Can high blood sugar cause panic attacks
5 Common Foods That Can Trigger Anxiety Symptoms : Intrepid Mental Wellness, PLLC: Psychiatric Nurse Practitioners
5 Common Foods That Can Trigger Anxiety Symptoms : Intrepid Mental Wellness, PLLC: Psychiatric Nurse Practitioners 5 Common Foods that Can Trigger Anxiety SymptomsFood can have a powerful impact on mood, stress levels, and mental health. Some foods have been shown to cause or worsen the symptoms of anxiety, depression, and other chronic mental-health conditions. While symptoms and triggers are unique to every individual, research studies have found several common foods that can induce anxiety.
Sugar
High sugar intake has been linked to many different health conditions, including obesity, high blood pressure, and tooth decay. Sugar has also been linked to depression, mood swings, and symptoms of anxiety. The initial energy boost gained from eating sugar keeps many people craving sugary foods and drinks.
However, once the energy boost has peaked, blood sugar levels drop quickly; this leads to lethargy, low mood, and further cravings. The continual boosts and drops in blood sugar levels can trigger the release of adrenalin and cortisol into the bloodstream, causing anxiety and sometimes even panic attacks.
Fried Foods
Junk food and fried foods, such as pizza, fried chicken, hamburgers, and fries, have little nutritional value and are extremely difficult for the body to digest. When the body is unable to digest and process food, excess gas, acid reflux, and other gastrointestinal complaints can produce symptoms that trigger anxiety. Long-term digestive health complaints, such as gastroesophageal reflux disease (GERD), sometimes cause sufferers to wake in the night gasping for breath, as acid reflux can bring about light vomiting that results in choking sensations.
Processed Foods
Processed foods, such as canned soups, cured meats, and processed cheeses, contain high amounts of salt.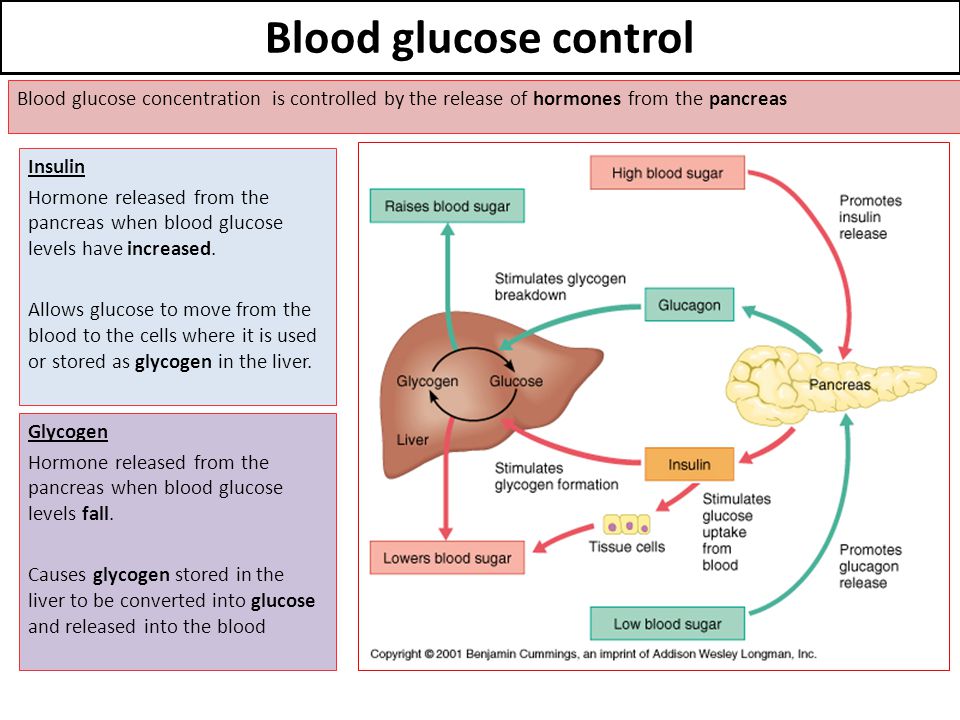 Excessive salt intake raises blood pressure and increases the workload of the heart, causing the body to release adrenalin into the bloodstream and leading to anxiety. In addition, many cans and plastic containers are lined with bisphenol A (BPA), a chemical that has been linked to changes in mood and blood pressure. While research is still being conducted into the possible dangers of BPA, many experts believe the chemical can seep into food or drink and produce harmful effects.
Excessive salt intake raises blood pressure and increases the workload of the heart, causing the body to release adrenalin into the bloodstream and leading to anxiety. In addition, many cans and plastic containers are lined with bisphenol A (BPA), a chemical that has been linked to changes in mood and blood pressure. While research is still being conducted into the possible dangers of BPA, many experts believe the chemical can seep into food or drink and produce harmful effects.
Food Additives
Food additives, including aspartame, monosodium glutamate (MSG), and some food dyes, have also been linked to anxiety, depression, and mood changes. Aspartame is an artificial sweetener used in many different foods, including sugar-free candies, chewing gum, and soft drinks, and studies have linked it to several health conditions, including anxiety and depression. Regular consumption of MSG, which is used to enhance the taste of many snacks, processed foods, and pre-cooked ready meals, has been linked to fatigue, headaches, depression, and anxiety.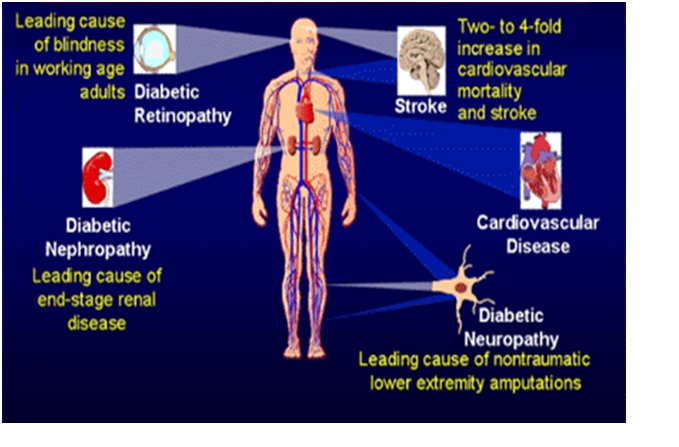 Some food dyes used in drinks, candies, cheese, and other processed foods have also been associated with anxiety symptoms.
Some food dyes used in drinks, candies, cheese, and other processed foods have also been associated with anxiety symptoms.
Caffeine
Caffeine can be found in a range of products, including coffee, tea, energy drinks, chocolate, and some painkillers. Many people can tolerate small amounts of caffeine, but because caffeine stimulates the central nervous system, excessive intake can lead to heart palpitations, shaking, irritability, and insomnia. Caffeine can also inhibit the absorption of some vitamins, including B vitamins, which are needed to aid relaxation and control mood. In addition, some people are more sensitive than others to the effects of caffeine, so even small amounts can cause headaches, shaking, and anxiety.
A balanced diet is essential for controlling anxiety, depression, and long-term mental health conditions. Eliminating or cutting down on foods known to trigger anxiety symptoms is an important step in managing chronic anxiety disorders.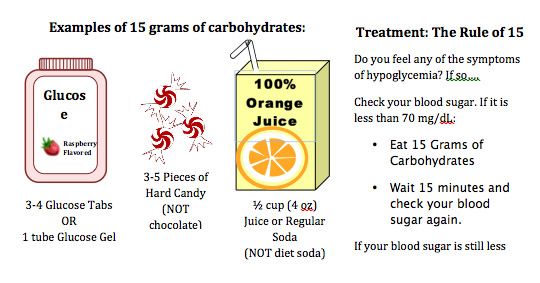 In addition, food sensitivities can precipitate a range of unpleasant symptoms that can mimic anxiety, so it's important to talk to your doctor if you suspect specific foods may be causing you distress.
In addition, food sensitivities can precipitate a range of unpleasant symptoms that can mimic anxiety, so it's important to talk to your doctor if you suspect specific foods may be causing you distress.
9 Tips for Managing Your Anxiety Right Now
Are you feeling overwhelmed with anxiety? Whether recent life changes have caused it or it's something you've been struggling with for a while, it can be challenging to know how to manage your anxiety. These nine tips can help you get started.
7 Foods You Should Avoid If You Have Depression
You probably already know that diet has a huge impact on your psychological and mental state. Excluding harmful foods from your diet is the first step towards a healthier brain and mind.
How to Use Food to Manage Your Mental Health
Moods are not created in the mind alone, but in partnership with the body.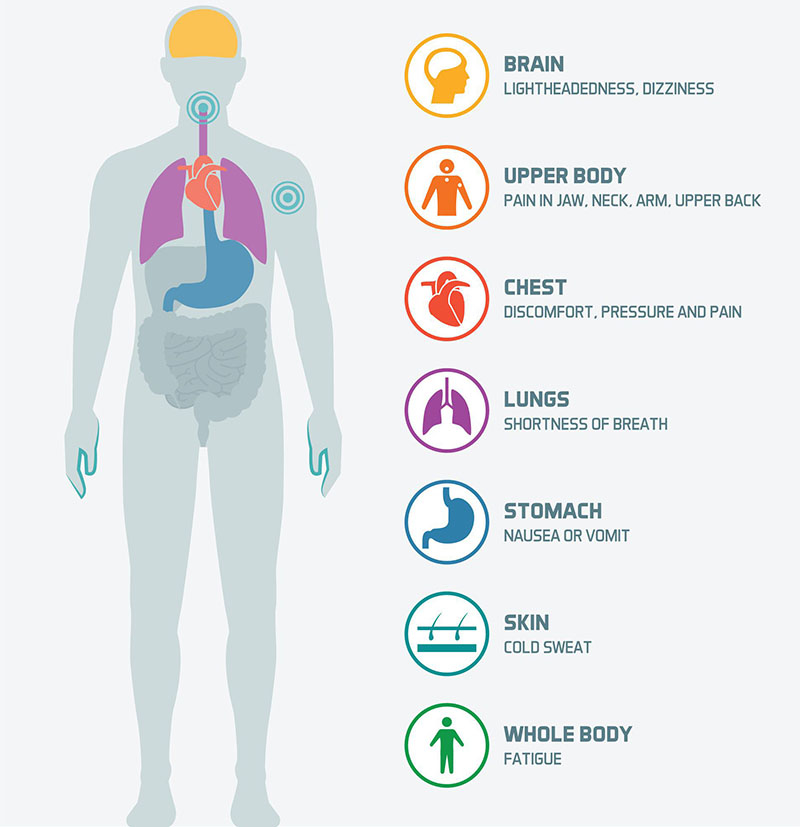 Ask anyone who has eaten ice cream to cheer themselves up, and they'll tell you that's true. What we feed the body can have an enormous impact on how we feel.
