Age of onset for adhd
Onset And Prevalence Of ADHD
MentalHelp independently researches, tests, and reviews products and services which may benefit our readers. Where indicated by "Medically Reviewed by", Healthcare professionals review articles for medical accuracy. If you buy something through our links, or engage with a provider, we may earn a commission.
Onset
Most research supports the theory that ADHD is a physiological condition and is therefore present at birth. However, the noticeable beginning of ADHD symptoms typically occurs early in childhood. Before the age of 5, ADHD symptoms may be difficult to diagnose, because most young children are highly energetic, easily distractible, and impulsive. Therefore, the average age of diagnosis is 8 years for ADHD and 10 years for ADD. The difference in diagnosis age likely occurs because hyperactive symptoms tend to draw more attention as a result of the child's active, noisy behavior than do pure attention problems that are calm and quiet.
Observers can hardly help but notice wild and out of control behavior, while they may have to carefully study a child to see the distracted and inattentive behaviors. Often, as children grow older, their ADHD symptoms decrease in severity. 30% to 70% of children with ADHD continue to experience symptoms into adulthood, though they may be less pronounced than they were during childhood.
Prevalence
By 1996, at least 40% of children referred to outpatient child psychiatry providers were diagnosed with ADHD. According to the Centers for Disease Control, 4.4 million youth between the ages of 4-17 have been diagnosed with Attention-Deficit/Hyperactivity Disorder. The DSM IV-TR suggests that the prevalence rate of ADHD in children is 3% to 7%, and 2% to 5% in adults. Using these prevalence rates it can be estimated that in a classroom of 25 to 30 children, at least one of those children will have ADHD.
Explore Your Options Today
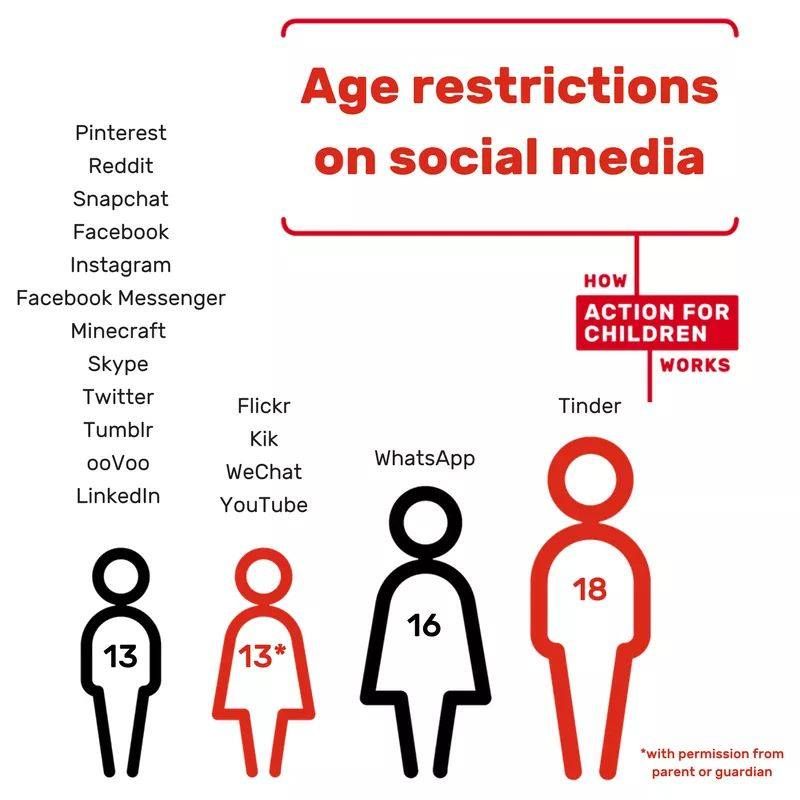
As of 2003, approximately 2. 5 million young people were being treated with medication for ADHD symptoms. Prescription medication rates for ADHD are increasing in usage dramatically in the United States, with certain geographical areas tripling or quadrupling the number of prescriptions written ten years ago. Although increasing medication rates may be related to improved awareness and diagnosis, some professionals have different theories. Some researchers speculate that increasing ADHD prevalence and treatment rates may be related to changes associated with living in the digital age, such as decreased levels of physical activity and less exposure to the natural environment, which is thought to lead to increased amounts of restless and impulsive behavior (we will discuss this idea further in our section on causes of ADHD).
