Beta blocker for stress
Benefits, Side Effects, and Risks
What are beta-blockers?
Beta-blockers are a class of medication that helps control your body’s fight-or-flight response and reduce its effects on your heart. Many people take beta-blockers to treat heart-related conditions, such as:
- high blood pressure
- heart failure
- an irregular heartbeat
Doctors can also prescribe beta-blockers for off-label use like for help managing anxiety symptoms. Read on to learn more about how beta-blockers impact anxiety, and whether they could work for you.
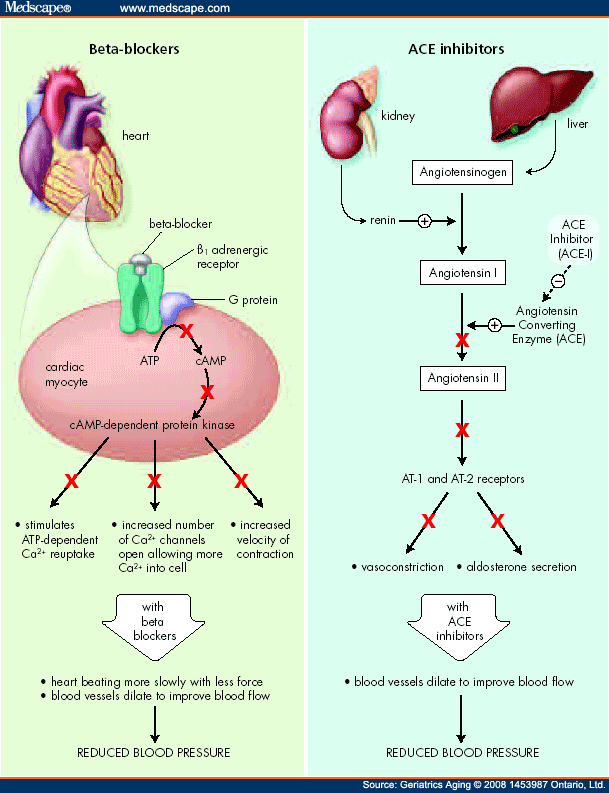
Beta-blockers are also called beta-adrenergic blocking agents. They prevent adrenaline — a stress-related hormone — from making contact with your heart’s beta receptors. This prevents adrenaline from making your heart pump harder or faster.
In addition to relaxing your heart, some beta-blockers also relax your blood vessels, which can help to reduce blood pressure.
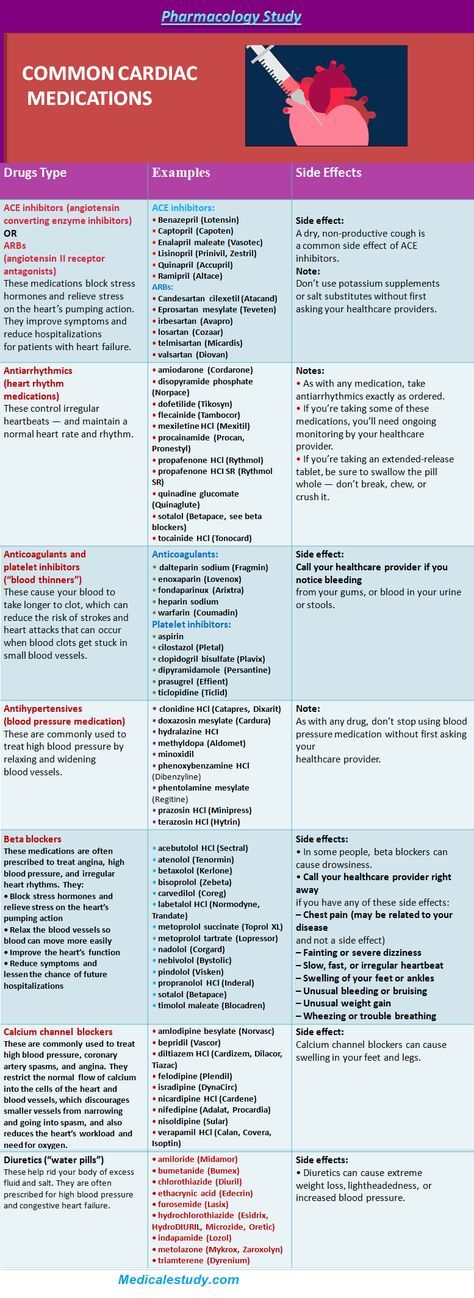
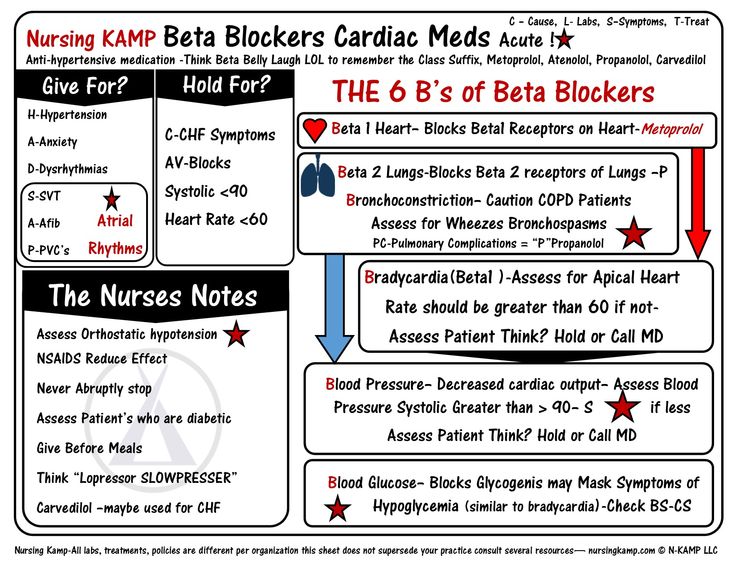
There are many beta-blockers available, but some of the more common ones include:
- acebutolol (Sectral)
- bisoprolol (Zebeta)
- carvedilol (Coreg)
- propranolol (Inderal)
- atenolol (Tenormin)
- metoprolol (Lopressor)
All beta-blockers used to treat anxiety are prescribed off-label. Propranolol and atenolol are two beta-blockers that are often prescribed to help with anxiety.
Off-label drug useUsing a drug off-label means that a drug has been approved by the FDA for one purpose, and it’s being used for a different purpose that hasn’t been approved. A doctor can still prescribe it for this purpose because the FDA regulates the testing and approval of drugs, not how doctors use them to treat their patients. Your doctor can prescribe a drug off-label if they think it’s best for your care.
Beta-blockers won’t treat the underlying psychological causes of anxiety, but they can help you manage some of your body’s physical reactions to anxiety, such as:
- a fast heart rate
- shaky voice and hands
- sweating
- dizziness
By decreasing your body’s physical reactions to stress, you may feel less anxious during stressful times.
