Case study of dependent personality disorder
Dependent Personality Disorder | Abnormal Psychology
Learning Objectives
- Describe the characteristics and diagnosis of dependent personality disorder
Dependent Personality Disorder
Dependent personality disorder (DPD) is a cluster C personality disorder characterized by a pervasive psychological dependence on other people.
| Avoidant | socially inhibited and oversensitive to negative evaluation; avoids occupations that involve interpersonal contact because of fears of criticism or rejection; avoids relationships with others unless guaranteed to be accepted unconditionally; feels inadequate and views self as socially inept and unappealing; unwilling to take risks or engage in new activities if they may prove embarrassing | C |
| Dependent | allows others to take over and run their life; is submissive, clingy, and fears separation; cannot make decisions without advice and reassurance from others; lacks self-confidence; cannot do things on their own; feels uncomfortable or helpless when alone | C |
| Obsessive-Compulsive | pervasive need for perfectionism that interferes with the ability to complete tasks; preoccupied with details, rules, order, and schedules; excessively devoted to work at the expense of leisure and friendships; rigid, inflexible, and stubborn; insists things be done a certain way; miserly with money | C |
Dependent personality disorder (DPD) is a long-term condition in which people depend on others to meet their emotional and physical needs, with only a minority achieving normal levels of independence.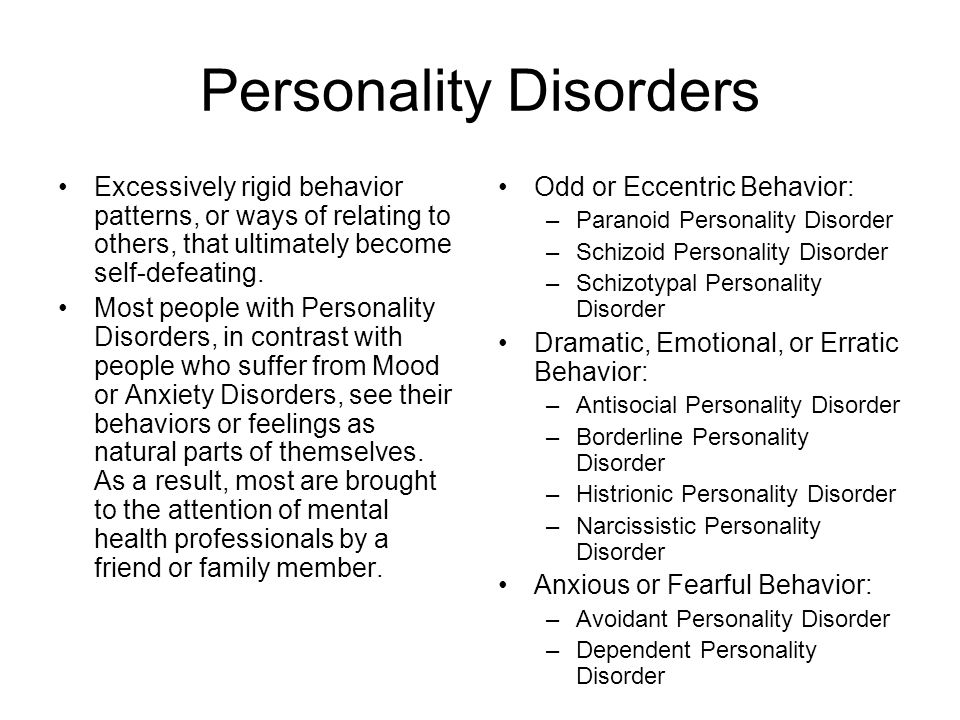 Dependent personality disorder (DPD) is characterized by excessive fear and anxiety. Dependent personality disorder (DPD) begins by early adulthood, is present in a variety of contexts, and is associated with inadequate functioning. Symptoms can include anything from extreme passivity, devastation, or helplessness when relationships end; avoidance of responsibilities; and severe submission.
Dependent personality disorder (DPD) is characterized by excessive fear and anxiety. Dependent personality disorder (DPD) begins by early adulthood, is present in a variety of contexts, and is associated with inadequate functioning. Symptoms can include anything from extreme passivity, devastation, or helplessness when relationships end; avoidance of responsibilities; and severe submission.
People who have dependent personality disorder are overdependent on other people when it comes to making decisions. They cannot make a decision on their own as they need constant approval from other people. Consequently, individuals diagnosed with DPD tend to place the needs and opinions of others above their own as they do not have the confidence to trust their decisions. This kind of behavior can explain why people with DPD tend to show passive and clingy behavior. These individuals display a fear of separation and cannot stand being alone. When alone, they experience feelings of isolation and loneliness due to their overwhelming dependence on other people.
DSM-5 Criteria
DSM-5 refers to dependent personality disorder as a pervasive and excessive need to be taken care of, which leads to submissive and clinging behavior and fears of separation. This behavior begins by early adulthood and can be present in a variety of contexts.
According to the DSM-5, the disorder is indicated by at least five of the following factors:
- has difficulty making everyday decisions without an excessive amount of advice and reassurance from others.
- needs others to assume responsibility for most major areas of their life.
- has difficulty expressing disagreement with others because of fear of loss of support or approval.
- has difficulty initiating projects or doing things on their own (because of a lack of self-confidence in judgment or abilities rather than a lack of motivation or energy).
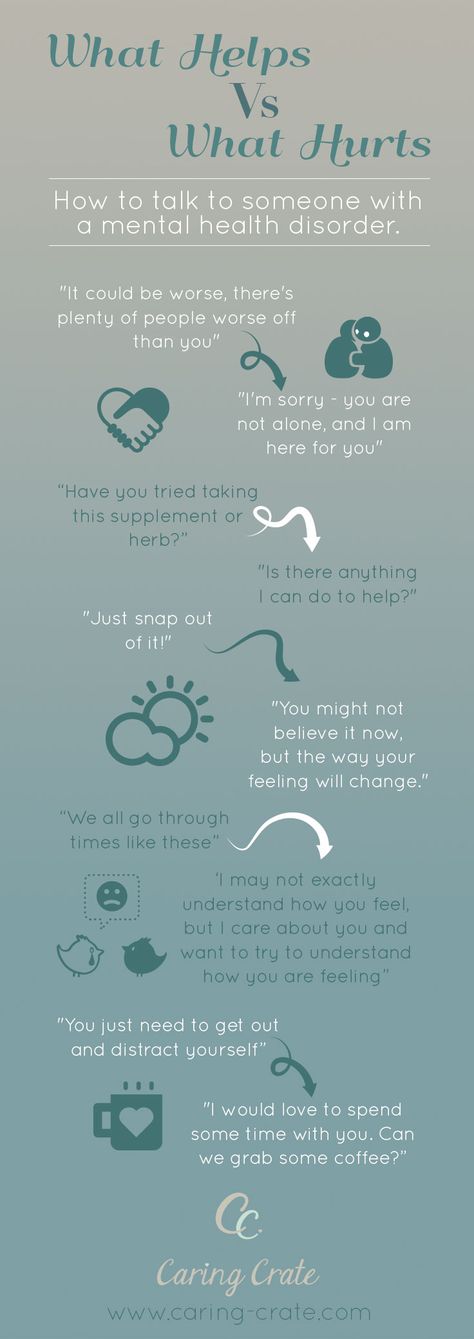
Figure 1. People with DPD can be clingy and may constantly need the approval of others.
- goes to excessive lengths to obtain nurturance and support from others, to the point of volunteering to do things that are unpleasant.
- feels uncomfortable or helpless when alone because of exaggerated fears of being unable to care for themselves.
- urgently seeks another relationship as a source of care and support when a close relationship ends.
- is unrealistically preoccupied with fears of being left to take care of themselves.
Differential Diagnosis
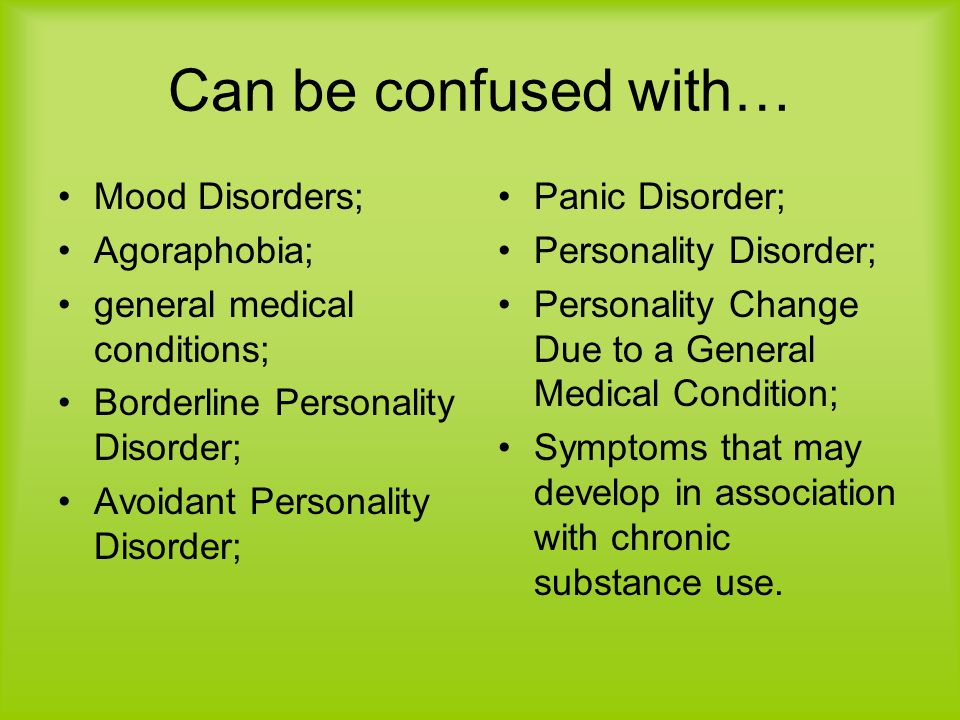
There are similarities between individuals with dependent personality disorder and individuals with borderline personality disorder in that they both have a fear of abandonment. Those with dependent personality disorder do not exhibit impulsive behavior, unstable affect, and poor self-image experienced by those with borderline personality disorder.
