Am i paranoid schizophrenia
Schizophrenia Symptoms and Coping Tips
schizophrenia
Recognizing the signs of schizophrenia in yourself or a loved one can be frightening. But with the right treatment and self-help, you can manage the disorder and lead a fulfilling life.
What is schizophrenia or paranoid schizophrenia?
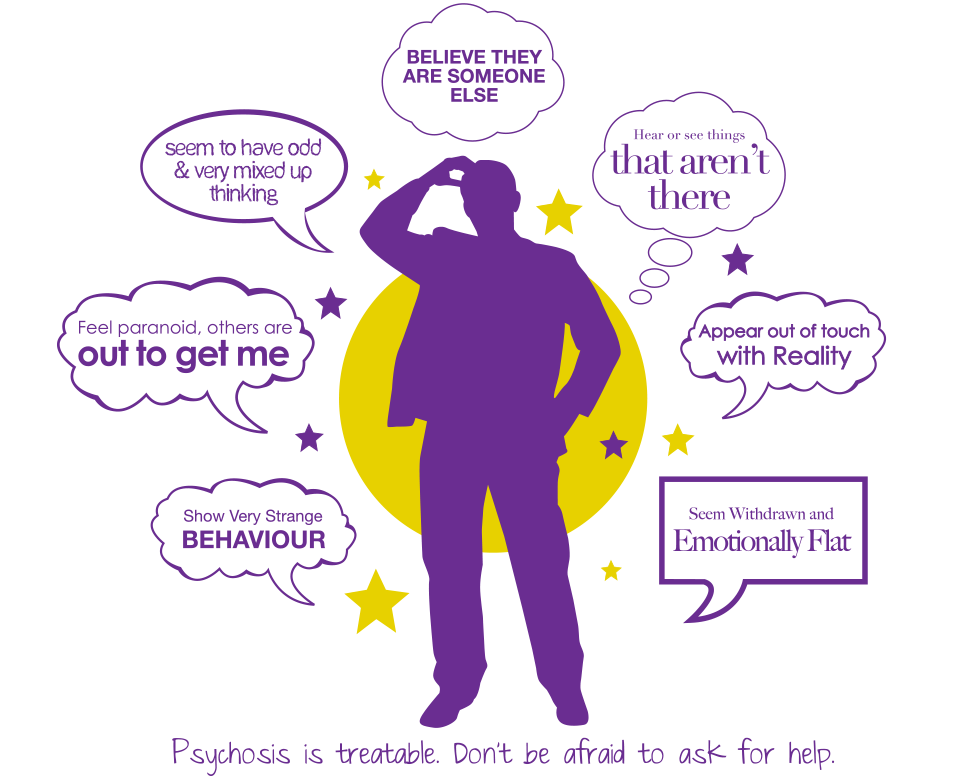
Schizophrenia is a challenging brain disorder that often makes it difficult to distinguish between what is real and unreal, to think clearly, manage emotions, relate to others, and function normally. It affects the way a person behaves, thinks, and sees the world.
The most common form is paranoid schizophrenia, or schizophrenia with paranoia as it's often called. People with paranoid schizophrenia have an altered perception of reality. They may see or hear things that don't exist, speak in confusing ways, believe that others are trying to harm them, or feel like they're being constantly watched. This can cause relationship problems, disrupt normal daily activities like bathing, eating, or running errands, and lead to alcohol and drug abuse in an attempt to self-medicate.
Many people with schizophrenia withdraw from the outside world, act out in confusion and fear, and are at an increased risk of attempting suicide, especially during psychotic episodes, periods of depression, and in the first six months after starting treatment.
Take any suicidal thoughts or talk very seriously…
If you or someone you care about is suicidal, call the National Suicide Prevention Lifeline in the U.S. at 1-800-273-TALK, visit IASP or Suicide.org to find a helpline in your country, or read Suicide Prevention.
While schizophrenia is a chronic disorder, many fears about the disorder are not based in reality. Most people with schizophrenia get better over time, not worse. Treatment options are improving all the time and there are plenty of things you can do to manage the disorder.
Schizophrenia is often episodic, so periods of remission are ideal times to employ self-help strategies to limit the length and frequency of any future episodes. Along with the right support, medication, and therapy, many people with schizophrenia are able to manage their symptoms, function independently, and enjoy full, rewarding lives.
| Common misconceptions about schizophrenia |
| Myth: Schizophrenia refers to a “split personality” or multiple personalities.
Fact: Multiple personality disorder is a different and much less common disorder than schizophrenia. People with schizophrenia do not have split personalities. Rather, they are “split off” from reality. |
| Myth: Schizophrenia is a rare condition.
Fact: Schizophrenia is not rare; the lifetime risk of developing schizophrenia is widely accepted to be around 1 in 100. |
| Myth: People with schizophrenia are dangerous.
Fact: Although the delusional thoughts and hallucinations of schizophrenia sometimes lead to violent behavior, most people with schizophrenia are neither violent nor a danger to others. |
Myth: People with schizophrenia can't be helped.
Fact: While long-term treatment may be required, the outlook for schizophrenia is far from hopeless. When treated properly, many people with schizophrenia are able to enjoy fulfilling, productive lives. |
In some people, schizophrenia appears suddenly and without warning. But for most, it comes on slowly, with subtle warning signs and a gradual decline in functioning, long before the first severe episode. Often, friends or family members will know early on that something is wrong, without knowing exactly what.
In this early phase of schizophrenia, you may seem eccentric, unmotivated, emotionless, and reclusive to others. You may start to isolate yourself, begin neglecting your appearance, say peculiar things, and show a general indifference to life. You may abandon hobbies and activities, and your performance at work or school can deteriorate.
The most common early warning signs include:
- Depression, social withdrawal
- Hostility or suspiciousness, extreme reaction to criticism
- Deterioration of personal hygiene
- Flat, expressionless gaze
- Inability to cry or express joy or inappropriate laughter or crying
- Oversleeping or insomnia; forgetful, unable to concentrate
- Odd or irrational statements; strange use of words or way of speaking
While these warning signs can result from a number of problems—not just schizophrenia—they are cause for concern.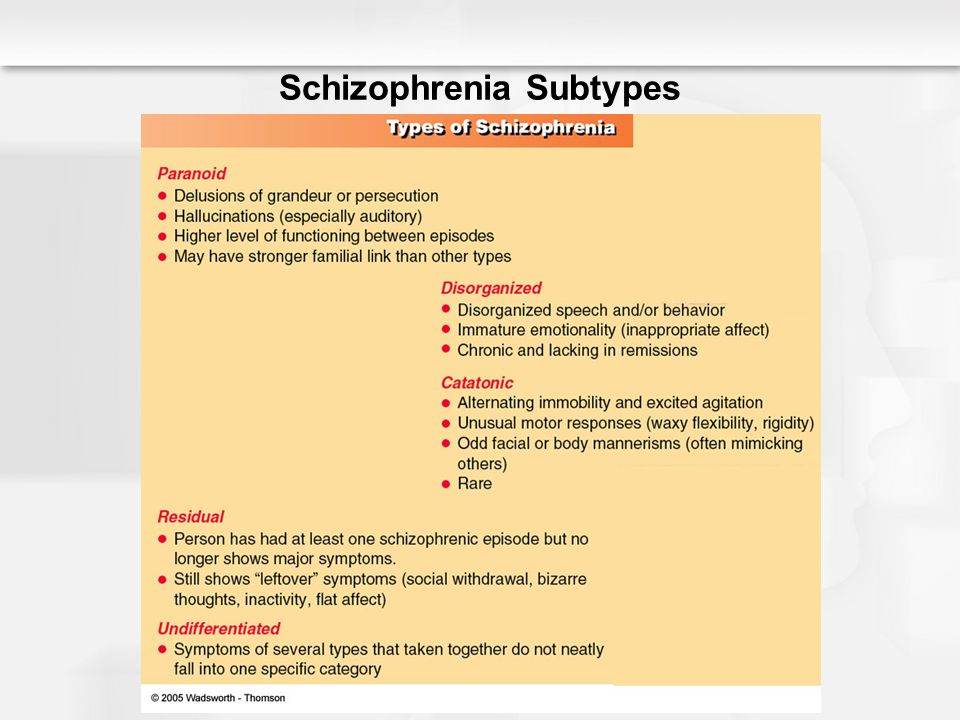 When out-of-the-ordinary behavior is causing problems in your life or the life of a loved one, seek medical advice. If schizophrenia or another mental problem is the cause, getting treatment early will help.
When out-of-the-ordinary behavior is causing problems in your life or the life of a loved one, seek medical advice. If schizophrenia or another mental problem is the cause, getting treatment early will help.
