Can fluoxetine make you tired
Fluoxetine | SSRI Uses, Warnings & Side Effects
About fluoxetine
Please note
Thinking about trying medication? Read our guide
How fluoxetine works
Fluoxetine is a type of antidepressant called a selective serotonin reuptake inhibitor (SSRI).
Research suggests that depression or low mood is more likely to occur when the brain doesn’t have enough serotonin.
Serotonin (also called '5HT') is a naturally-occurring chemical messenger (or “neurotransmitter”) that has an important role in areas of the brain that control mood and thinking.
Selective serotonin reuptake inhibitors (SSRIs) - like fluoxetine - are thought to work by increasing levels of serotonin in the brain. They do this by blocking the recycling of released serotonin back into the nerve endings.
Fluoxetine is often prescribed alongside a talking therapy.
Find out more about depressionFluoxetine and everyday life
Frequently asked questions
Antidepressants like fluoxetine can start to work on depression within the first two weeks of treatment, with the improvements continuing over the following weeks,
For anxiety, antidepressants like fluoxetine can take slightly longer to work. For some people, anxiety briefly increases at the start of treatment, but the anxiety does decrease with continued treatment.
Your weight can be affected by fluoxetine.
A side effect of fluoxetine can be not feeling as hungry as normal, which might lead to weight loss.
It is very difficult to know how this will affect each person who takes it.
Talk to your doctor about this if it worries you.
You may want to let your family and friends know you are taking fluoxetine effects.
For guidance on this, check out our page on getting support with your medication.
You can feel drowsy in the first few days of taking fluoxetine. However, it should get better after the first week or two. You may become more anxious, or it may make you irritable. This should settle after a couple of weeks.
If you feel very sleepy, and you’ve been taking it for more than a month, you should go back to the doctor and see what else you could do.
Alcohol
You can continue to drink some alcohol while taking fluoxetine, but it is best to do so in moderation. Fluoxetine can sometimes cause drowsiness as a side effect, so it is possible that alcohol might make you feel more drowsy than usual.
Drinking alcohol every day, however, can make the symptoms of depression worse and you will not feel the benefit of your medicine.
Side effects might make you sleepy or you might lose your focus when you first start taking fluoxetine.
This could be dangerous if you drive or use machines or do anything that needs a lot of focus.
During the first few days, it might be best to stop drinking alcohol until you see how the medicine affects you, or until the effects pass.
Street drugs
Be careful if you are also using street drugs.
Cannabis can have unpredictable effects when taken with fluoxetine, so great care is needed.
Cannabis and other drugs may have their own side effects on your mental health, like anxiety or psychosis. For more information, have a look at our drugs and alcohol page.
For more information, have a look at our drugs and alcohol page.
Methadone and fluoxetine together can seriously affect your heart so these should only be combined under doctor supervision.
Fluoxetine has been shown to dampen down the 'high' of cocaine.
Taking fluoxetine with cocaine, ecstasy or amfetamines could bring on serotonin syndrome. You could get a high temperature/fever, agitation, confusion, trembling or weird muscle movements. You need to go to hospital if this happens. Tell the doctor everything that you have taken.
Fluoxetine can produce a false positive test for amfetamines and LSD on a urine drug screen. Talk to your doctor about this if it is a problem for you.
Fluoxetine does not mix well with some other medicines and drugs.
Do not take fluoxetine if you take an antidepressant medicine called a monoamine oxidase inhibitor (MAOI), or if you have taken one in the last two weeks. MAOIs include moclobemide, isocarboxazid, phenelzine and tranylcypromine.
Tell your doctor or pharmacist before you take fluoxetine if you are prescribed any other medication, to check that the combination is safe.
Before you start taking fluoxetine, tell your doctor if you are taking any other medications, including things you have bought over the counter for common illnesses like colds and flu or topical applications that you put on your skin.
Let your pharmacist know if you have any food allergies or intolerances, and always check with them if you’re concerned about any of the ingredients in your medication.
Do not drive or ride a bike just after you start taking fluoxetine.
Taking fluoxetine may affect your ability to do things like drive a car, ride a bike, use machines, or anything else that needs a lot of focus.
It might be best to stop doing these things for the first few days, until you know how it affects you, or until the effects pass.
Do not worry - most people drive as normal while taking fluoxetine.
Pregnancy
If you become pregnant while you are on fluoxetine, you should carry on taking the medicine and go back to your doctor as soon as possible, to see if you should change or stop your medicine.
There is a slightly higher risk of problems in the developing baby if you take fluoxetine it in the early stages of pregnancy. However, fluoxetine and related antidepressants (known as SSRIs) are thought to be better choices if you need antidepressant medicine.
Remember that you need to stay well through your pregnancy, and you may need a medicine to help you to do that.
Fluoxetine may cause heart problems in the developing baby, and other symptoms in new-born babies.
If you and your doctor agree that you will continue taking fluoxetine during your pregnancy, then you should tell your midwife that you are taking it before you give birth.
Post-natal
If fluoxetine is taken in the last five months of a pregnancy, it can cause a serious condition called persistent pulmonary hypertension of the new-born (PPHN). This can make the baby breathe faster and look a bit blue in colour. PPHN affects around three in 1,000 babies born to mums who take SSRIs. This compares with a rate of two in 1,000 among babies born to mums who do not take SSRIs.
This can make the baby breathe faster and look a bit blue in colour. PPHN affects around three in 1,000 babies born to mums who take SSRIs. This compares with a rate of two in 1,000 among babies born to mums who do not take SSRIs.
PPHN appears in the first 24 hours after birth. You will need help from the midwife and doctors, so it is better if they are looking out for symptoms.
The newborn baby may also develop withdrawal effects, which might not appear straight away but might develop over the first few days of life. These could include:
- being irritable and crying a lot
- having difficulty sleeping or sucking
- poor weight gain
Breastfeeding
Fluoxetine is passed to the baby in breast milk, and side effects have been seen in breastfed babies. The main one is likely to be colic.
The amount of fluoxetine in breast milk is usually around 7% of the mum’s dose, but it can build up over time. This is because fluoxetine is hard for your baby to get rid of.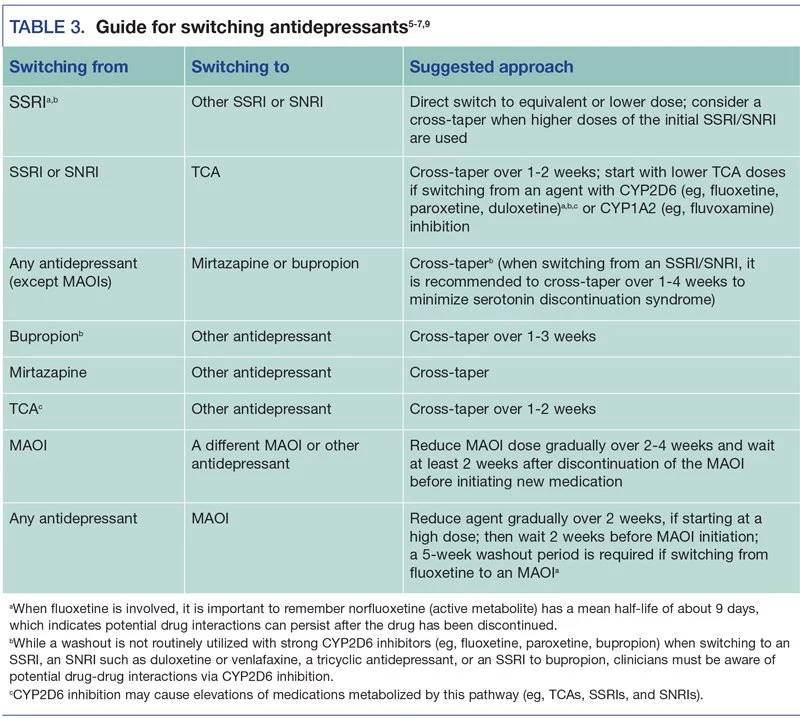 This does not mean breastfeeding will be a problem, but do look out for side effects.
