How do i know it ocd and not real
How to Know if Your New Thought is OCD, and 6 Concrete OCD-Repelling Strategies
This is a question we get asked a lot at our OCD clinic: “How do I know if this thought is my OCD or if it is a ‘normal’ thought?” It usually happens when a person in treatment has certain familiar “regular” OCD thoughts, but then suddenly gets hit with a new, unfamiliar, unwanted intrusive thought that may or may not be OCD-related.
So even if you know that you have OCD, you may still wonder about that new thought that suddenly popped into your mind, “Is this my OCD acting up again, or is it just a regular, weird thought?”
Some examples of such thoughts include:
What if I spilled water on the floor and an elderly lady will slip on it and die?
What if I get rabies from the road kill?
What if I am that hit-and-run driver that injured a pedestrian earlier today?
What if I stab myself with this knife?
What if I accidentally offended God?
What is the meaning of life?
What if I broke the law without noticing?
What if my thoughts are causing harm to other people?
What if I unintentionally confess to a crime that I didn’t commit?
What if I accidentally cheated on my partner?
What if I sexually assaulted somebody at a party years ago, but can’t remember?
The thing is, the content of these thoughts is not specific to people with OCD. Our brain is constantly generating all kinds of creative thoughts (some more disturbing than others) and our mind chooses which thoughts to engage with. The subtle distinction between the "normal" and the "problematic" lies not in the content of the thought, but in what we decide to do about it.
Anybody can have a random, scary, nonsensical what-if thought such as, "What if I will harm my baby?" "What if I just caused a hit-and-run accident?" "What if I’ll drive my car into the oncoming traffic?"
Non-sufferers usually quickly dismiss these thoughts and continue with their day. If you have a negative thought and shrug it off without giving it much attention, you are unlikely to become obsessed with it.
In this case, your thought process usually goes, "Wow. That was one weird thought.”
But people with OCD tend to take these thoughts very seriously. Their thinking process goes like this, "Oh no! Why did I just have this thought? I must be a horrible person and a danger to others. I should try to prevent this disaster from happening. And I should double-check. And I need to understand what this thought really means."
I should try to prevent this disaster from happening. And I should double-check. And I need to understand what this thought really means."
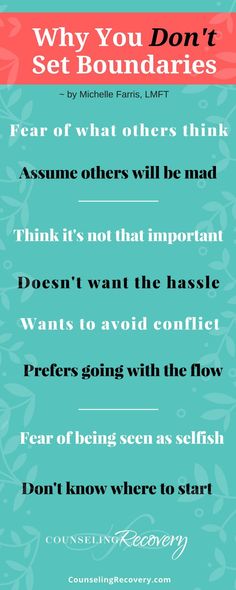
You may find yourself engaging with the new thought by:
Trying very hard to get rid of it.
Trying to replace it with ‘positive’ thoughts or images.
Attempting to figure out the exact message/meaning of this thought.
Wondering what having such thoughts might mean about you as a person.
Asking others for reassurance hoping to hear that the thought is not harmful.
Attempting to neutralize the thought with a mental ritual
If you catch yourself doing any of the above, it likely means that the thought has become an “OCD-thought” and that it interferes with your life.
This over-engagement with the thought creates a never-ending loop of you trying to figure out or neutralize the thought and the thought coming back with vengeance. The more you attempt to either push away or to "understand" the thought, the "stickier" the thought becomes.
The more you attempt to either push away or to "understand" the thought, the "stickier" the thought becomes.
When the thought feels uncontrollable and "sticky" and the efforts to get rid of it don't bring a lasting relief, this may be a sign that your OCD got you on the hook again.
It is especially difficult to identify the problematic “sticky” thoughts when a person has primarily obsessional (“Pure-O”) OCDEvery type of OCD is characterized by obsessions (thoughts that make a person anxious, distressed, fearful, or disgusted) and compulsions (things that the person does to reduce these uncomfortable feelings).