Affordable Online Therapy
Get professional help from BetterHelp's network of licensed therapists.
FIND A THERAPIST NOW
HelpGuide is reader supported. We may receive a commission if you sign up for BetterHelp through the provided link. Learn more.
Symptoms
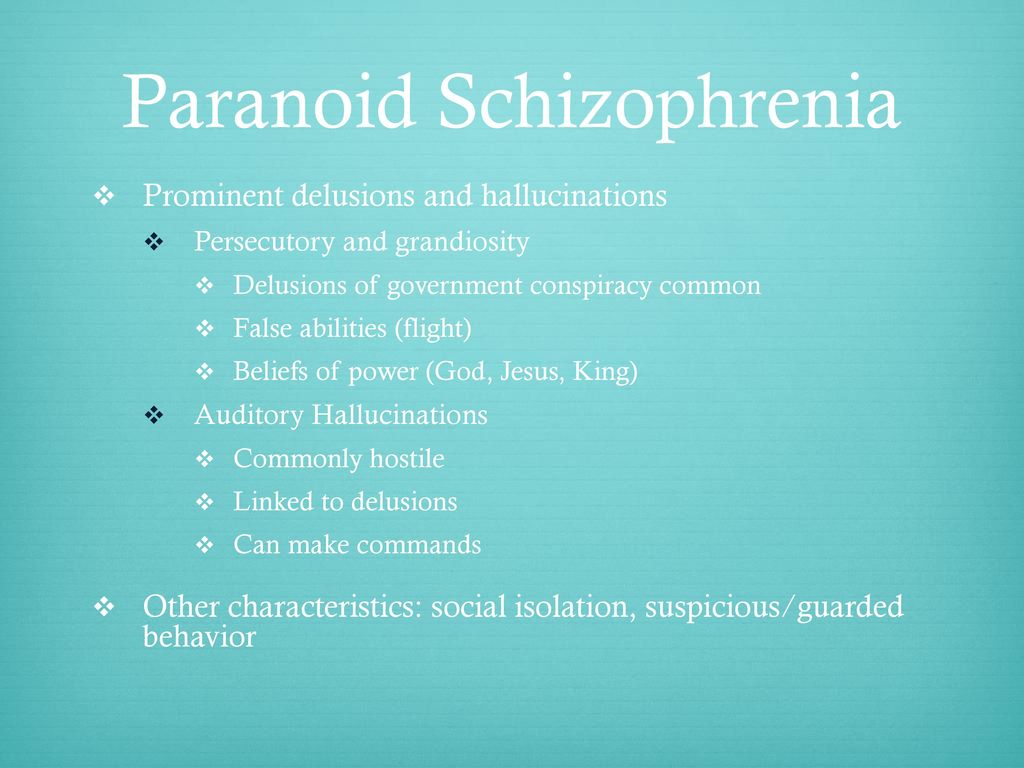
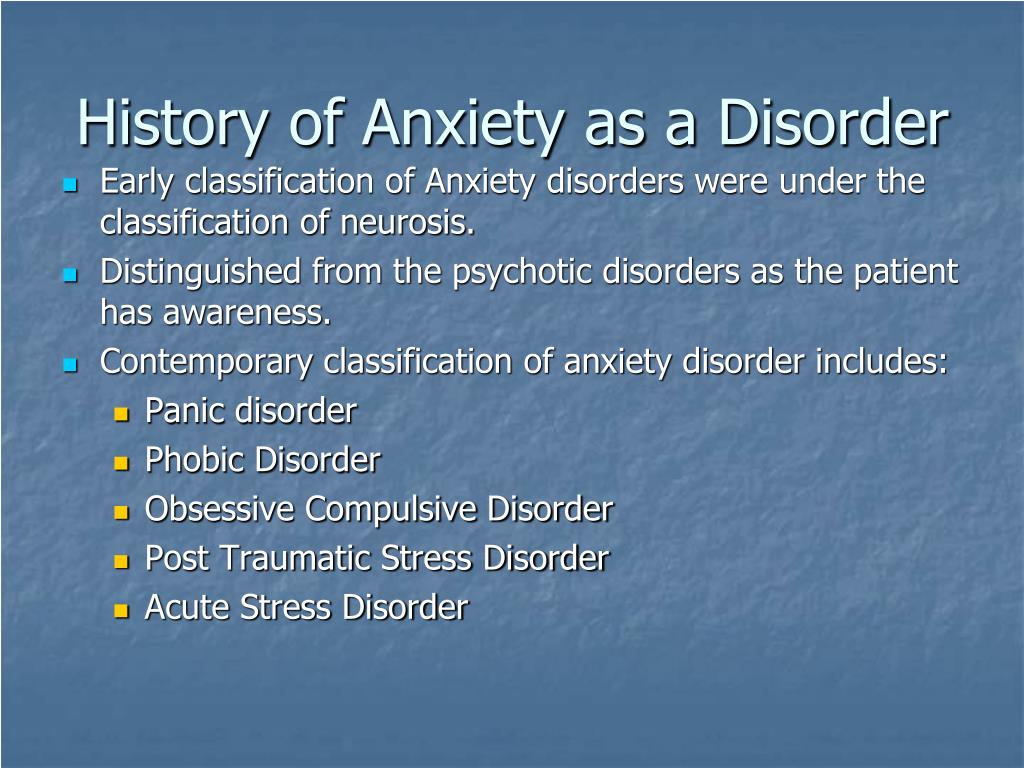
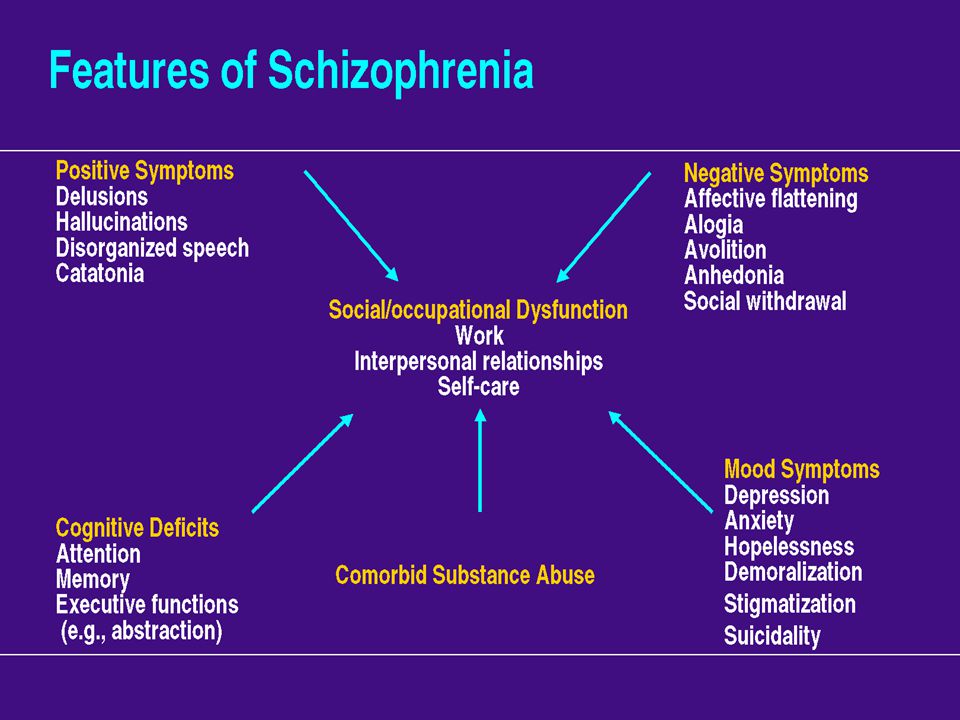
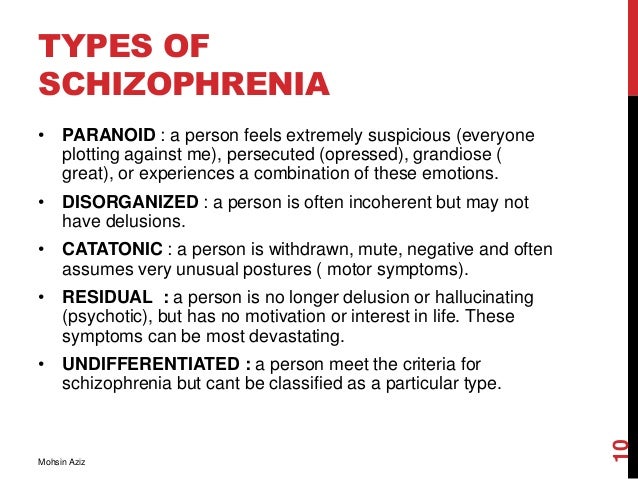
There are five types of symptoms characteristic of schizophrenia: delusions, hallucinations, disorganized speech, disorganized behavior, and the so-called “negative” symptoms. However, the symptoms of schizophrenia vary dramatically from person to person, both in pattern and severity. Not every person with schizophrenia will have all the symptoms, and the symptoms of schizophrenia may also change over time.