The following conditions are commonly comorbid with dependent personality disorder:
- mood disorders
- anxiety disorders
- adjustment disorder
- borderline personality disorder
- avoidant personality disorder
- histrionic personality disorder
Epidemiology
Based on a survey of 43,093 Americans, 0.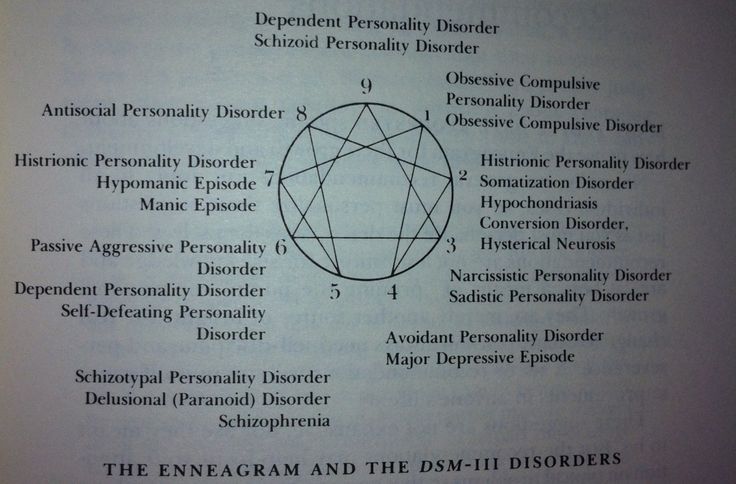 49% of adults meet diagnostic criteria for DPD (National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant et al., 2004). Traits related to DPD, like most personality disorders, emerge in childhood or early adulthood. DPD is more common among women compared to men as 0.6% of women have DPD compared to 0.4% of men. A 2004 twin study suggests a heritability of 0.81 for developing dependent personality disorder. Because of this, there is significant evidence that this disorder runs in families. Children and adolescents with a history of anxiety disorders and physical illnesses are more susceptible to acquiring this disorder.
49% of adults meet diagnostic criteria for DPD (National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant et al., 2004). Traits related to DPD, like most personality disorders, emerge in childhood or early adulthood. DPD is more common among women compared to men as 0.6% of women have DPD compared to 0.4% of men. A 2004 twin study suggests a heritability of 0.81 for developing dependent personality disorder. Because of this, there is significant evidence that this disorder runs in families. Children and adolescents with a history of anxiety disorders and physical illnesses are more susceptible to acquiring this disorder.
Etiology
Figure 2. Overprotective parenting behavior is a risk factor for DPD.
The exact cause of dependent personality disorder is unknown. A study in 2012 estimated that between 55% and 72% of the risk of the condition is inherited from one’s parents. The difference between a dependent personality and a dependent personality disorder is somewhat subjective, which makes diagnosis sensitive to cultural influences such as gender role expectations.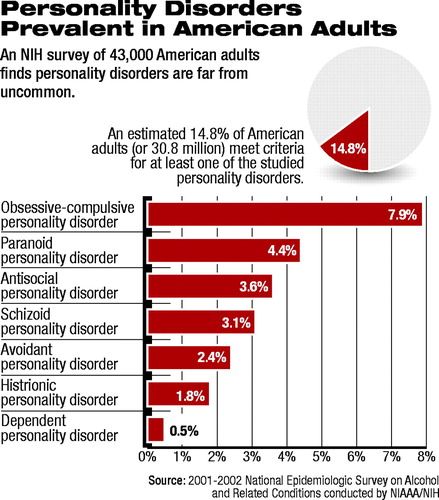 There is a higher frequency of the disorder seen in women than men.
There is a higher frequency of the disorder seen in women than men.
Dependent traits in children tended to increase with parenting behaviors and attitudes characterized by overprotectiveness and authoritarianism. Traumatic or adverse experiences early in an individual’s life, such as neglect and abuse or serious illness, can increase the likelihood of developing personality disorders, including dependent personality disorder, later on in life. This likelihood is especially prevalent for those individuals who also experience high interpersonal stress and poor social support.
Treatment
People who have DPD are generally treated with psychotherapy. The main goal of this therapy is to make the individual more independent and help them form healthy relationships with the people around them. This is done by improving their self-esteem and confidence.
Medication can be used to treat patients who suffer from depression or anxiety because of their DPD, but this does not treat the core problems caused by DPD.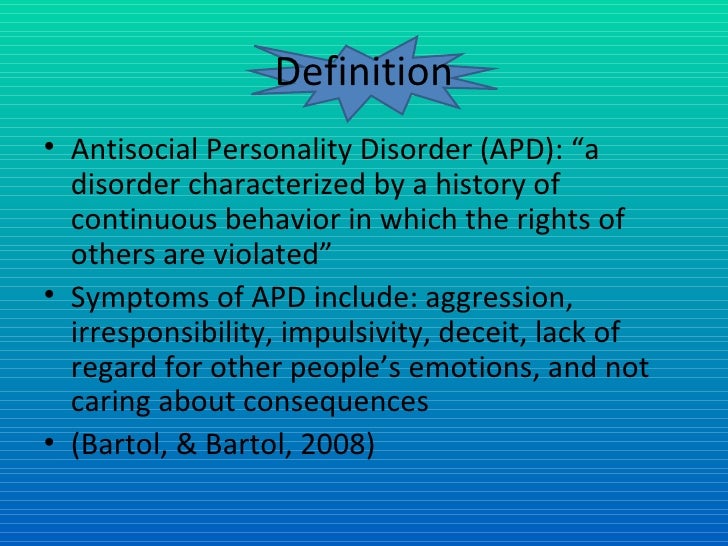
Key Takeaways: Dependent personality disorder
Case Study: DEPENDENT PERSONALITY DISORDER
This case study looks at the patient of a 27-year-old, white female named Sally. She works as an administrative assistant whose work required extensive data entry. Sally’s mother used her network to get this stable job for her daughter. Sally is consumed with pleasing her mother and even asks for her mother’s advice on what to wear to the office each day. Sally consistently worries about pleasing others and her colleagues at work, even at the expense to herself, which leads to the diagnosis of dependent personality disorder. The degree to which her self-destructive passivity and compliance at work stemmed from her early experiences within the family are unclear, but her parents’ overprotectiveness likely played some role in the etiology of her personality pathology.
Watch IT
This video describes the diagnostic criteria and treatment options for dependent personality disorder.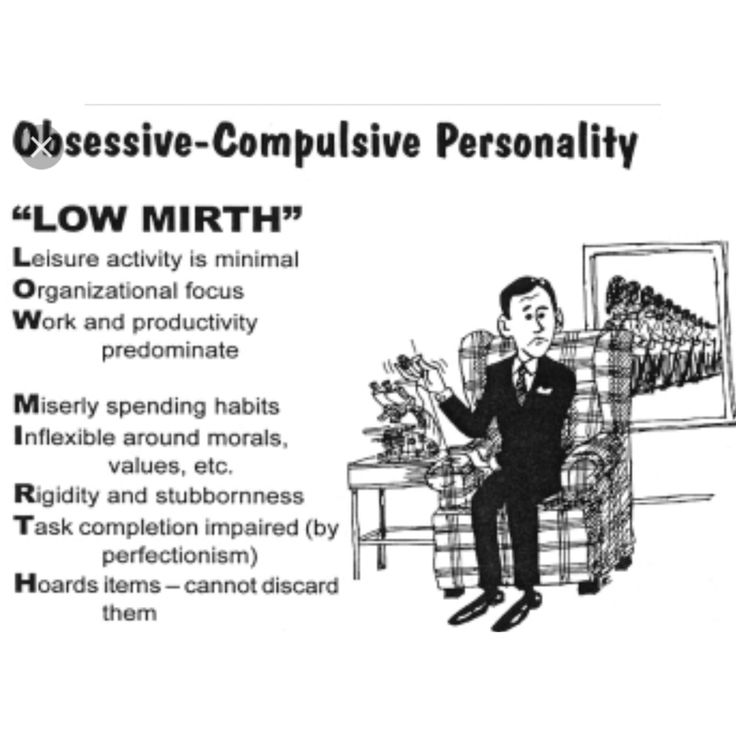
You can view the transcript for “What is Dependent Personality Disorder?” here (opens in new window).
Try It
Glossary
dependent personality disorder (DPD): a personality disorder characterized by a pervasive and excessive need to be taken care of, leading to a lack of independent action
The Dependent Patient - A Case Study
Sam Vaknin
Obtain insight into co-dependence. Read therapy notes from patient diagnosed with Dependent Personality Disorder.
Notes of first therapy session with Mona, female, 32, diagnosed with Dependent Personality Disorder (or Codependence)
"I know I won't actually die, but it often feels like it." - says Mona and nervously pats her auburn hair - "I can't live without him, that's for sure. When he is gone, it's like life switching from Technicolor to black and white. There is no excitement, this electricity in the air that seems to constantly surround him.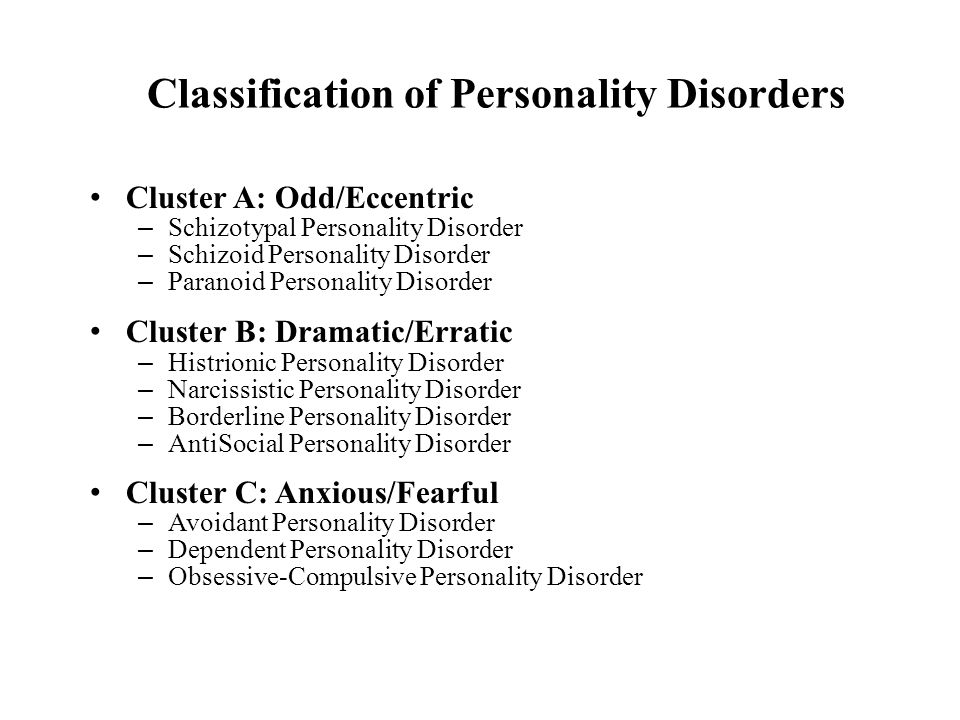 " She misses him so much that it physically hurts. Sometimes she feels like throwing up at the mere thought of separating or being abandoned by him. She is helpless without him: "He is so masterful and knows how to fix things around the house." He is gorgeous and a great lover.
" She misses him so much that it physically hurts. Sometimes she feels like throwing up at the mere thought of separating or being abandoned by him. She is helpless without him: "He is so masterful and knows how to fix things around the house." He is gorgeous and a great lover.
Is he intellectually stimulating? Do they talk a lot? She moves uncomfortably in her seat: "He is more the silent strong type." She is supporting him financially. "He is studying". In the last seven years he had switched from psychology to political science to physical therapy. How long will she underwrite his quest for self-realization? "As long as it takes. I love him".