5 million young people were being treated with medication for ADHD symptoms. Prescription medication rates for ADHD are increasing in usage dramatically in the United States, with certain geographical areas tripling or quadrupling the number of prescriptions written ten years ago. Although increasing medication rates may be related to improved awareness and diagnosis, some professionals have different theories. Some researchers speculate that increasing ADHD prevalence and treatment rates may be related to changes associated with living in the digital age, such as decreased levels of physical activity and less exposure to the natural environment, which is thought to lead to increased amounts of restless and impulsive behavior (we will discuss this idea further in our section on causes of ADHD).
Gender Differences
Boys are diagnosed with ADHD three times more often than girls; and adult males are diagnosed more often than adult females. Males of all ages tend to display, by far, more hyperactivity than females and slightly more symptoms of inattention than women. Approximately 10% of all males and 4% of females have been diagnosed with ADHD.
Approximately 10% of all males and 4% of females have been diagnosed with ADHD.
The difference in prevalence rates between males and females is an interesting phenomenon. Not only do boys tend to be more often hyperactive, but boys who are inattentive often play around (and get in trouble). In contrast, girls who are inattentive tend to daydream. These tendencies may at least partly explain why more males are diagnosed than females. However, it is not really clear whether there is a true gender-based difference in genetic susceptibility to ADHD, or if females are simply much less likely to be diagnosed than men. Research is being conducted to try to determine the source of these differences.
Cross-Cultural Differences
Although ADHD is more frequently diagnosed in the United States, it has been found in every country that has been studied. Prevalence rates range from 1.7-10% in Canada, Germany, the Netherlands, New Zealand, Norway, Puerto Rico, and the United Kingdom.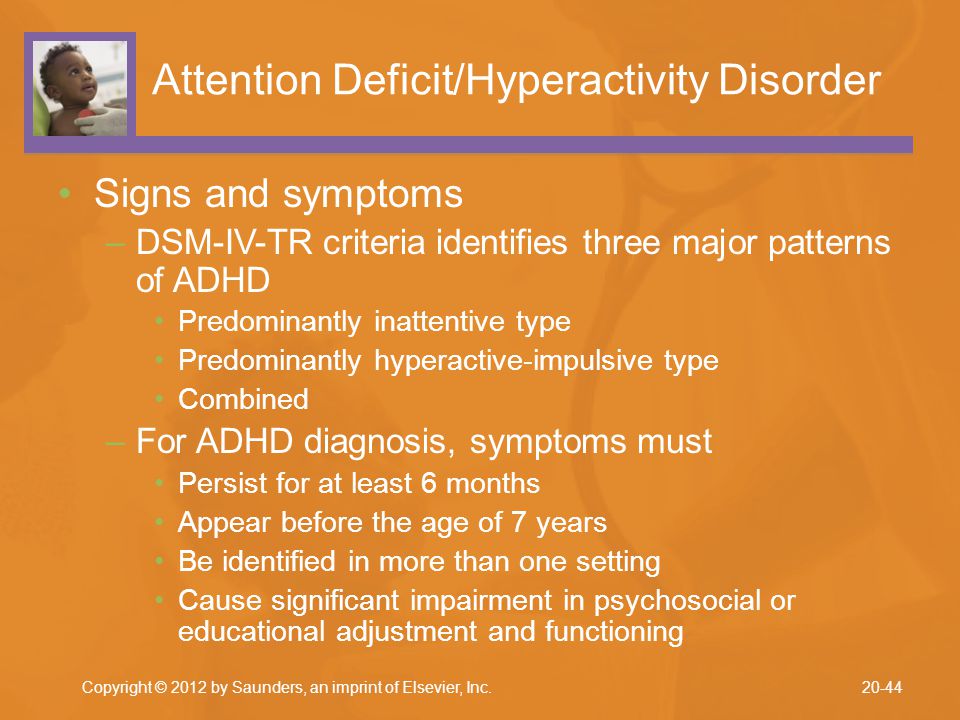 Interestingly, the rates of diagnosis are rising in industrialized countries. These increasing rates may be explained in part by an enhanced awareness of the disorder in other countries, resulting in improved diagnosis and treatment.
Interestingly, the rates of diagnosis are rising in industrialized countries. These increasing rates may be explained in part by an enhanced awareness of the disorder in other countries, resulting in improved diagnosis and treatment.
Myndfulness App
Designed to Help You Feel Better Daily
Download Now For Free
Learn More >
Trends in the Parent-Report of Health Care Provider-Diagnosis and Medication Treatment for ADHD
Researchers from the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration have published a study: “Trends in the Parent-Report of Health Care Provider-Diagnosed and Medicated ADHD: United States, 2003—2011.” Read the abstract 1. See below for a summary of the findings from this article.