Delusions
A delusion is a firmly-held idea that a person has despite clear and obvious evidence that it isn't true. Delusions are extremely common in schizophrenia, occurring in more than 90% of those who have the disorder. Often, these delusions involve illogical or bizarre ideas or fantasies, such as:
Delusions are extremely common in schizophrenia, occurring in more than 90% of those who have the disorder. Often, these delusions involve illogical or bizarre ideas or fantasies, such as:
Delusions of persecution – Belief that others, often a vague “they,” are out to get you. These harassing delusions often involve bizarre ideas and plots (e.g. “Martians are trying to poison me with radioactive particles delivered through my tap water”).
Delusions of reference – A neutral environmental event is believed to have a special and personal meaning. For example, you might believe a billboard or a person on TV is sending a message meant specifically for you.
Delusions of grandeur – Belief that you are a famous or important figure, such as Jesus Christ or Napoleon. Alternately, delusions of grandeur may involve the belief that you have unusual powers, such as the ability to fly.
Delusions of control – Belief that your thoughts or actions are being controlled by outside, alien forces. Common delusions of control include thought broadcasting (“My private thoughts are being transmitted to others”), thought insertion (“Someone is planting thoughts in my head”), and thought withdrawal (“The CIA is robbing me of my thoughts”).
Common delusions of control include thought broadcasting (“My private thoughts are being transmitted to others”), thought insertion (“Someone is planting thoughts in my head”), and thought withdrawal (“The CIA is robbing me of my thoughts”).
Hallucinations
Hallucinations are sounds or other sensations experienced as real when they exist only in your mind. While hallucinations can involve any of the five senses, auditory hallucinations (e.g. hearing voices or some other sound) are most common in schizophrenia. These often occur when you misinterpret your own inner self-talk as coming from an outside source.
Schizophrenic hallucinations are usually meaningful to you as the person experiencing them. Many times, the voices are those of someone you know, and usually they're critical, vulgar, or abusive. Visual hallucinations are also relatively common, while all hallucinations tend to be worse when you're alone.
Disorganized speech
Schizophrenia can cause you to have trouble concentrating and maintaining your train of thought, which may manifest itself in the way that you speak. You may respond to queries with an unrelated answer, start sentences with one topic and end somewhere completely different, speak incoherently, or say illogical things.
You may respond to queries with an unrelated answer, start sentences with one topic and end somewhere completely different, speak incoherently, or say illogical things.
Common signs of disorganized speech include:
Loose associations – Rapidly shifting from topic to topic, with no connection between one thought and the next.
Neologisms – Made-up words or phrases that only have meaning to you.
Perseveration – Repetition of words and statements; saying the same thing over and over.
Clang – Meaningless use of rhyming words (“I said the bread and read the shed and fed Ned at the head”).
Disorganized behavior
Schizophrenia disrupts goal-directed activity, impairing your ability to take care of yourself, your work, and interact with others. Disorganized behavior appears as:
- A decline in overall daily functioning
- Unpredictable or inappropriate emotional responses
- Behaviors that appear bizarre and have no purpose
- Lack of inhibition and impulse control
Negative symptoms (absence of normal behaviors)
The so-called “negative” symptoms of schizophrenia refer to the absence of normal behaviors found in healthy individuals, such as:
Lack of emotional expression – Inexpressive face, including a flat voice, lack of eye contact, and blank or restricted facial expressions.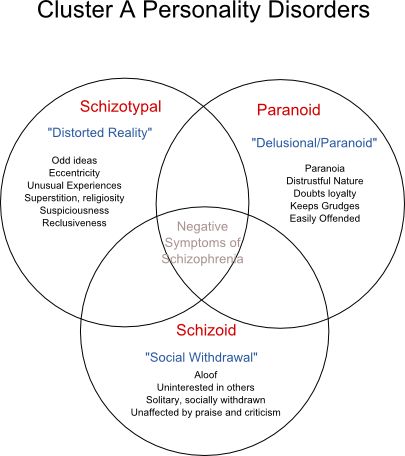
Lack of interest or enthusiasm – Problems with motivation; lack of self-care.
Seeming lack of interest in the world – Apparent unawareness of the environment; social withdrawal.
Speech difficulties and abnormalities – Inability to carry a conversation; short and sometimes disconnected replies to questions; speaking in a monotone.
Daniel's story
Daniel is 21 years old. Six months ago, he was doing well in college and holding down a part-time job in the stockroom of a local electronics store. But then he began to change, becoming increasingly paranoid and acting out in bizarre ways.
First, he became convinced that his professors were “out to get him” since they didn't appreciate his confusing, off-topic classroom rants. Then he told his roommate that the other students were “in on the conspiracy.” Soon after, he dropped out of school.
From there, his condition got worse. Daniel stopped bathing, shaving, and washing his clothes. At work, he became convinced that his boss was watching him through surveillance bugs planted in the store's TV screens. Then he started hearing voices telling him to find the bugs and deactivate them.
At work, he became convinced that his boss was watching him through surveillance bugs planted in the store's TV screens. Then he started hearing voices telling him to find the bugs and deactivate them.
Things came to a head when he acted on the voices, smashing several TVs and screaming that he wasn't going to put up with the “illegal spying” any more. His frightened boss called the police, and Daniel was hospitalized.
Treatment for schizophrenia
As upsetting as a diagnosis of schizophrenia can be, ignoring the problem won't make it go away. Beginning treatment as soon as possible with an experienced mental health professional is crucial to your recovery. At the same time, it's important not to buy into the stigma associated with schizophrenia or the myth that you can't get better. A diagnosis of schizophrenia is not a life-sentence of ever-worsening symptoms and recurring hospitalizations. With the right treatment and self-help, many people with schizophrenia are able to regain normal functioning and even become symptom-free.
Treatment basics
The most effective treatment strategy for schizophrenia involves a combination of medication, therapy, lifestyle changes, and social support.
Schizophrenia requires long-term treatment. Most people with schizophrenia need to continue treatment even when they're feeling better, in order to prevent new episodes and stay symptom-free. Treatment can change over time, though. As your symptoms improve, your doctor may be able to lower the dosage or change your medication.
Medication for schizophrenia works by reducing psychotic symptoms such as hallucinations, delusions, paranoia, and disordered thinking. But it is not a cure for schizophrenia. It is also much less helpful for treating symptoms such as social withdrawal, lack of motivation, and lack of emotional expressiveness. Finding the right drug and dosage is also a trial and error process. While medication should not be used at the expense of your quality of life, be patient with the process and discuss any concerns with your doctor.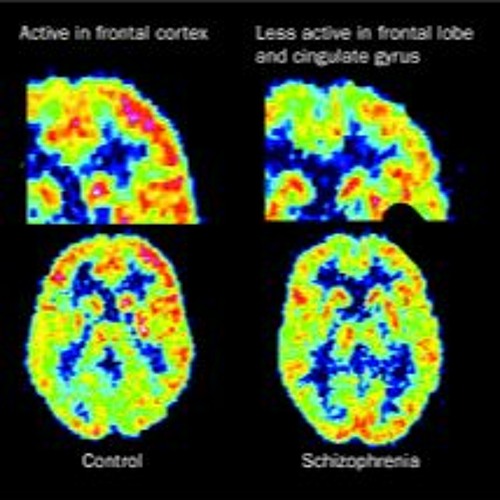
Therapy can help you improve coping and life skills, manage stress, address relationship issues, and improve communication. Group therapy can also connect you to others who are in a similar situation and are able to offer valuable insight into how they've overcome challenges.
Self-help
Medication and therapy can take time to take full effect but there are still ways you can manage symptoms, improve the way you feel, and increase your self-esteem. The more you do to help yourself, the less hopeless and helpless you'll feel, and the more likely your doctor will be able to reduce your medication.
Schizophrenia: The 7 keys to self-help
Seek social support. Friends and family vital to helping you get the right treatment and keeping your symptoms under control. Regularly connecting with others face-to-face is also the most effective way to calm your nervous system and relieve stress. Stay involved with others by continuing your work or education. If that's not possible, consider volunteering, joining a schizophrenia support group, or taking a class or joining a club to spend time with people who have common interests. As well as keeping you socially connected, it can help you feel good about yourself.
