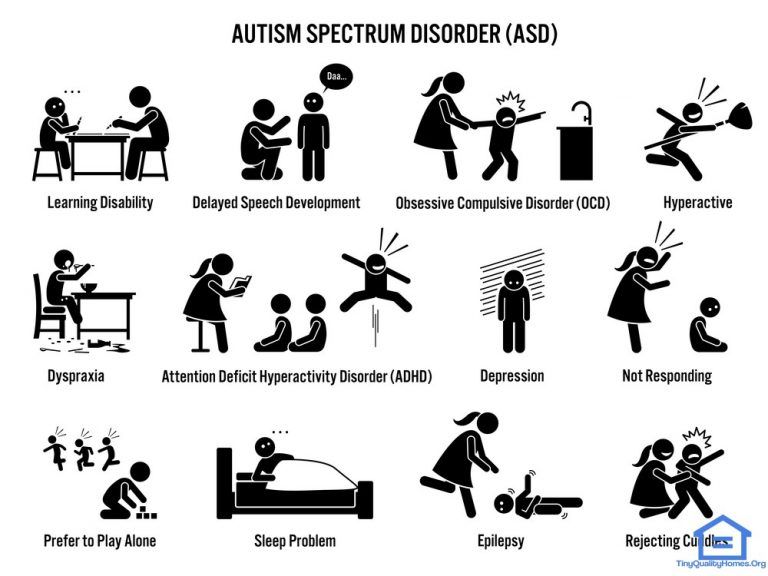 In 2019, GAD was found to affect 1 in 6 adults in the United States.
In 2019, GAD was found to affect 1 in 6 adults in the United States.
Symptoms of GAD include:
- Excessive worry that is accompanied by physical symptoms
- Restlessness
- Fatigue
- Difficulty concentrating
- Irritability
- Muscle tension
- Sleep problems
Think of GAD as a constant state of feeling apprehensive about something. Maybe you have a performance review at work in two months, and you worry constantly about the results. Perhaps your child is graduating from high school this year, and you worry about what will happen after graduation.
People with GAD worry about many things such as finances, work-related events or activities, family life, health concerns, or other issues. These worries are typically associated with at least three physical symptoms. There is no known cause for GAD, however some research suggests that environment, genetics and biology all play a role in the development of the condition.
GAD is usually diagnosed by a mental health professional, but can also be diagnosed by your general physician.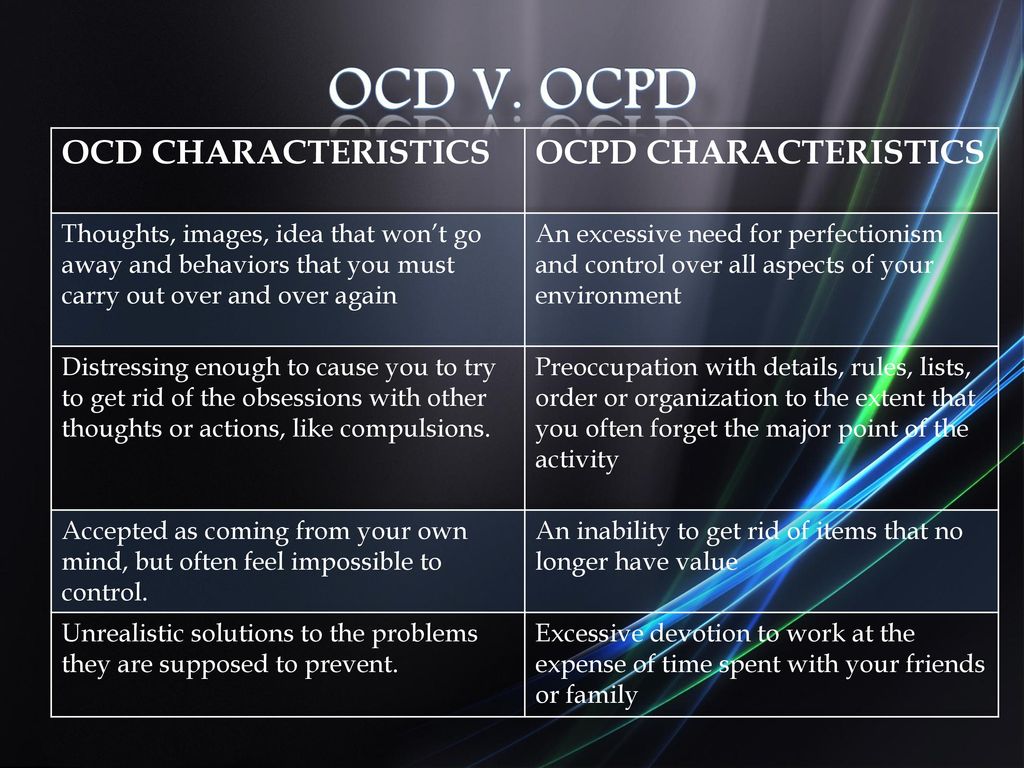 The condition is treatable with evidence-based psychotherapies and medication.