Ask anyone who has eaten ice cream to cheer themselves up, and they'll tell you that's true. What we feed the body can have an enormous impact on how we feel.
Beyond Depression: Recognizing the Signs and Symptoms of Bipolar Disorder
Depression is a complex disorder, a condition triggered by biochemical, environmental, and psychological influences. Although patients diagnosed with bipolar disorder often experience bouts of depression, their condition is far more complex.
Dietary Changes That Can Have Positive Effects on ADHD Symptoms
When parents suspect their child has attention deficit hyperactivity disorder (ADHD) or a diagnosis has already been made, making changes to the child's diet, for example, could have significant positive effects.
Gaslighting: Is Someone Meddling with Your Perception?
Does the way someone communicates with you make you question your reality? Then, perhaps they are gaslighting you.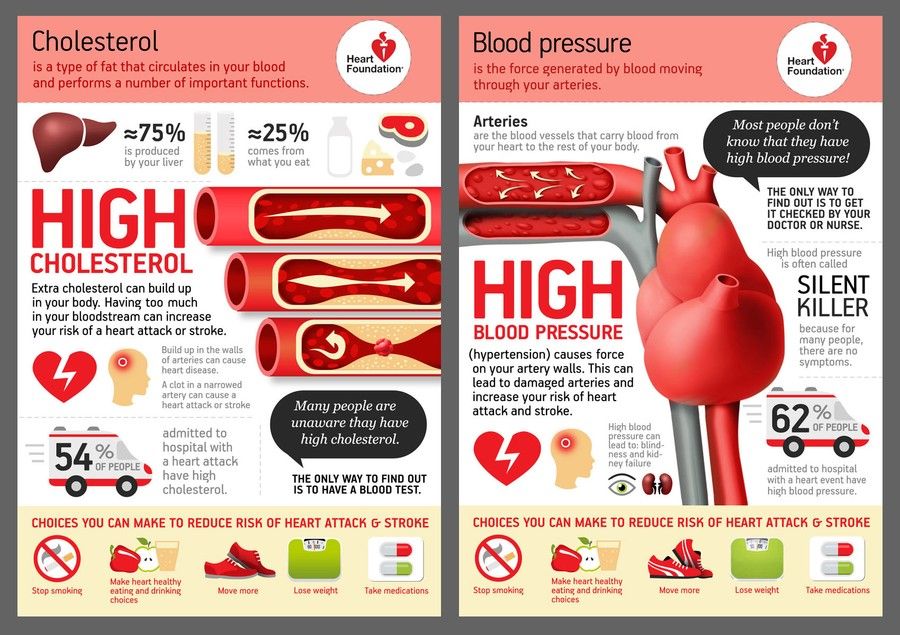 When you understand what gaslighting is, you can identify whether you are its victim and improve your life.
When you understand what gaslighting is, you can identify whether you are its victim and improve your life.
Diabetes and Anxiety: What’s the Connection?
Overview
While diabetes is typically a manageable disease, it can create added stress. People with diabetes may have concerns related to regularly counting carbohydrates, measuring insulin levels, and thinking about long-term health. However, for some people with diabetes, those concerns become more intense and result in anxiety.
Read on to find out more about the connection between diabetes and anxiety and what you can do to prevent and treat your symptoms.
Research has consistently uncovered a strong connection between diabetes and anxiety. One study found that Americans with diabetes are 20 percent more likely to be diagnosed with anxiety than those without diabetes. This was found to be particularly true in young adults and Hispanic Americans.
The link between anxiety and glucose levels
Stress can affect your blood sugars, though research tends to be mixed as to how.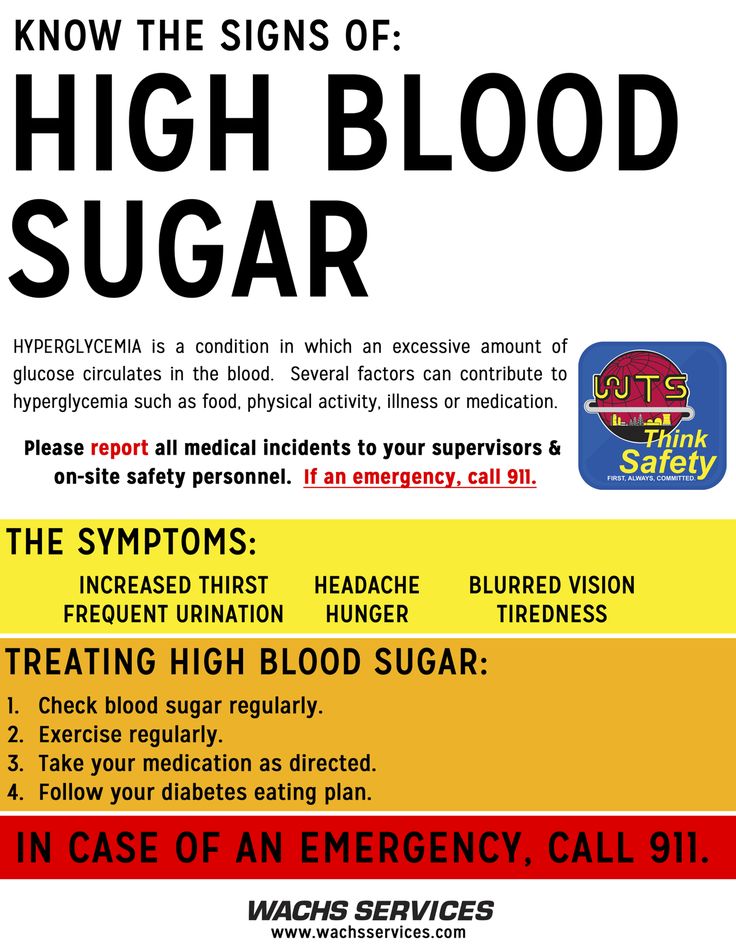 In some people, it appears to raise blood glucose levels, while in others it appears to lower them.
In some people, it appears to raise blood glucose levels, while in others it appears to lower them.
At least one study has shown there may also be an association between glycemic control and mental health conditions such as anxiety and depression, particularly for men.
However, another study found that general anxiety didn’t affect glycemic control, but diabetes-specific emotional stress did.
Other research has found that people with type 1 diabetes seem to be “more susceptible to physical harm from stress” while those with type 2 diabetes weren’t. One’s personality also seems to determine the effect to some extent as well.
People with diabetes may become anxious over a variety of things. These can include monitoring their glucose levels, weight, and diet.
They may also worry about short-term health complications, such as hypoglycemia, as well as long-term effects. People with diabetes are at higher risk for certain health complications, such as heart disease, kidney disease, and stroke.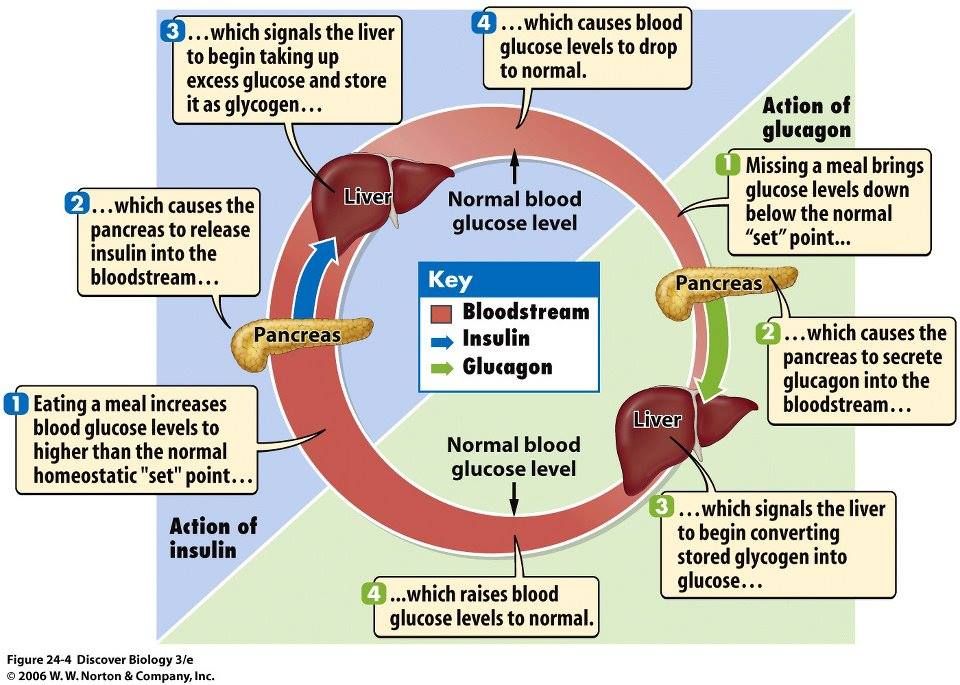 Knowing this can lead to further anxiety.
Knowing this can lead to further anxiety.
But keep in mind that the information can also be empowering if it leads to preventative measures and treatments. Learn about other ways one woman with anxiety feels empowered.
There is also some evidence that anxiety may play a role in causing diabetes. One study found that symptoms of anxiety and depression are significant risk factors for developing type 2 diabetes.