The kind of OCD that primarily has mental obsessions is often called "Pure O," implying that the obsessions and compulsions are purely mental (not visible). Unfortunately, health professionals often miss the diagnosis of OCD in these cases because they can't observe the compulsions. This is tragic as the sufferers go undiagnosed and untreated for many years (sometimes they suffer silently for their entire life).
The good news is that the "Pure O" kind of OCD is just as treatable as the other OCD categories with the same ERP approach.
Where to start when addressing the new obsession?The first step is to really understand how the vicious cycle of OCD develops. The more effort you put into getting rid of your thoughts, the more obsessed you are likely going to become. This includes following the popular (and uninformed) advice about trying to replace a negative thought with a positive one, to snap a rubber band on your wrist trying to stop the thought, or try to distract yourself from the thoughts by visualization, breathing, or relaxation. These tactics will force you to give these thoughts even more importance and hence, will gradually lead to more obsessing.
In fact, trying to get rid of the thoughts reinforces “the pathway of fear” in your brain. As this pathway strengthens, the mental rituals become almost automatic.
The goal of OCD treatment is to start creating and strengthening an alternative neural pathway – the pathway of “I can have an obsession and not succumb to OCD demands. ” The more you use this new neural pathway in various situations, at various times of day, with different people, and in different moods, the more you develop and fortify it.
” The more you use this new neural pathway in various situations, at various times of day, with different people, and in different moods, the more you develop and fortify it.
The following are some steps to start creating this new, healthy pathway:
6 strategies for nipping the sticky thoughts in the bud:1. Start practicing seeing your thought just as it is – a thought. It is not a fact or a threat.
2. When you notice an unwanted obsessive thought, label it as such. Say to yourself: “I notice that I'm having a thought that [X is going to happen].” This is how you learn to become an observer of your thoughts instead of a willing participant in useless rumination, negotiation, and other attempts to neutralize or figure out the thought.
3. Allow the thought to come and go without trying to force it to go away or to figure it out.
4. Let go of the illusion that you can control your thoughts. You may be able to do it temporarily, but it takes too much of your energy and time to sustain it in the long run.
5. In spite of what many OCD self-help books will teach you, don’t aim to lower your anxiety. If the anxiety goes down, enjoy the good feeling. If it doesn’t – it means that you have an extra opportunity to practice building your new robust neural super-highway, so having high anxiety and, nevertheless, resisting the compulsion will benefit you even more.
6. Reward yourself for having an OCD thought, experiencing high anxiety, and still not doing the mental ritual. This is how you know that you are on the right track.
Bonus point: If you just had a thought that the number of strategies above (6) may bring bad luck or cause harm to you or others, deem this thought an OCD-thought and practice the strategies described here right away.
Treatment: It is very important to seek treatment for OCD. The only evidence-based effective treatment for OCD is Exposure with Response Prevention (ERP), which is a very specific part of Cognitive Behavior Therapy (CBT). From our experience, when ERP is combined with Acceptance and Commitment Therapy (ACT), the treatment is even more effective. This disorder does not go away on its own and the earlier you start treatment, the better.
From our experience, when ERP is combined with Acceptance and Commitment Therapy (ACT), the treatment is even more effective. This disorder does not go away on its own and the earlier you start treatment, the better.
To summarize, it’s not the content of the thought that determines whether it’s an OCD thought. What gives you a clue is your appraisal of the thought, your level of engagement with it, and the extent to which you take the thought seriously.
Hence, if you are not sure, I suggest you assume that the thought is an OCD thought and treat it accordingly – with lack of attention and respect. Let the thought come and go, and re-focus on connecting to the present moment while practicing the strategies described above.
Have you had new obsessions pop up in your mind, masquerading as legitimate concerns? Have you learned to identify them early. Or have you been missing them? Please share in the comments below!
