Cleaning anxiety symptom
Understanding OCD and Cleaning
You like your kitchen sink to shine, and your stove can never be clean enough. Does that mean you have obsessive-compulsive disorder (OCD)?
Answering that question requires a deeper look into what OCD is — and why some people with OCD are compelled to clean.
The relationship between OCD and cleaning hinges on obsession (recurrent, intrusive thoughts) and compulsion (repeated behaviors or actions).
Obsessions and compulsions intertwine in OCD, and they can drive an overwhelming desire to repeatedly clean things.
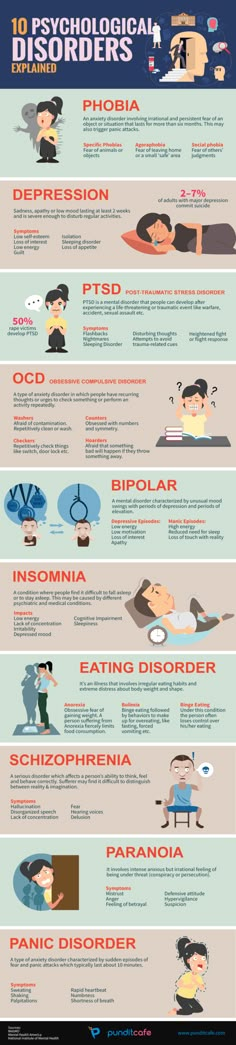
The new edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is an authoritative guide to psychological conditions. It describes OCD as a disorder that causes people to experience distressing thoughts and mental images that won’t go away.
In response to these unwanted thoughts, people with OCD may feel an intense urge to repeat certain actions. The actions may be physical behaviors (such as arranging objects in a particular order) or mental ones (like praying in a particular way).
Some people feel that completing these actions will neutralize a threat, make an obsessive thought stop, or relieve the anxiety that unwanted thoughts create.
DSM-5 emphasizes that compulsive acts can take up a lot of time. They can disrupt a person’s social, academic, or professional life. The need to precisely perform rituals and compulsive acts can cause serious anxiety.
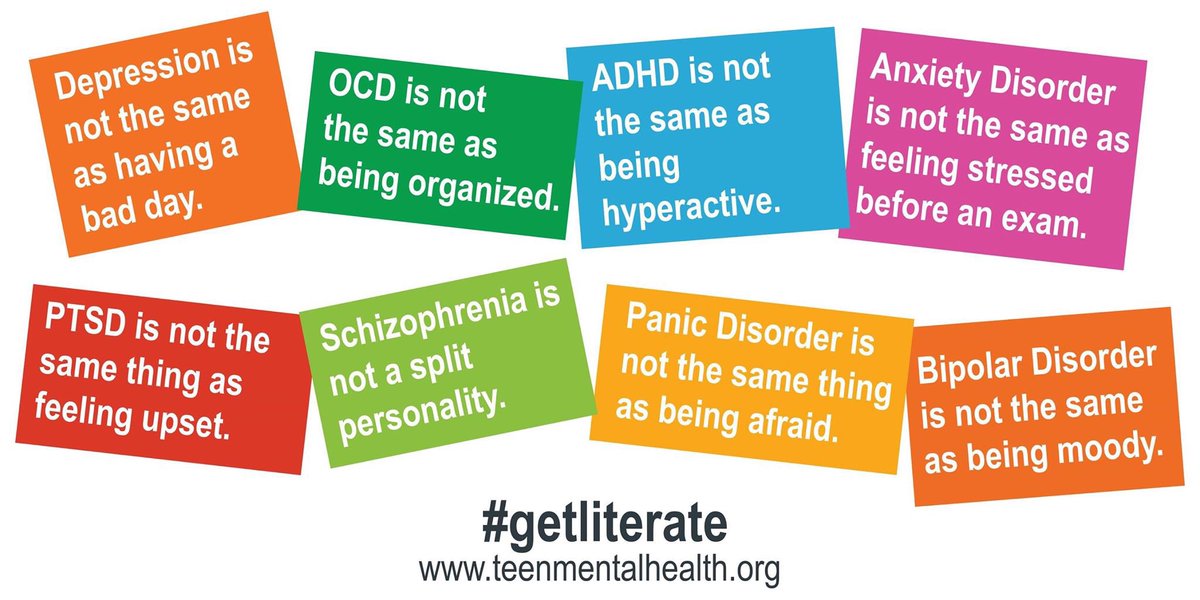
OCD, then, is much more than a desire to work or live in a clean environment or a preference for neatness. It involves a sometimes debilitating and distressing need to clean and reclean specific areas or items.
Although DSM-5 doesn’t list subtypes of OCD, some researchers group obsessions and compulsions into “symptom dimensions.” These clusters of symptoms share similar anxieties and behavior patterns.
