Avolition and anhedonia
Negative symptoms in schizophrenia - PMC
1. Kraepelin E. Dementia Praecox and Paraphrenia. Edinburgh: Livingstone; 1919. [Google Scholar]
2. Schneider K. Clinical Psychopathology. New York: Grune and Stratton; 1959. [Google Scholar]
3. Crow TJ. The two-syndrome concept: Origins and current status. Schizophr Bull. 1985;11:471–86. [PubMed] [Google Scholar]
4. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. [PubMed] [Google Scholar]
5. American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition Text Revision. Washington D.C: American Psychiatric Association; 2000. [Google Scholar]
6. Lewis S, Escalona PR, Keith SJ. Phenomenology of Schizophrenia. In: Sadock BJ, Sadock V, Ruiz P, editors. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. [Google Scholar]
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C: American Psychiatric Association; 2013. [Google Scholar]
8. World Health Organization. The Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) Geneva: World Health Organization; 1993. [Google Scholar]
9. Kirkpatrick B, Fenton WS, Carpenter WT, Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–9. [PMC free article] [PubMed] [Google Scholar]
10. Kirschner M, Aleman A, Kaiser S. Secondary negative symptoms - A review of mechanisms, assessment and treatment. Schizophr Res. 2016 pii: S0920-996430224-9. [PubMed] [Google Scholar]
11. Lyne J, O'Donoghue B, Owens E, Renwick L, Madigan K, Kinsella A, et al. Prevalence of item level negative symptoms in first episode psychosis diagnoses. Schizophr Res. 2012;135:128–33. [PubMed] [Google Scholar]
12. Möller HJ. Management of the negative symptoms of schizophrenia: New treatment options. CNS Drugs. 2003;17:793–823. [PubMed] [Google Scholar]
Möller HJ. Management of the negative symptoms of schizophrenia: New treatment options. CNS Drugs. 2003;17:793–823. [PubMed] [Google Scholar]
13. Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT., Jr A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58:165–71. [PubMed] [Google Scholar]
14. Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163:411–7. [PubMed] [Google Scholar]
15. Herbener ES, Harrow M, Hill SK. Change in the relationship between anhedonia and functional deficits over a 20-year period in individuals with schizophrenia. Schizophr Res. 2005;75:97–105. [PubMed] [Google Scholar]
16. Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: Distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–60. [PMC free article] [PubMed] [Google Scholar]
17. Foussias G, Remington G. Negative symptoms in schizophrenia: Avolition and Occam's razor. Schizophr Bull. 2010;36:359–69. [PMC free article] [PubMed] [Google Scholar]
Negative symptoms in schizophrenia: Avolition and Occam's razor. Schizophr Bull. 2010;36:359–69. [PMC free article] [PubMed] [Google Scholar]
18. Fonseca-Pedrero E, Gooding DC, Paino M, Lemos-Giráldez S, Muñiz J. Anhedonia: A Comprehensive Handbook Volume II. Netherlands: Springer; 2014. Measuring anhedonia in schizophrenia-spectrum disorders: A selective update; pp. 19–54. [Google Scholar]
19. Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS) Iowa City: University of Iowa; 1983. [Google Scholar]
20. Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
21. Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Carpenter WT., Jr The schedule for the deficit syndrome: An instrument for research in schizophrenia. Psychiatry Res. 1989;30:119–23. [PubMed] [Google Scholar]
22. Emsley R, Rabinowitz J, Torreman M RIS-INT- Early Psychosis Global Working Group. The factor structure for the Positive and Negative Syndrome Scale (PANSS) in recent-onset psychosis. Schizophr Res. 2003;61:47–57. [PubMed] [Google Scholar]
Schizophr Res. 2003;61:47–57. [PubMed] [Google Scholar]
23. Sergi MJ, Rassovsky Y, Widmark C, Reist C, Erhart S, Braff D, et al. Social cognition in schizophrenia: Relationships with neurocognition and negative symptoms. Schizophr Res. 2007;90:316–24. [PubMed] [Google Scholar]
24. Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The brief negative symptom scale: Psychometric properties. Schizophr Bull. 2011;37:300–5. [PMC free article] [PubMed] [Google Scholar]
25. Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): Final development and validation. Am J Psychiatry. 2013;170:165–72. [PMC free article] [PubMed] [Google Scholar]
26. Liemburg E, Castelein S, Stewart R, van der Gaag M, Aleman A, Knegtering H Genetic Risk and Outcome of Psychosis (GROUP) Investigators. Two subdomains of negative symptoms in psychotic disorders: Established and confirmed in two large cohorts. J Psychiatr Res. 2013;47:718–25. [PubMed] [Google Scholar]
J Psychiatr Res. 2013;47:718–25. [PubMed] [Google Scholar]
27. Levitt JJ, Rosow LK, Nestor PG, Pelavin PE, Swisher TM, McCarley RW, et al. A volumetric MRI study of limbic, associative and sensorimotor striatal subregions in schizophrenia. Schizophr Res. 2013;145:11–9. [PubMed] [Google Scholar]
28. Hovington CL, Lepage M. Neurocognition and neuroimaging of persistent negative symptoms of schizophrenia. Expert Rev Neurother. 2012;12:53–69. [PubMed] [Google Scholar]
29. Winograd-Gurvich C, Fitzgerald PB, Georgiou-Karistianis N, Bradshaw JL, White OB. Negative symptoms: A review of schizophrenia, melancholic depression and Parkinson's disease. Brain Res Bull. 2006;70:312–21. [PubMed] [Google Scholar]
30. John JP, Rangaswamy M, Thennarasu K, Khanna S, Nagaraj RB, Mukundan CR, et al. EEG power spectra differentiate positive and negative subgroups in neuroleptic-naive schizophrenia patients. J Neuropsychiatry Clin Neurosci. 2009;21:160–72. [PubMed] [Google Scholar]
31. Lavoie S, Schäfer MR, Whitford TJ, Benninger F, Feucht M, Klier CM, et al. Frontal delta power associated with negative symptoms in ultra-high risk individuals who transitioned to psychosis. Schizophr Res. 2012;138:206–11. [PubMed] [Google Scholar]
Lavoie S, Schäfer MR, Whitford TJ, Benninger F, Feucht M, Klier CM, et al. Frontal delta power associated with negative symptoms in ultra-high risk individuals who transitioned to psychosis. Schizophr Res. 2012;138:206–11. [PubMed] [Google Scholar]
32. Itoh T, Sumiyoshi T, Higuchi Y, Suzuki M, Kawasaki Y. LORETA analysis of three-dimensional distribution of delta band activity in schizophrenia: Relation to negative symptoms. Neurosci Res. 2011;70:442–8. [PubMed] [Google Scholar]
33. Featherstone RE, McMullen MF, Ward KR, Bang J, Xiao J, Siegel SJ. EEG biomarkers of target engagement, therapeutic effect, and disease process. Ann N Y Acad Sci. 2015;1344:12–26. [PubMed] [Google Scholar]
34. Thoma RJ, Hanlon FM, Moses SN, Ricker D, Huang M, Edgar C, et al. M50 sensory gating predicts negative symptoms in schizophrenia. Schizophr Res. 2005;73:311–8. [PubMed] [Google Scholar]
35. Brockhaus-Dumke A, Schultze-Lutter F, Mueller R, Tendolkar I, Bechdolf A, Pukrop R, et al. Sensory gating in schizophrenia: P50 and N100 gating in antipsychotic-free subjects at risk, first-episode, and chronic patients. Biol Psychiatry. 2008;64:376–84. [PubMed] [Google Scholar]
Sensory gating in schizophrenia: P50 and N100 gating in antipsychotic-free subjects at risk, first-episode, and chronic patients. Biol Psychiatry. 2008;64:376–84. [PubMed] [Google Scholar]
