Citalopram discontinuation syndrome
Citalopram withdrawal: What to expect
Anyone who takes citalopram or other antidepressants may experience withdrawal symptoms after stopping. Doctors recommend gradually tapering off antidepressant medications under medical supervision to minimize withdrawal symptoms.
Citalopram, which people may know by the brand name Celexa, can cause some people to experience withdrawal symptoms upon stopping the drug. These symptoms may include:
- muscle aches
- chills
- digestive upset
- changes in mood
Citalopram withdrawal symptoms can vary in their onset, duration, and intensity.
Withdrawal or discontinuation symptoms are common after discontinuing antidepressants. Some research suggests that these symptoms affect 56% of people who stop taking their depression medication.
In this article, we discuss citalopram withdrawal in more detail, including its symptoms and ways to minimize or prevent them.
Citalopram is one medication in a group of antidepressants known as selective serotonin reuptake inhibitors (SSRIs). It is available as a tablet or an oral solution.
SSRIs increase the available levels of serotonin in the brain. Serotonin is a neurotransmitter that boosts positive feelings and helps stabilize mood.
The Food and Drug Administration (FDA) has approved citalopram to treat depression in adults. Some medical professionals may also prescribe it to treat other conditions, such as:
- alcohol use disorder
- obsessive-compulsive disorder (OCD)
- panic disorder
- premenstrual dysphoric disorder (PMDD)
Some people might also take citalopram to treat specific symptoms, such as postmenopausal flushing.
Citalopram withdrawal occurs when a person abruptly stops taking the medication.
Symptoms can develop because the brain experiences rapid changes in the level of serotonin that is available to it.
A 2019 review states that more than half of people coming off various antidepressants experience withdrawal effects, with 46% of these individuals reporting “severe” symptoms.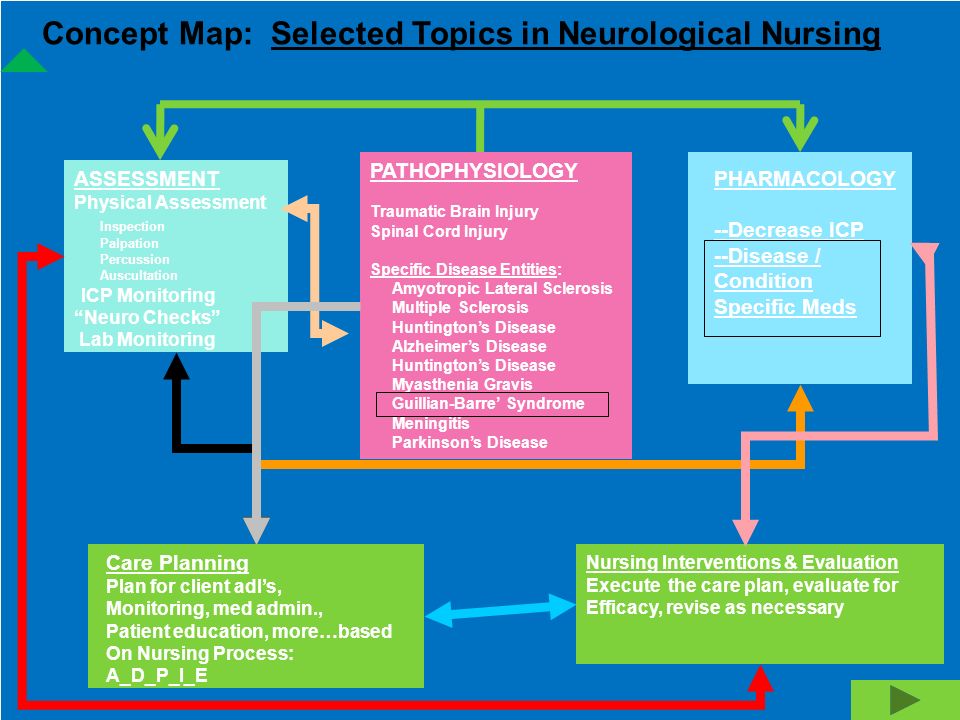
Citalopram, however, may pose a lower risk of these effects than other antidepressants. The reason for this is that compared with other common antidepressants, citalopram has a relatively long half-life of 38–48 hours.
The half-life of a drug is the time it takes for the amount of its active substance to reduce by half in the body.
Drugs with a longer half-life, such as citalopram, tend to cause fewer withdrawal symptoms than those with a short half-life.
However, citalopram may still cause the same or more symptoms than other antidepressants with a longer half-life, such as fluoxetine (Prozac).
Citalopram and other SSRIs may cause withdrawal symptoms such as:
- an electric shock-like sensation in the head
- anxiety
- changes in mood, such as depression, irritability, and mood swings
- digestive issues, including diarrhea, nausea, cramps, and vomiting
- dizziness or vertigo
- fatigue
- feeling “detached” from life or others
- flu-like symptoms, including chills and body aches
- movement problems, such as loss of balance or coordination
- problems concentrating
- ringing in the ears, known as tinnitus
- sensory disturbances, such as smelling things that are not there
- sleep problems, including vivid or distressing dreams
- thoughts of suicide
Withdrawal vs.
 return of symptoms
return of symptomsAlthough citalopram withdrawal may cause mood-related symptoms, this does not necessarily mean that someone is experiencing a return of depressive symptoms.
To distinguish between withdrawal and return, individuals should consider:
- The onset of symptoms: Withdrawal symptoms appear soon after coming off antidepressants, whereas returning depressive symptoms may take several weeks to emerge.
- The symptoms over time: Withdrawal symptoms will get better as the body adjusts to the lack of antidepressant medications, but returning symptoms of depression will persist or get worse.
Antidepressant withdrawal symptoms can last for a few weeks to a few months.
Typically, doctors advise that discontinuation symptoms are self-limiting and resolve within a couple of weeks.