She acknowledges that he is verbally and sometimes physically abusive. He has cheated on her more times than she can count, usually with classmates at the university. So, why is she still with him? "He has his good sides". Do they outweigh his bad ones? She is evidently displeased with my question but is reluctant to express her reservations.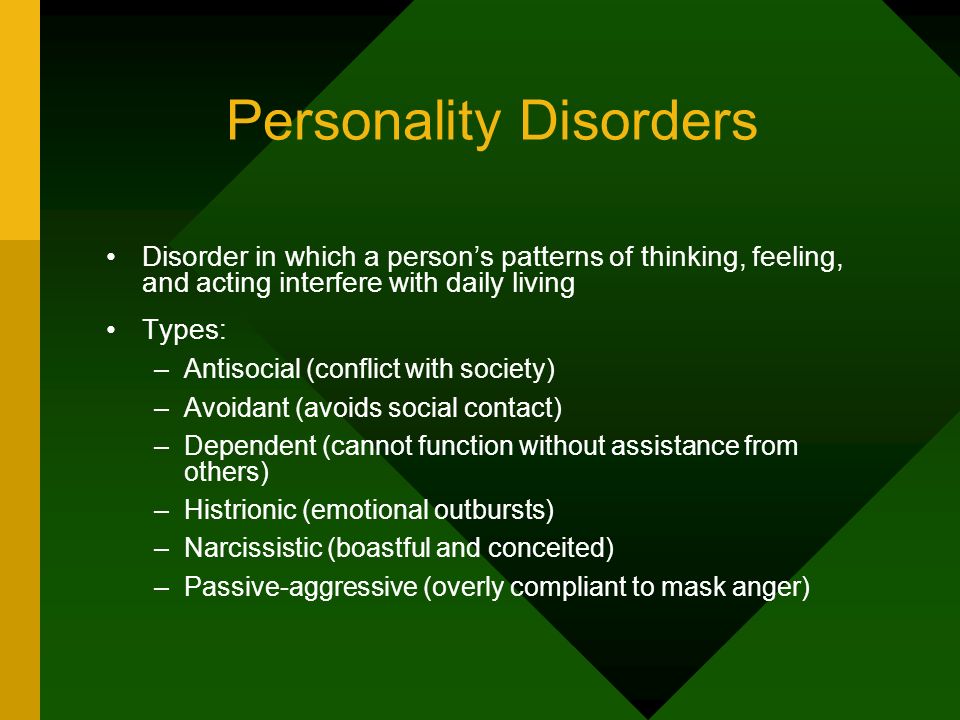
I tell her that - her intimate partner having refused to attend therapy - I am merely trying to get to know him better if only by proxy. Evidently something is bothering her, otherwise we wouldn't be having this therapy session. "I want to learn how to hold on to him."- she whispers - "He is a very special man and has special needs. I am looking for guidance on how to hook him. I want him to become addicted to me, like a junkie." She even participated in group sex once or twice to make his fantasies come true.
Does this strike her as the basis for a healthy relationship? She doesn't care. She consulted all her friends and even casual acquaintances but she doesn't know whether to trust them. Does she have many friends? Not any more. Why not? People get tired of her, they say that she is clinging. But that's not true - she only asks their advice on a regular basis. "What are friends for, anyhow?"
Does she have a job? She is a lawyer, but her dream is to become a film director. She vividly and enthusiastically describes what she would do behind the camera. What's holding her back? She laughs self-deprecatingly: "Except for mediocre talent, nothing."
She vividly and enthusiastically describes what she would do behind the camera. What's holding her back? She laughs self-deprecatingly: "Except for mediocre talent, nothing."
This article appears in my book, "Malignant Self Love - Narcissism Revisited"
next: The Obsessive-Compulsive Patient ~ back to: Case Studies: Table of Contents
APA Reference
Vaknin, S. (2009, October 1). The Dependent Patient - A Case Study, HealthyPlace. Retrieved on 2023, January 10 from https://www.healthyplace.com/personality-disorders/malignant-self-love/dependent-patient-a-case-study
Last Updated: July 5, 2018
Medically reviewed by Harry Croft, MD
Coping with Stalking and Stalkers - Domestic Violence Shelters
A Great Admiration (Narcissism and Grandiose Fantasies)
The Psychology of Serial and Mass Killers
The Narcissist in Therapy
Personality Disorders as an Insanity Defense
The Guilt of the Abused - Pathologizing the Victim
Exposure of the Narcissist - Excerpts Part 10
How to keep addictive personality disorder from blooming
July 6, 2021 Likbez Health
If you have grown up a long time ago, but still cannot live without care, it may be time to see a doctor.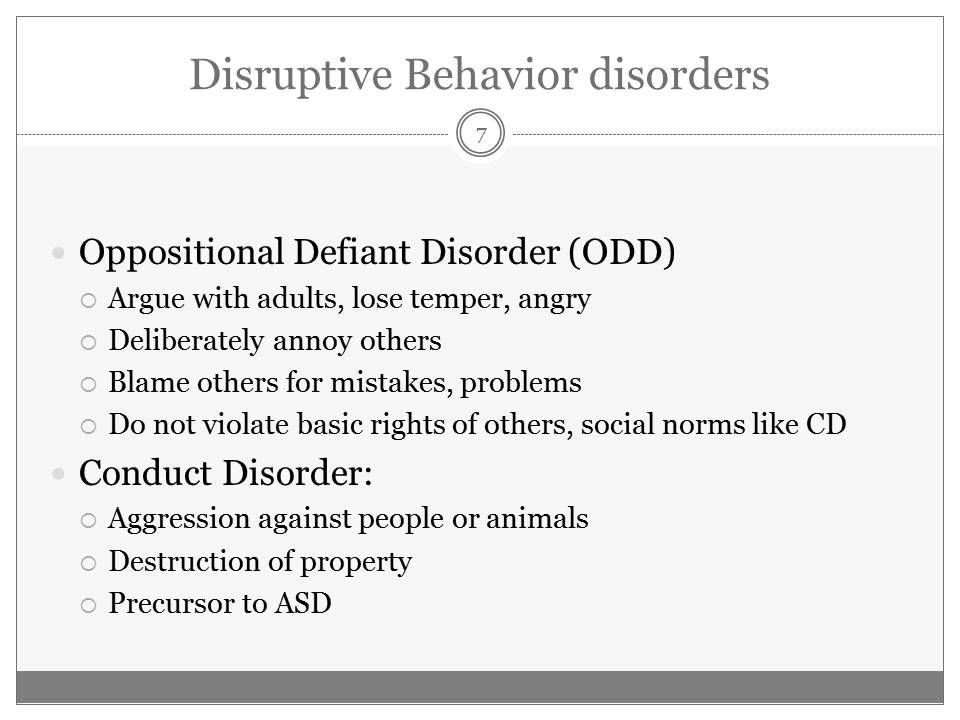
You can also listen to this article. If it's more convenient for you, turn on the podcast:
What is Dependent Personality Disorder
This is a mental disorder. People with dependent personality disorder find it difficult to make any decisions on their own, so they obey others. They often shift responsibility to someone else, are afraid to be alone, feel helpless and put other people's desires above their own. nine0003
Usually this deviation is found in young people. Both men and women suffer from it.
Other problems may appear along with the disorder: depression, phobias, anxiety, substance abuse. Sometimes people become victims of abusers. This is because, due to the fear of loneliness, it is difficult for them to part with a dominant partner.
Where addictive personality disorder comes from
No one knows for sure, but scientists suggest that it appears due to developmental and biological factors. For example, a person who grew up in strictness or overprotectiveness, in childhood was often ill and anxious due to separation from someone, is more at risk of experiencing a disorder.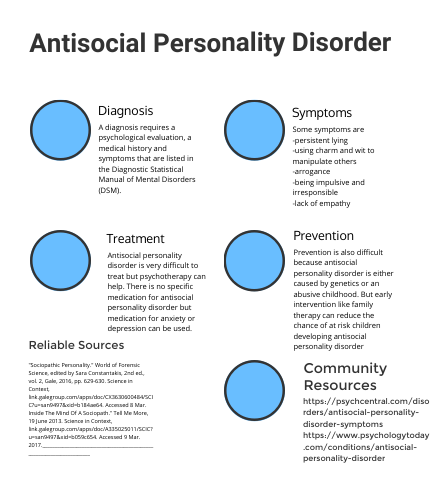 nine0003
nine0003
How to recognize dependent personality disorder
The Diagnostic and Statistical Manual of Mental Disorders lists eight main symptoms. To suspect a dependent personality disorder, it is enough to notice five signs.
1. Difficulty making everyday decisions
A person with a dependent disorder often needs someone else's advice or guidance. For example, he may depend on a spouse who tells you what to wear, where to work, and who to hang out with. nine0003
2. The need to shift responsibility for one's life to someone else
People with disabilities see themselves as inferior and think that they cannot take care of themselves. They become followers in order to get others to patronize them. Any criticism is perceived as proof of its failure.
3. Fear of disagreeing
If the opinion of a person with this disorder differs from someone else's, it will be difficult for him to express himself. Because of the fear of losing approval, he is more likely to agree with what he does not like. Moreover, for fear of losing support, he will not be angry with his loved ones, even if anger is appropriate. nine0003
Moreover, for fear of losing support, he will not be angry with his loved ones, even if anger is appropriate. nine0003
4. Difficulties with own projects
People with this disorder believe that they cannot do anything alone. Therefore, it is difficult for them to work independently or take on tasks that require personal responsibility. They consider themselves incompetent and seek someone's help. If the boss controls or approves, the person with a dependent disorder is more likely to act appropriately. But because of the fear of being abandoned, he is unlikely to have a desire to become a professional himself. nine0003
5. Willingness to make big concessions
Dependency disorder can cause a person to endure physical and emotional abuse, agree to unreasonable demands, and take on unpleasant assignments. He thinks that being submissive will help him get support.
6. Discomfort from loneliness
Staying with oneself is unpleasant for a person. He feels helpless and afraid that he won't be able to take care of himself.
7. Tendency to establish relationships with those who will help
People with the disorder tend to enter into relationships with those they can depend on. When the relationship ends, they immediately look for a replacement partner. The need for care leads to promiscuity.
8. Fear of being alone
Even if the threat of being left alone is unrealistic, a person with a dependent disorder will still be afraid of losing their "guardian".
How Dependent Personality Disorder is Treated
Most often, people are not even aware of the disorder. They seek help when problems arise that cannot be dealt with alone. For example, depression or anxiety. nine0003
If the patient has signs of an addictive disorder, the therapist starts an examination. First, he collects an anamnesis and conducts a basic examination. Sometimes people are sent for tests. This is necessary to exclude physical diseases, due to which the symptoms of the disorder may also appear.