If that's not possible, consider volunteering, joining a schizophrenia support group, or taking a class or joining a club to spend time with people who have common interests. As well as keeping you socially connected, it can help you feel good about yourself.
Manage stress. High levels of stress are believed to trigger schizophrenic episodes by increasing the body's production of the hormone cortisol. As well as staying socially connected, there are plenty of steps you can take to reduce your stress levels. Try adopting a regular relaxation practice such as yoga, deep breathing, or meditation.
ADVERTISEMENT
Get regular exercise. As well as all the emotional and physical benefits, exercise may help reduce symptoms of schizophrenia, improve your focus and energy, and help you feel calmer. Aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions. Try rhythmic exercise that engages both your arms and legs, such as walking, running, swimming, or dancing.
Get plenty of sleep. When you're on medication, you most likely need even more sleep than the standard 8 hours. Many people with schizophrenia have trouble with sleep, but getting regular exercise and avoiding caffeine can help.
Avoid alcohol, drugs, and nicotine. Substance abuse complicates schizophrenia treatment and worsens symptoms. Even smoking cigarettes can interfere with the effectiveness of some schizophrenia medications. If you have a substance abuse problem, seek help.
Eat regular, nutritious meals to avoid symptoms exacerbated by changes in blood sugar levels. Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds can help improve focus, banish fatigue, and balance your moods.
Causes
While the causes of schizophrenia are not fully known, it seems to result from a mix of genetic and environmental factors.
Genetic causes
While schizophrenia runs in families, about 60% of schizophrenics have no family members with the disorder. Furthermore, individuals who are genetically predisposed to schizophrenia don't always develop the disease, which shows that biology is not destiny.
Furthermore, individuals who are genetically predisposed to schizophrenia don't always develop the disease, which shows that biology is not destiny.
Environmental causes
Studies suggest that inherited genes make a person vulnerable to schizophrenia. Environmental factors then act on this vulnerability to trigger the disorder.
More and more research points to stress—either during pregnancy or at a later stage of development—as being a major environmental factor. Stress-inducing factors could include:
- Prenatal exposure to a viral infection
- Low oxygen levels during birth (from prolonged labor or premature birth)
- Exposure to a virus during infancy
- Early parental loss or separation
- Physical or sexual abuse in childhood
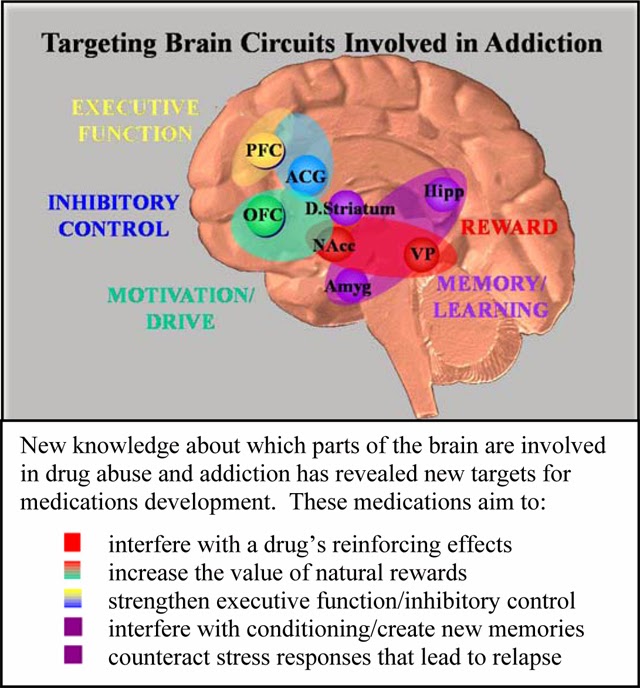
Abnormal brain structure
In addition to abnormal brain chemistry, abnormalities in brain structure may also play a role in schizophrenia development. However, it is highly unlikely that schizophrenia is the result of any one problem in any one region of the brain.
Diagnosing schizophrenia
A diagnosis of schizophrenia is based on a full psychiatric evaluation, medical history assessment, and physical exam. Lab tests can also help to rule out other medical causes of your symptoms.
Criteria to diagnose schizophrenia
The presence of two or more of the following symptoms for at least 30 days:
- Hallucinations
- Delusions
- Disorganized speech
- Disorganized or catatonic behavior
- Negative symptoms (emotional flatness, apathy, lack of speech)
Other diagnosis criteria:
- Have had significant problems functioning at work or school, relating to other people, and taking care of yourself.
- Shown continuous signs of schizophrenia for at least six months, with active symptoms (hallucinations, delusions, etc.) for at least one month.
- Have no other mental health disorder, medical issue, or substance abuse problem that is causing the symptoms.

Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
Last updated: November 2021
- References
Schizophrenia Spectrum and Other Psychotic Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x02_Schizophrenia_Spectrum
Patel, Krishna R., Jessica Cherian, Kunj Gohil, and Dylan Atkinson. “Schizophrenia: Overview and Treatment Options.” Pharmacy and Therapeutics 39, no. 9 (September 2014): 638–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159061/
Ganguly, Pronab, Abdrabo Soliman, and Ahmed A. Moustafa. “Holistic Management of Schizophrenia Symptoms Using Pharmacological and Non-Pharmacological Treatment.
 ” Frontiers in Public Health 6 (2018): 166. https://doi.org/10.3389/fpubh.2018.00166
” Frontiers in Public Health 6 (2018): 166. https://doi.org/10.3389/fpubh.2018.00166Aquino, Patrick. “Diagnosing and Treating Schizophrenia.” AMA Journal of Ethics 11, no. 1 (January 1, 2009): 43–48. https://doi.org/10.1001/virtualmentor.2009.11.1.cprl1-0901
Gage, S. H., H. J. Jones, S. Burgess, J. Bowden, G. Davey Smith, S. Zammit, and M. R. Munafò. “Assessing Causality in Associations between Cannabis Use and Schizophrenia Risk: A Two-Sample Mendelian Randomization Study.” Psychological Medicine 47, no. 5 (April 2017): 971–80. https://doi.org/10.1017/S0033291716003172
Chien, Wai Tong, Sau Fong Leung, Frederick KK Yeung, and Wai Kit Wong. “Current Approaches to Treatments for Schizophrenia Spectrum Disorders, Part II: Psychosocial Interventions and Patient-Focused Perspectives in Psychiatric Care.” Neuropsychiatric Disease and Treatment 9 (2013): 1463–81. https://doi.org/10.2147/NDT.S49263
Stępnicki, Piotr, Magda Kondej, and Agnieszka A.
 Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087
Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087Catts, Stanley Victor, and Brian Ignatius O’Toole. “The Treatment of Schizophrenia: Can We Raise the Standard of Care?” Australian & New Zealand Journal of Psychiatry 50, no. 12 (December 1, 2016): 1128–38. https://doi.org/10.1177/0004867416672725
Knight, Edward L. “Self-Help and Serious Mental Illness.” Medscape General Medicine 8, no. 1 (March 15, 2006): 68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/
“Self-Management: The Experiences and Views of Self-Management of People with a Diagnosis of Schizophrenia – Social Care Online.” Accessed November 2, 2021. https://www.scie-socialcareonline.org.uk/self-management-the-experiences-and-views-of-self-management-of-people-with-a-diagnosis-of-schizophrenia/r/a11G00000017tP5IAI
Sensky, T.