Beta-blockers work best for managing short-term anxiety about specific events, rather than long-term anxiety. For example, you can take a beta-blocker before giving a public speech if that’s something that makes you feel anxious.
For example, you can take a beta-blocker before giving a public speech if that’s something that makes you feel anxious.
A 2016 review of existing research about using short-term propranolol for treating different anxiety disorders found that its effects were similar to those of benzodiazepines. These are another class of medication that’s often used to treat anxiety and panic disorders. However, benzodiazepines can cause a range of side effects, and some people have a higher risk of becoming dependent on them.
Still, the same review found that beta-blockers weren’t very effective for social phobias.
People respond differently to medications, especially when it comes to treating mental health issues like anxiety. What works for one person may not work at all for someone else. You may also need additional treatment options for your anxiety while taking beta-blockers, to get to the more psychological aspects.
Both atenolol and propranolol come in pill form. The amount you should take depends on both the type of beta-blocker and your medical history.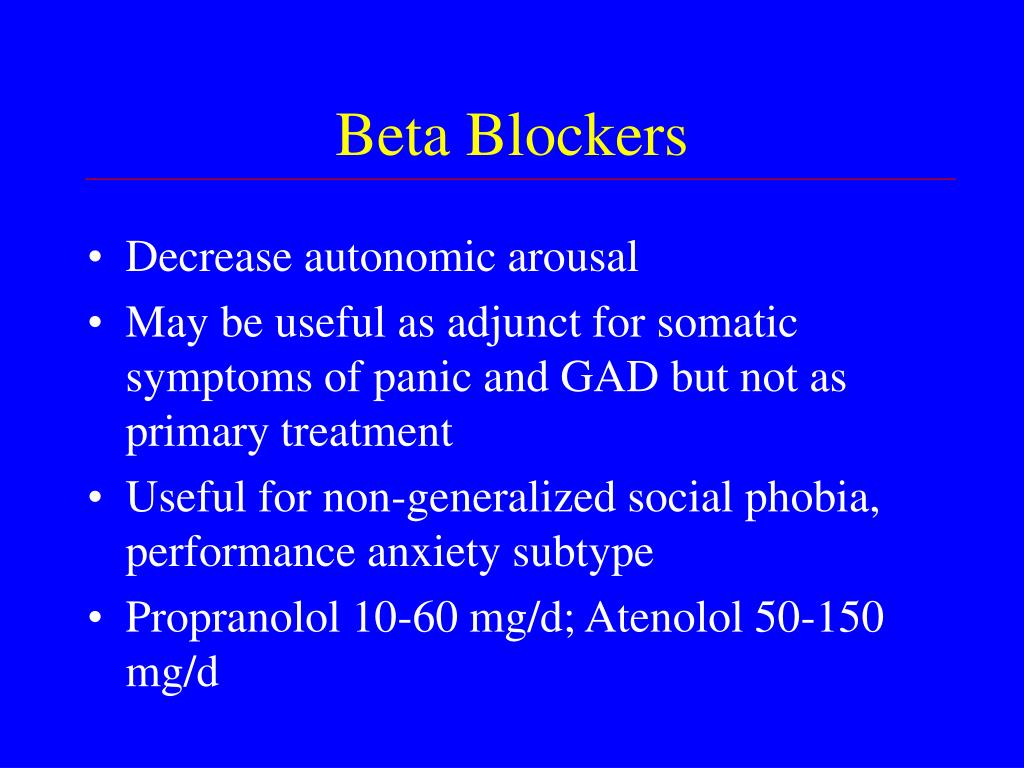 Never take more than what your doctor prescribes.
Never take more than what your doctor prescribes.
You’ll likely notice results the first time you take beta-blockers for anxiety, but they can take an hour or two to reach their full effect. During this time, you’ll feel your heart rate decrease, which might make you feel more relaxed.
Depending on your symptoms, your doctor might suggest taking a beta-blocker regularly or just before stressful events. Usually, beta-blockers will be used in combination with other treatments such as therapy, lifestyle changes, and other medications.
Beta-blockers can cause some side effects, especially when you first start taking them.
Possible side effects include:
- fatigue
- cold hands and feet
- headache
- dizziness or lightheadedness
- depression
- shortness of breath
- vomiting, diarrhea, or constipation
Call your doctor if you experience any more serious side effects, including:
- very slow or irregular heartbeat
- low blood sugar
- an asthma attack
- swelling and fluid retention, along with weight gain
If you notice mild side effects, don’t stop taking the beta-blocker without talking to your doctor first. If you take beta-blockers regularly, you may have serious withdrawal symptoms if you suddenly stop.
If you take beta-blockers regularly, you may have serious withdrawal symptoms if you suddenly stop.
For some people, the side effects of beta-blockers may actually cause anxiety symptoms. You should follow up with your doctor as soon as possible if you feel like taking beta-blockers is increasing your anxiety.
While beta-blockers are generally safe, certain people shouldn’t take them.
Before taking beta-blockers, make sure to tell your doctor if you have:
- asthma
- low blood sugar
- final stage heart failure
- very low blood pressure
- very slow heart rate
If you have any of these conditions or symptoms, you may still be able to take beta-blockers, but you’ll need to work with your doctor to weigh the risks and benefits.
Beta-blockers can also interact with other medications used to treat many heart conditions and antidepressants, so make sure you keep your doctor up to date about any medications, supplements, or vitamins you take.
Beta-blockers can be helpful in managing symptoms for some people with anxiety. It’s been shown as a viable treatment option for short-term anxiety, especially before a stressful event. However, beta-blockers aren’t as useful for long-term treatment.
If you’re interested in trying beta-blockers for managing your anxiety, speak with your doctor. They can advise on the best treatment plan for you that will help manage your specific symptoms.
Benefits & Risks – Cleveland Clinic
It’s not uncommon for certain situations to make your heart pump a bit faster or make your hands start a-trembling. Maybe it’s getting on an airplane. Or public speaking. Or taking a big test.
For people who experience situational or performance-related anxiety, beta-blockers (a medication commonly prescribed for heart conditions) can provide some relief.