However, a review of other studies indicates that this is not always the case. The authors note that, for some people, antidepressant withdrawal symptoms can persist for several weeks or months.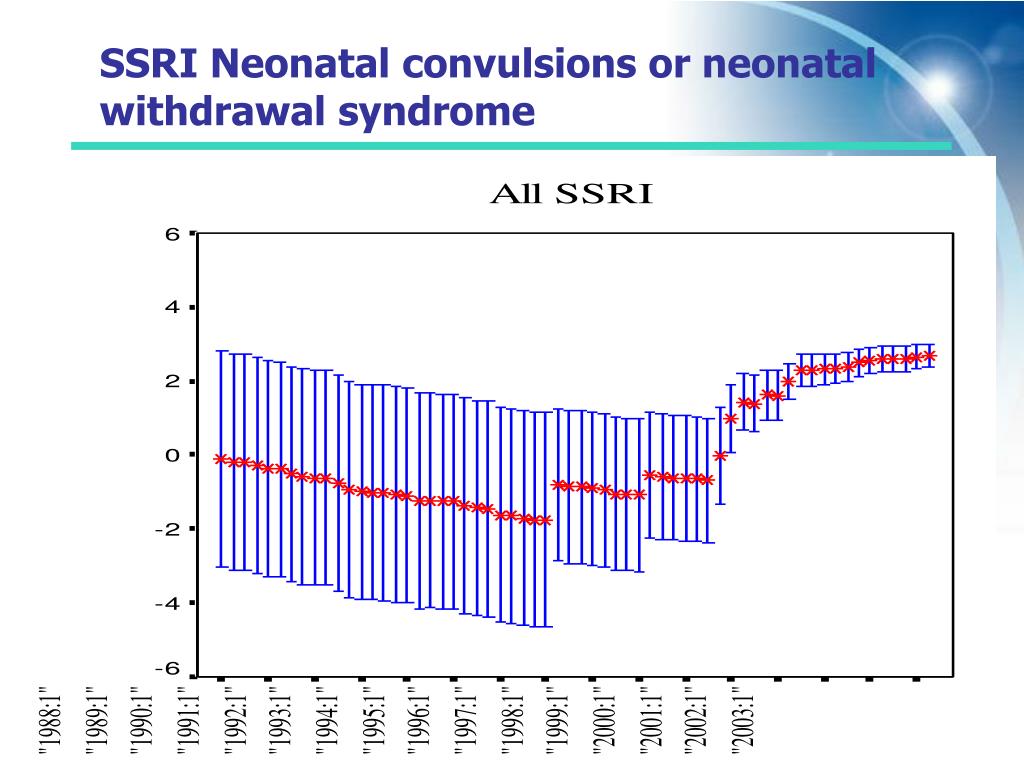
Some of the included research found that 40% of people had symptoms for at least 6 weeks, while 25% had them for 12 weeks or more.
Many treatments and self-care options exist to help people safely come off citalopram while minimizing potential symptoms. Options include:
- Discussing medication cessation with a doctor: A person should always speak with their doctor before making any medication changes. Suddenly stopping antidepressant use increases the risk of severe symptoms.
- Taking a tapering-off approach: Doctors typically advise people to reduce their antidepressant dosage slowly — usually over 2 to 4 weeks. This advice is especially relevant for those who have been taking the medication for an extended time or are on a higher dosage.
-
Taking medication for withdrawal symptoms: Some withdrawal symptoms may respond to medications. For example, people can try using pain relievers for muscle aches or sleep medications for insomnia.
- Seeing a doctor regularly: Regular medical checkups during the withdrawal process can help people better manage their symptoms and monitor for recurrent depression.
- Considering psychotherapy: Cognitive behavioral therapy (CBT) or mindfulness-based cognitive therapy (MBCT), for example, may support the discontinuation process without increasing the relapse risk.
- Leading a healthy lifestyle: Taking steps to exercise regularly, getting enough sleep, following a nutrient-dense diet, and practicing stress reduction techniques can help people manage depression symptoms without medication. These habits may also ease some withdrawal symptoms.
Talk with your medical professional if you are pregnant or planning to become pregnant. Research in animals suggests taking citalopram while pregnant may cause adverse effects on the fetus.
As a result, the FDA advises only taking citalopram during pregnancy in situations where the benefit to the pregnant person outweighs the potential risk to the fetus.
For example, a doctor may deem it necessary for some people to take SSRIs such as citalopram during their pregnancy to prevent the return of depression.
The National Alliance on Mental Illness advises anyone who becomes pregnant while taking citalopram to contact their doctor immediately.
Withdrawal symptoms during pregnancy are likely to resemble those in people who are not pregnant. The management techniques are also likely to be similar.
People should contact their doctor if they:
- develop adverse effects from antidepressant use and wish to discuss other options
- wish to stop taking citalopram in a safe manner under medical supervision
- experience withdrawal symptoms after stopping citalopram
Individuals should call a doctor immediately if any side effects are severe. They should call 911 if their symptoms feel life threatening.
It is essential to call 911 if someone is having suicidal thoughts and is at immediate risk of self-harm, suicide, or hurting another person.
The 988 Suicide and Crisis Lifeline is available 24/7 at 988 to provide support to those having thoughts of suicide.
The long-term use of citalopram is safe when people take it as their doctor prescribes.
However, research indicates that using any antidepressant for more than 6 weeks can cause withdrawal symptoms on tapering or stopping the drug.
Abruptly stopping or rapidly reducing the dosage can increase the risk of these symptoms.
Those taking citalopram or other antidepressants for an extended period should work with their doctor to find effective treatments and strategies to minimize withdrawal effects.
It is also important to monitor for the return of depressive symptoms after stopping long-term antidepressant use.
Coming off citalopram can lead to withdrawal symptoms, particularly if people have been taking it for more than 6 weeks.
Common discontinuation symptoms include flu-like symptoms, sleep disturbances, and mood changes.
It is important that people who wish to stop taking antidepressants do so under medical supervision.
Individuals should discuss their options with a doctor. These may include alternative medications and strategies for minimizing withdrawal symptoms and preventing the return of depressive symptoms.
Antidepressant Discontinuation Syndrome | AAFP
CHRISTOPHER H. WARNER, MAJ, MC, USA, WILLIAM BOBO, LCDR, MC, USN, CAROLYNN WARNER, MAJ, MC, USA, SARA REID, CPT, USAF, MC, AND JAMES RACHAL, MAJ, USAF, MC
Am Fam Physician. 2006;74(3):449-456
Patient information: See related handout on antidepressant discontinuation syndrome, written by the authors of this article.
Author disclosure: Nothing to disclose.
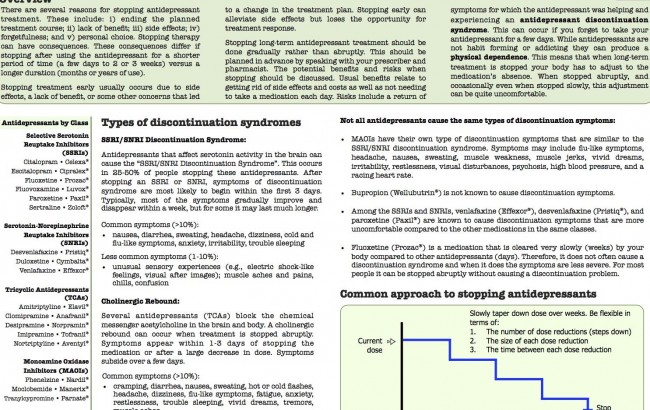
Antidepressant discontinuation syndrome occurs in approximately 20 percent of patients after abrupt discontinuation of an antidepressant medication that was taken for at least six weeks. Typical symptoms of antidepressant discontinuation syndrome include flu-like symptoms, insomnia, nausea, imbalance, sensory disturbances, and hyperarousal. These symptoms usually are mild, last one to two weeks, and are rapidly extinguished with reinstitution of antidepressant medication. Antidepressant discontinuation syndrome is more likely with a longer duration of treatment and a shorter half-life of the treatment drug. A high index of suspicion should be maintained for the emergence of discontinuation symptoms, which should prompt close questioning regarding accidental or purposeful self-discontinuation of medication. Before antidepressants are prescribed, patient education should include warnings about the potential problems associated with abrupt discontinuation. Education about this common and likely underrecognized clinical phenomenon will help prevent future episodes and minimize the risk of misdiagnosis.