36. Ribeyre JM, Lesieur P, Varoquaux O, Dollfus S, Pays M, Petit M. A comparison of plasma homovanillic acid in the deficit and nondeficit subtypes of schizophrenia. Biol Psychiatry. 1994;36:230–6. [PubMed] [Google Scholar]
37. Toda M, Abi-Dargham A. Dopamine hypothesis of schizophrenia: Making sense of it all. Curr Psychiatry Rep. 2007;9:329–36. [PubMed] [Google Scholar]
38. Siris SG, Bermanzohn PC, Gonzalez A, Mason SE, White CV, Shuwall MA. The use of antidepressants for negative symptoms in a subset of schizophrenic patients. Psychopharmacol Bull. 1991;27:331–5. [PubMed] [Google Scholar]
39. Yoshimura R, Hori H, Katsuki A, Atake K, Nakamura J. Serum levels of brain-derived neurotrophic factor (BDNF), proBDNF and plasma 3-methoxy-4-hydroxyphenylglycol levels in chronic schizophrenia.![]() Ann Gen Psychiatry. 2016;15:1. [PMC free article] [PubMed] [Google Scholar]
Ann Gen Psychiatry. 2016;15:1. [PMC free article] [PubMed] [Google Scholar]
40. Goff DC, Evins AE. Negative symptoms in schizophrenia: Neurobiological models and treatment response. Harv Rev Psychiatry. 1998;6:59–77. [PubMed] [Google Scholar]
41. Fawzi MH, Fawzi MM, Fawzi MM, Said NS. C-reactive protein serum level in drug-free male Egyptian patients with schizophrenia. Psychiatry Res. 2011;190:91–7. [PubMed] [Google Scholar]
42. Prasad KM, Eack SM, Goradia D, Pancholi KM, Keshavan MS, Yolken RH, et al. Progressive gray matter loss and changes in cognitive functioning associated with exposure to herpes simplex virus 1 in schizophrenia: A longitudinal study. Am J Psychiatry. 2011;168:822–30. [PMC free article] [PubMed] [Google Scholar]
43. Goff DC. D-cycloserine in Schizophrenia: New strategies for improving clinical outcomes by enhancing plasticity. Curr Neuropharmacol. 2017;15:21–34. [PMC free article] [PubMed] [Google Scholar]
44. Esterberg ML, Trotman HD, Holtzman C, Compton MT, Walker EF. The impact of a family history of psychosis on age-at-onset and positive and negative symptoms of schizophrenia: A meta-analysis. Schizophr Res. 2010;120:121–30. [PubMed] [Google Scholar]
The impact of a family history of psychosis on age-at-onset and positive and negative symptoms of schizophrenia: A meta-analysis. Schizophr Res. 2010;120:121–30. [PubMed] [Google Scholar]
45. Potkin SG, Macciardi F, Guffanti G, Fallon JH, Wang Q, Turner JA, et al. Identifying gene regulatory networks in schizophrenia. Neuroimage. 2010;53:839–47. [PMC free article] [PubMed] [Google Scholar]
46. Zai G, Robbins TW, Sahakian BJ, Kennedy JL. A review of molecular genetic studies of neurocognitive deficits in schizophrenia. Neurosci Biobehav Rev. 2017;72:50–67. [PubMed] [Google Scholar]
47. Green MJ, Cairns MJ, Wu J, Dragovic M, Jablensky A, Tooney PA, et al. Genome-wide supported variant MIR137 and severe negative symptoms predict membership of an impaired cognitive subtype of schizophrenia. Mol Psychiatry. 2013;18:774–80. [PubMed] [Google Scholar]
48. Bousman CA, Glatt SJ, Chandler SD, Lohr J, Kremen WS, Tsuang MT, et al. Negative symptoms of psychosis correlate with gene expression of the Wnt/ß-catenin signaling pathway in peripheral blood. Psychiatry J. 2013;2013:852930. [PMC free article] [PubMed] [Google Scholar]
Psychiatry J. 2013;2013:852930. [PMC free article] [PubMed] [Google Scholar]
49. Harvey PD, Koren D, Reichenberg A, Bowie CR. Negative symptoms and cognitive deficits: What is the nature of their relationship? Schizophr Bull. 2006;32:250–8. [PMC free article] [PubMed] [Google Scholar]
50. Heerey EA, Gold JM. Patients with schizophrenia demonstrate dissociation between affective experience and motivated behavior. J Abnorm Psychol. 2007;116:268–78. [PubMed] [Google Scholar]
51. Shallice T. From Neuropsychology to Mental Structure. New York: Cambridge University Press; 1988. [Google Scholar]
52. Heerey EA, Robinson BM, McMahon RP, Gold JM. Delay discounting in schizophrenia. Cogn Neuropsychiatry. 2007;12:213–21. [PMC free article] [PubMed] [Google Scholar]
53. Carpenter WT, Jr, Heinrichs DW, Alphs LD. Treatment of negative symptoms. Schizophr Bull. 1985;11:440–52. [PubMed] [Google Scholar]
54. Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet. 2013;382:951–62. [PubMed] [Google Scholar]
Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet. 2013;382:951–62. [PubMed] [Google Scholar]
55. Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, et al. Randomized controlled trial of the effect on quality of life of second- vs. first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1) Arch Gen Psychiatry. 2006;63:1079–87. [PubMed] [Google Scholar]
56. Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull. 2010;36:71–93. [PMC free article] [PubMed] [Google Scholar]
57. Singh SP, Singh V, Kar N, Chan K. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: Meta-analysis. Br J Psychiatry. 2010;197:174–9. [PubMed] [Google Scholar]
58. Lindenmayer JP, Nasrallah H, Pucci M, James S, Citrome L. A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities. Schizophr Res. 2013;147:241–52. [PubMed] [Google Scholar]
Lindenmayer JP, Nasrallah H, Pucci M, James S, Citrome L. A systematic review of psychostimulant treatment of negative symptoms of schizophrenia: Challenges and therapeutic opportunities. Schizophr Res. 2013;147:241–52. [PubMed] [Google Scholar]
59. Arango C, Garibaldi G, Marder SR. Pharmacological approaches to treating negative symptoms: A review of clinical trials. Schizophr Res. 2013;150:346–52. [PubMed] [Google Scholar]
60. Umbricht D, Martin-Facklam M, Pizzagalli F, Youssef E, Yoo K, Doerflinger E, et al. Glycine transporter type 1 (GLYT1) inhibitor RG1678: Results of the proof-of-concept study for the treatment of negative symptoms in schizophrenia. Schizophr Bull. 2011;37(Suppl 1):324. [Google Scholar]
61. Freedman R, Olincy A, Buchanan RW, Harris JG, Gold JM, Johnson L, et al. Initial phase 2 trial of a nicotinic agonist in schizophrenia. Am J Psychiatry. 2008;165:1040–7. [PMC free article] [PubMed] [Google Scholar]
62. Liu F, Guo X, Wu R, Ou J, Zheng Y, Zhang B, et al. Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: A double blind, randomized, controlled trial. Schizophr Res. 2014;153:169–76. [PubMed] [Google Scholar]
Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: A double blind, randomized, controlled trial. Schizophr Res. 2014;153:169–76. [PubMed] [Google Scholar]
63. Shi C, Yu X, Cheung EF, Shum DH, Chan RC. Revisiting the therapeutic effect of rTMS on negative symptoms in schizophrenia: A meta-analysis. Psychiatry Res. 2014;215:505–13. [PMC free article] [PubMed] [Google Scholar]
64. Melle I, Larsen TK, Haahr U, Friis S, Johannesen JO, Opjordsmoen S, et al. Prevention of negative symptom psychopathologies in first-episode schizophrenia: Two-year effects of reducing the duration of untreated psychosis. Arch Gen Psychiatry. 2008;65:634–40. [PubMed] [Google Scholar]
65. NICE National Clinical Guideline Number 82: Schizophrenia. National Institute for Health and Clinical Excellence. 2009. [Last accessed on 2013 Oct 09]. Available from: http://www.nice.org.uk/CG82fullguideline .