We talked with psychiatrist Jack Owens, MD, about how beta-blockers work for some people who experience short-lived anxiety in specific situations.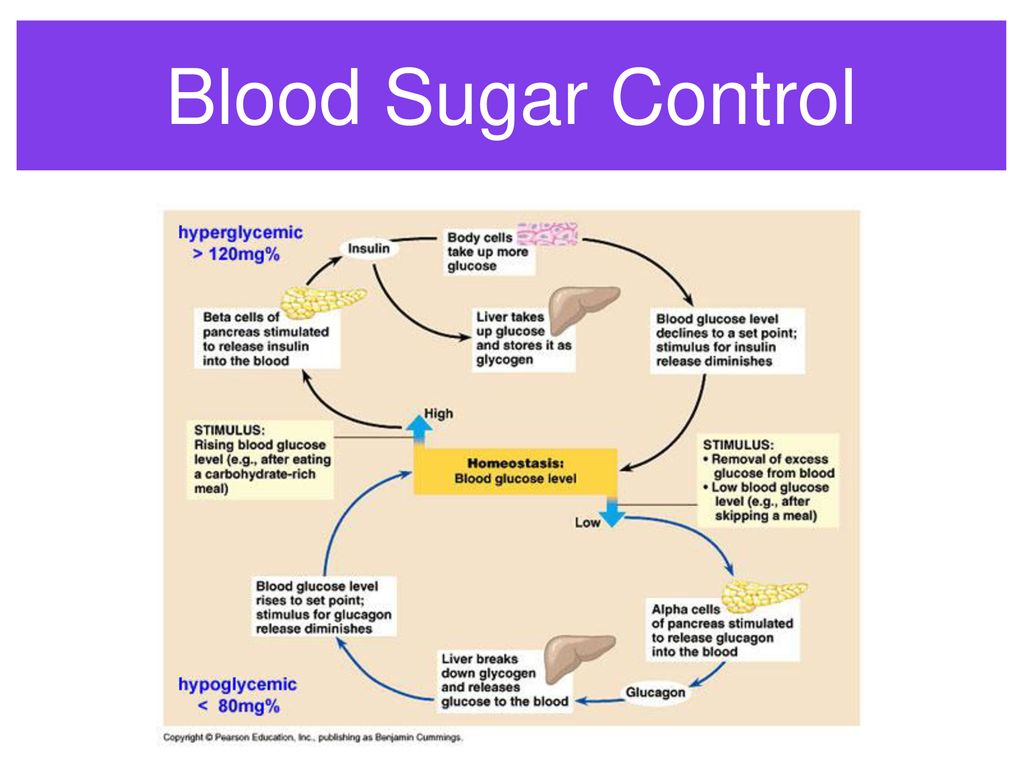
“Beta-blockers work to dampen down the body’s ‘fight-or-flight’ response,” Dr. Owens explains. “Often, when people think of anxiety or a panic attack, it’s accompanied by a racing heart, sweating or shaking. Beta-blockers can work by lessening those symptoms.”
What are beta-blockers, and are they the answer to your anxiety? Dr. Owens breaks it down.
What are beta-blockers?Beta-blockers are some of the most commonly prescribed medications in the United States. Approximately 30 million adults use a beta-blocker. For most people, these medications are prescribed for heart conditions like high blood pressure or an irregular heartbeat.
Are beta-blockers good for anxiety?The U.S. Food and Drug Administration (FDA) approves beta-blockers for treatment of heart-related conditions. Their use for anxiety is considered “off-label use.” That means beta-blockers aren’t specifically intended to be used for performance anxiety, but they can still be legally and safely prescribed for that use.
“‘Off-label’ means that we are using an FDA-approved medication but not necessarily for the condition the FDA approved it for,” Dr. Owens says. “Often, we use off-label medications because a drug has an unintended benefit or because there is some evidence to suggest it is helpful in other circumstances.”
Advertising Policy
The FDA says that after it approves a medication, it’s able to be used in other situations when medically appropriate.
Research has backed the use of beta-blockers to relieve the physical effects of anxiety, like sweating, shaking or a racing heart.
“When your doctor prescribes you a medication to be used off-label, it’s important to have an open risk-benefit discussion with them,” Dr. Owens advises. “As with any medication, you’ll want to be upfront about any other conditions you have and any other medications you may be taking.”
How do beta-blockers work?Beta-blockers slow down certain activities in your cells.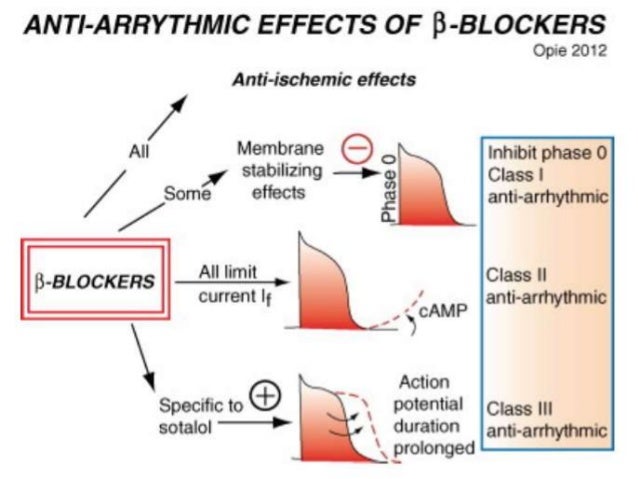 Essentially, they work like this:
Essentially, they work like this:
- Your body produces adrenaline (the body’s “fight-or-flight” hormone).
- Adrenaline goes around your body clinging to receptors — places on the surface of your cells that it can latch onto.
- When enough adrenaline sets up shop, it gets your cells all amped up and ready to spring into action. That can cause your heart to speed up or make you sweat or tremble.
Beta-blockers work by … well … blocking the receptors that adrenaline is looking for. It’s like a game of musical chairs, where the beta-blocker steals a seat and the adrenaline goes off and sits on the sidelines. If adrenaline can’t bind to your receptors, you don’t get those effects of adrenaline overload.
Who’s a candidate for beta-blockers for anxiety?Dr. Owens says beta-blockers are best used for people who experience anxiety in specific situations, like stage fright for example, rather than for people who live with a diagnosed anxiety disorder.
“Beta-blockers are usually reserved for people who experience anxiety around specific occasions but are otherwise able to function in their capacity,” Dr. Owens notes.
Advertising Policy
That’s because beta-blockers only deal with the physical effects of anxiety, not any underlying chemical imbalance or psychological reasons for anxiety. In this way, beta-blockers are like a bandage — they’ll stop the bleeding, but they won’t fix the uneven floorboard that you tripped over.
Are there risks to taking beta-blockers?Beta-blockers have been used and studied extensively since the 1960s and are generally well-tolerated by most people. Some people, including those living with asthma, COPD (chronic obstructive pulmonary disease) or diabetes shouldn’t take beta-blockers.
Side effects are usually mild and may include:
- Dizziness.
- Dry mouth or eyes.
- Fatigue.
- Insomnia, sleep changes and nightmares.
- Irregular heart rhythms (arrhythmias).
- Low blood pressure.
- Nausea.
- Slow heart rate.
Importantly, Dr. Owens says beta-blockers shouldn’t be used without a prescription from your healthcare provider. Your provider will be able to make the best determination as to whether you’re a good candidate for beta-blockers or other medication.
Other ways to manage anxietyThere are other options to help manage your in-the-moment anxiety. Dr. Owens suggests deep breathing techniques as a way to calm your nervous system when you find yourself in an anxiety-provoking situation.
“Controlling your breath is a good way to ‘trick’ your brain,” Dr. Owen explains. “Concentrating on breathing gives the subconscious part of your brain a specific task to do and distracts your mind from runaway thoughts.”