Education about this common and likely underrecognized clinical phenomenon will help prevent future episodes and minimize the risk of misdiagnosis.
Interruption of treatment with an anti-depressant medication is sometimes associated with an antidepressant discontinuation syndrome; in early reports it was referred to as a “withdrawal reaction.”1 Symptoms of antidepressant discontinuation syndrome can include flu-like symptoms, insomnia, nausea, imbalance, sensory disturbances, and hyperarousal. All approved anti-depressant agents have had case reports or warnings from their manufacturers of such reactions occurring in response to either abrupt discontinuation or medication tapering.
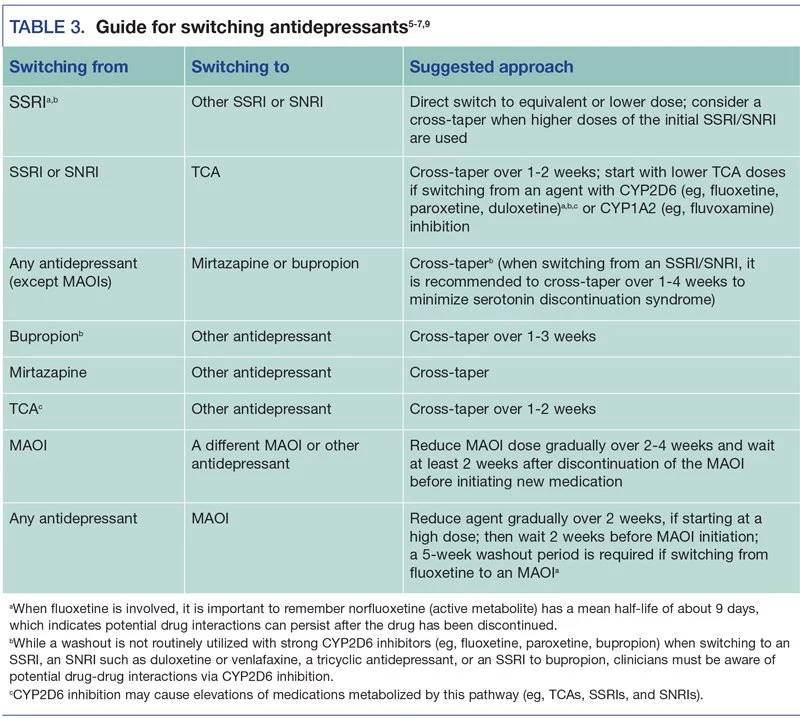
2 These medications include selective serotonin reuptake inhibitors (SSRIs),3 tricyclic antidepressants,4 monoamine oxidase inhibitors (MAOIs),5 and atypical agents such as venlafaxine (Effexor),6 mirtazapine (Remeron),7 trazodone (Desyrel),8 and duloxetine (Cymbalta). 9
9
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Maintain a high index of suspicion for antidepressant discontinuation syndrome. | C | 19 |
| Be alert to times when patients may need guidance on discontinuing an antidepressant or when they are likely to discontinue an antidepressant on their own. | C | 27,32 |
| Be sure to differentiate antidepressant discontinuation syndrome from relapse of depression and other psychiatric and medical conditions. | C | 19,27,28 |
| Gradually discontinue medication using one of the suggested tapering regimens (Table 5). | C | 16,17,21,22,27,28 |
The importance of understanding and recognizing antidepressant discontinuation syndrome is threefold: (1) though typically mild, antidepressant discontinuation syndrome symptoms are associated with significant discomfort, work absenteeism, other psychosocial problems, and may on rare occasions be severe enough to require hospitalization10–12; (2) failure to recognize antidepressant discontinuation syndrome may result in medical and psychiatric misdiagnosis, potentially exposing patients to unnecessary diagnostic investigations or potentially risky medical interventions; (3) patients may be unwilling to use psychotropic medications in the future, thereby increasing their vulnerability to future relapses of depressive or anxiety disorders.
Pathophysiology
Although several hypotheses exist, the definitive pathophysiologic explanation for antidepressant discontinuation syndrome remains unknown. Early reports of antidepressant discontinuation syndrome made heavy use of the term “withdrawal” to describe discontinuation symptoms; however, antidepressant medications are not believed to be habit forming and are not associated with drug-seeking behavior.13 Long-term use of SSRIs increases synaptic levels of serotonin through blockade of the serotonin reuptake pump, resulting in down-regulation of postsynaptic receptors.14
There is speculation concerning the possibility of a temporary deficiency of synaptic serotonin with abrupt withdrawal of an SSRI.15 This deficiency is compounded by the fact that down-regulated receptors will remain in their relatively hypoactive state for days to weeks.15 This is believed to result in antidepressant discontinuation syndrome directly or indirectly via downstream effects on other neurotransmitter systems (e. g., norepinephrine, dopamine, and γ-amino-butyric acid) implicated in depressive and anxiety disorders.15
g., norepinephrine, dopamine, and γ-amino-butyric acid) implicated in depressive and anxiety disorders.15
Because tricyclic antidepressants and MAOIs also are serotonergically active, the same mechanism is implicated for their respective antidepressant discontinuation syndromes; however, tricyclic antidepressants also affect the cholinergic system, so rapid discontinuation may cause signs of parkinsonism and problems with balance. Because MAOIs cause changes in the alpha2-adrenergic and dopaminergic receptors, their discontinuation may cause agitation and psychosis.
Epidemiology and Risk Factors
Because of the varied clinical presentation, transient nature, and lack of pathognomonic clinical features, there are relatively few data on incidence, prevalence, and other estimates of burden associated with antidepressant discontinuation syndrome. One observational study16 found that four of 45 patients (9 percent) given fluoxetine (Prozac) and 26 of 52 patients (50 percent) given paroxetine (Paxil) reported discontinuation symptoms, with a mean onset of two days and mean duration of five days.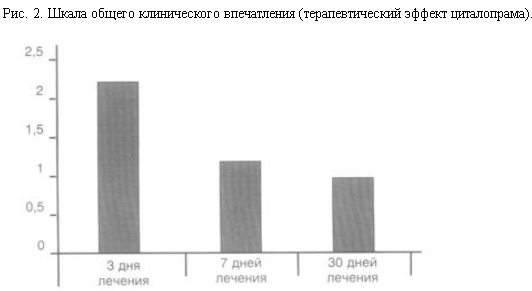 A randomized controlled trial17 (RCT) comparing three SSRIs found a lower incidence of antidepressant discontinuation syndrome with fluoxetine (14 percent) than with paroxetine (66 percent) or sertraline (Zoloft) (60 percent). This study was limited by its open-label design and was sponsored by the manufacturer of fluoxetine. In addition, a retrospective chart review13 of 350 patients using SSRIs showed no significant added risk associated with age, sex, or diagnosis.