The condition is treatable with evidence-based psychotherapies and medication.
People who live with obsessive-compulsive disorder (OCD), also a prevalent mental health condition in the U.S., wrestle with intrusive thoughts and intense feelings of fear, doubt and anxiety. Sounds like GAD, right? Sure. The symptoms of the two conditions can be difficult to distinguish, but there are differences.
It might even surprise you to learn that OCD is not considered an anxiety disorder, even though the symptoms of OCD often include anxiety and other symptoms of GAD. Let’s check out how these conditions differ and why OCD is in a class of its own.
What Is
Obsessive-Compulsive Disorder?OCD is a mental health condition characterized by persistent and unwanted thoughts, images, urges or doubts (obsessions) that result in significant distress and repetitive behaviors, or rituals (compulsions), to control the distress.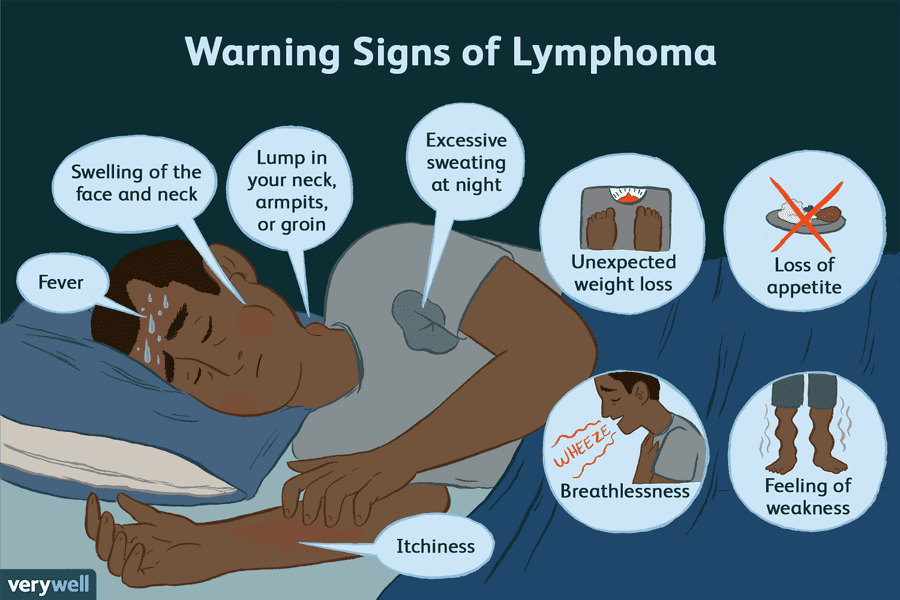 These repetitive actions could be physical behaviors or mental actions that are engaged repeatedly to cope with distressing thoughts. While most people have both obsessions and compulsions, it is possible to only have obsessive symptoms without compulsive symptoms.
