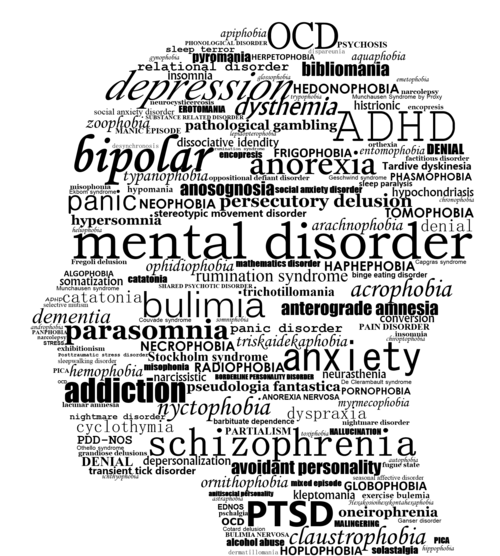
Example of bpd
NIMH » Borderline Personality Disorder
What is borderline personality disorder?
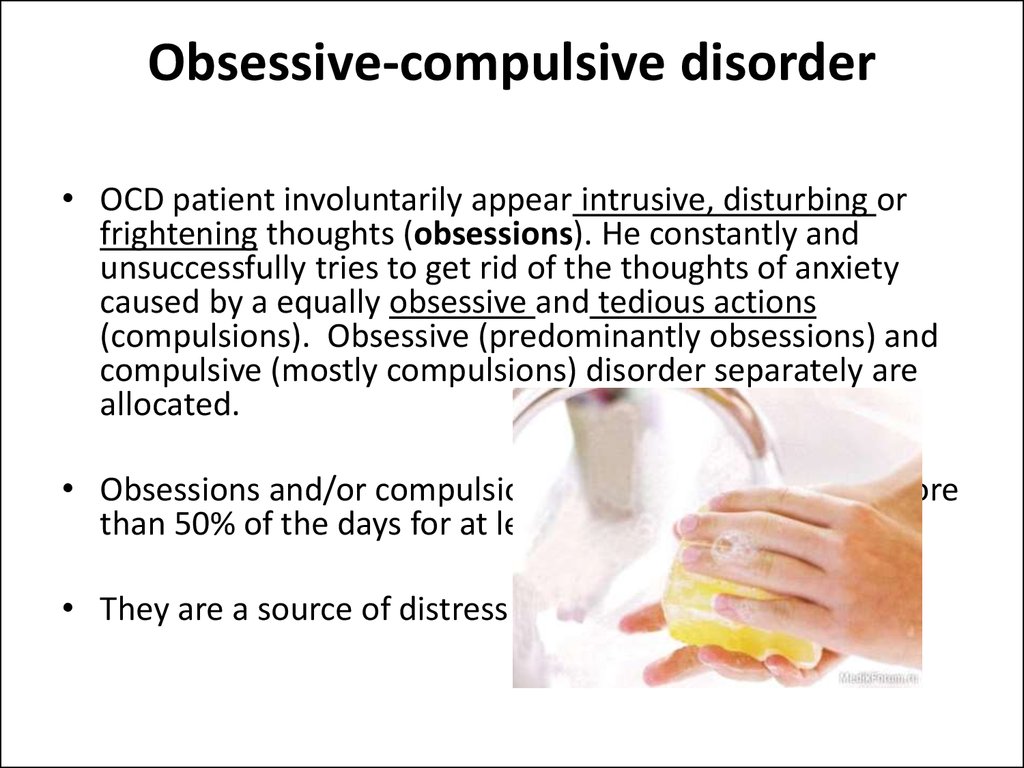
Borderline personality disorder is a mental illness that severely impacts a person’s ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others. Effective treatments are available to manage the symptoms of borderline personality disorder. Learn more about the disorder, how it’s diagnosed, and how to find support.
What are the signs and symptoms?
People with borderline personality disorder may experience intense mood swings and feel uncertainty about how they see themselves. Their feelings for others can change quickly, and swing from extreme closeness to extreme dislike. These changing feelings can lead to unstable relationships and emotional pain.
People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their interests and values can change quickly, and they may act impulsively or recklessly.
Other signs or symptoms may include:
- Efforts to avoid real or perceived abandonment, such as plunging headfirst into relationships—or ending them just as quickly.
- A pattern of intense and unstable relationships with family, friends, and loved ones.
- A distorted and unstable self-image or sense of self.
- Impulsive and often dangerous behaviors, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviors happen mostly during times of elevated mood or energy, they may be symptoms of a mood disorder and not borderline personality disorder.
- Self-harming behavior, such as cutting.
- Recurring thoughts of suicidal behaviors or threats.
- Intense and highly variable moods, with episodes lasting from a few hours to a few days.
- Chronic feelings of emptiness.
- Inappropriate, intense anger or problems controlling anger.
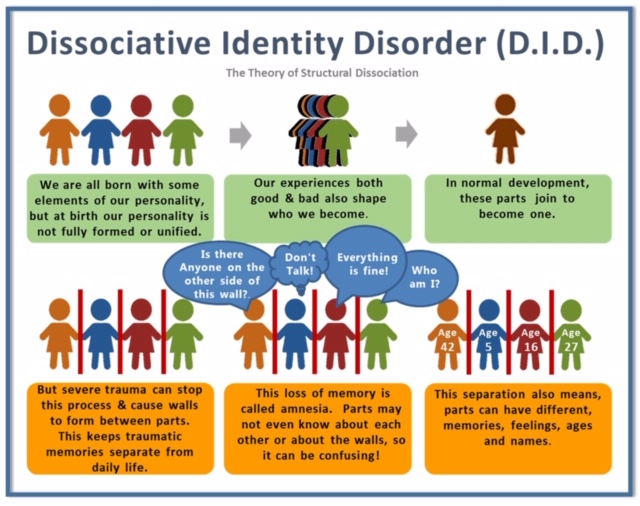
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality.
Not everyone with borderline personality disorder may experience all of these symptoms. The severity, frequency, and duration of symptoms depend on the person and their illness.
People with borderline personality disorder have a significantly higher rate of self-harming and suicidal behavior than the general population.
People with borderline personality disorder who are thinking of harming themselves or attempting suicide need help right away.
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
What causes borderline personality disorder?
Researchers aren’t sure what causes borderline personality disorder, but studies suggest that genetic, environmental, and social factors may increase the risk of developing it. These factors may include:
These factors may include:
- Family history: People who have a close family member (such as a parent or sibling) with the illness may be at a higher risk of developing borderline personality disorder.
- Brain structure and function: Research shows that people with borderline personality disorder may have structural and functional changes in the brain, especially in the areas that control impulses and emotion regulation. However, the studies do not demonstrate whether these changes were risk factors for the illness or if such changes were caused by the disorder.
- Environmental, cultural, and social factors: Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or hardship during childhood. Others may have been exposed to unstable, invalidating relationships or conflicts.
Although these factors may increase a person’s risk, it doesn’t mean it is certain that they’ll develop borderline personality disorder.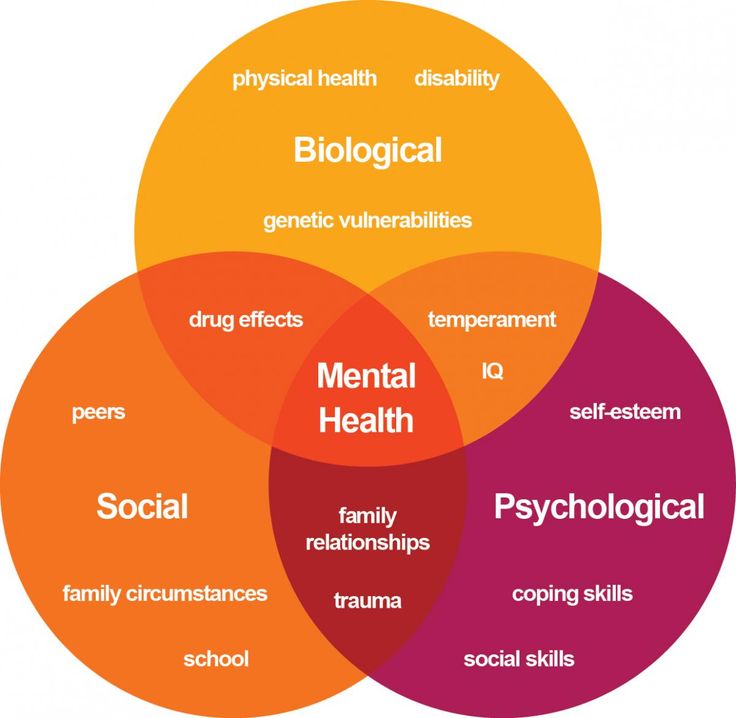 Likewise, people without these risk factors may develop the disorder in their lifetime.
