The pill mood swings
Does Birth Control Make You Moody?
Written by Hope Cristol
Medically Reviewed by Traci C. Johnson, MD on May 06, 2021
In this Article
- How Hormonal Contraceptives Work
- Is There a Link Between Birth Control and Emotions?
- Benefits
- Possible Explanations
- When to See a Doctor
Lots of women get irritable, depressed, or feel out of sorts just before their monthly periods. Those can be symptoms of a common condition called premenstrual syndrome (PMS).
But could your birth control pills and other hormonal contraceptives trigger similar emotional swings? Or might they do the reverse and actually improve your moods?
How Hormonal Contraceptives Work
Most birth control pills, patches, and rings combine two lab-made female sex hormones, estrogen and progestin. “Minipills” have only progestin, and in a smaller amount.
Combined hormonal contraceptives stop the normal rise and fall of your body’s natural hormones. That blocks your body from ovulating and releasing an egg to be fertilized by sperm.
Is There a Link Between Birth Control and Emotions?
Women have complained about mood-related changes like depression and anxiety ever since the pill came out in 1960. The newest generation of pills have lower doses of hormones. Even so, a sizeable number of women still quit the pill because of side effects.
During a typical 28-day menstrual cycle, estrogen levels reach their peak around day 14. That’s when many women feel best emotionally and physically. Most hormonal contraceptives smooth this mountain-shaped hormonal cycle into an even line for the first 21 days. Then the levels of estrogen and progestin plunge during the final 7 days.
Limited research suggests that compared with women who don’t use hormonal birth control, those who do are more likely report feeling depressed, anxious, and angry. But those symptoms don’t make the list of common side effects. Other studies have turned up no significant link between hormone combinations or concentrations and differences in mood. Still more research has found that women on the pill and those taking dummy pills report similar symptoms, suggesting that any effects they noticed were unrelated to the actual pills.
Still more research has found that women on the pill and those taking dummy pills report similar symptoms, suggesting that any effects they noticed were unrelated to the actual pills.
Benefits
Doctors sometimes prescribe hormonal contraceptives to ease the discomfort that practically every woman notices at one time or another during their monthly periods.
Symptoms of premenstrual syndrome can include:
- Angry outbursts
- Crying spells
- Confusion
- Feeling down or depressed
- Trouble sleeping
- Irritability
- Tender breasts
- Aches and pains
- Bloating or weight gain
- Headache
The FDA has approved a specific type of hormonal birth control pill -- containing drospirenone and ethinyl estradiol -- to treat a more serious form of PMS called premenstrual dysphoric disorder. But the hormones may work better to ease physical symptoms than mood-related ones. It also can take some trial and error for your doctors to hit on the right medication and dosage.
Possible Explanations
If scientists can’t firmly connect the dots between birth control hormones and emotional turbulence, why do some women believe there’s a link?
- Greater sensitivity to changes to levels of estrogen and other hormones
- Stress from the need to avoid pregnancy and to take the pill as prescribed
- Heightened perception of possible symptoms among women with existing depression, anxiety, or other mental health conditions
When to See a Doctor
If your mood swings are mild or moderate, exercise, healthier eating, relaxation, and other lifestyle changes may bring you relief. See your doctor if you feel depressed, feel no energy, or have other severe symptoms that interfere with your daily life.
Feel like a different person on the pill? Here’s how it affects your mood |
Science Mar 26, 2020 / Sarah E. Hill PhD
Dingding Hu
If you think your contraception is making you anxious or depressed, you’re not imagining things.
 Evolutionary psychologist Sarah E. Hill explains what happens to your brain on birth control.
Evolutionary psychologist Sarah E. Hill explains what happens to your brain on birth control.Most women know at least one or two other women who have had a bad reaction to the pill. In fact, the question that many of us have about the pill: “Why does the pill make me crazy?”
Before I get into what the research says about all this, let me just address the elephant in the room — the whole thing about women’s sex hormones influencing mood. Which they do. This might be the world’s oldest cliché about women, but that doesn’t make it any less true. Women’s sex hormones influence women’s moods. Men’s sex hormones affect men’s moods. It would be impossible for them not to.
Back to the question. To start with, all of us feel a little crazy sometimes. Life is hard and can make anyone feel anxious and overwhelmed at times. For some women, being on the pill can magnify these feelings, leading to anxiety disorders and depression. But if these things happen to you, it doesn’t mean you’re crazy; it just means you’re on the wrong pill.
Mood-related issues like anxiety and depression are super-common among women on the pill. Almost half of all women who go on the pill stop using it within the first year because of intolerable side effects, and the one most frequently cited is unpleasant changes in mood. Sometimes it’s intolerable anxiety; other times, it’s intolerable depression; or maybe both simultaneously. And even though some women’s doctors may tell them that those mood changes aren’t real or important, a growing body of research suggests otherwise.
The Scandinavian nation of Denmark is home to a number of nationwide registers, collections of data from its citizens on different health and social issues. Because all Danish citizens have a unique personal identification number, researchers have been able to link individual people’s data across different registers, giving them access to tons of information about patterns of health and social behavior in a whole population.