If you enjoyed this article, follow us on Facebook for more great tips and resources!
Anna Prudovski is a Psychologist and the Clinical Director of Turning Point Psychological Services. She has a special interest in treating anxiety disorders and OCD, as well as working with parents.
She has a special interest in treating anxiety disorders and OCD, as well as working with parents.
Anna lives with her husband and children in Vaughan, Ontario. When she is not treating patients, supervising clinicians, teaching CBT, and attending professional workshops, Anna enjoys practicing yoga, going on hikes with her family, traveling, studying Ayurveda, and spending time with friends. Her favorite pastime is reading.
Related Posts
How Do You Know If Your Intrusive Thoughts Are From OCD?
Almost everyone experiences unpleasant thoughts they would rather not have. But how can you tell when intrusive thoughts are an everyday part of life or a component of obsessive-compulsive disorder (OCD)?
What is an intrusive thought?
Intrusive thoughts are unwanted thoughts, images, or urges that pop into your head and can occur out of nowhere. They can be brief fleeting thoughts such as “What if I drop this glass of water?” or more distressing ones like “I’m an awful mom” because you aren’t 100% interested in playtime with your child, or “I’m contaminated after touching that public bathroom door with my bare hand!” These thoughts might be about a hypothetical violent scenario, for example, you might find yourself wondering, “What if I pushed this guy next to me in front of the oncoming train?”
Intrusive thoughts can be about relationships, such as wondering if you’re a good partner, safety, fear of death, or protection of a loved one. Everyone has intrusive thoughts, and usually, they leave your mind as quickly as they come, and you don’t identify with them as something that makes you a bad person.
Everyone has intrusive thoughts, and usually, they leave your mind as quickly as they come, and you don’t identify with them as something that makes you a bad person.
For people with OCD, it’s more complicated. People with OCD may experience intrusive thoughts more often and may become more worried by them than people without OCD. The thoughts latch onto your mind, and you often fear they won’t cease until you can find a way to relieve yourself of the anxiety. You start thinking more and more about this initial thought, and suddenly it grows in your head. What if I really am a bad mother? What if I never want to play with my own child again? Generally, the thoughts center around something that matters deeply to you where the consequences are devastating, which is partially why it can feel so distressing.
When you have OCD, these thoughts become distressing to the point where you feel you must find a way to eradicate them through taking action.Here’s where compulsions come into play. For someone with OCD, it can feel impossible to let these thoughts go, no matter how irrational they seem, and they lead you to engage in compulsions in order to alleviate the intrusive thoughts. For example, you might find yourself spending hours on Google trying to figure out how to know whether you’re a good mother. What makes a good mother? How can you tell if you are a bad one or a good one? This might lead to a downward spiral that won’t stop until you have enough reassurance against what you’re afraid of.
For someone with OCD, it can feel impossible to let these thoughts go, no matter how irrational they seem, and they lead you to engage in compulsions in order to alleviate the intrusive thoughts. For example, you might find yourself spending hours on Google trying to figure out how to know whether you’re a good mother. What makes a good mother? How can you tell if you are a bad one or a good one? This might lead to a downward spiral that won’t stop until you have enough reassurance against what you’re afraid of.
The compulsions could also be mental, where you find yourself thinking about particular anxiety for hours on end about something that happened in the past. For example, you can’t stop remembering all the times you babysat kids and gave them baths but not being 100% certain you didn’t touch them inappropriately. You might replay these memories for hours until you feel reassured enough for these thoughts to temporarily loosen their grip on your mind.
What characterizes an intrusive thought as a component of OCD is how much emotional distress these thoughts cause you and whether you try to neutralize these thoughts via compulsions.
Even if it might seem like these intrusive thoughts will always be running your life, fortunately, there are treatment options available to people suffering from them. Exposure Response Prevention (ERP), a type of Cognitive Behavior Therapy, can help you gain some distance from these thoughts so that they no longer control your actions. Rather than trying to get rid of the intrusive thoughts completely, which isn’t possible, ERP can help you alleviate the distress these thoughts cause.