A randomized controlled trial17 (RCT) comparing three SSRIs found a lower incidence of antidepressant discontinuation syndrome with fluoxetine (14 percent) than with paroxetine (66 percent) or sertraline (Zoloft) (60 percent). This study was limited by its open-label design and was sponsored by the manufacturer of fluoxetine. In addition, a retrospective chart review13 of 350 patients using SSRIs showed no significant added risk associated with age, sex, or diagnosis.
Perhaps the best evidence comes from an RCT18 that found mild to moderate antidepressant discontinuation symptoms in 35 percent of patients given paroxetine and 14 percent given placebo who were abruptly withdrawn from treatment after 12 weeks. The difference of approximately 20 percent between active treatment and placebo for one of the drugs most commonly associated with antidepressant discontinuation syndrome may provide an upper boundary for the probability of the condition.18
DURATION OF TREATMENT
Although unconfirmed by prospective clinical trials, case reports of antidepressant discontinuation syndrome reactions are rare among individuals who have received less than six to eight weeks of antidepressant treatment. 19 This generalization applies to antidepressant discontinuation syndrome that occurs in the settings of both abrupt and gradual antidepressant discontinuation. Such a time frame may be required to allow the synaptic changes that occur during long-term pharmacologic antidepressant treatment.
19 This generalization applies to antidepressant discontinuation syndrome that occurs in the settings of both abrupt and gradual antidepressant discontinuation. Such a time frame may be required to allow the synaptic changes that occur during long-term pharmacologic antidepressant treatment.
PHARMACOLOGIC PROFILE
For SSRIs, a relatively homogenous drug class, differences among the pharmacokinetic properties such as elimination half-life and metabolism may be the most clinically relevant (Table 1).20,21 Specifically, antidepressant discontinuation syndrome is more common in patients discontinuing agents with relatively short half-lives, such as paroxetine, than in those with longer half-lives, such as fluoxetine.13,16,17,19,22 In recent years, slow-, extended-, or controlled-release formulations of venlafaxine (Effexor XR), paroxetine (Paxil CR), and fluoxetine (Prozac Weekly) have become available. Although there are limited data concerning weekly fluoxetine, antidepressant discontinuation syndrome reactions have been reported with controlled-release paroxetine and extended-release venlafaxine.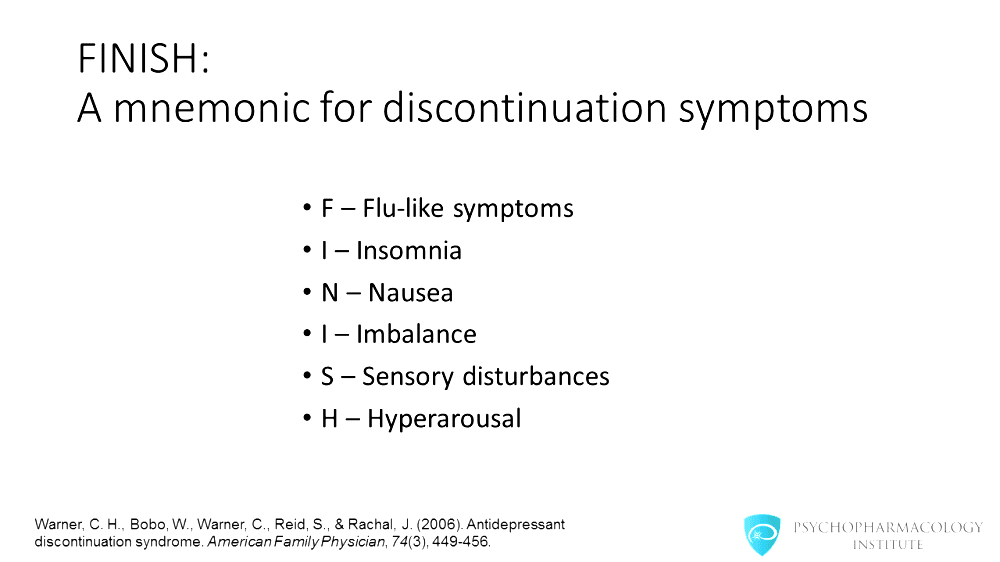 14,23
14,23
| Drug | Dosage range (mg per day) | Half-life (hours) | Active metabolite? |
|---|---|---|---|
| Selective serotonin reuptake inhibitor | |||
| Citalopram (Celexa) | 10 to 60 | 35 | No |
| Escitalopram (Lexapro) | 10 to 30 | 27 to 32 | No |
| Fluoxetine (Prozac) | 20 to 80 | 84 to 144 | Yes |
| Paroxetine (Paxil) | 10 to 60 | 21 | No |
| Paroxetine CR (Paxil CR) | 12.5 to 62.5 | 15 to 20 | No |
| Sertraline (Zoloft) | 50 to 200 | 26 | Yes |
| Atypical antidepressant | |||
| Bupropion (Wellbutrin) | 75 to 450 | 12 to 30 | Yes |
| Buproprion SR (Wellbutrin SR) | 100 to 400 | 12 to 30 | Yes |
| Buproprion XL (Wellbutrin XL) | 150 to 450 | 12 to 30 | Yes |
| Duloxetine (Cymbalta)* | 40 to 60 | 11 to 16 | Yes |
| Mirtazapine (Remeron) | 15 to 45 | 20 to 40 | No |
| Trazodone (Desyrel) | 50 to 400 | 7. 1 1 | Yes |
| Venlafaxine (Effexor) | 75 to 450 | 3 to 13 | Yes |
| Venlafaxine XR (Effexor XR) | 75 to 450 | 3 to 13 | Yes |
| Monoamine oxidase inhibitors | |||
| Phenelzine (Nardil) | 15 to 90 | 1.2 | Yes |
| Tricyclic antidepressant* | |||
| Amitriptyline | 25 to 300 | 9 to 25 | Yes |
| Clomipramine (Anafranil) | 25 to 250 | 22 to 84 | No |
| Desipramine (Norpramin) | 25 to 300 | 14.3 to 24.7 | No |
| Doxepin (Sinequan) | 25 to 300 | 11 to 23 | No |
| Imipramine (Tofranil) | 25 to 300 | 10 to 16 | Yes |
| Nortriptyline (Pamelor) | 25 to 150 | 18. 2 to 35 2 to 35 | No |
Clinical Manifestations and Pathophysiology
CLINICAL MANIFESTATIONS
Antidepressant discontinuation syndrome involves a large number of psychological and physiological signs and symptoms. Case reports, audits of adverse drug reaction databases, and clinical trials report certain characteristic symptoms. These symptoms depend on the class of antidepressant used (Table 2).2,13,16,17,19,22,24,25 In a recent retrospective chart review13 of patients on antidepressants and two small, prospective, randomized controlled trials,16,24 patients' SSRIs were replaced with placebo for five days or their antidepressant medication was abruptly discontinued. All noted that the most common symptoms of SSRI withdrawal were dizziness, gastrointestinal upset, lethargy or anxiety/hyperarousal, dysphoria, sleep problems, and headache.13,16,24