66. Seruya BB. The effects of training on body-size estimation of schizophrenics. Dissertation Abstr Int. 1977;38:1421B. [Google Scholar]
Dissertation Abstr Int. 1977;38:1421B. [Google Scholar]
67. Müller N, Krause D, Dehning S, Musil R, Schennach-Wolff R, Obermeier M, et al. Celecoxib treatment in an early stage of schizophrenia: Results of a randomized, double-blind, placebo-controlled trial of celecoxib augmentation of amisulpride treatment. Schizophr Res. 2010;121:118–24. [PubMed] [Google Scholar]
What is Avolition and Can It Be Treated?
From time to time, getting things done may be challenging. With avolition, this difficulty may become persistent and distressing.
Motivation can ebb and flow. Whether it’s paying the bills or cleaning up dishes, it’s natural to drag your feet on occasion. Then there’s avolition, a core symptom of several mental health conditions, which is more than just a lack of motivation.
If you constantly feel you want to complete a task, but do not have the emotional bandwidth or the physical ability to do so, you may be experiencing avolition.
Avolition may feel paralyzing, and it may be a challenge to overcome it by reason, logic, or willpower alone.
But lifestyle adjustments, like therapy or medications, can help you overcome avolition.
Avolition is a term used to describe a significant or severe lack of motivation or a pronounced inability to complete purposeful tasks. It is a behavioral symptom rather than a mental health condition.
Avolition can make it hard to get things done even if there will be consequences, like losing your job or falling behind on bills.
Research shows that even when presented with an award, those living with conditions that present with avolition may not be able to complete a task.
For some, it can be so overpowering that it’s hard to stay on top of your health or keep up your personal hygiene or appearance.
You may not even be aware that it’s happening to you until a loved one points it out.
It’s important to note that avolition is different from procrastination, which is looking for distractions in order to put off something until a later time.
Avolition looks different for everyone. It can affect multiple areas of your life, and it’s not about willingness or laziness.
It can affect multiple areas of your life, and it’s not about willingness or laziness.
At home
- lying in bed for hours
- allowing dishes or trash to pile up
- skipping showers or brushing your teeth
- experiencing difficulty with putting things back where they belong
- struggling to throw away empty boxes
- finding it difficult to meet deadlines, like keeping medical appointments or filing taxes
- watching a whole day pass by, without much getting done
At work
- difficulty starting projects
- trouble completing tasks
- challenges organizing work station
- disjointed or disconnected in conversations
- little enthusiasm or “zest” for work
In relationships
- feeling detached and uninterested
- skipping usual social activities
- withdrawing from social contact
- ignoring texts, phone calls, and emails
- experiencing challenges with making eye contact
- having limited or halted speech with others
Avolition is considered a symptom rather than a mental health condition on its own.
It is a common symptom for people living with:
- schizophrenia
- depression
- bipolar disorder
This does not mean that everyone experiencing avolition has any of these mental health conditions. Only a health professional will be able to reach an accurate diagnosis.
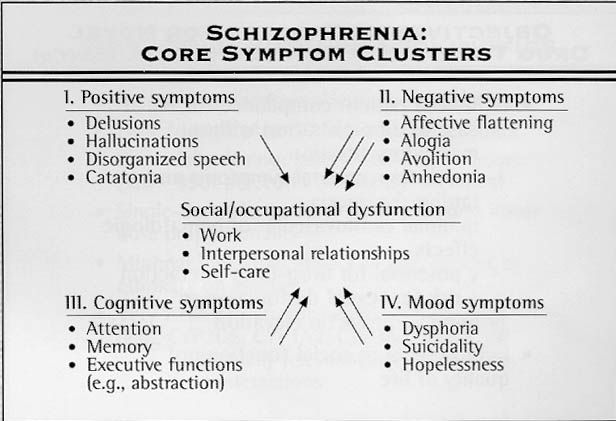
When you live with schizophrenia, your symptoms usually fall into two categories: positive or negative.
“Positive” refers to a symptom that is not present in those without schizophrenia, like hallucinations, paranoia, or delusions.
A “negative” symptom is a lack of a typical emotion, behavior, or thought. Avolition — as a lack of usual motivation — falls under the negative symptom category.
Research shows that 60% of those with schizophrenia experience negative symptoms, which includes avolition.
Avolition often coincides with similar symptoms. These include:
- Aboulia is the inability to make decisions or set goals. It’s a lack of will, rather than a lack of motivation.
It’s considered a more severe form of apathy.
- Alogia is the inability to speak.
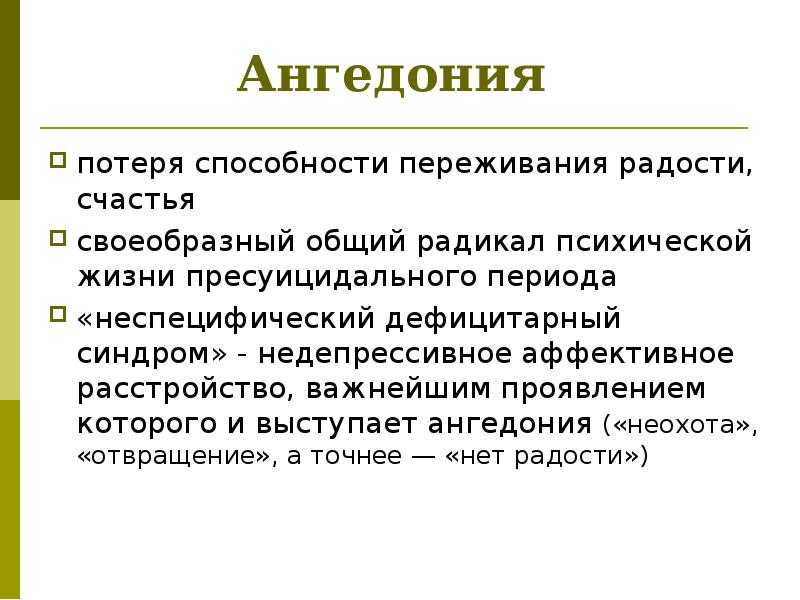
- Anhedonia is the inability to experience pleasure, which can lead to a lack of motivation.
- Asociality is a disinterest in being social.
All of these symptoms combined may make it difficult to complete everyday tasks.
While most associated with schizophrenia, avolition can also be associated with:
- bipolar disorder
- depression
- post-traumatic stress disorder (PTSD)
- premenstrual dysphoric disorder
- traumatic brain injury
- Alzheimer’s disease
Avolition can also be caused by a lack of mental stimulation or solitary confinement, such as the experiences of those who are incarcerated, especially when they’re incarcerated for a long time.
Avolition is often confused with apathy or laziness, which can be a facet of your personality. However, these traits are considered milder and may not point to a mental health condition.
With apathy and laziness, people are more likely to change their behaviors if a consequence is present.
With avolution, research shows this may not make a difference. That is part of what differentiates it as a symptom of a condition, not just a personality trait.
Researchers still don’t know why some people develop avolition, while others don’t.
Some studies suggest that avolition has to do with structural abnormalities in the key areas of the brain that manage motivation and reward, specifically in those with schizophrenia.
Some contributing factors may include:
- genetics
- brain development
- neurochemicals
- pregnancy or childbirth complications
Avolition is typically addressed as part of a mental health condition. Depending on what this condition is, treatments may vary. In general, the earlier you start treatment, the better you may feel.
Treatment for conditions related to avolition usually includes a combination of psychotherapy, medications, and lifestyle adjustments.