The next step is a visit to a psychotherapist or psychiatrist. These specialists have questionnaires and tests to diagnose disorders. But even here it is not so simple. It is easy to confuse dependent disorder with borderline because of the similar symptoms. But still there are differences. For example, people with the first type, because of the fear of loneliness, become submissive or look for new relationships, with the second, they react with anger, they have a feeling of emptiness. nine0003
A psychiatrist or psychotherapist prescribes therapy when an accurate diagnosis is made.
Psychotherapy
This is the main treatment that helps people with addictive disorder to become more active and build normal relationships with others. There are several suitable types of psychotherapy.
- Social skills training. Helps you understand verbal and non-verbal cues during communication, keep a conversation going and communicate with confidence.
 In therapy, the patient may be offered role-playing games and simulations. This type of treatment is often combined with others. nine0077
In therapy, the patient may be offered role-playing games and simulations. This type of treatment is often combined with others. nine0077 - Cognitive behavioral therapy. Needed by patients to become more self-confident. In the classroom, people with a disorder try to change their opinion of themselves and their abilities, struggle with destructive beliefs and fear of judgment.
- Circuit therapy. Based on the fact that a person has a set of behaviors that he repeats throughout his life. Some of them may turn out to be maladaptive, that is, incorrect. Treatment aims to reinforce healthy patterns and eradicate unhealthy ones. Another psychotherapist may emphasize the re-education of the patient in order to meet his childhood needs. For example, a doctor will praise, set limits, and provide secure attachment. Also during therapy, a person with a disorder gains knowledge about basic needs, functional and dysfunctional behavior. nine0077
- Mindfulness-based cognitive therapy.
Helps to assess yourself and your strengths. Patients who underwent therapy learned to be more attentive to their hunches, emotions, and communication with others. For example, some people realize that “I am helpless” or “I am weak” attitudes are just thoughts, not facts.
Medications
Doctors rarely prescribe drugs to treat addiction. But if a person has anxiety or depression, they may be prescribed monoamine oxidase inhibitors or selective serotonin reuptake inhibitors. nine0003
How to help yourself if you have a dependent personality disorder
Psychotherapy is the best way to get rid of the disorder. But treatment can be supplemented with self-help. Here are some tips to help you deal with addictive personality disorder faster.
Enjoy your company
Think about what you can do when you are alone. It could be yoga classes, ten minutes of meditation, or reading a book during your lunch break.
Pick up a hobby
Ask yourself some questions. What would you like to know about? What brought you joy as a child? What subjects did you like the most at school? Perhaps the answers will tell you what you would be interested in doing in your free time.
What would you like to know about? What brought you joy as a child? What subjects did you like the most at school? Perhaps the answers will tell you what you would be interested in doing in your free time.
Maintain your independence
Make a list of the things someone else does for you. Then find one small task that you can take on. Consider this an opportunity to grow, hone your skills, and build your confidence. nine0003
Develop a healthy relationship with yourself
Start small: think about what you like about yourself and give a compliment. Relax and get some sleep. Try self-compassion meditation to accept your shortcomings and stop criticizing yourself.
Read also 😣😮😫
- What is bipolar affective disorder and how to live with it
- How to recognize and deal with histrionic personality disorder
- 9 symptoms of obsessive-compulsive disorder that should not be ignored
- When passive aggression becomes a personality disorder and what to do about it
- How to recognize alcoholism, depression and other mental disorders
Dependent Personality Disorder
Dependent personality disorder.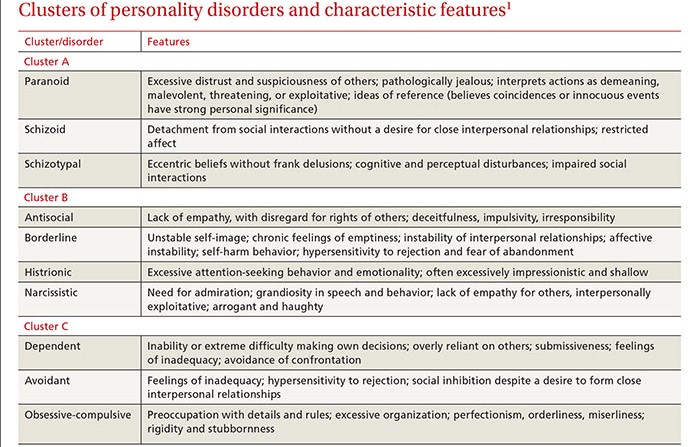
Addiction and affection are considered universal and perhaps defining forms behavior in mammals (Frances, 1988). rely to some extent on others - it is certainly adaptive behavior but overdependence can create significant problems and extreme forms of dependence are defined in DSM-III how dependent personality disorder (PDD) (ARA, 1980). In the treatment of SPD, a psychotherapist faces an interesting dilemma. AT at the beginning of psychotherapy, these patients may seem easily cured. They are so attentive and receptive to effort psychotherapist that he can finally breathe a sigh of relief after work with many other patients who clearly do not listen to the therapist or do not respect his words. These patients are easily involved in the process. treatment, and they are so disposed to cooperation at the beginning of psychotherapy, that there is hope for a very fast progress. But such expectations exacerbate the psychotherapist's frustration at later stages of treatment, when these patients are clearly clinging to treatment, resisting the efforts of the psychotherapist, aimed at encouraging them to be more autonomy. nine0003
nine0003
hill (Hill, 1970) lists some of the difficulties work with these patients, describing initial improvement in the addict's condition patient: "The patient feels revitalized because some new person shows interest in her her need for dependency and offers a more worthwhile life for her ... But the state any patient invariably returns to the original when she realizes that psychotherapy is not a passive experience" (p. 39). Help the patient to acted independently of the psychotherapist, and encouraging his autonomy from the therapist and other significant people for the patient is the most difficult task in work with ZRL. nine0132 Historic review.
First descriptions of addicted people were often derogatory. In the work of psychiatrists XIX century passivity, inefficiency and excessive obedience, characteristic of these patients were considered as failures in moral development, and for descriptions of these people were used terms like "helpless", "weak-willed" and "degenerates".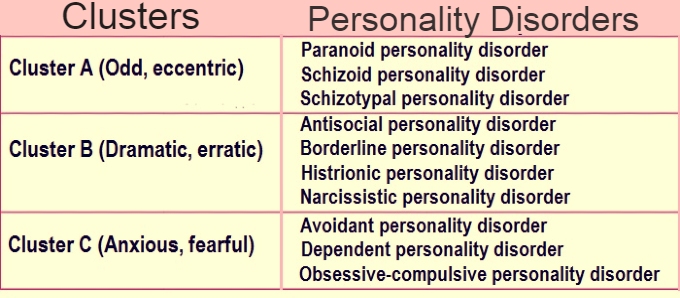 Although overly dependent personality type was noted quite often, in the most early classification systems no diagnosis. nine0003
Although overly dependent personality type was noted quite often, in the most early classification systems no diagnosis. nine0003
Absolutely a different point of view was held by the early theorists of psychoanalysis. Both Freud and Abraham described "oral-receptive" character as a result of either excessive indulgence, or deprivation on the oral, or infant, stage of development. Abraham (1924/1948) stated: some people are dominated by the belief that there will always be some a kind person - of course, a substitute mother, to take care of them and give them everything they need. it optimistic conviction dooms them to inaction ... They do not undertake no effort and in some cases even considered below their dignity earn your own bread" (p. 399-400).
predecessor diagnostic categories passive-aggressive and dependent personality types were related to World War II period concept "immature response", defined as "reaction of a neurotic type to ordinary military stress, manifested in helplessness or inadequate reactions, passivity, obstructionism or outbursts of aggression” (Anderson, 1966, p.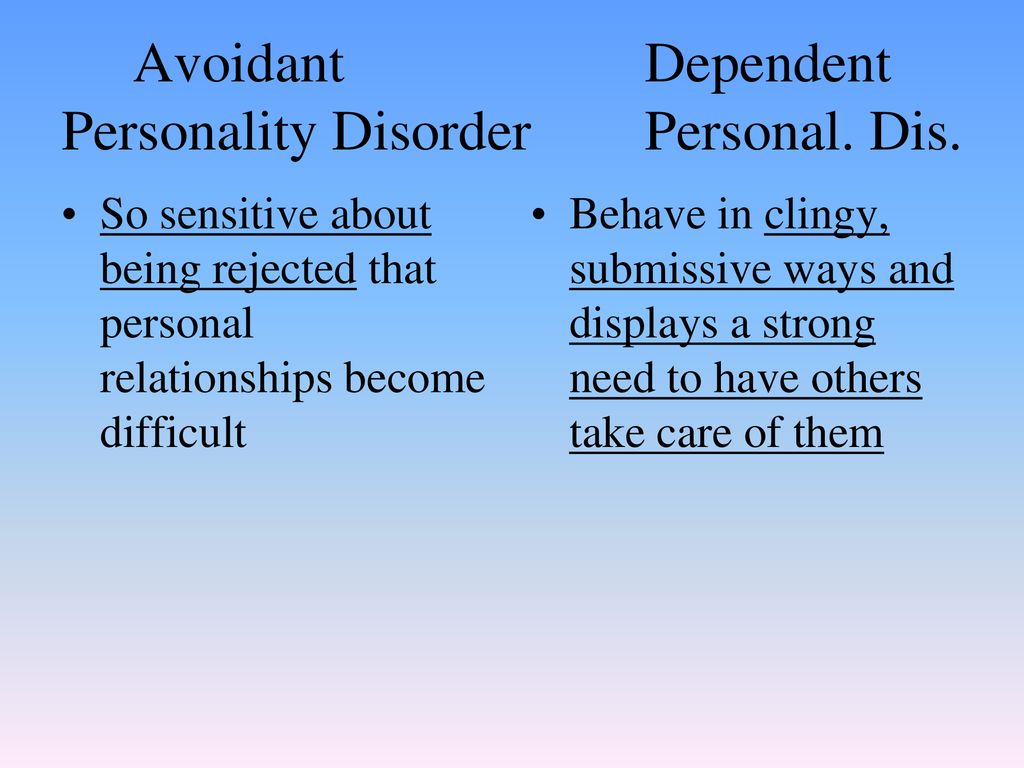 756). The addict was only briefly mentioned in DSM-I (ARA, 1952) as a passive dependent subtype passive-aggressive disorder characterized by inadequate attachment due to frustration, caused by the environment. concept "dependent personality" absent at DSM-II (ARA, 1968), and the closest category was an inadequate personality, characterized "ineffective responses to emotional, social, intellectual and physical incentives. Although the patient does not appear physically or mentally ill, he poorly adapted, unintelligent, unreasonable, socially unstable and is characterized by a lack of physical and emotional endurance” (p. 44).
756). The addict was only briefly mentioned in DSM-I (ARA, 1952) as a passive dependent subtype passive-aggressive disorder characterized by inadequate attachment due to frustration, caused by the environment. concept "dependent personality" absent at DSM-II (ARA, 1968), and the closest category was an inadequate personality, characterized "ineffective responses to emotional, social, intellectual and physical incentives. Although the patient does not appear physically or mentally ill, he poorly adapted, unintelligent, unreasonable, socially unstable and is characterized by a lack of physical and emotional endurance” (p. 44).