| SSRI | Atypical antidepressant | Tricyclic antidepressant | MAOI | |
|---|---|---|---|---|
| General | ||||
| Flu-like symptoms | + | + | + | — |
| Headache | + | + | + | + |
| Lethargy | + | + | + | — |
| Gastrointestinal | ||||
| Abdominal cramping | + | — | + | — |
| Abdominal pain | + | — | + | — |
| Appetite disturbance | + | + | + | — |
| Diarrhea | + | + | — | |
| Nausea/vomiting | + | + | + | — |
| Sleep | ||||
| Insomnia | + | + | + | + |
| Nightmares | + | + | + | + |
| Balance | ||||
| Ataxia | + | — | + | — |
| Dizziness | + | + | + | — |
| Lightheadedness | + | — | + | — |
| Vertigo | + | + | + | — |
| Sensory | ||||
| Blurred vision | + | — | — | — |
| “Electric shock” sensations | + | + | — | — |
| Numbness | + | — | — | — |
| Paresthesia | + | + | — | — |
| Movement | ||||
| Akathisia | + | + | + | — |
| Myoclonic jerks | — | — | — | + |
| Parkinsonism | + | — | + | — |
| Tremor | + | — | + | — |
| Affective | ||||
| Aggression/irritability | + | — | — | + |
| Agitation | + | — | + | + |
| Anxiety | + | + | + | — |
| Low mood | + | + | + | + |
| Psychosis | ||||
| Catatonia | — | — | — | + |
| Delirium | — | — | — | + |
| Delusions | — | — | — | + |
| Hallucinations | — | — | — | + |
Antidepressant discontinuation syndrome is most often seen in the primary care office in association with SSRI discontinuation, because SSRIs are the most commonly prescribed class of antidepressant medications. In 2000, a systematic review25 of 46 case reports of SSRI discontinuation proposed the diagnostic criteria listed in Table 3.25 The FINISH mnemonic (Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, Hyperarousal) was created to facilitate rapid recognition (Table 4).26 However, neither set of criteria25,26 has been formally validated.
In 2000, a systematic review25 of 46 case reports of SSRI discontinuation proposed the diagnostic criteria listed in Table 3.25 The FINISH mnemonic (Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, Hyperarousal) was created to facilitate rapid recognition (Table 4).26 However, neither set of criteria25,26 has been formally validated.
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
| Flu-like symptoms |
| Fatigue |
| Lethargy |
| General malaise |
| Muscle aches/headaches |
| Diarrhea |
| Insomnia |
| Nausea |
| Imbalance |
| Gait instability |
| Dizziness/lightheadedness |
| Vertigo |
| Sensory disturbances |
| Paresthesia |
| “Electric shock” sensations |
| Visual disturbance |
| Hyperarousal |
| Anxiety |
| Agitation |
Multiple case reports demonstrate that antidepressant discontinuation syndrome associated with tricyclic antidepressants closely mimics that of the SSRIs. 3,4 However, signs of parkinsonism and profound problems with balance appear to be especially characteristic of antidepressant discontinuation syndrome caused by tricyclic antidepressant discontinuation.3,4 Additionally, case reports have noted that the antidepressant discontinuation syndrome associated with MAOIs may involve more serious symptomatology such as aggressiveness, agitation, catatonia, severe cognitive impairment, or myoclonus and psychotic symptoms and may require more intensive management.4,5
3,4 However, signs of parkinsonism and profound problems with balance appear to be especially characteristic of antidepressant discontinuation syndrome caused by tricyclic antidepressant discontinuation.3,4 Additionally, case reports have noted that the antidepressant discontinuation syndrome associated with MAOIs may involve more serious symptomatology such as aggressiveness, agitation, catatonia, severe cognitive impairment, or myoclonus and psychotic symptoms and may require more intensive management.4,5
ONSET AND COURSE
Discontinuation symptoms typically appear within three days of stopping antidepressant medication or initiating a medication taper, though it has been reported that reactions may occur within hours of the first missed dose.9 Untreated symptoms are usually mild and resolve spontaneously in one to two weeks.19 In rare but more serious cases involving psychosis, catatonia, or severe cognitive impairment, immediate psychiatric consultation may be required.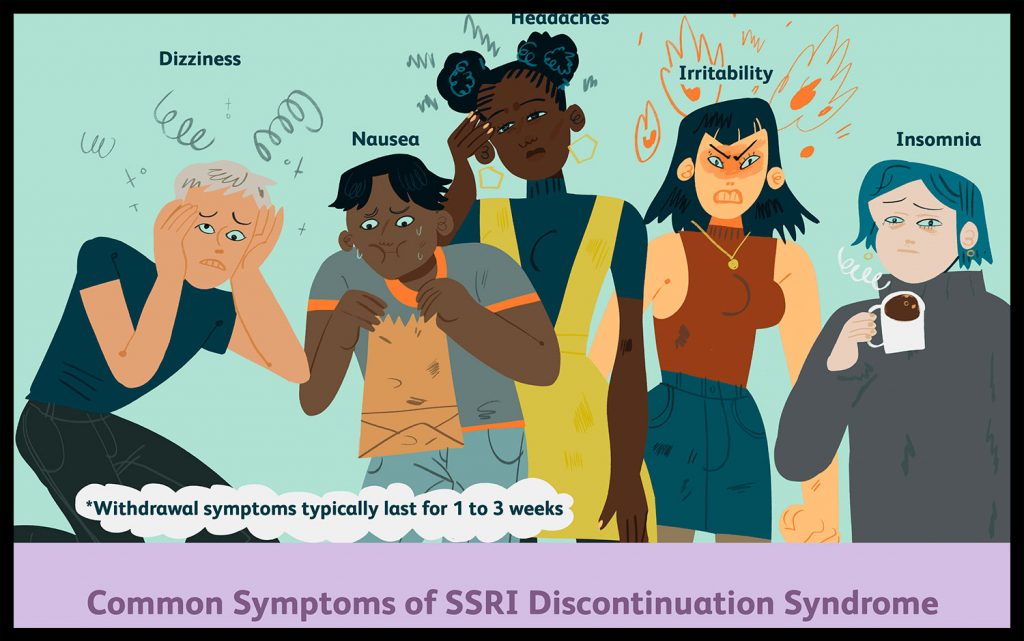
Diagnostic considerations
MAINTAIN A HIGH INDEX OF SUSPICION
Any uncomfortable symptoms reported by patients receiving antidepressants should prompt close questioning for missed doses, unreported downward adjustments in dosage, or outright medication discontinuation.
