Different types of ssris
Overview - SSRI antidepressants - NHS
Selective serotonin reuptake inhibitors (SSRIs) are a widely used type of antidepressant.
They're mainly prescribed to treat depression, particularly persistent or severe cases, and are often used in combination with a talking therapy such as cognitive behavioural therapy (CBT).
SSRIs are usually the first choice medicine for depression because they generally have fewer side effects than most other types of antidepressant.
As well as depression, SSRIs can be used to treat a number of other mental health conditions, including:
- generalised anxiety disorder (GAD)
- obsessive compulsive disorder (OCD)
- panic disorder
- severe phobias, such as agoraphobia and social phobia
- bulimia
- post-traumatic stress disorder (PTSD)
SSRIs can sometimes be used to treat other conditions, such as premenstrual syndrome (PMS), fibromyalgia and irritable bowel syndrome (IBS). Occasionally, they may also be prescribed to treat pain.
How SSRIs work
It's thought that SSRIs work by increasing serotonin levels in the brain.
Serotonin is a neurotransmitter (a messenger chemical that carries signals between nerve cells in the brain). It's thought to have a good influence on mood, emotion and sleep.
After carrying a message, serotonin is usually reabsorbed by the nerve cells (known as "reuptake"). SSRIs work by blocking ("inhibiting") reuptake, meaning more serotonin is available to pass further messages between nearby nerve cells.
It would be too simplistic to say that depression and related mental health conditions are caused by low serotonin levels, but a rise in serotonin levels can improve symptoms and make people more responsive to other types of treatment, such as CBT.
Doses and duration of treatment
SSRIs are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
SSRIs usually need to be taken for 2 to 4 weeks before the benefit is felt. You may experience mild side effects early on, but it's important that you don't stop taking the medicine. These effects will usually wear off quickly.
If you take an SSRI for 4 to 6 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying an alternative antidepressant.
A course of treatment usually continues for at least 6 months after you feel better, although longer courses are sometimes recommended and some people with recurrent problems may be advised to take them indefinitely.
Things to consider
SSRIs aren't suitable for everyone. They're not usually recommended if you're pregnant, breastfeeding or under 18, because there's an increased risk of serious side effects. However, exceptions can be made if the benefits of treatment are thought to outweigh the risks.
However, exceptions can be made if the benefits of treatment are thought to outweigh the risks.
SSRIs also need to be used with caution if you have certain underlying health problems, including diabetes, epilepsy and kidney disease.
Some SSRIs can react unpredictably with other medicines, including some over-the-counter painkillers and herbal remedies, such as St John's wort. Always read the information leaflet that comes with your SSRI medicine to check if there are any medicines you need to avoid.
Side effects
Most people will only experience a few mild side effects when taking SSRIs. These can be troublesome at first, but they'll generally improve with time.
Common side effects of SSRIs can include:
- feeling agitated, shaky or anxious
- diarrhoea and feeling or being sick
- dizziness
- blurred vision
- loss of libido (reduced sex drive)
- difficulty achieving orgasm during sex or masturbation
- in men, difficulty obtaining or maintaining an erection (erectile dysfunction)
You'll usually need to see your doctor every few weeks when you first start taking SSRIs to discuss how well the medicine is working. You can also contact your doctor at any point if you experience any troublesome or persistent side effects.
You can also contact your doctor at any point if you experience any troublesome or persistent side effects.
Types of SSRIs
There are currently 8 SSRIs prescribed in the UK:
- citalopram (Cipramil)
- dapoxetine (Priligy)
- escitalopram (Cipralex)
- fluoxetine (Prozac or Oxactin)
- fluvoxamine (Faverin)
- paroxetine (Seroxat)
- sertraline (Lustral)
- vortioxetine (Brintellix)
Page last reviewed: 8 December 2021
Next review due: 8 December 2024
SSRIs: Uses, Side-Effects, and Cessation
Written by Matthew Hoffman, MD
In this Article
- How Do SSRIs Work?
- Types of SSRIs
- Side Effects
- How Long Do They Take to Work?
- Stopping Treatment
Everyone feels down from time to time. But for people with depression, the feelings of sadness can be so severe that they interfere with everyday life. It can become hard to function at home or at work, and the feelings can lead to a variety of physical and emotional problems.
But for people with depression, the feelings of sadness can be so severe that they interfere with everyday life. It can become hard to function at home or at work, and the feelings can lead to a variety of physical and emotional problems.