Using as the basis of classical polarity "active-passive", "pain-pleasure" and "I-others", Millon (Millon, 1969) created classification, which distinguishes 8 basic personality types. passive dependent pattern (originally known as submissive personality highlighted by Millon) involves seeking pleasure and pain avoidance as well as passive hope that other people will satisfy these needs.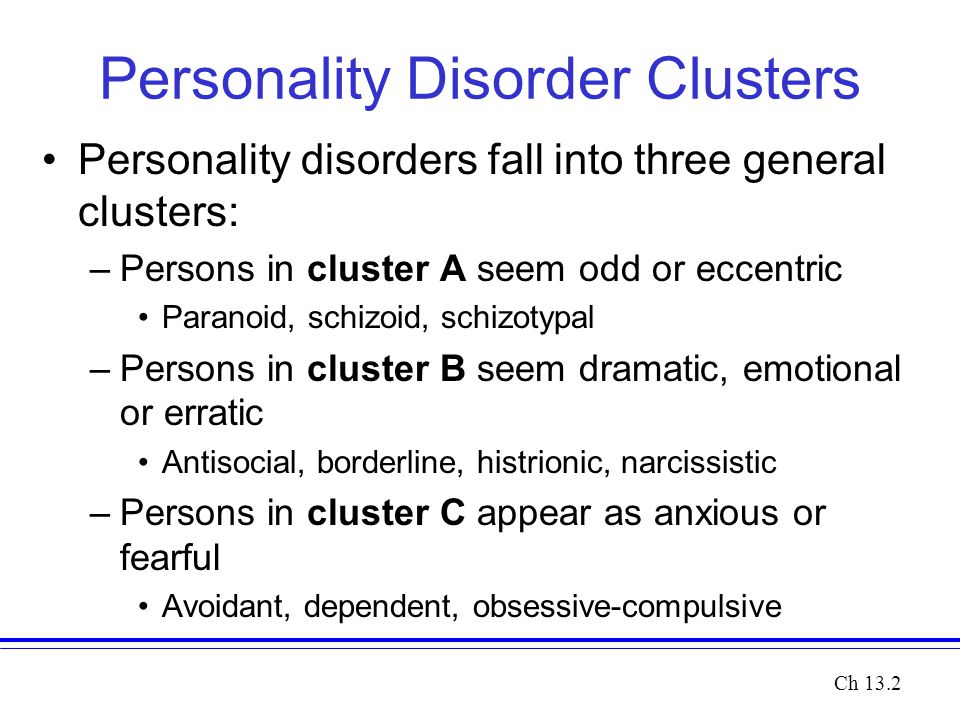 This classification was expanded in several works by Millon, resulting in the formulation concept of "addictive disorder" personality", first introduced in DSM-III (APA, 1980).
This classification was expanded in several works by Millon, resulting in the formulation concept of "addictive disorder" personality", first introduced in DSM-III (APA, 1980).
According to modern psychodynamic interpretation SPD, overindulgence or deprivation can lead to excessive and maladaptive dependency resulting from fixation on oral (infant) stages of development. In my study Levi's excessive mothering (Levy, 1966) suggests that excessive indulgence leads to the development of overly dependent traits such as dependency, disadvantage initiatives and demands on others to they did for these people what they they cannot do it themselves. In some cases of overdependence seen as regressive expression of unsatisfied phallic desires in women who hope that through addiction they will get a penis, necessary, in their opinion, to improve self-assessments (Esman, 1986). Esman (Esman, 1986) emphasizes the importance of hidden and unconscious hostility to significant for a dependent person to people and overkill sweetness and submissiveness, considered as jet formations directed against the expression of hostile feelings, that could threaten existence relationships that are considered vital.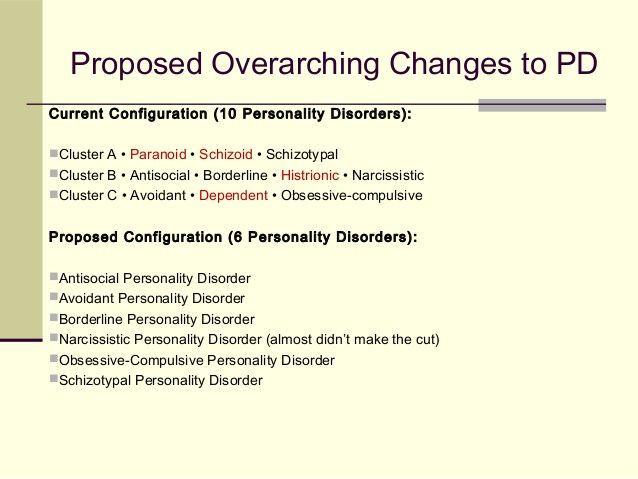
West and Sheldon (West & Sheldon, 1988) consider PPD as an obvious example of a disorder attachment system, which is the most fully discussed in the works of Bowlby (Bowlby, 1969, 1977). attachment pattern, the most typical for ZRL is "anxious attachment" pattern, which, according to Bowlby, arises on the basis of experiences leading to the fact that a person begins to doubt the availability and responsiveness of the figure to which he attached. When these people set relationships, they become overly dependent and live in constant fear loss of object of affection.
Research attachments and addictions continued Pilkonis (Pilkonis, 1988). He used modified prototype method to justify differentiated approach to the concepts of overdependence and excessive autonomy, which followed by clinicians who have experience in the treatment of depression. signs excessive addictions are grouped into two subtypes: indicators of "anxious attachments" and features, usually associated with borderline disorder personality. Subtype characteristics "anxious attachment" (including items such as "tend to too dependent on other people, "rejection by another person leads to loss of trust and self-esteem" and "usually feeling helplessness"), apparently the most closely match the diagnosis. ZRL. nine0132 Characteristics ZRL.
Subtype characteristics "anxious attachment" (including items such as "tend to too dependent on other people, "rejection by another person leads to loss of trust and self-esteem" and "usually feeling helplessness"), apparently the most closely match the diagnosis. ZRL. nine0132 Characteristics ZRL.
According to DSM-III-R (ARA, 1987, b. 354), an essential feature of the ZRL consists in the "total pattern of dependent and submissive behavior that occurs in early adulthood and manifested in different contexts” (see Table 13.1). These people are unable or unwilling to accept everyday decisions if they don't have lots of advice and support from other people and until agree with what others have to say people. They have difficulty getting started realization of their intentions or independent actions, feeling such discomfort in loneliness that can go to any lengths not to stay one. They feel empty and helplessness when close relationships run out and are usually preoccupied fear of being abandoned.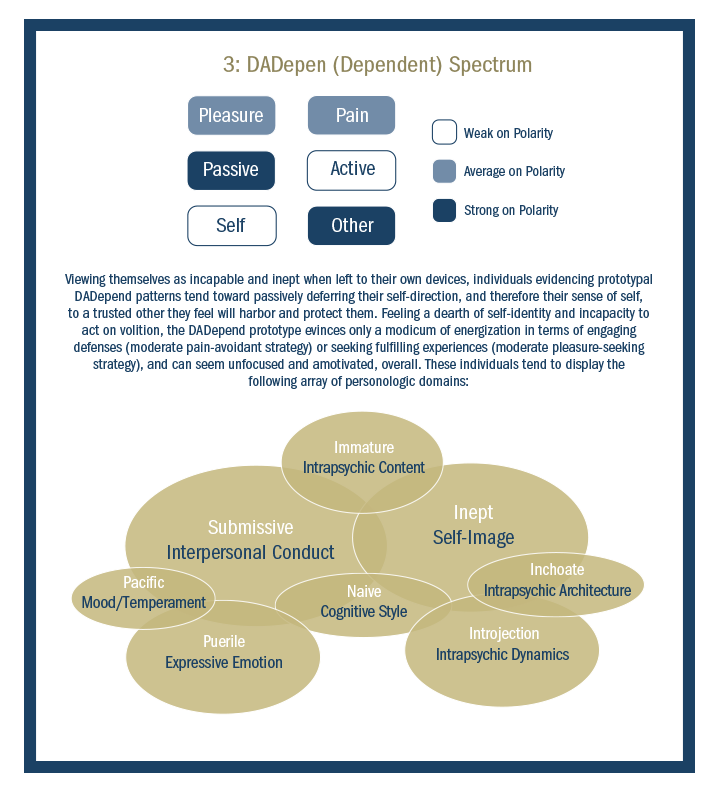 They are vulnerable to disapproval, tend to obey other people and will do anything to make them please. They are so afraid rejections that will agree with surrounding in everything, even if they believe that the person is wrong. Such people experience lack of self-confidence and tendency to underestimate one's abilities and strength. With ZRL one of the most common problems is depression. In fact, major depression and adaptation disorder are diagnoses Axes I, which are most often linked with ZRL Koenigsberg, Kaplan, Gilmour and Cooper (Koenigsberg, Kaplan, Gilmore, & Cooper, 1985). Using the criteria of personality questionnaires, Reich and Noyes (1987) found that that 54% of the studied depressive patients were diagnosed with ADHD. Overholser, Kabakoff and Norman (Overholser, Kabakoff, & Norman, 1989) point out, that the SRL criteria contain many features, commonly associated with depression, including lack of initiative helplessness and difficulty accepting solutions. Because they are excessive rely on support and care from sides of others and feel their own helplessness in front of the potential rupture of relations, they, apparently, are more prone to depression (Birtchnell, 1984; Zuroff & Mongrain, 1987).
They are vulnerable to disapproval, tend to obey other people and will do anything to make them please. They are so afraid rejections that will agree with surrounding in everything, even if they believe that the person is wrong. Such people experience lack of self-confidence and tendency to underestimate one's abilities and strength. With ZRL one of the most common problems is depression. In fact, major depression and adaptation disorder are diagnoses Axes I, which are most often linked with ZRL Koenigsberg, Kaplan, Gilmour and Cooper (Koenigsberg, Kaplan, Gilmore, & Cooper, 1985). Using the criteria of personality questionnaires, Reich and Noyes (1987) found that that 54% of the studied depressive patients were diagnosed with ADHD. Overholser, Kabakoff and Norman (Overholser, Kabakoff, & Norman, 1989) point out, that the SRL criteria contain many features, commonly associated with depression, including lack of initiative helplessness and difficulty accepting solutions. Because they are excessive rely on support and care from sides of others and feel their own helplessness in front of the potential rupture of relations, they, apparently, are more prone to depression (Birtchnell, 1984; Zuroff & Mongrain, 1987).
table 13.1. Criteria for dependent disorder identity according to DSM-III-R
Total pattern of dependent and submissive behavior, occurring in early adulthood and appearing in different contexts indicated by at least five signs of the following:
1) unable to take daily solutions without a lot of advice or support of others;
2) allows others to take over most important decisions where to live, what kind of work to get; nine0003
3) out of fear of rejection agrees with people, even when he believes that they are not right;
four) having difficulty getting started own intentions or independent actions;
five) voluntarily makes unpleasant or humiliating things to please other people;
6) feels uncomfortable or helpless alone or goes to great lengths to not be alone;
7) Feeling empty or helpless when close relationships end; nine0003
8) often preoccupied with the fear that quit;
nine) vulnerable to criticism or disapproval.