Likewise, people without these risk factors may develop the disorder in their lifetime.
How is borderline personality disorder diagnosed?
A licensed mental health professional—such as a psychiatrist, psychologist, or clinical social worker—who is experienced in diagnosing and treating mental disorders can diagnose borderline personality disorder based on a thorough interview and a discussion about symptoms. A careful and thorough medical exam also can help rule out other possible causes of symptoms. In diagnosing the illness, providers will discuss a person’s symptoms and ask about family medical histories, including histories of mental illness.
Borderline personality disorder is usually diagnosed in late adolescence or early adulthood. Occasionally, a person younger than age 18 may be diagnosed with borderline personality disorder if symptoms are significant and last at least a year.
What other illnesses can co-occur with borderline personality disorder?
Borderline personality disorder often occurs with other mental illnesses, such as post-traumatic stress disorder (PTSD). These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
How is borderline personality disorder treated?
Borderline personality disorder historically has been viewed as challenging to treat. But with newer, evidence-based treatment, many people with this disorder experience fewer and less severe symptoms, improved functioning, and better quality of life. It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
Many factors affect the length of time it takes for symptoms to improve once treatment begins. It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
It is important to seek—and stick with—treatment.
Studies funded by the National Institute of Mental Health (NIMH) indicate that individuals with borderline personality disorder who don’t receive adequate treatment are more likely to develop other chronic medical or mental illnesses and are less likely to make healthy lifestyle choices.
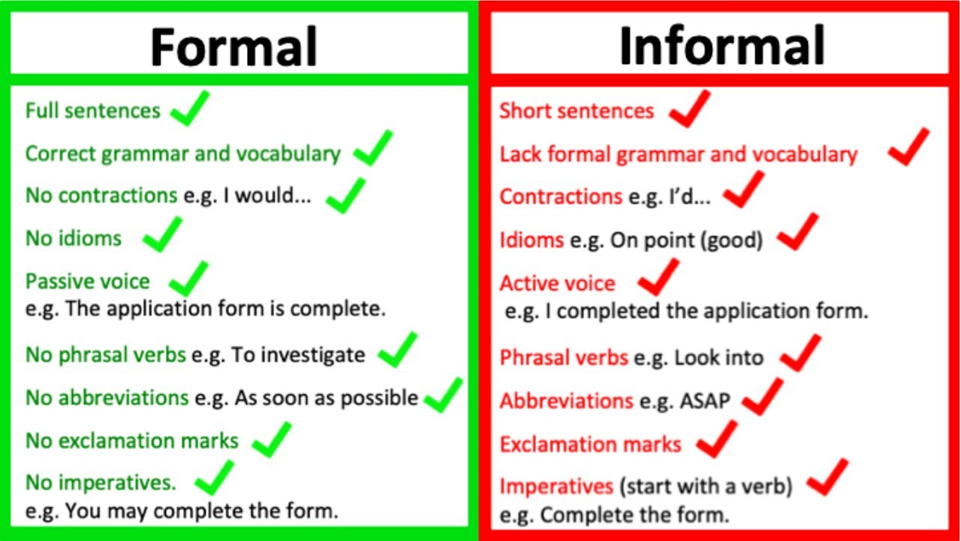
Psychotherapy
Psychotherapy, sometimes called “talk therapy,” is the first-line treatment for people with borderline personality disorder. Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Two examples of psychotherapies used to treat borderline personality disorder are:
- Dialectical Behavior Therapy (DBT): This treatment was developed specifically for individuals with borderline personality disorder.
 DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships.
DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships. - Cognitive Behavioral Therapy (CBT): This treatment can help people identify and change core beliefs and behaviors that come from inaccurate perceptions of themselves and others and problems interacting with others. It may help people reduce mood swings and anxiety symptoms and may reduce the number of self-harming or suicidal behaviors.
Read more on NIMH’s psychotherapies webpage.
Medications
Because the benefits of prescription medication for borderline personality disorder are unclear, medications aren’t typically used as the primary way to treat the illness. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms or co-occurring mental disorders such as mood swings or depression.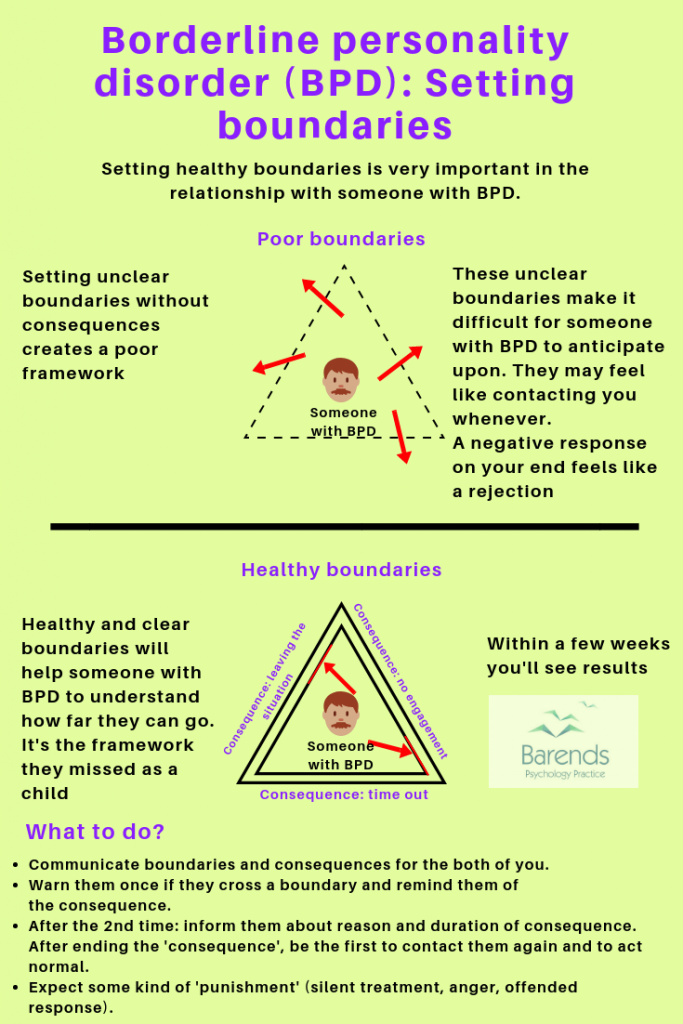 Treatment with medications may require coordinated care from more than one medical professional.
Treatment with medications may require coordinated care from more than one medical professional.
Medications also can sometimes cause side effects in some people. Talk to your provider about what to expect from a particular medication. Read more on NIMH’s mental health medications webpage.
Where can I find help?
If you’re not sure where to get help, a health care provider can refer you to a licensed mental health professional, such as a psychiatrist or psychologist with experience treating borderline personality disorder. If you need help starting the conversation, check out the Tips for Talking With Your Health Care Provider fact sheet.
Other resources include:
- Substance Abuse and Mental Health Services Administration’s Behavioral Health Treatment Services Locator, a tool for finding mental health services in your area
- NIMH’s Help for Mental Illnesses webpage
- Agency for Healthcare Research and Quality’s website
Therapy for Caregivers and Family Members
Having a relative or loved one with the disorder can be stressful, and family members or caregivers may unintentionally act in ways that can worsen their loved one’s symptoms.
Although more research is needed to determine how well family therapy helps with borderline personality disorder, studies on other mental disorders show that including family members can help support a person’s treatment. Families and caregivers also can benefit from therapy.
Family therapy helps by:
- Allowing the relative or loved one to develop skills to understand and support a person with borderline personality disorder.
- Focusing on the needs of family members to help them understand the obstacles and strategies for caring for someone with the disorder.
How can I help a friend or family member with borderline personality disorder?
Here are some ways to help a friend or relative with the disorder:
- Take time to learn about the illness to understand what your friend or relative is experiencing.
- Offer emotional support, understanding, patience, and encouragement. Change can be difficult and frightening to people with borderline personality disorder, but things can improve over time.

- Encourage your loved one in treatment for borderline personality disorder to ask about family therapy.
- Seek counseling for yourself. Choose a different therapist than the one your relative is seeing.
How can I learn more about clinical trials studying borderline personality disorder?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions, including borderline personality disorder. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit NIMH’s clinical trials webpage.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. We encourage you to reproduce and use NIMH publications in your efforts to improve public health. If you do use our materials, we request that you cite the National Institute of Mental Health. To learn more about using NIMH publications, refer to NIMH's reprint guidelines.