 , D. Turkington, D. Kingdon, J. L. Scott, J. Scott, R. Siddle, M. O’Carroll, and T. R. Barnes. “A Randomized Controlled Trial of Cognitive-Behavioral Therapy for Persistent Symptoms in Schizophrenia Resistant to Medication.” Archives of General Psychiatry 57, no. 2 (February 2000): 165–72. https://doi.org/10.1001/archpsyc.57.2.165
, D. Turkington, D. Kingdon, J. L. Scott, J. Scott, R. Siddle, M. O’Carroll, and T. R. Barnes. “A Randomized Controlled Trial of Cognitive-Behavioral Therapy for Persistent Symptoms in Schizophrenia Resistant to Medication.” Archives of General Psychiatry 57, no. 2 (February 2000): 165–72. https://doi.org/10.1001/archpsyc.57.2.165Pilling, S., P. Bebbington, E. Kuipers, P. Garety, J. Geddes, G. Orbach, and C. Morgan. “Psychological Treatments in Schizophrenia: I. Meta-Analysis of Family Intervention and Cognitive Behaviour Therapy.” Psychological Medicine 32, no. 5 (July 2002): 763–82. https://doi.org/10.1017/s0033291702005895
Turkington, Douglas, David Kingdon, and Peter J. Weiden. “Cognitive Behavior Therapy for Schizophrenia.” The American Journal of Psychiatry 163, no. 3 (March 2006): 365–73. https://doi.org/10.1176/appi.ajp.163.3.365
Schizophrenia – Overview of causes, symptoms, diagnosis, treatment and current research on schizophrenia. (National Institute of Mental Health)
(National Institute of Mental Health)
Schizophrenia: The Journey to Recovery (PDF) – Handbook discusses diagnosis and treatment issues. (Canadian Psychiatric Association)
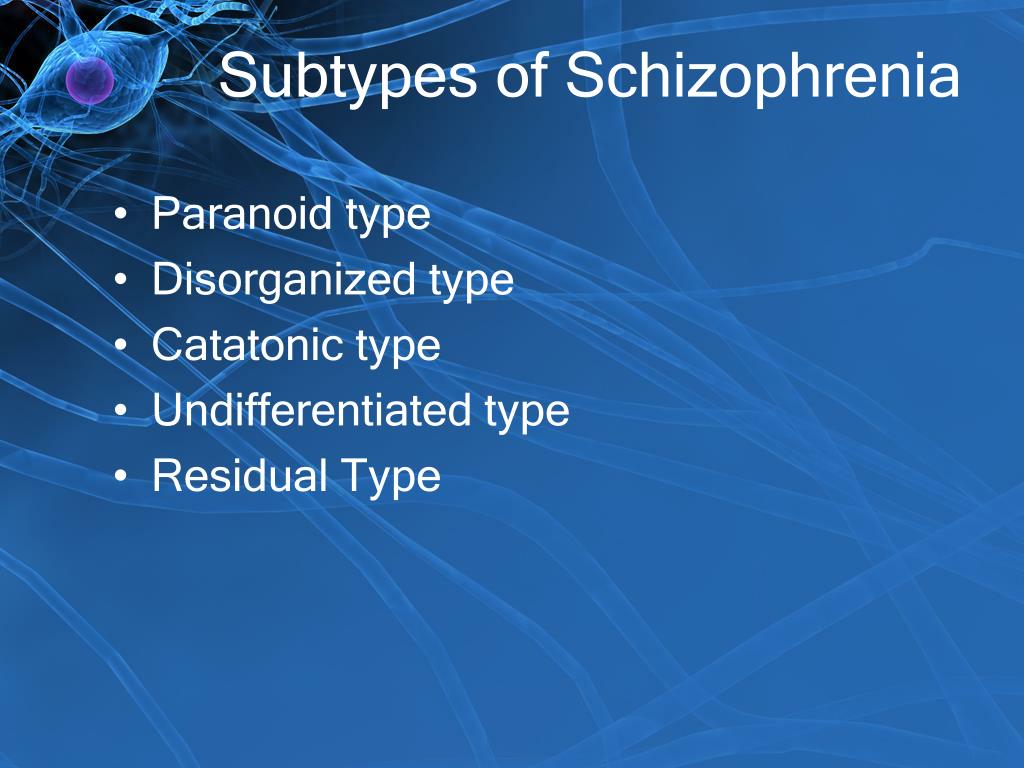
Catatonic Schizophrenia – Signs, symptoms, causes, and effects. (Schizophrenic.com)
Disorganized Schizophrenia – Signs and symptoms of this subtype. (PsychCentral)
Around the web
Last updated: October 13, 2022
When It Happens and Early Warning Signs
Written by WebMD Editorial Contributors
Schizophrenia usually takes hold after puberty. Most people are diagnosed in their late teens to early 30s.
What Is the Typical Age of Onset for Schizophrenia?
Men and women are equally likely to get this brain disorder, but guys tend to get it slightly earlier. On average, men are diagnosed in their late teens to early 20s. Women tend to get diagnosed in their late 20s to early 30s. People rarely develop schizophrenia before they're 12 or after they're 40.
The Turning Point: Adolescence
An interaction between something in your genes and something in your environment probably causes the disease. Researchers still have a lot to learn about it, but it's likely that many things play a role. Some, like exposure to a virus or malnutrition (according to one theory about causes), might have happened while you were still in your mother's womb. For vulnerable individuals, cannabis use can increase the risk of developing psychotic disorders such as schizophrenia.
No one knows exactly why it usually crops up in late adolescence, but there are many theories.
Your brain changes and develops a lot during puberty. These shifts might trigger the disease in people who are at risk for it.
Some scientists believe it has to do with development in an area of the brain called the frontal cortex. Others think it has to do with too many connections between nerve cells being eliminated as the brain matures.
Hormones also play a major role in puberty. One theory is that women get schizophrenia later than men because they go through puberty earlier and the hormone estrogen might somehow protect them. Know how to recognize the signs of schizophrenia in teens.
Know how to recognize the signs of schizophrenia in teens.
Early Warning Signs of Schizophrenia
Schizophrenia can be hard to diagnose for a few reasons. One is that people with the disorder often don't realize they're ill, so they're unlikely to go to a doctor for help.
Another issue is that many of the changes leading up to schizophrenia, called the prodrome, can mirror other normal life changes. For example, a teen who's developing the illness might drop their group of friends and take up with new ones. They may also have trouble sleeping or suddenly start coming home with poor grades.
Some research suggests that if a doctor strongly thinks someone is getting the disorder while still in this early phase, low doses of antipsychotic medication might delay it. More studies need to be done to know whether these drugs work for young people at risk for the disease. Cognitive behavioral therapy, family therapy, and social skills training appear to have clearer benefits for them, at least in the short term, when used early on. Learn more about the prodrome phase of schizophrenia.
Learn more about the prodrome phase of schizophrenia.
How Many People Have Schizophrenia?
About 3.5 million people in the United States are diagnosed with schizophrenia. It affects about 1.1% of the world’s population.
Characteristics of Schizophrenia
Schizophrenia is a syndrome. People with schizophrenia have several types of symptoms:
- Hallucinations. You hear voices or see or smell things that others say aren't there. The voices might criticize or threaten you. They might tell you to do things you otherwise wouldn't.
- Delusions. You believe things that aren't true, even when others show you proof or share facts that explain why your beliefs are wrong. Delusions can seem bizarre to others.
- For example, you might think that the TV is sending you special messages or that the radio is broadcasting your thoughts for everyone to hear. You might also feel paranoid and believe that others are trying to harm you.

- Thought disorders. You might have trouble organizing your thoughts, and you might speak in a way that's hard for others to understand. Perhaps you stop talking in the middle of a thought because you feel like it’s been taken out of your head. This is called thought withdrawal. Another type of disordered thinking, called thought blocking, happens when someone has a sudden stopping of their flow of thinking and as a consequence they may become silent until a new thought enters their mind.
- Movement disorders. You might move your body over and over again as if you're upset, or you might stop moving and responding. Doctors call this catatonia.
- Negative symptoms. Maybe you speak in a dull, flat tone, have trouble following through, lack interest in your daily life, and find it hard to keep up relationships. You might appear to be depressed. But while sadness, tearfulness, and other symptoms point to depression, so-called negative symptoms more likely point to a problem with the way the brain works.
Read more about the symptoms of schizophrenia.
Late-Onset Schizophrenia
Schizophrenia can develop later in life. Late-onset schizophrenia is diagnosed after the person is 45. People who have it are more likely to have symptoms like delusions and hallucinations. They’re less like to have negative symptoms, disorganized thoughts, impaired learning, or trouble understanding information.
Doctors think genetics may be to blame, just as it is with early-onset schizophrenia. They also think late onset might be a subtype that doesn’t affect the person until the right trigger appears. People with cognitive, vision, or hearing problems, or those who are suspicious, isolated, or reclusive may be more likely to get it.
Early-Onset Schizophrenia
It’s rare for someone younger than 13 to be diagnosed with schizophrenia, but it can happen. In young children, early-onset schizophrenia often causes:
- Talking delays
- Late or unusual crawling
- Late walking
- Unusual movements like arm flapping or rocking
Parents of teens might notice:
- Not spending as much time with friends and family
- Drop in school performance
- Trouble sleeping
- Bad mood
- Depression
- No motivation
- Using drugs or alcohol
- Odd behavior
Teens are less likely to have delusions but more likely to have visual hallucinations. Find out more on early childhood schizophrenia symptoms.
Find out more on early childhood schizophrenia symptoms.
Paranoid schizophrenia, causes, treatment, prevention of schizophrenia no
Paranoid schizophrenia is the most common form of schizophrenia, which is characterized by delusions, hallucinations, delusional ideas and limited social contacts. The reasons for the development of the disease are not exactly known, they speak of a combination of factors, including heredity, prenatal pathologies, severe stress suffered in childhood. In old age, the disease can develop against the background of Alzheimer's disease.