Health care providers who care for children with attention-deficit/hyperactivity disorder (ADHD) and public health practitioners should be aware that an estimated two million more US children were reported by their parents to be diagnosed by a health care provider with ADHD and a million more were reported to be taking medication for ADHD in 2011, compared to 2003. These health professionals should also be aware of the changing patterns of ADHD in the United States.
These health professionals should also be aware of the changing patterns of ADHD in the United States.
About attention-deficit/hyperactivity disorder and this study:
ADHD is a neurobehavioral disorder of childhood that often persists into adulthood. CDC uses national surveys that ask parents about their child’s health to monitor the number of children with ADHD and the treatment patterns for these children. The largest of these surveys is the National Survey of Children’s Health, which has been collected every four years since 2003. Previous results from the 2003 and 2007 surveys found that 7.8% and 9.5% of US children aged 4-17 years were reported by their parents to have ever been diagnosed with ADHD by a health care provider in 2003 and 2007, respectively. The current study looked at data from the third National Survey of Children’s Health, conducted in 2011-2012. The findings tell us more about ADHD diagnosis and treatment patterns, and reflect the substantial impact that ADHD has on families.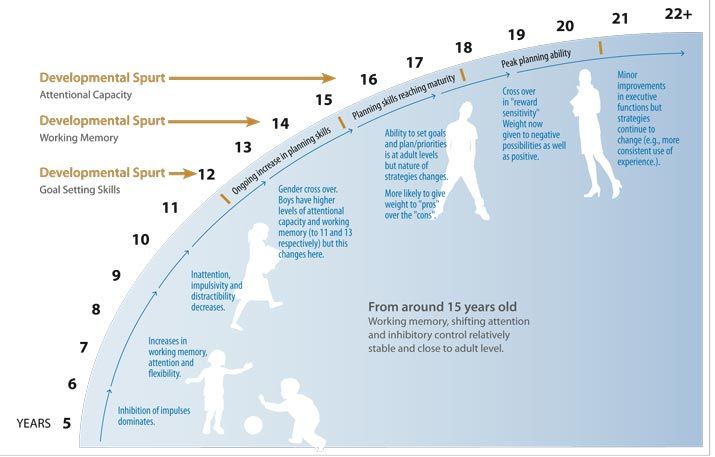
Learn more about the data source: National Survey of Children’s Health
Important findings from this study include:
- More than 1 in 10 (11%) US school-aged children had received an ADHD diagnosis by a health care provider by 2011, as reported by parents.
- 6.4 million children reported by parents to have ever received a health care provider diagnosis of ADHD , including:
- 1 in 5 high school boys
- 1 in 11 high school girls
- 6.4 million children reported by parents to have ever received a health care provider diagnosis of ADHD , including:
- The percentage of US children 4-17 years of age with an ADHD diagnosis by a health care provider, as reported by parents, continues to increase.
- A history of ADHD diagnosis by a health care provider increased by 42% between 2003 and 2011:
- 7.8% had ever had a diagnosis in 2003
- 9.5% had ever had a diagnosis in 2007
- 11.0% had ever had a diagnosis in 2011
- Average annual increase was approximately 5% per year
- A history of ADHD diagnosis by a health care provider increased by 42% between 2003 and 2011:
- The percentage of children 4-17 years of age taking medication for ADHD, as reported by parents, increased by 28% between 2007 and 2011.
- Percentage of children taking medication for ADHD was:
- 4.8% in 2007
- 6.1% in 2011
- Average annual increase was approximately 7% per year
- Percentage of children taking medication for ADHD was:
- The average age of ADHD diagnosis was 7 years of age, but children reported by their parents as having more severe ADHD were diagnosed earlier.
- 8 years of age was the average age of diagnosis for children reported as having mild ADHD
- 7 years of age was the average age of diagnosis for children reported as having moderate ADHD
- 5 years of age was the average age of diagnosis for children reported as having severe ADHD
- More US children were reported by their parents to be receiving ADHD treatment in 2011 compared to 2007, however treatment gaps may exist.
- In 2011, as many as 17.5% of children with current ADHD were reported by their parents as not receiving either medication for ADHD or mental health counseling
- More than one-third of children reported by their parents as not receiving treatment were also reported to have moderate or severe ADHD
- The patterns in ADHD diagnosis and medication treatment showed increases in the percentages overall, however some new patterns emerged between 2007 and 2011.