For More Information
Medline Plus (National Library of Medicine) (en español)
ClinicalTrials.gov (en español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 22-MH-4928
Revised 2022
Borderline Personality Disorder: What You Need To Know
Borderline personality disorder (BPD) is a complex condition. It affects how a person feels about themselves and others. BPD is characterized by intense, unstable emotions and relationships as well as insecurity and self-doubt.
BPD makes everything about a person feel unstable, ranging from moods, thinking, behavior, relationships, and sometimes identity. People with this condition have described BPD as the feeling of having an exposed nerve ending, essentially leaving someone to be easily triggered by small things.
But there are effective treatments for it.
Keep Reading To Learn
- The truth about borderline personality disorder
- How to recognize BPD in yourself and other people
- How borderline personality disorder is diagnosed and treated
- Common myths and misconceptions about BPD
Understanding the Rollercoaster of BPD
People with borderline personality disorder often feel a huge amount of emotional instability. It impacts a person’s self-image, likes and dislikes, and goals. This often makes them confused about their sense of self. The condition makes it difficult for a person to be comfortable in their skin.
Many people with BPD act impulsively, have intense emotions, and experience dissociation and paranoia when most distressed.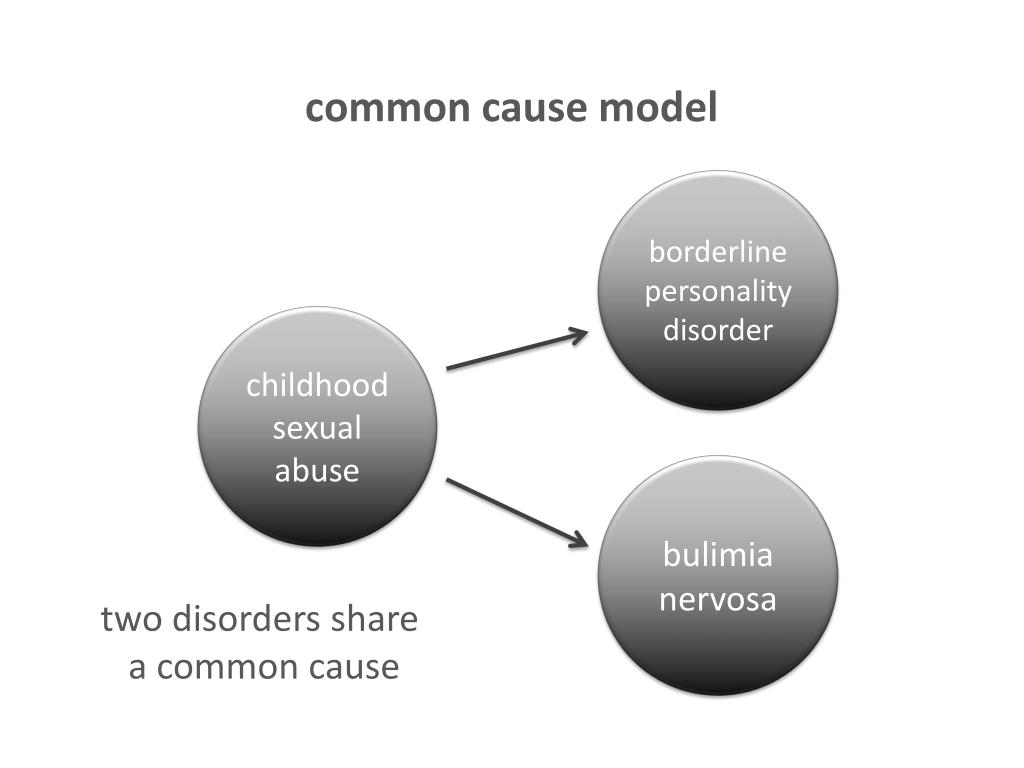 This emotional volatility can cause relationship turmoil. Also, the inability to self-soothe can lead to impulsive, reckless behavior.
This emotional volatility can cause relationship turmoil. Also, the inability to self-soothe can lead to impulsive, reckless behavior.
1.4% of American adults experience BPD
People with BPD are often on edge. They have high distress and anger levels, so they may be easily offended. They struggle with beliefs and thoughts about themselves and others, which can cause distress in many areas of their lives.
People living with BPD often have an intense fear of instability and abandonment. As a result, they have problems being alone.
The condition is also known for anger, mood swings, and impulsiveness. These qualities can dissuade people from being around someone with BPD. On top of this, many people with the condition struggle with self-awareness and how others perceive them. This makes them extremely sensitive.
BPD is a mind and body condition. Its symptoms begin to manifest during the early teenage years and gradually improve during adult life.
Watch Now!
Dr. Lois Choi-Kain helps us understand borderline personality disorder
What Causes Borderline Personality Disorder?
BPD may be caused by genetics, brain abnormalities, and/or environmental factors. Due to the wide variety of suspected risk factors, it’s hard to determine who will develop it.
Environmental Factors
Early childhood adversity, such as child abuse or neglect, may be a cause.
Genetics
Research suggests that it may be an inherited genetic condition or linked with other mental disorders among other family members.
Brain Abnormalities
Certain brain differences are thought to be contributing causes of the disorder. When certain brain chemicals responsible for mood regulation don’t function properly, there are changes in some areas of the brain. This has been linked to aggression, difficulty regulating destructive urges, and depression.
This has been linked to aggression, difficulty regulating destructive urges, and depression.
BPD Doesn’t Often Occur Alone
Effective treatment involves addressing related disorders.
Many people diagnosed with borderline personality disorder experience other conditions, including:
- Depression
- Anxiety disorders
- Eating disorders
- Post-traumatic stress disorder (PTSD)
- Bipolar disorder
- Substance use disorder
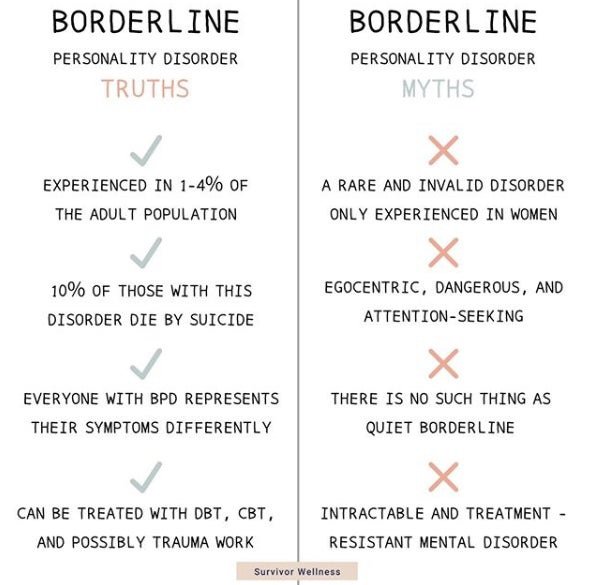
There Are Many Misconceptions
This disorder is misunderstood by many, including some mental health practitioners. This confusion can impact and influence the way that people are treated. Even worse, long-standing myths can discourage people from seeking help for the condition, especially if they feel their experience is being misunderstood.