However, depression is one of the most treatable mental disorders. Between 80% and 90%of people who have it benefit from treatment. The kind of management you need depends on your specific situation, but for some people, medication can be very helpful.
That’s because brain chemistry may contribute to the condition, so taking antidepressants can actually change your brain chemistry and help you feel better.
The most common antidepressants are called selective serotonin reuptake inhibitors (SSRIs). They’re considered relatively safe and cause fewer side effects than other kinds of medications used to treat depression.
How Do SSRIs Work?
SSRIs work by enhancing the function of nerve cells in the brain that regulate emotion. Information is communicated between your brain cells with signals. The chemical messengers that deliver these signals are called neurotransmitters. Serotonin is one type of neurotransmitter.
Information is communicated between your brain cells with signals. The chemical messengers that deliver these signals are called neurotransmitters. Serotonin is one type of neurotransmitter.
When these brain cells (called neurons) send signals to one another, they release a little bit of a neurotransmitter so that the message can be delivered. They then have to take back the neurotransmitter they released so they can send the next message. This process of replacing the neurotransmitter is called “reuptake.”
If you’re struggling with depression, the areas of your brain that regulate mood and send messages using serotonin might not function properly. SSRIs help make more serotonin available by blocking the reuptake process. This allows serotonin to build up between neurons so messages can be sent correctly. They’re called “selective” serotonin reuptake inhibitors because they specifically target serotonin.
Types of SSRIs
The FDA is in charge of deciding which medications are safe and effective for which reasons. The following SSRIs are approved to treat depression, anxiety, and other mood disorders:
The following SSRIs are approved to treat depression, anxiety, and other mood disorders:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox, Luvox CR)
- Paroxetine (Paxil, Paxil CR)
- Sertraline (Zoloft)
Vilazodone (Viibryd)
Side Effects
Most people who use SSRI antidepressants don’t have major problems, but every kind of medical treatment carries some risk. The possible side effects of these antidepressants include:
- Insomnia
- Headaches
- Rash
- Blurred vision
- Drowsiness
- Dry mouth
- Agitation or nervousness
- Feeling dizzy
- Pain in the joints or muscles
- Upset stomach, nausea, or diarrhea
- Reduced sexual desire
- Problems with erection or ejaculation
Some people, especially children and young adults, may be more likely to have suicidal thoughts when they take SSRIs. Studies show that when compared to results from taking a placebo, chances of having suicidal thoughts doubled -- from between 1% and 2% to between 2% and 4% -- when taking any kind of antidepressant, including an SSRI. If you have thoughts of hurting yourself while taking an SSRI, call 911.
If you have thoughts of hurting yourself while taking an SSRI, call 911.
There are also important safety issues to consider about SSRIs. Although it’s rare, if too much serotonin accumulates in your system, you can develop a condition called serotonin syndrome. This happens most often if two different medications that increase serotonin are combined.
SSRIs can also have dangerous interactions with some medicines, both prescription and over-the-counter, including herbs and supplements. Before starting on an SSRI, make sure to tell your doctor all the different kinds of medications and supplements you're taking.
Since all SSRIs work in a similar way, the side effects tend to be similar no matter what kind you take. But each SSRI has a different chemical makeup, so it’s possible that if you’re having side effects from one, you may not experience as many or any at all if you switch to another.
While some people do have side effects, others do not, and in many cases, the side effects disappear after a few weeks of treatment. It’s important to work with your doctor to find a medication that’s right for you.
It’s important to work with your doctor to find a medication that’s right for you.
How Long Do They Take to Work?
Everyone is different when it comes to seeing improvements on SSRIs. But people typically start noticing positive changes after about 4 to 6 weeks of treatment. It can take several months to feel the full effect of the medication.
But if you’re not feeling any improvements after about 6 to 8 weeks, talk to your doctor about trying another treatment or adjusting your dosage.
Stopping Treatment
Even though SSRIs aren’t habit-forming, it can be dangerous to stop them suddenly or miss several doses in a row. Doing this can lead to a condition called discontinuation syndrome that causes withdrawal-like symptoms.
If you do experience discontinuation syndrome, you might start to feel like you have the flu and/or notice symptoms like:
- Nausea
- Dizziness
- Uneasiness
- Fatigue or lethargy
That’s why it’s important to work up to your prescribed dosage slowly with the help of your doctor, and to step down gradually if you agree it’s time to stop.