DIFFERENTIATION FROM RELAPSE
The symptoms of antidepressant discontinuation syndrome that are associated with most antidepressants share features of major depression, including dysphoria, appetite changes, sleep problems, cognitive problems, and fatigue. By focusing on symptoms that distinguish antidepressant discontinuation syndrome from depressive illness relapse (e.g., dizziness, “electric shock” sensations, “rushing” sensations in the head, headache, and nausea) and observing for rapid (i.e., within a few days) reversal of symptoms after restarting the antidepressant or complete resolution of symptoms in one to two weeks (highly uncharacteristic of a depressive relapse), a definitive diagnosis is fairly easy to make. 19,27 Depressive relapses or recurrences typically occur after at least two to three weeks or longer after cessation of medication and are most often marked by gradual worsening of depression, insomnia, and psychomotor symptoms.28
19,27 Depressive relapses or recurrences typically occur after at least two to three weeks or longer after cessation of medication and are most often marked by gradual worsening of depression, insomnia, and psychomotor symptoms.28
DIFFERENTIATION FROM OTHER CONDITIONS
Irritability, sleeplessness, and anxiety or agitation in a patient taking antidepressants may appropriately raise suspicion of an antidepressant-associated bipolar manic episode that must be distinguished from antidepressant discontinuation syndrome. The development of these symptoms should prompt close questioning about medication adherence, as previously mentioned. If such symptoms appear shortly after discontinuation or during dose reduction, rapid symptom resolution after restoring the antidepressant medication will lead to the correct diagnosis.
Antidepressant discontinuation syndrome also may be misdiagnosed as severe conditions including stroke, other neurologic conditions, infectious diseases, and adverse effects of other medications the patient is taking._Oral_Tablet_0.jpg) 29 Antidepressant discontinuation syndrome has been reported when switching from one antidepressant agent to another.30 When the new agent has different pharmacologic mechanism reactions than the first agent, antidepressant discontinuation syndrome may be misinterpreted as intolerable side effects from the new medication.29
29 Antidepressant discontinuation syndrome has been reported when switching from one antidepressant agent to another.30 When the new agent has different pharmacologic mechanism reactions than the first agent, antidepressant discontinuation syndrome may be misinterpreted as intolerable side effects from the new medication.29
Prevention and management
USE OF ANTIDEPRESSANTS
For optimal treatment of most psychiatric conditions, and especially anxiety and depressive disorders, psychosocial interventions should be recommended along with or considered as alternatives to pharmacologic therapies. The all-too-common practice of “short-term” prescriptions for off-label, non–mental health reasons (e.g., irritable bowel syndrome, weight loss, headaches, insomnia) has been associated with early antidepressant discontinuation and may increase the risk of antidepressant discontinuation syndrome.31
PATIENTS AT RISK OF DISCONTINUATION
Patients may be tempted to discontinue their antidepressant medication after they begin to feel better, a practice that invites both early relapse of illness and antidepressant discontinuation syndrome. Women may discontinue antidepressant use after discovering that they are pregnant. Ideally, patients should be counseled regarding the risks of illness relapse, the importance of treating symptoms to remission, the need for continuation and (where appropriate) maintenance pharmacotherapy, and the need for gradual discontinuation of medications before discontinuing care.27,32
Women may discontinue antidepressant use after discovering that they are pregnant. Ideally, patients should be counseled regarding the risks of illness relapse, the importance of treating symptoms to remission, the need for continuation and (where appropriate) maintenance pharmacotherapy, and the need for gradual discontinuation of medications before discontinuing care.27,32
DISCONTINUING MEDICATION
Although there are no clinical trials comparing abrupt discontinuation with tapered discontinuation of antidepressants, tapering is recommended by experts, based on the suspected pathophysiology of antidepressant discontinuation syndrome.33 Patients should be forewarned of the possibility of antidepressant discontinuation syndrome if antidepressants are discontinued, and that supervised tapering of medication over six to eight weeks may be required to minimize discontinuation symptoms. Several RCTs have shown that with abrupt cessation of antidepressants, symptoms can begin within days. 16,17,22 It may be possible to discontinue medication more quickly if doses are low; discontinuation may take longer (three months or more) after maintenance therapy. It may be possible to stop fluoxetine therapy without tapering. There are no clear, validated tapering recommendations. However, Table 527 offers one expert's recommendations for tapering rates.
16,17,22 It may be possible to discontinue medication more quickly if doses are low; discontinuation may take longer (three months or more) after maintenance therapy. It may be possible to stop fluoxetine therapy without tapering. There are no clear, validated tapering recommendations. However, Table 527 offers one expert's recommendations for tapering rates.
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
MANAGEMENT
If antidepressant discontinuation syndrome occurs and other serious causes of these symptoms have been ruled out, the physician should begin by providing reassurance to the patient that the condition is reversible, is not serious or life threatening, and will run its course within one to two weeks. The physician should then consider restarting the antidepressant medication with a slow dose taper or providing support if the patient desires not to restart the antidepressant.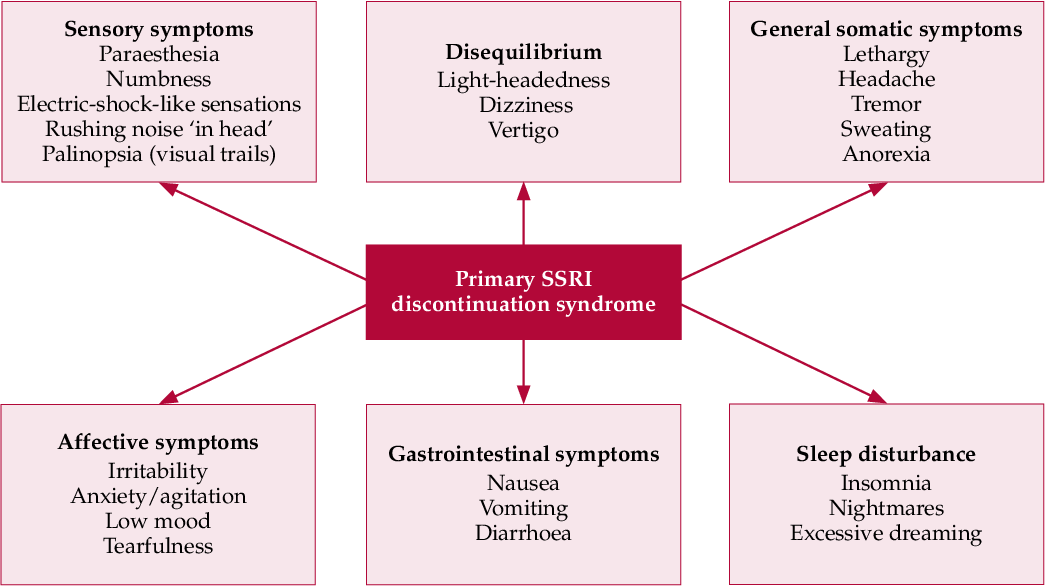 Severe symptoms should resolve in fewer than three days, and often within 24 hours. If the antidepressant discontinuation syndrome occurs during a tapering of the antidepressant, consider restarting at the original dose and then taper at a slower rate. In cases where slow tapering is poorly tolerated, a medicine with a longer half-life such as fluoxetine may be substituted for the shorter half-life agent.