- The percentage of children reported by their parents to have a history of health care provider diagnosed ADHD increased for most demographic groups (for example, across racial groups, boys and girls) from 2003 to 2011; however,
- Between 2007 and 2011, the percentage of children reported by their parents to have a history of a health care provider diagnosed ADHD:
- Was similar among older teens
- Decreased among multiracial children and children of other races when compared to black or white children
- The number of US families impacted by ADHD continues to increase.
- An estimated 2 million more children were reported by their parents to be diagnosed by a health care professional with ADHD in 2011, compared to 2003
- By 2011, 6.4 million children were reported by their parents to be diagnosed by a health professional with ADHD compared to 4.4 million in 2003
- An estimated 1 million more children were reported by their parents to be taking medication for ADHD in 2011, compared to 2003.
- By 2011, 3.5 million children were reported by their parents to be taking medication for ADHD compared to 2.5 million in 2003
- An estimated 2 million more children were reported by their parents to be diagnosed by a health care professional with ADHD in 2011, compared to 2003
ADHD: CDC’s Activities
CDC monitors the number of children who have been diagnosed with ADHD through the use of national survey data. Including questions about ADHD on national or regional surveys helps us learn more about the number of children with ADHD, their use of ADHD treatments, and the impact of ADHD on children and their families. CDC has previously used national survey data to document increasing estimates of the number of children with ADHD from 2003-2007.2 CDC has also used these data to estimate the percentage of children taking medication for ADHD, nationally and by state.3
CDC also conducts community-based studies to better understand the impact of ADHD. The Project to Learn about ADHD in Youth (PLAY) study methods have been implemented in four community sites. Information from the PLAY study helps us better understand ADHD as well as the needs of children and families living with ADHD.
CDC supports the National Resource Center on ADHD, a program of Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD), which is a Public Health Practice and Resource Center. Their web site (http://www.help4adhd.org/NRC.aspx) has links to information based on the current best medical evidence about the care for people with ADHD and their families. The National Resource Center operates a call center with trained, bilingual staff to answer questions about ADHD. Their phone number is 1-800-233-4050.
More Information
To learn more about ADHD, please visit https://www.cdc.gov/adhd.
References
- Visser S, Danielson M, Bitsko R, et al. Trends in the Parent-Report of Health Care Provider-Diagnosis and Medication Treatment for ADHD disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014,53(1):34–46.e2.
- Centers for Disease Control and Prevention. Increasing Prevalence of Parent-Reported Attention-Deficit/Hyperactivity Disorder Among Children — United States, 2003 and 2007.
 MMWR. 2010;59(44):1439-1443.
MMWR. 2010;59(44):1439-1443. - Visser SN, Blumberg SJ, Danielson ML, Bitsko RH, Kogan MD. State-Based and Demographic Variation in Parent-Reported Medication Rates for Attention-Deficit/Hyperactivity Disorder, 2007-2008. Prev Chronic Dis. Jan 2013;10:E09.
How to recognize ADHD in a child and help him
November 23, 2019 Likbez Adviсe
This disorder is often confused with ordinary bad manners. Nevertheless, we are talking about a serious diagnosis.
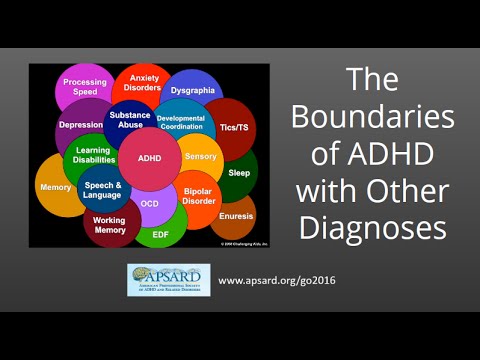
What is ADHD
Attention Deficit Hyperactivity Disorder (ADHD) is a neurological behavioral disorder that the affected person cannot control (this is important). It has three key manifestations. Or, in some cases, their combination:
- Carelessness. It is difficult for a child to concentrate on a task. He lacks the persistence to continue what he started for more than a couple of minutes. And these problems are not related to the fact that he "does not obey" or does not understand the question.

- Hyperactivity. The child cannot sit still, including in situations where calm and silence are required. He jumps, twists, taps his foot, asks a million questions, scratches, giggles, or is just plain nervous.