Here’s a brief look at the symptom dimensions as currently described in scientific literature:
Contamination and cleaning
Some people have an extreme fear of becoming contaminated by germs, bodily fluids, or other substances — including abstract contaminants like evil or bad luck. People may even fear that they’re contaminating others.
People may even fear that they’re contaminating others.
An obsession with contamination can lead to a cleaning compulsion. People may believe that by cleaning objects or spaces in a specific order or with a particular frequency, they can avoid or recover from contamination or infection.
Symmetry and ordering
Some people become preoccupied with arranging objects in a certain order, often because of a kind of magical thinking or magical ideation. For example, individuals with OCD may think, “If I don’t line up my toiletries exactly this far apart, someone is going to harm me today, or if I clean my sink five times this morning, my brother won’t get sick today.”
Researchers have found that people with symmetry obsession and an ordering compulsion often have trouble expressing anger in healthy ways and may have a personal history of trauma.
Doubt about harm and checking
Some people have intrusive thoughts and fears about harming others or being harmed themselves. An excessive dread of being responsible for harm can lead to compulsive checking behaviors — for example, repeatedly making sure you’ve turned off the stove or an iron.
An excessive dread of being responsible for harm can lead to compulsive checking behaviors — for example, repeatedly making sure you’ve turned off the stove or an iron.
People affected by checking compulsions describe a feeling of incompleteness unless they perform certain rituals or behaviors. Other common compulsions include repeating mantras, prayers, or safety words to ward off danger or reduce anxiety.
Similar to symmetry and order compulsions, checking compulsions have been associated with anger and trauma.
Unacceptable thoughts and mental rituals
Some people experience frequent intrusive thoughts about things that violate their own sense of morality and goodness. Often, these unwanted thoughts involve sex, violence, or religious images.
Although people with this symptom cluster generally have no history of violence, they spend a lot of time and energy trying to suppress or erase these thoughts. Trying to squelch the thoughts can lead to even more anxiety, which tends to produce more unwanted thoughts — resulting in an unhealthy cycle.
Two of these symptom dimensions have a clear link to cleaning tasks: contamination and cleaning as well as symmetry and ordering.
You can’t prevent OCD, though doctors say an early diagnosis and intervention may mean you spend less time dealing with the difficulties this disorder can present.
About 2 percent of the general population has OCD. The disorder tends to appear at an earlier age in males. By midlife, though, more women than men have symptoms of OCD.
Here’s what we know about the risk factors, causes, and triggers of this disorder.
Genetics
Researchers continue to explore the influence of genetics on whether someone develops OCD.
As of now, scientists know that if your parent or sibling has OCD, you’re more likely to develop the condition. Some studies have found that the symptom dimensions involving OCD cleaning and ordering are especially likely to run in families.
Brain structure
Researchers are finding differences in the brain structures of people with OCD, along with differences in how their brain functions.
For example, one 2017 study found that in people with OCD, there’s greater connectivity and activity in parts of the brain associated with habit formation and in parts that process emotions — especially fear.
Brain scans also reveal differences in estrogen receptors and in the amount of white and gray matter in the brains of people with the contamination and cleaning symptom dimensions.
Understanding differences in brain structures is important because it may point to new directions for treating the condition.
Environment
Behavioral researchers have long known that stress and trauma are associated with a higher risk of developing OCD.
For example, 2015 study involving 22,084 Swedish twins indicates that two kinds of childhood trauma are particularly likely to lead to symptoms of OCD: abuse and family disruption.