An ERP-trained therapist can help by reviewing which intrusive thoughts are causing you anxiety and then work with you to come up with a specialized treatment plan to help alleviate them through gradual exposure. For example, a therapist might have you write down an intrusive thought that is causing you anxiety, and work towards exposure until these thoughts are no longer as triggering or the urge to use compulsions lessens.
If you’re interested in learning more about ERP, you can schedule a free call with the NOCD clinical team to find out how this type of treatment can help you. All of our therapists specialize in OCD and receive ERP-specific training. ERP is considered the gold standard for OCD treatment and has been found to be 90% effective.
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed.
 Do I have OCD?
Do I have OCD? Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasurable.
 The fact that an action will help reduce anxiety is not considered pleasant in this sense.
The fact that an action will help reduce anxiety is not considered pleasant in this sense. - Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist.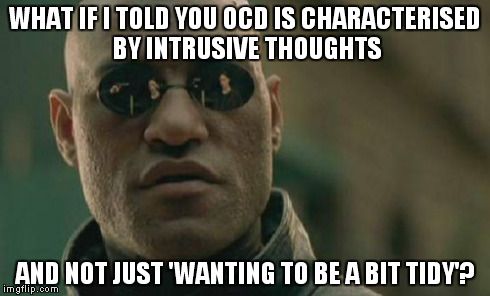 At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order.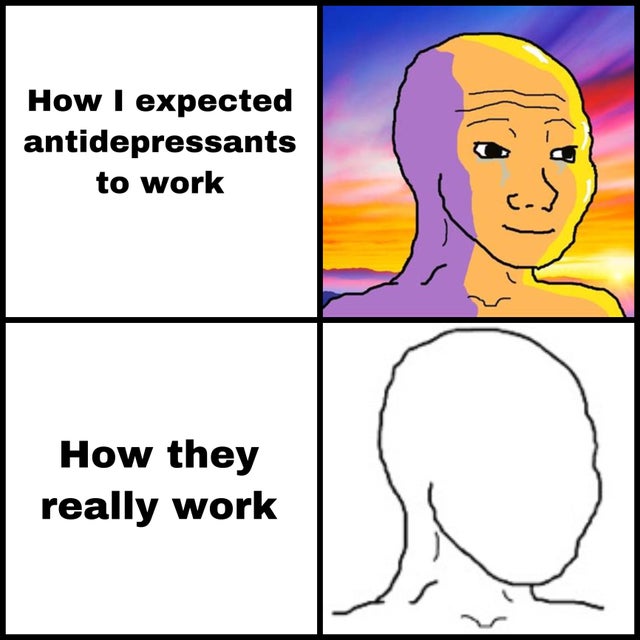 Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
This is how a referral for hospitalization to a day hospital looks like The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man did not let me stop the treatment
They noticed the changes, but my young man did not let me stop the treatment Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 P |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refusedTreatment
Second hospitalization and psychotherapy After six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job.
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
What is alexithymia and how to understand your feelings
Alexithymia is not a psychiatric diagnosis, it is a condition in which a person is unable to describe and understand his feelings and emotions. It leads not only to problems in interpersonal relationships, but can also cause psychosomatic illnesses. We talked to people living with alexithymia and learned from experts how to deal with it.
We talked to people living with alexithymia and learned from experts how to deal with it.
“It’s like not being able to taste and smell”
Tatyana, 21 years old
I have schizoaffective disorder, obsessive-compulsive disorder and Asperger’s syndrome — the first signs were in adolescence, diagnosed several years ago. As a child, for the first time, I realized that it was difficult for me to define emotions and feelings. I could cry and didn't realize why. Because of the pain or because I'm sad.