Depression. Serotonin. Myths. - Articles
Science and Society
Natallia Niachai
2093 views
Over the years I have discovered something very strange in the antidepressant literature. When antidepressants are compared, their effects are remarkably similar. I first noticed this when Guy Sapirstein and I conducted our meta-analysis of the published literature in 1998. When we first saw how weak the actual effect of drugs was, we thought we might be doing something wrong. We may have made a mistake and included tests that evaluated different types of antidepressants. We may have underestimated the actual effectiveness of antidepressants by including clinical trials of less effective drugs. Next, we will continue to talk about depression, serotonin and myths about them.
Before publishing our work for publication, we went back to the data and checked the type of antidepressant used in each test: some were selective serotonin reuptake inhibitors (SSRIs), others were tricyclic drugs; we called those antidepressants that were neither SSRIs nor tricyclides "other antidepressants. " We then found that in the analyzes we analyzed, there was a fourth category of drugs that were administered to patients with depression and assessed for their effect on depression that were not considered at all, such as tranquilizers and thyroid medications. When we analyzed drug and placebo responses for each type of drug, another surprise awaited us: It did not matter what type of drug the patient received in the test, the response was always the same , and a 75% response was also found in the placebo groups. I remember being struck by the similarity of the results, but I have since learned that this is not unusual at all. Further, I found this phenomenon again and again. In the STAR*D study, the most expensive US$35 million clinical trial of antidepressants, patients who did not respond to their prescribed SSRIs were given a different drug.
" We then found that in the analyzes we analyzed, there was a fourth category of drugs that were administered to patients with depression and assessed for their effect on depression that were not considered at all, such as tranquilizers and thyroid medications. When we analyzed drug and placebo responses for each type of drug, another surprise awaited us: It did not matter what type of drug the patient received in the test, the response was always the same , and a 75% response was also found in the placebo groups. I remember being struck by the similarity of the results, but I have since learned that this is not unusual at all. Further, I found this phenomenon again and again. In the STAR*D study, the most expensive US$35 million clinical trial of antidepressants, patients who did not respond to their prescribed SSRIs were given a different drug.
Some switched to SNRI, a drug thought to increase both norepinephrine and serotonin in the brain; others have switched to NDRI, which is said to increase norepinephrine and dopamine without affecting serotonin. And other patients were simply given another SSRI. Approximately one in four patients had a clinical reaction to a new drug, but it did not matter which new drug it was. The effect was 26% to 28%; in other words, 90,011 patients responded the same regardless of drug type.
And other patients were simply given another SSRI. Approximately one in four patients had a clinical reaction to a new drug, but it did not matter which new drug it was. The effect was 26% to 28%; in other words, 90,011 patients responded the same regardless of drug type.
The most commonly prescribed antidepressants are SSRIs, which are believed to selectively affect the neurotransmitter serotonin. However, there is an antidepressant that works in a completely different way. It is tianeptine and has been approved by the French Medicines Registry for prescription as an antidepressant. Tianeptine is an SSRis, a selective serotonin reuptake enhancer that, instead of increasing the amount of serotonin in the brain, decreases it.
If the theory is that depression is caused by a deficiency of serotonin , the depression may worsen. However, this is not so, one of the myths. In clinical trials comparing tianeptine with SSRis and tricyclic antidepressants, 63% of patients showed a significant improvement (arbitrarily defined as a 50% reduction in symptoms), i. e. the same reaction rate as found in this type of testing with SSRis, NDRis and tricyclides (see Figure 5). It just doesn't matter what the drug contains - whether it increases or decreases serotonin, or does not affect serotonin at all. The effect on depression remains the same.
e. the same reaction rate as found in this type of testing with SSRis, NDRis and tricyclides (see Figure 5). It just doesn't matter what the drug contains - whether it increases or decreases serotonin, or does not affect serotonin at all. The effect on depression remains the same.
What would you call pills that work regardless of their chemical composition? I call them "placebos".
Antidepressants as active placebos
All antidepressants appear to be equally effective, and although the difference between medication and placebo is not clinically significant, it is statistically significant. Thus, the question arises: what do all these active drugs have in common that their effect on depression is small, but statistically significantly better than placebo?