- Impulsivity. This means that children do what they want, instantly, without thinking about the consequences. For example, another child takes their car in the sandbox - they beat the offender. It is necessary to the carousel - they run towards it, pushing the rest with their shoulders. I wonder what the appearance of others is connected with - they directly and loudly ask: “Why is this old aunt so fat?”
Most often, ADHD is associated only with hyperactivity. But this is a mistake. The child can be reserved and balanced phlegmatic. Just extremely careless.
For a doctor to make a diagnosis, it is enough that one or two of the manifestations of the disease indicated above are observed. In this case, ADHD is divided into types: predominantly inattentive and predominantly hyperactive-impulsive. But in most children, all three problems are present in a complex - this type of ADHD is called combined.
But in most children, all three problems are present in a complex - this type of ADHD is called combined.
How to recognize ADHD
If you think that almost all children exhibit this behavior from time to time, you don't. Almost everyone at some point in their lives may behave like someone with ADHD. That is why there is an opinion that this disorder does not exist - they say, these are inventions designed to hide poor upbringing or, let's say, a low level of intelligence.
But despite the controversy, ADHD is quite an official medical diagnosis. The International Classification of Diseases ICD-11 refers it to neurodevelopmental disorders - diseases in which the psyche fails and produces a pathological reaction to sensory information coming from outside.
And there are quite clear diagnostic criteria that help recognize ADHD.
1. Age
Symptoms of ADHD most often first appear between the ages of 3 and 6, but most cases are diagnosed between 6 and 12 years of age.
If you suspect ADHD in a teenager, but you are not sure if he had the same problems in preschool age, most likely it is some other disorder. Or just behavior problems that don't have neurological implications.
2. Symptoms that last at least 6 months
Diagnosis requires long-term observation of the child's behavior, at least six months. And not only in the family or familiar environment, but also in kindergarten or school.
A pediatrician, neurologist, psychologist, psychiatrist should talk in detail with the parents and the child himself. And also, ideally, interview other people working with him - educators or teachers. Only this allows you to put together a whole picture.
3. Symptoms that recur both at home and in kindergarten or school
A child with ADHD cannot control their behavior. Therefore, the symptoms will be the same - in the familiar environment, in the kindergarten or school.
If your child seems to be unable to sit still even for a second, blows up the house and exhausts you with endless questions, but behaves normally in kindergarten, this is not about attention deficit hyperactivity disorder.
4. Symptoms that reduce the quality of life
You can be diagnosed if you notice at least a few of the following symptoms every day.
In case of inattentive ADHD, the child:
- Not able to keep attention on one thing for a long time (at least 5 minutes).
- Easily distracted, instantly forgetting what he was doing just now.
- He regularly makes elementary mistakes: in the example “1 + 2”, he can forget that the first digit was a unit, and output the answer 4. Or, when reading, skip a line and not even notice it.
- Often, being distracted, he cannot perform a simple task that other children can easily cope with.
- Regularly does not hear the speech of a parent, educator or teacher addressed to him, because his thoughts are somewhere far away.
- Cannot keep things in order, even when this is specially emphasized to his attention.
- Loses things endlessly - mittens, pencils, books, wallets, keys.
- When going somewhere, he “digs” all the time – he cannot quickly put together the necessary accessories, even if there are very few of them.
With hyperactive-impulsive ADHD child:
- Cannot sit still for more than a few minutes. In the literal sense: fidgeting, wriggling, twisting with brushes and knocking with his feet.
- Often forgets and jumps out of place in situations where it is impossible to do this, for example, in a lesson.
- Shows aimless motor activity: jumping, waving his arms, climbing or running somewhere.
- Does not know how to play quietly and thoughtfully, for example, to assemble a construction set on his own.
- Cannot wait in line. So, the teacher's question can be answered by interrupting the classmate to whom this question was addressed.
- He can be very talkative and often quite tactless.
- Seems to lack a sense of danger that could threaten his life.
With combined ADHD, the symptoms may be combined. And in any type, they obviously interfere with the child. For example, due to restlessness or lack of concentration, he cannot learn a lesson or complete an assignment. And because of tactlessness or slowness, it causes irritation in others.
And because of tactlessness or slowness, it causes irritation in others.
Why ADHD is dangerous
Inattention, hyperactivity and impulsivity can persist into adulthood. This often leads to serious psychosocial problems:
- poor academic performance and, as a result, the inability to get a good education;
- lack of friends and support;
- ridicule and related mental trauma;
- low self-esteem;
- inability to make and keep plans;
- optional, which has a bad effect on career and relationships within the team;
- frequent mood swings;
- vehemence, inclination to commit rash acts;
- persistently high levels of stress, which can lead to the development of other mental disorders such as anxiety or depression;
- inability to build long-term relationships, including family ones;
- alcohol and drug abuse;
- problems with paying debts and the law.