These repetitive actions could be physical behaviors or mental actions that are engaged repeatedly to cope with distressing thoughts. While most people have both obsessions and compulsions, it is possible to only have obsessive symptoms without compulsive symptoms.
Symptoms of OCD include:
- Persistent unwanted thoughts, images and urges
- Attempts to control the thoughts with rituals
- Intrusive (unwanted and come out of nowhere) thoughts
- Time spent each day avoiding or preventing thoughts, images, or urges
- Thoughts, images, or urges are patterned around, or fixated on, a particular fear that does not align with who you are or what you know about yourself or the world
OCD can only be diagnosed by a mental health professional. The most effective treatment for OCD is exposure and response prevention (ERP) therapy, however other forms of cognitive behavioral therapy (CBT) and medications are also used in the treatment of OCD.
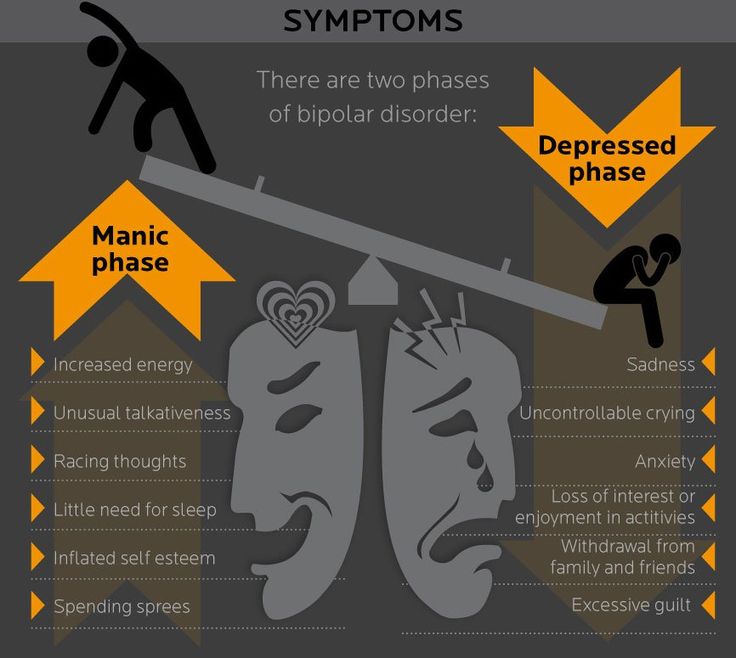
OCD was historically conceptualized as an anxiety disorder because of the intense anxiety or fear associated with the symptoms of OCD.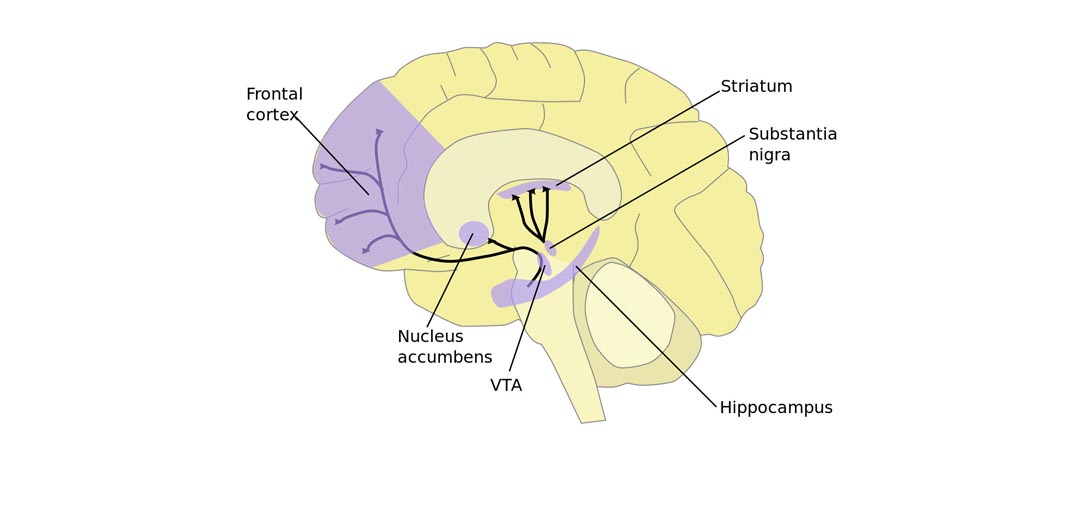 However, in 2013 the American Psychiatric Association removed OCD from the anxiety disorders classification and assigned a unique classification to OCD.