From these registers, we’ve learned valuable lessons about the powerful effects that the birth control pill can have on mood. In the first of these studies, the researchers looked at the records of all the healthy, nondepressed women living in Denmark between the ages of 15 and 34. They then followed the prescription and mental health records of these women (more than a million of them) for 14 years to see whether going on hormonal contraceptives influenced the likelihood of later being diagnosed with depression or being prescribed antidepressants.
In the first of these studies, the researchers looked at the records of all the healthy, nondepressed women living in Denmark between the ages of 15 and 34. They then followed the prescription and mental health records of these women (more than a million of them) for 14 years to see whether going on hormonal contraceptives influenced the likelihood of later being diagnosed with depression or being prescribed antidepressants.
The researchers found that women on hormonal contraceptives were 50 percent more likely to be diagnosed with depression six months later, compared with women who were not prescribed hormonal contraceptives during this time. They also found the women on hormonal contraceptives were 40 percent more likely to be prescribed an antidepressant than were women who weren’t prescribed hormonal contraceptives during this time. The results of this study, as well as others, suggest the pill can increase some women’s risk of depression. This seemed particularly true for non-oral products (such as a patch, vaginal ring or hormonal IUD) and for young women (ages 15 to 19), whose brains are not yet done developing and may be more prone to the influence of hormonal signaling.
As a scientist, I’m obliged to point out we don’t know for sure that the pills caused this increase. Correlation doesn’t equal causation. It’s possible the researchers found pill taking and depression to be related because they were each related to some other third variable. For instance, women who seek medical interventions to prevent pregnancy might be more likely to seek medical interventions for depression. Or, getting into a new sexual relationship (which can prompt a pill prescription) could be what’s increasing women’s depression risk.
However, the researchers statistically tested for the influence of a number of third variables, and each of these tests found that hormonal contraceptives predicted depression risk even after statistically controlling for these third variables. Even though this wasn’t a double-blind, placebo-controlled experiment, the researchers took great care with their study design and data analysis and the results were published in the New England Journal of Medicine, the top medical journal in the US.
More recently, the same team looked at whether hormonal contraceptives might increase women’s risk of suicide. Researchers tracked hormonal contraceptive usage and suicide attempts and deaths in all Danish women who’d turned 15 between 1996 and 2013. (As in their prior study, they did not include any women who had previously diagnosed psychological problems or who had used antidepressants. They also didn’t include women already on hormonal contraceptives when they entered the study.) They followed the women for an average of eight years and then compared the likelihood of having attempted or successfully committed suicide among the women who were prescribed hormonal contraceptives and those who were not.
The women on hormonal contraceptives were twice as likely to have attempted suicide during this time than the women not on hormonal contraceptives. But the risk of successful suicide attempts was actually higher: It was triple that of women not on hormonal contraceptives. As with depression risk, the biggest negative impact of hormonal contraceptives on suicide risk was found for young women (ages 15 to 19) on non-oral products.
As with depression risk, the biggest negative impact of hormonal contraceptives on suicide risk was found for young women (ages 15 to 19) on non-oral products.
When it comes to why the pill can mess with your mood, the two systems that shoulder most of the blame are the HPA axis and some of our neurotransmitter systems. First, the HPA axis (or hypothalamic-pituitary-adrenal axis). It’s made up of three systems working together — the hypothalamus, the pituitary gland, the adrenal glands — and plays a central role in the body’s stress response. The type of blunting of the HPA axis we tend to see in pill-taking women is a known contributor to mental health problems, including the types of mood disturbances characteristic of PTSD. Because lacking the biological tools necessary to deal with stress literally harms your ability to cope, having a broken stress response might be a key player in the development of anxiety and depression. It could also harm emotional well-being in indirect ways through its negative impact on our ability to absorb emotionally meaningful events from our environments.
The second piece is the role that neurotransmitter systems play in making women feel lousy on the pill. Before I explain, I need you to know three quick things.
Quick Thing 1: Neurotransmitters are chemicals that the brain uses to communicate with itself and the rest of the body.
Quick Thing 2: Excitatory neurotransmitters tell your brain cells to get ready for action, making them more likely to fire off messages to other brain cells.
Quick Thing 3: Inhibitory neurotransmitters tell your brain cells to slow their roll, making them less likely to fire off messages to other cells in the brain.
The most prevalent and frequently used inhibitory neurotransmitter in the brain is GABA. It’s often on the scene in a big way when your brain is trying to slow itself down. GABA gets released when you’re relaxing in your PJ pants, and it’s also released when doing things like meditation and yoga.
Interestingly, you can get a relaxed GABA-rific experience from other things that stimulate GABA receptors, such as alcohol and benzodiazepines like Xanax. And our bodies actually produce compounds that work much like alcohol and Xanax. One of the most powerful is allopregnanolone, a neurosteroid. It gets synthesized when progesterone is broken down in the body and has the effect of kick-starting action by your GABA receptors.
And our bodies actually produce compounds that work much like alcohol and Xanax. One of the most powerful is allopregnanolone, a neurosteroid. It gets synthesized when progesterone is broken down in the body and has the effect of kick-starting action by your GABA receptors.