Note. From "Guidelines for the diagnosis and statistical classification of mental disorders" (3rd ed., revised), ( Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.). American Psychiatric Association, 1987, Washington, DC: Author, p. 354). ©1987, American psychiatric association. reproduced with permission.
Among people with ADHD are also common anxiety disorders. Since in matters of survival they count on others, they are especially prone to anxiety, associated with parting, and are worried about being abandoned and left alone. When they wait and fear new responsibilities, with whom they think they don't cope, they can happen panic attacks. Phobias tend to call for care and protection others, as well as avoidance of responsibility, providing a secondary benefit that fully consistent with the main dependent orientation of these people (Millon, 1981). Reich, Noyce and Troughton in their study of patients with panic disorder (Reich, Noyes, & Troughton, 1987) found that ZRL is the most common Axis II diagnosis, especially in subgroups with phobic avoidance. Depending on the used instrument, about 40% of those examined with phobic avoidance satisfied the criteria of the SRL. In addition, in the sample psychiatric patients Overholser and colleagues (Overholser, Kabakoff, & Norman, 1989) found in dependent patients profiles MMPI, speaking about the presence of anxiety, self-doubt and social alertness, regardless on the level of depression.
Depending on the used instrument, about 40% of those examined with phobic avoidance satisfied the criteria of the SRL. In addition, in the sample psychiatric patients Overholser and colleagues (Overholser, Kabakoff, & Norman, 1989) found in dependent patients profiles MMPI, speaking about the presence of anxiety, self-doubt and social alertness, regardless on the level of depression.
Others characteristic problems of people with ADHD are somatic complaints, conversion symptoms to hypochondria, and somatization. In the study of 50 passively dependent women who were treated as outpatients, Hill (Hill, 1970) found that all women had somatic complaints, which usually resulted in to increased attention to them from families and professionals. Many of these patients resorted to medication treatment as the main opportunity to help yourself. Greenberg & Dattore (Greenberg & Dattore, nineteen81) found that people with somatic diseases (cancer, benign tumors, hypertension, or stomach ulcers) in the premorbid period had significantly higher scores for related scale dependent MMPI , than people who did not have such diseases in over a 10 year period.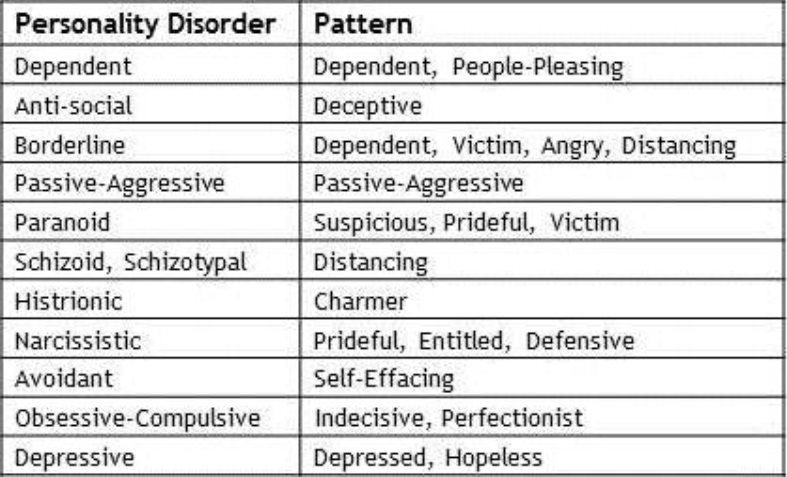 similar way Vaillant (Vaillant, 1978) and Hinkle (Hinkle, 1961) found an association between dependent personality traits and general predisposition to illness. In a recent review of empirical Literature Greenberg and Bornstein (Greenberg & Bornstein, 1988a) come to the conclusion that "a person with a dependent orientation personality is undoubtedly more susceptible various somatic diseases, and not predisposed to one specific type of symptom” (p. 132). In addition, they conclude that dependent people are more tend to look at their problems somatic, not psychological concepts, more often seek help from specialists to solve their problems, start seeking help earlier and more conscientious attitude to treatment than independent people. nine0003
similar way Vaillant (Vaillant, 1978) and Hinkle (Hinkle, 1961) found an association between dependent personality traits and general predisposition to illness. In a recent review of empirical Literature Greenberg and Bornstein (Greenberg & Bornstein, 1988a) come to the conclusion that "a person with a dependent orientation personality is undoubtedly more susceptible various somatic diseases, and not predisposed to one specific type of symptom” (p. 132). In addition, they conclude that dependent people are more tend to look at their problems somatic, not psychological concepts, more often seek help from specialists to solve their problems, start seeking help earlier and more conscientious attitude to treatment than independent people. nine0003
Alcoholism and other forms of abuse psychoactive substances are also common problems in addicted people, since these substances are often considered as an easy, passive way to solve problems, or at least escape from them. In their review of the empirical literature (containing primarily estimates of oral signs of addiction obtained with using projective tests), Greenberg and Bornstein (Greenberg & Bornstein, 1988b) come to the conclusion that a person with an addiction personality orientation is predisposed to various psychopathological conditions, including depression, alcoholism, overeating and addiction tobacco.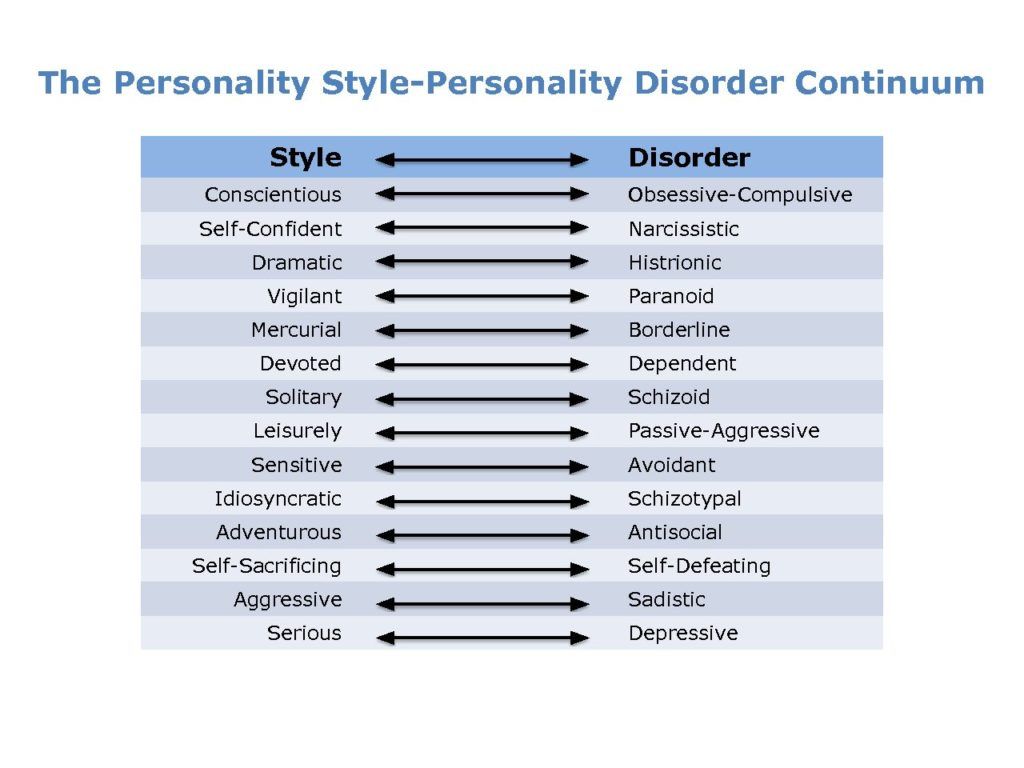 nine0132 Diagnostics.
nine0132 Diagnostics.
When a person comes to treatment with low self-confidence and obviously high the need for support, be considered a diagnosis of ADHD. For example, Karen, a 45 year old married woman, was referred for treatment by her physician due to with panic attacks. During the evaluation, she seemed preoccupied, sensitive and naive. She was easily overwhelmed by emotions. and she cried from time to time along the way sessions. During the evaluation, for any opportunities for self-criticism. For example, when asked how she gets along with other people, she reported: "Others think I'm dumb and inadequate" although she did not mention any facts that might make her think so. She said she didn't love go to school because "I was dumb" I also always felt that I was not good enough. She really needed in support of a psychotherapist, even, for example, when performing a task, take away 7 out of 100, which was used during diagnostics. In addition to attacks panic and avoidance she reported severe depression, which happened several times she has for the last 5 years, and about having severe premenstrual syndrome. Finally, she spoke about drinks one to three daily small portions of liquor, but does not count it's a problem. nine0003
Finally, she spoke about drinks one to three daily small portions of liquor, but does not count it's a problem. nine0003
However when diagnosing SPD, it is important to go beyond scope of initial complaints and carefully evaluate the patient's relationship history, especially noting how he reacts to ending relationships and how others feedback about the patient. Might be helpful inquire in detail about how solutions, and pay attention to how everyday and important life solutions. must also be collected information about how the patient behaves feels if it stays for a long time loneliness. It is also useful to ask patient, how he behaves if with someone does not agree or if required do something nasty or humiliating. About the patient's IPD can speak and own reaction psychotherapist. If the therapist finds himself starting to feel savior of the patient or inclined to do unusual exceptions for him, in which he allegedly needs, it should be assumed the patient has a PPD and start collecting information that confirms or refutes this diagnosis. nine0003
nine0003
Karen announced that her first marriage lasted 10 years though "it was hell". Her husband cheated her with many women and was inclined to verbal aggression. She many times I tried to leave him, but gave in repeated requests to return. Finally she was able to divorce him and soon met her current husband and married him. She described her husband as kind, sensitive and responsive. Karen stated that prefers someone to take important decisions for her, and agrees with people to avoid conflict. Her worried about loneliness when there is no one take care of her, and she reported feelings of helplessness in the absence support from outside. She also reported that is easily injured, so she tries not to do anything that might provoke criticism. nine0003
Addiction may be part of various disorders, therefore care must be taken and differentiate ZRL from others disorders that some similar characteristics. For example, although direct and engaging patients seem to have both histrionic and dependent personality disorder, patients with a recent diagnosis of less than bright, self-centered and superficial than patients with the first diagnosis.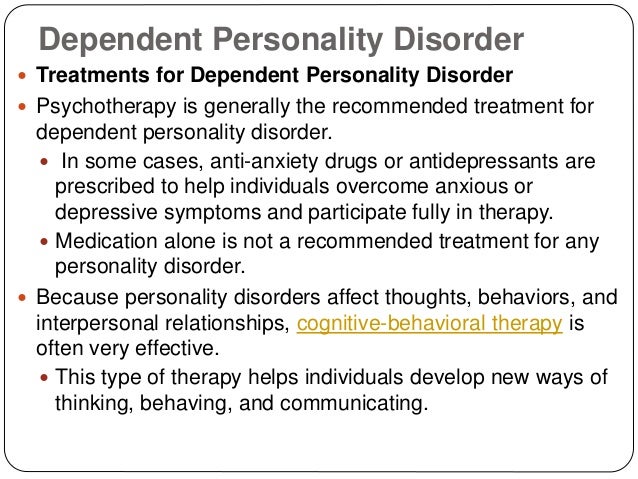 Man with ZRL is usually passive, submissive, modest and obedient; this contrasts with active manipulativeness, sociability, charm and a penchant for captivating person with histrionic disorder personality. Man with avoidant also experiencing personality disorder a strong need for love, but doubts she is afraid that such love is impossible; a person with ADHD is inclined to trust and sincerely rely on people, expecting it efforts will be rewarded with love and care. Agoraphobic patients quite dependent on other people in a specific way, they need in a reliable person to accompany them in different places so they don't afraid of panic attacks happening, when they are alone. Agoraphobic patients are generally more assertive about their addiction than people with ADHD, actively demanding to be accompanied everywhere, wherever they go. But there are cases when the patient meets the criteria and panic disorder with agoraphobia, and ZRL, and then you should put both diagnosis (according to Axes I and II).