If you experience more chronic anxiety and find that anxiety is keeping you from enjoying your life or going about your day-to-day activities, talk to a healthcare provider. They’ll be able to help you determine a treatment plan that’s right for you.
They’ll be able to help you determine a treatment plan that’s right for you.
types, principle of action and areas of application
- Action of beta-blockers
- Discovery history
- Classification of beta-blockers
- Applications
Image by Freepik
Cardiac activity is completely subordinated to adrenaline release, which speeds up the pulse, increases blood pressure and heart rate. Beta-blockers help slow down the process to protect the heart from the long-term effects of epinephrine and norepinephrine (catecholamines). nine0013
Action of beta-blockers
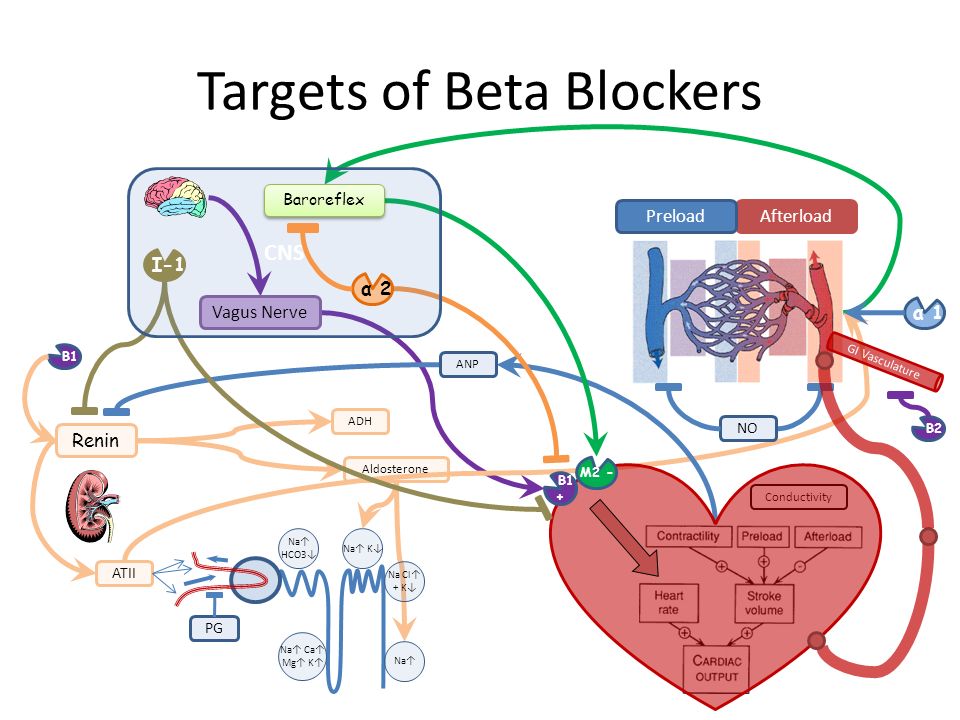
Beta-blockers stop the transmission of certain nerve impulses. When a nerve is stimulated, the ends of some nerves release a chemical (a neurotransmitter) called norepinephrine. This chemical then stimulates beta-adrenergic receptors. There are two different types: beta1 (β1)-adrenergic receptors, which affect the strength and frequency of heart contractions, as well as blood pressure. Beta2 (β2)-adrenergic receptors cause relaxation of the smooth muscles of the bronchi, uterus and blood vessels. nine0013
Beta2 (β2)-adrenergic receptors cause relaxation of the smooth muscles of the bronchi, uterus and blood vessels. nine0013
In the body, beta-blockers inhibit the action of the stress hormone adrenaline and the messenger substance norepinephrine. This leads to a decrease in heart rate. The heart muscle requires less oxygen and relaxes, which is especially important for patients with chronic heart failure or coronary heart disease.
Physicians commonly combine beta-blockers with other active ingredients to lower blood pressure, and their arousal-suppressing effect makes them the #1 drug in the fight against cardiac arrhythmias. Beta-blockers are available in the form of tablets, only a small part is for intravenous use. nine0013
Discovery history
In 1948, the American Raymond Ahlquist established the importance of the participation of norepinephrine in the transmission of nerve impulses. By this time, two types of adrenergic receptors were also known: alpha, which are most often present in the contractile tissues (smooth muscles) of the brain and liver, and beta, concentrated in the endocrine and external secretion glands, heart and kidneys.
In 1958, pharmacologist James Black from Scotland got a job as a young specialist at ICI Pharmaceuticals, choosing the most promising area - pharmacotherapy to improve myocardial blood supply. Thanks to Black at 19In 1968, the first beta-blocker, Propranolol, rolled off the assembly line. For his discovery and development, James Black was awarded the Nobel Prize in Physiology or Medicine in 1988.
Over the entire history, about a hundred drugs have been synthesized, 30 of them are used in modern practice. The last revolutionary drug of the new generation, Nebivolol, was developed in 2001. It combines the developments of previous generations with a small addition - a vasodilating effect. nine0013
Classification of beta-blockers
-
Selective / non-selective. Non-selective equally affect both types of β1 / β2 receptors. Selective ones are directed only to β1 receptors.
-
Lipophilic or fat soluble. It is better to overcome the blood-brain barrier between the circulatory and central nervous system, the drug is excreted by the liver, because of this, it should be carefully used by people suffering from liver failure.
 Absorption - 70–90%.
Absorption - 70–90%. -
Hydrophilic, or water-soluble, are metabolized in the liver for an order of magnitude longer, which means a prolonged effect of action. Excreted by the kidneys. Absorption - 30-50%.
-
Amphiphilic blockers are lipid and water soluble. Absorption of the drug - 40-60%. It is equally well excreted by both the liver and the kidneys.
Applications:
-
hypertension. Beta-blockers prevent the negative effects of the sympathetic nervous system on the heart. The need for oxygen decreases, blood pressure stabilizes;
-
heart failure. Studies have shown that the use of beta-blockers reduces the risk of death from heart failure by 30% and the risk of severe conditions requiring hospitalization by 40%. Among patients with chronic or long-term heart failure, the risk of sudden death is reduced by 38%. Beta-blockers that are useful for heart failure include carvedilol, bisoprolol, nebivolol, and long-acting metoprolol; nine0013
-
acute myocardial infarction or heart attack.