However, in 2013 the American Psychiatric Association removed OCD from the anxiety disorders classification and assigned a unique classification to OCD.
The change was made to emphasize distinctions in brain chemistry and function in those with OCD and related disorders, as compared to those with anxiety disorders. Areas of the brain that reveal abnormal results in studies, and that respond when anxious feelings are triggered, are different in those with OCD than in those with anxiety disorders such as GAD. These differences are important to understanding and treating both conditions effectively.
Both OCD and GAD are long-lasting, and both involve excessive anxiety, rumination and intrusive thoughts. It can be difficult to figure out which you might be experiencing. While it is possible for people who have been diagnosed with OCD to also have GAD, let’s check out the key differences in symptoms:
OCD:
- Obsessive (unwanted, persistent and repeated) thoughts, images, urges, and doubts
- Attempt to control/remove anxiety with rituals
- Attempts to suppress, neutralize or replace thoughts
- Unrealistic/hypothetical uncertainty
- Control anxiety with behaviors that are irrational or illogical
- Does not align with values or self-perception
- A single fixation (theme) is not necessarily associated with physical symptoms
GAD:
- Thoughts or images
- Worrisome (a train of thought that is an attempt to problem-solve)
- No rituals
- Attempts to examine thoughts
- Worry over more than one realistic negative outcome
- Multiple areas of focus, life areas or activities
- Accompanied by at least three physical symptoms
As you can see from above, the presence of obsessions and compulsions (not just worry) are a key distinction of OCD. Repetitive or ritualized behavior (compulsions) is not present in GAD or other anxiety-related conditions. Other key distinctions are that anxiety that is due to GAD is accompanied by physical symptoms, whereas physical symptoms are not often reported in those who experience OCD alone.
Repetitive or ritualized behavior (compulsions) is not present in GAD or other anxiety-related conditions. Other key distinctions are that anxiety that is due to GAD is accompanied by physical symptoms, whereas physical symptoms are not often reported in those who experience OCD alone.
The primary feature of OCD is the presence of obsessions and compulsions (repetitive behaviors or mental actions aimed at relieving distress), so if you identify with these descriptions — even if you have been diagnosed with GAD — it is possible that you have OCD.
After reading the comparisons between OCD and GAD, you might identify with the symptoms of OCD. If that is the case, there are a few steps you can take to find out for sure:
- Talk about your concerns with someone you trust: Sometimes the content of intrusive thoughts can feel scary, embarrassing or even shameful. That can make it difficult to reach out for help.
 A good starting place is to find someone in your life who you trust to share those concerns with. Perhaps it is a parent, a close friend or a partner, or maybe it’s a member of your local community. The first step to getting help is getting around people who support your efforts.
A good starting place is to find someone in your life who you trust to share those concerns with. Perhaps it is a parent, a close friend or a partner, or maybe it’s a member of your local community. The first step to getting help is getting around people who support your efforts. - Get connected with an OCD specialist for assessment: OCD specialists are expertly trained in the assessment, diagnosis and treatment of OCD. Some even have additional expertise in treating conditions related to OCD, such as trichotillomania, hoarding or excoriation. On the day of your appointment, your specialist will gather brief information about any relevant medical history, past therapy or other diagnoses you might have, and your family and social life. Then they will offer you a chance to share your experience with anxiety and fear, and about how your symptoms have been impacting your life. Assessment sessions can take anywhere from 45 to 90 minutes, and at the end of it, they will tell you if you meet the diagnostic criteria for OCD and offer you resources for getting treatment.