This does not mean breastfeeding will be a problem, but do look out for side effects.
If your baby was premature or has health problems, then you may be better off not breastfeeding as your baby will likely struggle even more to get rid of the fluoxetine.
Talk to your doctor or midwife about your feeding options.
Sex
Fluoxetine can have side effects that might affect your sex life. These include:
- painful erections that last for a long time (this is rare but serious - visit a hospital or see your doctor straight away if you experience this side effect), or problems getting an erection (getting hard) and ejaculating (coming)
- bleeding from the vagina
- difficulty reaching orgasm the same way as before
- some growth of the breasts and some milk flow, regardless of gender
- you may have a lower sex drive
Fluoxetine has been known to slow growth and delay sexual development (puberty) in a small number of children and young people. Your doctor should check your growth while you are taking it. If this worries you, talk to your doctor or pharmacist about it.
Your doctor should check your growth while you are taking it. If this worries you, talk to your doctor or pharmacist about it.
These effects should pass after the first couple of weeks. If they do not, and this is a problem for you, go back to the doctor and see what else you could try.
The good effects of fluoxetine may, after a while, have a positive impact on your sex life as your mood lifts and you become interested in life and relationships again.
Fertility
Fluoxetine does not seem to affect human fertility.
Talk to your doctor about your fluoxetine if you are trying to get pregnant.
Fluoxetine is not a banned substance in sport.
Taking fluoxetine may affect your ability to do things like riding a bike, competitive gymnastics, or anything else that needs a lot of focus.
It might be best to stop such sports for the first few days, until you know how it affects you or the effects get better.
Do not worry - most people play sports as normal while taking fluoxetine.
Try not to take fluoxetine for the first time just before your exams.
Taking fluoxetine may affect your ability to do things that need a lot of focus, like exams.
You should talk to your doctor about any future exams if you are starting fluoxetine.
You might decide together to delay starting it until you have done them. If they are more than a month away, however, you might find that it is better to start fluoxetine to lift your mood and improve your motivation to study.
Do not worry - most people do exams as normal while taking fluoxetine.
Uses, warnings, safety and side effects of fluoxetine
Taking fluoxetine
How long will I need to take fluoxetine for?
Most people take fluoxetine for at least six to 12 months after they start to feel better.
If you have suffered from depression in the past, you should keep taking this medication for at least two years after you start to feel better.
You and your doctor should talk about how long you need to take fluoxetine before you begin your treatment.
If you stop taking the fluoxetine too soon, the chance that your mental health symptoms will come back increases.
You should only take fluoxetine as agreed with your doctor
You will get the best effect from fluoxetine if you take it every day at the dose prescribed by your doctor.
Your doctor might start you on a low dose and then increase it to your full dose slowly over two to four weeks.
Make sure that you know your dose. If it's not written on the label, check with your pharmacist or doctor.
Young people aged eight to 18 may start taking fluoxetine at a lower dose using the liquid, and then move on to the capsules if the dose increases.
It is usually best to take fluoxetine in the morning. This is to reduce the chance of it causing insomnia (difficulty sleeping). However, it is important to choose a time each day that you can always remember. This could be when you wake up, a mealtime, or when you brush your teeth.
Fluoxetine is best taken after food.
Swallow the capsule with a drink of water - if you chew it, it tastes bitter.
What should I do if I miss a dose of fluoxetine?
If you remember later during the day, take it as soon as possible.
You may find it difficult to sleep if you take it towards bedtime.
If you forget to take it by the time of your next dose, just take the next dose.
Do not take a double dose.
What will happen if I forget to take my fluoxetine?
If you forget to take it for a few days, you may start getting withdrawal symptoms and should talk to your doctor about it.
Stopping the use of fluoxetine
Stopping fluoxetine suddenly can sometimes cause side effects, which are usually mild, but for a few people can be severe. Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases.
Once you start taking an SSRI, the brain adjusts to having a new level of serotonin around. If you stop taking the SSRI suddenly, the balance starts to change again.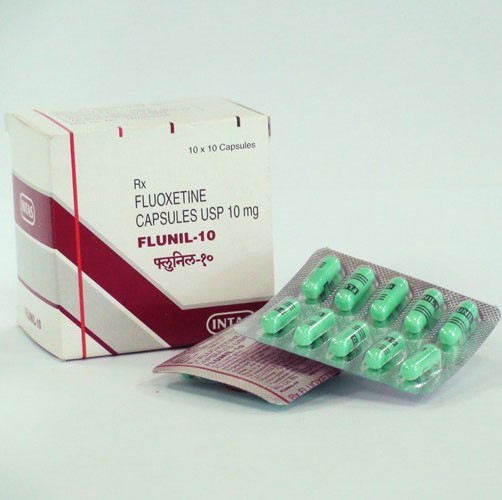 You could get some symptoms from the change.
You could get some symptoms from the change.
Fluoxetine is less likely to cause withdrawal effects upon stopping than other antidepressant medicines. This is because your body takes longer to get rid of it.
You can stop taking fluoxetine safely with your doctor’s help. Many people who take 20mg or less of fluoxetine can stop taking it without problems. For people on higher doses of fluoxetine, the dose may be stepped down over a few weeks to reduce the chance of withdrawal effects.
Fluoxetine and other antidepressants are not addictive. Although there can be withdrawal effects when they are stopped, you will not have cravings for or get ‘hooked’ on an antidepressant.
Some of the withdrawal effects you might get when fluoxetine is stopped include:
- flu-like symptoms such as chills, muscle aches, excessive sweating, headache, and feeling or being sick
- feeling unusually tired or weak
- sleep disturbances such as difficulty sleeping or vivid dreams
- electric shock-like sensations - especially down the spine (back)
- dizziness, especially when moving
- feeling anxious, restless, irritable, or agitated
- difficulty remembering things or concentrating on things
These symptoms should stop after two weeks for most people, but some people can get them for a few months.
Warnings and safety
Safety headlines
If you have taken more fluoxetine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking fluoxetine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Fluoxetine can also cause rare but serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), rashes or blotches on your skin, and a rare condition called serotonin syndrome (see 'Side Effects'). Go to a hospital with your medicine if you get any of these symptoms.
Do not take fluoxetine if you have taken a monoamine oxidase inhibitor antidepressant (MAOI) like moclobemide, phenelzine, isocarboxazid or tranylcypromine in the last 14 days.
Stopping fluoxetine suddenly can sometimes cause withdrawal effects, which are usually mild, but for a few people can be severe. Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases. See your doctor if you want to stop fluoxetine or have withdrawal effects after stopping it.
Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases. See your doctor if you want to stop fluoxetine or have withdrawal effects after stopping it.
You might not be able to concentrate very well, and may feel sleepy, in the first few days after taking fluoxetine. Do not drive a car, ride a bike or operate machines until you see how this affects you.
If you are pregnant, or thinking of becoming pregnant, please read the pregnancy section (see ‘Side Effects') because fluoxetine may affect the developing baby.