Research shows that cognitive behavioral therapy (CBT) may help you strengthen tools to carry out daily activities and develop social skills to stay connected with loved ones.
MedicationsAntipsychotic medications are usually prescribed for schizophrenia. Some, like aripiprazole (Abilify), may help with avolition.
Others include:
- Brexpiprazole (Rexulti)
- Cariprazine (Vraylar)
- Clozapine (Clozaril)
- Haloperidol (Haldol)
- Iloperidone (Fanapt)
- Olanzapine (Zyprexa)
- Risperidone (Risperdal)
- Quetiapine (Seroquel)
- Ziprasidone (Geodon)
Sometimes, medication can make avolition worse. It may also be hard to keep track of taking your medications.
You may want to ask your doctor if injections are available. You may be able to come in for a shot every 2 weeks, every month, or once a quarter.
Brain stimulation therapiesIf medications do not help with treatment, your doctor may recommend electroconvulsive therapy (ECT).
While under anesthesia, a specialist will use electrodes. These are placed on your scalp and send controlled electrical currents through your brain, according to the National Alliance on Mental Illness (NAMI).
As an alternative, research shows that intermittent theta burst stimulation (iTBS) may be a promising treatment for those with avolition, anhedonia, and blunted affect. This includes magnetic stimulation over the front of your brain (prefrontal cortex).
Self-care strategiesAs part of a healthy, balanced lifestyle, there are also several science-backed lifestyle adjustments to help improve your overall quality of life. These include:
- diet of nutrient-rich, unprocessed foods
- 7 to 9 hours of sleep every night
- reflective activities, like journaling
- talking or spending time with loved ones
- spending an hour a day in nature
- a mindfulness practice, like meditation
You may want to consider talking with family and friends about avolition so they understand better what you’re experiencing.
It may help if you or your loved ones create a schedule or list of important activities, like chores, medications, personal hygiene, or mealtimes. Apps like Todoist may assist you.
Avolition can affect every area of your life, from personal relationships to work, classes, home life, and other activities.
Everyday responsibilities, like washing the dishes or taking out the trash, may feel downright impossible.
Know that this is not your fault or a lack of willpower. Avolition, and the mental health conditions associated with it, are complex.
Avolition is a treatable symptom, though. A combination of therapy, medication, and lifestyle adjustments may help treat some of the conditions associated with avolition.
These resources could help:
- American Psychiatric Association’s Find a Psychiatrist tool
- American Psychological Association’s Find a Psychologist tool
- Asian Mental Health Collective’s therapist directory
- Association of Black Psychologists’ Find a Psychologist tool
- National Alliance on Mental Illness Helplines and Support Tools
- National Institute of Mental Health’s Helpline Directory
- National Queer and Trans Therapists of Color Network
- Inclusive Therapists
causes, symptoms, treatment in Moscow, making an appointment and consultation
Contents↓[show]
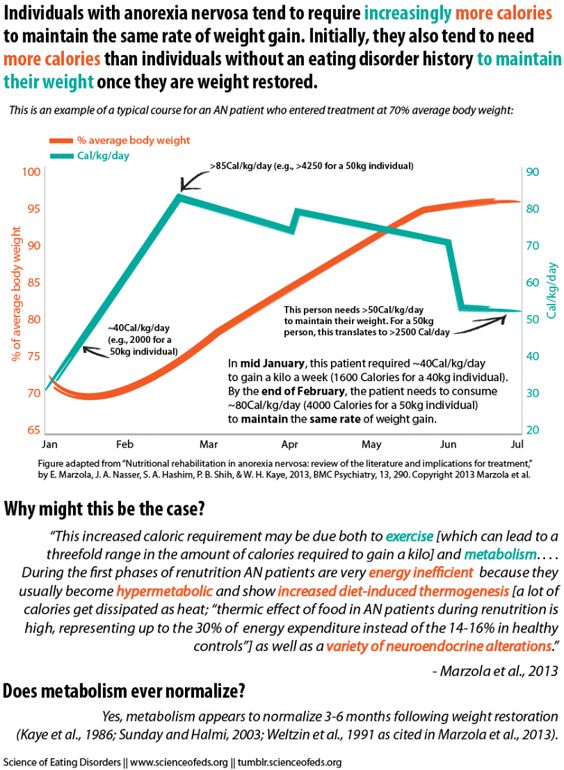
Anhedonia is a mental state of the patient, which is often found in mental disorders.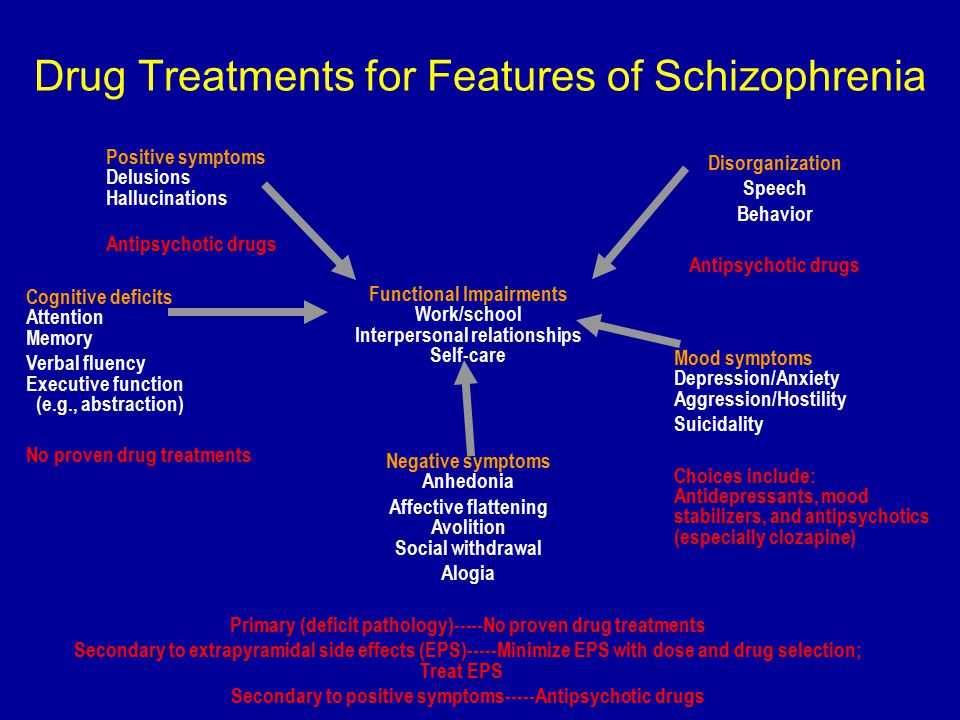 Anhedonia is characterized by a complete or partial loss of the ability to experience pleasure. The pathological state of the psyche leads to a loss of motivation to do what you love, hobbies, sports, music, interest in sexual life, social contacts is lost. Anhedonia is a symptom of various mental disorders such as: schizophrenia, depression, personality disorder, Parkinson's disease, post-traumatic stress and others. Anhedonia is most often diagnosed in patients with depressive disorders. nine0003
Anhedonia is characterized by a complete or partial loss of the ability to experience pleasure. The pathological state of the psyche leads to a loss of motivation to do what you love, hobbies, sports, music, interest in sexual life, social contacts is lost. Anhedonia is a symptom of various mental disorders such as: schizophrenia, depression, personality disorder, Parkinson's disease, post-traumatic stress and others. Anhedonia is most often diagnosed in patients with depressive disorders. nine0003