Unfortunately for women on the pill, the artificial progestins in the pill don’t seem to offer this same benefit. In fact, research suggests that women on the pill may have lower levels of these natural sedatives relative to what’s observed in its absence, regardless of the point in the cycle.
This can mean bad news for women’s mental health. When GABA receptors aren’t properly stimulated, it’s known to make people feel anxious, overwhelmed and depressed. A number of mental-health-related issues, including panic disorder, depression, bipolar disorder and the mood-related symptoms of PMS, are characterized by lower-than-average levels of GABAergic activity. Lack of such activity can also increase a person’s risk of alcohol dependence.
Research suggests that changes in dopamine and serotonin signaling may also play a role in mood-related changes seen on the pill. Dopamine and serotonin, like GABA, are neurotransmitters. These chemicals come on the scene when we’re spending time with people we love, eating hot fudge sundaes, falling in love, having sex and having orgasms.
Not surprisingly, these neurotransmitter systems change what they do in response to women’s cyclically changing sex hormones. In particular, the research finds that estrogen makes rewarding things feel even more rewarding than they do in its absence and that progesterone attenuates these effects. Estrogen makes sex feel sexier, chocolate taste yummier, and getting status boosts feel boost-ier.
Given that the pill keeps estrogen levels low across the cycle and stimulates progesterone receptors, it’s possible the pill might have the effect of dampening reward processing in the brain. And if the world seems unrewarding, this makes us feel depressed. One hallmark symptom of depression is that people no longer find pleasure in things that they used to find pleasure in. So it’s also possible that the pill might increase a person’s risk of depression by making pleasure less pleasurable. Consistent with this idea, research finds that pill-taking women — when compared with their naturally cycling counterparts — have a blunted positive emotional response to happy things and don’t experience activity in the reward centers of their brains when looking at pictures of their romantic partners.
One hallmark symptom of depression is that people no longer find pleasure in things that they used to find pleasure in. So it’s also possible that the pill might increase a person’s risk of depression by making pleasure less pleasurable. Consistent with this idea, research finds that pill-taking women — when compared with their naturally cycling counterparts — have a blunted positive emotional response to happy things and don’t experience activity in the reward centers of their brains when looking at pictures of their romantic partners.
It seems pretty clear from the research that the pill can cause some women some pretty serious problems with their mental health, but the science isn’t yet at a point where we can make strong predictions about exactly what’s going to happen to whom, and on what.
However, according to the research, you might have a greater risk of experiencing negative mood effects on the pill if:
- You have a history of depression or mental illness (although there is also evidence that the pill can stabilize mood in certain women with mental illness).

- You have a personal or family history of mood-related side effects on the birth control pill.
- You are taking progestin-only pills.
- You are using a non-oral product.
- You are taking multi-phasic pills (pills with an increasing dose of hormones across the cycle rather than a constant dose).
- You are 19 or younger.
These bullet points can give you a starting point to initiate a conversation with your doctor about any mental health concerns. They aren’t your fate, though. Even if you’re an 18-year-old with a family history of depression and you’re on the birth control patch, if you aren’t experiencing signs of troubled mental health, the chances are incredibly low that you’re going to suddenly develop mood problems from birth control. This is especially true if you’ve been on it for a while and seem to be tolerating it well.
What’s more, while some women experience negative mood changes on the pill, some women experience the opposite reaction. They feel a whole lot better and mentally healthier on the pill than off it. Research also finds that the pill can offer huge mood-stabilizing benefits to women who have severe PMS.
They feel a whole lot better and mentally healthier on the pill than off it. Research also finds that the pill can offer huge mood-stabilizing benefits to women who have severe PMS.
The most critical thing about the pill’s effects will come from you: How do you feel on it?
Any time you start a new pill, please let someone close to you know about it. Ask them to make note and tell you if they notice any changes in your behavior that might suggest the onset of depression.
Because the hormones in the pill influence what the brain does, it’s almost impossible to separate out what the hormones are doing from who we are. We feel like the version of reality that is created by our brain on the pill is real. This can make it difficult to notice depression creeping in. Rather than feeling like the pill is messing with our mood, it just feels like our life is getting crappier or our job has gotten more stressful. If you tell your person that you are trying a new pill, they may be able to help you recognize problems that start to develop so that you can look for a new pill or an alternative means of protecting yourself from pregnancy.
On top of this, consider keeping a journal. If possible, start it before going on the pill so you have a log of how you were feeling before and after. Having hard evidence of your mood prior to the pill can be a good way for you to think about your past more objectively, making it easier to recognize any changes. In each entry, make note of your mood, energy level and well-being using some sort of scale (1=”I feel sad/anxious” and 10=”I feel great”). This will help you keep tabs on how things change for you (or not) when trying out a new pill.
If you’re already on the pill, it’s not too late to keep track of how you’re feeling. Make a note of your patterns. If you have more happy days than sad ones, that probably means everything’s on the right track. None of us feel happy all the time, but we should feel happier more often than sad when things in our lives are going well. If you have fewer happy days than you think you should, talk to your doctor. It could be time to try a new pill or address an issue with your mental health that you’ve let go too long.
It could be time to try a new pill or address an issue with your mental health that you’ve let go too long.