When to go to the hospital
If you have taken more fluoxetine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
Go to A&E. Take your medicine with you to show to the doctors. Tell them how much you have taken. Get a friend or family member to go with you, if you can, just in case you feel ill on the way.
You might get any of the following signs:
- feeling sick or being sick
- having seizures (fits)
- an irregular heartbeat or a heart attack
- breathing difficulties
- a change in the way you feel, ranging from agitation to falling into a coma
You are also at risk of getting ‘serotonin syndrome’ (symptoms include a high fever, agitation, confusion, trembling, shivering and excessive sweating or weird movements of your muscles). This is rare, but you should watch out for it.
If you have any thoughts of taking your own life or of other ways of hurting yourself, go straight to a hospital with your medicine. This may be a side effect and is more common at the start of treatment. Thoughts of suicide are more likely to occur if you are under 25 years old. Fluoxetine is safer than other antidepressants for people under the age of 18.
You must stop taking Fluoxetine and go straight to hospital if you have any of the following symptoms:
- tiredness, confusion, headache, irritability, feeling or being sick (nausea and vomiting), and muscle twitching.
 These can be symptoms of a low blood level of sodium, but some of these are also symptoms of serotonin syndrome
These can be symptoms of a low blood level of sodium, but some of these are also symptoms of serotonin syndrome - rashes; blotches; itching; blistering; redness; peeling; or ulcers on your skin, in your mouth, or in your genital area. These can be symptoms of a rare but serious skin reaction
- difficulty breathing, swelling of your face or throat, and itching skin lumps. These may be symptoms of an allergic reaction
- having seizures (fits)
- feeling very excited or ‘high’
Go to a doctor or hospital straight away but do not stop taking your fluoxetine if you get the following symptoms:
- your behaviour changes because you feel irritated or agitated
- you get an erection that is painful and lasts for a long time (priapism)
Side effects of fluoxetine
Side effects of fluoxetine
Please do not be worried by the side effects listed on this page. Many people take fluoxetine without any side effects or only a few mild side effects. Starting with a lower dose can sometimes help if side effects do occur.
Starting with a lower dose can sometimes help if side effects do occur.
Side effects that do appear should disappear or get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the fluoxetine until you talk to your doctor, or you may get withdrawal symptoms as well.
Very common side effects when taking fluoxetine (affecting more than one in ten people) include:
- insomnia (sleep problems)
- headache and feeling tired
- diarrhoea (loose poo)
- nausea (feeling sick)
Common side effects of taking fluoxetine (affecting up to one in ten people) include:
- not feeling hungry
- weight loss
- nervousness, anxiety, restlessness, poor concentration, feeling tense
- decreased sex drive or sexual problems, including difficulty maintaining an erection (staying hard)
- sleep problems, unusual dreams, tiredness or sleepiness
- dizziness
- change in taste, or dry mouth
- uncontrollable shaking movements
- blurred vision
- heartbeat feels quick and uneven
- flushing, sweating more, feeling shaky or chills
- yawning
- indigestion, being sick
- rash, itching lumps (hives, urticaria), other skin itching
- joint pain
- needing to wee more often
- unexplained vaginal bleeding
There are other side effects that you can get when taking this medicine – we have only included the most common ones here.
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
Taking fluoxetine
How long will I need to take fluoxetine for?
Most people take fluoxetine for at least six to 12 months after they start to feel better.
If you have suffered from depression in the past, you should keep taking this medication for at least two years after you start to feel better.
You and your doctor should talk about how long you need to take fluoxetine before you begin your treatment.
If you stop taking the fluoxetine too soon, the chance that your mental health symptoms will come back increases.
You should only take fluoxetine as agreed with your doctor
You will get the best effect from fluoxetine if you take it every day at the dose prescribed by your doctor.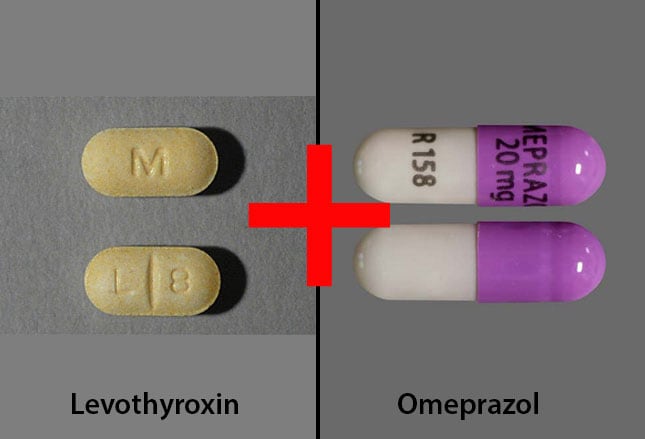
Your doctor might start you on a low dose and then increase it to your full dose slowly over two to four weeks.
Make sure that you know your dose. If it's not written on the label, check with your pharmacist or doctor.
Young people aged eight to 18 may start taking fluoxetine at a lower dose using the liquid, and then move on to the capsules if the dose increases.
It is usually best to take fluoxetine in the morning. This is to reduce the chance of it causing insomnia (difficulty sleeping). However, it is important to choose a time each day that you can always remember. This could be when you wake up, a mealtime, or when you brush your teeth.
Fluoxetine is best taken after food.
Swallow the capsule with a drink of water - if you chew it, it tastes bitter.
What should I do if I miss a dose of fluoxetine?
If you remember later during the day, take it as soon as possible.
You may find it difficult to sleep if you take it towards bedtime.
If you forget to take it by the time of your next dose, just take the next dose.
Do not take a double dose.
What will happen if I forget to take my fluoxetine?
If you forget to take it for a few days, you may start getting withdrawal symptoms and should talk to your doctor about it.
Stopping the use of fluoxetine
Stopping fluoxetine suddenly can sometimes cause side effects, which are usually mild, but for a few people can be severe. Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases.
Once you start taking an SSRI, the brain adjusts to having a new level of serotonin around. If you stop taking the SSRI suddenly, the balance starts to change again. You could get some symptoms from the change.
Fluoxetine is less likely to cause withdrawal effects upon stopping than other antidepressant medicines. This is because your body takes longer to get rid of it.
You can stop taking fluoxetine safely with your doctor’s help. Many people who take 20mg or less of fluoxetine can stop taking it without problems. For people on higher doses of fluoxetine, the dose may be stepped down over a few weeks to reduce the chance of withdrawal effects.
Many people who take 20mg or less of fluoxetine can stop taking it without problems. For people on higher doses of fluoxetine, the dose may be stepped down over a few weeks to reduce the chance of withdrawal effects.
Fluoxetine and other antidepressants are not addictive. Although there can be withdrawal effects when they are stopped, you will not have cravings for or get ‘hooked’ on an antidepressant.
Some of the withdrawal effects you might get when fluoxetine is stopped include:
- flu-like symptoms such as chills, muscle aches, excessive sweating, headache, and feeling or being sick
- feeling unusually tired or weak
- sleep disturbances such as difficulty sleeping or vivid dreams
- electric shock-like sensations - especially down the spine (back)
- dizziness, especially when moving
- feeling anxious, restless, irritable, or agitated
- difficulty remembering things or concentrating on things
These symptoms should stop after two weeks for most people, but some people can get them for a few months.
Warnings and safety
Safety headlines
If you have taken more fluoxetine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking fluoxetine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Fluoxetine can also cause rare but serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), rashes or blotches on your skin, and a rare condition called serotonin syndrome (see 'Side Effects'). Go to a hospital with your medicine if you get any of these symptoms.