When I realize that I feel something, I try to pay attention to the sensations in my body. If heaviness appears in the chest, most likely, these are negative emotions - sadness, sadness, resentment. If warmth is felt in the body and limbs, then it must be positive.
For a long time I did not understand what love and sympathy are and whether I can experience them. I was able to distinguish them from other feelings when I met my boyfriend at the age of eighteen. This is a completely different level of feelings that I felt physically : my heart beat faster when I thought about him, I wanted to be near him, when talking it became hot, my palms sweated, there was a feeling of intoxication in my head. And somehow I realized that this is something new and that I can love someone.
This is a completely different level of feelings that I felt physically : my heart beat faster when I thought about him, I wanted to be near him, when talking it became hot, my palms sweated, there was a feeling of intoxication in my head. And somehow I realized that this is something new and that I can love someone.
Fear also manifests itself more physically: lack of air, headache, severe tinnitus, spasm in the intestines, muscle stiffness, coldness in the body, trembling. It looks like the beginning of a cold - I would say so that it was more understandable.
The most difficult thing for me is to tell my relatives how I feel if they ask me about it or wait in a conversation for me to say something about emotions. I just feel like I can't find the words for this, it's like there aren't any, and I don't know what to say. At such moments, people think that I do not feel anything, and my silence confuses them.
Sometimes relatives get angry - apparently, they are waiting for an emotional response in the course of a conversation, and I often don’t know what to do, what emotion to show, squeeze out of myself. But I think that they are not angry on purpose. Once I talked with my mother about further education, I explained where and for whom I want to study, to which she replied that I was speaking without interest and emotions, as if I didn’t care.
But I think that they are not angry on purpose. Once I talked with my mother about further education, I explained where and for whom I want to study, to which she replied that I was speaking without interest and emotions, as if I didn’t care.
You seem to be deprived of the opportunity to fully experience emotions. It’s like they don’t exist, and you don’t know what they are, because anger and joy feel equally insipid. For me, it's like living with a constant runny nose and not feeling the taste and smell.
I didn't tell my parents about alexithymia and Asperger's syndrome. They are of the old school, all people with autism for them are those who cannot speak and are kept in boarding schools. Also, we are not very close, and I don’t even know how to gently talk about my states. I tried to explain my mental disorder to my mother, but for her it’s “you can’t control yourself”, so all my stories and articles shown on this topic are useless. I have a physical disability - my parents treat me the way they treat people with disabilities in Russia: they consider me weak and unable to work. They are aware that I am mentally ill, but if you also tell them about problems with emotions and Asperger's syndrome, they will treat me with even more pity and think that I am not like normal children, and that this is their punishment from God. But my young man is aware of my problems, and after he found out about them, we began to understand each other better.
They are aware that I am mentally ill, but if you also tell them about problems with emotions and Asperger's syndrome, they will treat me with even more pity and think that I am not like normal children, and that this is their punishment from God. But my young man is aware of my problems, and after he found out about them, we began to understand each other better.
I am in therapy and it is very difficult for me to talk about how I feel about my emotions. But the more time passes, the more I learn to describe my emotions in images. For example, sadness is a dark and cloudy cloud . It's a strange experience, but I like it.
"I was considered a callous and unsociable person"
White, 35 years old
I have Bipolar 2 disorder. I am currently in remission and continue medication. I have long felt that it is difficult for me to describe emotions and feelings, but for the first time I realized this about ten years ago. Then we often played word games in the company, and several times I got questions of the format “what do you feel about . .. (a person, phenomenon, event, and so on)?” Such questions plunged me into a stupor, and at the same time I noticed that other people had no problems with answers. I tried to understand how they find words so quickly, for a while I even suspected that they were making them up on the go. Later, I accidentally stumbled upon an article on alexithymia on the Internet and recognized the familiar symptoms.