Man with ZRL is usually passive, submissive, modest and obedient; this contrasts with active manipulativeness, sociability, charm and a penchant for captivating person with histrionic disorder personality. Man with avoidant also experiencing personality disorder a strong need for love, but doubts she is afraid that such love is impossible; a person with ADHD is inclined to trust and sincerely rely on people, expecting it efforts will be rewarded with love and care. Agoraphobic patients quite dependent on other people in a specific way, they need in a reliable person to accompany them in different places so they don't afraid of panic attacks happening, when they are alone. Agoraphobic patients are generally more assertive about their addiction than people with ADHD, actively demanding to be accompanied everywhere, wherever they go. But there are cases when the patient meets the criteria and panic disorder with agoraphobia, and ZRL, and then you should put both diagnosis (according to Axes I and II). nine0003
nine0003
Although Karen sought treatment for panic attacks and found total avoidance patterns during the last seven years old, she admitted that many of her problems existed much earlier panic attacks and agoraphobia. She doesn't liked to do things alone long before she started panic attacks, and she had such thoughts like "I'm a worthless person" at least since third grade. She clearly met the criteria for the SRL and panic disorder with agoraphobia, as well as major depression. nine0132 Theoretical comprehension.
Comprehensive SPD criteria in the behavioral literature are not yet available. Common when describing people with this disorder is that they are characterized as "extremely insecure" (Marshall & Barbaree, 1984, p. 417). But Turkat and Carlson (Turkat & Carlson, 1984) take a different approach and in case of one patient with IPD formulate the main problem as anxiety when making independent decisions, although they do not consider this is a common problem for all patients.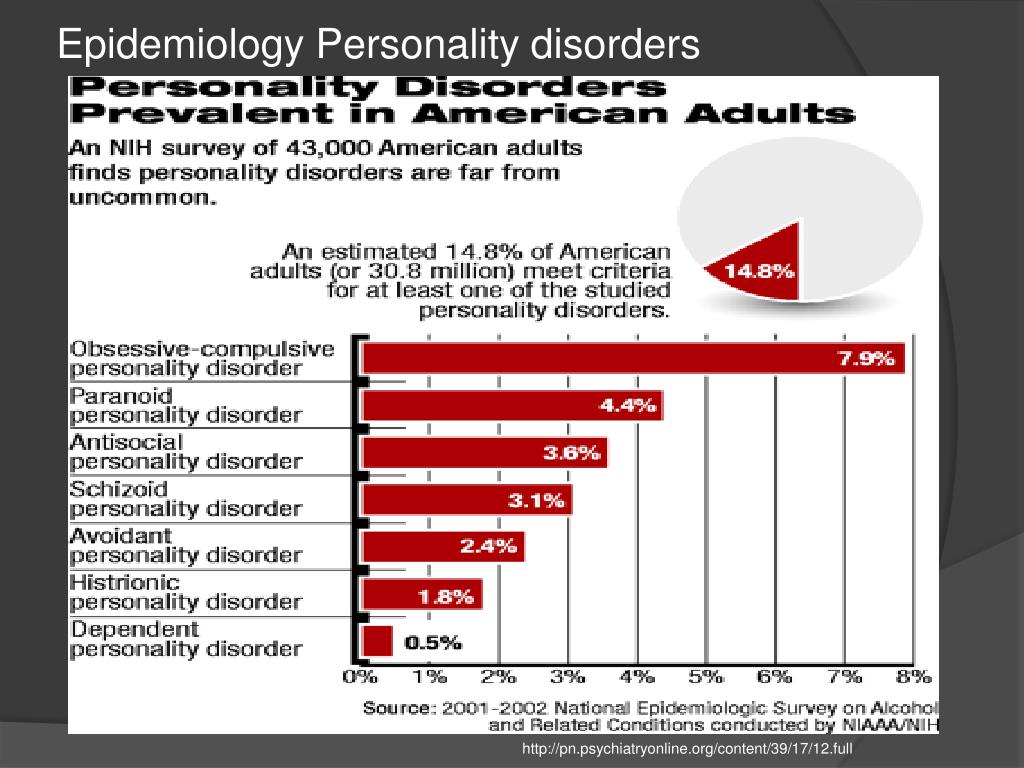 Really people with SRL often extremely shy at the same time and are very afraid to accept independent solutions, but comprehensive cognitive-behavioral reasoning must include not only two characteristics. nine0003
Really people with SRL often extremely shy at the same time and are very afraid to accept independent solutions, but comprehensive cognitive-behavioral reasoning must include not only two characteristics. nine0003
ZRL can be seen as taking place from two key assumptions. Firstly, these people consider themselves inadequate and helpless and therefore incapable live independently. They are considering world as inhospitable, lonely or even a dangerous place where they cannot survive in alone. Second, they conclude that the solution to the problem of their inadequacy in a frightening world is to try to find someone who can cope with life's difficulties protect and take care of them. Dependent people decide what to give up responsibility and submit to needs and desires of another person in exchange for care. Such an adaptation of course, it carries unfavorable effects. On the one hand, relying on others in problem solving and acceptance decisions, a person has few opportunities acquire the skills needed to independence. Some people never do not learn independent skills life (such as self-confidence, problem solving and decision making) while others are unaware of skills, which they possess and therefore do not use them, thus securing their addiction. Moreover, the idea of to become more competent frighten addicted people because they afraid that if they become less needy, they will be abandoned and they will have to live on their own, although they are completely not ready for this. nine0003
Some people never do not learn independent skills life (such as self-confidence, problem solving and decision making) while others are unaware of skills, which they possess and therefore do not use them, thus securing their addiction. Moreover, the idea of to become more competent frighten addicted people because they afraid that if they become less needy, they will be abandoned and they will have to live on their own, although they are completely not ready for this. nine0003
Such changes have several additional inconvenience for the addict. He should always be very careful to give pleasure another person and avoid conflict for fear of endangering meaningful relationship and being alone. So there can be no question of certainty in oneself and expressing one's own opinion. In addition, an addict may seem so hopeless distressed and clingy, that he it's hard to find a partner who wants or can satisfy him needs for an arbitrarily long time. If this relationship ends, man feels completely empty and sees no alternative to look for a new dependency object.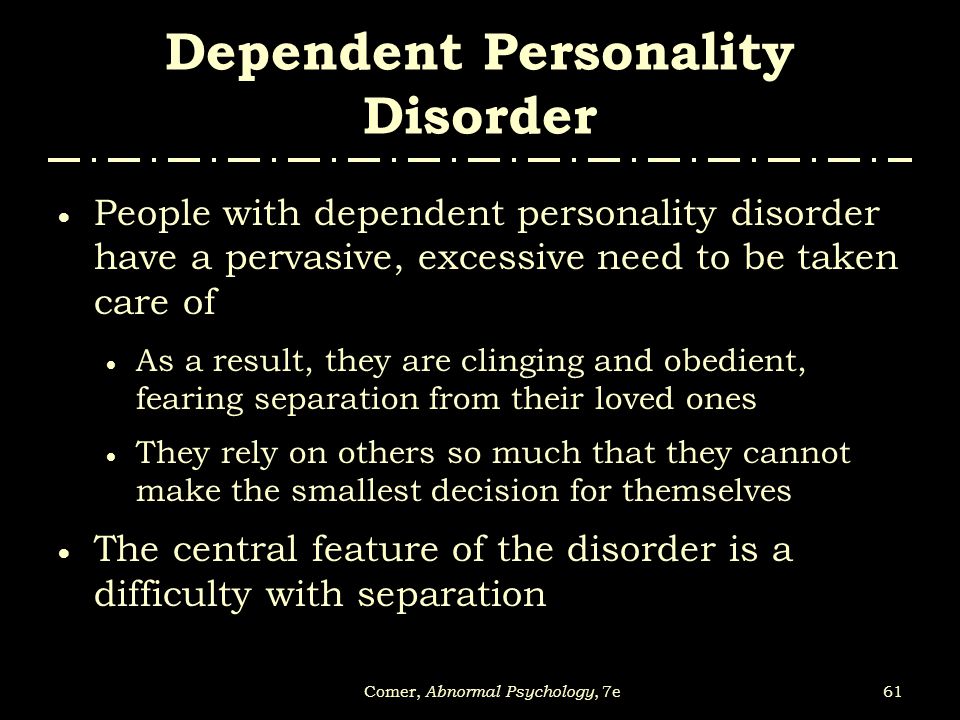 nine0003
nine0003
Main beliefs and cognitive biases SRLs lead to such automatic thoughts, like "I can't", "I'll never learn do it" and "I'm too stupid and weak." When asked to do something, they have thoughts such as "Oh my husband could do it much better" and "I'm sure they understand that I I can not". For example, when Karen was asked subtract 7 out of 100 during the initial ratings, she commented on it something like this: “Oh, I don’t understand anything about math, I'll never be able to do” and “Is it really necessary? I AM I mean, I can't do it." During the first session of psychotherapy, when psychotherapist outlined a treatment plan, she said, "Oh, I can't record thoughts" and "I'm sure others helps, but I'm too dumb to have it worked out." nine0132 Approaches to treatment.
Easy suggest that the goal of treatment for IPD is independence. Actually the worst fears of many addicts patients are that psychotherapy will lead to complete independence and isolation and they must face the challenges of life alone, without help or support surrounding. The best name for a goal psychotherapy SPD - "autonomy". Autonomy defined as the ability to act independent of others, but at the same time ability to establish close relations (Birtchnell, 1984). In order to achieve this, it is necessary to help the patient gradually learn to live more regardless of others (including psychotherapist) and develop confidence and a sense of self-efficacy. But given the common fear that competence will lead to give up, it must be done gradually and with a certain delicacy.