Do not take fluoxetine if you have taken a monoamine oxidase inhibitor antidepressant (MAOI) like moclobemide, phenelzine, isocarboxazid or tranylcypromine in the last 14 days.
Stopping fluoxetine suddenly can sometimes cause withdrawal effects, which are usually mild, but for a few people can be severe. Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases. See your doctor if you want to stop fluoxetine or have withdrawal effects after stopping it.
Also, if you stop taking fluoxetine too soon, the chance that your mental health symptoms will come back increases. See your doctor if you want to stop fluoxetine or have withdrawal effects after stopping it.
You might not be able to concentrate very well, and may feel sleepy, in the first few days after taking fluoxetine. Do not drive a car, ride a bike or operate machines until you see how this affects you.
If you are pregnant, or thinking of becoming pregnant, please read the pregnancy section (see ‘Side Effects') because fluoxetine may affect the developing baby.
When to go to the hospital
If you have taken more fluoxetine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
Go to A&E. Take your medicine with you to show to the doctors. Tell them how much you have taken. Get a friend or family member to go with you, if you can, just in case you feel ill on the way.
You might get any of the following signs:
- feeling sick or being sick
- having seizures (fits)
- an irregular heartbeat or a heart attack
- breathing difficulties
- a change in the way you feel, ranging from agitation to falling into a coma
You are also at risk of getting ‘serotonin syndrome’ (symptoms include a high fever, agitation, confusion, trembling, shivering and excessive sweating or weird movements of your muscles). This is rare, but you should watch out for it.
If you have any thoughts of taking your own life or of other ways of hurting yourself, go straight to a hospital with your medicine. This may be a side effect and is more common at the start of treatment. Thoughts of suicide are more likely to occur if you are under 25 years old. Fluoxetine is safer than other antidepressants for people under the age of 18.
You must stop taking Fluoxetine and go straight to hospital if you have any of the following symptoms:
- tiredness, confusion, headache, irritability, feeling or being sick (nausea and vomiting), and muscle twitching.
 These can be symptoms of a low blood level of sodium, but some of these are also symptoms of serotonin syndrome
These can be symptoms of a low blood level of sodium, but some of these are also symptoms of serotonin syndrome - rashes; blotches; itching; blistering; redness; peeling; or ulcers on your skin, in your mouth, or in your genital area. These can be symptoms of a rare but serious skin reaction
- difficulty breathing, swelling of your face or throat, and itching skin lumps. These may be symptoms of an allergic reaction
- having seizures (fits)
- feeling very excited or ‘high’
Go to a doctor or hospital straight away but do not stop taking your fluoxetine if you get the following symptoms:
- your behaviour changes because you feel irritated or agitated
- you get an erection that is painful and lasts for a long time (priapism)
Side effects of fluoxetine
Side effects of fluoxetine
Please do not be worried by the side effects listed on this page. Many people take fluoxetine without any side effects or only a few mild side effects. Starting with a lower dose can sometimes help if side effects do occur.
Starting with a lower dose can sometimes help if side effects do occur.
Side effects that do appear should disappear or get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the fluoxetine until you talk to your doctor, or you may get withdrawal symptoms as well.
Very common side effects when taking fluoxetine (affecting more than one in ten people) include:
- insomnia (sleep problems)
- headache and feeling tired
- diarrhoea (loose poo)
- nausea (feeling sick)
Common side effects of taking fluoxetine (affecting up to one in ten people) include:
- not feeling hungry
- weight loss
- nervousness, anxiety, restlessness, poor concentration, feeling tense
- decreased sex drive or sexual problems, including difficulty maintaining an erection (staying hard)
- sleep problems, unusual dreams, tiredness or sleepiness
- dizziness
- change in taste, or dry mouth
- uncontrollable shaking movements
- blurred vision
- heartbeat feels quick and uneven
- flushing, sweating more, feeling shaky or chills
- yawning
- indigestion, being sick
- rash, itching lumps (hives, urticaria), other skin itching
- joint pain
- needing to wee more often
- unexplained vaginal bleeding
There are other side effects that you can get when taking this medicine – we have only included the most common ones here.
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
The information on this page was reviewed by the College of Mental Health Pharmacy in March 2020.
Visit the CMHP websiteCMHP. College of Mental Health Pharmacy
Side effects of fluoxetine - NHS
Like all medicines, fluoxetine can cause side effects in some people, but many people have no side effects or only minor ones.
Some of the common side effects will gradually improve as your body gets used to it.
Common side effects
These common side effects of fluoxetine happen in more than 1 in 100 people. There are things you can do to help cope with them:
Feeling sick (nausea)Try taking fluoxetine with or after food. It may also help to stick to simple meals and avoid rich or spicy food.
It may also help to stick to simple meals and avoid rich or spicy food.
Make sure you rest and drink plenty of fluids. Try not to drink too much alcohol. Ask your pharmacist to recommend a painkiller.
Headaches usually go away after the first week of taking fluoxetine. Talk to your doctor if they last longer than a week or are severe.
Being unable to sleepTake fluoxetine first thing in the morning.
DiarrhoeaDrink plenty of water or other fluids to avoid dehydration. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee.
Do not take any other medicines to treat diarrhoea without speaking to a pharmacist or doctor.
If you take contraceptive pills and you have severe diarrhoea for more than 24 hours, your contraceptive pills may not protect you from pregnancy. Check the pill packet to find out what to do.
Check the pill packet to find out what to do.
If fluoxetine makes you feel tired or weak, stop what you’re doing and sit or lie down until you feel better.
Do not drive, ride a bike or use tools or machinery if you’re feeling tired. It’s best not to drink alcohol as it will make you feel worse.
If these symptoms do not go away after a week or two, ask your doctor for advice.
Speak to a doctor or pharmacist if the advice on how to cope does not help and a side effect is still bothering you or does not go away.
Serious side effects
It happens rarely (in less than 1 in 100 people), but some people may have serious side effects when taking fluoxetine.
Book an appointment with your doctor if you:
- gain weight gain or lose weight without trying
- get changes in your periods such as heavy bleeding, spotting, or bleeding between periods
Call a doctor or contact 111 straight away if you:
- get feelings of overwhelming happiness (euphoria), excessive enthusiasm or excitement, or a feeling of restlessness that means you cannot sit or stand still
- are bleeding from the gums or get bruises that appear without a reason or that get bigger
- are coughing up blood, or have blood in your pee
- have black or red poo, or blood in your vomit – these can be signs of bleeding in your stomach
Go to 111. nhs.uk or call 111.
nhs.uk or call 111.
Immediate action required: Call 999 or go to A&E now if:
- you get chest pain or pressure, or shortness of breath
- you get severe dizziness or pass out
- you get painful erections that last longer than 2 hours – this may happen even when you are not having sex
- you have a fit or seizure
- you get headaches, have trouble focusing, have memory problems, cannot think clearly, have a seizure or fit, or lose your balance – these can be signs of low sodium levels
- you have thoughts about harming yourself or ending your life
- you get any severe bleeding, or bleeding that you cannot stop, such as cuts or nosebleeds that do not stop within 10 minutes
Serious allergic reaction
In rare cases, it's possible to have a serious allergic reaction (anaphylaxis) to fluoxetine.