Severe symptoms should resolve in fewer than three days, and often within 24 hours. If the antidepressant discontinuation syndrome occurs during a tapering of the antidepressant, consider restarting at the original dose and then taper at a slower rate. In cases where slow tapering is poorly tolerated, a medicine with a longer half-life such as fluoxetine may be substituted for the shorter half-life agent.
GENERIC DRUGS AND SUBSTITUTIONS
Not all formulations of the same drug are bioequivalent. Generic drugs are allowed up to a 20 percent difference. This may result in an unintended sudden reduction in drug concentration if a patient's medication is switched to a generic or alternative brand.
TRICYCLIC ANTIDEPRESSANTS
Antidepressant discontinuation syndrome symptoms caused by tricyclic antidepressants that suggest cholinergic rebound (e.g., parkinsonism and other problems with movement) may respond to short-term use of anticholinergic agents such as atropine (Atropisol) or benztropine (Cogentin). This should be considered especially for patients who are opposed to restarting their tricyclic antidepressant.34
Antidepressant discontinuation syndrome: diagnosis, prevention and treatment
04/18/2017
UP TO ZMISTU NUMBER
Withdrawal symptoms may occur after discontinuation of any class of antidepressants. The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), apparently due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This condition is also called antidepressant withdrawal syndrome, although this is not entirely correct. The appearance of symptoms after stopping therapy does not mean that the drug is addictive. Antidepressants do not have addictive potential and do not cause addiction. This is an important positive point that should be communicated to patients, since most people will stop taking the prescribed treatment as soon as possible in case of fear of becoming dependent on the drug.
Why is it important to recognize antidepressant withdrawal syndrome?
There are three reasons: discomfort for the patient, diagnostic problem and possible compliance problems. Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
For example, consider two typical scenarios. Convinced of achieving remission of major depressive disorder, the doctor hurries to please the patient that the antidepressant can be stopped, but forgets to tell how to do it correctly. The patient takes everything literally and the next day forgets about the medicine. A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.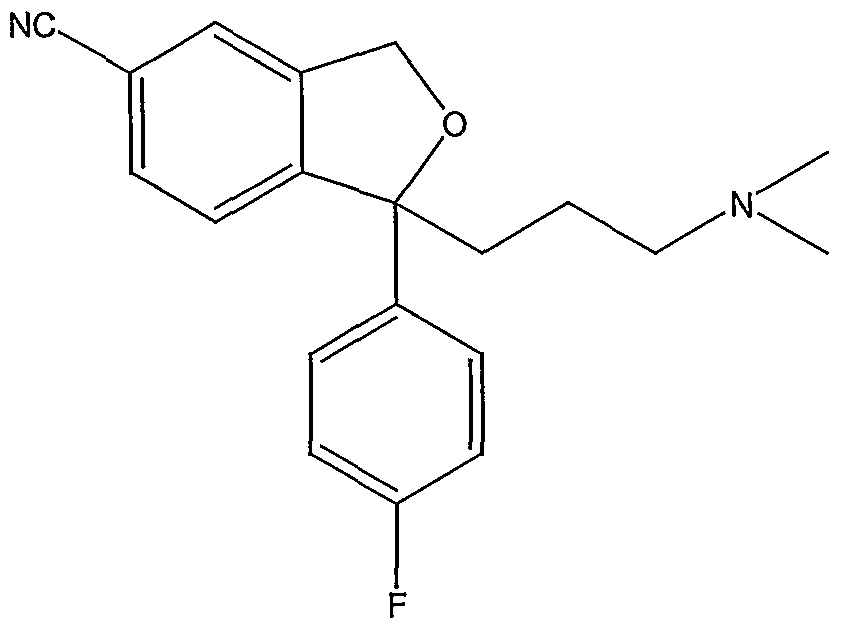
In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety.
Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
At first, information about the listed manifestations was accumulated from reports of clinical cases. Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy.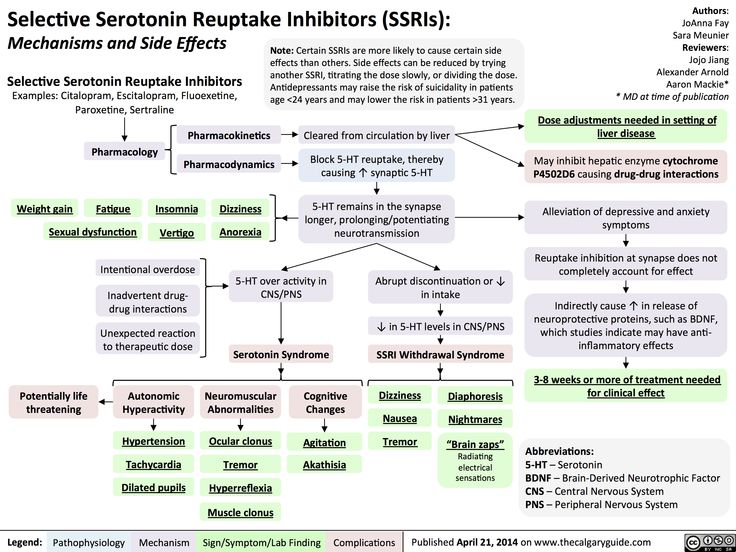
In English literature, a mnemonic device is used to memorize the spectrum of antidepressant withdrawal syndrome: the main symptoms are encrypted in the word FINISH.
F - from "flu-like" - flu-like symptoms;
I - insomnia;
N - from "nausea" - nausea;
I - from "imbalance" - imbalance;
S - sensory symptoms;
H - from "hyperarousal" - increased excitability, which reflects affective disorders.
It should be noted that the symptoms presented in the figure are mainly associated with discontinuation of SSRIs and serotonin and norepinephrine reuptake inhibitors. The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
When do withdrawal symptoms appear and how long do they last?
They usually appear within the first week after stopping the antidepressant; according to studies, on average on the second day. Spontaneous resolution occurs at different times - from 1 day to 3 weeks, on average, patients continue to experience symptoms for 10 days.
What causes withdrawal syndrome?
The syndrome occurs when all classes of antidepressants are discontinued. The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms.
For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
Can antidepressant discontinuation syndrome be distinguished from depression relapse?