Anhedonia is being treated at the Yusupov hospital. The neurology clinic of the Yusupov Hospital specializes in the treatment of Parkinson's disease, various types of depressive disorders, Alzheimer's disease, dementia and other neurological diseases. The Yusupov Hospital uses innovative medicines certified in Russia, modern methods for diagnosing and treating depression and various mental disorders. The reasons for the development of anhedonia can be psychological and physiological. In the brain, “happiness hormones” (serotonin and dopamine) cease to be produced in the right amount, norepinephrine and adrenaline, “stress hormones,” are produced in large quantities.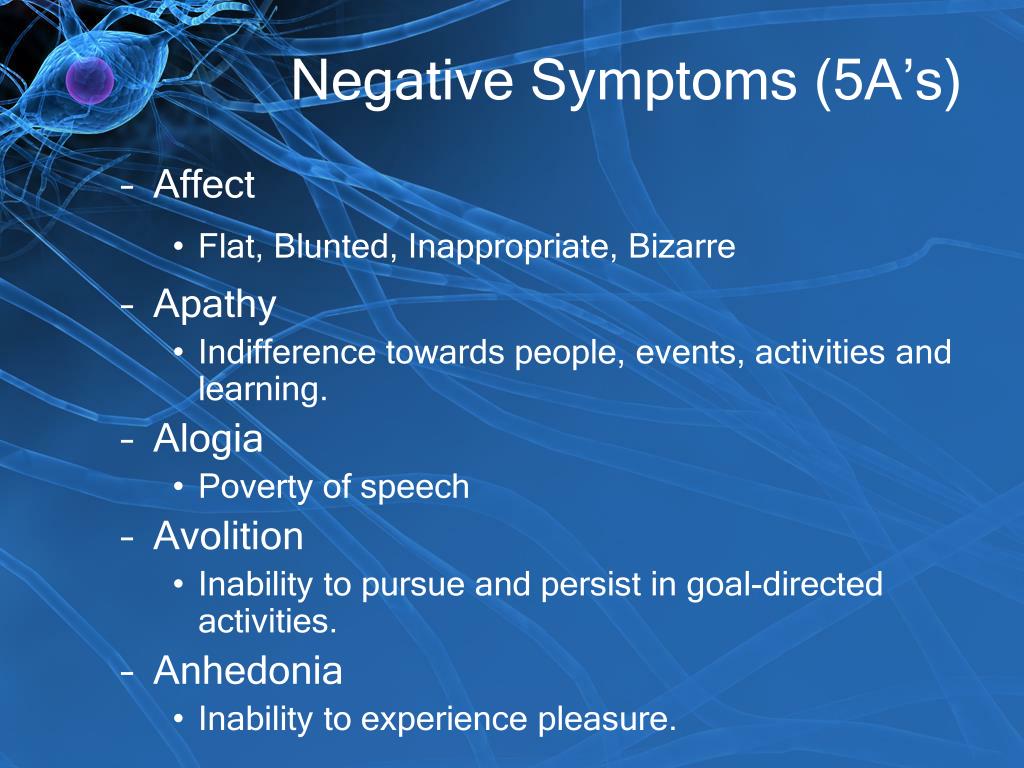 nine0003
nine0003
Anhedonia can develop as a result of prolonged stress, brain diseases, after a brain injury, severe viral diseases and infections. Anhedonia accompanies various mental disorders - depression, schizophrenia, bipolar disorder, paranoia. The development of anhedonia is promoted by psychological reasons - pessimism, workaholism, nervous shocks. Characteristic features of the patient, busy work schedule, chronic stress do not allow to see the world in all colors, make life monotonous, dull, joyless. nine0004
CAC anhedonia
Different tests measure anhedonia differently. Anhedonia as a symptom is not included in the PANSS (Positive and Negative Syndrome Test), the SANS test does not distinguish between anticipatory and consummatory anhedonia, the symptom of anhedonia is considered together with asociality. In the BNSS scale, the symptom is considered as three separate components, a general analysis of the patient's behavior is carried out according to his demographic indicators. In the GAINS scale, anhedonia is defined by five points, there is no item on physical pleasure. Other tests based on self-assessment have been created that serve to determine anhedonia in any mental disorder:
In the GAINS scale, anhedonia is defined by five points, there is no item on physical pleasure. Other tests based on self-assessment have been created that serve to determine anhedonia in any mental disorder:
- SAS (SAS) - a scale for determining social anhedonia.
- PAS - physical anhedonia scale.
- TEPS - Temporal Pleasure Experience Scale.
- ACIPS - Anticipatory and Consumatory Interpersonal Pleasure Scale.
Inability to get joy and pleasure from life due to psycho-emotional clamps, loss of interest in people, lack of attention and love for relatives, social isolation, rupture of social contacts - this is social anhedonia. nine0003
Anhedonia: how to treat
Several types of anhedonia are described:
- Social. Social anhedonia is manifested by a loss of interest in people, including close people. Social contacts are broken, the quality of life decreases, the patient has no goals in life.
- Physical.
 Physical anhedonia is characterized by a violation of sexual feelings, a decrease in the desire for intimacy (orgasmic anhedonia), the patient is not attracted to tasty food, pleasant aromas. nine0019
Physical anhedonia is characterized by a violation of sexual feelings, a decrease in the desire for intimacy (orgasmic anhedonia), the patient is not attracted to tasty food, pleasant aromas. nine0019 - Intellectual and aesthetic. Anhedonia of this type is characterized by a lack of interest in hobbies, the patient stops doing his favorite activities, loses interest in books, music, television, loses interest in everything that pleased before.
There are a number of factors that influence the development of a mental disorder:
- Violation of neuroendocrine regulation. Lack or excess of neurotransmitters leads to a loss of feelings of joy and happiness.
- Traumatic injury. The negative impact of the injury can take several years to show.
- Age changes. With age, changes occur - the hormonal system is rebuilt, brain cells lose their adaptive properties, regeneration properties, all processes in the body proceed slowly, the structure of nerve fibers changes, cognitive properties and emotionality are disturbed.
Anhedonia often develops in people who are conscientious and responsible, people who are used to solving their problems themselves and do not accept outside help. Among workaholics, women are more likely to suffer from the disorder. This is due to hormonal fluctuations in the body of a woman. In some cases, anhedonia develops with the use of antipsychotics. Treatment of the disorder will be more effective when the patient's attitude is positive. There are a number of recommendations that should be followed in order to achieve a positive result:
- Sleep at least 7-8 hours a day.
- No more than 8 hours a day.
- Strict daily routine with observance of hours of work and rest.
- Daily outdoor walks.
- Complete nutrition.
- Sports, dancing.
- Watching positive programs and films.
- Concentration of attention on positive emotions.