A common feature of all antidepressants is that they cause side effects. Why is this important? Imagine that you are a subject in a clinical trial. You are told that this is a double-blind study and that you can get a placebo. They will also tell you what the side effects of the medication are. The therapeutic effect of the drug can be felt only after a few weeks, however, side effects may appear faster. Will you wonder if you were placed in the drug or placebo group, and if you experience any of the listed side effects, will you conclude that you received the real drug? In one study 89% of depressed patients in the antidepressant drug group correctly "guessed" that they were receiving a real antidepressant (Rabkin et al., 1986), and in another study in which antidepressants and benzodiazepines were used to treat panic disorders, group with the active drug were also correctly "guessed" which group they belonged to (Margraf et al., 1991).
You are told that this is a double-blind study and that you can get a placebo. They will also tell you what the side effects of the medication are. The therapeutic effect of the drug can be felt only after a few weeks, however, side effects may appear faster. Will you wonder if you were placed in the drug or placebo group, and if you experience any of the listed side effects, will you conclude that you received the real drug? In one study 89% of depressed patients in the antidepressant drug group correctly "guessed" that they were receiving a real antidepressant (Rabkin et al., 1986), and in another study in which antidepressants and benzodiazepines were used to treat panic disorders, group with the active drug were also correctly "guessed" which group they belonged to (Margraf et al., 1991).
Not only do patients recognize the distribution in the appropriate group, but also practitioners who rate them on the HAM-D scale (Margraf et al., 1991; Rabkin et al., 1986). Patients with the real drug "guess" pretty well that they are in the drug group, but those in the placebo group are much more accurate.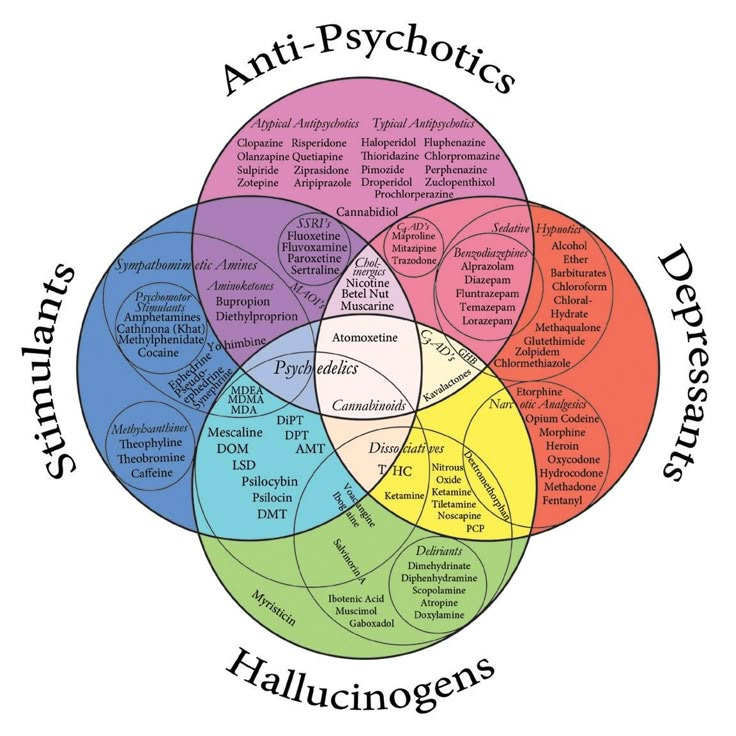 On the other hand, clinicians very accurately recognize the distribution of patients in both the drug and placebo groups. Clinician reports were taken in all antidepressant tests as the primary result for submission to the FDA. The use of scales on which patients rate their depressive symptoms may provide more accurate estimates of the difference between a drug and placebo. In other words, clinical trials are not bilaterally secret. Many patients realize this when they are given the real drug, as do clinicians who assess depression, is most likely due to the side effects of the drugs. What are the possible effects of antidepressants?
On the other hand, clinicians very accurately recognize the distribution of patients in both the drug and placebo groups. Clinician reports were taken in all antidepressant tests as the primary result for submission to the FDA. The use of scales on which patients rate their depressive symptoms may provide more accurate estimates of the difference between a drug and placebo. In other words, clinical trials are not bilaterally secret. Many patients realize this when they are given the real drug, as do clinicians who assess depression, is most likely due to the side effects of the drugs. What are the possible effects of antidepressants?