Common symptoms include dysphoria, decreased appetite, sleep disturbances and fatigue. But there are also distinctive features—symptoms that are rarely seen in depression, such as sensory phenomena (paresthesias) as well as dizziness, headache, and nausea. In addition, in the case of withdrawal syndrome, a rapid (within 1 day) improvement can be observed when the drug is resumed, while recurrent depression does not respond so quickly to therapy.
Who is at risk for developing antidepressant withdrawal syndrome?
Typically, these are patients who begin to feel better after a few weeks of taking an antidepressant and are not sufficiently informed about the need for long-term maintenance therapy. Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
How to stop antidepressants to minimize the risk of withdrawal?
Patients should be explained in an accessible form the features of the action of the prescribed antidepressant, the rules for increasing and gradually reducing the dose, and warn about a possible deterioration in well-being with an abrupt cessation of therapy. But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned. However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.
But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned. However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.
If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms.
How to help patients who complain of feeling worse after stopping antidepressants?
If this does happen, explain to the patient that the symptoms are not life-threatening and usually resolve within a few days. If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
Literature
1. Haddad P.M., AndersonI.M. (2007). Recognizing and managing antidepressant discontinuation symptoms. Advances in Psychiatric treatment, 13(6): 447-457.
2. Warner C.H., Bobo W., Warner C., Reid S., Rachal J. (2006). Antidepressant discontinuation syndrome. American Family Physician, 74(3): 449-456.
3. Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Prepared by Dmitry Molchanov
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No. 1 (40), March 2017
21.10.2022 PsychiatryFrequency and variability of non-negligible cases and associations with antidepressants: results of a systematic review, netting meta-analysis and economic modeling
Great depressive discord affects approximately 350 million people in the whole world as the 13th cause of loss of health, followed by a global burden of illness [1, 2]. Antidepressants are the main means of treating the great depressive disorder. As previous studies have shown, drugs of the same class may have similar efficacy, but they may also vary significantly in the profile of side effects [3, 6-10]. Such manifestations as anxiety, sleeplessness, sexual dysfunction, changes in body mass, anhedonia (lack of satisfaction), are blamed practically on another patient's skin for depression, which can be overcome by the influx of antidepressants, which often become a cause [4]. Also, current recent data on side effects can help clinicians choose antidepressants to treat their patients....
Antidepressants are the main means of treating the great depressive disorder. As previous studies have shown, drugs of the same class may have similar efficacy, but they may also vary significantly in the profile of side effects [3, 6-10]. Such manifestations as anxiety, sleeplessness, sexual dysfunction, changes in body mass, anhedonia (lack of satisfaction), are blamed practically on another patient's skin for depression, which can be overcome by the influx of antidepressants, which often become a cause [4]. Also, current recent data on side effects can help clinicians choose antidepressants to treat their patients....
10/17/2022 PsychiatryPost-traumatic stress disorder in the minds of the military camp: space and possibility of phytotherapy Our viiSkovі struggle in the minds of trival, the sobbing of the sovereign Zhitta Sustyatyv, and our civilian is the country of the same novin, about the no -reasoning of the testing of the Teriye, we have a signs of the rocket of the rocket. It negatively affects the psycho-emotional state of people, so now not only psychiatrists, but representatives of other medical specializations and non-medical doctors can get stuck with post-traumatic stress disorder (PTSD) ....
It negatively affects the psycho-emotional state of people, so now not only psychiatrists, but representatives of other medical specializations and non-medical doctors can get stuck with post-traumatic stress disorder (PTSD) ....
10/17/2022 PsychiatryGamalate-V6 in the wake of the anxious states
The anxious state is an emotional discord, mindful of anxiety for the restlessness in front of the future podia or in a situation of innocence. These physical changes are accompanied by organic symptoms (psychosomatic illnesses). On the other hand, organic illness can be troublesome, as if causing illness, pain, suffering of the patient, disrupted by the rhythm of that special social life, just work. Sedative drugs, especially benzodiazepines and sedatives, are most commonly seen in anxiety states. ...
...
02.10.2022 Psychiatry Troubled discord in the practice of a family doctor: how can you safely repair it?
Scientific and practical conference “Until the Day of the Medical Practitioner (19.06.2022). International Conference on Advances in Health and Medical Science 2022 practitioners in various specialties for the development of topical nutrition and medical assistance to patients of a therapeutic profile. As part of the call, the professor of the Department of Internal Medicine of the Kharkiv National University named after I. V.N. Karazina, Doctor of Medical Sciences Marini Mykolaivna Kochueva "Anxious patient at the reception of a family doctor: how to recognize her safely repair?"....
Antidepressant withdrawal syndrome.
 How to survive?
How to survive? Do not stop your medications unless directed by your doctor. This is usually done gradually, the dosage is reduced every few days. But in the case of a phase inversion, when you switch from depression to hypomania or mania, withdrawal may occur more quickly.
If you're thinking of changing or stopping antidepressants, you need to know how your body might respond to chemical changes in your body, and it's even more important to know how you can ease withdrawal symptoms.
Best possible situation: you don't even need to read this article because there is no syndrome (hooray!).
Another option: you are experiencing withdrawal reactions, but you are ready for them and you know that they are temporary.
What to expect after stopping antidepressants
Many symptoms are associated with depression or anxiety, so it's worth keeping an eye on how you feel and how long it lasts. Often the withdrawal syndrome manifests itself as:
Don't stop antidepressants unless your psychiatrist tells you to.
It's easy to make the decision, "I don't want to burden the doctor" and start changing or stopping medication on your own. But please don't change anything unless your doctor tells you to, even if it's a small dose reduction. Antidepressants are helpful but potent, so it's important to consult a professional for the slightest change.
When you see a psychiatrist, ask how best to change your treatment. Usually, your doctor can make a plan to reduce your dosage instead of stopping abruptly. If you start a new medication, it is likely that it will be introduced gradually while lowering the level of the current medication. This will help alleviate withdrawal symptoms.
Get ready for panic attacks
You may feel panic during antidepressant withdrawal— either intermittently or continuously.
If you have already experienced panic attacks, use the techniques that are already suitable for you. If you haven't encountered them, place a paper bag next to your bed to breathe into during attacks. Practice deep breathing and count the objects in the room until your heartbeat stops.
Practice deep breathing and count the objects in the room until your heartbeat stops.
Cry
Tears go hand in hand with panic attacks. In some cases, you can be very tearful. Our advice is to cry if you want to. You shouldn't be ashamed of it, and honestly, thanks to tears, you can feel quite refreshed. Do not be afraid.
Free up time in case of withdrawal
Especially if you stop treatment completely, free up a week or two of hard work to deal with it. Even a couple of days off can help. Give yourself time to adjust.
Of course, not everyone can take a day off at any time, but you can start “putting away” medication before the weekend, or at least clear your schedule. If you're feeling really bad from withdrawal, stay in bed as much as you can. A long sleep will help you recover.
Don't forget to go to the store before starting to stop your medication. If you experience dizziness and panic, it will be difficult for you to leave the house until it passes.