Just as not all anxiety is created equal, neither are all OCD therapies. Now that you have a diagnosis for OCD, finding the right therapy is crucial. Exposure and Response Prevention (ERP) is considered the front-line treatment for OCD and is regarded as the most effective treatment for the condition. Research has found that people with OCD do not experience significant relief with talk therapy, medication alone, or traditional behavior-based therapies such as aversion therapy or systematic desensitization—this means that the therapist you choose must specialize in ERP.
ERP is a form of CBT that teaches you to allow those scary and intrusive thoughts to enter your mind and those anxious feelings to emerge, while refraining from doing something to make the anxiety or discomfort go away. Your specialist will help you to face the fears you feel — safely, in a structured and gradual way — while not giving in to the urge to try to make those feelings or thoughts go away through compulsions.
If this sounds scary to you, don’t fret! You can always begin with CBT without doing ERP right away. CBT helps you identify patterns of thought that create anxiety, or amplify it, and adapt them so that, over time, those anxieties lessen. The CBT therapist can help you to think about yourself, the world (and the things you obsess about) in more healthful ways.
Where to find an OCD specialist:- NOCD: Our staff is clinically trained to treat obsessive-compulsive disorder by using the gold standard in OCD treatment: ERP. A 15 minute phone call with our staff can explain to you the benefits and the amazing results we’ve seen as a result of ERP therapy.
- International OCD Foundation: The IOCDF is a great resource if you are looking for help in your area. The website offers a resource directory that you can search based on your city, state or treatment interest (e.g., community group, in-person, virtual).
 Their directory includes providers who have been trained by the IOCDF in the specialized treatment of OCD.
Their directory includes providers who have been trained by the IOCDF in the specialized treatment of OCD. - Psychology Today: Well-known as a source for finding a therapist, this might be a good place to find a provider for OCD. The “Find a Therapist” feature is highly customizable, so you will have better luck finding a therapist who is the right fit.
If you or someone you know is struggling with OCD, you can schedule a free call today with the NOCD clinical team to learn more about how a licensed therapist can help. At NOCD, all therapists specialize in OCD and receive ERP-specific training. ERP is most effective when the therapist conducting the treatment has experience with OCD and training in ERP.
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance.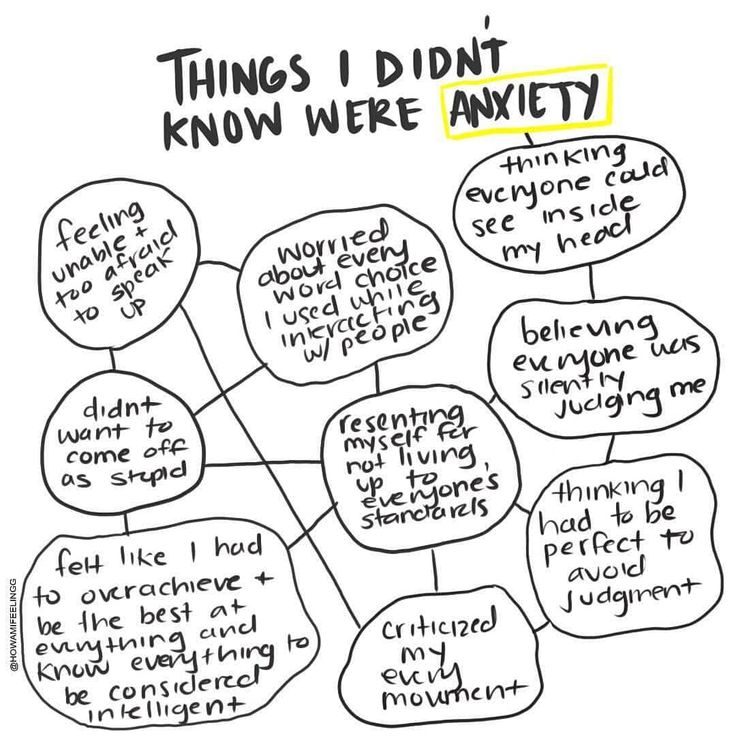 Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.

- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, rapid heartbeat, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gaining self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Rakhmanov Vladimir Alexandrovich
Psychiatrist, CBT-, ACT- and CFT-psychotherapist.
in the clinic online
Adults (over 18 years old) Elderly (from 60 years old)
Scientific approach. Horizon.
Founder and CEO of the Neuro-Psi network. Psychiatrist and psychotherapist.
As a psychiatrist, Vladimir works strictly in the evidence-based approach (Evidence-based Medicine). As a psychotherapist uses modern "rational" methods of psychotherapy (CBT, ACT, CFT, Schematherapy)
Vladimir is distinguished by a broad clinical outlook, professional awareness, and a comprehensive understanding of the patient's problem. These qualities are especially important in dealing with complex cases.
Vladimir specializes in working with the following client problems: professional burnout, depressed mood, excessive anxiety, despondency, indecision, regret about missed opportunities, intolerance for uncertainty, loss of meaning and direction in life. Chronic pain, psychosomatic and somatopsychic diseases. Isolation, avoidance of difficulties, loneliness. Does not work with suicidal behavior, addictions of any type, does not conduct outpatient appointments for patients who are hospitalized.
“Difficult tasks, whether it be a health problem or a life catastrophe, require not only perseverance in overcoming. Often a negative course of events changes the intellectual effort - making meaningful decisions based on objective data.
Read more
★9.81 based on 15 reviews
- Chibikova Evgenia Yurievna
Child psychiatrist, adult psychiatrist.
at the clinic online
Children (0-17 years old) Adults (18 to 60 years old)
Concentration.
Care.
Regularly trains and studies abroad. Thanks to this, he is able to prescribe effective, but at the same time the safest drugs.
Filigree in neurochemistry.
Read more
★9.71 based on 112 reviews
- Kuznetsov Sergey Olegovich
Psychologist. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Teenagers (16 to 17 years old) Adults (18 to 60 years old)
Clarity. Impartiality.
Outline your problem and steps to fix it. Support on the path of real change. Shows the problem for what it is. Do not embellish and do not add something of their own. Demonstrates an alternative attitude in therapy so that you can live it from your own experience, and not theoretically.
Read more
★9.
83 based on 52 reviews
- Dobrovidova Natalya Alexandrovna
Psychologist. Cognitive behavioral psychotherapist. PhD
in the clinic online
Adults (18 to 60 years old) Adolescents (from 14 to 17 years old)
Humanism. Environmental friendliness.
Will teach you how to manage your mental life. She is convinced that "our thoughts are the basis of our mental health and happiness", "and neurosis is a choice." It will help you make a choice in your favor. In fact, it forms a new way of thinking and new habits (which is so difficult to do without help and support). Such changes in the psyche lead to significant changes in life. He believes in every person and considers this the basis of quality therapy.
Read more
★9.64 based on 41 reviews
- Trofimova Marina Ivanovna
Psychologist.
Sexologist.
in the clinic online
Adults (from 18 to 60 years old)
Non-judgmental. Result.
Can quickly and clearly show the connection between thoughts and emotions that affect life. Teaches you to overestimate the beliefs and attitudes that reduce the quality of life. Helps clients to move towards the goal step by step, respects the choice of the patient, gently and confidently accompanies along the way.
Read more
★9.43 based on 31 reviews
- Vyrikov Artur Igorevich
Clinical psychologist. ACT psychotherapist. Cognitive behavioral psychotherapist
in clinic online
Adults (18 to 55 years old)
Trust. Simplicity.