Excerpted with permission from the new book This Is Your Brain on Birth Control: The Surprising Science of Women, Hormones, and the Law of Unintended Consequences by Sarah E. Hill PhD. Published by Avery, an imprint of Penguin Random House, LLC. © 2019 by Sarah E. Hill.
Watch her TEDxVienna Talk now:
Mood swings
I confirm More
- INVITRO
- Library
- Symptoms
- Mood swings
Menopause
Climax
2075 25-th of August
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Mood is usually called a stable emotional state of a person, which determines his perception of reality.
A stable positive attitude is the basis for health, and frequent mood swings disrupt not only the mental, but also the physiological activity of a person.
Human emotions are diverse, and their occurrence is regulated by several hormones:
- serotonin, or the hormone of pleasure, is responsible for a good mood, increases optimism and revives hope;
- dopamine, or the hormone of motivation and joy, contributes to the feeling of pleasure;
- adrenaline, a stress hormone, causes rage, anger, tension and fear;
- endorphins - hormones of joy and euphoria;
- Phenylethylamine is responsible for falling in love and romantic experiences;
- for confidence in victory - testosterone;
- Oxytocin, the hormone of trust and tenderness, which plays an important role during pregnancy, childbirth and breastfeeding, causes tender attachment to relatives in the human heart.
The production and metabolism of hormones entail a chain of complex sequential reactions that enable a person to make certain decisions. A number of hormones have a serious impact on the functioning of the brain.
A number of hormones have a serious impact on the functioning of the brain.
Any failure in the “hormone-brain” circuit can lead to uncontrolled mood swings and cause unmotivated behavior.
Possible causes
Sudden and unreasonable mood swings can be caused by physiological and pathological factors.
Physiological reasons. If we consider hormonal fluctuations as the causes of mood swings, then a person is exposed to them throughout life: during growth, maturation, in the reproductive and post-reproductive periods. These are physiological cycles of development, and the body independently copes with hormonal changes.
The first period of powerful hormonal adjustment becomes adolescence . At this moment, the production of sex hormones increases sharply, which can cause unjustified aggression in boys, a desire to lead and prove the right to their own opinion. In girls, the production of estrogens, which affect mood swings, occurs cyclically and may be associated with the irregularity of menstruation during puberty. Psychological factors affecting the mood of adolescents are associated with difficulties in adequately perceiving one's body: a changed figure can cause irritation, despondency, and shame. This reaction is typical for girls. A change in testosterone levels in adolescents of both sexes contributes to the development of an unmotivated sense of protest, increased demands on others, emotional overexcitation, and reduced criticism of one's own actions.
Psychological factors affecting the mood of adolescents are associated with difficulties in adequately perceiving one's body: a changed figure can cause irritation, despondency, and shame. This reaction is typical for girls. A change in testosterone levels in adolescents of both sexes contributes to the development of an unmotivated sense of protest, increased demands on others, emotional overexcitation, and reduced criticism of one's own actions.
It is very important during this period not to miss the signs of latent depression, which is difficult to diagnose because of the variety of its forms and symptoms.
When diagnosing depressive conditions, somatic symptoms come to the fore, that is, complaints about a state of health disorder, problems in the gastrointestinal tract, cardiovascular system, as well as a sharp change in mood. Sometimes mood swings get out of control and cause an emotional overreaction.
After a regular menstrual cycle is established, monthly hormonal fluctuations can cause premenstrual syndrome , which is manifested by a deterioration in well-being and a sharp change in mood.
A pronounced premenstrual syndrome negatively affects the daily activity of a woman, causes physical and emotional problems, and reduces the quality of life.
The main manifestations of premenstrual syndrome include fluid retention in the body and swelling due to increased levels of prolactin, mood swings, irritability, tearfulness, and fatigue due to impaired serotonin metabolism. Increased production of prostaglandins leads to headache, swelling and swelling of the mammary glands.
During pregnancy , especially in the first trimester, a woman's mood and health are directly dependent on hormonal balance. During this period, the main complaints are irritability, resentment, and sudden mood swings. After the fourth month of pregnancy, the woman's emotional background stabilizes.
Big troubles are brought by postpartum depression , which can be accompanied not only by a depressed emotional state, but also by suicidal attacks.
If mood swings disturbed a woman in the first trimester of pregnancy, the likelihood of postpartum depression increases significantly.
Menopausal syndrome is another emotional period in a woman's life when mood can be determined by changes in hormonal levels. Vegetovascular manifestations (hot flashes, sweating, blood pressure surges) may be associated with endocrine diseases (metabolic syndrome, thyroid disease) and emotional and mental disorders (mood swings, tearfulness, irritability, fatigue).
In men, age-related hormonal changes can also be accompanied by emotional instability: they become more irritable and aggressive. Mood swings in men tend to be less pronounced.
Pathological causes . A hormonal imbalance that causes sudden mood swings can occur with thyroid diseases , most often with thyrotoxicosis. In this case, an excess of the hormones thyroxine and triiodothyronine (T4 and T3) leads to malfunctions in the body. Diseases that cause increased production of thyroid hormones include diffuse toxic goiter, multinodular toxic goiter, etc. The instability of the emotional background in thyroid pathologies is accompanied by symptoms of cardiovascular diseases (arrhythmias, increased blood pressure), pathologies of the musculoskeletal system (muscle atrophy , osteoporosis), impaired functioning of the nervous system.