 Beta-blockers such as Carvedilol and Netoprolol may reduce the risk of heart attack and death. The drugs are especially useful for high-risk patients who have prolonged cardiac ischemia or left ventricular dysfunction;
Beta-blockers such as Carvedilol and Netoprolol may reduce the risk of heart attack and death. The drugs are especially useful for high-risk patients who have prolonged cardiac ischemia or left ventricular dysfunction; -
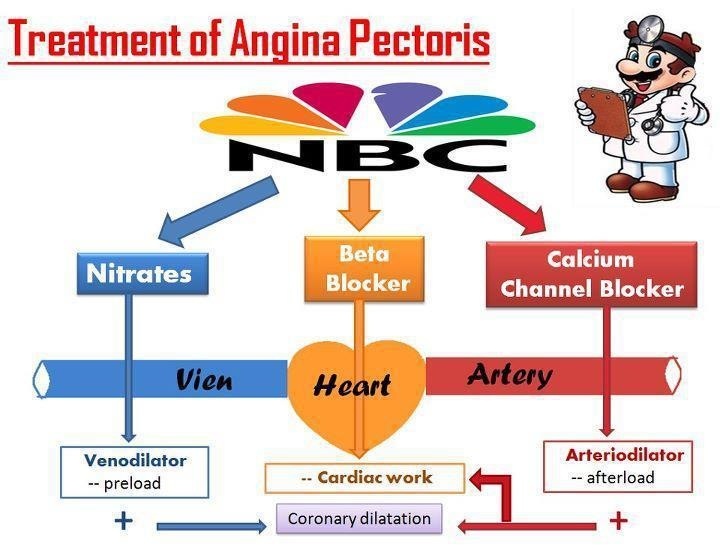
chronic stable angina. Patients with this disease experience a lack of blood supply (ischemia) to the heart muscles, resulting in chest pain, especially during exercise. Beta-blockers reduce myocardial oxygen demand and heart rate. A special form of angina pectoris called "Prinzmetal's angina" should not be treated with non-selective beta-blockers, since the components can aggravate the condition; nine0013
-
cardiac arrhythmias or arrhythmias. Some beta-blockers can be used to treat arrhythmias, such as Sotalol, Esmolol, and Propranolol. Beta-blockers are recommended in cases of arrhythmias involving the ventricles to reduce the risk of cardiac death from ventricular arrhythmias. Beta-blockers are also effective in treating an inherited arrhythmia called "Long Interval Syndrome";
nine0003 -
anxiety. Drugs neutralize the effect of stress hormones on the psychological state. As a result, the frequency of physical manifestations of anxiety, tremor, sweating is significantly reduced. Many public figures take beta-blockers before performances to relieve emotional stress. However, in case of clinical manifestation of anxiety, it is necessary to consult with a specialized doctor; nine0013
-
overactive thyroid. Medicines reduce the frequency of symptomatic manifestations (tremors, heart palpitations) by blocking the action of thyroid hormone in the bloodstream;
-
essential tremor. Studies show that 50-60% of people notice an improvement in their condition after taking Propranolol, hand tremor stops.
glaucoma.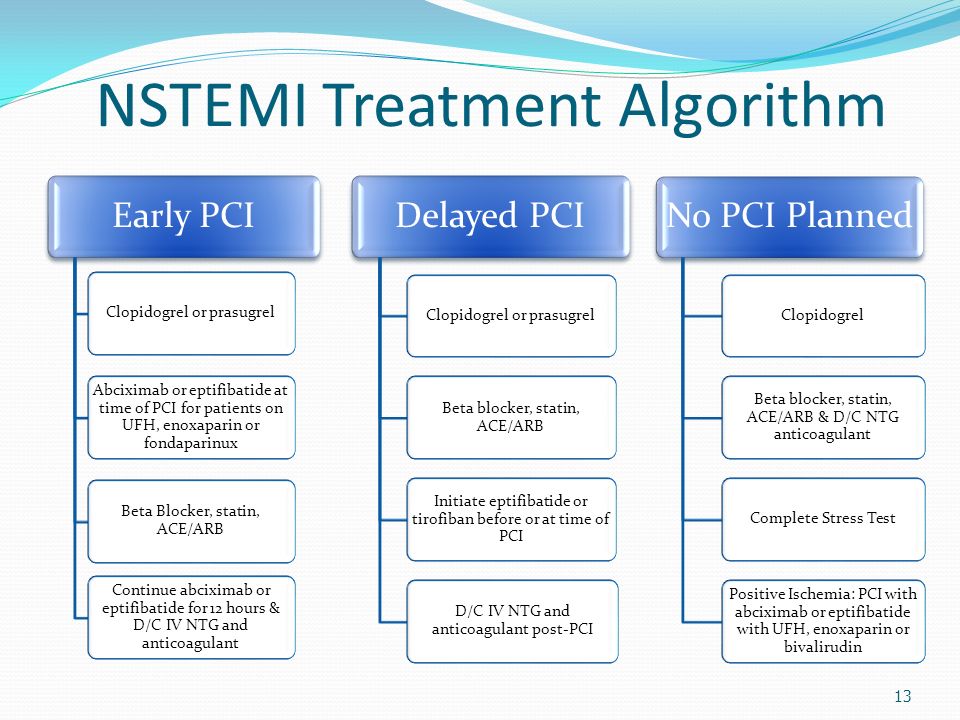 This condition, in which pressure builds up in the eye due to fluid buildup, is a common cause of vision loss among older adults. Eye drops containing beta-blockers reduce fluid production and normalize eye pressure;
This condition, in which pressure builds up in the eye due to fluid buildup, is a common cause of vision loss among older adults. Eye drops containing beta-blockers reduce fluid production and normalize eye pressure;
The duration of treatment is determined on the basis of the patient's condition and diseases. Some people only need to take beta-blockers for a few weeks or months, such as those with an overactive thyroid. Others - all their lives, for example, after a heart attack (myocardial infarction). nine0013
Beta blockers: humble saviors of humanity
This group of drugs, not being heard by the general public, has been confidently on the list of bestsellers for many decades in a row. Experts consider their development one of the main breakthroughs in drug therapy of the 20th century, and the Nobel Committee adheres to the same opinion, which awarded the creator of adrenaline beta receptor antagonists, or beta-blockers, the most prestigious scientific award. nine0013
On my own
In 1958, Scottish pharmacologist James Black joined ICI. The young specialist, whose father had recently died of a heart attack, intended to develop drugs for the treatment of coronary heart disease. The causes of the disease were generally known, but pharmacotherapy left much to be desired: nitrates were the only widely used agent, but their effectiveness was recognized as very limited.
The causes of the disease were generally known, but pharmacotherapy left much to be desired: nitrates were the only widely used agent, but their effectiveness was recognized as very limited.
The most promising direction in the treatment of coronary artery disease at that time were considered substances that can increase the delivery of oxygen to the heart muscle (that is, improve the blood supply to the myocardium). However, Black chose a different path: not to satisfy the "increased demands" of the heart, but to try to minimize them. The scientist intended to achieve this by suppressing the effects of adrenaline and norepinephrine.