Immediate action required: Call 999 or go to A&E now if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you're wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
Long-term side effects
Sexual side effects, such as problems getting an erection or a lower sex drive, have been reported after taking fluoxetine for a long time. In some cases, these can continue even after stopping the medicine.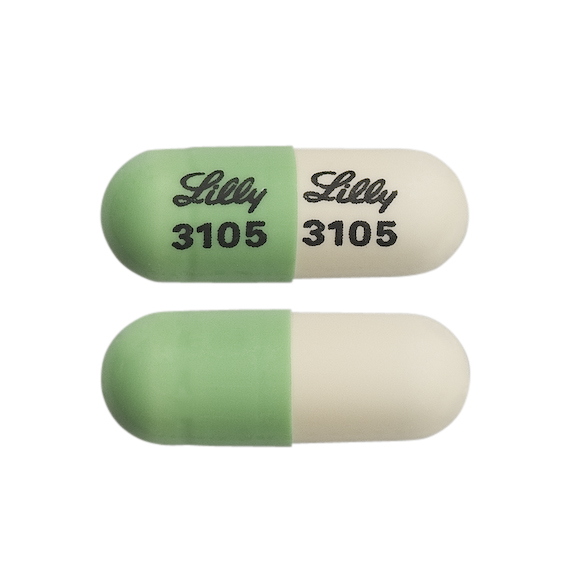
There do not seem to be any lasting harmful effects from taking fluoxetine for many months and years but if you are worried, speak to your doctor.
Other side effects
These are not all the side effects of fluoxetine. For a full list, see the leaflet inside your medicine packet.
Information:
You can report any suspected side effect using the Yellow Card safety scheme.
Visit Yellow Card for further information.
Page last reviewed: 10 February 2022
Next review due: 10 February 2025
Prodep. Capsule Drug Handbook. Tomsk
//= $single_post["name_eng"] ?> //= $single_post["name_eng"] ?>
Packaging
CapsulePharmacological action
Antidepressant, propylamine derivative. The mechanism of action is associated with selective blockade of neuronal reuptake of serotonin in the CNS. Fluoxetine is a weak antagonist of cholino-, adreno- and histamine receptors. Unlike most antidepressants, fluoxetine does not appear to cause a decrease in the functional activity of postsynaptic β-adrenergic receptors. Helps improve mood, reduces feelings of fear and tension, eliminates dysphoria. Does not cause sedation. When taken in average therapeutic doses, it practically does not affect the functions of the cardiovascular and other systems.
Fluoxetine is a weak antagonist of cholino-, adreno- and histamine receptors. Unlike most antidepressants, fluoxetine does not appear to cause a decrease in the functional activity of postsynaptic β-adrenergic receptors. Helps improve mood, reduces feelings of fear and tension, eliminates dysphoria. Does not cause sedation. When taken in average therapeutic doses, it practically does not affect the functions of the cardiovascular and other systems. Indications for use
Depression of various etiologies, bulimia.Presentation
Capsules 20 mg; blister 10 cardboard pack 6;Pharmacodynamics
Selectively inhibits the reuptake of serotonin, which leads to an increase in its concentration in the synaptic cleft, an increase and prolongation of its action on postsynaptic receptors. By increasing serotonergic transmission, it inhibits the metabolism of a neurotransmitter by a negative feedback mechanism. With prolonged use, it lowers the activity of 5-HT1 receptors. It also blocks the reuptake of serotonin in platelets. Weakly affects the reuptake of norepinephrine and dopamine. It does not have a direct effect on serotonin, m-cholinergic, H1-histamine and alpha-adrenergic receptors. Unlike most antidepressants, it does not cause a decrease in the activity of postsynaptic beta-adrenergic receptors. Effective in endogenous depression and obsessive-compulsive disorders. Improves mood, reduces tension, anxiety and fear, eliminates dysphoria. It has an anorexigenic effect, can cause weight loss. In patients with diabetes mellitus, it can cause hypoglycemia, with the abolition of fluoxetine - hyperglycemia. A pronounced clinical effect in depression occurs after 1-4 weeks of treatment, in obsessive-compulsive disorders - after 5 weeks or more.
It also blocks the reuptake of serotonin in platelets. Weakly affects the reuptake of norepinephrine and dopamine. It does not have a direct effect on serotonin, m-cholinergic, H1-histamine and alpha-adrenergic receptors. Unlike most antidepressants, it does not cause a decrease in the activity of postsynaptic beta-adrenergic receptors. Effective in endogenous depression and obsessive-compulsive disorders. Improves mood, reduces tension, anxiety and fear, eliminates dysphoria. It has an anorexigenic effect, can cause weight loss. In patients with diabetes mellitus, it can cause hypoglycemia, with the abolition of fluoxetine - hyperglycemia. A pronounced clinical effect in depression occurs after 1-4 weeks of treatment, in obsessive-compulsive disorders - after 5 weeks or more. Pharmacokinetics
Absorbed from the gastrointestinal tract. Weakly metabolized during the "first pass" through the liver. Eating does not affect the degree of absorption, although it may slow down its rate. Cmax in plasma is achieved after 6-8 hours. Css in plasma is achieved only after continuous administration for several weeks. Protein binding 94.5%. Easily penetrates through the BBB. It is metabolized in the liver by demethylation to form the main active metabolite of norfluoxetine. T1 / 2 fluoxetine is 2-3 days, norfluoxetine - 7-9days. Excreted by the kidneys 80% and through the intestines - about 15%.
Cmax in plasma is achieved after 6-8 hours. Css in plasma is achieved only after continuous administration for several weeks. Protein binding 94.5%. Easily penetrates through the BBB. It is metabolized in the liver by demethylation to form the main active metabolite of norfluoxetine. T1 / 2 fluoxetine is 2-3 days, norfluoxetine - 7-9days. Excreted by the kidneys 80% and through the intestines - about 15%. Use during pregnancy
Contraindicated in pregnancy and lactation.Contraindications for use
Glaucoma, bladder atony, severe renal dysfunction, benign prostatic hyperplasia, simultaneous administration of MAO inhibitors, convulsive syndrome of various origins, epilepsy, pregnancy, lactation, hypersensitivity to fluoxetine.Side effects
From the side of the central nervous system: anxiety, tremor, nervousness, drowsiness, headache, sleep disturbances are possible. From the digestive system: diarrhea, nausea are possible. From the side of metabolism: increased sweating, hypoglycemia, hyponatremia (especially in elderly patients and with hypovolemia) are possible. From the reproductive system: decreased libido. Allergic reactions: possible skin rash, itching. Other: pain in the joints and muscles, shortness of breath, fever.