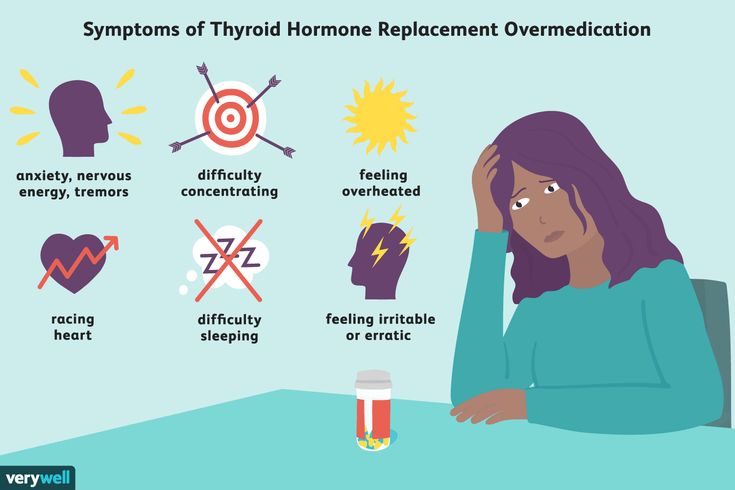
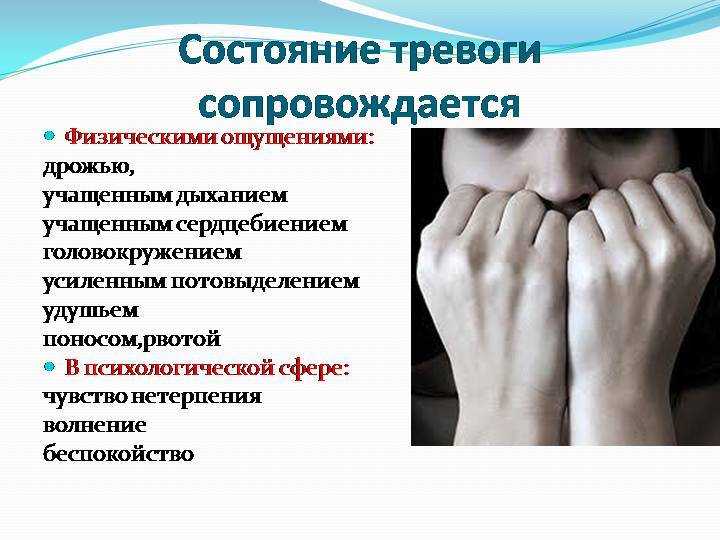
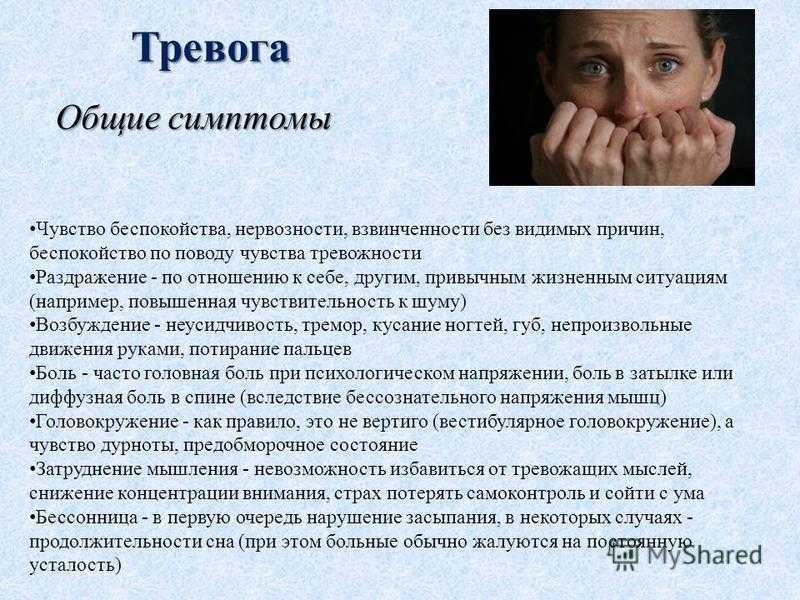
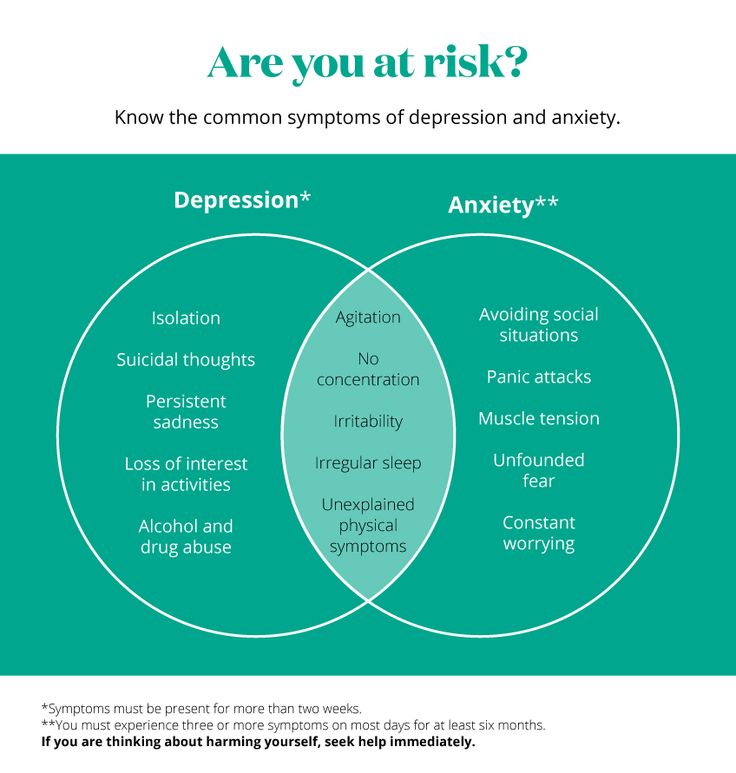
OCD symptoms include not only obsessions and compulsions, but significant anxiety as well. You may feel stressed in circumstances where you feel out of control or uncertain.