While it might initially stem from stress or a stressful situation, anxiety is more than just feeling stressed. It’s excessive, unrealistic worry that can interfere with relationships and daily life. Anxiety symptoms vary from person to person. There are several types of anxiety disorders, which include:
- agoraphobia (a fear of certain places or situations)
- generalized anxiety disorder
- obsessive-compulsive disorder (OCD)
- panic disorder
- post-traumatic stress disorder (PTSD)
- selective mutism
- separation anxiety disorder
- specific phobias
While each disorder has distinct symptoms, common symptoms of anxiety include:
- nervousness, restlessness, or being tense
- feelings of danger, panic, or dread
- rapid heart rate
- rapid breathing, or hyperventilation
- increased or heavy sweating
- trembling or muscle twitching
- weakness and lethargy
- difficulty focusing or thinking clearly about anything other than the thing you’re worried about
- insomnia
- digestive or gastrointestinal problems, such as gas, constipation, or diarrhea
- a strong desire to avoid the things that trigger your anxiety
- obsessions about certain ideas, a sign of OCD
- performing certain behaviors over and over again
- anxiety surrounding a particular life event or experience that has occurred in the past (especially indicative of PTSD)
In some cases, anxiety can cause panic attacks, which are sudden, intense episodes of fear that aren’t related to any apparent threat or danger. Symptoms of panic attacks are very similar to those of hypoglycemia. Hypoglycemia is a dangerous condition in which a person’s blood sugar can become too low.
Symptoms of panic attacks are very similar to those of hypoglycemia. Hypoglycemia is a dangerous condition in which a person’s blood sugar can become too low.
Symptoms of hypoglycemia
- rapid heartbeat
- blurry vision
- sudden mood changes
- sudden nervousness
- unexplained fatigue
- pale skin
- headache
- hunger
- shaking
- dizziness
- sweating
- difficulty sleeping
- skin tingling
- trouble thinking clearly or concentrating
- loss of consciousness, seizure, coma
Symptoms of a panic attack
- chest pain
- difficulty swallowing
- difficulty breathing
- shortness of breath
- hyperventilating
- rapid heartbeat
- feeling faint
- hot flashes
- chills
- shaking
- sweating
- nausea
- stomach pain
- tingling or numbness
- feeling that death is imminent
Both conditions require treatment by a medical professional.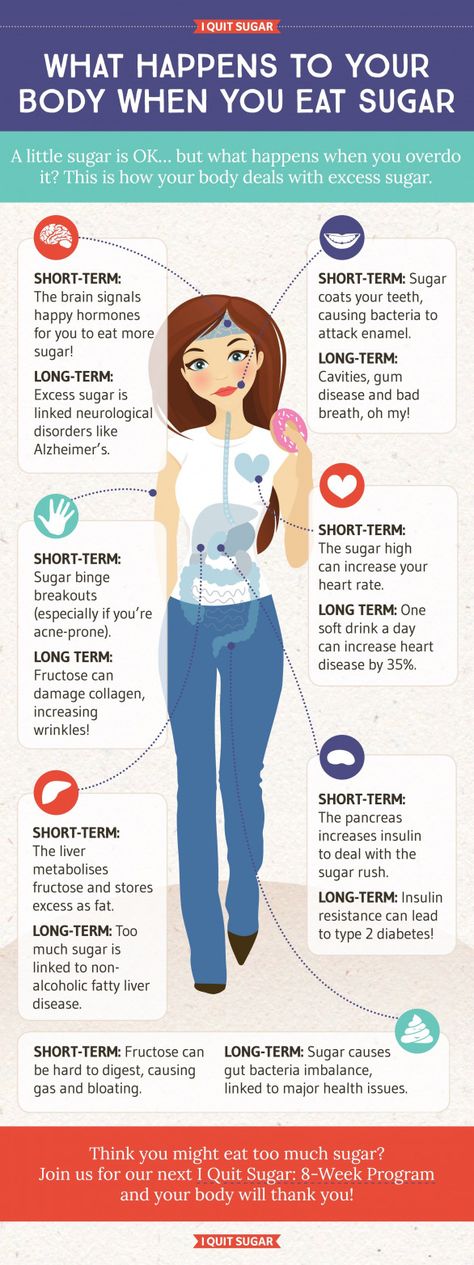 Hypoglycemia is a medical emergency that may require immediate treatment, depending on the person. If you experience any of the symptoms of hypoglycemia, even if you suspect anxiety, you should check your blood sugar and try to eat 15 grams of carbohydrates right away (about the amount in a slice of bread or small piece of fruit). Review the symptoms with your doctor as soon as possible.
Hypoglycemia is a medical emergency that may require immediate treatment, depending on the person. If you experience any of the symptoms of hypoglycemia, even if you suspect anxiety, you should check your blood sugar and try to eat 15 grams of carbohydrates right away (about the amount in a slice of bread or small piece of fruit). Review the symptoms with your doctor as soon as possible.
There are a variety of anxiety orders, and the treatment for each varies. However, in general, the most common treatments for anxiety include:
Lifestyle changes
Things such as getting exercise, avoiding alcohol and other recreational drugs, limiting caffeine, maintaining a healthy diet, and getting enough sleep can often help to calm anxiety.
Therapy
If lifestyle changes aren’t enough to manage anxiety, your doctor may suggest you see a mental health provider. Therapy techniques used to treat anxiety include:
- cognitive behavioral therapy (CBT), which teaches you to recognize anxious thoughts and behaviors and change them
- exposure therapy, in which you’re exposed gradually to things that make you anxious to help manage your feelings
Medications
In some cases, medication may be prescribed to treat anxiety.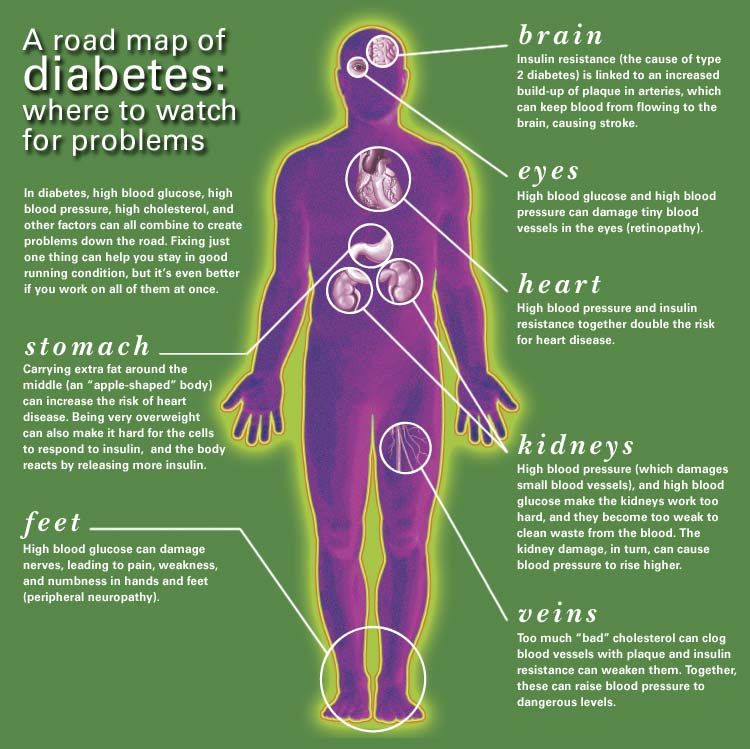 Some of the most common include:
Some of the most common include:
- antidepressants
- anti-anxiety medications such as buspirone
- a benzodiazepine for relief of panic attacks
There’s a strong connection between diabetes and anxiety. People with diabetes may want to manage stress through healthy lifestyle choices such as diet, exercise, and other stress-relieving activities.
If you begin seeing symptoms that aren’t manageable with such changes, consult with your doctor. They can help you determine the best strategies for managing your anxiety.
Anxiety disorders in patients with diabetes mellitus uMEDp
Anxiety disorders are common in patients with diabetes mellitus (DM), especially in patients with type 2 diabetes. Anxiety disorders significantly worsen the compensation of the disease. Consequently, the risk of developing diabetic complications increases, and the quality of life of patients decreases. In this regard, timely detection of anxiety disorders in this group of patients is necessary.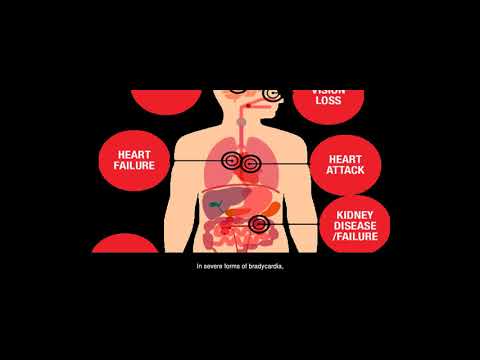
The treatment of anxiety disorders in patients with DM is a difficult task due to numerous comorbid somatic diseases. Tofisopam (Grandaxin®) is an effective and safe treatment for anxiety disorders in these patients.
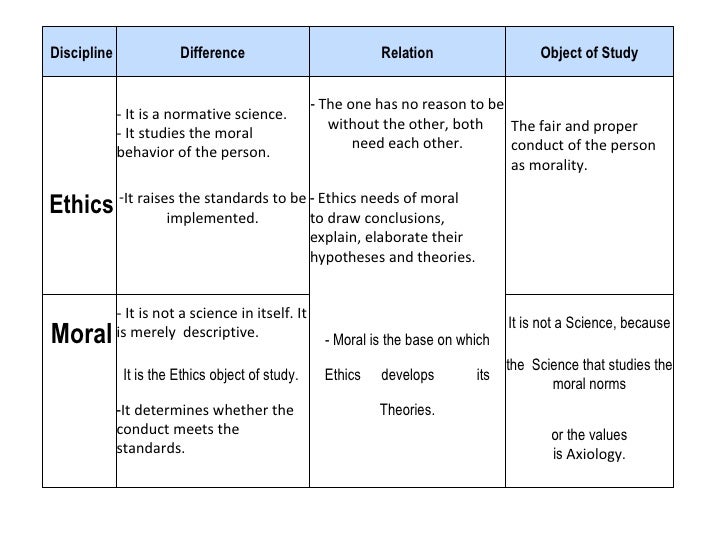
Table. Efficacy of Grandaxin and Atarax in the treatment of TR in patients with DM, M ± m
Diabetes mellitus (DM) is a chronic disease characterized by metabolic disorders and persistent pathological hyperglycemia. It ranks fifth among diseases in terms of prevalence and sixth among the causes of death in the elderly.