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
Paranoid schizophrenia is the most common form of schizophrenia and is dominated by paranoid or paraphrenic delusions and hallucinations, as well as affective flattening and incoherent speech. During illness, a person loses touch with reality, but the ability to think is preserved, unlike other forms of schizophrenia. During remission, a person is capable of self-care. According to statistics, the incidence of paranoid schizophrenia is about 1% of the total population. The debut, or the first vivid episode of the manifestation of the disease, occurs before the age of 30 years. It is important to understand that concomitant symptoms and signs can be observed for a long time before the first attack, but they must be recognized and classified in a timely manner. Schizophrenia itself appears without any external reasons for that - it is believed that the hereditary factor plays a big role in this case. Paranoid schizophrenia significantly affects the daily functioning, communication with others, personal life and work status of the patient.
During remission, a person is capable of self-care. According to statistics, the incidence of paranoid schizophrenia is about 1% of the total population. The debut, or the first vivid episode of the manifestation of the disease, occurs before the age of 30 years. It is important to understand that concomitant symptoms and signs can be observed for a long time before the first attack, but they must be recognized and classified in a timely manner. Schizophrenia itself appears without any external reasons for that - it is believed that the hereditary factor plays a big role in this case. Paranoid schizophrenia significantly affects the daily functioning, communication with others, personal life and work status of the patient.
Symptoms of paranoid schizophrenia
The main symptom of paranoid schizophrenia is delusions that distort the world around you. Thus, the patient may feel that he is being persecuted, or that he belongs to some ancient royal family. If we talk about hypochondriacal delirium, then in this case it cannot be associated with real sensations. For example, such patients are sure that they have installations in their bodies, thanks to which UFOs monitor their behavior and the functioning of the body. Often there is also a love delirium, when it seems to patients that this or that person is in love with them. Often such people suffer from hallucinations - auditory and visual. The clinical picture of paranodal schizophrenia is:
If we talk about hypochondriacal delirium, then in this case it cannot be associated with real sensations. For example, such patients are sure that they have installations in their bodies, thanks to which UFOs monitor their behavior and the functioning of the body. Often there is also a love delirium, when it seems to patients that this or that person is in love with them. Often such people suffer from hallucinations - auditory and visual. The clinical picture of paranodal schizophrenia is:
- depersonalization;
- emotional inadequacy;
- alarm;
- social isolation;
- senestopathy.
Paranoid schizophrenia, causes of occurrence
Functional disorders of the brain are considered the main, however, by no means the only factor in the development of paranoid schizophrenia. In addition to a violation of the functional activity of the brain, the causes of the onset of the disease can be a viral disease of the mother during pregnancy, severe stress, lack of a balanced diet during pregnancy, taking psychotropic drugs during puberty, Alzheimer's disease (in old age). Symptoms of paranoid schizophrenia:
Symptoms of paranoid schizophrenia:
- Delirium - obsessive suspicions, thoughts, manias, delusions. The most common delusion of influence occurs when the patient believes that they want to poison, kill, harm or delusion of persecution, when it seems to the patient that he is being followed by special services, aliens, etc. Also, delusions of grandeur often occur, the patient sincerely considers himself to be some outstanding person (president, Napoleon, Superman, etc.) and behaves accordingly, but if reasonable attempts are made to convince him of the opposite, aggression arises.
- Hallucinations - a violation of the perception of reality, when it seems to a person that he hears voices, they can give him commands, criticize, mock, provoke the patient to action. Sometimes hallucinations become so strong that the patient is talking with imaginary interlocutors, arguing or swearing with them.
- Disturbances in thinking, attention or inability to concentrate are extremely rare in patients with paranoid schizophrenia and should not prevail.
- Irritability, anger, phobias.
The development of paranoid schizophrenia
The first signs of paranoid schizophrenia usually appear at the age of 25, but sometimes even earlier. At first, the disease develops slowly and often unnoticed by others. The first signs can be manifested in an increase in the level of anxiety, suspicion, isolation, rigidity. This period can last from several months to several years. Further, the disease manifests itself, and symptoms appear in the form of hallucinations, delusions, or mixed states. Depending on the type of course of the disease, paranoid schizophrenia is divided into chronic and episodic. Gradually, in the course of the development of the disease, hallucinations and delusions become less pronounced, weaken and are replaced by long meaningless monologues. To any, the simplest question, the patient embarks on lengthy discussions, this is how irreversible changes in the psyche or a schizophrenic defect manifest themselves.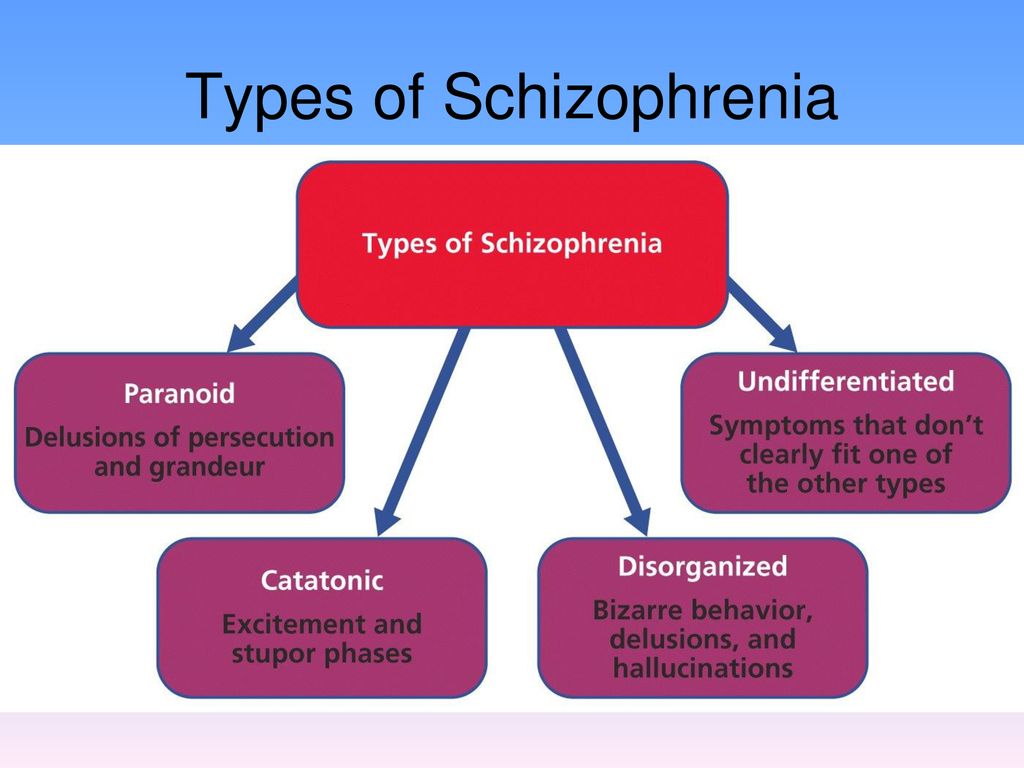 In addition to monologues, a person develops emotional callousness, interest disappears, and depression develops. It is impossible to prevent the development of a schizophrenic defect, it can only be slowed down, this requires timely and qualified treatment in Israel.
In addition to monologues, a person develops emotional callousness, interest disappears, and depression develops. It is impossible to prevent the development of a schizophrenic defect, it can only be slowed down, this requires timely and qualified treatment in Israel.
Paranoid schizophrenia, treatment
Only a qualified doctor can diagnose paranoid schizophrenia. This is a complex, chronic disease that needs to be treated as early as possible. At IsraClinic, a comprehensive program is selected for each patient to prevent the development of symptoms of paranoid schizophrenia and its treatment, depending on the degree of development of the disease, as well as the individual characteristics of the patient's personality. Paranoid schizophrenia is a chronic disease, and its treatment depends on the period of the course of the disease.
- Active therapy is used during exacerbations of the disease, its main task is to relieve the productive symptoms of the disease.
 The duration of treatment in this phase usually takes about a month. Depending on the prevalence of symptoms (hallucinations or delusions) and their severity, antipsychotics are usually prescribed, which quickly stop the symptoms. In the course of active treatment of psychopathic schizophrenia, specialists of the IsraClinic center also use atypical antipsychotics, which effectively combat the productive symptoms of the disease and, in addition, slow down the development of a schizophrenic defect, and the release of drugs in various dosages makes it possible to choose an individual, therapeutic dose.