If you have OCD and contamination or cleaning are important to you, you may notice that you:
- feel disgust or fear over certain objects or substances, including dirt, illness, body secretions, trash, or chemicals
- believe you or others can be contaminated by magical or spiritual means — such as by saying certain names or numbers
- have a strong urge to wash your hands or shower frequently
- use a very specific process or ritual for washing yourself or your surroundings
- change clothes several times a day
- avoid places or people that may have been infected
- conduct precise decontaminating rituals
- refuse to allow others into your safe spaces
- damage your skin or body through excessive cleaning
If you have OCD and it’s important for you to keep things symmetrical or arranged in a precise order, you may notice that you:
- experience serious anxiety if certain things are not arranged “just right”
- feel an urge to repeat what happens to one side of your body on the other side of your body
- fear that if something is unbalanced or uneven, a catastrophe could happen
- perform touching or tapping rituals
- count things habitually
A doctor, psychologist, or psychiatrist can diagnose your condition by interviewing you about your thought and behavior patterns or by asking you about symptoms listed in DSM-5.
A physical examination could help your doctor determine whether an underlying health condition is causing your symptoms.
OCD is well researched. Doctors, psychiatrists, and psychologists have found a number of treatments that can decrease your symptoms and improve your daily functioning.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is an effective treatment for many people dealing with OCD.
In a CBT session, you meet with a therapist who can help you decrease your anxiety by identifying thought patterns that distort your view of reality and cause stress. Your therapist can then help you learn to restructure these thoughts in productive ways.
Studies have shown that CBT strengthens connections throughout your brain, especially in areas that deal with your ability to control your thinking and balance your emotions.
Online therapy options
Read our review of the best online therapy options to find the right fit for you.
Exposure and response prevention
Exposure and response prevention (ERP) is another type of therapy known to be effective in treating OCD.
In ERP, you and your therapist work together to identify external and internal triggers that cause you stress and make you want to behave compulsively.
You also describe your obsessive thoughts and your compulsive behaviors to your therapist. You explain what you fear will happen if you don’t follow through with a behavior or rituals.
Your therapist then helps you practice gradually facing stressful situations — both in your imagination and in real life — without using your compulsions.
Medication
Your doctor may prescribe an antidepressant to reduce your OCD symptoms. Some of the more common medications prescribed for OCD are:
- Anafranil
- Fluvoxamine
- Paxil
- Prozac
- Zoloft
If you take one of these medications to treat OCD, it’s important to talk to your doctor before you change your dose.
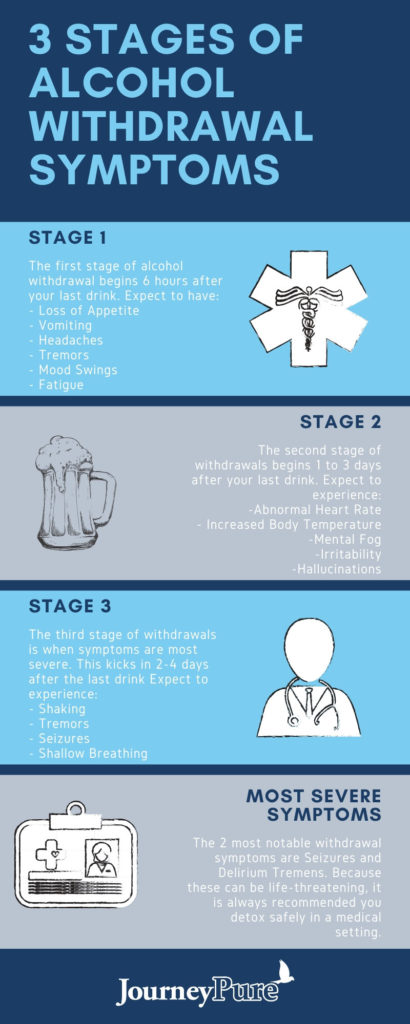
You shouldn’t stop taking your medication suddenly, because in some cases it can cause:
- a relapse of your symptoms
- serious changes in your mood
- an increased risk of suicidal thoughts
Deep brain stimulation
Your doctor may recommend deep brain stimulation (DBS) if more conservative treatment methods aren’t working for you.
During DBS, doctors implant electrodes in targeted areas of your brain. The electrodes produce electrical pulses that may help change your thoughts and behaviors.
Transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is another approach to consider if other treatments aren’t helping you.