Some common myths and misconceptions are:
Myth: It’s Not Treatable
Borderline personality disorder is very treatable. In the past, since BPD affects someone’s personality, many were quick to conclude that it was untreatable because someone’s personality cannot be changed.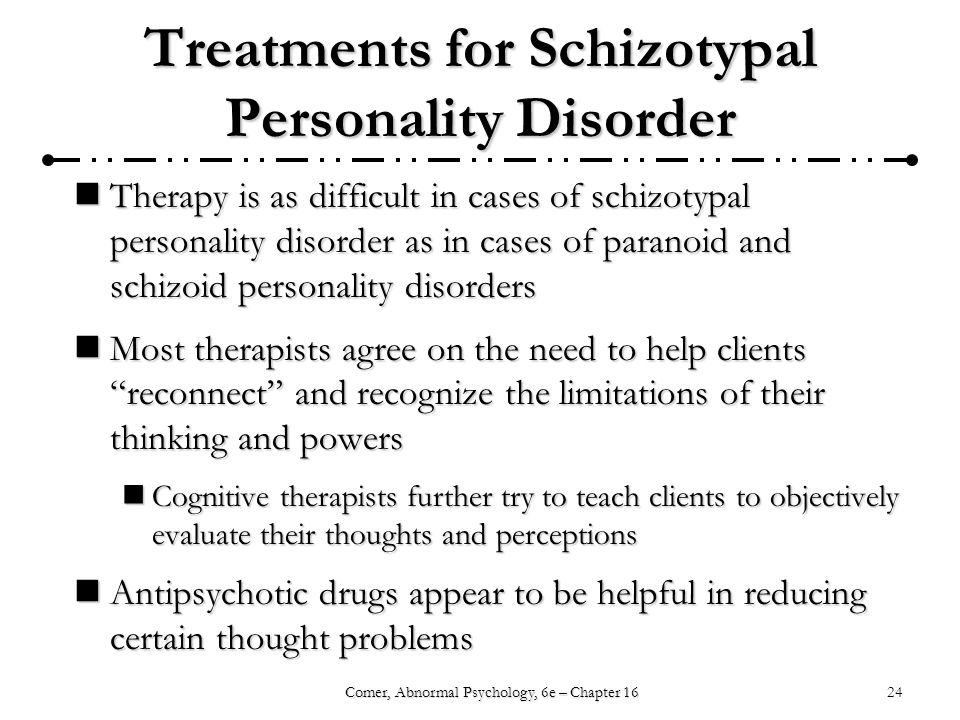
More recently, many therapies have been proven effective as treatments, including dialectical behavior therapy (DBT), mentalization-based treatment (MBT), and transference-focused psychotherapy (TFP). Now, a growing number of less intensive, generalist approaches, like general psychiatric management (GPM), are also being practiced around the world.
A BPD diagnosis doesn’t mean that someone will live with symptoms forever. With treatment, the symptoms ebb and flow. Many people with the condition can have high-functioning lives.
Myth: People With BPD Are Victims of Child Abuse
This is not always the case.
While some cases of borderline personality disorder stem from childhood trauma, a diagnosis is more likely to be the result of a combination of environmental factors. These can include attachment, childhood trauma, biological factors, and social factors.
Myth: It Affects Only Women
It’s estimated that over 14 million Americans have BPD. Once more commonly diagnosed in women, the largest study done on psychiatric disorders shows that it occurs equally often in women and men.
One explanation behind it appearing to affect more women is that women are more likely to seek mental health care than men. Since research on BPD is often conducted in a psychiatric setting, it was previously less likely for men with borderline personality disorder to be included in these research efforts.
Another explanation is that BPD is often misdiagnosed in men. Many men with the condition are often diagnosed with depression or PTSD.
Meg’s Journey With BPD
Meg is a participant in McLean’s Deconstructing Stigma campaign, and she struggles with BPD.
Read more about Meg’s mental health story and her message of hope for those who are also struggling.
Meg’s Story
Recognizing Borderline Personality Disorder in Yourself—or Others
People with borderline personality disorder struggle with self-regulation. Self-regulation is the ability to manage emotions, thoughts, and behaviors in ways that have positive outcomes, like self-esteem and good relationships.
Self-regulation is the ability to manage emotions, thoughts, and behaviors in ways that have positive outcomes, like self-esteem and good relationships.
To be officially diagnosed, a person has to exhibit five or more related symptoms. These symptoms have to be ongoing and impact various aspects of life.
There are a handful of medically recognized symptoms of borderline personality disorder.
Instability in Relationships
Intense and short-lived relationships are common for people with BPD. It’s very common for someone with this disorder to have intense, unstable relationships filled with drastic and quick-changing feelings.
A person with BPD may fall in love quickly and assume that the other person will make them happy. Typically, this results in the person feeling hurt and disappointed and can further intensify emotional swings. People with this condition may have either perfect or horrible relationships, with rapid changes in perception resulting from anger, hate, and devaluation.
Extreme Emotional Swings
Someone with this condition often experiences unstable moods and emotions. The little things that don’t mean much to others—like someone not holding the door open for you or meeting a new friend—can be either very exciting or frustrating.
Many with this condition can be happy one moment and extremely sad or disappointed the next. Their moods are also very intense and unpredictable in timing. They can last anywhere from a few minutes to a few hours or longer.
Explosive Feelings of Anger
Many people with BPD struggle with intense anger and a short temper. This makes it difficult for them to feel in control of their emotions once they have been provoked. They can quickly fill with rage, though this anger may not always be outwardly directed and can result in self-harm. Sometimes the person might be angry at themselves and not at anyone or anything else.
Self-Harm
Self-harm is risky behavior that may make the person feel good at the moment of distress.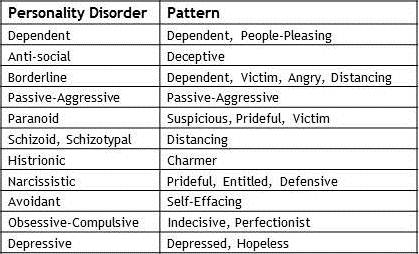 Many people with BPD often engage in self-harming activities, think about suicide, and make suicidal gestures and threats.
Many people with BPD often engage in self-harming activities, think about suicide, and make suicidal gestures and threats.
Many people with borderline personality disorder engage in sensation-seeking behavior that could be harmful, especially when they are angry.
Risky or deliberate self-harm activities may include:
- Engaging in dangerous and unhealthy binge drinking
- Cutting or other self-injury
- Going on shopping and spending sprees
- Regularly engaging in unsafe sex
- Using drugs
Not all self-harm is intended to end in death. It’s important to remember that it’s often used as a way to feel better in a grim moment. However, if it goes untreated, these risky behaviors can end in suicide.
McLean’s Michael Hollander, PhD, an expert in self-harm in adolescents, helps us understand more about teen cutting and self-injury.
Lingering Feelings of Emptiness or Worthlessness
A lot of people with the condition struggle with emptiness or worthlessness. Many with BPD report feeling like there is a void inside of them or like they don’t matter. As a result, they often turn to sex, drugs, or food to try to feel satisfied.
Many with BPD report feeling like there is a void inside of them or like they don’t matter. As a result, they often turn to sex, drugs, or food to try to feel satisfied.
Feeling Out of Touch With Reality
Many diagnosed with BPD feel suspicious about events in their lives. They struggle with feelings of suspicion and paranoia about the intentions of people around them. When they are stressed, they may lose touch with reality and become disassociated. Disassociation feels like being spaced out, foggy, or as if you exist outside of your own body.
BPD can be confused with other forms of mental illness, so a diagnosis is important. If you or someone close to you often has feelings of emptiness, loneliness, or insecurity that cause irrationality or impulsivity, it’s important to talk to your health care provider.
Have You Been Watching?
Mental Health Webinars
McLean develops free and reliable mental health resources for the public and professionals to promote healthy individuals and communities.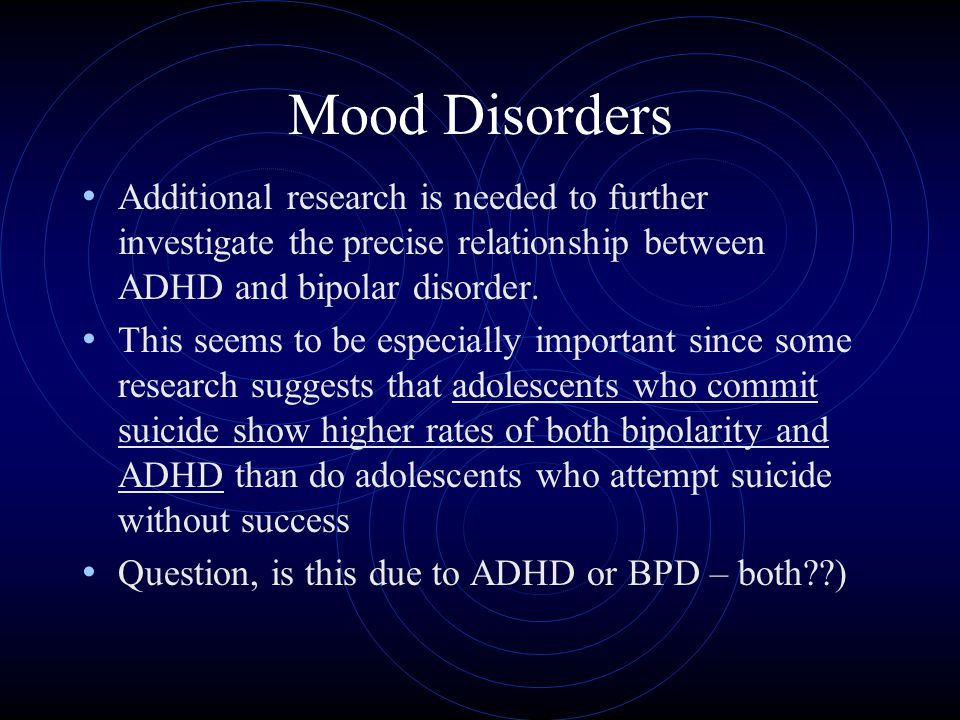
Sign Up Now!