Conclusion: if the diagnosis of ADHD is made, the disease must be corrected.
How to treat ADHD
Good news first.
Between 30% and 70% of children diagnosed with the syndrome "outgrow" it with age.
In other children, the disorder remains for life. It is not always possible to cure it completely. However, there are quite effective methods of correction that can reduce symptoms.
1. Psychotherapy
In particular, we are talking about behavioral therapy. A qualified psychotherapist will help the child cope with emotions and disappointments, teach social skills in a playful way, for example, wait in line and share, and will not let self-esteem sink.
2. Work in the family
Family relationships are a key part of successful correction. It is extremely important for parents to do everything so as not to increase the already high level of stress in the child.
Do not scold him for inattention, slowness or restlessness: children with ADHD are objectively unable to cope with this. Your task is to be supportive, to show the child that he is loved no matter what. You may also need psychotherapy, which will teach you to control your own emotions and tell you where to draw the psychological resource necessary for communication.
Your task is to be supportive, to show the child that he is loved no matter what. You may also need psychotherapy, which will teach you to control your own emotions and tell you where to draw the psychological resource necessary for communication.
Here's what mom and dad can do:
- Organize your child's home life. Try to follow a strict daily regimen with clearly defined times for getting up, having breakfast, getting ready for the garden or school, bathing, going to bed. It is also worth making a schedule that will remind the child what he should do during the day. Be sure to place your schedule sheet somewhere visible, such as a magnet on the refrigerator door.
- Adjust diet. Diet research has yielded mixed results. But still, there is reason to believe that certain foods can help the brain cope with the disorder. Add high protein foods to your daily diet - meat, eggs, beans, nuts. Try to replace fast carbohydrates like sweets and cakes with slow ones like fruits, whole grain bread.
 An important nuance: before changing the diet, you should consult on this topic with the pediatrician observing the child.
An important nuance: before changing the diet, you should consult on this topic with the pediatrician observing the child. - Limit time for watching TV and playing with gadgets. No more than 2 hours a day!
- Be consistent in your actions. Children with ADHD need clear and predictable rules to follow.
3. Drug therapy
The most commonly used in the correction of ADHD are nootropics (substances that improve brain function) and psychostimulants (help control behavior). Which drug is needed in your case, only a doctor can decide.
One must be prepared for the fact that the chosen medicine may not be effective, and then a change in the drug will be required.
In addition, any side effects that occur, including loss of appetite or trouble sleeping, should be reported to the physician. This is also an indication for looking for another remedy.
Where ADHD comes from
The exact cause of the development of the disorder has not been established. But it is known that an excess of sugar or excessive TV viewing does not cause attention deficit hyperactivity disorder. An unbalanced diet or obsession with gadgets can make ADHD difficult to manage. But they are not able to provoke its development.
But it is known that an excess of sugar or excessive TV viewing does not cause attention deficit hyperactivity disorder. An unbalanced diet or obsession with gadgets can make ADHD difficult to manage. But they are not able to provoke its development.
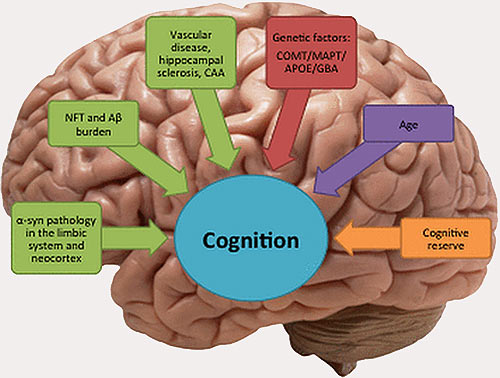
Scientists have only been able to identify a number of factors that seem to play a role in causing ADHD.
1. Heredity
The syndrome runs in families, which makes it possible to link it with genetics. It has been found that if one parent had ADHD, the child has a 50% chance of inheriting the disorder. If the family already has an older brother or sister with the syndrome, the risks of the younger one are 30%.
2. Preterm birth
ADHD is often diagnosed in babies born prematurely or with low birth weight (less than 2,500 g).