The best name for a goal psychotherapy SPD - "autonomy". Autonomy defined as the ability to act independent of others, but at the same time ability to establish close relations (Birtchnell, 1984). In order to achieve this, it is necessary to help the patient gradually learn to live more regardless of others (including psychotherapist) and develop confidence and a sense of self-efficacy. But given the common fear that competence will lead to give up, it must be done gradually and with a certain delicacy.
As when dealing with any of the disorders personality, early stages of treatment include achievement of the goals set by the patient goals, as well as the definition and revision dysfunctional automatic thoughts. Although for a psychotherapist from the very at the beginning, it may be obvious that the dependence - the main problem of the patient, the patient rarely acknowledges it as part of his problems. In fact, even the use of words "dependency", "independence" or "autonomy" can frighten the patient in the early stages of treatment, if not willing to deal with these issues.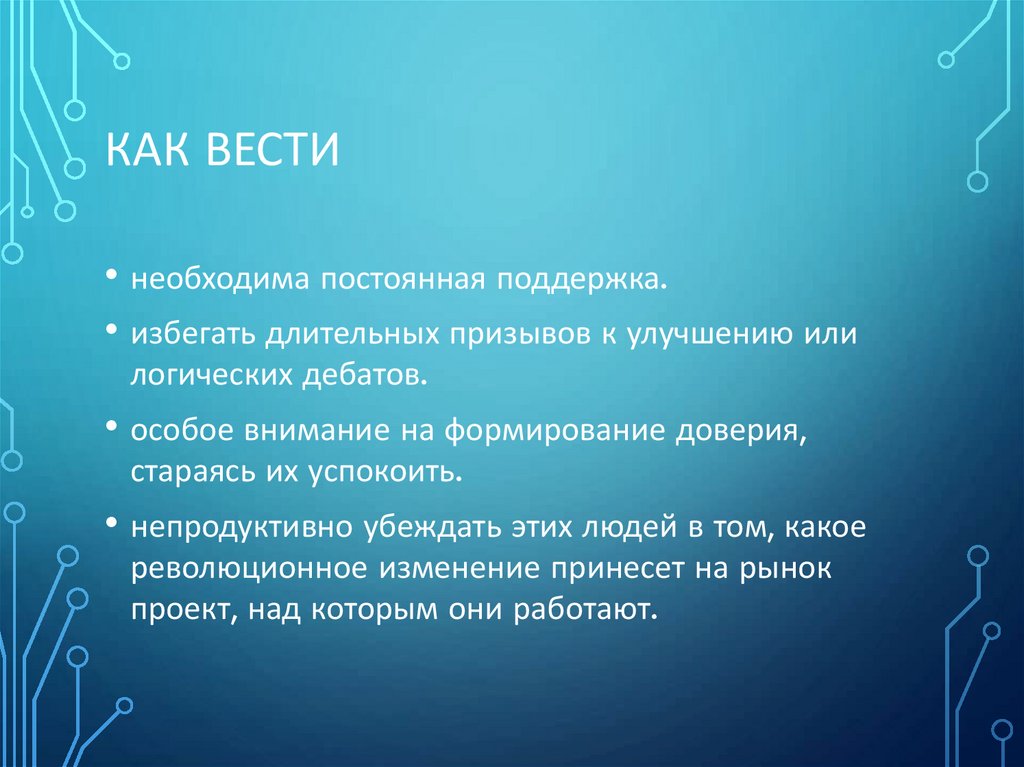 Regardless of specific goals psychotherapy, addiction problem become apparent as the treatment progresses and for psychotherapist and for the patient. However less if the patient first uses this concept, he is better aware of his problem and be less scared. nine0003
Regardless of specific goals psychotherapy, addiction problem become apparent as the treatment progresses and for psychotherapist and for the patient. However less if the patient first uses this concept, he is better aware of his problem and be less scared. nine0003
Although words like addiction used in the first sessions, Karen could articulate goals clearly psychotherapy, for example: “Increase self-confidence so that I can: a) be more sociable and be the first to contact to people; b) propose projects; c) take for completing tasks at work; d) more feel comfortable with people; e) reduce the fear of failure and more praise myself for what I do."
At working with patients suffering from dependent personality disorder, it is especially important to use guided discovery and questions revealing internal contradictions. These patients are likely will consider the psychotherapist an "expert" and catch his every word, and may be tempted to just report it patients, what exactly is problem and what they should do, so assuming an authoritarian role.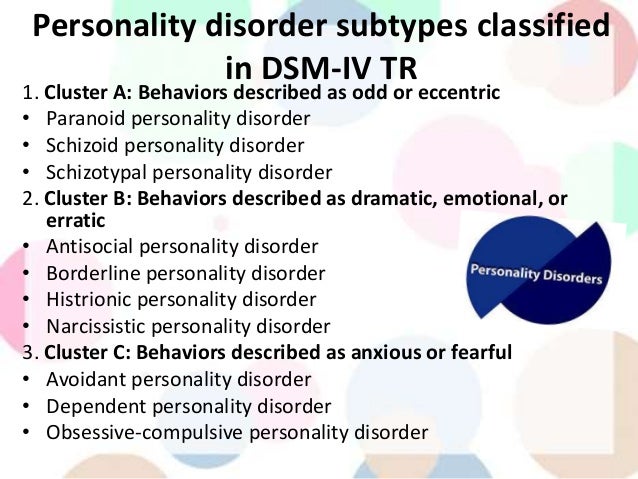 Unfortunately it encourages patient to being addicted from a psychotherapist, not to develop autonomy. These patients are at least initially, really need in some active leadership and practical suggestions from psychotherapist to get involved in treatment. Completely non-directive approach may cause them anxiety. However when the patient asks the therapist told him what to do, psychotherapist should be careful when using questions, revealing internal contradictions and guided opening, help the patient make a decision yourself. nine0003
Unfortunately it encourages patient to being addicted from a psychotherapist, not to develop autonomy. These patients are at least initially, really need in some active leadership and practical suggestions from psychotherapist to get involved in treatment. Completely non-directive approach may cause them anxiety. However when the patient asks the therapist told him what to do, psychotherapist should be careful when using questions, revealing internal contradictions and guided opening, help the patient make a decision yourself. nine0003
Relationships between therapist and patient.
Especially it is important to pay attention to one factor, which is often ignored in works of cognitive-behavioral psychotherapists: the relationship between psychotherapist and patient. dependent the behavior of a patient with IPD has enough total character and intense manifested in psychotherapeutic relationships. This led to the assumption that humanistic or non-directive approaches are preferred over directive cognitive-behavioral, encouraging the patient to he submitted to a dominant psychotherapist (for example: Millon, 1981).
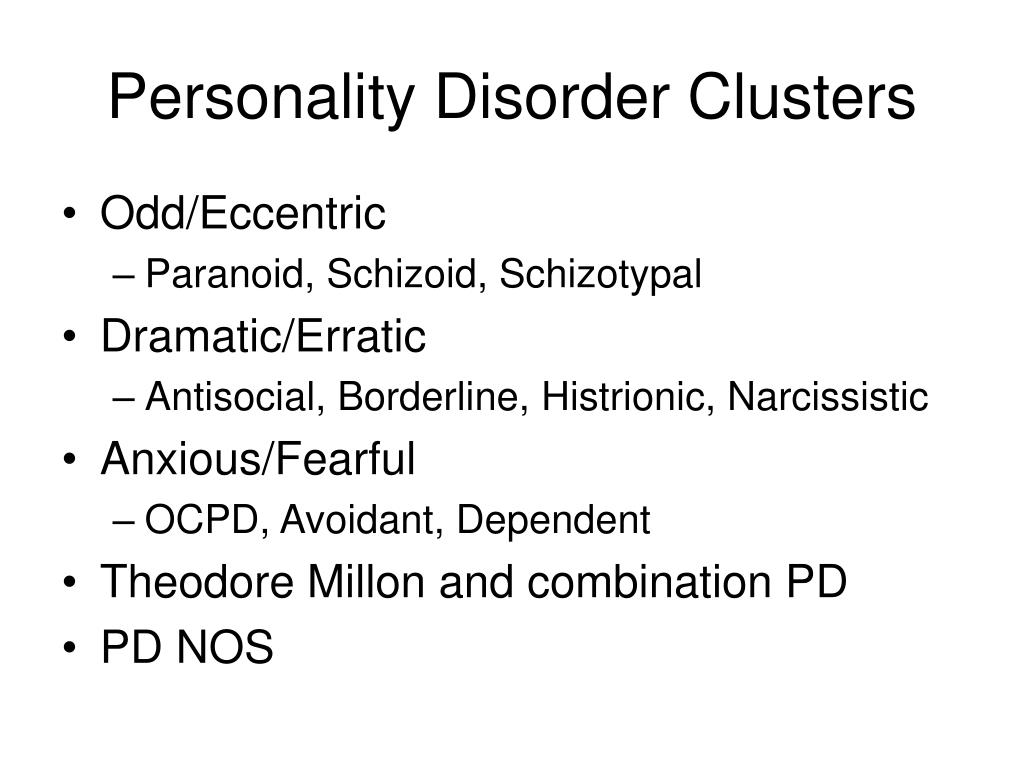
 Cluster C includes Avoidant (socially inhibited and oversensitive to negative evaluation; avoids occupations that involve interpersonal contact because of fears of criticism or rejection; avoids relationships with others unless guaranteed to be accepted unconditionally; feels inadequate and views self as socially inept and unappealing; unwilling to take risks or engage in new activities if they may prove embarrassing), Dependent (allows others to take over and run her life; is submissive, clingy, and fears separation; cannot make decisions without advice and reassurance from others; lacks self-confidence; cannot do things on her own; feels uncomfortable or helpless when alone), and Obsessive-Compulsive (pervasive need for perfectionism that interferes with the ability to complete tasks; preoccupied with details, rules, order, and schedules; excessively devoted to work at the expense of leisure and friendships; rigid, inflexible, and stubborn; insists things be done his way; miserly with money).
Cluster C includes Avoidant (socially inhibited and oversensitive to negative evaluation; avoids occupations that involve interpersonal contact because of fears of criticism or rejection; avoids relationships with others unless guaranteed to be accepted unconditionally; feels inadequate and views self as socially inept and unappealing; unwilling to take risks or engage in new activities if they may prove embarrassing), Dependent (allows others to take over and run her life; is submissive, clingy, and fears separation; cannot make decisions without advice and reassurance from others; lacks self-confidence; cannot do things on her own; feels uncomfortable or helpless when alone), and Obsessive-Compulsive (pervasive need for perfectionism that interferes with the ability to complete tasks; preoccupied with details, rules, order, and schedules; excessively devoted to work at the expense of leisure and friendships; rigid, inflexible, and stubborn; insists things be done his way; miserly with money). ">
">