Creates a friendly atmosphere of understanding and ease, communicates in simple language.
Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path.
Read more
★9.52 based on 82 reviews
- Yarygin Anton Igorevich
Adult psychiatrist.
in the clinic online
Adults (over 18 years old) Elderly (over 60)
Confidence. Efficiency.
First class and highly organized specialist.
Anton is maximally focused on the healing process. Able to quickly evaluate incoming information, make objective and accurate decisions. Works with full dedication, passionate about the work process.
Competently arranges treatment and brings the case to a positive result.
Read more
★9.27 based on 37 reviews
- Shlyapnikov Sergei Anatolievich
Psychiatrist.
in the clinic online
Adults (18-60) Elderly (from 60 years old) Adolescents (16 to 17 years old)
Perseverance. Result.
Strengths. An incredibly empathetic psychiatrist who works effectively with patients of all ages. He specializes in working with anxiety, panic, depression, obsessions and, in general, in working with neurotic disorders.
“I am convinced that psychiatry is one of the most interesting branches of medicine. Seeing the patient feel better is priceless.”
Able to smooth out sharp corners in a humorous way. Sense of humor.
More details
★8.
23 based on 13 reviews
Obsessive-compulsive disorder - what is it. Symptoms and basic principles of treatment for OCD
Doctors Reviews
Obsessive-compulsive disorder (OCD) is a condition characterized by obsessions and compulsions (recurring behaviors or rituals).
Obsessions are repetitive thoughts, images or urges that a person at the initial stage of the disease himself evaluates as obsessive or unfounded; later they cause him anxiety or guilt. The most common obsession concerns infections (the threat of infection) and tends to wash hands unnecessarily frequently.
Obsessions can also come from the fear of causing misfortune, injury, or accident, such as leaving the house unlocked or forgetting to turn off the gas. People with OCD feel compelled to reexamine themselves repeatedly. Intrusive thoughts related to violence, murder, blasphemy, or sex are also driven by the fear of harm.
Obsessive actions or rituals (compulsions) are actions that people are forced to purposefully repeat in order to try to reduce their psychological discomfort or avoid it. Most common compulsions:
- frequent checks to prevent possible danger;
- excessive brushing or washing of hands;
- re-search for confirmation;
- re-counting or touching to reduce the risk of disaster;
- organization or arrangement of objects or activities;
- repeatedly asking questions or telling about one's actions;
- storage of useless or worn-out property.
Leave a request for a consultation
and our specialist will contact you at any time convenient for you
Our doctors
Abdulova Laysan Rustamovna
Psychiatrist
Specialist experience over
2 years
Arbuzov Igor Evgenievich
Psychiatrist
Specialist experience over
8 years
Bazanova Irina Sergeevna
Psychiatrist
Specialist experience over
2 years
Butarny Alexander Olegovich
Psychiatrist
Specialist experience over
3 years
Zuikova Nadezhda Leonidovna
Psychotherapist
Specialist experience over
35 years
Kakadzhikova Jamal Guychgeldiyevna
Psychiatrist
Specialist experience over
1 year
Komova Alexandra Vladimirovna
Psychiatrist
Specialist experience over
1 year
Korobkova Irina Grigorievna
Psychiatrist
Professional experience over
9 years
Korobushkina Natalya Valerievna
Psychiatrist
Specialist experience over
3 years
Mikhailova Zoya Igorevna
Psychiatrist
Specialist experience over
5 years
Parshakova Ekaterina Sergeevna
Psychiatrist
Sarycheva Anna Aleksandrovna
Psychiatrist
Tsyganova Anna Sergeevna
Psychiatrist
Comprehensive diagnostics
in 3 days
Diagnostic and treatment programs for anxiety, depression
and sleep disorders in our hospital
Read more>>>
Reviews
Read all reviews
Nadezhda Leonidovna thank you for being you! thanks to you, life is changing for the better, I admire in .