The duration of treatment in this phase usually takes about a month. Depending on the prevalence of symptoms (hallucinations or delusions) and their severity, antipsychotics are usually prescribed, which quickly stop the symptoms. In the course of active treatment of psychopathic schizophrenia, specialists of the IsraClinic center also use atypical antipsychotics, which effectively combat the productive symptoms of the disease and, in addition, slow down the development of a schizophrenic defect, and the release of drugs in various dosages makes it possible to choose an individual, therapeutic dose. - Stabilizing therapy, used after the removal of acute manifestations of the disease. At this stage, the treatment regimen is reviewed. The dosage of the drugs used is reduced. The duration of treatment on stabilizing therapy is up to six months.
- Maintenance therapy is aimed at maximizing remission and fixing the achieved result, as well as preventing relapse.
Unfortunately, today there are no methods to completely cure, just as there are no methods for the prevention of paranoid schizophrenia.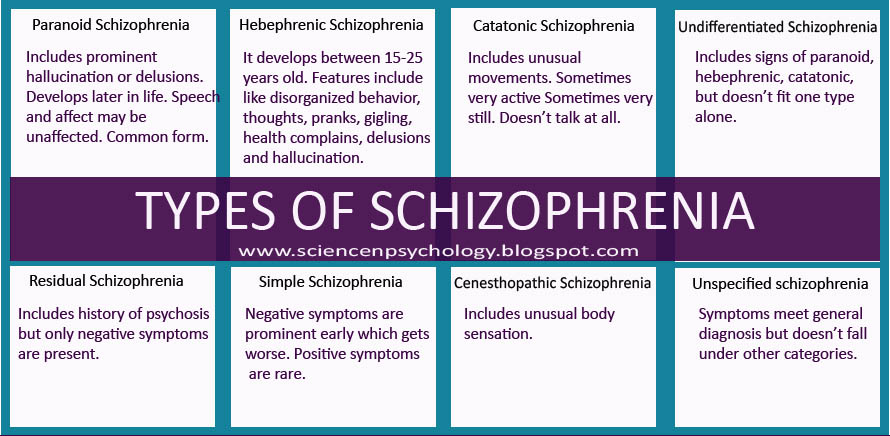 However, thanks to highly professional specialists and modern drugs, the development of the disease can be significantly slowed down, and the patient can be brought into a long-term remission, during which he can lead a normal life.
However, thanks to highly professional specialists and modern drugs, the development of the disease can be significantly slowed down, and the patient can be brought into a long-term remission, during which he can lead a normal life.
Methods for the treatment of paranoid schizophrenia
As already mentioned, the main treatment methods are drugs from the group of neuroleptics. Depending on the phase of the disease and the therapy strategy (active, stabilizing, supportive), different dosages of drugs are used in various combinations. At the stage of stabilizing and supportive therapy, psychotherapy can be connected. As a rule, we are talking about supportive psychotherapy, the purpose of which is to give the patient psychological tools with which he can integrate into society, perform feasible work, and lead the most normative way of life in his case. Also, psychotherapy is designed to teach the patient to recognize the deterioration of the condition, to take timely measures in order to prevent exacerbation. Note that the success of treatment depends on how timely paranoid schizophrenia is detected. The earlier the disease is detected, the less likely it is that a schizophrenic defect can exert its negative impact.
Note that the success of treatment depends on how timely paranoid schizophrenia is detected. The earlier the disease is detected, the less likely it is that a schizophrenic defect can exert its negative impact.
Paranoid schizophrenia: prevention
There is no universal prevention against schizophrenia, since this disease does not develop from external causes. Paranoid schizophrenia is an endogenous disease that develops for genetic reasons and due to hereditary predisposition. Therefore, the only prevention of paranoid schizophrenia will be mental hygiene. If you or your loved one in the family has relatives with mental illness, in particular, with schizophrenia, it is necessary to avoid stressful situations, taking psychoactive substances as much as possible, visit a psychologist or psychotherapist if the person has experienced a strong emotional shock, if he is in a state of chronic stress. In the event that the disease is diagnosed, it is important not to stop taking medications, follow all the recommendations of specialists, and constantly visit the attending psychiatrist. It is also very important to lead a socialized life as much as possible, to do all possible work, not to become isolated and not to move away from the outside world, to observe the daily routine, to have a good rest.
It is also very important to lead a socialized life as much as possible, to do all possible work, not to become isolated and not to move away from the outside world, to observe the daily routine, to have a good rest.
FGBNU NTsPZ. ‹‹Endogenous mental illness››
Paranoid schizophrenia occurs most often at the age of 30-35 years (sometimes earlier) and occurs mainly with delusional and hallucinatory disorders.
In the development of the disease, a number of clear stages are noted, described at the end of the last century by V. Magnan (1891) and characterizing the picture of chronic delirium. In the stereotype of the development of delusional syndromes, in typical cases, there is a stage of delirium that is not accompanied by hallucinations and phenomena of mental automatism - paranoid syndrome, stages of paranoid delirium - Kandinsky-Clerambault syndrome and fantastic delirium - paraphrenic syndrome [Kurashev S.V., 1955; Elgazina L. M., 1958; Shumsky N. G., 1958].
Depending on the predominance of delusional disorders or hallucinations in the picture of the disease, delusional and hallucinatory (pseudo-hallucinatory) variants of the course of paranoid schizophrenia are distinguished.
The disease develops gradually, the manifestations of the initial period are diverse: obsessions, psychopathic disorders, depersonalization phenomena, senesto-hypochondriac pictures. Against their background, at first unstable episodic, and later recurring delusional ideas of various content arise. The initial period of the disease with the listed disorders and mild personality changes allows us to characterize it as a stage of a sluggish course, the presence of which does not exclude the further course of the disease according to the laws and stereotype of classical paranoid schizophrenia. But in some patients, already in the initial period of the disease, a narrowing of the circle of interests, rigidity, distrust, and fading of emotional reactions are observed. The duration of this period is different - from 10 years or more.
The duration of this period is different - from 10 years or more.
The manifestation of the disease is manifested by the development of interpretive delusions with a greater or lesser degree of systematization of delusional ideas.
In the delusional variant of paranoid schizophrenia, the manifest period of the disease is characterized by the formation of an interpretive, highly systematized (paranoid) delusion with a different plot (jealousy, ideas of attitude, invention, reformism, etc.). The possibility of the development of a polythematic delirium (simultaneous existence of several plots of delirium, as a rule, connected with each other) is not excluded. The development of highly systematized syndromes of interpretive delusions occurs gradually, through the stages of overvalued formations and then overvalued delirium [Birnbaum K., 1844].
The formation of an interpretive delusion with a high degree of systematization is accompanied by a high activity of patients: jealous people do everything possible to search for and expose their imaginary rivals, patients with delusions of reformism or invention turn to various authorities in order to immediately implement their ideas, patients with delusions of persecution seek to discover their enemies.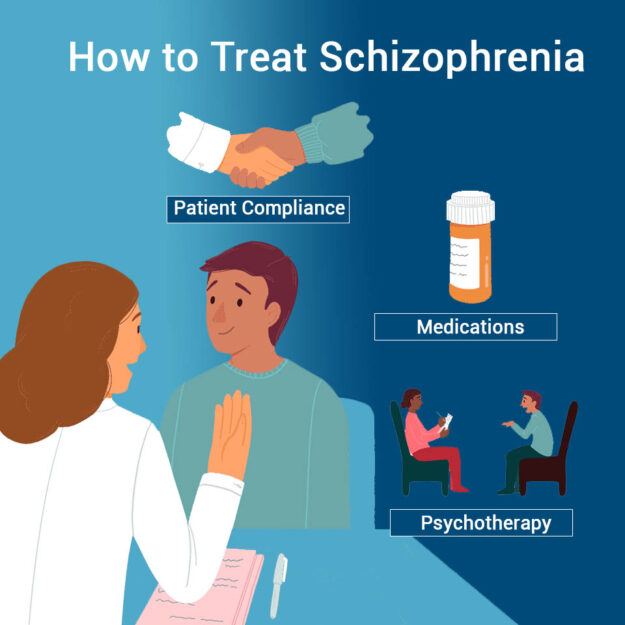 Due to the fact that the content of delusions often reflects real life situations and conflicts, the circle of supporters of patients who naturally do not understand the painful nature of the patient's experiences is revealed and expanded. This circle involves not only individuals, but government agencies and law enforcement agencies.
Due to the fact that the content of delusions often reflects real life situations and conflicts, the circle of supporters of patients who naturally do not understand the painful nature of the patient's experiences is revealed and expanded. This circle involves not only individuals, but government agencies and law enforcement agencies.
With the expansion of the plot of delirium, ideas of reassessment of one's personality and capabilities appear.
In some cases, the interpretive mechanism of delusional formation persists throughout the course of the disease. It differs in that the paraphrenia following immediately after this stage of the disease is not accompanied by the development of mental automatisms.