During TMS, a doctor places an electromagnetic coil on your head. Magnetic fields interact with nerve cells in your brain in an attempt to lessen your OCD symptoms.
If you have OCD and a cleaning or ordering compulsion, your symptoms can be treated. There’s a good outlook for people who seek treatment for their OCD.
The best outcomes happen when people are diagnosed early and start a robust treatment program right away.
Sometimes OCD goes into remission on its own, especially if it initially appears during childhood. Other times people need long-term treatment to keep symptoms in check.
Being a perfectionist about cleaning doesn’t necessarily mean you have OCD. Individuals with OCD experience persistent intrusive thoughts and a compulsion to carry out certain ritualistic behaviors.
OCD produces serious anxiety. Compulsive cleaning is often related to fears of contamination, and compulsive arranging can be caused by a need for symmetry and balance.
This disorder can be treated with therapy, medications, and procedures that stimulate parts of your brain known to be affected by the disorder. If you are diagnosed early and you participate in a treatment program consistently, it’s possible you’ll be able have a good quality of life.
What Causes Compulsive Cleaning? - Renewed Freedom Center
Maintaining a clean and tidy home is usually a sign of good emotional health. When cleaning becomes obsessive, however, an underlying mental disorder may be the cause. Obsessive fears of contamination along with cleaning and sanitizing compulsions is one of many subtypes of OCD (obsessive-compulsive disorder). Obsessive compulsive cleaners are compelled to clean, spending hours every day in ritualized activities that offer only temporary relief, leaving them prisoners of their own behavior, while alienating them from friends and loved ones.
When cleaning becomes obsessive, however, an underlying mental disorder may be the cause. Obsessive fears of contamination along with cleaning and sanitizing compulsions is one of many subtypes of OCD (obsessive-compulsive disorder). Obsessive compulsive cleaners are compelled to clean, spending hours every day in ritualized activities that offer only temporary relief, leaving them prisoners of their own behavior, while alienating them from friends and loved ones.
Here is what causes this type of obsessive cleaning to take hold.
Clean Freak or Cleaning Disorder?
OCD cleaning goes beyond a simple need to maintain an orderly, hygienic home. It is a symptom of one of the many subtypes of obsessive compulsive disorder. Sufferers of compulsive cleaning may have a pervasive feeling of contamination by dirt, germs environmental contaminants, or chemical toxins. They may fear getting ill or contracting certain diseases, such as the flu, cancer, or HIV. Their compulsive cleaning may even be associated with magical thinking that if they washed/cleaned sufficiently, a negative catastrophic consequence can be avoided. Unfortunately, the compulsive cleaning is never quite sufficient, and thus, the feared consequence persists triggering further obsessive-compulsive cleaning.
Unfortunately, the compulsive cleaning is never quite sufficient, and thus, the feared consequence persists triggering further obsessive-compulsive cleaning.
The OCD Cycle
In order to understand why people clean obsessively, it’s important to know the OCD cycle.
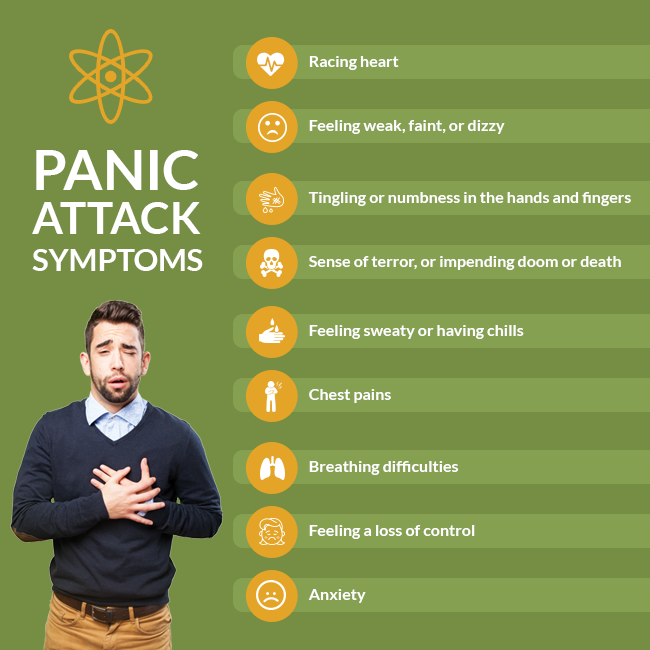
1. Obsessions
The obsession is an involuntary and intrusive thought or sensation. It triggers cleaning behavior by bombarding the OCD sufferer with fears that a particular surface or object is somehow contaminated or wrong.
2. Anxiety
The obsessive thought leads to a build-up of unbearable anxiety.