Diseases that cause increased production of thyroid hormones include diffuse toxic goiter, multinodular toxic goiter, etc. The instability of the emotional background in thyroid pathologies is accompanied by symptoms of cardiovascular diseases (arrhythmias, increased blood pressure), pathologies of the musculoskeletal system (muscle atrophy , osteoporosis), impaired functioning of the nervous system.
Along with increased excitability and anxiety, patients with hyperthyroidism complain of emotional instability, rapid mood swings, irritability, and tearfulness.
Sleep disorders can be both a cause and a consequence of a sudden change in mood and psychological instability.
Mental disorders are often accompanied by emotional instability. A striking example is bipolar affective disorder .
Bipolar disorder is characterized by a sudden change in mood, from intense arousal to depression.
The causes of this disease are not fully understood, but experts prefer the genetic theory. With age, the mental disorder worsens, the duration of periods of depression increases.
With age, the mental disorder worsens, the duration of periods of depression increases.
Unmotivated mood swings can be observed in persons suffering from psychopathy (most often hysterical), and in people with borderline personality disorder . In these cases, a sharp change in mood is accompanied by other signs of altered behavior (theatricality, a tendency to lie, exaggeration).
Drug dependence on hormones and psychoactive substances taken is another cause of severe mood swings.
With the regular use of alcohol and drugs, the joy and excitement after their use is suddenly replaced by depression or anger.
An unmotivated change in mood can be observed with hormonal therapy for oncological diseases and .
Which doctors to contact
Mood swings due to physiological causes do not require medical attention. If depression persists or is accompanied by other symptoms, you should first consult with the therapist who will determine the plan for the diagnostic search.
If the cause of emotional instability is related to hormonal changes in the female body, consultation is recommended gynecologist-endocrinologist, and if a man experiences these symptoms - urologist-andrologist. If thyroid disease is suspected, visit endocrinologist. If the patient's hormonal background is not disturbed, consultation is necessary neurologist or psychoneurologist.
Diagnosis and examination
Finding the cause of extreme mood swings is quite difficult. With the cyclical repetition of episodes of emotional instability and their coincidence with the onset of menstruation or menopause, the diagnosis can be made on the basis of the results of tests for sex hormones: estradiol, progesterone, luteinizing hormone, follicle-stimulating hormone, anti-Mullerian hormone.
Estradiol (E2, Estradiol)
Synonyms: Blood test for estradiol. 17-beta-estradiol. Brief description of the analyte Estradiol Estradiol is a steroid hormone with maximum estr. ..
..
Up to 1 business day
Available with home visit
715 RUB
Add to cart
Progesterone
Synonyms: Progestin; Gestagen. P4; Pregn-4-ene-3,20-dione. Brief description of the analyte Progesterone Progesterone is produced in the ovaries and in a small...
Up to 1 business day
Available with home visit
705 RUB
Add to cart
Luteinizing Hormone (LH)
Synonyms: Glycoprotein gonadotropic hormone; luteotropin; Lutropin. luteinizing hormone; LH; Lutropin; Interstitial cell stimulating hormone; ICSH. Brief characteristic determined ...
Up to 1 business day
Available with house call
715 RUB
Add to cart
Follicle Stimulating Hormone (FSH)
Synonyms: Blood test for FSH; Follitropin. Follicle-Stimulating Hormone; follitropin; FSH. Brief description of the analyte Follicle-stimulating hormone ...
Up to 1 business day
Available with home visit
715 RUB
Add to cart
Anti-Mullerian Hormone (AMH, Mullerian Inhibiting Substance, MIS)
Synonyms: Blood test for AMH; Mueller inhibitor.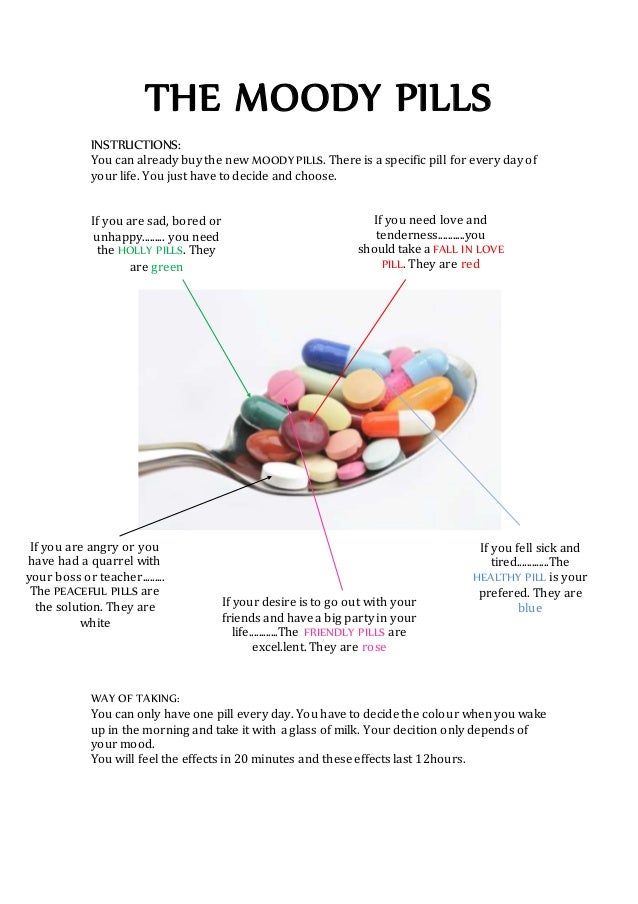 Anti-Müllerian hormone; AMH; Müllerian inhibiting factor; MIF; Müllerian-inhibiting hormone; M.I.H.; Müllerian-inhibiting substance; MIS. Short...