Sometimes psychotic states characterized by a high degree of systematization of delusions (paranoid syndromes) drag on for a sufficiently long period. Such cases are described in the literature as an independent variant of paranoid schizophrenia - paranoid schizophrenia. A state with paranoid delusions, sufficient stabilization of the picture and mild personality changes has a number of features, and in these cases a distinction is required from paranoid states of non-schizophrenic origin.
A state with paranoid delusions, sufficient stabilization of the picture and mild personality changes has a number of features, and in these cases a distinction is required from paranoid states of non-schizophrenic origin.
In the hallucinatory variant of paranoid schizophrenia, the states with interpretive delusions are shorter, the delusions do not reach a high degree of systematization. It is formed relatively quickly by the type of crystallization of delirium or sudden insight, which is accompanied by a subjective feeling of relief and the disappearance of internal tension.
In the initial period of the hallucinatory variant of paranoid schizophrenia, neurosis-like and psychopathic disorders can be observed [Elgazina L. M., 1958].
The development of the Kandinsky-Clerambault syndrome, both in cases of delusional and hallucinatory variants of paranoid schizophrenia, is preceded by an acutely developing state of anxious-fearful arousal with verbal hallucinations, mental automatisms that first appear, a sense of impending danger and fear.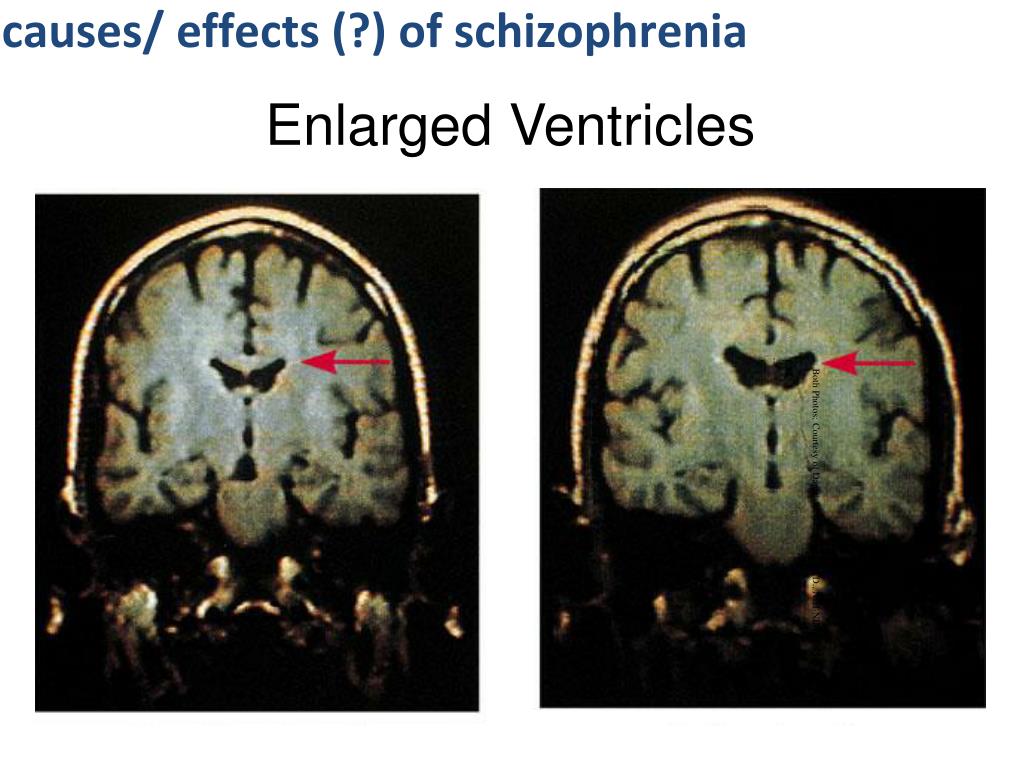 Its formation occurs in different ways: in some cases, along with the ideas of persecution and influence, ideational or other types of automatisms develop with a gradual expansion of their range and the formation of a total mastery syndrome; in other cases, its development is limited to delusional disorders and one or two types of mental automatisms, without a tendency to their further expansion.
Its formation occurs in different ways: in some cases, along with the ideas of persecution and influence, ideational or other types of automatisms develop with a gradual expansion of their range and the formation of a total mastery syndrome; in other cases, its development is limited to delusional disorders and one or two types of mental automatisms, without a tendency to their further expansion.
In the hallucinatory variant of paranoid schizophrenia, verbal illusions arise, individual verbal hallucinations such as hails and swear words addressed to the patient, followed by the development of a true verbal hallucinosis of commentary content, then the voices become “made”, begin to sound in the head, i.e. transform into pseudohallucinations. Often this transition is not accompanied by signs of an aggravation of the picture of psychosis, and sometimes one has to observe anxiety, fear, episodes of acute sensual delirium. The abundance of pseudohallucinations is combined with individual mental automatisms, however, they occupy a secondary place in the picture of the state, while the core disorder is verbal pseudohallucinosis. Delusional disorders that occur in the picture of the state are closely related to the content of hallucinosis (hallucinatory delusions). Pseudohallucinosis is highly resistant to therapy.
Delusional disorders that occur in the picture of the state are closely related to the content of hallucinosis (hallucinatory delusions). Pseudohallucinosis is highly resistant to therapy.
The next stage in the development of paranoid schizophrenia is paraphrenia. Some researchers point out that the development of paraphrenia is preceded by a state of anxiety-fearful excitement, similar to that observed at the moment of transformation of a paranoid state into a hallucinatory-paranoid one. But these observations are not supported by clinical practice. The formation of paraphrenia occurs gradually and the first signs of paraphrenia appear in the picture of the Kandinsky-Clerambault syndrome.
The beginning of the transformation of the syndrome, as a rule, is a change in the nature of the impact experienced by the patient - harmful to "benevolent". This happens against the backdrop of a somewhat elated mood, when patients begin to talk about the emergence of their unusual abilities to recognize the thoughts of others and influence their well-being. There is a symptom of “unwinding of memories”, accompanied by pseudo-hallucinatory memories (according to K. Kahlbaum “memory hallucinations”): the patient is “forced” to recall the events of the past, their details, which were actually absent; they emerge in the patient's memory with a feeling that the oblivion has passed and he again recalled the details of the events of past years. Then, ideas of greatness of fantastic, absurd content, typical of paraphrenia, arise: patients claim that they are special personalities, they are entrusted with special missions, that they influence the fate of people and the universe; patients believe that in the world there is a struggle between the supporters of the patient and his opponents. However, unlike acute paraphrenic conditions, the patient does not see signs of this struggle in his environment. In the pseudohallucinatory variant of paranoid schizophrenia, the paraphrenic state acquires a picture of pseudohallucinatory paraphrenia with the development of delusions that are identical in content to pseudohallucinations.
There is a symptom of “unwinding of memories”, accompanied by pseudo-hallucinatory memories (according to K. Kahlbaum “memory hallucinations”): the patient is “forced” to recall the events of the past, their details, which were actually absent; they emerge in the patient's memory with a feeling that the oblivion has passed and he again recalled the details of the events of past years. Then, ideas of greatness of fantastic, absurd content, typical of paraphrenia, arise: patients claim that they are special personalities, they are entrusted with special missions, that they influence the fate of people and the universe; patients believe that in the world there is a struggle between the supporters of the patient and his opponents. However, unlike acute paraphrenic conditions, the patient does not see signs of this struggle in his environment. In the pseudohallucinatory variant of paranoid schizophrenia, the paraphrenic state acquires a picture of pseudohallucinatory paraphrenia with the development of delusions that are identical in content to pseudohallucinations. The possibility of developing confabulatory disorders of fantastic content (confabulatory paraphrenia) is not ruled out.
The possibility of developing confabulatory disorders of fantastic content (confabulatory paraphrenia) is not ruled out.
The end state of paranoid schizophrenia is characterized by "schizophasia". Its first sign is a symptom of a monologue, manifested by infinitely long answers to simple questions, when the answers (for example, about well-being) contain information that has nothing to do with the content of the question. In the future, the actual phenomenon of schizophasia may develop - grammatically correct speech, devoid of any meaning and content. The appearance of neologisms in speech is characteristic. Quite often in such speech of patients nevertheless it is possible to catch separate fragments of paraphrenic delirium. The behavior of patients with schizophasia is outwardly correct. Patients can perform even simple work.
Sometimes in patients at the paraphrenic stage of the disease, short states of arousal may occur, which are explained by the revival of the "extinct" paraphrenic delirium.