.. (a person, phenomenon, event, and so on)?” Such questions plunged me into a stupor, and at the same time I noticed that other people had no problems with answers. I tried to understand how they find words so quickly, for a while I even suspected that they were making them up on the go. Later, I accidentally stumbled upon an article on alexithymia on the Internet and recognized the familiar symptoms.
In my case, alexithymia does not affect creativity and professional tasks: I love fiction based on the problems of human relationships, sometimes I write prose, poetry, songs myself. Feelings are easier to formulate on behalf of a lyrical hero, besides, this is verbalization training.
But in my personal life and communication with friends, alexithymia leads to problems: relatives often noticed that I had difficulties with expressing emotions - before, they were mostly angry and took the position “why can’t I immediately say normal.” For a long time I was considered a callous and unsociable person, because I did not understand how to express various kinds of empathy. Several times I quarreled with my girlfriend almost to the point of breaking up, because my reaction was “wrong”: it did not correspond to the situation and incorrectly displayed my own emotions.
Several times I quarreled with my girlfriend almost to the point of breaking up, because my reaction was “wrong”: it did not correspond to the situation and incorrectly displayed my own emotions.
After I started to warn about my problem, there were fewer conflicts, we started talking more about feelings with loved ones.
I also have trouble making decisions because of the inability to understand what feeling guides the opinion, but this is rather good: you have to learn to look at things from a rational position, fixing the pros and cons, instead of succumbing to emotions.
“My feelings are a mystery to myself”
Anton, 30 years old
Until recently, I did not know about such a problem as alexithymia, but I began to notice that I did not understand my emotions and feelings in my youth. I could not understand how to react to the actions of classmates and friends - when to laugh, get angry and upset. I still can't tell a joke from an insult if it's not obvious. For example, I can be offended to tears if they say “fool” to me in a friendly way, and laugh when I hear a mate addressed to me.
For example, I can be offended to tears if they say “fool” to me in a friendly way, and laugh when I hear a mate addressed to me.
Trying to socialize, I repeated after other people, but it looked awkward, I did not catch the norms. I was bullied at school, but I didn’t know how to react: I was silent on insults, and for a slight irony I could get into a fight, then I was ashamed and apologized.
When I started working, I could not settle down in the team, because I did not read other people's attitude towards me and, accordingly, did not know how I should treat people. Many said that I was being arrogant, which surprised and upset me, because I was just silent all the time. My unsociableness leads to the fact that, despite high professional performance, career growth and a leadership position do not shine for me. In the humanitarian field in which I work, relationships with people, the ability to understand and read the emotions of others, are extremely important, especially if you want to manage a team.
Relations with friends and close people do not develop for the same reason - mutual misunderstanding, which even strong romantic or friendly affection could not overcome. I felt the difference in the direction of these attachments only by the presence of sexual desire, which manifests itself in a standard human way. However, his absence did not stop me from rash acts: I confessed my romantic love to my girlfriends and even friends, although I did not think about sexual relations with them, I was simply drawn to them and in their presence it became physically warm and comfortable. People, to put it mildly, were surprised in response to my proposal to meet, and the guys expressed dislike. Relations with many wonderful people were ruined once and for all, even an apology did not help restore friendship.
And after the breakup, I didn't understand what I was feeling - sometimes I was sad, sometimes I was happy, and it drove me crazy. When the ex-girlfriend moved out from me, my breath often took hold in an empty apartment, my pulse quickened, especially when I recalled our life. The reasons are not clear, because there is nothing to be offended and angry at, because we parted on my initiative. And somehow a friend posted a photo from the party, and everything boiled inside me, my breath also caught (it seems that this is my standard reaction to anything), but I did not understand what was happening inside me. I called him and asked why he went there, which sounded very stupid - he did not understand this question, and I no longer understood why I was asking it, and even in a breaking voice. My friends know that I am not a party lover in principle, and I know this about myself, so I did not hold any claims in my mind, but some emotions were overwhelmed, judging by the physical manifestations. I would call them meaningless, phantom.