3. Compulsive Behavior
In order to alleviate anxiety, the individual resorts to their compulsive cleaning rituals. They might restrict their activity to one area — some OCD cleaners focus on handwashing and showers or disinfecting doorknobs and light switches — or it could extend to their entire lives.
4. Temporary Relief
Cleaning brings relief from the obsessive fears. However, the relief is only temporary. Soon, obsessive thoughts of contamination return, and the cycle repeats again many times in a single day.
Soon, obsessive thoughts of contamination return, and the cycle repeats again many times in a single day.
Breaking the Cycle of Obsessive Cleaning
The key to stop OCD cleaning rituals is to break the cycle. This can be accomplished by taking the following steps.
Confront Your Fears
Rather than avoid intrusive thoughts of contamination, the key is to face them and try to resist the temptation to respond with compulsive cleaning. The goal is to separate the thought from the action. In time, exposing yourself to the feared trigger will reduce the intrusive obsessions and subsequent discomfort.
Be Mindful
You can anticipate OCD urges, and eventually lessen the need to clean the same thing repeatedly, by being mindful when you clean an area rather than simply responding mindlessly to the trigger.
Accept Uncertainty
OCD thrives on uncertainty and is inherently a doubting disease. When “what if” thoughts begin to pile up, the best approach is to accept that no matter how much you clean and sanitize, you have no control of anything being absolutely clean.
Renewed Freedom Center Can Help
To learn more about how we can free you from the grips of OCD, contact us today. Our specialists are available to answer your questions or concerns, and help you determine whether one of our programs is right for your needs.
forms, symptoms, diagnosis, treatment and prevention
July 30, 2021
Gingivitis is an inflammatory gum disease characterized by bleeding that occurs when brushing teeth and eating. If left untreated, the inflammation can progress and lead to destruction of the attachment site of the gum to the tooth, which can lead to tooth loss.
How common is gigivitis?
Gingivitis is a fairly common disease. I'm suffering from 50 to 90% of the population. 1.2 Gingivitis is a "disease of the young". Over time, it often turns into periodontitis - gum disease, accompanied by loss of teeth.
ICD classification of gingivitis:
- K05.
 0. Acute gingivitis
0. Acute gingivitis - K05.00 Acute streptococcal gingivostomatitis
- K05.08 Other specified acute gingivitis
- K05.09 Acute unspecified gingivitis
- K05.1. Chronic gingivitis
- K05.10 Simple marginal gingivitis
- K05.19 Chronic gingivitis, unspecified
- K06.0. Gingival recession
- K06.1. Gingival hypertrophy
- K06.2. Lesions of the gingiva and edentulous alveolar margin due to trauma
- K06.9. Changing the gums and the ineustible alveolar edge Unsuitable
Classification of gingivitis in the form of disease
3- Cataral Hypertrophic
- Cavalry 97
Classification of gingivitis according to the prevalence of the disease
- localized
- generalized
With localized gingivitis, the gum is affected only in a few teeth, and with a generalized form, the entire gum.
Causes of gingivitis
1) Local factors
4- Poor oral hygiene.
 This is the most common cause, because plaque and tartar, which are formed due to insufficient hygiene, multiply bacteria, which provoke inflammation of the gums. nine0018
This is the most common cause, because plaque and tartar, which are formed due to insufficient hygiene, multiply bacteria, which provoke inflammation of the gums. nine0018 - Injuries and burns of mucous membranes resulting from eating hard or hot food. If injury occurs regularly, inflammation may develop.
- Injury to the gums with old fillings , crowns and braces.
- Smoking. Tar and other substances from cigarettes settle on the teeth, forming plaque and irritating the gums. Nicotine, in turn, impairs blood flow to the gums.
- Wisdom teeth eruption. If a tooth is cut for a long time and incorrectly, it can become a source of constant inflammation and provoke gingivitis.
2) General factors
- Improper nutrition with insufficient vitamins
- Weakened immunity , immunodeficiency states
- Antibiotics
- 0006 6
- DISECTIONS DRIVATIONAL SYSTEM (Crohn's Disease)
- Frequent Angines , tonsillitis , sinusitis
- CTESS
- Pregnancy , since it changes the hormone and worse.
 gums
gums - Diabetes mellitus
Symptoms of gingivitis
- Bleeding gums is the main symptom of gingivitis. Bleeding can occur both while brushing your teeth and while eating. Spontaneous bleeding also occurs0018
- Swelling and puffiness of the gums, which may make the teeth appear smaller.
- Pain of varying severity
- Discoloration of the gums: it becomes bright red or turns blue.
- Deterioration of general condition, fever, weakness, headache
The presence of symptoms and their severity depends on the form and severity of the disease.