Anti-Müllerian hormone; AMH; Müllerian inhibiting factor; MIF; Müllerian-inhibiting hormone; M.I.H.; Müllerian-inhibiting substance; MIS. Short...
Up to 3 working days
Available with home visit
RUB 1,670
Add to cart
With the appearance of emotional instability, which is accompanied by arrhythmia, trembling fingers, sweating, tests for thyroid hormones (T3, T4, TSH) and antibodies to thyroglobulin (AT-TG) are necessary.
Free Triiodthyronine (Free T3, Free Triiodthyronine, FT3)
Synonyms: Free triiodothyronine. Free T3. Brief description of the test substance Triiodothyronine free Free triiodothyronine (T3free) belongs to the thyroid . ..
..
Up to 1 business day
Available with home visit
RUB 685
Add to cart
Free thyroxine (T4 free, Free Thyroxine, FT4)
Free thyroxine, not bound to plasma transport proteins. Synonyms: Blood test for free thyroxine. Free T4; Free Form of Thyroxin. Short description ...
Up to 1 business day
Available with home visit
665 RUB
Add to cart
Thyroid Stimulating Hormone (TSH)
A pituitary hormone that regulates thyroid function. One of the most important tests in the laboratory diagnosis of thyroid diseases. Synonym...
One of the most important tests in the laboratory diagnosis of thyroid diseases. Synonym...
Up to 1 business day
Available with house call
620 RUB
Add to cart
Thyroglobulin Antibodies (AT-TG, Anti-Thyroglobulin Autoantibodies, Thyroglobulin Antibodies)
Synonyms: Blood test for AT-TG; Antibodies to TG; ATTG; AntiTG; Anti-TG. Tg Autoantibody; TgAb; Anti-Tg Ab; ATG. Brief description of the study "Antibodies to thyroglobulin&raq...
Up to 1 business day
Available with home visit
790 RUB
Add to cart
Diagnosis of mental disorders is complex and is based not so much on laboratory tests as on behavioral characteristics and symptoms of the disease.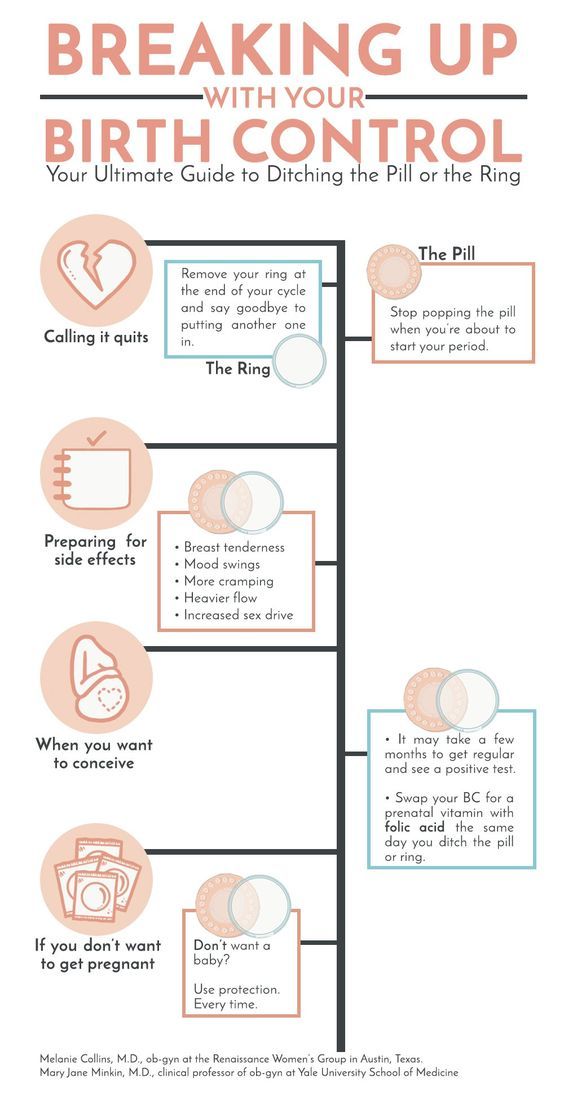 If you suspect the abuse of narcotic and psychotropic substances, you can ask the patient to take a urine test for toxic substances - a set of studies "Bad Habits".
If you suspect the abuse of narcotic and psychotropic substances, you can ask the patient to take a urine test for toxic substances - a set of studies "Bad Habits".