If you cannot cope with the disorder on your own, you should contact a specialist - a psychotherapist.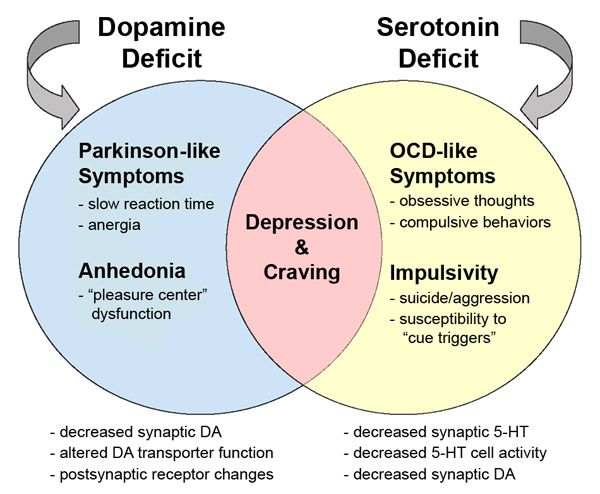 The disease is difficult to treat, the restoration of the level of “happiness hormones” is required. nine0004
The disease is difficult to treat, the restoration of the level of “happiness hormones” is required. nine0004
Paranoia and anhedonia: diagnosis and treatment
Paranoia is a mental disorder characterized by impaired cognitive functions, thinking, accompanied by obsessive-compulsive states. Paranoia is caused by brain disorders. Subject to paranoia are people with damage to the vessels of the brain, the elderly. Most often, paranoia accompanies diseases - Parkinson's disease, Alzheimer's disease, Huntington's disease, bad habits - alcohol, drugs, some medicines - can provoke the development of the disorder. Paranoia in some cases may be accompanied by depression with symptoms of anhedonia - loss of interest in life, the ability to enjoy. nine0003
The patient becomes distrustful, touchy, secretive, does not trust even the closest people. Unlike schizophrenics, the paranoid most often lacks the progression of negative symptoms, personality changes, hallucinations and illusions.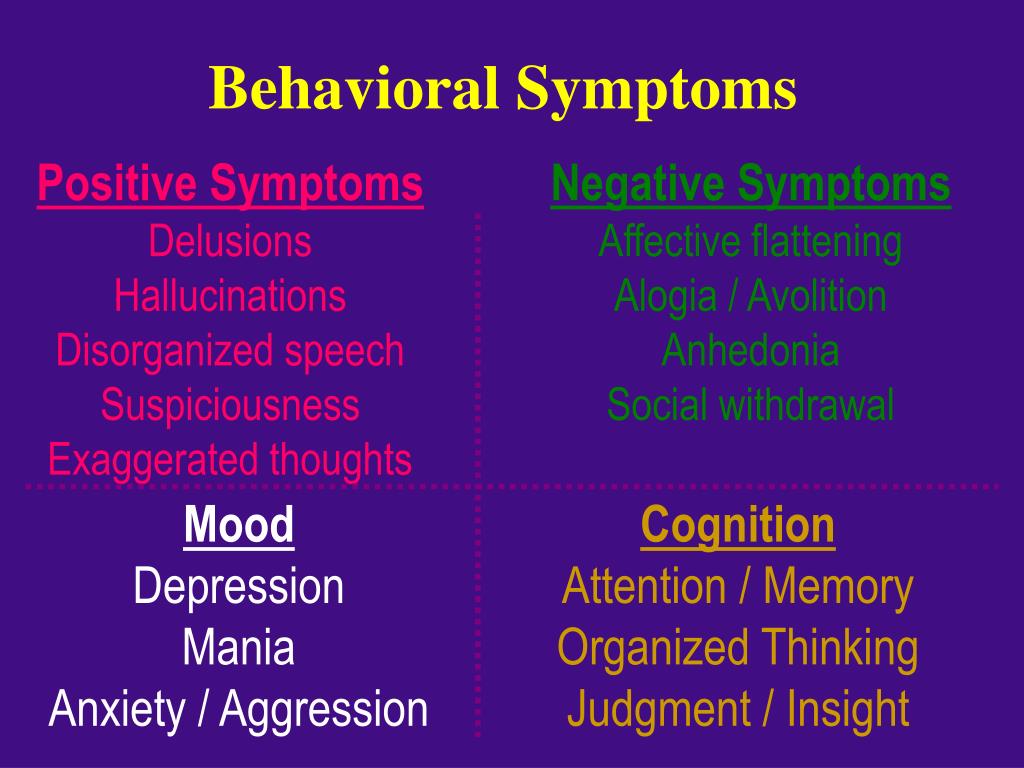 Paranoids are able to function normally in society, unlike schizophrenics. The patient's condition may worsen after a stressful situation, he becomes more suspicious, aggressive, loses social skills, breaks social ties, paranoid delusions increase. The patient is in conflict with other people, repetitive stressful situations worsen the condition. nine0003
Paranoids are able to function normally in society, unlike schizophrenics. The patient's condition may worsen after a stressful situation, he becomes more suspicious, aggressive, loses social skills, breaks social ties, paranoid delusions increase. The patient is in conflict with other people, repetitive stressful situations worsen the condition. nine0003
The development and course of anhedonia depends on the personality of the patient and the type of depressive disorder. An important role in the treatment of anhedonia is played by effective diagnosis and psychopathological analysis. If anhedonia is diagnosed, treatment can be done in specialized hospitals and clinics, medical centers, as well as in the Yusupov hospital. The Yusupov hospital is equipped with modern diagnostic equipment, the hospital includes a laboratory, a diagnostic center, various clinics, a rehabilitation center, and a hospital. You can make an appointment to see a doctor by calling the hospital. nine0003
What is avolition and how to deal with it?
Understanding freedom
“Persistence” is a term used to describe a lack of motivation or ability to perform tasks or activities that have an end in mind, such as paying bills or attending school activities.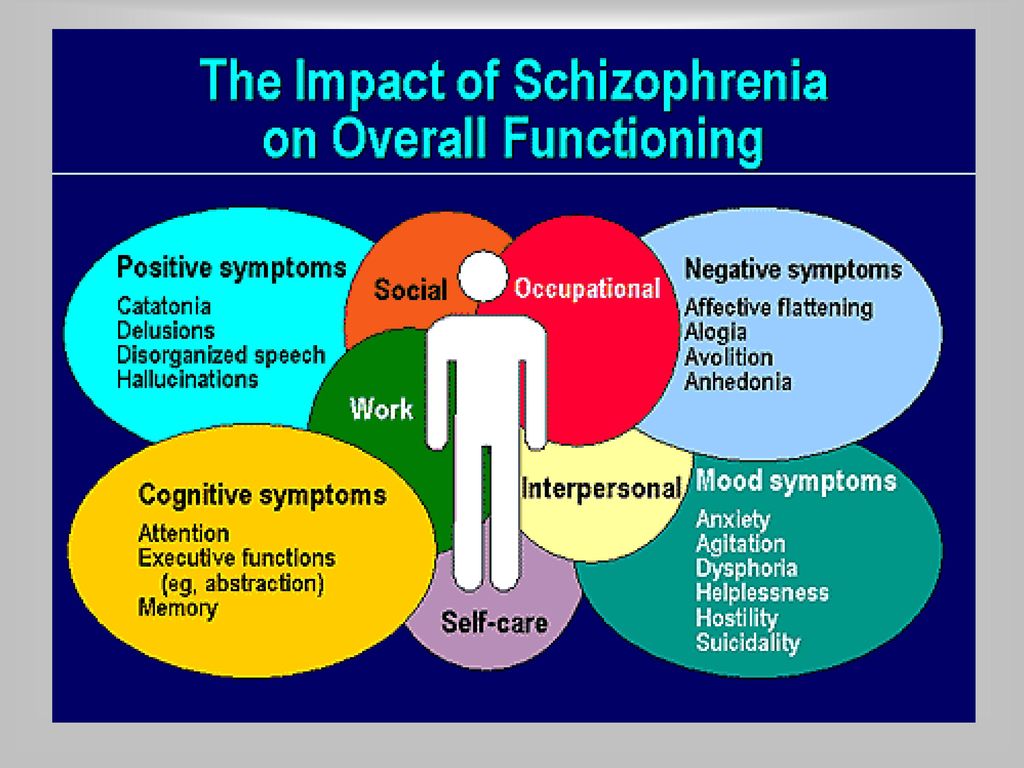
Abolition is most common in schizophrenia, depression and bipolar disorder.
In schizophrenia, the symptoms are divided into positive and negative. Most people have a combination of these two factors. Avolition is considered a negative symptom. nine0003
Negative symptoms reflect loss of ability to do or feel anything. Examples of avolia in schizophrenia would be an inability to take care of personal hygiene or participate in work or leisure activities.
Positive symptoms are behaviors or actions that are not commonly seen in people who do not have schizophrenia, although they may be present in other psychiatric disorders. Hallucinations, delusions, and disorganized speech are common positive symptoms. However, negative symptoms are often the first sign of schizophrenia, appearing before hallucinations or delusions. nine0003
Continue reading to learn more about the characteristics of evolution and how it can be controlled.