From the reproductive system: decreased libido. Allergic reactions: possible skin rash, itching. Other: pain in the joints and muscles, shortness of breath, fever. Method of administration and dosage
Initial dose - 20 mg 1 time / day; if necessary, the dose can be increased after 3-4 weeks. Reception frequency - 2-3 The maximum daily oral dose for adults is 80 mgOverdose
Symptoms: nausea, vomiting, agitation, restlessness, hypomania, convulsions, grand mal seizures. Two deaths from acute overdose of fluoxetine (in combination with maprotiline, codeine, temazepam) have been described. Treatment: gastric lavage, activated charcoal, sorbitol, ECG monitoring, symptomatic and supportive therapy, with convulsions - diazepam. There is no specific antidote. Forced diuresis, peritoneal dialysis, hemodialysis, blood transfusion are ineffective.Interaction with other drugs
When used simultaneously with drugs that have a depressant effect on the central nervous system, with ethanol, a significant increase in the inhibitory effect on the central nervous system, as well as an increase in the likelihood of convulsions, is possible. With simultaneous use with MAO inhibitors, furazolidone, procarbazine, tryptophan, serotonin syndrome may develop (confusion, hypomania, restlessness, agitation, convulsions, dysarthria, hypertensive crisis, chills, tremor, nausea, vomiting, diarrhea). With simultaneous use, fluoxetine inhibits the metabolism of tricyclic and tetracyclic antidepressants, trazodone, carbamazepine, diazepam, metoprolol, terfenadine, phenytoin, which leads to an increase in their concentration in blood serum, an increase in their therapeutic and side effects. With simultaneous use, it is possible to inhibit the biotransformation of drugs metabolized with the participation of the CYP2D6 isoenzyme. With simultaneous use with hypoglycemic agents, their action may be enhanced. There are reports of an increase in the effects of warfarin when it is used simultaneously with fluoxetine. With simultaneous use with haloperidol, fluphenazine, maprotiline, metoclopramide, perphenazine, periciazine, pimozide, risperidone, sulpiride, trifluoperazine, cases of extrapyramidal symptoms and dystonia have been described; with dextromethorphan - a case of the development of hallucinations is described; with digoxin - a case of increasing the concentration of digoxin in the blood plasma.
With simultaneous use with MAO inhibitors, furazolidone, procarbazine, tryptophan, serotonin syndrome may develop (confusion, hypomania, restlessness, agitation, convulsions, dysarthria, hypertensive crisis, chills, tremor, nausea, vomiting, diarrhea). With simultaneous use, fluoxetine inhibits the metabolism of tricyclic and tetracyclic antidepressants, trazodone, carbamazepine, diazepam, metoprolol, terfenadine, phenytoin, which leads to an increase in their concentration in blood serum, an increase in their therapeutic and side effects. With simultaneous use, it is possible to inhibit the biotransformation of drugs metabolized with the participation of the CYP2D6 isoenzyme. With simultaneous use with hypoglycemic agents, their action may be enhanced. There are reports of an increase in the effects of warfarin when it is used simultaneously with fluoxetine. With simultaneous use with haloperidol, fluphenazine, maprotiline, metoclopramide, perphenazine, periciazine, pimozide, risperidone, sulpiride, trifluoperazine, cases of extrapyramidal symptoms and dystonia have been described; with dextromethorphan - a case of the development of hallucinations is described; with digoxin - a case of increasing the concentration of digoxin in the blood plasma. With simultaneous use with lithium salts, an increase or decrease in the concentration of lithium in the blood plasma is possible. With simultaneous use, it is possible to increase the concentration of imipramine or desipramine in the blood plasma by 2-10 times (may persist for 3 weeks after the abolition of fluoxetine). With simultaneous use with propofol, a case is described in which spontaneous movements were observed; with phenylpropanolamine - a case is described in which dizziness, weight loss, hyperactivity were observed. With simultaneous use, it is possible to enhance the effects of flecainide, mexiletine, propafenone, thioridazine, zuclopenthixol.
With simultaneous use with lithium salts, an increase or decrease in the concentration of lithium in the blood plasma is possible. With simultaneous use, it is possible to increase the concentration of imipramine or desipramine in the blood plasma by 2-10 times (may persist for 3 weeks after the abolition of fluoxetine). With simultaneous use with propofol, a case is described in which spontaneous movements were observed; with phenylpropanolamine - a case is described in which dizziness, weight loss, hyperactivity were observed. With simultaneous use, it is possible to enhance the effects of flecainide, mexiletine, propafenone, thioridazine, zuclopenthixol. Precautions
Use with caution in the elderly, with cardiovascular disease, insufficiency of liver and / or kidney function. Careful monitoring of patients with suicidal tendencies is required, especially at the beginning of treatment. The highest risk of suicide is in patients who have previously taken other antidepressants and in patients who experience excessive fatigue, hypersomnia, or restlessness during treatment with fluoxetine. When treating patients with low body weight, the anorexigenic properties of fluoxetine should be taken into account. When conducting electroconvulsive therapy while taking fluoxetine, prolonged epileptic seizures are possible. The interval between the withdrawal of MAO inhibitors and the start of taking fluoxetine should be more than 2 weeks, and between the withdrawal of fluoxetine and taking MAO inhibitors - at least 5 weeks. Use with caution for drivers of vehicles and people whose activities require increased concentration of attention and speed of psychomotor reactions. Alcohol should be avoided during treatment.
When treating patients with low body weight, the anorexigenic properties of fluoxetine should be taken into account. When conducting electroconvulsive therapy while taking fluoxetine, prolonged epileptic seizures are possible. The interval between the withdrawal of MAO inhibitors and the start of taking fluoxetine should be more than 2 weeks, and between the withdrawal of fluoxetine and taking MAO inhibitors - at least 5 weeks. Use with caution for drivers of vehicles and people whose activities require increased concentration of attention and speed of psychomotor reactions. Alcohol should be avoided during treatment. Special instructions for taking
Use with extreme caution in patients with impaired liver and kidney function, with a history of epileptic seizures, cardiovascular diseases. In patients with diabetes mellitus, a change in blood glucose levels is possible, which requires correction of the dosing regimen of hypoglycemic drugs. When used in debilitated patients while taking fluoxetine, the likelihood of developing epileptic seizures increases. With the simultaneous use of fluoxetine and electroconvulsive therapy, prolonged epileptic seizures may develop. Fluoxetine can be used no earlier than 14 days after the abolition of MAO inhibitors. The period after the abolition of fluoxetine before the start of therapy with MAO inhibitors should be at least 5 weeks. Elderly patients require correction of the dosing regimen. The safety of fluoxetine in children has not been established. Avoid drinking alcohol during treatment. Influence on the ability to drive vehicles and control mechanisms During the period of treatment, one should refrain from potentially hazardous activities that require increased attention and rapid psychomotor reactions.
With the simultaneous use of fluoxetine and electroconvulsive therapy, prolonged epileptic seizures may develop. Fluoxetine can be used no earlier than 14 days after the abolition of MAO inhibitors. The period after the abolition of fluoxetine before the start of therapy with MAO inhibitors should be at least 5 weeks. Elderly patients require correction of the dosing regimen. The safety of fluoxetine in children has not been established. Avoid drinking alcohol during treatment. Influence on the ability to drive vehicles and control mechanisms During the period of treatment, one should refrain from potentially hazardous activities that require increased attention and rapid psychomotor reactions. Storage conditions
List B.: In a dry, dark place, at a temperature not exceeding 30 °C.Shelf life
48 months.Treatment of asthenia. Can you suggest something new? | Drobizhev M.Yu., Fedotova A.V., Kikta S.V.
Asthenia cannot be called a syndrome, which attracts close attention of scientists both in our country and abroad. Suffice it to point out that since 2000, the PubMed database of the US National Library of Medicine [1] contains summaries of only 124 articles in which this term is used in the title. A similar indicator in the domestic database eLIBRARY.ru [2] is also small - only 137 publications in various journals. In other words, only 7–8 articles per year are devoted to asthenia. Moreover, abroad, this syndrome, as a rule, is not even considered as an independent target for drug therapy. For example, on the American portal rxlist.com [3], which contains a list of diagnoses that are indications for prescribing drugs, there is not even a mention of asthenia or synonyms for this syndrome.