The creator of 2 drugs that brought multibillion-dollar profits to manufacturers, led an extremely modest lifestyle and was a reclusive person who earned himself the reputation of a stubborn eccentric and "weird type" among representatives of pharmaceutical companies. Upon learning that he had become a Nobel Prize winner, he, in his own words, “fell into horror and despair”: he was oppressed by the need to participate in solemn events and speak to a huge audience.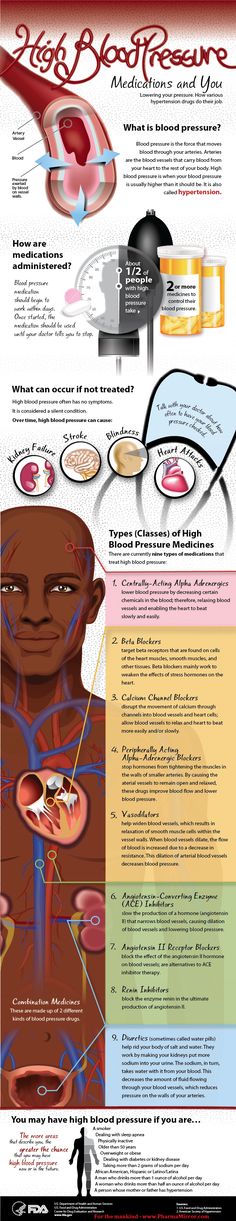 nine0013
nine0013
The physiological function of adrenaline (or rather, an extract of the adrenal glands, the active substance of which has not yet been isolated in its pure form) was already known by the beginning of the 20th century. But only in 1948, the American Raymodn Ahlquist managed to establish the role of the analog of adrenaline - norepinephrine in the transmission of nerve impulses and describe the principles of operation of the receptors that these substances act on.
Somewhat later it turned out that adrenergic receptors are of 2 main types - alpha, which are found mainly in the smooth muscles of various organs, the brain and liver, and beta, located mainly in the heart, blood vessels, kidneys, glands of external and internal secretion. All this data was useful to a young pharmacologist from ICI Pharmaceuticals. nine0013
According to Black's plan, blocking beta receptors should have led to a reduction in heart rate and cardiac output and, as a result, to a decrease in the heart's need for oxygen.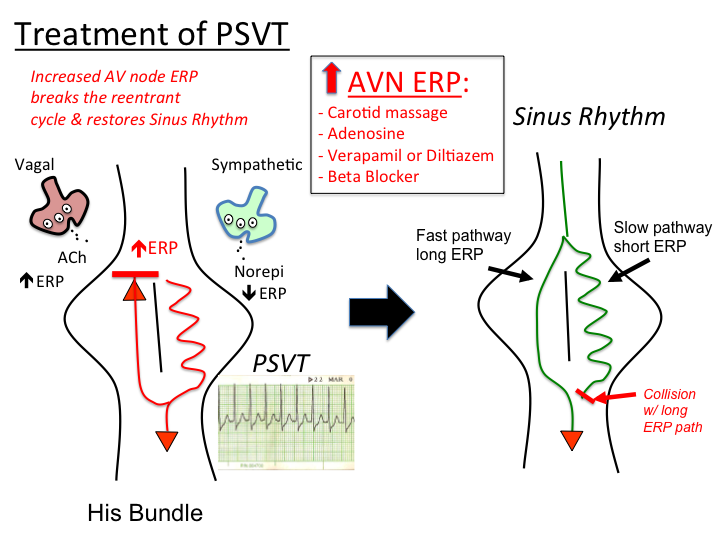 As a result, one could expect a decrease in the number of angina attacks in patients with coronary artery disease and a drop in blood pressure.
As a result, one could expect a decrease in the number of angina attacks in patients with coronary artery disease and a drop in blood pressure.
With the development of beta-blockers, James Black succeeded in creating yet another revolution, this time in the treatment of stomach ulcers. Moreover, in order to develop a new class of drugs, the scientist had to change his employer, as his plans seemed unpromising to the ICI leadership. Cimetidine, the first histamine h3-receptor blocker that reduces gastric acid production, was introduced to the market by Smith Kline in 1973 and immediately became a new bestseller, surpassing sales including propranolol. Black's achievements were recognized with the 1988 Nobel Prize in Physiology or Medicine, as well as a number of other prestigious awards. The Scottish researcher is rightfully considered one of the most prominent pharmacologists of the 20th century.
Not only the heart
After several setbacks, Black and his colleagues finally found a compound that interacted effectively with adrenergic receptors and met safety requirements.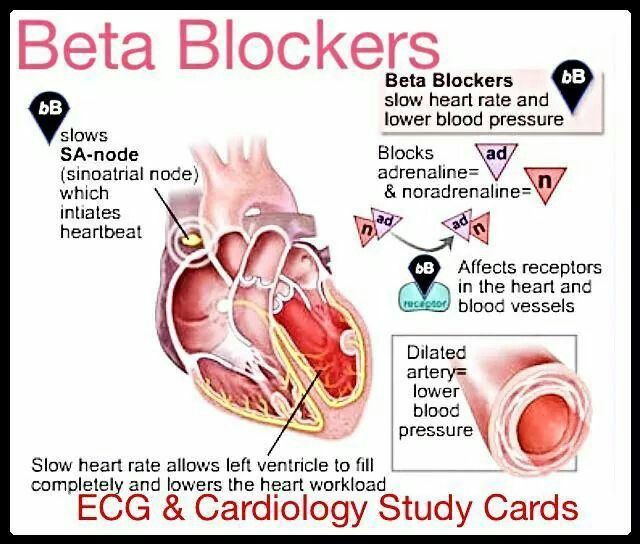 The first drug from the group of beta-blockers, propranolol, entered the market in 1964, exceeded all expectations and made a real revolution in cardiology. The new drug not only reduced the frequency and intensity of angina attacks, but also 4 times reduced the likelihood of heart attacks in patients with coronary artery disease. In addition, propranolol showed excellent results in the treatment of myocardial infarction, tachyarrhythmias (including hyperthyroidism, neuroses and other conditions), glaucoma, tremors of various origins, many types of headaches (including migraine) and a number of mental illnesses. Because of this, it quickly took the first place in the world in terms of sales among prescription drugs. nine0013
The first drug from the group of beta-blockers, propranolol, entered the market in 1964, exceeded all expectations and made a real revolution in cardiology. The new drug not only reduced the frequency and intensity of angina attacks, but also 4 times reduced the likelihood of heart attacks in patients with coronary artery disease. In addition, propranolol showed excellent results in the treatment of myocardial infarction, tachyarrhythmias (including hyperthyroidism, neuroses and other conditions), glaucoma, tremors of various origins, many types of headaches (including migraine) and a number of mental illnesses. Because of this, it quickly took the first place in the world in terms of sales among prescription drugs. nine0013
This advance paved the way for the synthesis of other beta-blockers with different pharmacological profiles. The discovery of beta receptor subtypes has made these drugs even more selective; in addition, it turned out that their action is influenced by a number of parameters, such as intrinsic sympathomimetic activity and lipo- or hydrophilicity. This, as well as the duration of action, determines the difference in indications for the use of beta-blockers.
This, as well as the duration of action, determines the difference in indications for the use of beta-blockers.