ADVERTISEMENT
Conventional Therapy - Done Online
Choose from BetterHelp's network of therapists for the symptoms of your disorder and stay connected by phone, video or chat. Plans start at $60 per week + an additional 20% off the first month.
Plans start at $60 per week + an additional 20% off the first month.
GET 20% OFF
A person experiencing evolution may withdraw from social contacts and normal activities. They are often unenthusiastic and take little pleasure in life. Their emotions may become dull and conversations may become incoherent. nine0003
Abolition is often mistaken for depression. This is more clearly identified and understood when the person also exhibits positive symptoms of schizophrenia. It is important to remember that a person with evolution does not avoid activities. They just don't have the ability to act.
Examples of failure
Evolution affects every aspect of daily life—personal relationships, home, and school.
A person with evolution may experience the following:
- does not make eye contact when talking or talking to someone
- limited or stopped speech
- stops attending events or meetings
- avoids making or receiving phone calls
- has trouble starting or completing projects
- not attending or enthusiastic about special occasions or events
- unable to book for an appointment, for example, with a doctor or a tax inspector
Avolation is not the same as laziness
Someone may assume that this is due to laziness or irresponsibility of a person.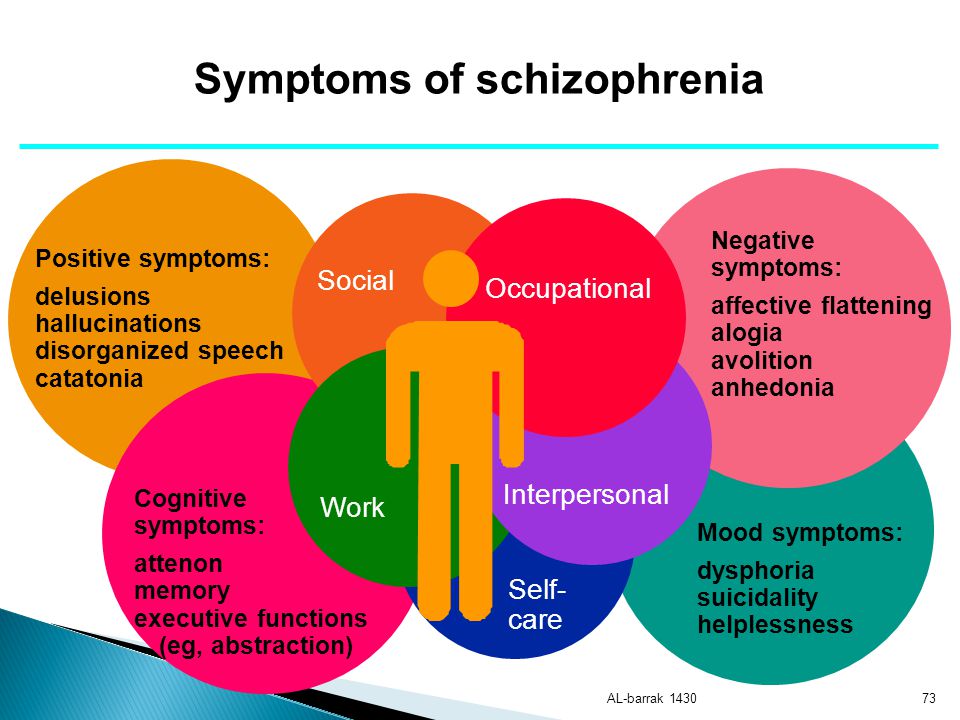 But people with evolution are not able to act. In a way, it is like the paralysis of apathy, or the inability to anticipate or experience the reward of completing a task. On the contrary, laziness can be considered an act of will of a person who does not suffer from a mental disorder. nine0003
But people with evolution are not able to act. In a way, it is like the paralysis of apathy, or the inability to anticipate or experience the reward of completing a task. On the contrary, laziness can be considered an act of will of a person who does not suffer from a mental disorder. nine0003
Avolition is one of the most common negative symptoms of schizophrenia. It is also seen in other psychiatric and neurological disorders.
It is not clear what causes schizophrenia, although the following may be involved:
- genetics
- brain development
- chemicals in the brain
- complications of pregnancy and childbirth . nine0003
When a person has two or more Reliable Source negative symptoms for more than 12 months, the Reliable Source was clinically stable, otherwise they are said to have deficiency schizophrenia syndrome. About 25 percent of people with schizophrenia have this syndrome.
People with deficient schizophrenia tend to have more severe negative symptoms that are more difficult to treat.
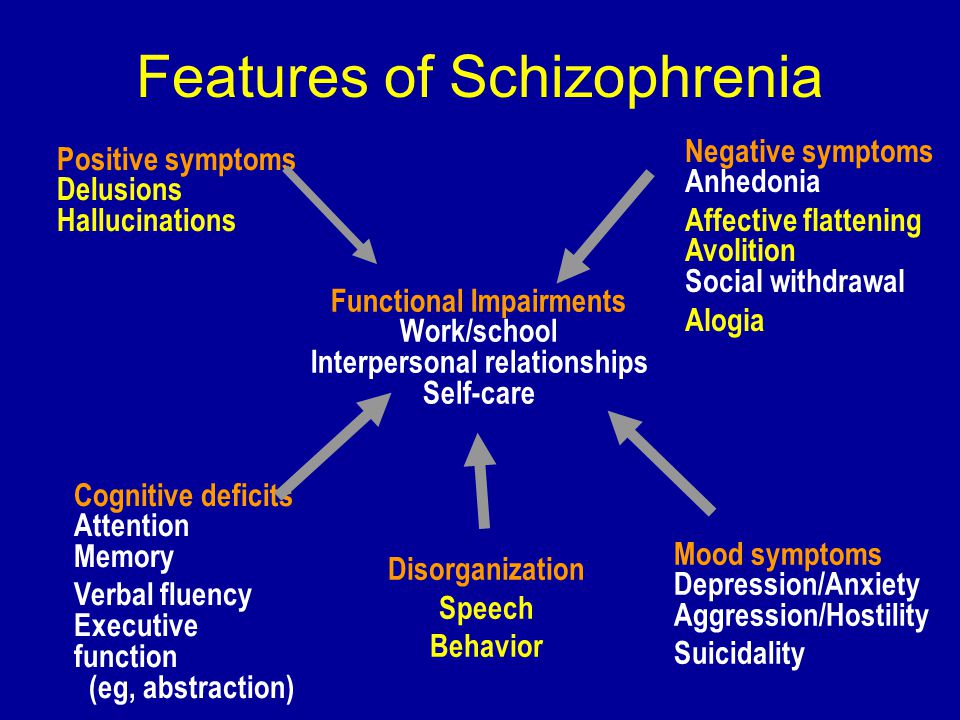 While positive symptoms such as delusions and hallucinations may seem more disturbing, negative symptoms tend to have a greater impact on a person's ability to function. nine0003
While positive symptoms such as delusions and hallucinations may seem more disturbing, negative symptoms tend to have a greater impact on a person's ability to function. nine0003 Other negative symptoms
Other negative symptoms of schizophrenia are similar to those of avolution. Mental health professionals often combine some of these into one symptom.
It is easy to see why, given how interrelated the following symptoms are:
Anhedonia: is the inability to experience pleasure or anticipate reward.
Affective dullness or flattening: when a person cannot show or express emotions, this is called dullness or flattening. The lack of emotional expression may be evident when the person speaks or by their body language. nine0003
Alogia: this refers to problems with speaking or continuing your part of the conversation. This may include refusing to ask or answer questions. People with alogia often have trouble forming thoughts and maintaining a conversation, especially when the speaker switches from one topic to another.