When Is It Time To See a Professional?
If you are experiencing any of the previously mentioned signs and symptoms associated with borderline personality disorder, please consult a mental health professional. This condition is common and treatable.
You should see a doctor any time your symptoms are triggered. If you are unsure of your triggers, try to think of a time in the past when you experienced raging and intense emotions, acted impulsively, or had a desire to harm yourself. The events before this emotion are likely your triggers.
Many who have BPD experience suicidal thoughts. These can include but aren’t limited to mental images and fantasies about self-harm and plotting suicide. If you are experiencing suicidal thoughts and may harm yourself or someone else, call 911 immediately or visit your nearest emergency room.
Understanding and Recognizing Symptoms
People with BPD are sensitive to stress, so stressful situations activate symptoms related to the condition. The stressors that promote BPD’s most volatile symptoms can be external or internal, and they often vary from one person to another. There are both interpersonal and mental triggers of borderline personality disorder, many of which are unique to the individual.
The stressors that promote BPD’s most volatile symptoms can be external or internal, and they often vary from one person to another. There are both interpersonal and mental triggers of borderline personality disorder, many of which are unique to the individual.
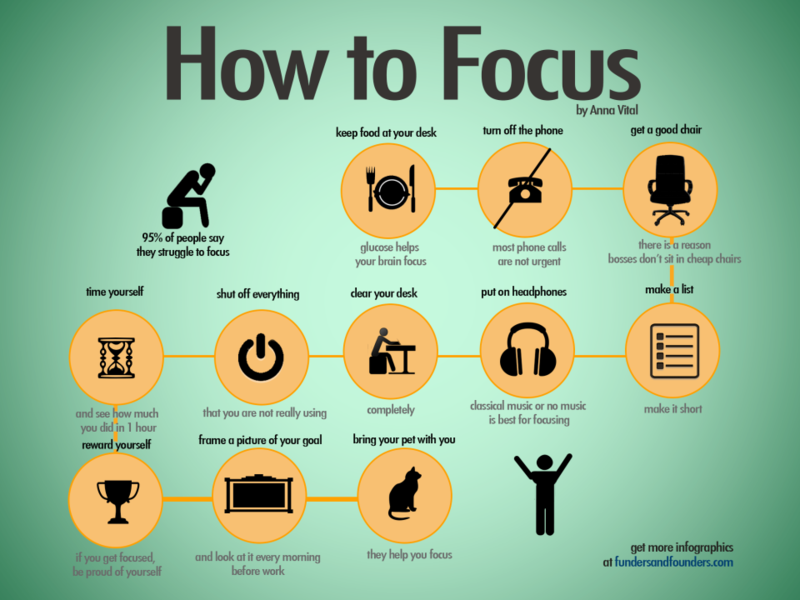
Managing these symptoms, either for yourself or your partner, starts by understanding emotions, thoughts, and memories that set off symptoms. Then you can better manage addressing the symptoms if a stressor is unavoidable. You should work with a mental health professional to learn physical and mental exercises to understand triggers and develop skills to successfully manage them.
Interpersonal Relationship Events
Separations, disagreements, and rejections—real or perceived—are the most common triggers for symptoms. A person with BPD is highly sensitive to abandonment and being alone, which brings about intense feelings of anger, fear, suicidal thoughts and self-harm, and very impulsive decisions.
When something happens in a relationship that makes them feel abandoned, criticized, or rejected, their symptoms are expressed. People with borderline personality disorder experience rejection sensitivity, which makes relationships very intense and dependent. Events that can worsen this can be losing a job, ending a relationship, or experiencing rejection of any type.
People with borderline personality disorder experience rejection sensitivity, which makes relationships very intense and dependent. Events that can worsen this can be losing a job, ending a relationship, or experiencing rejection of any type.
Identifying Episodes
To better manage triggers, it is crucial to understand episodes. These episodes are highly dependent on the situation at hand and the specific individual, but there are common red flags for recognizing an episode.
Things that can indicate an episode is occurring:
- Intense angry outbursts
- Suicidal thoughts and self-harm behavior
- Going to great lengths to feel something, then becoming increasingly avoidant and withdrawn
- Paranoia, feeling as if there is someone out to get you
These episodes can also involve extreme feelings of positivity and euphoria. People with this condition can be very impulsive. It’s important to note these emotional highs as signs of an episode because they may be involved in risky behavior as well.
Understanding BPD in Teens
The difference between typical teen behaviors and emerging personality disorders can be hard to recognize. How can you tell which is which?
Read the Article
Treating Borderline Personality Disorder
Treatment involves breaking down the dysfunctional patterns of the brain’s thinking, feeling, and behavior that cause distress to maintain a better emotional balance. Sometimes health care providers may suggest medication as part of a care plan.
The treatment options often used are general psychiatric management (GPM), dialectical behavior therapy (DBT), mentalization-based treatment (MBT), and transference-focused psychotherapy (TFP).
General Psychiatric Management
Sometimes referred to as good psychiatric management, GPM is designed to provide “good enough” treatment to most patients. This treatment is not inferior to others. Studies have shown that GPM can be as effective as DBT in treating patients.
Studies have shown that GPM can be as effective as DBT in treating patients.
GPM combines the essential ingredients of other treatments to provide care to the patient, even when specialized or more resource-intensive treatments are not available.
Learn more about general psychiatric management
Dialectical Behavior Therapy
DBT is known as the gold standard BPD treatment. It emphasizes the development of four skill sets: mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. DBT teaches patients to control their intense emotions and minimize their destructive patterns.
Through DBT, patients can also learn how to build interpersonal skills and develop self-awareness.
DBT has been clinically tested, proven to be effective in borderline personality disorder and depression treatment in adolescents and adults, and is used extensively at McLean Hospital.
Learn more about dialectical behavior therapy
Watch Now!
Dr. Lois Choi-Kain talks about treating BPD
Mentalization-Based Treatment
MBT aims to help patients by improving interpersonal and relationship skills while reducing self-destructive behaviors. Mentalizing focuses on the ability to differentiate and concentrate on your emotional state of mind and separate your own thoughts and feelings from those around you.
Since individuals with BPD can find it difficult to recognize the impacts of their behaviors, MBT encourages focusing and reflecting on mental states to better understand how mental state affects behavior in ourselves and others.
Learn more about mentalization-based treatment
Transference-Focused Psychotherapy
TFP focuses on the patient’s sense of identity and aims to create more stable and realistic experiences of both self and others. With BPD, one’s sense of identity may feel contradicted. TFP focuses on addressing identity-based problems with interpersonal relationships, self-esteem, and mood.
With BPD, one’s sense of identity may feel contradicted. TFP focuses on addressing identity-based problems with interpersonal relationships, self-esteem, and mood.
By helping patients learn to verbalize what they are feeling—versus acting impulsively on emotions—TFP helps with increased functioning and satisfaction in interpersonal relationships.
In addition to these therapies, group and individual therapy may be useful as well. Group and individual therapies cover a broad range of topics and are not necessarily sessions dedicated to BPD. Group and individual therapy can be beneficial for addressing mindfulness, interpersonal relationships, stress management, emotion regulation, and family relationships.
Learn more about transference-focused psychotherapy
How Is Borderline Personality Disorder Diagnosed?
Borderline personality disorder is a complex condition that doesn’t present itself the same way in every person.
Some mental and psychological disorders have similar symptoms, so it’s vital to see a licensed mental health professional for an assessment and the right diagnosis.
To diagnose, your provider may go through the following:
- A detailed interview with your doctor, a mental health provider, or both
- A psychological evaluation
- Medical history and/or a medical exam
- Discussing signs and symptoms, including criteria in the hallmark signs of BPD
Most diagnoses are in patients 18 and older. BPD can, however, be diagnosed in younger patients.
If you are experiencing the mentioned signs and symptoms associated with borderline personality disorder, please consult a mental health professional.
People with this condition often experience suicidal thoughts, such as mental images and fantasies about self-harm and plotting suicide. You should contact a suicide hotline number, a close loved one, or a mental health provider to get help.
Suicide prevention resources can be found below.
Good News: There’s Hope for Folks With BPD!
Because borderline personality disorder is as unique as each person who lives with it, treatment requires a specialized approach.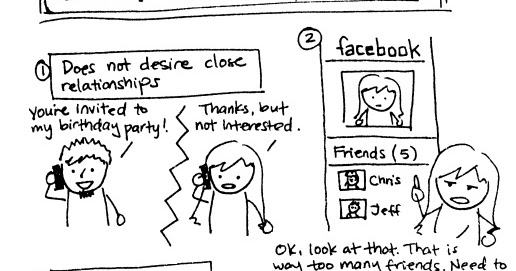
Many people have BPD and, at times, experience emotional anguish from the condition. However, you don’t have to resort to living a life that’s full of pain and heartbreak. It’s important to take care of yourself, recognize your triggers, and work with your health care team to determine what treatments will help keep it in check.
By committing to care and learning as much as possible about it, you can make a difference in your quality of life—and the lives of those around you.
McLean Is Here to Help
McLean offers world-class care for teens and adults who struggle with borderline personality disorder. Contact us today to find the care that’s right for yourself or your loved one.
877.372.3068877.372.3068
Want More Info?
Looking for even more information about borderline personality disorder? You may find these resources helpful.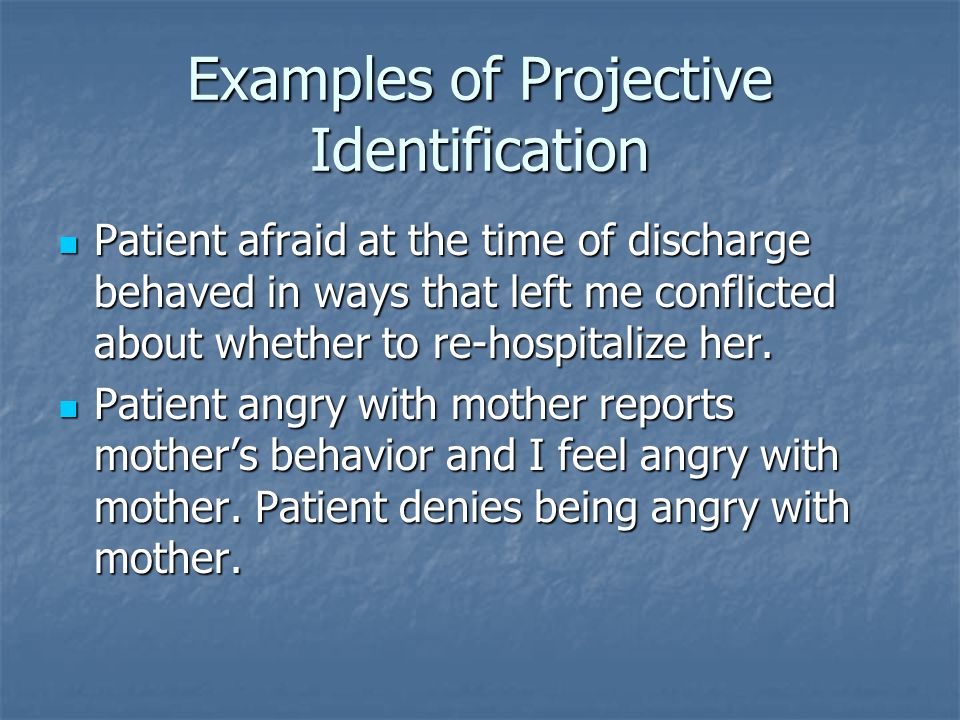
Interesting Articles, Videos, and More
Learn more about borderline personality disorder and what you can do if you or a loved one is displaying signs of BPD.
- 4 Myths About Borderline Personality Disorder
- The Impact of COVID-19 on Individuals With Borderline Personality Disorder
- Video: Remaining in Control of Our Emotions
- How Working Improves Your Mental Health
- Video: Courtney Cook Is Living Her Life With BPD
- Podcast: Living a Life of Empathy and Experience
- Find access to all of McLean’s resources on BPD
Helpful Links
These organizations may also have useful information:
Behavioral Tech: Training for Mental Health Professionals
Behavioral Tech provides robust training for clinicians, especially in dialectical behavior therapy and other treatments for borderline personality disorder. Behavioral Tech also offers resources for providers and consumers in an effort to bring ever-better treatments to those in need. The organization supports advocacy efforts and BPD research.
The organization supports advocacy efforts and BPD research.
Borderline Personality Disorder Resource Center
The mission of the Borderline Personality Disorder Resource Center (BPDRC) is to promote BPD education and connect those affected by BPD to established resources for treatment and support. The BPDRC is affiliated with the Personality Disorders Institute at New York-Presbyterian Hospital/Westchester Division, and their efforts are overseen by innovators in the research and treatment of personality disorders. Among many resources, the BPDRC maintains a nationwide database of clinicians, agencies, and facilities that focus on treating BPD and co-occurring disorders.
National Education Alliance for Borderline Personality Disorder
This group provides education, while raising public awareness and understanding, in an attempt to reduce stigma and promote research and enhance the quality of life of those affected by borderline personality disorder. They work with Congress to enhance the quality of life for those individuals affected by this serious but treatable mental illness. NEABPD’s many resources include BPD Family Guidelines, The Family Connections Program, and Family Education Workshop videos.
NEABPD’s many resources include BPD Family Guidelines, The Family Connections Program, and Family Education Workshop videos.
New England Personality Disorder Association
NEPDA’s mission is to promote education, support, and advocacy in the field of personality disorders, with a concentration on borderline personality disorder. NEPDA sponsors workshops, conferences, and small group meetings for family members, friends and other loved ones, consumers of mental health services, professionals, and the community at large to improve awareness of personality disorders and reduce the stigma that is often associated with them.
Personality Disorder Awareness Network (PDAN)
A not-for-profit organization dedicated to increasing public awareness of personality disorders, alleviating the impact of personality disorders on families, and preventing the development of personality disorders in children.
Treatment and Research Advances Association for Borderline Personality Disorder
The TARA for Borderline Personality Disorder’s mission is to foster education and research in the field of personality disorders, like borderline personality disorder. They support and encourage educational programs and endeavors targeting mental health professionals, consumers of mental health services, families, and communities to reduce stigma and increase awareness, to disseminate available information on etiology and treatment, and to advocate for accomplishments of these goals.
They support and encourage educational programs and endeavors targeting mental health professionals, consumers of mental health services, families, and communities to reduce stigma and increase awareness, to disseminate available information on etiology and treatment, and to advocate for accomplishments of these goals.
Suicide Prevention Resources
Although it is not possible to predict suicide with any certainty, our best tool is recognition of the signs that many people exhibit when contemplating suicide. The following three behaviors should prompt you to seek immediate help for yourself or a loved one:
- Talking about wanting to die or to kill oneself
- Looking for a way to kill oneself, such as searching online or obtaining a gun
- Talking about feeling hopeless or having no reason to live
If You or Someone You Know Needs Help
- Call 1.800.273.8255 or 988 for the National Suicide Prevention Lifeline
- Text HELLO to 741-741 for free, 24-hour support from the Crisis Text Line
- Outside of the U.
 S., visit the International Association for Suicide Prevention for a database of resources
S., visit the International Association for Suicide Prevention for a database of resources - Contact your mental health professional
- Call us at McLean at 617.855.3141 for information on admission
Find more suicide prevention resources.
If you are suicidal or are a danger to yourself or others, please call 9-1-1 or visit your nearest emergency room immediately.
These organizations also offer suicide prevention resources:
Suicide Prevention Lifeline
If you are suicidal, please call 988 or 800.273.TALK (8255). You’ll be connected to a skilled, trained counselor at a crisis center in your area. Counselors are available 24 hours a day, seven days a week. The Suicide Prevention Lifeline website also offers many resources for those looking for support.
American Foundation for Suicide Prevention
The American Foundation for Suicide Prevention (AFSP) is dedicated to saving lives and bringing hope to those affected by suicide.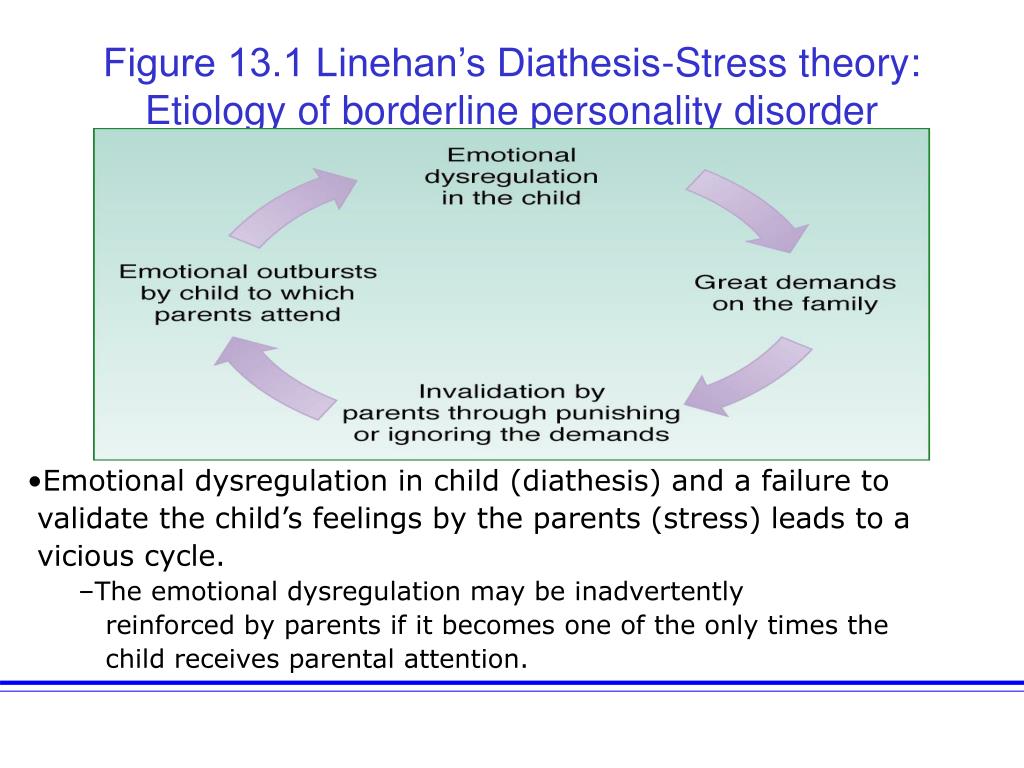 AFSP creates a culture that’s smart about mental health through education and community programs, develops suicide prevention through research and advocacy, and provides support for those affected by suicide. AFSP has local chapters in all 50 states, with programs and events nationwide.
AFSP creates a culture that’s smart about mental health through education and community programs, develops suicide prevention through research and advocacy, and provides support for those affected by suicide. AFSP has local chapters in all 50 states, with programs and events nationwide.
Samaritans: Massachusetts 24-Hour Crisis HelpLine
A non-denominational, not-for-profit volunteer organization dedicated to reducing the incidence of suicide by befriending individuals in crisis and educating the community about effective prevention strategies. The Samaritans provide a free and confidential 24-hour phone befriending line. Call or text the 24/7 statewide Helpline at 877.870.4673.
Stop A Suicide Today!
Stop A Suicide Today is a nationwide campaign by Screening for Mental Health, Inc., to empower individuals to help themselves, colleagues, friends, and loved ones who are concerned about or feel suicidal.
Suicide Prevention Resource Center
The Suicide Prevention Resource Center is the only federally supported resource center devoted to advancing the implementation of the National Strategy for Suicide Prevention.
Books About BPD
Topics
- Borderline Personality Disorder
- DBT
BPD-24, BPD-40 power unit - NPO Promavtomatika, Yekaterinburg
| specifications | BPD-24 | BPD-40 |
| output voltage, V | 24 | 36 |
| voltage Uxx at intrinsically safe input | - | - |
| allowed | +0. | +0.1 |
| output ripple | 0.25 | 0.1 |
| input signal measurement range, mA | - | - |
| output signal measurement range, mA | - | - |
| conversion error, % | - | - |
| | 50 | 50 |
| protection operation current, mA |
|
|
| short circuit | 50 | 45 |
| at overload | 80 | 80 |
Benefits
- indication of switching on and presence of supply voltage - each channel of blocks BPD-24, BPD-40 is a converter of AC voltage into a stabilized DC voltage
- protection against short circuit and overload of the supply circuit
Brief description
Number of channels: 2 or 4 galvanically isolated channels
Ambient parameters:
- for BPD-24: temperature -30.
 ..+50°C / humidity up to 80% at 25°C (UHL4.2)
..+50°C / humidity up to 80% at 25°C (UHL4.2) - for BPD-40: temperature -10...+60°C/humidity up to 80% at 25°C (UHL4.2)
Housing protection: dust and moisture protection - IP30 version / vibration resistance - L3 version
Delivery version:
- ordinary,
- export
Power: AC 220 V, 50 Hz
Power consumption:
- no more than 16 V.A (BPD-24),
- 18В.А(BPD-40)
Scope
Power supplies BPD-24 and BPD-40 are used in process control systems in metallurgy, energy, chemical, petrochemical, oil refining, food, pulp and paper and other industries. Blocks BPD-24, BPD-40 are designed to power non-explosion-proof sensors with a unified current output signal (pressure, flow, temperature, etc.)
Gabarit dimensions, drawing
Gabarit dimensions, installation
Gabarit dimensions: 72x144x180 mm
Installation: shield (cutout 70x140 mm)
are installed outside the explosive premises!
Wiring diagram
Order card
4 8 pcs.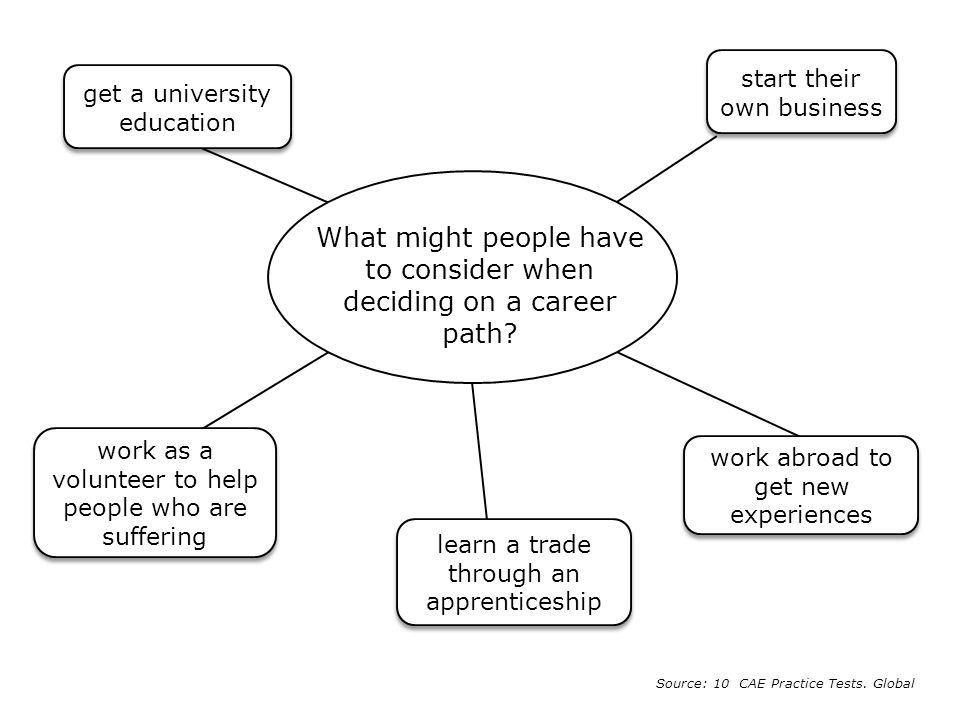
Note:
when supplying power supplies outside the CIS, the following must be indicated in the order: execution according to the terms of delivery for export
Explosion-proof sound detector IZV-301
- home
- Control and signaling devices
- Explosion-proof sound detector IZV-301
Explosion-proof sound detector IZV-301 (hereinafter referred to as the detector) is designed for alarm signaling in fire and explosion hazardous industries in all industries.
Principle of operation
The principle of operation of the detector is to generate an electrical sound frequency signal and convert it into vibrations of a piezoelectric sound emitter.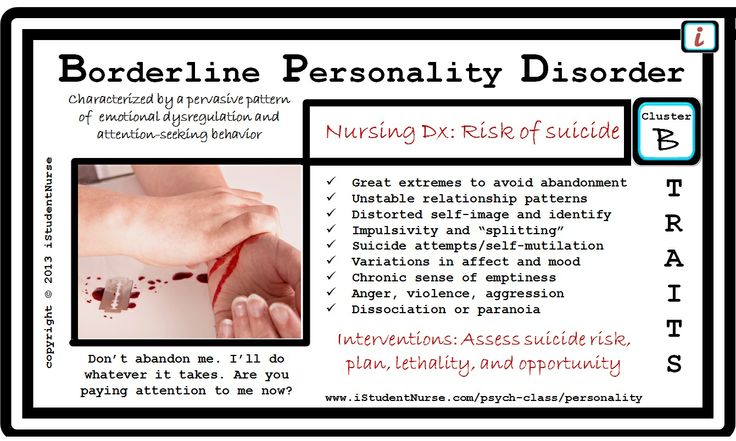
Versions
The detector is available in three versions:
| Product code | Type of protection | Explosion protection marking | Supply voltage | Power consumption, W |
| IZV-301-1 | Flameproof enclosure | 1ExdIICT6 | = 16 ÷ 30 V | Max. 6 |
| IZV-301-2 | ≈ 220 V, 50 Hz | Max. 15 | ||
| IZV-301-I | intrinsically safe electrical circuit | 0ExiaIICT5X | = 12 ± 2 V | Max. 0.5 |
Specifications
The detector belongs to the audible signaling devices for non-verbal messages according to GOST 21786-81.