The chronic course of DM, the nature of complications, the need for frequent self-monitoring of glycemia using an invasive method cause an increased risk of developing mental disorders, especially anxiety and depressive states. It should be noted that in patients with DM, anxiety disorders (AD) are often combined with depression. And if much attention is currently paid to the study of the development of depression in this group of patients, the relationship between TR and DM remains poorly understood. However, TR in patients with DM occurs no less frequently than depression. Thus, the results of a study conducted by E.G. Starostina et al. showed that in patients with DM the frequency of TR is comparable to the frequency of depression - 39.5 vs. 40.0% [1].
However, TR in patients with DM occurs no less frequently than depression. Thus, the results of a study conducted by E.G. Starostina et al. showed that in patients with DM the frequency of TR is comparable to the frequency of depression - 39.5 vs. 40.0% [1].
The incidence of TR in patients with DM is higher than that in patients with other chronic somatic diseases. Particularly significant are such types of AD as phobias, panic disorder, generalized anxiety disorder (GAD), organic anxiety disorder (GAD).
Traditionally, pathological anxiety is considered as a patient's reaction to the presence of DM. The role of TR in the development of DM has not yet been studied.
According to the existing theory, the biochemical and pathogenetic relationship between TR and DM is explained by dysfunction of the hypothalamic-pituitary-adrenal axis in response to chronic stress. One of the neuroendocrine manifestations of psycho-emotional stress is the secretion of corticoliberin by the hypothalamus, followed by activation of the adrenal glands and an increase in their production of glucocorticosteroids.
Chronic stress can lead not only to adrenal exhaustion, but also to disruption of the negative feedback mechanisms of cortisol secretion. The latter is often observed in endocrine pathologies: obesity, impaired glucose tolerance, as well as in some mental disorders - depression, TR. Chronic hypercortisolism contributes to an increase in visceral fat, a violation of carbohydrate and lipid metabolism. The relationship between chronic anxiety and cortisol hypersecretion was revealed using the dexamethasone test [2].
The association of TR with DM and obesity has been demonstrated in a number of studies. So, in the screening study of A.N. Niles et al. when examining 42,249 patients, it was found that TRs significantly increase the risk of developing diabetes (relative risk (RR) 1.3) and obesity (RR 1.2) [3]. In a large population study, I.C. Chien et al. the frequency of DM in patients with TR was significantly higher than in the general population - 11.89 vs. 5.92%, respectively.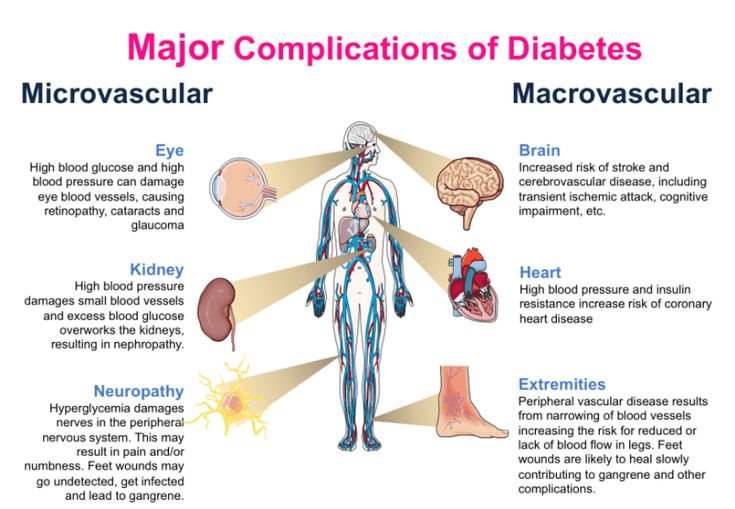 The prevalence of DM in the group of patients with TR was also higher than in the group of patients without TR - 2.25 vs. 1.11%, respectively [4].
The prevalence of DM in the group of patients with TR was also higher than in the group of patients without TR - 2.25 vs. 1.11%, respectively [4].
Epidemiology of anxiety disorders
Symptoms of pathological anxiety in patients with DM, according to the literature, are observed in 40.0% of cases. At the same time, GAD - in 14.0% of cases, subsyndromal anxiety - in 27.0%, which is six to seven times more than in the population.
For patients with type 2 diabetes, permanent forms of anxiety are more typical - GAD, OTR and subsyndromal, for patients with type 1 diabetes - paroxysmal anxiety in the form of a phobia of hypoglycemia and injections [5].
GAD is associated with increased nonspecific inflammatory response, obesity, and arterial hypertension, factors that make a significant contribution to the development of DM. In addition, GAD can cause an unhealthy lifestyle - insufficient physical activity, overeating, smoking, which also contributes to the development of type 2 diabetes.
Research by S.S. Deschenes et al. demonstrated that GAD occurs in 60% of patients with type 1 diabetes. Diabetes increases the risk of developing GAD or exacerbates the symptoms of an anxiety disorder. When GAD is combined with depression, the risk of developing type 2 diabetes is doubled (RR 1.99 at 95% confidence interval (CI) (1.22–3.25), p = 0.006). The relationship between isolated GAD and DM has not been identified. These results were obtained by statistical analysis, taking into account socio-demographic factors, as well as factors related to the state of health (smoking, alcohol consumption, body mass index (BMI)) [6].
E.G. Starostina et al. when examining 228 patients with type 1 and type 2 diabetes, TR was detected in 39.5% of cases, 15.0% of them were GAD. Anxiety disorders were more common among patients with type 2 diabetes (60.0 vs. 35.0%). Patients with type 2 diabetes were more likely than patients with type 1 diabetes to have persistent anxiety disorders: generalized (22.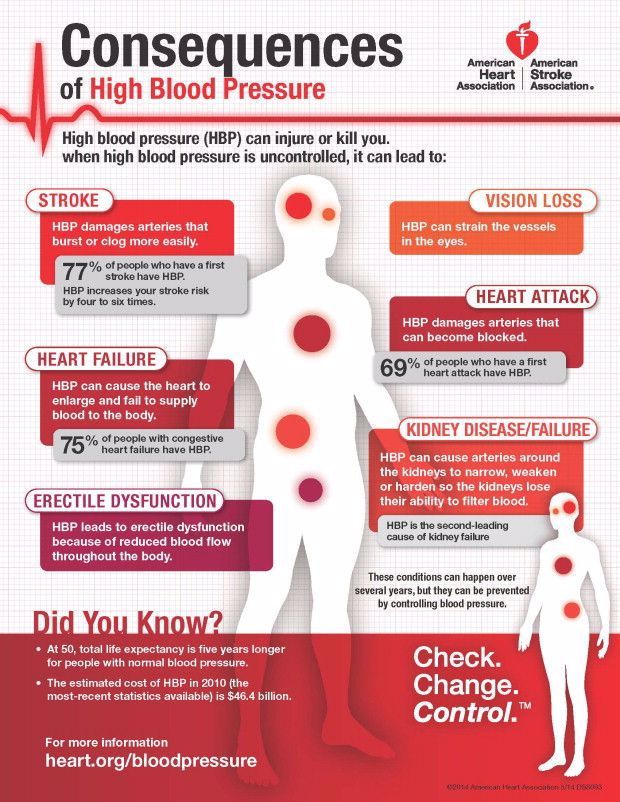 4 versus 9.3%) and organic (18.0 vs. 0%). However, pathological phobias of hypoglycemia and insulin injections were recorded eight times more often in patients with type 1 diabetes - 14.8 vs. 1.7%. It is important to note that in this study, the diagnosis of "anxiety disorder" was made based on the results of not only psychometric scales, but also consultations with a psychiatrist [2]. In another study by the same author, during which 200 people (48 men and 152 women) with DM were examined (type 1 DM - 61 patients, type 2 DM - 139patients), "pure" TRs were studied in patients with DM. The impact of TP on the course of DM was assessed by comparing data from 87 patients with DM and TP and data from 46 patients with DM but without TP. Anxiety disorders were identified in 44% of participants. At the same time, in patients with type 1 diabetes, they were recorded less frequently than in patients with type 2 diabetes - 26.2 and 51.2% of cases, respectively [5].
4 versus 9.3%) and organic (18.0 vs. 0%). However, pathological phobias of hypoglycemia and insulin injections were recorded eight times more often in patients with type 1 diabetes - 14.8 vs. 1.7%. It is important to note that in this study, the diagnosis of "anxiety disorder" was made based on the results of not only psychometric scales, but also consultations with a psychiatrist [2]. In another study by the same author, during which 200 people (48 men and 152 women) with DM were examined (type 1 DM - 61 patients, type 2 DM - 139patients), "pure" TRs were studied in patients with DM. The impact of TP on the course of DM was assessed by comparing data from 87 patients with DM and TP and data from 46 patients with DM but without TP. Anxiety disorders were identified in 44% of participants. At the same time, in patients with type 1 diabetes, they were recorded less frequently than in patients with type 2 diabetes - 26.2 and 51.2% of cases, respectively [5].
In the screening study L.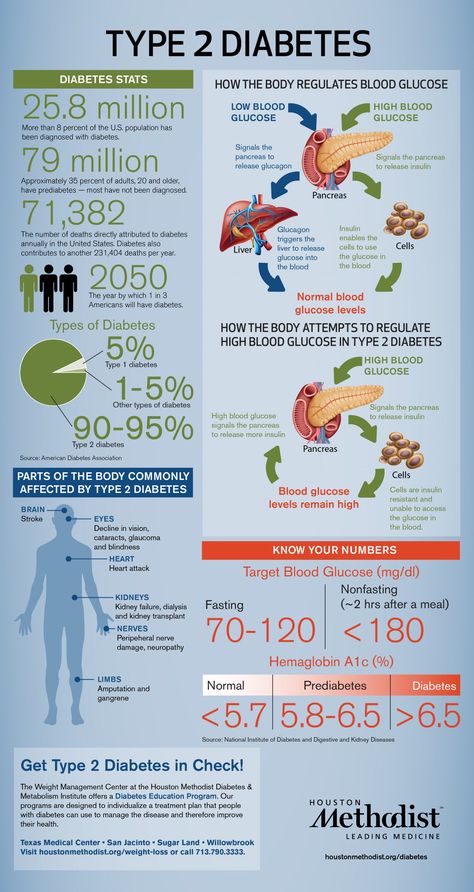 T. Wu et al. anxiety disorders were found in 14% of patients with type 2 diabetes. In persons without DM, their frequency was 7.5%. Using logistic regression analysis, it has been demonstrated that the presence of type 2 diabetes increases the likelihood of developing TR, as well as other mental disorders [7].