Although beta-blockers can cause excessive blood pressure reduction, muscle weakness, drowsiness, depression, and libido suppression, many musicians, actors, politicians, and other celebrities use them without medical advice in public speaking to reduce anxiety, embarrassment, and panic. or tremor. Due to the similar effects of beta-blockers, they are considered doping in sports that require precise coordination of movements and composure: shooting, golf, billiards, etc. nine0013
In a basement somewhere nearby. After creating beta-blockers, James Black managed to create another revolution - this time in the treatment of stomach ulcers. Moreover, in order to develop a new class of drugs, the scientist had to change his employer, as his plans seemed unpromising to the ICI leadership. Cimetidine, the first histamine h3 receptor blocker to reduce stomach acid production, was introduced to the market by Smith Kline in 1973 and immediately became a new bestseller, outselling propranolol as well.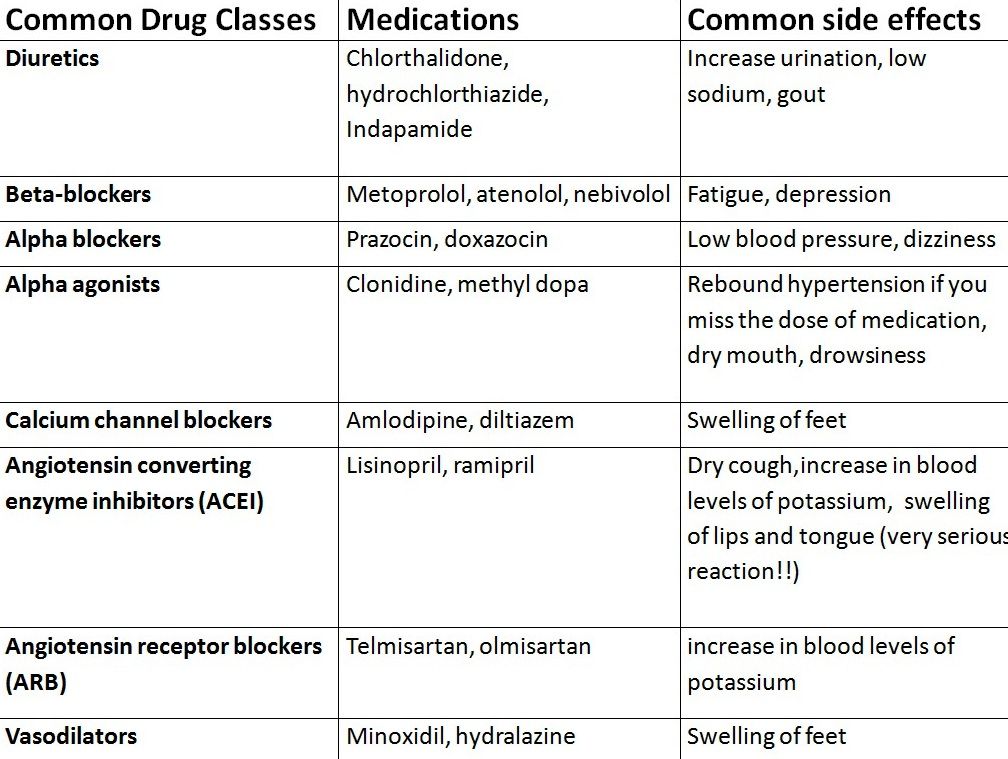 Black's achievements were awarded the Nobel Prize in Physiology or Medicine1988 years old, as well as a number of other prestigious awards. The Scottish researcher is rightfully considered one of the most prominent pharmacologists of the 20th century.
Black's achievements were awarded the Nobel Prize in Physiology or Medicine1988 years old, as well as a number of other prestigious awards. The Scottish researcher is rightfully considered one of the most prominent pharmacologists of the 20th century.
James Black (1924–2010)
The creator of 2 drugs that brought multibillion-dollar profits to manufacturers, led an extremely modest lifestyle and was an introverted person who earned himself the reputation of a stubborn eccentric and "weird type" among representatives of pharmaceutical companies. Upon learning that he had become a Nobel Prize winner, he, in his own words, “fell into horror and despair”: he was oppressed by the need to participate in solemn events and speak to a huge audience. nine0104
How it works
To understand the difference between selective and non-selective varieties of these drugs, it is necessary to consider the effects of individual subtypes of adrenaline beta receptors.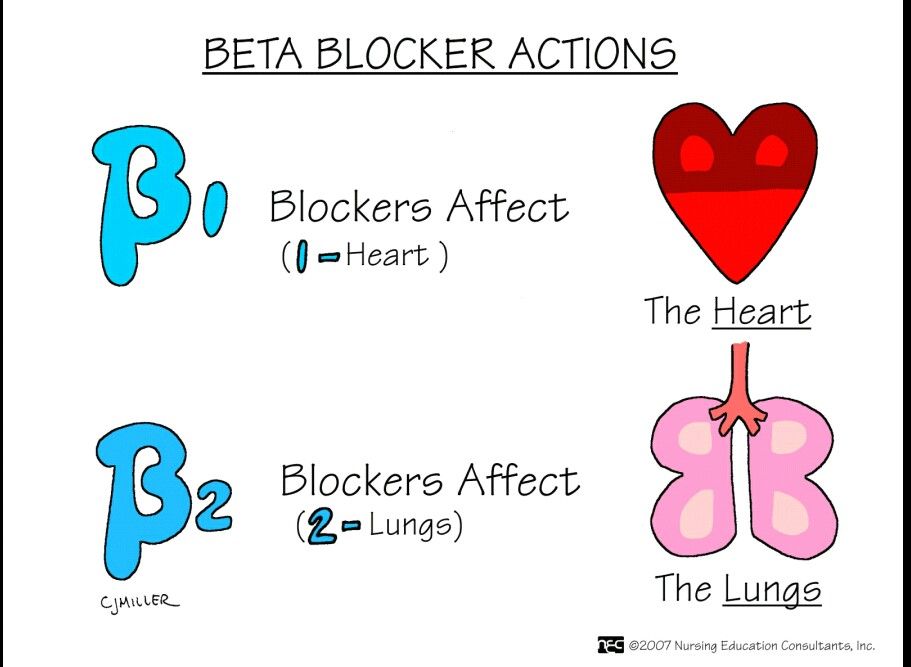 Currently, there are 3 of them, although it is possible that this list will be expanded in the future.
Currently, there are 3 of them, although it is possible that this list will be expanded in the future.
Beta1 receptors are located predominantly in the heart and kidneys. In the heart, their stimulation leads to an increase in heart rate (due to the action on the sinus node and the conduction system of the heart) and myocardial contractility, which increases cardiac output and oxygen consumption by the heart muscle. nine0013
In a healthy person, these effects are a normal response to stress or exercise, but in coronary artery disease they exacerbate angina pectoris and, in severe cases, may contribute to the development of a heart attack. In heart failure, “boosting” an already overloaded myocardium paradoxically reduces the efficiency of cardiac activity. In addition, in predisposed individuals, excessive stimulation of beta1 receptors leads to the development of various types of tachyarrhythmias.