The reasons are not clear, because there is nothing to be offended and angry at, because we parted on my initiative. And somehow a friend posted a photo from the party, and everything boiled inside me, my breath also caught (it seems that this is my standard reaction to anything), but I did not understand what was happening inside me. I called him and asked why he went there, which sounded very stupid - he did not understand this question, and I no longer understood why I was asking it, and even in a breaking voice. My friends know that I am not a party lover in principle, and I know this about myself, so I did not hold any claims in my mind, but some emotions were overwhelmed, judging by the physical manifestations. I would call them meaningless, phantom.
Trying to explain to people that I have problems with emotions does not help: even those closest to me are sure that this is a whim and I just don't want to control myself and "try to understand others."
When I first went to a psychiatrist, he said that problems with emotions are a neurosis. I was treated with various drugs for a long time, but the situation did not get better, until now my feelings are a mystery to myself. Psychotherapy is weak, but it helps: the doctor taught to determine how feelings differ from emotions, but it is still difficult to recognize them. I learned that emotion is a small, short-term acute sensation, like a flash, lightning, you don’t have time to think about anything. And a feeling is a long-term state accompanied by a bunch of thoughts. For example, I hit a chair and screamed, my hands clenched, instinctively hit the chair in response - it means that the emotion of anger arose. But I had a colleague at a former job who set me up, and if we went on the same shift, then I felt muscle tension, heart palpitations and often thought about how he could be such a lousy person.
I was treated with various drugs for a long time, but the situation did not get better, until now my feelings are a mystery to myself. Psychotherapy is weak, but it helps: the doctor taught to determine how feelings differ from emotions, but it is still difficult to recognize them. I learned that emotion is a small, short-term acute sensation, like a flash, lightning, you don’t have time to think about anything. And a feeling is a long-term state accompanied by a bunch of thoughts. For example, I hit a chair and screamed, my hands clenched, instinctively hit the chair in response - it means that the emotion of anger arose. But I had a colleague at a former job who set me up, and if we went on the same shift, then I felt muscle tension, heart palpitations and often thought about how he could be such a lousy person.
The hardest thing for me is to tell the doctors what I'm experiencing: no matter what words I choose, everything seems like a lie or a fantasy. This applies to both mental and physical sensations. As soon as I go into the office of a gastroenterologist or a therapist and start complaining, I listen to myself more carefully and start thinking that I dreamed the sensations. It’s the same with a psychotherapist and a psychiatrist: it seems that I’m actually a healthy dreamer, because I can’t convey exactly how I feel, and specialists are not telepaths and cannot understand.
As soon as I go into the office of a gastroenterologist or a therapist and start complaining, I listen to myself more carefully and start thinking that I dreamed the sensations. It’s the same with a psychotherapist and a psychiatrist: it seems that I’m actually a healthy dreamer, because I can’t convey exactly how I feel, and specialists are not telepaths and cannot understand.
"I can't put my feelings into human language"
Kristina, 28 years old
I went to a psychologist with borderline and depression issues, one day he asked me to describe myself and I felt confused because I didn't know Who am I. I told him that I consist of layers: on the outside there is a polite shell, under it is an evil gopnik, and under it is a kind soul that saves everyone, and it is she who is protected by the gopnik. Then again something dark that I do not understand and am afraid to analyze, and so on ad infinitum. Later, these layers emerged into some subpersonalities, and their emotions were perceived as alien, which I cannot understand or control. I gave them names, and they speak in my head like separate parts of me: kind, aggressive, overly emotional, my ordinary.
I gave them names, and they speak in my head like separate parts of me: kind, aggressive, overly emotional, my ordinary.
I can describe my feelings with the help of a table of feelings, in psychotherapy pairs (I studied as a doctor) we were offered to use it to tell others about our feelings. But sometimes I experience things that are not in this table or there is no name for these feelings.