T. Wu et al. anxiety disorders were found in 14% of patients with type 2 diabetes. In persons without DM, their frequency was 7.5%. Using logistic regression analysis, it has been demonstrated that the presence of type 2 diabetes increases the likelihood of developing TR, as well as other mental disorders [7].
The relationship between TR and DM differs between men and women. So, R. Demmer et al. found that the cumulative incidence of DM over 17 years of follow-up was 11.0% in men and 8.0% in women (p
In another screening study, N. Sun et al. the prevalence of TR among patients with type 2 diabetes was 43.6%. At the same time, it was higher among women than among men [9].
The relationship between TR and SD was also evaluated in a longitudinal study by S. Hasan et al. The observation period is 27 years. Number of participants - 3489. The authors showed that DM increases the risk of only post-traumatic stress disorder throughout life. Women with DM had a longer duration of TR compared with women without DM [10].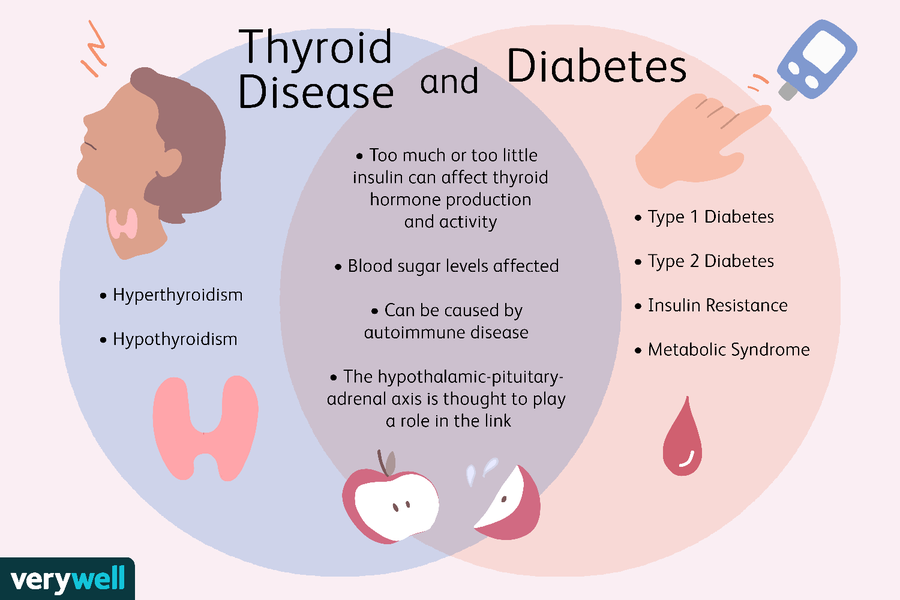
Influence of anxiety disorders on the course of diabetes mellitus and the development of complications
Anxiety disorders in patients with DM primarily lead to poor compliance with treatment and adherence to dietary recommendations. So, L. Gentil et al. found that TR in combination with depression is accompanied by a significant deterioration in compliance with oral antidiabetic drugs [11]. If a patient has an insulin phobia, he stubbornly refuses such therapy. With a phobia of hypoglycemia, the patient tries to maintain a higher level of glucose in the blood. E.G. Starostina et al. showed that in patients with a phobia of hypoglycemia, the average level of glycated hemoglobin (HbA1c) is 1.3% higher than in patients without a phobia. This difference is clinically significant in relation to the risk of developing complications of DM [2].
Anxiety disorders are associated with overeating. In patients with DM and TP, BMI values are significantly higher than in patients with DM but without TP [6, 8].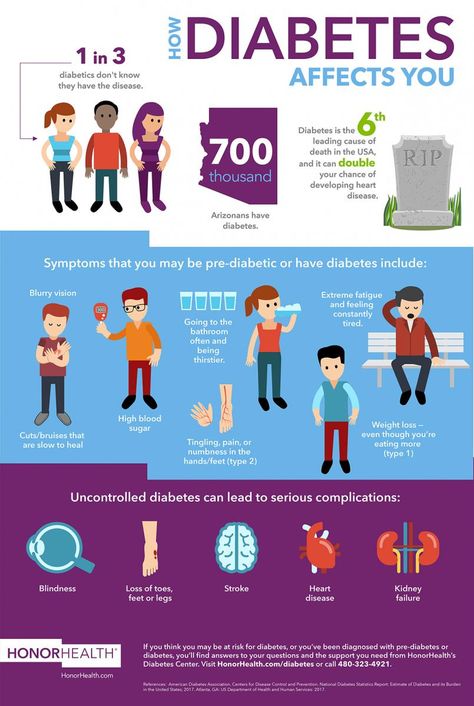
Patients with TR are also more prone to smoking and other bad habits.
In a study by N. Sun et al. it has been noted that the combination of TR with depression leads to poor glycemic control in patients with diabetes [9].
TRs are an independent risk factor for the development of cardiovascular diseases and their adverse outcomes. In particular, in the work of M. Tsai et al. with participation 40 896 patients with DM demonstrated an association of TR with an increased risk of stroke [12].
The results of the study by E.G. Starostina et al. indicate that in patients with DM and TR, the level of HbA1c is higher than in patients with DM without TR. For patients with type 1 diabetes, the difference was 0.9%, for patients with type 2 diabetes, it was 0.5% [2]. In the presence of DM and TP, higher values of both systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded, the incidence of arterial hypertension was 85.0 vs. 46.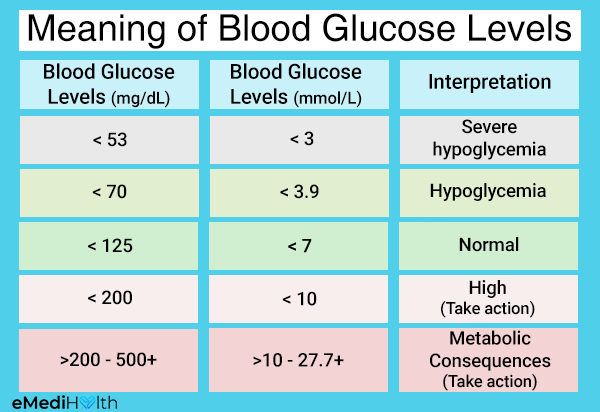 0% of cases, respectively (p
0% of cases, respectively (p
In addition to the negative impact on the course of diabetes, TRs significantly worsen the quality of life of patients.
Diagnostics
Timely detection of TR is a difficult task, since there are a number of somatic symptoms that are similar to those of diabetic autonomic and distal neuropathy, micro- and macroangiopathies. It is possible to identify TR in patients with DM using psychometric scales - the Hospital Anxiety and Depression Scale (HADS), the Spielberg-Khanin scale. These diagnostic methods are available to both endocrinologists and primary health care professionals.
The International GAD Guideline Group invites general practitioners to ask two questions in order to screen for a disease:
- have you felt restless, tense or anxious most of the time in the last four weeks;
- Do you often have a feeling of tension, irritability and sleep disturbance?
If at least one of the questions received an affirmative answer, it is necessary to ask additional questions to identify TR [13].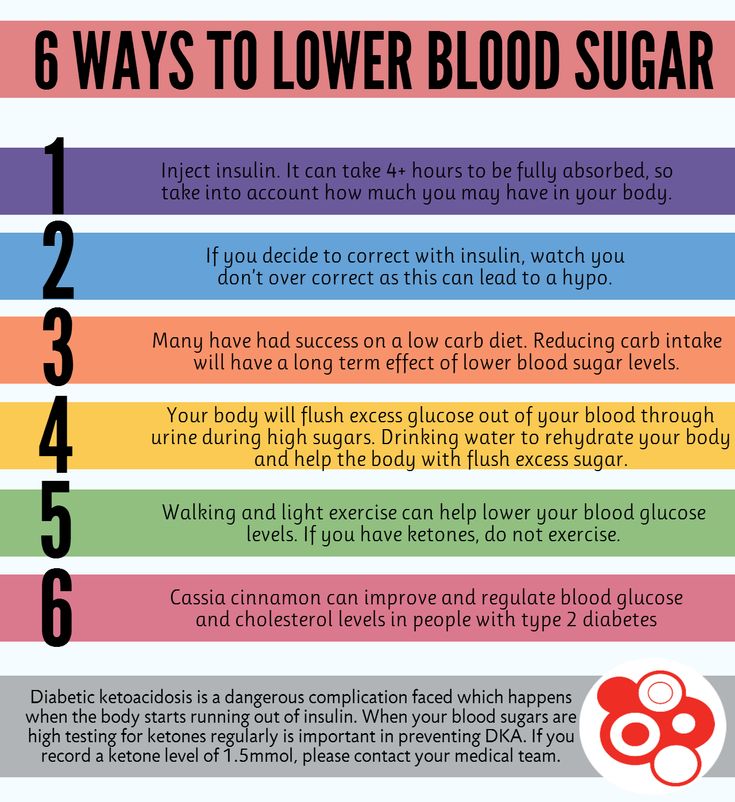
The risk groups for developing TR are patients with severe diabetes. TR should be suspected in patients with labile diabetes, difficult-to-control glycemia, poor adherence to treatment, and non-compliance with lifestyle recommendations. Patients with chronic pain due to diabetic neuropathy are a special risk group. Patients who have a pronounced increase in body weight should also be examined for the presence of TR.
Symptoms of TR can be constant and paroxysmal.
Anxiety can be associated with situations that do not pose a real danger. It is characterized by anxiety of expectation, fears, a tendency to negative forecasts. Often there is unreasonable anxiety.