Forms of gingivitis
Catarrhal gingivitisThis is the classic form of gingivitis, the most common. Many encounter him at school, but do not pay attention. If you experience even slight bleeding while brushing your teeth, you should contact your doctor as soon as possible. In addition to bleeding, symptoms such as bad breath, itching, and burning may occur.
 nine0003
nine0003
Hypertrophic gingivitisIn this form of the disease, the gums increase in size and can cover half of the tooth or more. This form of gingivitis can be caused by hormonal changes in pregnant women and adolescents, as well as medications.
Ulcerative gingivitisThe most dangerous and hard tolerable form of gingivitis, it causes necrosis (death) of the gums, severe pain, very sharp and bad breath. Sometimes it is painful for a person suffering from ulcerative gingivitis to even eat and speak, and the general condition is also disturbed. This form of gingivitis affects people with weakened immune systems. nine0003
Desquamative gingivitis
Manifested by swelling, bleeding and pain of the gums. The gum becomes bright red, "glazed", it is easy to injure. 5
Atrophic gingivitisIt is characterized by a decrease in the size of the gum: it becomes thin, easily injured, the roots of the teeth are exposed.
 The teeth seem longer, there is pain from cold, hot. This form of the disease is rare.
The teeth seem longer, there is pain from cold, hot. This form of the disease is rare. Gingivitis diagnosis
A complete history is important for a correct diagnosis, as gingivitis is a chronic disease and can begin in childhood. 6
It is worth paying attention to the general condition of the body, because gingivitis can be a symptom of a general disease. The dentist can refer the patient to the following specialists:
- Endocrinologist - for diseases of the endocrine system (diabetes mellitus, hyperfunction of the thyroid gland and adrenal glands). nine0018
- Hematologist - in case of blood diseases, consultation is required for differential diagnosis and complex treatment.
- Gastroenterologist - gingivitis is usually accompanied by chronic diseases of the digestive system.
- Related physicians, who in turn may order a number of other tests to treat the pathology, such as complete blood count, biochemical blood test, gastroscopy, ultrasound, etc.
The following diagnostic tests can be performed in the dental office:
- Probing is a diagnostic method that determines the features of attachment of the gums to the teeth.
- Gingival staining with iodine solutions: this shows if the gum is inflamed. With gingivitis, the gums turn brown.
- Determination of the level of hygiene, that is, how well a person brushes his teeth.
- Panoramic x-ray of teeth: this is to see if the inflammation has affected the bone or not, and also shows the condition of all teeth, fillings and crowns. nine0018
Answers to popular questions
1. How to stop bleeding gums at home?
Herbal rinses (such as oak bark) will help stop the bleeding, but they only work temporarily and mask the problem.
2. Can a hard brush cause gingivitis?
No, the brush itself does not cause gingivitis, but too hard bristles can damage the enamel. Most people are fine with medium-hard brushes.
 nine0003
nine0003 3. I have no problems with my gums, but my gums often hurt and bleed in only one place, what should I do?
Seek medical attention. Most likely, there is an old filling in this place, in which food gets stuck and inflammation begins.
4. Is gingivitis treatable or is it permanent?
Fortunately, yes, if you follow all the recommendations, you can get rid of gingivitis once and for all.
Treatment of gingivitis
Treatment of gingivitis should be complex.
- Local treatment
- General treatment
Local treatment of gingivitis
1. Removal of plaque and calculus. Since calculus and plaque are the main causes of gingivitis, they must be removed. This is done using special dental instruments, ultrasound, laser, hand tools - the method is selected depending on the condition of the gums. If gingivitis has already occurred - home cleaning of the teeth will not be enough, you should consult a doctor.
 nine0003
nine0003 2. Treatment of caries and its complications , replacement of old crowns and fillings. In the presence of injuries from braces, it is necessary to use a special wax.
3. Drug therapy for includes taking antiseptic, anti-inflammatory, antibacterial and analgesic drugs, such as Tantum ® Verde.
4. Surgical operations. If the gum has grown too large or, conversely, exposed the roots of the teeth too much, surgical intervention may be required. nine0003
5. Teaching good hygiene. This is necessary to consolidate the result of treatment and recovery. The doctor helps you choose the right hygiene products
and teaches you how to properly brush your teeth.
Tantum
® Verde for the treatment of gingivitisEffective treatment is possible with the use of anti-inflammatory drugs, which include Tantum ® Verde .