I have developed empathy, I easily understand others, but inside of me is either a mixture [of feelings], or nothing at all. This does not affect my hobby: I draw the necessary emotions for my characters, sometimes the drawing helps me figure out what I feel, or others begin to understand it - sometimes they are horrified. Due to alexithymia, I do not communicate with people much, because I cannot respond with the emotional reactions they need.
For example, if a person raised their voice at me, I may cry, even if I just feel like I'm being pressured, or I get too angry and yell. There is no average response to pressure. If they regret it, I roar.
There is no average response to pressure. If they regret it, I roar.
The most difficult thing is to tell those who expect warmth from me that I experience this warmth, but I don’t show it, because I don’t know how. This feeling is blurred, it is impossible to concretize it in words. Also, I can’t tell people what specifically offended me, because words get stuck or I can’t put feelings into human language. It's hard to be locked up and not understand how I really feel . I ignore my feelings more often than I track.
Alexithymia often leads to psychosomatic manifestations: when I am nervous, the temperature rises to 37–37.5 degrees, pains in the abdomen, heart, head, teeth ache, allergies begin (I itch, I get covered with a rash), breathing problems (I can’t do breath or I don’t feel oxygen in the air), anything can hurt at all, regardless of the absence of physical pathology.
Why does alexithymia occur and how to deal with it?
Alexithymia is most characteristic of autism spectrum disorders, but can accompany any mental disorder (depression, personality disorders, etc. ). It is associated with the mechanism of formation and maintenance of a psychosomatic symptom, but not the only reason for its occurrence. Clients with alexithymia, as a rule, first of all turn to somatic doctors with physical discomfort.
). It is associated with the mechanism of formation and maintenance of a psychosomatic symptom, but not the only reason for its occurrence. Clients with alexithymia, as a rule, first of all turn to somatic doctors with physical discomfort.
According to the results of some studies, difficulties with the expression of emotions are more common in men than in women, alexithymia is practically not studied in people of a different gender identity. However, the quality of most research on alexithymia is quite low.
The exact causes of this condition have not yet been identified. There is evidence that mirror neurons are involved in the occurrence of alexithymia, structures such as the amygdala, insula and cerebellum are involved. Violation of dopaminergic metabolism in these structures is associated with manifestations of alexithymia.
Nevertheless, the environment plays a significant role in the development of difficulties with understanding one's emotions: whether the child sees the expression of emotions, hears their names, whether they tell him what emotions are, how they manifest themselves.
Alexithymia can lead to difficulties in building or maintaining interpersonal relationships - in these cases, I would recommend contacting a specialist. If you notice that it is difficult for you to interact with people, there is a feeling that no one understands your goals, motives, and it is often difficult for you to understand people when they talk about their emotions, you can independently study materials about emotions, gradually learn to notice them from yourself and other people, observe them and express.
By itself, this problem does not require medical treatment. A psychotherapist works with alexithymia at the beginning of any psychotherapy, since it is important for a specialist to understand how the client feels in problem situations.
Relatives can help a person by talking about their emotions and thereby showing the experience of living them, and also by asking about the person's experiences, thereby drawing his attention to the emotional sphere.
Alexithymia is indeed common among my clients and makes interaction in the first meetings much more difficult. At the beginning of the work, the specialist collects information about what is happening with the client (about his behavior, thinking, emotions), of course, alexithymia hinders this process. In such cases, we dedicate several meetings to the client to find out what emotions are, how they manifest themselves, how they feel, learn to notice them in themselves, name them, observe them. The most difficult for me case of alexithymia in a client required eight meetings of work on the identification, observation, description and expression of emotions.
How does alexithymia affect physical health?
Alexithymia can lead to the occurrence of psychosomatic symptoms - pain, squeezing, bursting, tingling and others, but at the same time, according to tests and studies, doctors do not find anything.
There is evidence that patients with higher levels of alexithymia suffering from bronchial asthma require longer hospital stays.