"Bad habits" (Urine test for nicotine, psychotropic and narcotic substances, psychoactive drugs)
Synonyms: Comprehensive urine analysis "Bad habits"; comprehensive urinalysis for nicotine, psychotropic and narcotic substances, psychoactive drugs...
Up to 4 business days
Available with home visit
3 920 RUB
Add to cart
When pregnancy occurs, a study of chorionic gonadotropin, a specific hormone of pregnancy, is recommended; Ultrasound study.
Human chorionic gonadotropin (hCG, beta-hCG, b-hCG, Human Chorionic)
Synonyms: Beta-hCG generic. Human Chorionic Gonadotropin; hCG; Pregnancy Quantitative hCG; Beta hCG; Total beta hCG. Brief description of the analyte Human chorionic gonadotropin ...
Human Chorionic Gonadotropin; hCG; Pregnancy Quantitative hCG; Beta hCG; Total beta hCG. Brief description of the analyte Human chorionic gonadotropin ...
Up to 1 business day
Available with home visit
RUB 685
Add to cart
Ultrasound diagnosis of pregnancy
Examination to confirm pregnancy and determine the place of attachment of the ovum (to exclude ectopic pregnancy).
RUB 2,290 Sign up
Treatment
You can cope with mood swings only after finding out their causes, consulting with specialists and treating the underlying disease.
What to do
Mood swings observed in adolescents require daily attention and patience from relatives. If a feeling of depression, sleep disturbance, tearfulness are combined with somatic ailments (headache, pain in the abdomen, muscles) and a desire to isolate oneself from the outside world, one should definitely consult a child with a psychoneurologist.
To improve your mood, you should lead an active and healthy lifestyle.
You need a proper diet, regular exercise and adequate sleep. Attention to your mood is a simple rule of taking care of your own health.
Sources:
- A.V. Vasilieva, T.B. Morgunova, Yu.P. Thyrotoxicosis after childbirth: difficulties in differential diagnosis. Medical business. 2020;1:97-100. DOI: 10.24411/2071-5315-2020-12200
- Menopausal hormone therapy and maintaining the health of women of mature age. Clinical guidelines (Protocols). Ministry of Health of the Russian Federation.
 2014.
2014. - Clinical guidelines "Depressive episode, recurrent depressive disorder". Developed by: Russian Society of Psychiatrists. – 2021.
- Tokareva D.V., Dikareva E.S., Zakirova I.I. Psychiatric disorders developing against the background of neurosurgical diseases. Bulletin of Medical Internet Conferences (ISSN 2224-6150). 2019;9(5).
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Gastrointestinal bleeding
617 29 September
-
Intestinal colic
4639 28 September
-
Exanthema
4909 12-th of September
Show more
Menopause
Climax
Diabetes mellitus
Thyrotoxicosis
"Widow's hump" or "withers"
"Widow's hump": causes, in what diseases it occurs, diagnosis and methods of treatment.
More
Menopause
Acne (acne)
Thyrotoxicosis
Climax
Pregnancy
PCOS
Delayed menstruation
Delayed menstruation is a problem that every woman has faced at least once in her life. The main thing is to understand what caused the delay, and then decide what to do next.
More
Menopause
Thyrotoxicosis
Encephalitis
Night sweats
According to statistics, more than a third of patients complain of periodic sweating that occurs during the day. Far from always, this condition is a sign of a disease, but if such a symptom occurs regularly for no apparent reason and at night, this should be paid attention to.
Far from always, this condition is a sign of a disease, but if such a symptom occurs regularly for no apparent reason and at night, this should be paid attention to.
More
Diabetes mellitus
Thyrotoxicosis
Menopause
Colitis
Rheumatism
Arthritis
Pain when turning the head
Pain when turning the head: causes, in which diseases it occurs, diagnosis and treatment.