 Benzydamine in mouthwash Tantum ® Verde has a complex effect on the gums: reduces swelling, relieves inflammation, reduces pain and kills microbes on the surface and inside the affected tissues 11,12,13 . Benzydamine penetrates well into tissues 12 , which gives it an advantage over most drugs, it has antibacterial and antifungal activity 13.15 . From the first minute Tantum ® Verde has an anti-inflammatory and local analgesic effect on the symptoms of gingivitis: pain, burning sensation, swelling and swelling of the gums, etc. 11.14 For home use, it is better to use the solution form, and the spray and tablets are convenient to take with you. 7.8.9
Benzydamine in mouthwash Tantum ® Verde has a complex effect on the gums: reduces swelling, relieves inflammation, reduces pain and kills microbes on the surface and inside the affected tissues 11,12,13 . Benzydamine penetrates well into tissues 12 , which gives it an advantage over most drugs, it has antibacterial and antifungal activity 13.15 . From the first minute Tantum ® Verde has an anti-inflammatory and local analgesic effect on the symptoms of gingivitis: pain, burning sensation, swelling and swelling of the gums, etc. 11.14 For home use, it is better to use the solution form, and the spray and tablets are convenient to take with you. 7.8.9 Spray Tantum ® Verde
more
- Treatment of general diseases
- Anti-inflammatory, antimicrobial therapy
- Antiallergics
Prevention of gingivitis
Prevention is always easier than cure. Therefore, it is very important to follow the following recommendations for the prevention of gingivitis: 10
Therefore, it is very important to follow the following recommendations for the prevention of gingivitis: 10
- Brush your teeth at least 2 times a day: morning and evening.
- You don't have to brush your teeth after every meal, you just need to rinse your mouth with water.
- It is very important to use all personal hygiene products and do it correctly. nine0018
- Visit the dentist once or twice a year for an examination and professional cleaning. It will remove plaque and be able to recognize gingivitis at an early stage.
- Treat all comorbidities of the body.
- If the installed structures in the mouth (fillings, dentures, braces) injure the mucous membrane, consult a doctor.
- Lead a healthy lifestyle: engage in hardening, exercise, eat right.
These steps will help you avoid gum disease and keep your mouth healthy. nine0003
Blockage of lacrimal ducts | CooperVision Russia
If you've seen a crying baby or the latest sentimental Hollywood movie recently, you're well aware that tears run down your face
However, we also have a tear duct (also called "nasolacrimal duct" and "tear duct"). through which tears pass through the nose. These drainage tubes lead to a runny nose while crying or an allergic reaction in the eyes.
through which tears pass through the nose. These drainage tubes lead to a runny nose while crying or an allergic reaction in the eyes.
When the tear duct becomes blocked, problems arise. Let's look at the causes of blocked tear ducts, how it happens and how to get rid of it. nine0003
Why does tear duct blockage occur?
Blockage of the tear ducts occurs for many reasons.
Congenital blockage: One fifth of all babies are born with blocked tear ducts. It may be caused by an underdeveloped or abnormal canal or developmental problems in the structure of the face and skull.
Age narrowing: In adults, there may be a narrowing of the entrance of the lacrimal duct, which increases the likelihood of blockage of the lacrimal duct. nine0003
Infections and inflammations: Infections and inflammations of the tear duct, eyes and nose can also cause blockage of the tear duct. Blockage of the tear duct itself can lead to infection and inflammation.
Bruises and injuries of the face: Any bruises that affect the lacrimal ducts and the bone structure around them can lead to blockage of the lacrimal duct.
Tumors, cysts and calculi: Blockage of the tear duct can be caused by tumors and other growths.
As you can see, while the blockage of the lacrimal canal produces many symptoms, it can also indicate a primary disease. Always consult your ophthalmologist for eye problems so that he can provide timely assistance. nine0003
Symptoms of clogged tear ducts
A clogged tear duct or an infection caused by a blockage can be characterized by a number of symptoms. These include:
- Watery eyes and excessive tearing
- Recurrent inflammations and infections (infections may be caused by blockage or lead to blockage)
- Accumulation or secretion of mucus
- Pain and swelling in the corners of the eyes
- Blurred vision
- Bloody Tears
Your ophthalmologist will be able to assess the function of the drainage of the lacrimal duct and decide on the treatment options.
Treatment of blocked tear ducts
The best treatment for blocked tear ducts is determined by its cause. Your ophthalmologist will recommend trying the least invasive method first and then choosing what works for you and when you need to switch to other treatments.
The following are common treatments for blocked tear ducts. nine0003
Blockage of tear ducts in infants
In many newborns, blockage of the tear ducts resolves within the first year of life. However, there are cases when treatment is necessary. The first treatment for blocked tear ducts in infants includes dilatation (gentle widening of the duct), probing, and lavage. If this does not help, the ophthalmologist will sometimes insert a dilating probe to further widen the canal.
Blockage of lacrimal ducts in adults
Blockage of the tear ducts in adults usually indicates a narrowing or other problem that does not go away on its own. The first stage of treatment is the same as for infants: dilation, probing and lavage.