We don't have to guess. Bret Rutherford and his colleagues at Columbia University provided the answer. They tested response to antidepressants using studies without a placebo group versus studies with a placebo group (Rutherford, Sneed & Roose, 2009). The main difference was that in the first case, the patients and classifiers were confident that the patients were being given an active antidepressant, while in the placebo-controlled trials they knew they could have received a placebo. Knowing that all patients were receiving the active drug greatly increased its effectiveness. This supports the hypothesis that the relatively small difference between medication and placebo in antidepressant tests is due, at least in part, to "guessing" which group the patient belongs to and therefore knowing that the patient is in the medication group. Due to side effects caused by the drug.
Knowing that all patients were receiving the active drug greatly increased its effectiveness. This supports the hypothesis that the relatively small difference between medication and placebo in antidepressant tests is due, at least in part, to "guessing" which group the patient belongs to and therefore knowing that the patient is in the medication group. Due to side effects caused by the drug.
What to do?
Thus, there is a strong therapeutic effect on antidepressants. However, placebo response is almost as strong . This leads to a therapeutic dilemma. The medicinal effect of antidepressants is not clinically significant, but there is a placebo effect. Given these results, what should be done clinically?
One option would be to give a placebo, but that would be a scam. In addition to being ethically questionable, there is also the risk of breaching trust, and trust is one of the most important clinical tools that clinicians have. Another suggestion was to use antidepressants as the active placebo. But this alternative is problematic because of the risks associated with antidepressants.
Another suggestion was to use antidepressants as the active placebo. But this alternative is problematic because of the risks associated with antidepressants.
Side effects of antidepressants include
Side effects of antidepressants include : Sexual dysfunction (which may affect 70% to 96% of patients receiving SSRI; Clayton et al., 2006; Serretti et al., 2009), large, 2009 weight gain, insomnia, nausea and diarrhea.
Many people who want to stop taking antidepressants experience withdrawal symptoms (Rosenbaum et al., 1998).
Antidepressants have also been associated with increased rates of suicide, violence and crime in children, adolescents and young adults (Molero et al., 2015; Stone, 2014; Stone et al., 2009).
Older people have an increased risk of stroke, as well as the risk of all possible health problems that will be fatal (Andrews et al., 2012).
Pregnant women taking antidepressants are at greater risk of miscarriage and their children are more likely to be born with autism, birth defects, and chronic pulmonary hypertension (Dolmar et al. , 2013). In addition, some of these risks are associated with taking antidepressants in early pregnancy, when women do not yet know they are pregnant.
, 2013). In addition, some of these risks are associated with taking antidepressants in early pregnancy, when women do not yet know they are pregnant.
However, one of the most surprising health effects of antidepressant use affects all age groups: antidepressants increase the risk of relapse . After treatment with antidepressants, the likelihood of recurrent depression is much higher than with treatment with other agents, including treatment with placebo (Andrews et al., 2012; Babyak et al., 2000; Dobson et al., 2008). The risk of relapse depends on the degree of neurotransmitter change in the brain caused by the respective antidepressant.
Given these health risks, antidepressants should not be used as the first choice in the treatment of depression. The best alternative is to use non-drug treatments. My colleagues and I conducted a meta-analysis of various treatments for depression, including antidepressants, psychotherapy, a combination of psychotherapy and antidepressants, and “alternative” forms of treatment, including acupuncture and physical training (Khan et al. , 2012; see Fig. 6) .
, 2012; see Fig. 6) .
We found no significant differences between these treatments and various approaches to psychotherapy. When different treatments are equally effective, the choice must be made in terms of risk and harm, with antidepressants are the most risky and destructive of all these treatments (this is not a myth and serotonin has nothing to do with it) . If anything, they should be used as a last resort if the depression is extremely severe and all other treatment options have been tried and failed.
The best researched alternative to antidepressants is cognitive behavioral therapy. For short-term use, it is just as effective, although more expensive, than drug therapy. In the long term, however, it is more effective and less expensive than pharmacotherapy (Dobson et al., 2008). Patients with depression also prefer cognitive behavioral therapy to pharmacotherapy in a 3:1 ratio (McHugh et al., 2013). Finally, there is evidence that hypnosis, in addition to behavioral therapy, can increase its effectiveness (Alladin, 2013; Kirsch et al. , 1995) and that hypnosis treatment is clearly preferable to antidepressant treatment (Dobbin et al., 2009).
, 1995) and that hypnosis treatment is clearly preferable to antidepressant treatment (Dobbin et al., 2009).
Irwin Kirsch
In the Freud's Heritage club, at your request, we will create a therapeutic group using the method of cognitive behavioral therapy (psychologist Dmitry Korenev) in tandem with other methods of psychology (club psychologists) and body-oriented practices (Mikhail Grishchenko).