Patients appear tense, restless, fussy. They tend to constantly adjust their clothes or hair. Patients are not able to completely relax, muscle tone is increased. Patients with TR often replay past and expected events in their heads, which may lead to sleep disorders, difficulty concentrating, and memory impairment.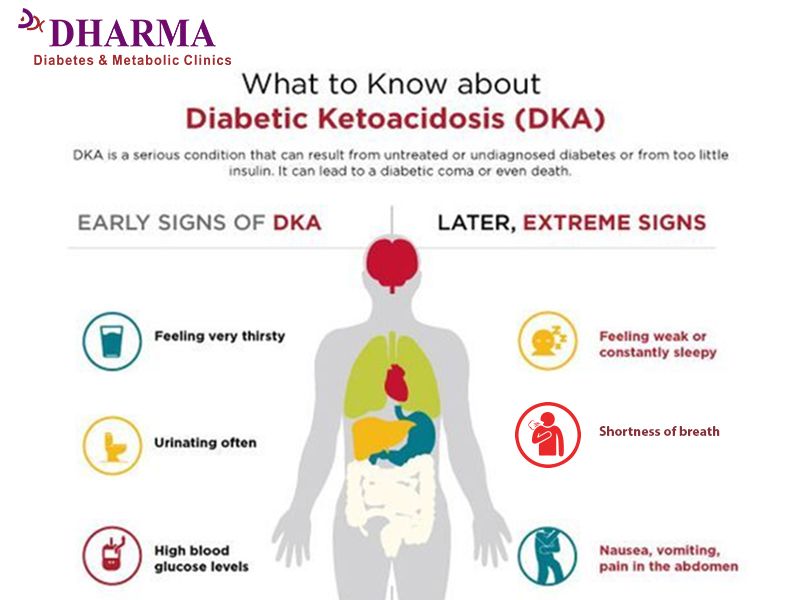 Such patients are characterized by general weakness and increased fatigue.
Such patients are characterized by general weakness and increased fatigue.
However, general weakness in patients with diabetes can be associated with both the presence of TR and long-term decompensation of diabetes. The latter condition can be ruled out by laboratory testing.
Autonomic symptoms of anxiety include palpitations, fluctuations in blood pressure, headaches, nausea, diarrhea, increased urination, pallor or redness of the skin.
The autonomic symptoms of TR need to be differentiated from complications of DM, such as autonomic diabetic neuropathy. Diabetic complications can be identified with special diagnostic tests.
Paroxysmal anxiety proceeds as a panic attack - attacks of pronounced anxiety or fear with various vegetative manifestations (palpitations, sweating, feeling of suffocation, nausea). Often there is a fear of death, a fear of going crazy. Paroxysmal anxiety (panic disorders) should be differentiated from hypoglycemia.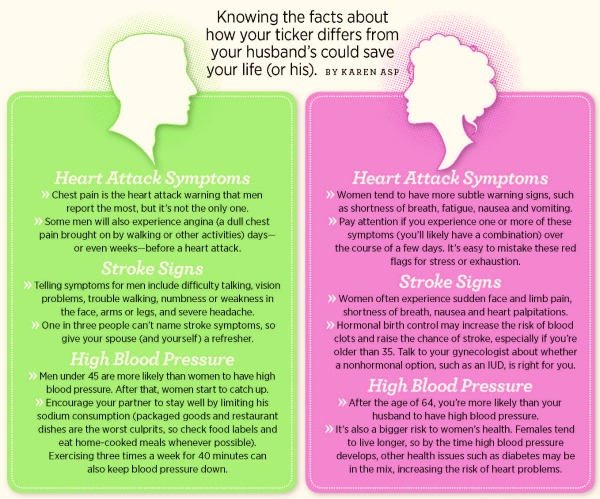 The only reliable confirmation of the latter is the level of glucose in the blood below 3.3 mmol / l, determined using a glucometer.
The only reliable confirmation of the latter is the level of glucose in the blood below 3.3 mmol / l, determined using a glucometer.
If the patient suffers from cardiovascular diseases, panic attacks should also be differentiated from angina attacks, cardiac arrhythmias.
Treatment
With TR, both medication and psychotherapy (mainly cognitive-behavioral and relaxation techniques) are indicated.
Unfortunately, today high-quality psychotherapeutic care is not available to the majority of the population, so pharmacotherapy is of particular importance.
Among patients with DM and TR (n = 90), examined by E.G. Starostina et al., most of them took anti-anxiety drugs prescribed by therapists, neurologists or on their own. At the same time, their doses were insufficient, the courses of treatment were short or, on the contrary, very long. The drugs turned out to be ineffective (herbal remedies) or had a high dependence potential and other side effects (phenobarbital as part of Corvalol and analogues, benzodiazepines) [2].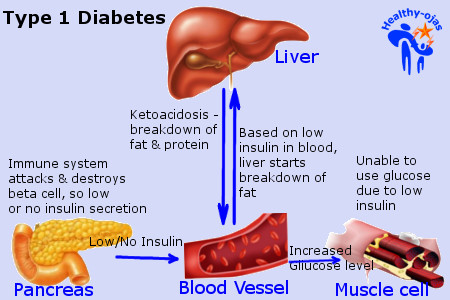 In another study, E.G. Starostina et al. of 87 patients with TR and DM, only 8.0% had previously consulted a psychiatrist and neurologist. Psychotropic drugs previously taken 59.8% of patients with TR, and in 82.7% of cases on their own, without consulting a psychiatrist or neurologist. In the vast majority of cases, these were drugs containing phenobarbital and benzodiazepines [5].
In another study, E.G. Starostina et al. of 87 patients with TR and DM, only 8.0% had previously consulted a psychiatrist and neurologist. Psychotropic drugs previously taken 59.8% of patients with TR, and in 82.7% of cases on their own, without consulting a psychiatrist or neurologist. In the vast majority of cases, these were drugs containing phenobarbital and benzodiazepines [5].
Today, antidepressants, antipsychotics, and anxiolytics are used for TR. From the first group of drugs, selective serotonin reuptake inhibitors (SSRIs) and tricyclics (TCs) can be used. It is necessary to prescribe TC to patients with DM with caution due to the risk of weight gain and deterioration of the glycemic profile during such therapy. In addition, these drugs have pronounced cholinergic and adrenergic side effects, which limits their use in patients with concomitant somatic diseases. A relative disadvantage of SSRIs is an increase in the early stages of treatment of individual symptoms of TR and a delayed anti-anxiety effect. Among the adverse reactions of SSRIs are nausea, increased appetite, sexual dysfunction. The use of antipsychotics in patients with DM also has a number of limitations: the risk of weight gain, dizziness, excessive sedation.
Among the adverse reactions of SSRIs are nausea, increased appetite, sexual dysfunction. The use of antipsychotics in patients with DM also has a number of limitations: the risk of weight gain, dizziness, excessive sedation.
Traditional benzodiazepines (phenazepam, alprazolam, clonazepam), related to anxiolytics, are not recommended for long-term use, since pharmacological dependence develops after 14 days from the start of treatment.
Grandaxin
Therapy for TR requires long-term use of anti-anxiety medications. Of the benzodiazepines, only tofisopam (Grandaxin, Hungary) is allowed for use for three months.
Grandaxin has anti-anxiety and vegetostabilizing effects, while there are no sedative and muscle relaxant effects, which is extremely important for elderly and senile patients [14]. In addition, Grandaxin does not have cardiotoxicity, which is important for patients with diabetes and concomitant diseases of the cardiovascular system [15].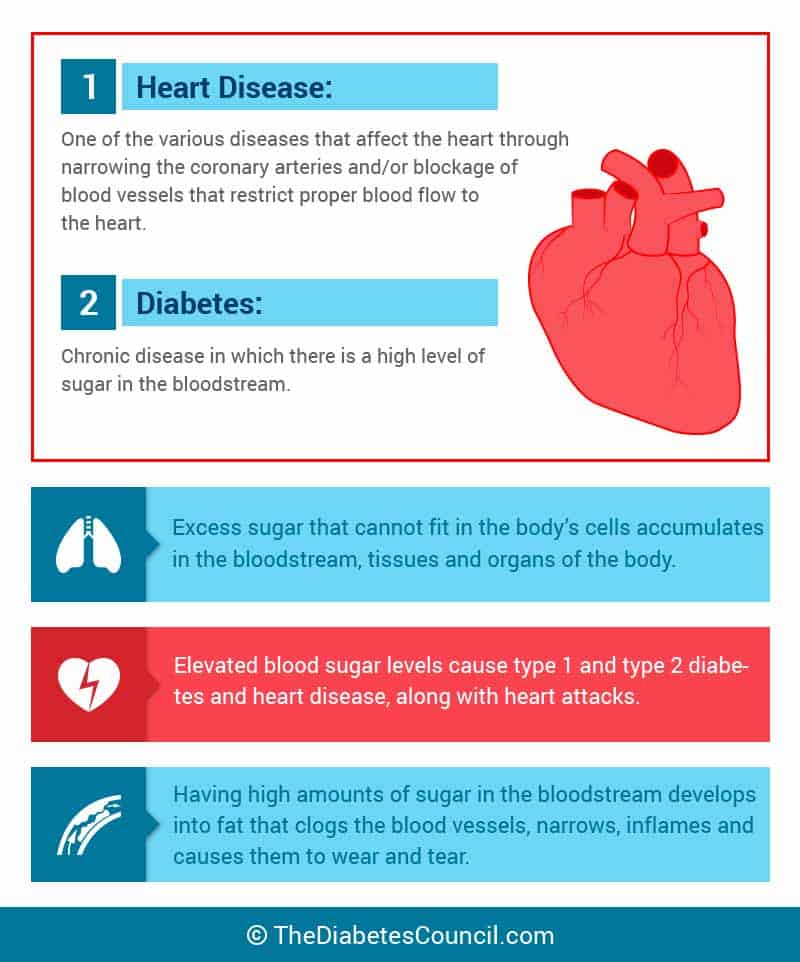
Convenient dosing regimen and low cost are additional advantages of Grandaxin.
The effectiveness of TR therapy with tofisopam (Grandaxin) and hydroxyzine (Atarax) in patients with DM was studied by E.G. Starostina et al. in an open, comparative, randomized prospective study. Participants - 60 patients with DM and TR. The duration of treatment is three months. The follow-up period after discontinuation of drugs is one month. The condition of patients before the start of treatment, after three months of treatment, and one month after its completion was assessed using the Spielberg-Khanin scale, the Giessen Psychosomatic Complaints Questionnaire (GOSP). Tofisopam was prescribed at an average therapeutic dose of 50 mg three times a day.