3. Bad habits of the mother during pregnancy
The risk of ADHD in a child increases if the mother smoked, consumed alcohol or drugs while carrying the fetus.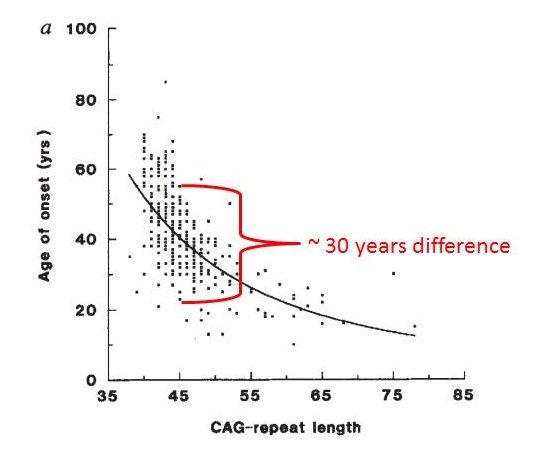
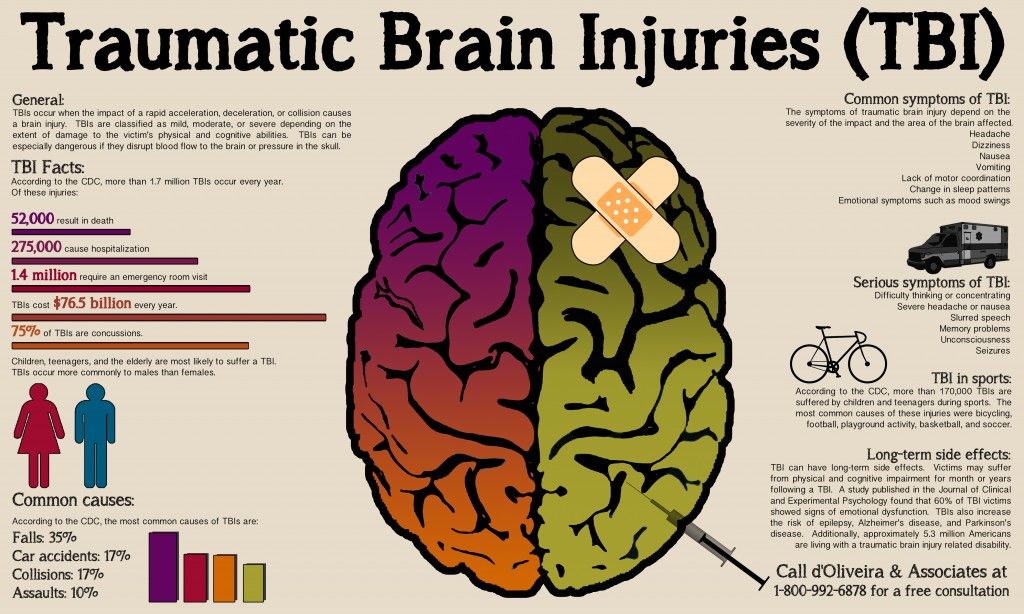
4. Damage to the frontal lobe of the brain
For example, during falls. The frontal lobe is responsible for controlling emotions and behavior.
5. Exposure to toxins in infancy
Talking about lead or pesticides. The poisoning caused by them can also provoke the development of ADHD.
Read also 🤱🧒👶
- Allergy in a child: everything parents should know about diagnosis and treatment
- What to do if a child has diabetes
- How to raise an independent child: the method of a lazy mother
- What to do if the child is overweight
- 5 mistakes of parents, due to which the child's eyesight deteriorates
Adult Attention Deficit Hyperactivity Disorder
Attention Deficit Hyperactivity Disorder (ADHD) is a neurological-behavioral developmental disorder usually diagnosed in childhood. However, in most cases, the symptoms of this disease persist for life and require treatment in adults.
The symptoms of Attention Deficit Hyperactivity Disorder in adults are similar to those in children. Adults with ADHD usually have difficulty concentrating. They find it difficult to concentrate on boring, monotonous work and keep material in their working memory for a long time. Such people usually find it difficult to restrain their impulsiveness.
This disorder always develops from birth, but it is not always correctly diagnosed in childhood or not detected at all.
A person suffering from ADHD is born with a pathology of neurodevelopment - a delay in the development of certain areas of the brain responsible for concentration, memory and restraint of impulsivity. The formation of these areas of the brain occurs in each person with ADHD, at their own pace. For some, they are fully formed by the age of 16, for someone by the age of 30, and for some, the development of these parts of the brain never reaches the optimal level.