Technical characteristics of detectors IZV-301-1 and IZV-301-2:
- intermittent signal with a carrier frequency of 2000 Hz, with an interval duration of 0.
 2 ÷ 0.8 s;
2 ÷ 0.8 s; - alarm sound pressure level at a distance of 1 m from the detector is not less than 100 dB at a supply voltage of 26 V DC for IZV-301-1 and 220 V AC for IZV-301-2.
Technical characteristics of the IZV-301-I detector:
- intermittent signal with a carrier frequency (3500 ± 15%) Hz at intervals of 0.2 - 1.5 s;
- alarm sound pressure level at a distance of 1 m from the detector is not less than 100 dB at a supply voltage of 14 V DC.
In explosive areas of premises and outdoor installations, the IZV-301-I detector is powered by a voltage of (12 ± 2) V DC from intrinsically safe circuits of barriers (blocks) having the type of explosion protection "intrinsically safe electrical circuit" with the explosion protection level of the intrinsically safe circuit "ia" for explosive mixtures corresponding to the subgroup of explosion-proof equipment IIC. The intrinsic safety of electrical circuits must be achieved by limiting the current (I short circuit ≤ 25 mA) and voltage (U x.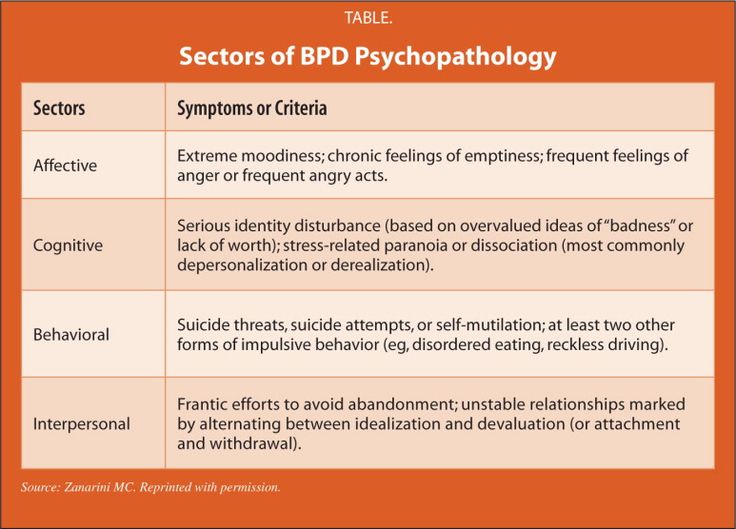 x ≤ 14 V) to intrinsically safe values. It is recommended to use the intrinsically safe signal-blocking module MSBI-302.
x ≤ 14 V) to intrinsically safe values. It is recommended to use the intrinsically safe signal-blocking module MSBI-302.
Degree of protection of the detector against ingress of solid bodies and water - IP54 according to GOST 14254-96.
Overall dimensions of IZV-301-1 and IZV-301-2 detectors are shown in Figure 1, IZV-301-I - in Figure 2.
- Detector weight:
- IZV-301-1 - no more than 1.1 kg;
- IZV-301-2 - no more than 1.4 kg;
- IZV-301-I - no more than 0.5 kg.
Explosion protection
IZV-301-1, IZV-301-2 detectors have an explosion-proof level of explosion protection, type of protection "explosion-proof enclosure", explosion protection marking 1ExdIIST6, complies with the requirements of GOST 30852.0-2002, GOST 30852.1-2002.
IZV-301-I detector has the type of explosion protection "intrinsically safe electrical circuit", explosion protection marking 0ЕхiaIICT5X, complies with GOST 30852.0-2002, GOST 30852. 10-2002.
10-2002.
The detector complies with the requirements of the "General rules of explosion safety for explosive chemical, petrochemical and oil refining industries" PB 09-540-03 and is suitable for use in automatic emergency protection systems (EPS).
The detectors can be used in explosive areas of all classes of premises and outdoor installations according to Ch. 7.3 PUE and Ch. 3.4 PTEEP.
Installation and operation
Operating conditions:
- ambient temperature for IZV-301-1 and IZV-301-2 - from minus 50 °C to plus 50 °C;
- ambient temperature for IZV-301-I - from minus 35 °С to plus 75 °С;
- 95% relative humidity at 35°C or lower, non-condensing;
- sinusoidal vibration in the frequency range from 10 to 55 Hz with a displacement amplitude of 0.35 mm.
Installation dimensions of IZV-301-1 and IZV-301-2 are shown in fig. 1.
Installation dimensions of IZV-301-I are shown in fig. 2.
Electrical installation of IZV-301-1 and IZV-301-2 is carried out with a 3x0.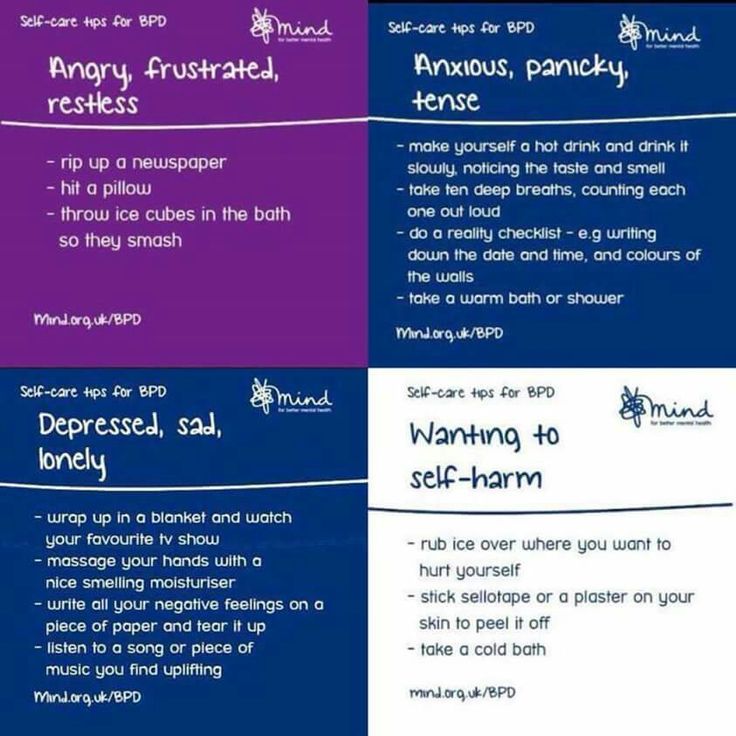 35 mm2 MKSH cable in accordance with the diagrams shown in fig. 3. Installation of the cable is carried out in a water and gas pipe with a diameter of 3/4", which is connected to the detector by means of a coupling in accordance with GOST 8954 with a conditional passage Dу=20 mm. shown in Fig. 4.
35 mm2 MKSH cable in accordance with the diagrams shown in fig. 3. Installation of the cable is carried out in a water and gas pipe with a diameter of 3/4", which is connected to the detector by means of a coupling in accordance with GOST 8954 with a conditional passage Dу=20 mm. shown in Fig. 4.
Manufacturer's warranty
Warranty period of storage - 3 years.
Warranty period - 18 months.
Completeness
Delivery set includes:
- Explosion-proof sound detector IZV-301-1 or IZV-301-1 or IZV-301-I - 1 pc.
- set of mounting parts (for IZV-301-1 and IZV-301-2) - 1 set.
- instruction manual - 1 copy.
- passport - 1 copy.
An example of a designation entry when ordering
- a detector with a supply voltage of 16 ÷ 30 V DC:
"Explosion-proof sound detector IZV-301-1 SELHA0.239.001 TU".
Overall and mounting dimensions IZV-301-1 and IZV-301-2
Figure 1
Figure 2
Figure 3
Figure 4
53
Permits
Certificate of ConformityNo.
 5
5