Anti-anxiety therapy was accompanied by a reduction in the psychological symptoms of TR. A good effect was observed in about 30.0% of patients, satisfactory - in 60.0%, no effect - in 9.0% of patients. The results of comparing the effectiveness of Atarax and Grandaxin are presented in the table.
In patients treated with Grandaxin, an improvement in carbohydrate metabolism was observed - a decrease in the level of HbA1c. In those taking Atarax, the dynamics of HbA1c did not reach statistical significance. In addition, treatment with Grandaxin, in contrast to treatment with Atarax, was accompanied by a significant decrease in heart rate, SBP and DBP.
At the end of the course of treatment, Grandaxin was canceled immediately; no signs of withdrawal syndrome were recorded in patients. Tolerability of Grandaxin was characterized as good. A month after treatment, there was no recurrence of TR [16].
The positive effect of Grandaxin on the cardiovascular system in patients with coronary heart disease (CHD) was also demonstrated in a study by K.Yu. Skvortsova et al. It was shown that the addition of Grandaxin to complex antianginal therapy in patients with IHD was accompanied not only by a decrease in the severity of anxiety and depressive disorder, but also by a more pronounced decrease in the total duration of ischemia (by 53. 0% compared with patients who did not receive Grandaxin) [17].
0% compared with patients who did not receive Grandaxin) [17].
In the work of E.V. Kuleshova drug Grandaxin was used in 23 patients with coronary artery disease and various types of pain syndrome. During therapy, a decrease in psychoemotional disorders was observed in 19 (82.0%) cases. In eight out of 12 patients with atypical pain syndrome, its decrease was recorded. In none of the patients, the frequency and intensity of typical exertional angina attacks changed significantly [15].
Thus, Grandaxin can be considered as an effective and safe drug for the treatment of TR in patients with DM.
Panic attack in diabetes: hypoglycemia
Diabetes mellitus is an endocrine disease that develops due to a violation of the secretion of the hormone insulin, the absorption of glucose by the body, as a result, the level of glucose in the patient's blood rises. The nature of the course of the disease is chronic, fat, carbohydrate, water-salt, mineral and protein metabolism is disturbed.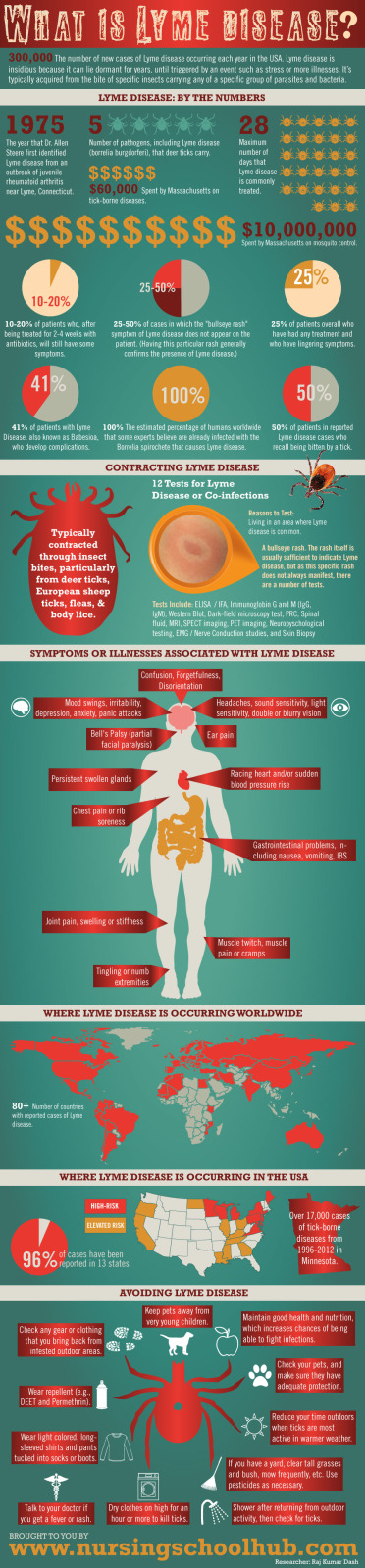 The disease is common. Diabetes mellitus is a common cause of death for older people, it occurs with various complications, often patients suffer from anxiety disorders, depression.
The disease is common. Diabetes mellitus is a common cause of death for older people, it occurs with various complications, often patients suffer from anxiety disorders, depression.
Causes
An important role in the development of the disease is played by psychogenic and somatogenic factors. Studies have shown that anxiety disorders are important manifestations of the disease, have a negative impact on the treatment process, provoke an increased risk of carbohydrate metabolism decompensation, and the development of complications. Panic attacks in diabetes develop with dysfunction of the hypothalamic-pituitary-adrenal system. Severe stress provokes a violation - the hypothalamus begins to secrete corticoliberin, the adrenal glands are activated, the secretion of glucocorticosteroids increases. Prolonged psycho-emotional stress depletes the adrenal glands, violates the principle of negative feedback, in the normal state of which an increase in cortisol levels affects a decrease in the level of corticoliberin.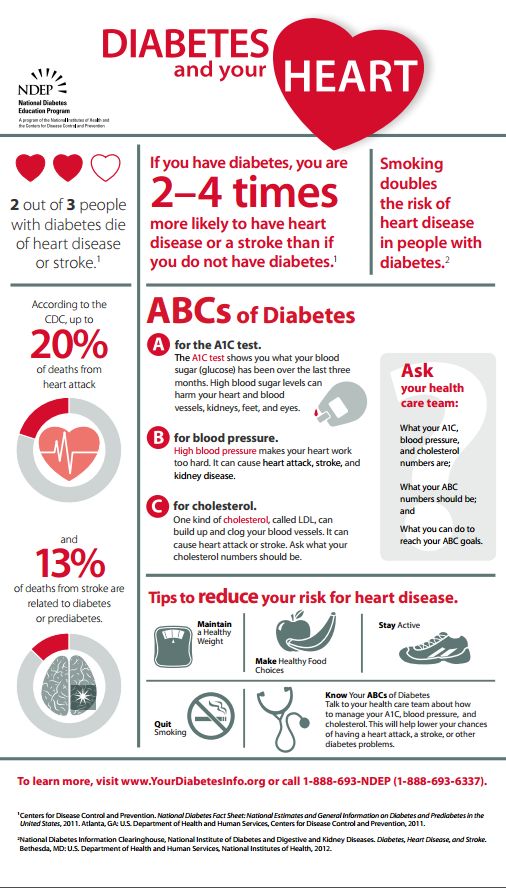
Prolonged stress leads to an increase in the level of the hypothalamic hormone corticoliberin. An increase in the level of corticoliberin affects the central nervous system:
- Disrupts sleep.
- Impairs sexual activity.
- Causes tension, anxiety.
- Provokes fear, severe anxiety.
- Reduces appetite.
- Enhances the reaction of orientation, activation, increases the level of excitability of certain areas of the cerebral cortex.
Panic attack in diabetes and other anxiety disorders lead to a violation of the doctor's recommendations and prescriptions, the patient does not follow the diet, violates the medication. Complicating the course of a chronic disease is the addition of depression to panic disorder. An attack attack causes severe emotional stress, fear of a recurrence of a state of panic. Repeated attacks provoke the development of other mental disorders, worsen the course of the disease. Panic attacks, anxiety disorders affect the social adaptation of patients, reduce the quality of life, patients cease to control their condition.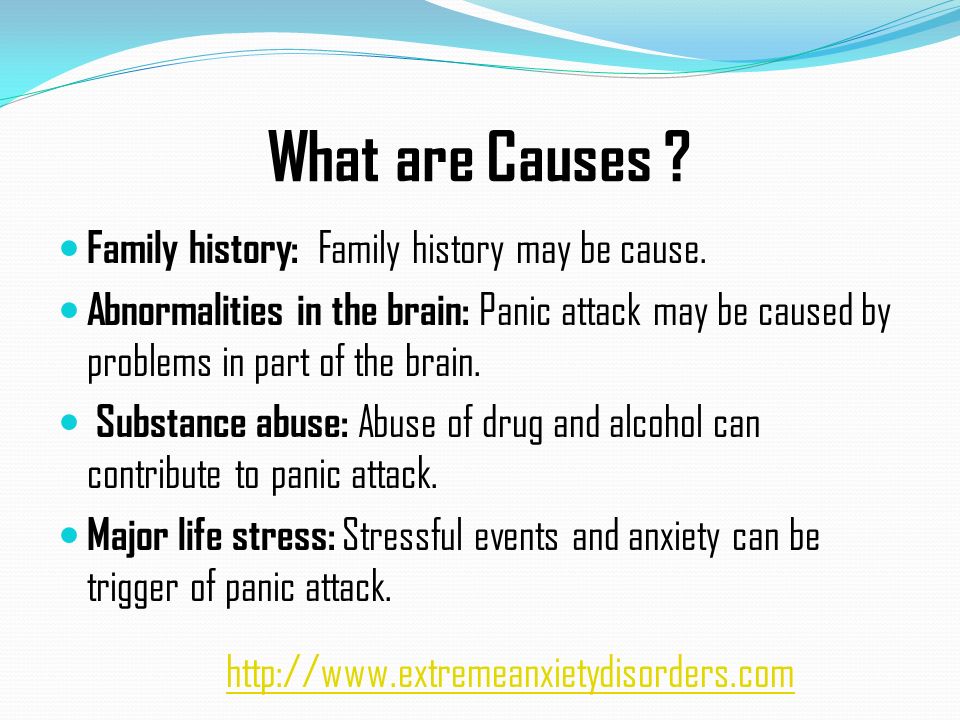
Prolonged emotional stress provokes the development of visceral-vegetative disorders, somatic diseases of organs and body systems. Increase the risk of panic attacks, anxiety disorders in a patient with diabetes bad habits (alcoholism, smoking). The risk group for panic attacks includes patients with severe diabetes mellitus, with chronic, severe pain in diabetic neuropathy, patients with obesity. The disorder can manifest itself in the form of periodic attacks or disturb constantly in the form of strong, often causeless anxiety.