ADHD never appears in adulthood. This disorder always develops from birth, but it is not always correctly diagnosed in childhood or not detected at all. The diagnosis is usually made at 7-8 years of age. If the right treatment is given at this age, there is a high chance that by the age of 16, the child will stop taking medication and be able to cope with cognitive tasks on his own. As a result of working with specialists, the child will develop areas of the brain responsible for the symptoms, and he will need to take drugs only in exceptional cases, for example, before an exam.
See also
How to treat ADHD in children?
If a person is diagnosed with ADHD in childhood, he grows up with the understanding that he has a problem. A person realizes that there are things that are difficult for him, and with the help of psychotherapy and special training, he constantly works on this. If the treatment is positive, by the age of 16 the child has enough skills to perform monotonous work and be focused without medication. This is an ideal scenario for a person with Attention Deficit Hyperactivity Disorder. In adulthood, such a person does not need constant treatment, but can only occasionally take medication. There are also cases when a person suffering from ADHD has such a high cognitive potential inherent in him genetically that until adulthood it helps him to cope with difficult tasks without resorting to treatment.
This is an ideal scenario for a person with Attention Deficit Hyperactivity Disorder. In adulthood, such a person does not need constant treatment, but can only occasionally take medication. There are also cases when a person suffering from ADHD has such a high cognitive potential inherent in him genetically that until adulthood it helps him to cope with difficult tasks without resorting to treatment.
Like any drug aimed at treating a mental disorder, Ritalin has many side effects.
Patients with ADHD, who were not treated in childhood, often cannot be professionally realized or rise above a certain position. Very often, such people are aware of their abilities, but with all their efforts they cannot achieve their plans due to the inability to keep their attention. Sometimes they make mistakes even in very simple and routine activities. There is a strong possibility that with quality treatment in childhood, such a person would have had the opportunity to achieve much higher professional or academic results.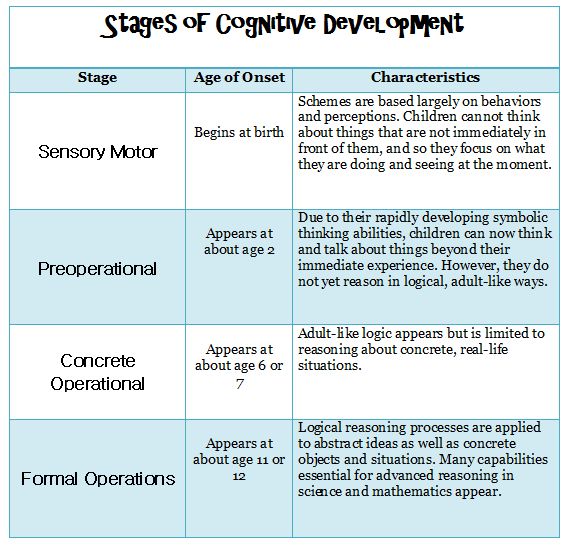
To be diagnosed and diagnosed, an adult patient needs to meet with a psychiatrist and undergo computer testing. The test shows how a person performs various tasks on attentiveness and impulsivity. After conducting these checks, the psychiatrist makes a diagnosis and prescribes treatment.
Attention deficit hyperactivity disorder in adults is usually treated with medication. The most effective drug that is used in the treatment of this disorder is Ritalin. This drug and the drugs that are part of its group have been on the market for a long time, and many studies confirm their effectiveness. Like any drug aimed at treating a mental disorder, Ritalin has many side effects. Therefore, it is very important to choose a medicine, taking into account the individual characteristics of the patient. The course of drug treatment is selected depending on the lifestyle and reactions of the human body.
After the start of treatment, a person begins to experience much less difficulties in solving problems that were previously given to him with difficulty.
![]()
As an additional treatment method, the specialist may suggest biofeedback and neurofeedback. This technique helps to capture brain activity in real time, improve the patient's cognitive function and reduce the symptoms of the disorder. With the help of special electrodes, the device reads information about the work and activity of the brain and translates these data into physiological indicators. Through brain activity, the patient directs the game on the screen and thus learns and improves his cognitive functions. Unfortunately, at the moment there is not enough data confirming the 100% effectiveness of this technique for adults. For children with ADHD, with weekly training, this technique gives very tangible results. It can be assumed that after 2-3 years of neurofeedback and biofeedback treatment, an adult will need to take less Ritalin than before treatment. However, there are no studies to date to support this assumption.
See also
Why do we need a psychotherapist?
A person suffering from ADHD in adulthood must take drugs throughout his life.