More
Atherosclerosis
Menopause
Atrial fibrillation
Heart attack
IBS
Myocarditis
Cardiomyopathy
Hypothyroidism
Intoxication
Climax
Heart sinking
Heart sinking: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
More
Nothing found
Try changing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from the list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Try changing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data
Subscribe
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Otrivin,Home
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself, as these are complex drugs with certain restrictions, side effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself, as these are complex drugs with certain restrictions, side effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by depression
Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood.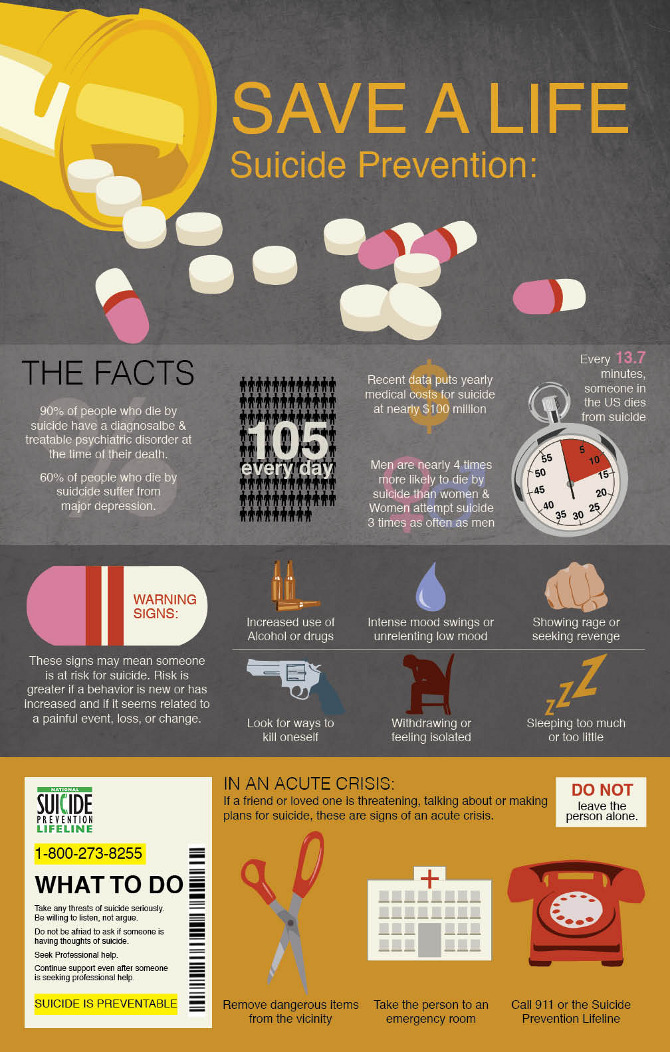 Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are drugs, whose action is aimed precisely at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are drugs, whose action is aimed precisely at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
You can only take these drugs with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of treatment. Sustainable action - after six months. All this time, you need to take the remedy without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
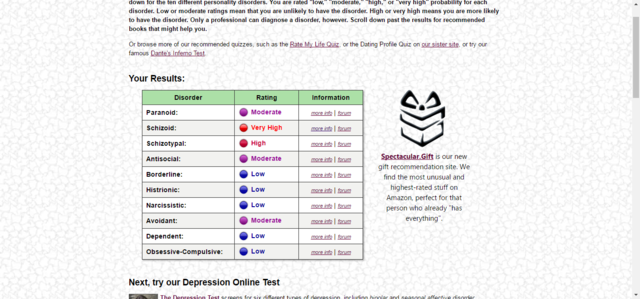
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors.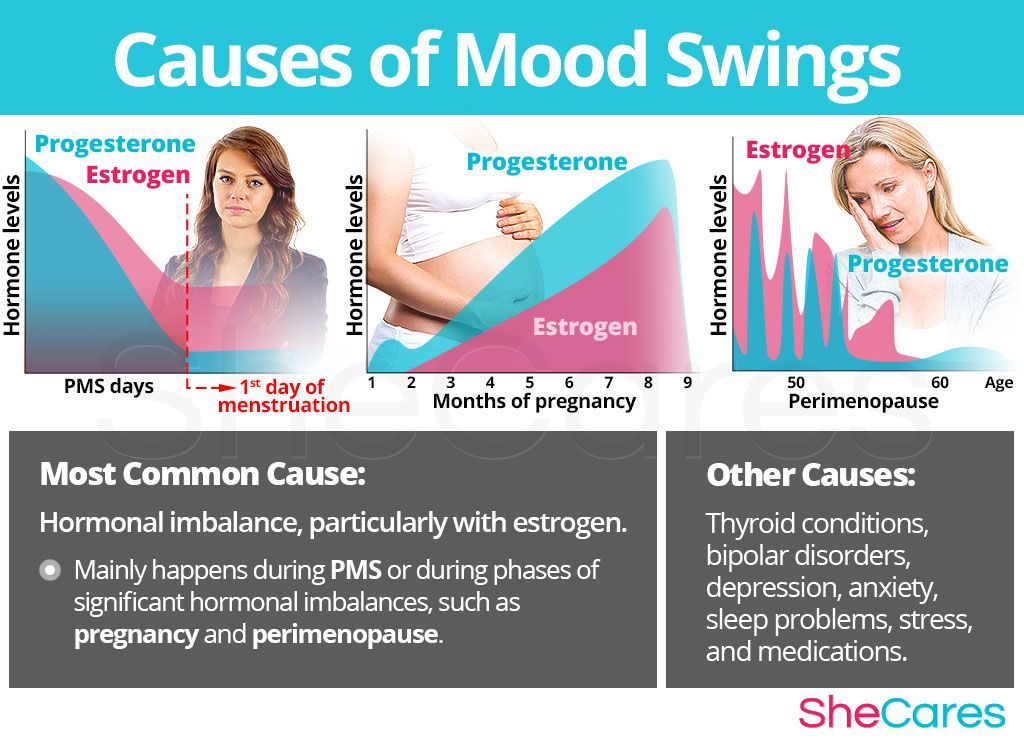 The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No correlation with blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
— Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed in patients who are contraindicated in tricyclic drugs.
Pluses
+ A lasting effect occurs after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
— Anxiety may increase in the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a mild sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Combines well with most drugs in the general group.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the admission period, you must drive carefully and engage in potentially dangerous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most widely used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
- Gastrointestinal disorders, insomnia, agitation are possible.