In the kidneys, these receptors activate the renin-angiotensin-aldosterone system, which increases blood pressure by increasing vascular resistance and blood volume.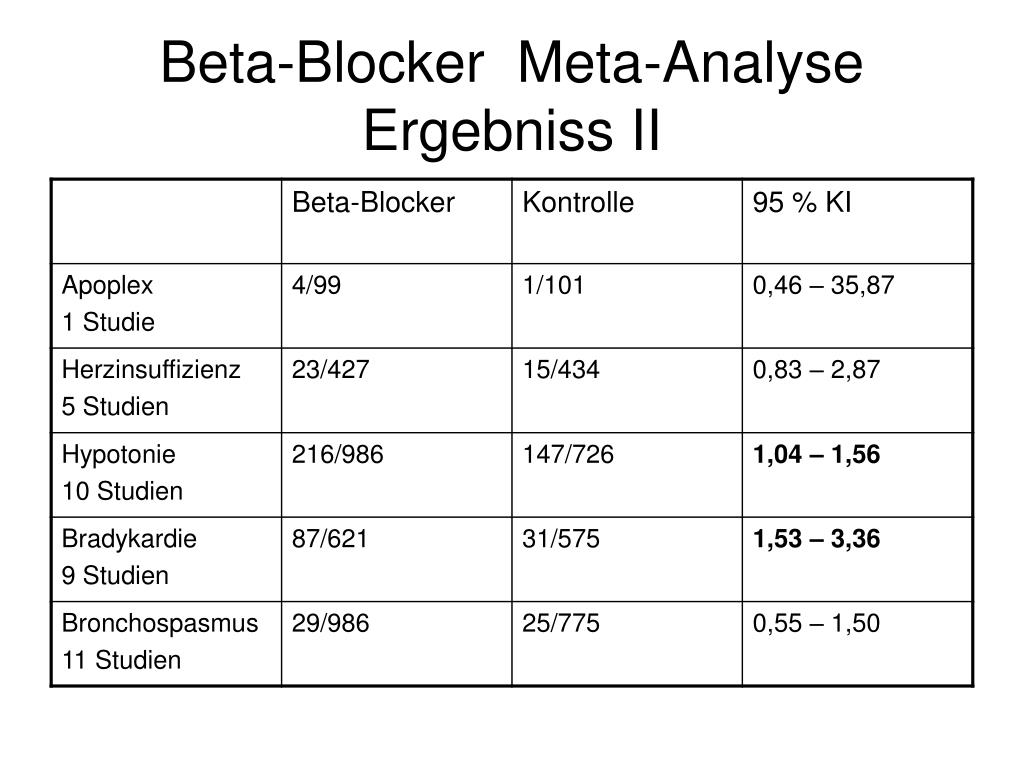 The suppression of these effects is predominantly used in the treatment of coronary artery disease, hypertension and myocardial infarction. Due to the predominant effect of selective beta1-blockers (bisoprolol, betaxolol and metoprolol in the form of succinate, atenolol and nebivolol) on the heart, they are often called cardioselective. nine0013
The suppression of these effects is predominantly used in the treatment of coronary artery disease, hypertension and myocardial infarction. Due to the predominant effect of selective beta1-blockers (bisoprolol, betaxolol and metoprolol in the form of succinate, atenolol and nebivolol) on the heart, they are often called cardioselective. nine0013
Although beta-blockers can cause excessive blood pressure reduction, muscle weakness, drowsiness, depression, and libido suppression, many musicians, actors, politicians, and other celebrities use them without medical advice in public speaking to suppress anxiety, confusion, panic, or tremor. Due to the similar effects of beta-blockers, they are considered doping in sports that require precise coordination of movements and composure: shooting, golf, billiards, etc. nine0104
Beta1-blockers are absolutely contraindicated in unstable heart failure, blockade, severe hypotension, severe bradycardia, and sick sinus syndrome.
Beta2 receptors are located primarily in smooth muscle cells of internal organs, eyes and blood vessels, as well as in skeletal muscle, liver, pancreas and salivary glands. In the heart, the effect of these receptors is similar to beta1, but much less pronounced.
Stimulation of beta2 receptors leads to bronchial dilatation, slowing peristalsis and increased tone of the gastrointestinal sphincters (resulting in a slowdown in digestion), relaxation of the uterus, bladder and urinary tract sphincters, increased glycogen utilization by the liver and skeletal muscles, as well as a decrease in circulatory tone. vessels. nine0013
Because of this, only non-selective beta-blockers - propranolol, nadolol, oxprenolol, timolol and many others - are effective for tremor and vasospastic headaches (although only propranolol is used for these indications), as well as glaucoma (timolol is used). Contraindications for beta1-blockers include bronchial asthma, diabetes mellitus, Raynaud's syndrome and, in some cases, uterine hypertonicity.
Beta3 receptors are located in adipose tissue and "manage" its catabolism, but this effect is not used purposefully in the clinic. nine0013
Currently, beta-blockers remain practically the only drugs that have a pronounced effect on the prognosis of cardiac patients. These drugs improve the quality and duration of life, as well as reduce the risk of heart attacks and strokes in millions of patients worldwide.
The use of beta-blockers in arrhythmias deserves special mention. To control persistent tachycardia, including symptomatic (for example, with thyrotoxicosis or panic conditions), any drugs in this group are theoretically suitable, but preference is given to selective ones. In the treatment of acute tachycardia, which significantly affects hemodynamics, ultrashort-acting drugs (esmolol) are used, which are easy to titrate when administered by infusion. Atrial fibrillation (atrial fibrillation) is treated with a variety of medications, but amiodarone and sotalol are most commonly used in the absence of contraindications.
 In addition to beta-blocking action, they have a number of effects on the myocardium, which are far beyond the scope of this article. nine0104
In addition to beta-blocking action, they have a number of effects on the myocardium, which are far beyond the scope of this article. nine0104 Oleg Lischuk
Journal "Russian Pharmacies" №24, 2012
You may like other articles:
Pharmclass
Standing, sitting, lying down
The instructions for the medicine usually indicate how to take it: before, after or with meals. But about the position of the body to swallow the pill, so far, no accompanying documents ...
Read more
Pharmclass
Healthy Throat Recipe
In autumn, literally not a day goes by in a pharmacy without requests for remedies to relieve a sore throat - a common symptom of a cold, tonsillitis or pharyngitis 1 .
Read more
Pharmclass nine0013
Type II collagen: cartilage base
Among the proteins of the human body, collagen accounts for at least 25–45%. This essential structural component of the extracellular matrix provides strength, elasticity, regulation...
Read more
Pharmclass
Starry night Digoxin
An outstanding researcher and therapist of the 19th century, Sergei Botkin, believed that foxglove is the most precious remedy. For many years, preparations based on it remained vital ...
Read more
Pharmclass
Universal skin protection
Damage to the epidermal barrier is one of the causes of dryness and inflammation, including in atopic dermatitis 1 .