Suffice it to point out that since 2000, the PubMed database of the US National Library of Medicine [1] contains summaries of only 124 articles in which this term is used in the title. A similar indicator in the domestic database eLIBRARY.ru [2] is also small - only 137 publications in various journals. In other words, only 7–8 articles per year are devoted to asthenia. Moreover, abroad, this syndrome, as a rule, is not even considered as an independent target for drug therapy. For example, on the American portal rxlist.com [3], which contains a list of diagnoses that are indications for prescribing drugs, there is not even a mention of asthenia or synonyms for this syndrome.
A completely different situation with the treatment of asthenia has developed in our country. This syndrome is mentioned as an independent indication for the prescription of various substances and, according to the portal of the Register of Medicines of Russia [4], has many identical designations:
1. Asthenic disorders.
Asthenic disorders.
2. Asthenic conditions.
3. Asthenic phenomena.
4. Asthenic syndrome.
5. Asthenic disorder.
6. Asthenic condition.
7. Asthenic phenomenon.
8. Asthenia.
9. Astheno-adynamic subdepressive states.
10. Asthenovegetative symptoms.
11. Astheno-vegetative symptoms.
12. Astheno-vegetative disorder.
13. Asthenodepressive disorder.
14. Astheno-depressive disorder.
15. Astheno-depressive state.
16. Astheno-depressive state.
17. Asthenoneurotic disorder.
18. Astheno-neurotic condition.
19. Quick fatigue.
20. Influenza of young workaholics.
21. Yuppie flu.
22. Diabetic asthenia.
23. Exhaustion of the nervous system.
24. Physical exhaustion.
25. Malaise.
26. Nervous exhaustion with depression.
27. General mental fatigue.
28. General physical fatigue.
29. General malaise.
30. Pathological fatigue.
31. Increased fatigue.
32. Increased fatigue.
33. Mental fatigue.
34. Mental exhaustion.
35. Mental fatigue.
36. Asthenovegetative syndrome.
37. Chronic fatigue syndrome.
38. Decrease in overall activity.
39. The state of increased fatigue.
40. Conditions of increased fatigue.
41. Mental fatigue.
42. Loss of strength.
43. Fatigue.
44. Fatigue.
45. Fatigue.
46. Physical fatigue.
47. Physical and mental overwork.
48. Physical overwork.
49. Functional asthenic conditions.
50. Chronic fatigue.
51. Chronic asthenic conditions.
82 active ingredients are recommended for the treatment of asthenia, contained in 742 preparations, of which 179 have trade names [4]. In particular, among them there are quite a lot of biologically active additives (BAA) to food, which are concentrates of natural natural food and biologically active substances isolated from animal, vegetable raw materials or obtained by chemical synthesis. They also recommend macro- and microelements - minerals that ensure the constancy of the internal environment of the body, acid-base balance, water-salt metabolism. Among the substances under consideration there are also vitamins, which are indispensable elements necessary for the growth, development and life of a person.
They also recommend macro- and microelements - minerals that ensure the constancy of the internal environment of the body, acid-base balance, water-salt metabolism. Among the substances under consideration there are also vitamins, which are indispensable elements necessary for the growth, development and life of a person.
An important component of the recommendations is general tonic agents, mainly of plant origin, which have an insignificant non-specific effect on the central nervous system, possibly due to increased appetite, increased tone of the hollow organs, secretion of the gastrointestinal glands, and a slight increase in blood pressure [4]. In addition, antihypoxants are considered to be indicated for asthenia, which improve the utilization of oxygen by the body and reduce the need for it, and antioxidants that restore free radicals to a stable molecular form (not able to participate in the autoxidation chain).
It is obvious that such obvious differences in ideas about the treatment of asthenia in our country and abroad [3, 4] may be due to significant differences in views on the etiology, pathogenesis and diagnosis of asthenia. Indeed, in our country, this syndrome (at least in some reference books) is classified [4] within the class XVIII ICD-10 [5]): symptoms, signs and abnormalities identified during studies, not classified in other headings (headings R00 -R99). Meanwhile, this class of ICD-10 includes conditions that can be defined as "unspecified", "not otherwise specified", "transient". And these diagnoses are used only when, for some reason, it is impossible to make a more accurate clinical conclusion.
Indeed, in our country, this syndrome (at least in some reference books) is classified [4] within the class XVIII ICD-10 [5]): symptoms, signs and abnormalities identified during studies, not classified in other headings (headings R00 -R99). Meanwhile, this class of ICD-10 includes conditions that can be defined as "unspecified", "not otherwise specified", "transient". And these diagnoses are used only when, for some reason, it is impossible to make a more accurate clinical conclusion.
As a result, there is nothing surprising in the fact that in our country there are a large number of synonyms for asthenia, as well as views on the causes of its occurrence (nutrient deficiency, decreased blood pressure or tone of hollow internal organs, impaired secretion of the gastrointestinal glands, oxygen starvation of body tissues, excess free radicals, etc.) [4]. At the same time, there are recommendations for the treatment of the syndrome in question with the help of numerous dietary supplements, macro- and microelements, vitamins, general tonics, antihypoxants, antioxidants, clearly based on the notion that it occurs for many reasons [4].
Meanwhile, abroad, asthenia is diagnosed mainly within class V of the ICD-10 [5]: mental and behavioral disorders. In this case, 2 headings F06.6 (organic emotionally labile (asthenic) disorder) and F48.0 (neurasthenia) are used. In the first case, asthenia occurs due to damage to brain neurons by certain diseases (trauma, vascular atherosclerosis, epilepsy, viral or bacterial neuroinfections, a tumor). In the second case, the nature of neuronal damage remains unknown. Accordingly, in the first case, for the treatment of asthenia, it is necessary to treat the underlying disease that contributed to the damage to brain neurons, and any anti-asthenic drug therapy is simply not required [3]. In the second case, drug therapy for asthenia is difficult due to the lack of ideas about which neurons are affected and how this happens [3]. But in both cases, asthenia is difficult (if not impossible) to consider as an independent target for therapy.
Obviously, practitioners in our country can independently decide which of the two approaches to the diagnosis and treatment of asthenia they should follow. However, the first of them, which uses non-specific rubrics R00-R99 and is very vulnerable from scientific and clinical points of view, looks much more attractive in the eyes of a practitioner. Indeed, in this case, he can use many active substances both sequentially and simultaneously. In addition, many of them are available in the form of drugs that are dispensed without a prescription, or even simply included in dietary supplements.
However, the first of them, which uses non-specific rubrics R00-R99 and is very vulnerable from scientific and clinical points of view, looks much more attractive in the eyes of a practitioner. Indeed, in this case, he can use many active substances both sequentially and simultaneously. In addition, many of them are available in the form of drugs that are dispensed without a prescription, or even simply included in dietary supplements.
Another thing is the second approach. It is obvious that for the treatment of an organic emotionally labile (asthenic) disorder, a strictly limited range of medications can be used, intended for the treatment of certain brain diseases. As for neurasthenia, the possibilities of using drugs seem even more doubtful. As a result, the practitioner is forced to take a passive position, which is unlikely to please a specialist aimed at providing immediate assistance to the patient.
It seems, however, that this situation can be changed, at least in relation to neurasthenia, by putting forward several assumptions regarding its pathogenesis and the possibility of drug treatment. To do this, it is necessary to take into account that, according to ICD-10 [5], the distinguishing features of this diagnosis clearly “intersect” with the criteria for a depressive or anxiety disorder. It remains to be recalled that the manifestations of depression include (along with depressed mood) a loss of interest and pleasure, a decrease in energy, which can lead to increased fatigue (even with little effort), decreased activity, impaired concentration, and impaired attention. As for neurasthenia, it is characterized by anhedonia (loss of feelings of joy, pleasure) and a slight degree of depression. In addition, the main symptoms of this disorder are complaints of increased fatigue after mental work (unpleasant interference with distracting associations or memories, inability to concentrate and unproductive thinking), decreased professional productivity or efficiency in daily activities, or physical weakness and exhaustion after minimal effort.