Find article
Areas of life
Self-knowledge (44)
Children. From 0 to 18 (12)
Career (28)
Relationships (136)
Compatibility (30)
Love stories (47)
Health and body (110)
9002 90Science and society (120)
Personality types (25)
From the life of Freud's legacy (10)
are ssris - Translation into Russian - examples English
Premium History Favorites
Advertising
Download for Windows It's free
Download our free app
Advertising
Advertising
No ads with Premium
English
Arabic German English Spanish French Hebrew Italian Japanese Dutch Polish Portuguese Romanian Russian Swedish Turkish Ukrainian Chinese
Russian
Synonyms Arabic German English Spanish French Hebrew Italian Japanese Dutch Polish Portuguese Romanian Russian Swedish Turkish Ukrainian Chinese Ukrainian
Suggestions: are serious are risks are strict are risk are sisters
These examples may contain rude words based on your search.
These examples may contain colloquial words based on your search.
ssris
SSRIs SSRI SSRIs antidepressants serotonin
So are SSRIs to be shunned or saluted?
Saving Yaroslav : pattern or luck?
"This may be clinically significant for people because almost a quarter of middle-aged women in the United States take antidepressants, the most prescribed of which are SSRIs ."
This may be clinically significant in humans because nearly a quarter of middle-aged women in the US are taking antidepressants, the most commonly prescribed being are SSRIs ."
The drugs of first choice are SSRIs .
First choice drugs - loop .
Why are SSRIs so similar?
Why are REE so similar?
These are ssris . They've been effective in treating OCD.
These are selective serotonin reuptake inhibitors they have shown to be effective in the treatment of obsessive compulsive disorder
Other results
Otherwise, SSRIs are often the initial drugs of choice.
On the other hand, SSRIs are often prescribed as first choice drugs.
All the active metabolites are also SSRIs , although weaker than the parent compound.
All active metabolites are also SSRI , although weaker than the parent compound.
Some children with ASD who are taking SSRIs can suddenly have a sharp rise in serotonin levels.
Some children with ASD who are taking SSRI may experience a sudden increase in serotonin levels.
Atypical antidepressants are non- SSRI and non-TCA antidepressants that work by distinct pharmacodynamic mechanisms.
Atypical antidepressants are not are SSRIs and non-TCA antidepressants that work by different pharmacodynamic mechanisms.
Treatment: the SSRIs are the agents of choice in treating social phobia, although MAOIs and BZs are also effective.
Treatment: SSRIs are the agents of choice in the treatment of social phobia, although MAOIs and BZs are also effective.
SSRIs are drugs used to modify behavior.
Antidepressants - behavioral drugs.
Experts say that SSRIs are not only very effective in treating depression; they also have fewer side-effects than the other types.
Experts say SSRIs are not only very effective in treating depression; they also have fewer side effects than other types.
Eminent psychologist Irving Kirsch has found that for many patients, SSRIs are no more effective than a placebo pill.
And the famous psychologist Irving Kirsch found that for many patients SSRIs are not more effective than placebo pills.
However, the two most dangerous side effects of SSRIs are birth defects and suicide.
However, the two most dangerous side effects of SSRIs are birth defects and suicide.
SSRIs are used for long-term anxiety treatment and are generally prescribed for one year or more.
SSRIs are used by to manage long-term anxiety and are typically prescribed for one year or more.
SSRIs are designed to increase serotonin levels in the brain by preventing its reabsorption.
SSRIs are designed to increase serotonin levels in the brain by preventing its reabsorption.
SSRIs are usually prescribed to those who have not had an improvement after taking tricyclic antidepressants.
As a rule, MAOIs are prescribed for those patients who have not improved after a course of treatment with tricyclic antidepressants.
SSRIs are the most common type of antidepressant prescribed in Sweden.
SSRI is the most commonly used type of antidepressant in Sweden.
And SSRIs are usually the drug of choice.
SSRIs are generally the drugs of choice.
SSRIs are the first line treatment for severe PMT or PMDD.
SSRIs are the first line treatment for severe PMS or PMDD.
Possibly inappropriate content
Examples are used only to help you translate the word or expression searched in various contexts. They are not selected or validated by us and can contain inappropriate terms or ideas. Please report examples to be edited or not to be displayed. Rude or colloquial translations are usually marked in red or orange.
Register to see more examples It's simple and it's free
Register Connect
No results found for this meaning.