Hypoglycemia and panic attacks
Hypoglycemia has a negative impact on the patient's psyche, it causes mood swings, panic fear, depression, impaired concentration, convulsions, cognitive impairment and other disorders, up to coma. With hypoglycemia, the patient's brain does not receive the glucose necessary for normal functionality, a lack of energy is created. Such a violation is often interpreted by doctors as a panic attack, while a panic attack can be diagnosed as hypoglycemia due to the similarity of symptoms.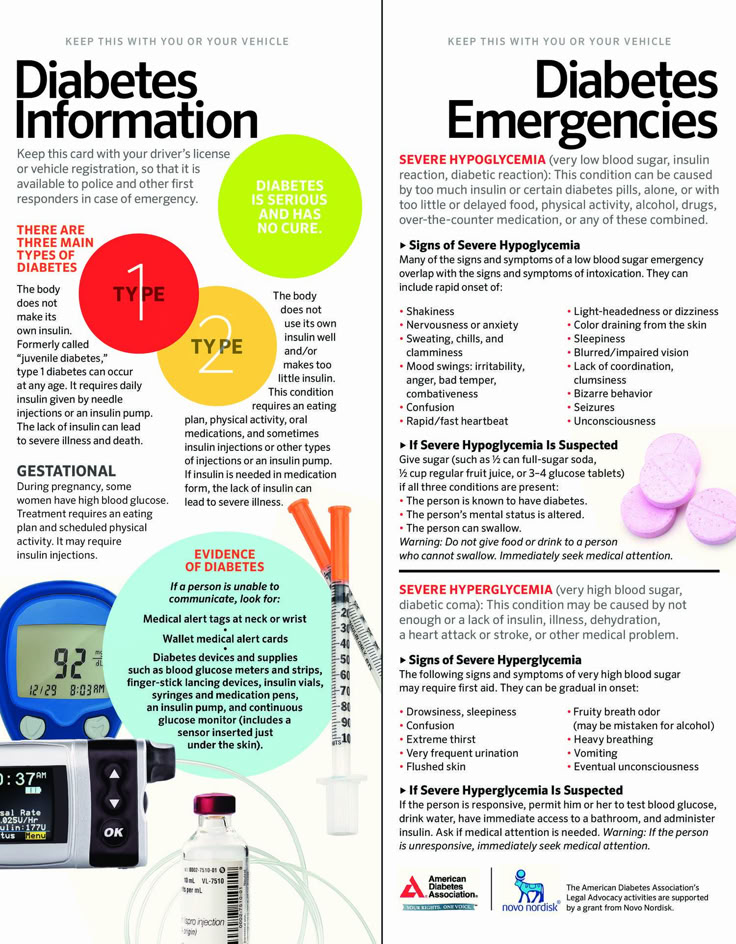
Panic attacks are a more complex psycho-emotional state, which is caused by a combination of various factors.
Diagnosis and treatment
The HADS and the Spielberg-Khanin scale are used to assess the mental state of patients with diabetes mellitus. Scales help to determine the level of depression and anxiety. The disorder is treated with medication and psychotherapy. The main methods of psychotherapy for the treatment of panic attacks are cognitive-behavioral and relaxation techniques. Depending on the individual characteristics of the psyche, concomitant diseases, patients are prescribed antipsychotics, antidepressants (SSRIs, TC), anxiolytics. The disadvantage of SSRI drugs is the side effect in the form of increased panic attacks at the initial stage of treatment, nausea, sexual dysfunction.
A side effect of antipsychotics is the risk of obesity, severe dizziness, lethargy and drowsiness. Long-term use of benzodiazepines is not recommended, they cause dependence.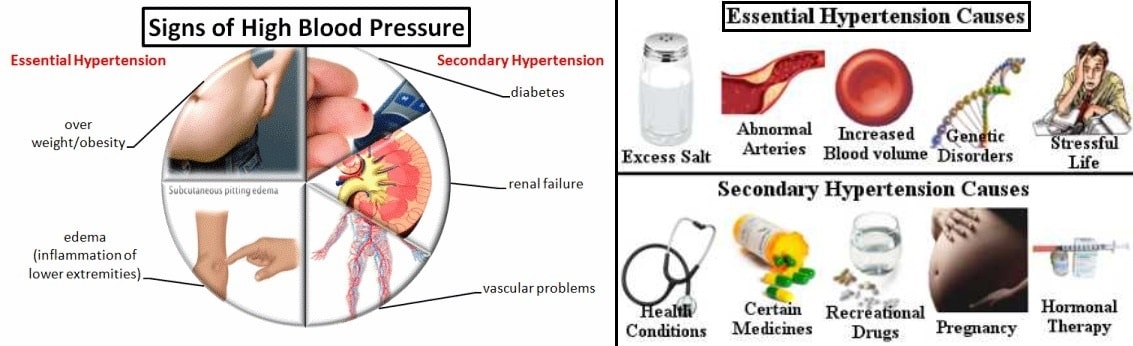 Preparations for panic attacks for a patient with diabetes are selected by a doctor, taking into account concomitant somatic diseases, the severity of the condition.
Preparations for panic attacks for a patient with diabetes are selected by a doctor, taking into account concomitant somatic diseases, the severity of the condition.
- #Articles
Similar articles
13.12.2020
Olga Butakova
Psychosomatics of tongue ulcers
Direction: Psychosomatics
Mouth ulcers are characterized by damage to soft tissues in the area of the tongue, cheeks, lips, palate and larynx. This area is irritated and inflamed, forming a small wound or sore. Ulcers are at risk of bleeding, so it is important to control them and treat them promptly. However, it is not always possible to establish the physical cause of the appearance of such tissue defects. In this case, most likely, psychosomatics takes place [...]
Full text
- #Articles
03/24/2021
Olga Butakova
Psychosomatics of shortness of breath
Direction: Psychosomatics
Shortness of breath can accompany many diseases, in particular the heart or cardiovascular system.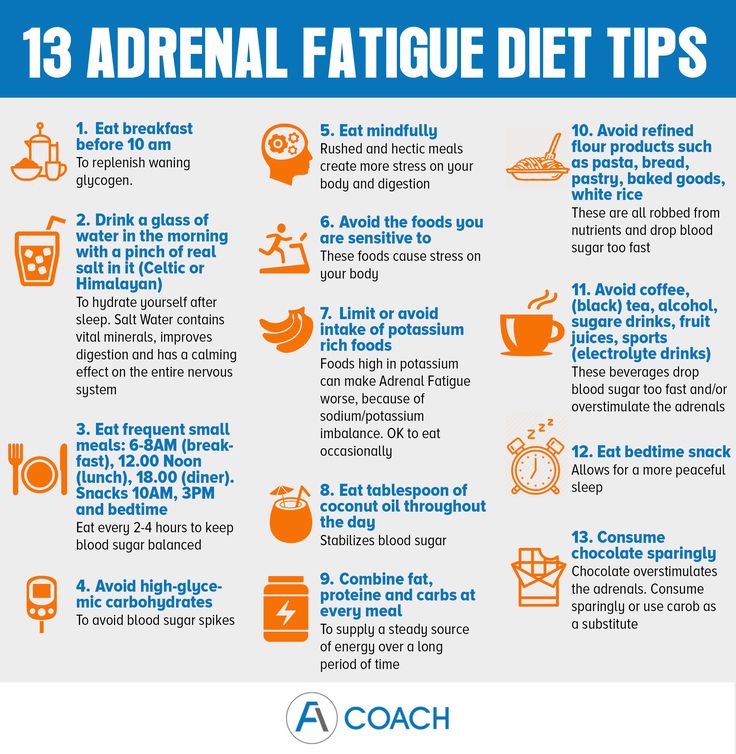 However, it is also a companion of neurotic disorders, when, against the background of emotional overstrain, the normal functioning of the human body is disrupted. This phenomenon is referred to as psychosomatic symptoms. In this case, difficulty in breathing is usually not associated with any physical pathology, so this condition requires a special therapeutic approach. Shortness of breath and […]
However, it is also a companion of neurotic disorders, when, against the background of emotional overstrain, the normal functioning of the human body is disrupted. This phenomenon is referred to as psychosomatic symptoms. In this case, difficulty in breathing is usually not associated with any physical pathology, so this condition requires a special therapeutic approach. Shortness of breath and […]
Full text
14.12.2020
Olga Butakova
Psychosomatics of testicular cysts in men
Direction: Psychosomatics
Spermatocele (also called an epididymal cyst) is a dense sac filled with a liquid substance (including seminal fluid) that grows close to the outer layer of the skin. This sac is located in the scrotum and surrounds the back and top of the testicle. There are several main reasons for the development of this disease, but including the psychosomatics of the testicular cyst […]
Full text
- #Articles
11/21/2020
Olga Butakova
Cat allergy psychosomatics
Specialization: Psychosomatics
Allergic reactions are a common problem in modern society. Allergy to animal hair can appear suddenly, it causes unpleasant symptoms, which many people fight with the help of pharmaceutical drugs. However, in some cases, drugs do not bring positive results, since an allergy to animal hair may be due to psychosomatic causes. Psychosomatics is one of […]
Allergy to animal hair can appear suddenly, it causes unpleasant symptoms, which many people fight with the help of pharmaceutical drugs. However, in some cases, drugs do not bring positive results, since an allergy to animal hair may be due to psychosomatic causes. Psychosomatics is one of […]
Full text
- #Articles
11/23/2020
Olga Butakova
Psychosomatics of warts
Direction: Psychosomatics
Warts are small benign formations that appear on the skin. They are also called papillomas because they are the result of the activity of the human papillomavirus (HPV). Nodules can appear on the body as a result of a decrease in immune defense, which occurs during hypothermia, after an illness, or due to stress. Therefore, in the treatment of these neoplasms, the psychosomatics of the wart plays an important role. What are warts […]
Full text
- #Articles
11/23/2020
Olga Butakova
Throws into a fever during a panic attack
Direction: Psychosomatics
Panic attack is not a cause, but a symptom.