To do this, it is necessary to take into account that, according to ICD-10 [5], the distinguishing features of this diagnosis clearly “intersect” with the criteria for a depressive or anxiety disorder. It remains to be recalled that the manifestations of depression include (along with depressed mood) a loss of interest and pleasure, a decrease in energy, which can lead to increased fatigue (even with little effort), decreased activity, impaired concentration, and impaired attention. As for neurasthenia, it is characterized by anhedonia (loss of feelings of joy, pleasure) and a slight degree of depression. In addition, the main symptoms of this disorder are complaints of increased fatigue after mental work (unpleasant interference with distracting associations or memories, inability to concentrate and unproductive thinking), decreased professional productivity or efficiency in daily activities, or physical weakness and exhaustion after minimal effort.
Anxiety (along with fear, the severity of which varies from mild discomfort to horror) is characterized by complaints of motor and autonomic symptoms: a feeling of nervousness, trembling, muscle tension, sweating, palpitations, dizziness and discomfort in the epigastric region. Similar clinical signs are observed in neurasthenia. Characterized by moderate anxiety with concern about mental and physical distress, irritability. Muscle pain, inability to relax, dizziness, tension headaches, and symptoms of dyspepsia are also common.
Similar clinical signs are observed in neurasthenia. Characterized by moderate anxiety with concern about mental and physical distress, irritability. Muscle pain, inability to relax, dizziness, tension headaches, and symptoms of dyspepsia are also common.
It is fundamentally important that, in contrast to neurasthenia, there are fairly detailed ideas about what happens to the work of neurons during depression and anxiety in different areas of the brain [6–8]. Thus, the symptoms of depression are associated with a decrease in the activity of primarily dopamine (DA), serotonin (SE), norepinephrine (NA) nerve cells (Table 1). Anxiety reduces the activity (Table 2) of the main inhibitory neurons, the neurotransmitter of which is gamma-aminobutyric acid (GABA) [6–8]. This leads to the disinhibition of the already mentioned dopamine, serotonin, norepinephrine, as well as acetylcholine (ACC) and glutamate (GLU) nerve cells.
The presented data suggest what happens to the activity of neurons in neurasthenia by analogy with the disorders listed above (Table 3). At the same time, it becomes clear that neurasthenia (unlike depression and anxiety) is indeed a much more complex and heterogeneous mental disorder. Its symptoms may be based on changes in the activity of a large number of neuronal systems. Moreover, it is quite possible that neurons belonging to the same system in different areas of the brain change their vital activity in different ways.
At the same time, it becomes clear that neurasthenia (unlike depression and anxiety) is indeed a much more complex and heterogeneous mental disorder. Its symptoms may be based on changes in the activity of a large number of neuronal systems. Moreover, it is quite possible that neurons belonging to the same system in different areas of the brain change their vital activity in different ways.
To treat this condition, it is really difficult to choose the necessary psychotropic drug, based on its mechanism of action. For example, most modern antidepressants that are used in the treatment of depression can only increase the activity of various neurons (Table 4). As for the tranquilizers used to treat anxiety, they tend to activate inhibitory GABA neurons and suppress the activity of other nerve cells (Table 5). Thus, both antidepressants and tranquilizers, due to their mechanism of action, are not very suitable for the treatment of neurasthenia, if we take into account the assumptions about the change in neuronal activity (Tables 3–5).
Fortunately, there are exceptions. This is, for example, the antidepressant milnacipran, which at doses of 25–75 mg/day mainly increases the activity of norepinephrine neurons, and at a dose of 100 mg/day its action becomes more balanced in relation to serotonin and norepinephrine [8]. The norepinephrine activity of milnacipran is the highest among SNRIs [9]. In addition to an increase in the level of serotonin and norepinephrine in the hippocampus, a significant increase in the level of serotonin, norepinephrine, and dopamine in the prefrontal cortex was noted, which is associated with an increase in physical and mental activity [10, 11]. The proposed clinical effects were confirmed in a double-blind comparison study with paroxetine in patients with depression who had more than 3 points on the HDRS scale section 8, which is characterized by slowing of thought, speech, concentration and decreased motor activity. Milnacipran outperformed paroxetine by almost 2 times in terms of the number of patients responding to therapy (p<0.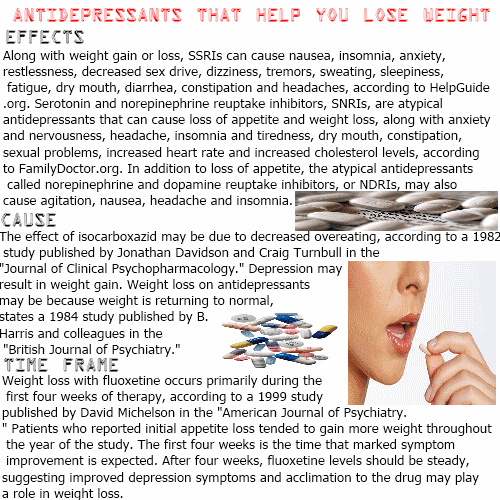 05) [10].
05) [10].
These properties of an antidepressant may well be in demand in the treatment of those clinical variants of neurasthenia, whose clinical picture is similar to that of depression (Table 1), especially if the structure of neurasthenia is dominated by symptoms that milnacipran, due to its mechanism of action, can “fend off” (Table 1). 6).
There are several tranquilizers whose mechanism of action is clearly better suited for the treatment of symptoms of neurasthenia, the clinical manifestations of which are close to those of anxiety. These include adamantylbromophenylamine, aminophenylbutyric acid, baclofen (Table 5). Unlike other tranquilizers, they not only activate the inhibitory GABAergic system and, therefore, suppress the activity of norepinephrine, serotonin, acetylcholine, and glutamate neurons, but are also able to increase the activity of dopamine neurons (Table 5). The latter property is associated with rather complex mechanisms (direct action on dopamine neurons by adamantylbromphenylamine [12] and differences in the sensitivity of GABAB receptors on different cells [13–15]), which even required the introduction of a new term, the so-called selective (mild, moderate) inhibition. .
.
However, it should be borne in mind that aminophenylbutyric acid and baclofen have a more effective mechanism of action in relation to the GABAergic system in comparison with adamantylbromophenylamine [12, 13]. The latter affects this system indirectly. This drug reduces the expression of a gene that controls protein synthesis, which in turn reuptakes GABA. At the same time, the amount of this neurotransmitter increases. And it already acts on GABAA receptors, as a result of which the main pharmacological effects of the drug in question develop. As for baclofen and aminophenylbutyric acid, these drugs can directly affect the GABAergic system by acting on GABA receptors. However, this property is clearly more pronounced in baclofen and is associated with a pronounced muscle relaxant effect, which makes it difficult to use it in neurasthenia [14]. Accordingly, aminophenylbutyric acid (Anvifen) (orally after meals in 2-3-week courses, adults and children from 14 years of age, 250-500 mg 3 times a day, the maximum daily dose is 2500 mg) [16] may well be used for neurasthenia , if its structure is dominated by symptoms close to those of anxiety (Table 7).