Attention impairment: Many people with schizophrenia have trouble concentrating. They may not be able to filter out unwanted noises and stimulation. Also memory problems are not uncommon. nine0003
Anosognosia: this refers to a lack of understanding or awareness often used to describe a person's inability to recognize that they have a mental illness. At least 50 percent of Reliable Sources of people with schizophrenia are unaware of their condition. Anosognosia is one of the main reasons many people with this condition do not take medication.
The negative symptoms of schizophrenia are usually more difficult to treat than the positive ones. And there is no gold standard for their treatment. nine0003
Treatment is usually most effective when it is started early, so it is important to start it when the disorder is first identified. It may take several weeks for the medicine to start working.
Treatment usually involves a combination of drugs and therapy.
Medications
Antipsychotics are most effective in treating positive symptoms of schizophrenia, including delusions and hallucinations. They are supposed to work by adjusting neurotransmitter levels in the brain. Neurotransmitters are chemicals that help brain cells communicate with each other. nine0003
Antipsychotics help four out of five people who take them. However, some antipsychotic medications can increase avolution and other negative symptoms.
General neuroleptics taken inward include:
- Klosapin (Klosaril)
- Risperidone (Risperdal)
- Kariprazin (Vnuylar)
- Aripprazole (Abilifi) 900 (Serokvelol)
Side effects are common and may include: - trembling
- slowness or lethargy
- abnormal movement of the tongue and jaw
- sexual problems
- Set up a schedule for them, including self-care, medication, meal times, bedtime, and other regular activities. Post it as a list or calendar in a place where it will be a reminder of readiness.
- Make sure your medications are taken correctly. Keep records for the doctor of any side effects and how the person reacts to the medication. nine0019
- All communications, especially instructions, must be clear and simple.
- Stay calm and encourage. Use gentle reminders, not whining.
- Be prepared for their condition to reach crisis proportions.
Many people have fewer side effects with newer antipsychotics such as clozapine and risperidone.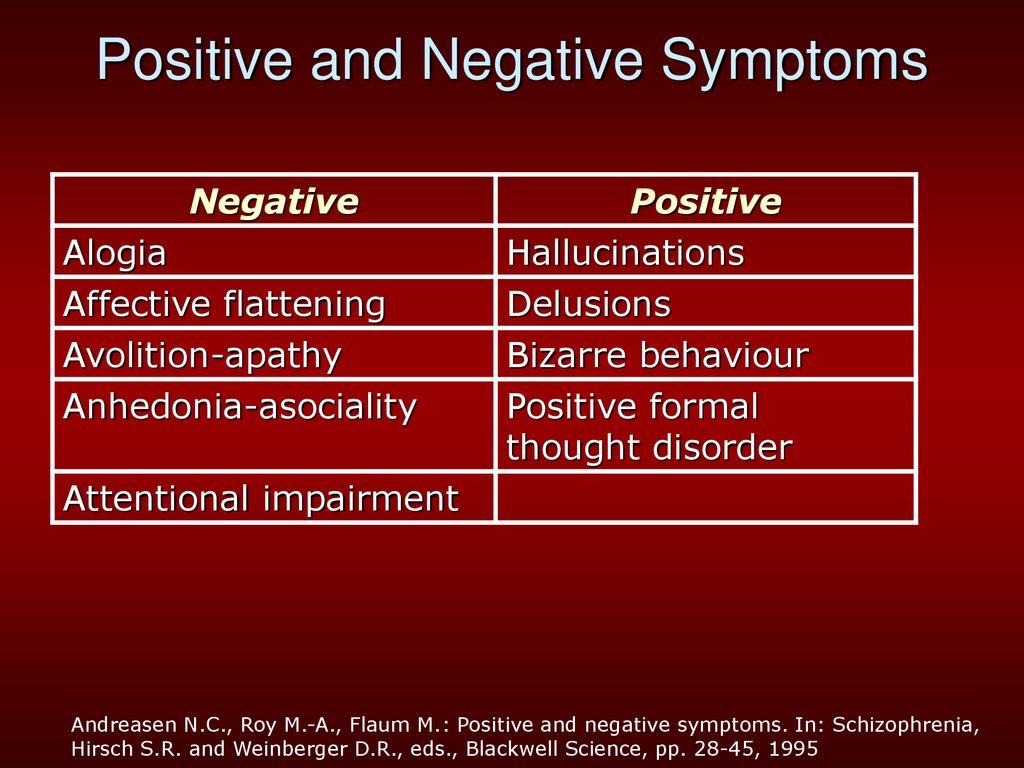 However, they may have elevated blood sugar, cholesterol, or triglycerides.
However, they may have elevated blood sugar, cholesterol, or triglycerides.
Some antipsychotics are given by injection every two weeks, four weeks, or four times a year. This may be helpful for people who forget to take their medications. nine0003
Antidepressants are sometimes prescribed together with antipsychotics.
Learn more: Depression drugs and side effects »
Therapy
Cognitive Behavioral Therapy, or Talking Therapy, and Cognitive Improvement Therapy can be very helpful in helping people acquire the skills they need for daily activities.
Electroconvulsive therapy may be recommended if antipsychotics are not effective. nine0003
Treatment can help control the symptoms of schizophrenia in many people, allowing them to lead independent, productive lives. For those who are not helped by treatment, mental health facilities can provide information about services to meet basic needs, such as housing, work, and health care.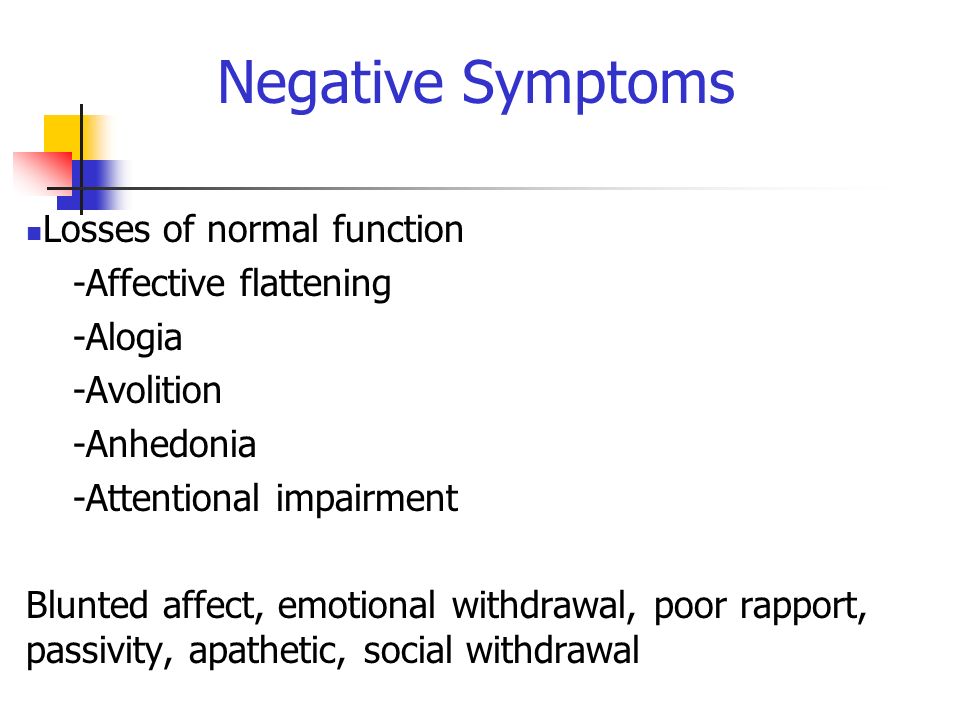
Caring for someone can be difficult for both you and the person you are caring for. It can be difficult to accept help, especially if it seems unnecessary. It can also be difficult to offer help when it doesn't seem to be appreciated. nine0003
It is important to be patient with yourself and with the person you are caring for. Together you will be able to overcome any obstacles you face.
Here are some other helpful approaches: