295.70 schizoaffective disorder bipolar type
Schizoaffective Disorder - StatPearls - NCBI Bookshelf
Continuing Education Activity
Schizoaffective disorder is among the most frequently misdiagnosed psychiatric disorders in clinical practice. Due to concerns about the reliability and utility of the diagnostic criteria for schizoaffective disorder, some researchers have proposed revisions, while others have suggested altogether removing the diagnosis from the Diagnostic and Statistical Manual of Mental Disorders. This activity describes limitations and challenges related to the diagnostic criteria and highlights the interprofessional team's role in caring for patients with psychiatric disorders.
Objectives:
Describe the pathophysiology of schizoaffective disorder.
Outline the classic clinical presentation of a patient with schizoaffective disorder.
Summarize the treatment options for patients with schizoaffective disorder.
Describe the importance of collaboration and communication amongst the interprofessional team to improve patient compliance with treatment and thus improve outcomes for patients with schizoaffective disorder.
Access free multiple choice questions on this topic.
Introduction
Schizoaffective disorder is one of the most misdiagnosed psychiatric disorders in clinical practice.[1] In fact, some researchers have proposed revisions to the diagnostic criteria, and others have suggested removing the diagnosis altogether from the DSM-5.[2] There were significant concerns regarding the reliability and utility of the diagnosis when it was first introduced in the DSM.[2] The challenges lie within the diagnostic criteria itself since the disorder is part of a spectrum that shares criteria with many other prominent psychiatric disorders found in clinical practice.
Etiology
The term schizoaffective disorder first appeared as a subtype of schizophrenia in the first edition of the DSM. It eventually became its own diagnosis despite a lack of evidence for unique differences in etiology or pathophysiology. Therefore, there have been no conclusive studies on the etiology of the disorder. However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
Some studies show that as high as 50% of people with schizophrenia also have comorbid depression.[3] The pathogenesis of both mood disorders and schizophrenia is multifactorial and covers a range of risk factors, including genetics, social factors, trauma, and stress.[4] Among people with schizophrenia, there is a possible increased risk for first-degree relatives for schizoaffective disorder and vice-versa; there may be increased risk among individuals for schizoaffective disorder who have a first-degree relative with bipolar disorder schizophrenia, or schizoaffective disorder.[5]
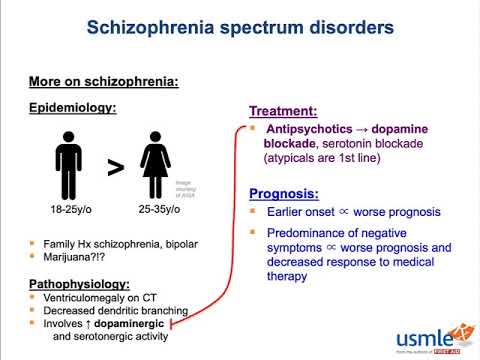
Epidemiology
The diagnostic criteria for schizoaffective disorder have been reworded and addended since its inclusion in the DSM, making it difficult to subsequently conduct appropriate epidemiological studies. Thus, there have been no large-scale studies on the epidemiology, incidence, or prevalence of schizoaffective disorder.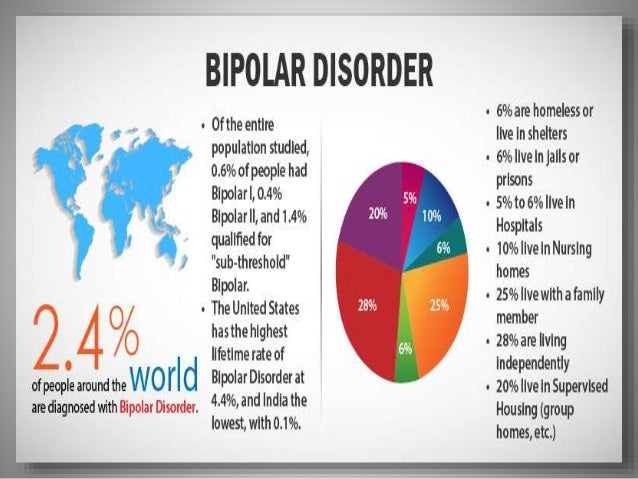 Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Pathophysiology
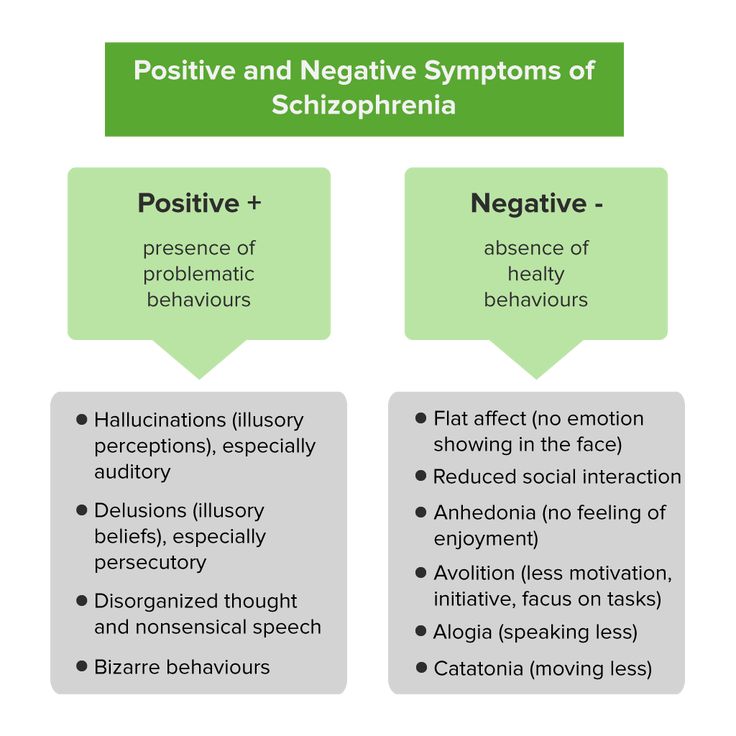
The exact pathophysiology of schizoaffective disorder is currently unknown. Some studies have shown that abnormalities in dopamine, norepinephrine, and serotonin may play a role.[9] Also, white matter abnormalities in multiple areas of the brain, particularly the right lentiform nucleus, left temporal gyrus, and right precuneus, are associated with schizophrenia and schizoaffective disorder.[10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
History and Physical
The first step in evaluation is obtaining a complete medical history while focusing on the diagnostic criteria for schizoaffective disorder.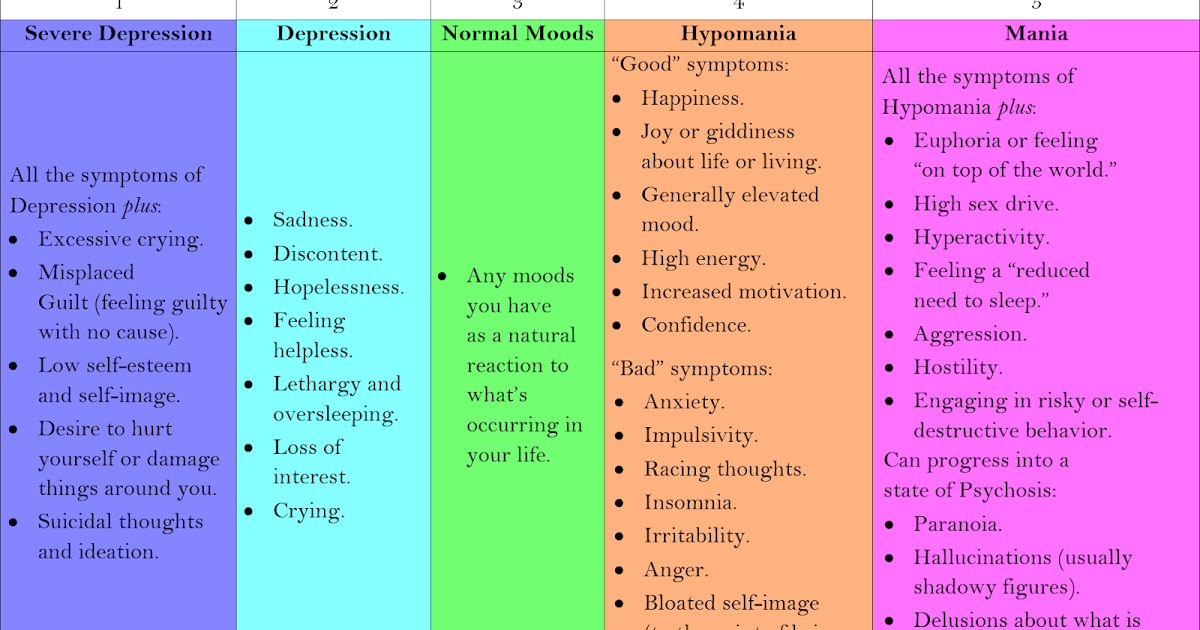
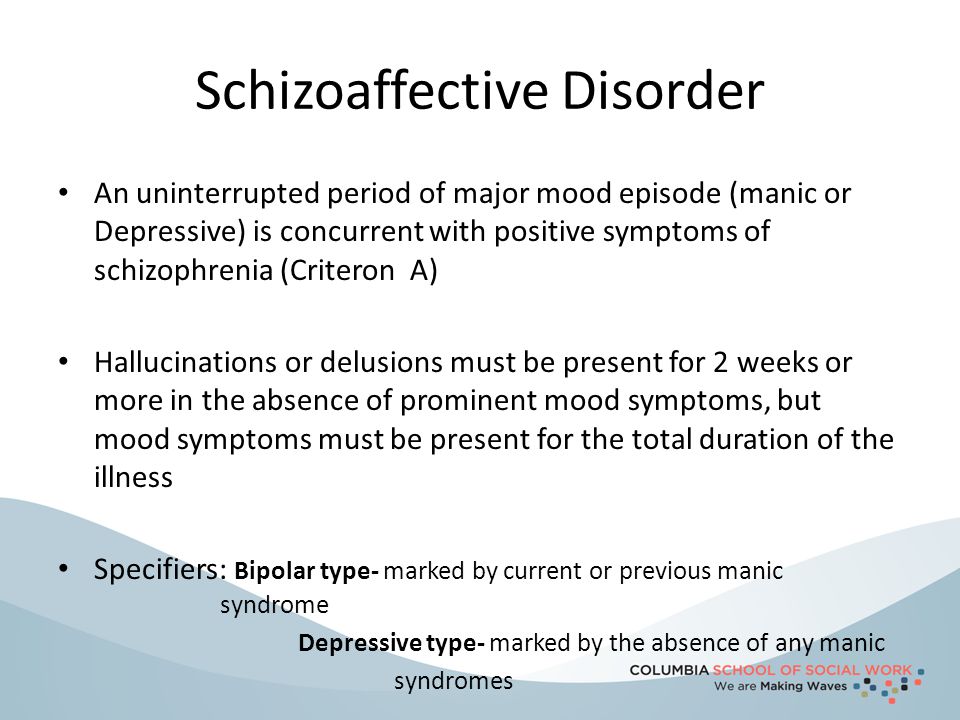
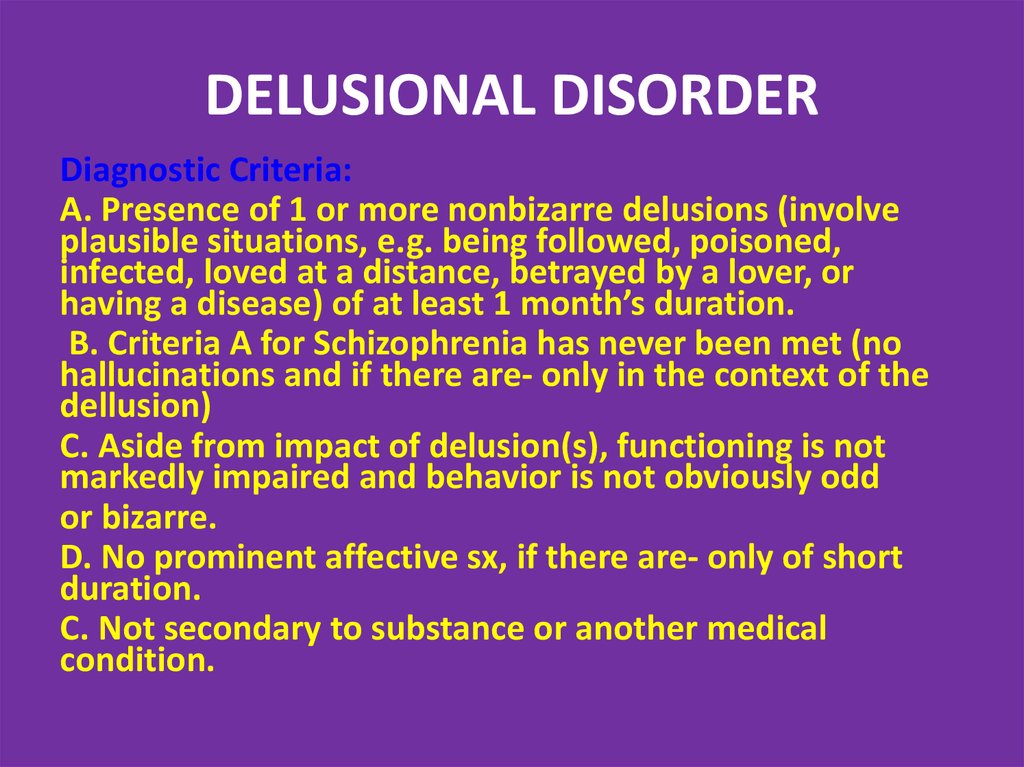
The specific DSM-5 criteria for schizoaffective disorder are as follows[1]:
A. An uninterrupted duration of illness during which there is a major mood episode (manic or depressive) in addition to criterion A for schizophrenia; the major depressive episode must include depressed mood.
Criterion A for schizophrenia is as follows[13]:
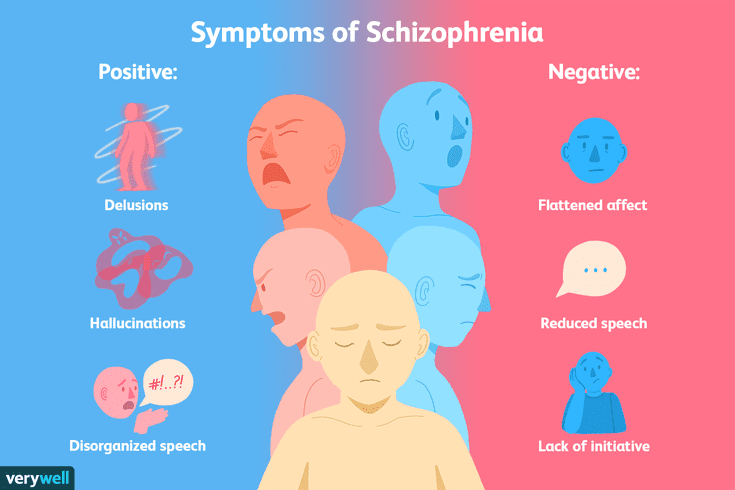
Two or more of the following presentations, each present for a significant amount of time during a 1-month period (or less if successfully treated). At least one of these must be from the first three below.
Delusions
Hallucinations
Disorganized speech (e.g., frequent derailment or incoherence).
Grossly disorganized or catatonic behavior
Negative symptoms (i.e., diminished emotional expression or avolition.)
B. Hallucinations and delusions for two or more weeks in the absence of a major mood episode (manic or depressive) during the entire lifetime duration of the illness.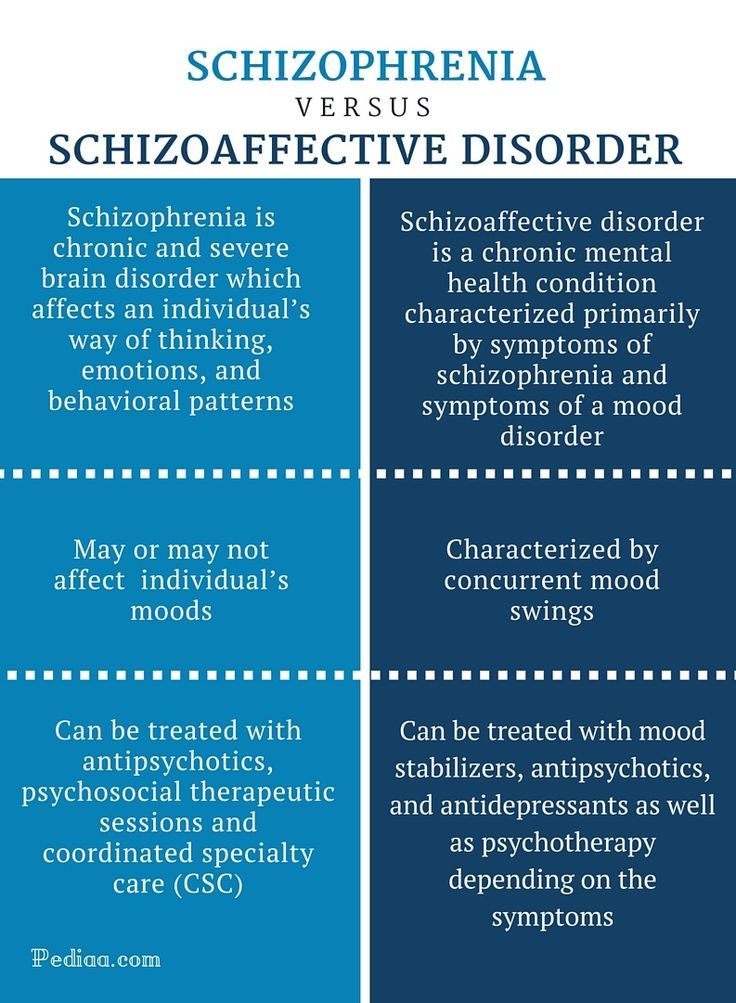
C. Symptoms that meet the criteria for a major mood episode are present for most of the total duration of both the active and residual portions of the illness.
D. The disturbance is not the result of the effects of a substance (e.g., a drug of misuse or a medication) or another underlying medical condition.
The following are specifiers based on the primary mood episode as part of the presentation.
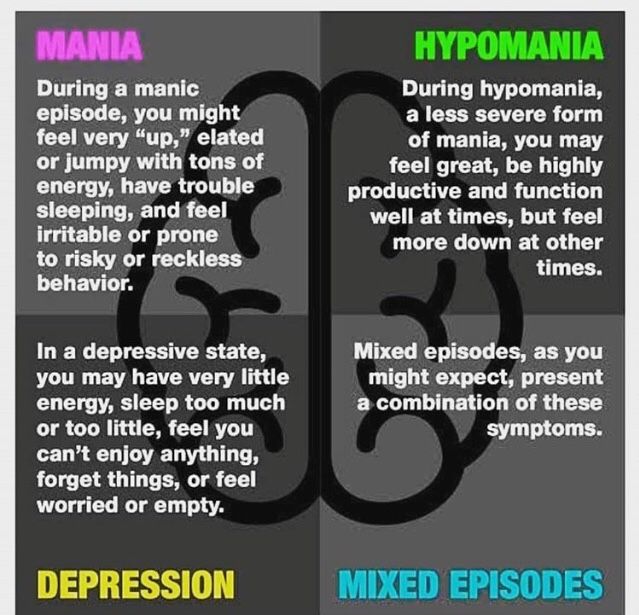
Bipolar type: includes episodes of mania and sometimes major depression.
Depressive type: includes only major depressive episodes.
Please note the patient must meet the criteria for A-D above to be diagnosed with schizoaffective disorder. It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
The next step of evaluation is the objective and physical portion. A thorough mental status examination (MSE), physical examination, and neurologic examination should be completed to help rule out other differential diagnoses.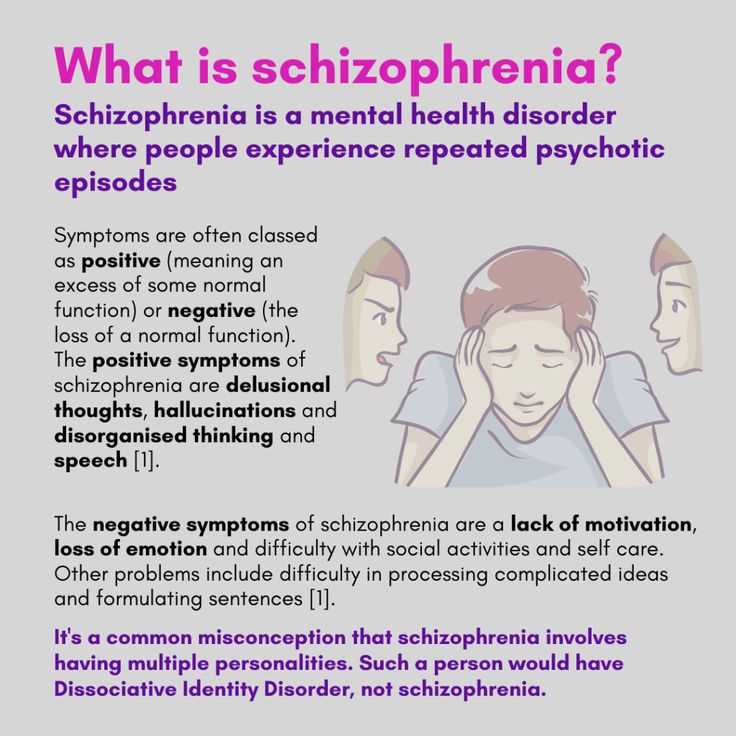
Evaluation
The following workup is optional and typically not needed to make the diagnosis. The history and physical are the mainstays of diagnosis. However, some elect to include additional tests or imaging to aid in the diagnosis, such as MRI (magnetic resonance imaging), EEG (electroencephalography), or CT (computed tomography).
Laboratory studies are tailored to the patient’s history, especially for those who have an atypical presentation.
Complete blood count (CBC)
Lipid panel
Urine drug screen
Urine pregnancy test
Urinalysis
Thyroid-stimulating hormone (TSH) level
Rapid plasma reagent
HIV test
If the patient's neurologic exam is found to be aberrant, performing a brain MRI or CT to rule out any suspected intracranial abnormalities may be considered.
Treatment / Management
The treatment of schizoaffective disorder typically involves both pharmacotherapy and psychotherapy. The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
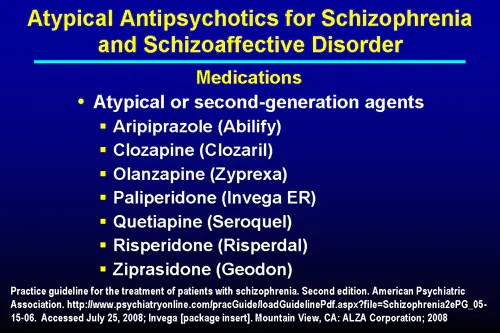
Pharmacotherapy
Antipsychotics: Used to target psychosis and aggressive behavior in schizoaffective disorder. Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
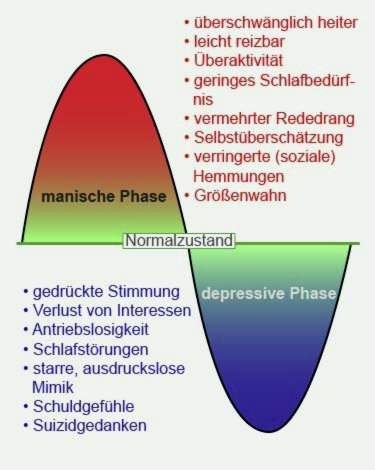
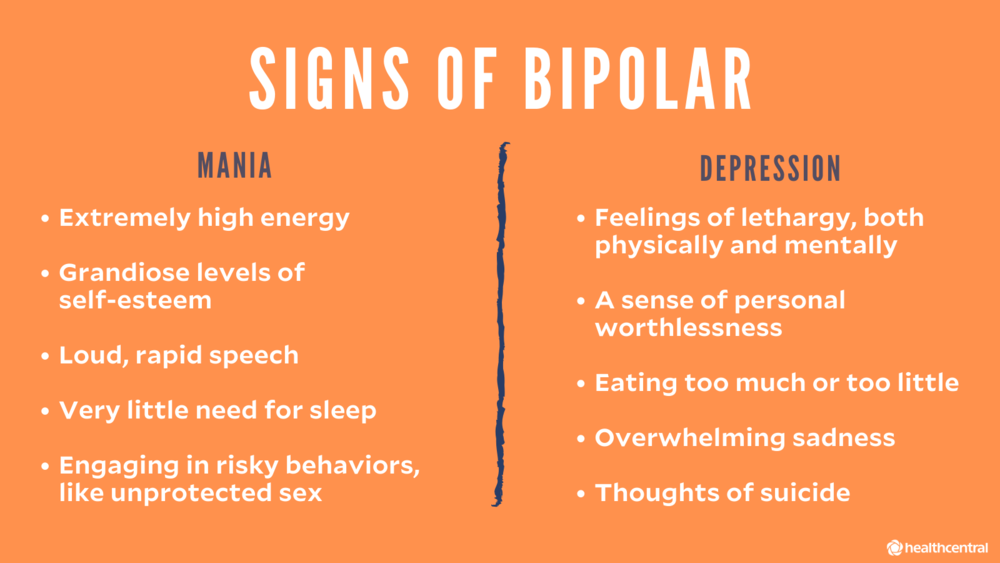
Mood-stabilizers: Patients who have periods of distractibility, indiscretion, grandiosity, a flight of ideas, increased goal-directed activity, decreased need for sleep, and who are hyper-verbal fall under the bipolar-specifier for schizoaffective disorder. Consider the use of mood-stabilizers if the patient has a history of manic or hypomanic symptoms. These include medications such as lithium, valproic acid, carbamazepine, oxcarbazepine, and lamotrigine which target mood dysregulation.[21][22][23][24]
Antidepressants: Used to target depressive symptoms in schizoaffective disorder. Selective-serotonin reuptake inhibitors (SSRIs) are preferred due to lower risk for adverse drug effects and tolerability when compared to tricyclic antidepressants and selective norepinephrine reuptake inhibitors.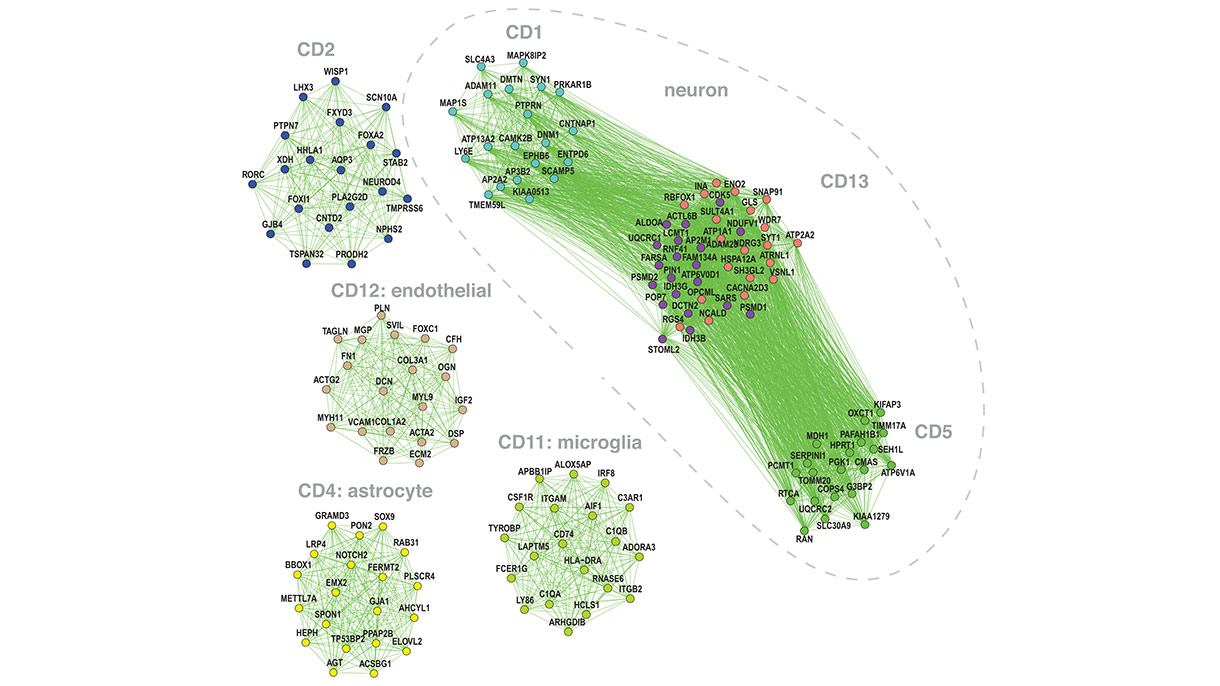 [25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
[25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
Psychotherapy
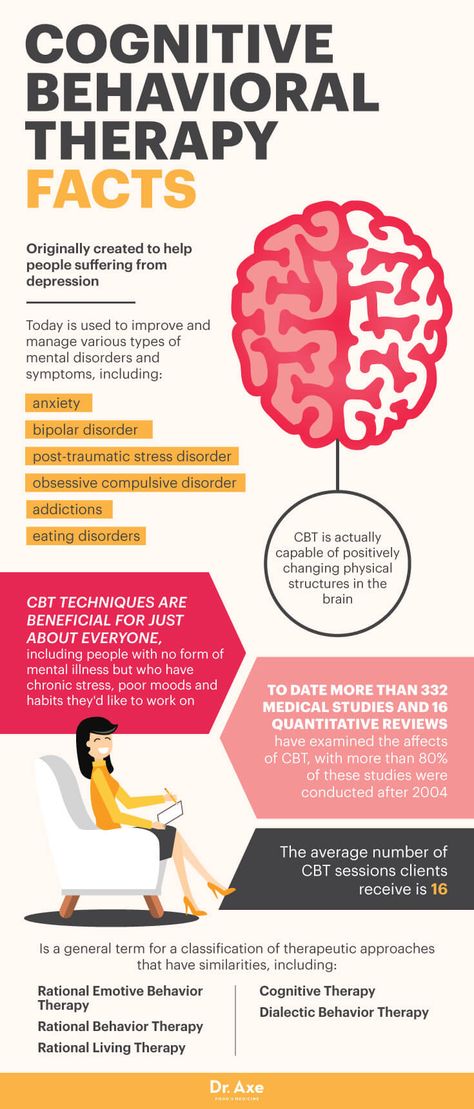
Patients who have schizoaffective disorder can benefit from psychotherapy, as is the case with most mental disorders.
Treatment plans should incorporate individual therapy, family therapy, and psychoeducational programs. The aim is to develop their social skills and improve cognitive functioning to prevent relapse and possible rehospitalization.[27] This treatment plan includes education about the disorder, etiology, and treatment.
Individual therapy: This type of treatment aims to normalize thought processes and better help the patient understand the disorder and reduce symptoms. Sessions focus on everyday goals, social interactions, and conflict; this includes social skills training and vocational training.
Family and/or group therapy: Family involvement is crucial in the treatment of this schizoaffective disorder. [28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
[28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
ECT (Electroconvulsive Therapy)
ECT is usually a last resort treatment. However, not only has it been used in urgent cases and treatment resistance, but it should also merit consideration in augmentation of current pharmacotherapy.[29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
Differential Diagnosis
Because of criteria that encompass both psychotic and mood symptoms, schizoaffective disorder is easy to mistake for other mental disorders. Disorders that must be ruled out during the workup of schizoaffective disorder include:
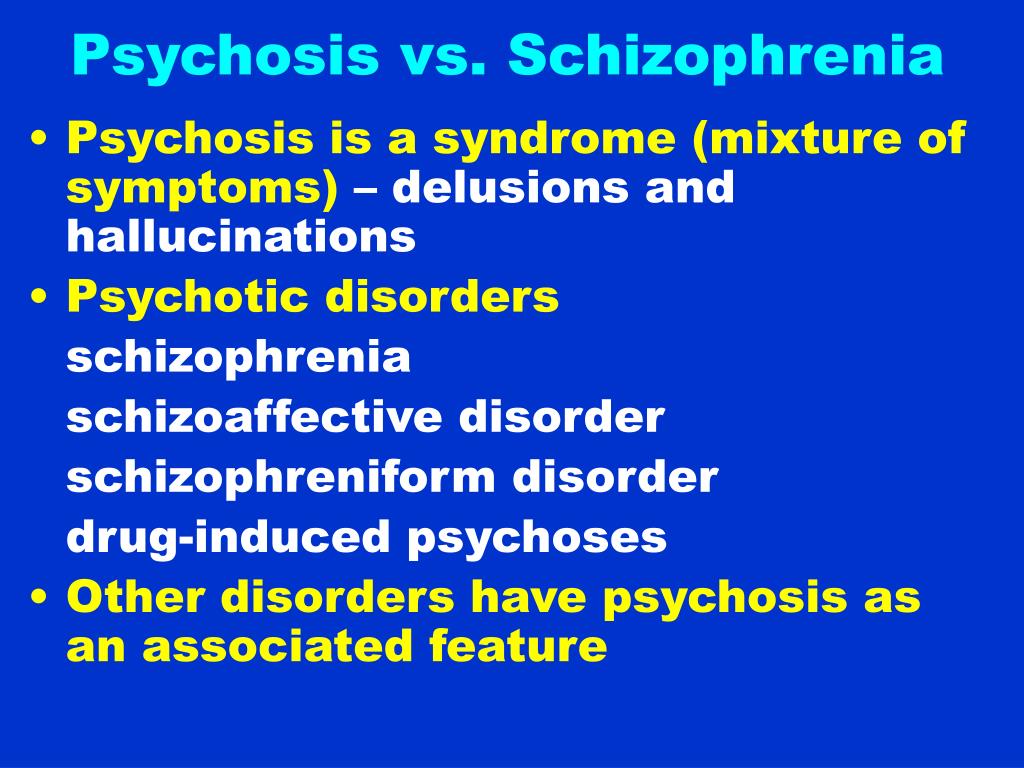
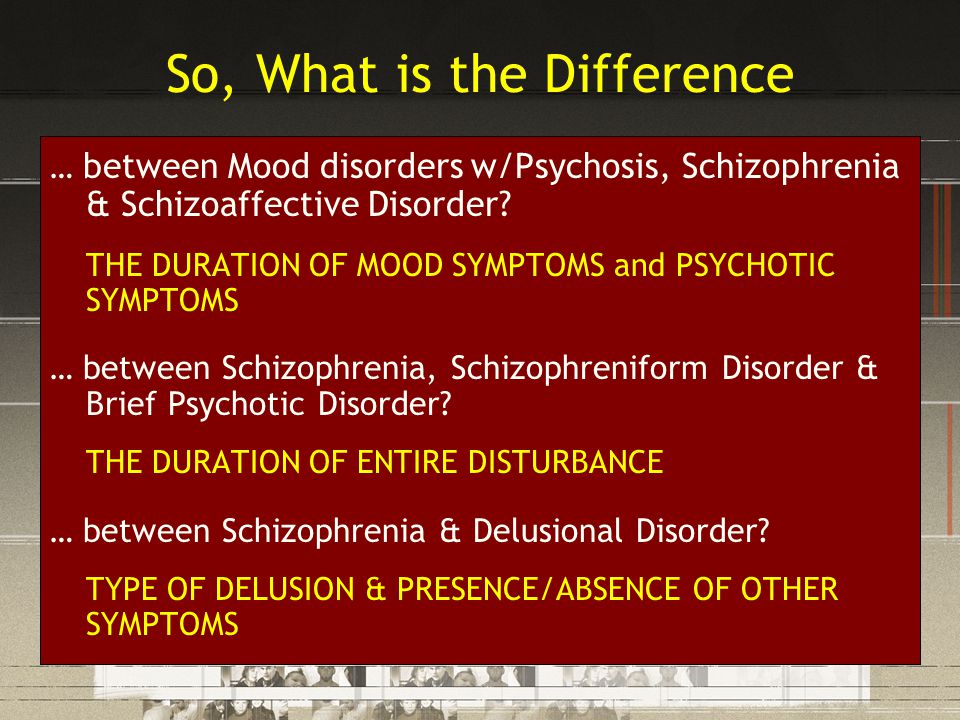
Schizophrenia and Schizoaffective Disorder: There has to be a definite period of at least two weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms to diagnose schizoaffective disorder. However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.
However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.
Major Depressive Disorder Psychotic Features and Schizoaffective Disorder: Patients with major depression with psychotic features (MDD with PF) only experience psychotic features during their mood episodes. In contrast, schizoaffective requires at least 2 weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms. Patients with MDD with PF do not meet criterion A of schizoaffective disorder.
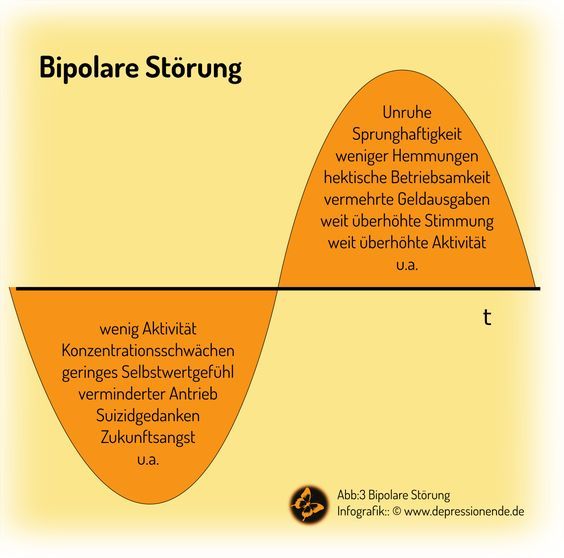
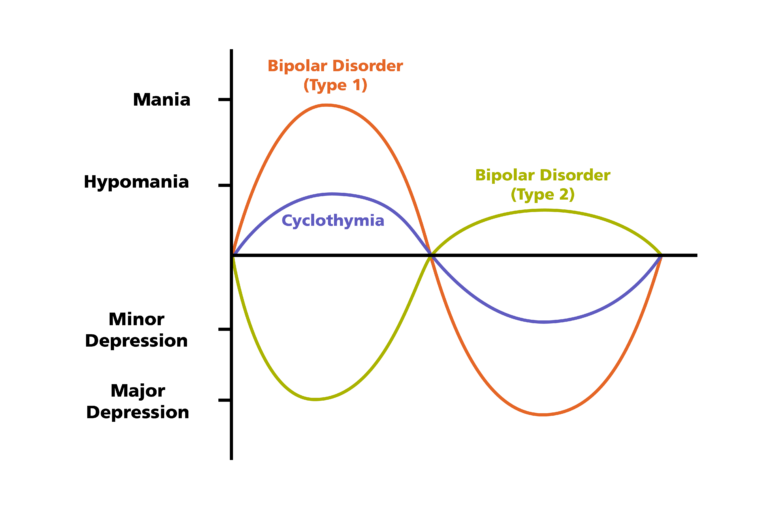
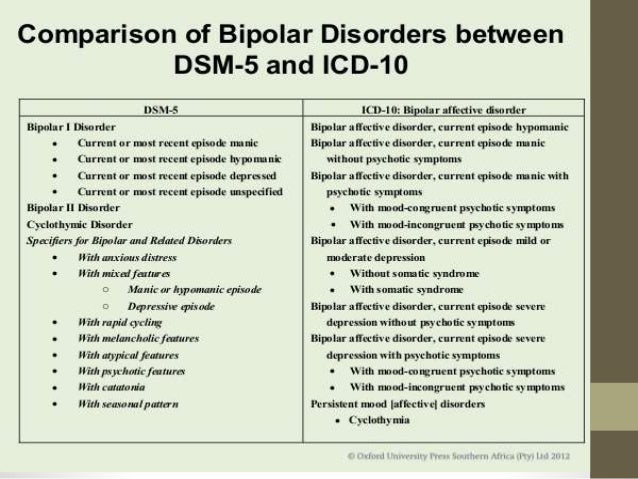
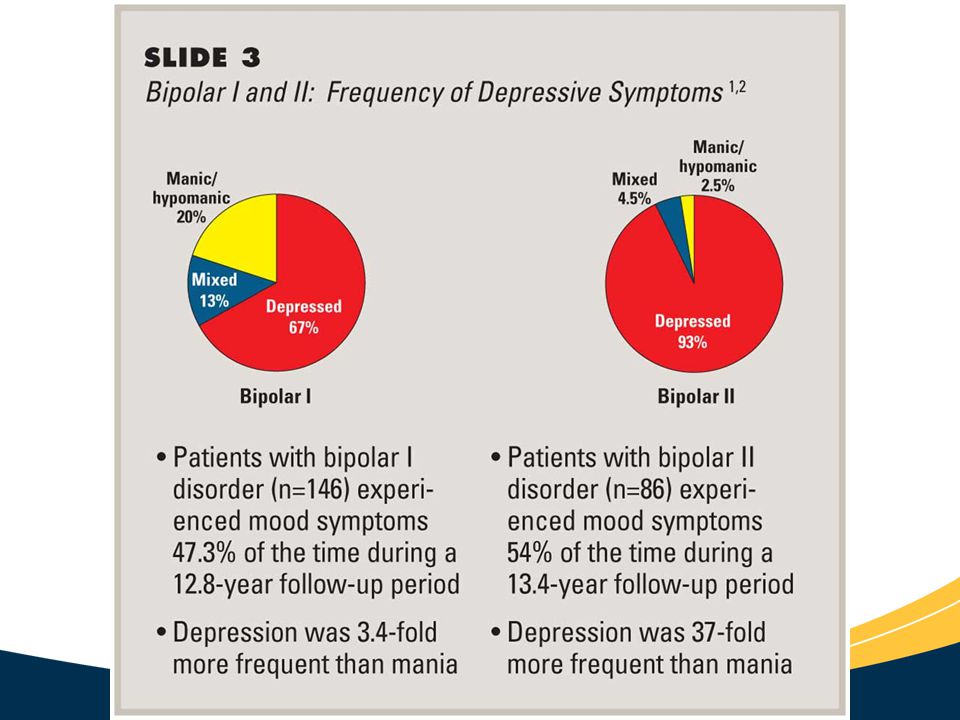
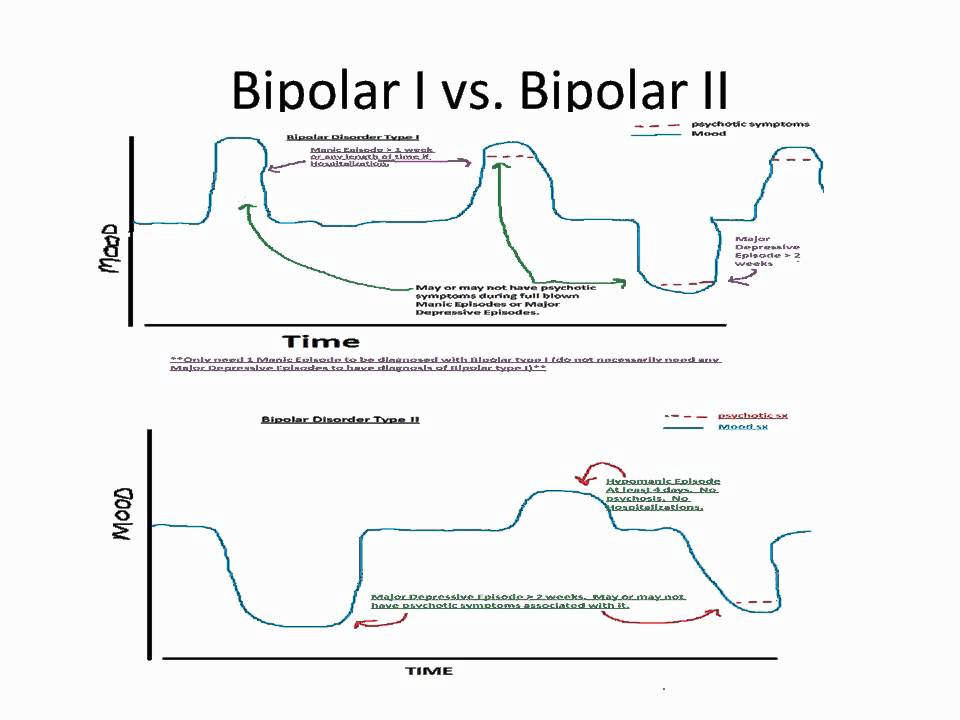
Bipolar Disorder and Schizoaffective Disorder: Similar to the contrasts of MDD w/ PF, patients with bipolar disorder with psychotic features only experience psychotic features (delusions and hallucinations) during a manic episode. Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Prognosis
Given that the diagnostic criteria of schizoaffective disorder change periodically, prognostic studies have been challenging to conduct. However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
Complications
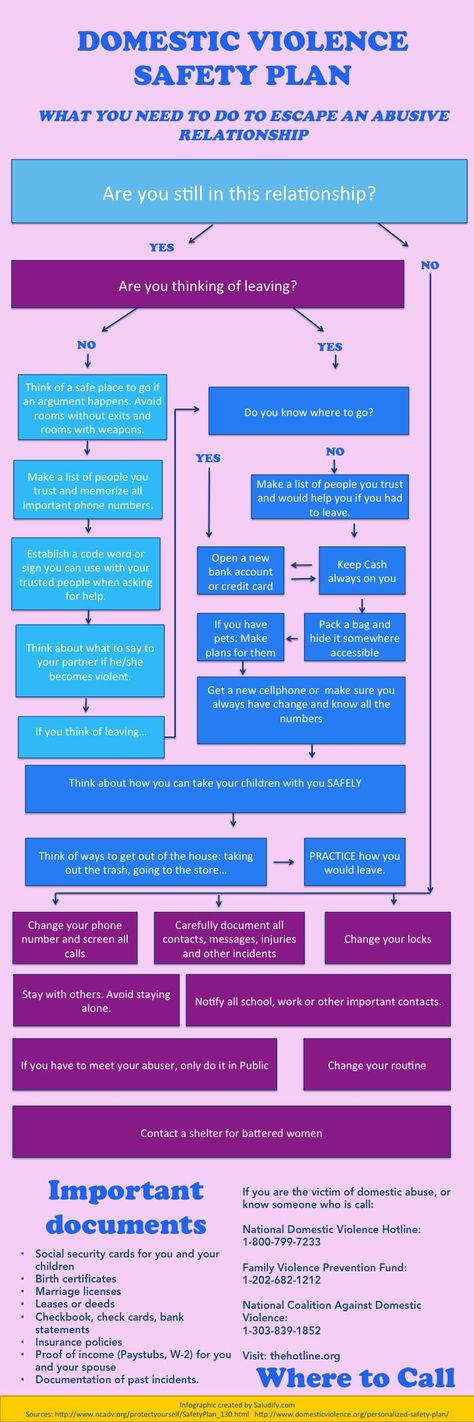
Left untreated, schizoaffective disorder has many ramifications in both social functioning and activities of daily living. These include unemployment, isolation, impaired ability to care for self, etc. Untreated mental disorders have more than just social and functional consequences.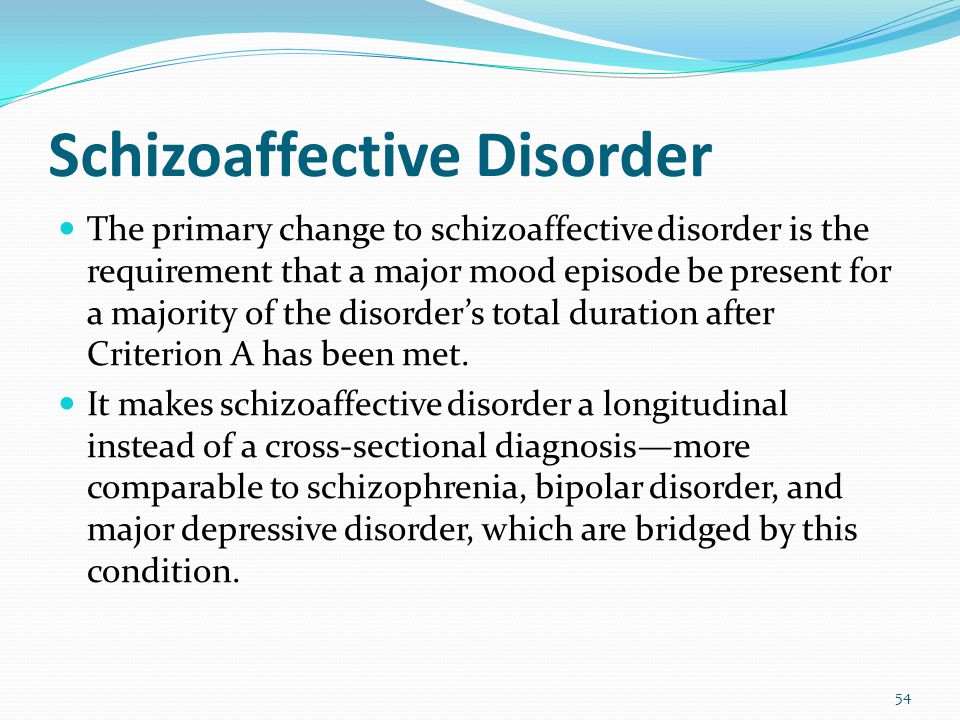 Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Deterrence and Patient Education
Patients and their families can benefit from education regarding the condition and steps to manage it.
Encourage the patient to undergo treatment and rehabilitation
Cognitive behavior therapy
Interventions for drug and alcohol misuse
Social skills training
Provide emotional and life support
Teach them skills and measures that promote self-care and independence
Supported employment
Pearls and Other Issues
Working through the differential of schizoaffective disorder is often a daunting task, and many clinicians continue to have trouble making the diagnosis. [2] A few considerations when working through the differential diagnosis include:
[2] A few considerations when working through the differential diagnosis include:
Observe the criteria for each diagnosis carefully.
Do not "fill in blanks" with preconceived notions about the patient's history. Take what the patient tells you and what family/collateral information tells you when working through a differential.
Time frames often give clues towards one specific diagnosis. Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.
Criterion B of schizoaffective disorder is key for the following reasons. One must tease out a 2 week or longer period of just psychotic symptoms in the patient's history. If one finds that the patient has always had mood symptoms during their entire illness, the diagnosis by definition is not a schizoaffective disorder.
Enhancing Healthcare Team Outcomes
As with most mental disorders, schizoaffective disorder is best managed by an interprofessional team including psychiatric specialty nurses and pharmacists, and clinicians that practice close interprofessional communication. [Level 5] Pharmacotherapy, psychotherapy, skills training, and vocational training work in tandem to create a holistic treatment plan. In addition to what the information alluded to in previous sections, psychotherapy strongly influences medication compliance.[34] An ideal treatment course to improve outcomes around patient-centered care may include:
Early detection of mental disorder in the primary care setting
Referral to a psychiatrist for further evaluation
A psychiatrist would stabilize the patient with pharmacotherapy or defer to a clinical psychologist for diagnosis or additional therapy
If the patient requires inpatient hospitalization, the nursing staff and case management become crucial in providing optimal patient care
It is critical to determine if the patient is competent to make healthcare decisions independently; otherwise, a proxy must be a consideration.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malaspina D, Owen MJ, Heckers S, Tandon R, Bustillo J, Schultz S, Barch DM, Gaebel W, Gur RE, Tsuang M, Van Os J, Carpenter W. Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]
- 2.
Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014 Feb;264(1):29-34. [PMC free article: PMC4207055] [PubMed: 23625467]
- 3.
Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009 Mar;35(2):383-402. [PMC free article: PMC2659306] [PubMed: 19011234]
- 4.
Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry.
 2006 Jan;163(1):115-24. [PubMed: 16390898]
2006 Jan;163(1):115-24. [PubMed: 16390898]- 5.
Laursen TM, Munk-Olsen T, Nordentoft M, Bo Mortensen P. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a danish population-based cohort. J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]
- 6.
Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long-term course. Acta Psychiatr Scand. 1990 Nov;82(5):352-8. [PubMed: 2281805]
- 7.
Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008 Dec;4(6):1089-109. [PMC free article: PMC2646642] [PubMed: 19337453]
- 8.
Azorin JM, Kaladjian A, Fakra E. [Current issues on schizoaffective disorder]. Encephale.
 2005 May-Jun;31(3):359-65. [PubMed: 16142051]
2005 May-Jun;31(3):359-65. [PubMed: 16142051]- 9.
Meltzer HY, Arora RC, Metz J. Biological studies of schizoaffective disorders. Schizophr Bull. 1984;10(1):49-70. [PubMed: 6422546]
- 10.
Antonius D, Prudent V, Rebani Y, D'Angelo D, Ardekani BA, Malaspina D, Hoptman MJ. White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]
- 11.
Radonić E, Rados M, Kalember P, Bajs-Janović M, Folnegović-Smalc V, Henigsberg N. Comparison of hippocampal volumes in schizophrenia, schizoaffective and bipolar disorder. Coll Antropol. 2011 Jan;35 Suppl 1:249-52. [PubMed: 21648342]
- 12.
Smith MJ, Wang L, Cronenwett W, Mamah D, Barch DM, Csernansky JG. Thalamic morphology in schizophrenia and schizoaffective disorder. J Psychiatr Res. 2011 Mar;45(3):378-85. [PMC free article: PMC2996474] [PubMed: 20797731]
- 13.
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013 Oct;150(1):3-10. [PubMed: 23800613]
- 14.
Vieta E. Developing an individualized treatment plan for patients with schizoaffective disorder: from pharmacotherapy to psychoeducation. J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]
- 15.
Cascade E, Kalali AH, Buckley P. Treatment of schizoaffective disorder. Psychiatry (Edgmont). 2009 Mar;6(3):15-7. [PMC free article: PMC2719459] [PubMed: 19724749]
- 16.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002 Sep;63(9):763-71. [PubMed: 12363115]
- 17.
Addington DE, Pantelis C, Dineen M, Benattia I, Romano SJ.
 Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]
Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]- 18.
Ciapparelli A, Dell'Osso L, Bandettini di Poggio A, Carmassi C, Cecconi D, Fenzi M, Chiavacci MC, Bottai M, Ramacciotti CE, Cassano GB. Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]
- 19.
Ghaemi SN, Goodwin FK. Use of atypical antipsychotic agents in bipolar and schizoaffective disorders: review of the empirical literature. J Clin Psychopharmacol. 1999 Aug;19(4):354-61. [PubMed: 10440464]
- 20.
Gunasekara NS, Spencer CM, Keating GM. Spotlight on ziprasidone in schizophrenia and schizoaffective disorder.
 CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]
CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]- 21.
Baethge C, Gruschka P, Berghöfer A, Bauer M, Müller-Oerlinghausen B, Bschor T, Smolka MN. Prophylaxis of schizoaffective disorder with lithium or carbamazepine: outcome after long-term follow-up. J Affect Disord. 2004 Apr;79(1-3):43-50. [PubMed: 15023479]
- 22.
Bogan AM, Brown ES, Suppes T. Efficacy of divalproex therapy for schizoaffective disorder. J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]
- 23.
Dietrich DE, Kropp S, Emrich HM. [Oxcarbazepine in the treatment of affective and schizoaffective disorders]. Fortschr Neurol Psychiatr. 2003 May;71(5):255-64. [PubMed: 12740757]
- 24.
Leucht S, McGrath J, White P, Kissling W. Carbamazepine for schizophrenia and schizoaffective psychoses. Cochrane Database Syst Rev. 2002;(3):CD001258. [PubMed: 12137621]
- 25.
Koenig AM, Thase ME. First-line pharmacotherapies for depression - what is the best choice? Pol Arch Med Wewn.
 2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]
2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]- 26.
McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. Prim Care Companion CNS Disord. 2014;16(5) [PMC free article: PMC4321017] [PubMed: 25667812]
- 27.
Fitzgerald P, de Castella A, Arya D, Simons WR, Eggleston A, Meere S, Kulkarni J. The cost of relapse in schizophrenia and schizoaffective disorder. Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]
- 28.
Pharoah FM, Rathbone J, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2003;(4):CD000088. [PubMed: 14583908]
- 29.
Phutane VH, Thirthalli J, Kesavan M, Kumar NC, Gangadhar BN. Why do we prescribe ECT to schizophrenia patients? Indian J Psychiatry. 2011 Apr;53(2):149-51. [PMC free article: PMC3136018] [PubMed: 21772648]
- 30.
Iancu I, Pick N, Seener-Lorsh O, Dannon P. Patients with schizophrenia or schizoaffective disorder who receive multiple electroconvulsive therapy sessions: characteristics, indications, and results.
 Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]
Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]- 31.
Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, Dube KC, Ganev K, Giel R, an der Heiden W, Holmberg SK, Janca A, Lee PW, León CA, Malhotra S, Marsella AJ, Nakane Y, Sartorius N, Shen Y, Skoda C, Thara R, Tsirkin SJ, Varma VK, Walsh D, Wiersma D. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]
- 32.
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010 Nov;24(4 Suppl):81-90. [PMC free article: PMC2951591] [PubMed: 20923923]
- 33.
Suominen K, Isometsä E, Heilä H, Lönnqvist J, Henriksson M. General hospital suicides--a psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002 Nov-Dec;24(6):412-6. [PubMed: 12490343]
- 34.
Stentzel U, van den Berg N, Schulze LN, Schwaneberg T, Radicke F, Langosch JM, Freyberger HJ, Hoffmann W, Grabe HJ.
 Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
Schizoaffective Disorder - StatPearls - NCBI Bookshelf
Continuing Education Activity
Schizoaffective disorder is among the most frequently misdiagnosed psychiatric disorders in clinical practice. Due to concerns about the reliability and utility of the diagnostic criteria for schizoaffective disorder, some researchers have proposed revisions, while others have suggested altogether removing the diagnosis from the Diagnostic and Statistical Manual of Mental Disorders. This activity describes limitations and challenges related to the diagnostic criteria and highlights the interprofessional team's role in caring for patients with psychiatric disorders.
Objectives:
Describe the pathophysiology of schizoaffective disorder.
Outline the classic clinical presentation of a patient with schizoaffective disorder.
Summarize the treatment options for patients with schizoaffective disorder.
Describe the importance of collaboration and communication amongst the interprofessional team to improve patient compliance with treatment and thus improve outcomes for patients with schizoaffective disorder.
Access free multiple choice questions on this topic.
Introduction
Schizoaffective disorder is one of the most misdiagnosed psychiatric disorders in clinical practice.[1] In fact, some researchers have proposed revisions to the diagnostic criteria, and others have suggested removing the diagnosis altogether from the DSM-5.[2] There were significant concerns regarding the reliability and utility of the diagnosis when it was first introduced in the DSM.[2] The challenges lie within the diagnostic criteria itself since the disorder is part of a spectrum that shares criteria with many other prominent psychiatric disorders found in clinical practice.
Etiology
The term schizoaffective disorder first appeared as a subtype of schizophrenia in the first edition of the DSM. It eventually became its own diagnosis despite a lack of evidence for unique differences in etiology or pathophysiology. Therefore, there have been no conclusive studies on the etiology of the disorder. However, investigating the potential causes of mood disorders and schizophrenia as individual disorders allows for further discussion.
Some studies show that as high as 50% of people with schizophrenia also have comorbid depression.[3] The pathogenesis of both mood disorders and schizophrenia is multifactorial and covers a range of risk factors, including genetics, social factors, trauma, and stress.[4] Among people with schizophrenia, there is a possible increased risk for first-degree relatives for schizoaffective disorder and vice-versa; there may be increased risk among individuals for schizoaffective disorder who have a first-degree relative with bipolar disorder schizophrenia, or schizoaffective disorder.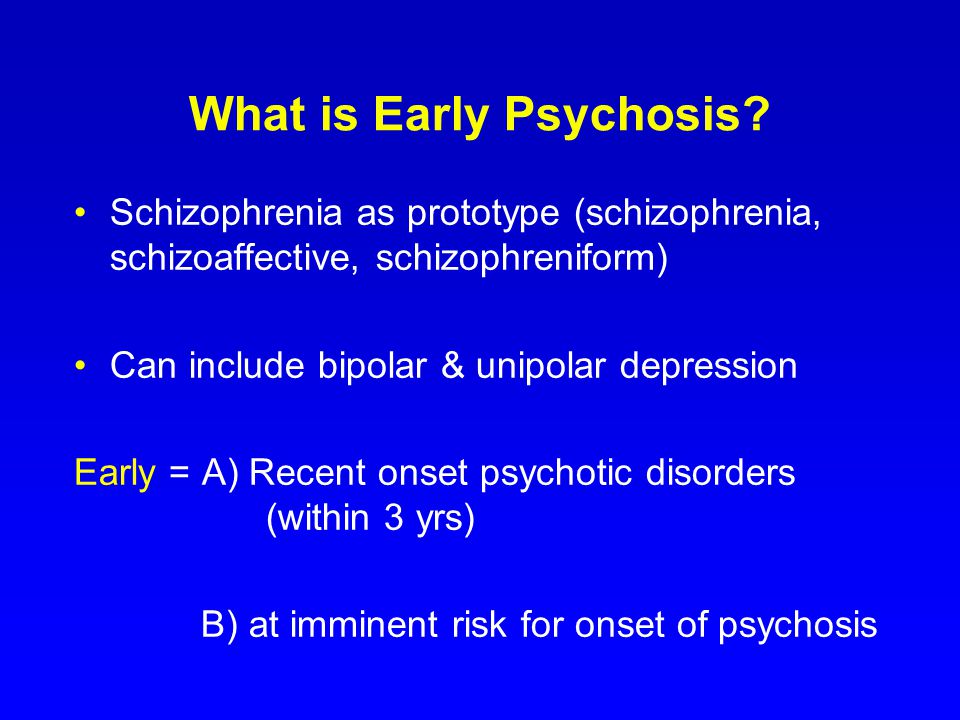 [5]
[5]
Epidemiology
The diagnostic criteria for schizoaffective disorder have been reworded and addended since its inclusion in the DSM, making it difficult to subsequently conduct appropriate epidemiological studies. Thus, there have been no large-scale studies on the epidemiology, incidence, or prevalence of schizoaffective disorder. Research shows that 30% of cases occur between the ages of 25 and 35, and it occurs more frequently in women.[6][7] Schizoaffective disorder occurs about one-third as frequently as schizophrenia, and the lifetime prevalence appears to be around 0.3%.[5] Estimates are that schizoaffective disorder comprises 10 to 30% of inpatient admissions for psychosis.[8]
Pathophysiology
The exact pathophysiology of schizoaffective disorder is currently unknown. Some studies have shown that abnormalities in dopamine, norepinephrine, and serotonin may play a role.[9] Also, white matter abnormalities in multiple areas of the brain, particularly the right lentiform nucleus, left temporal gyrus, and right precuneus, are associated with schizophrenia and schizoaffective disorder.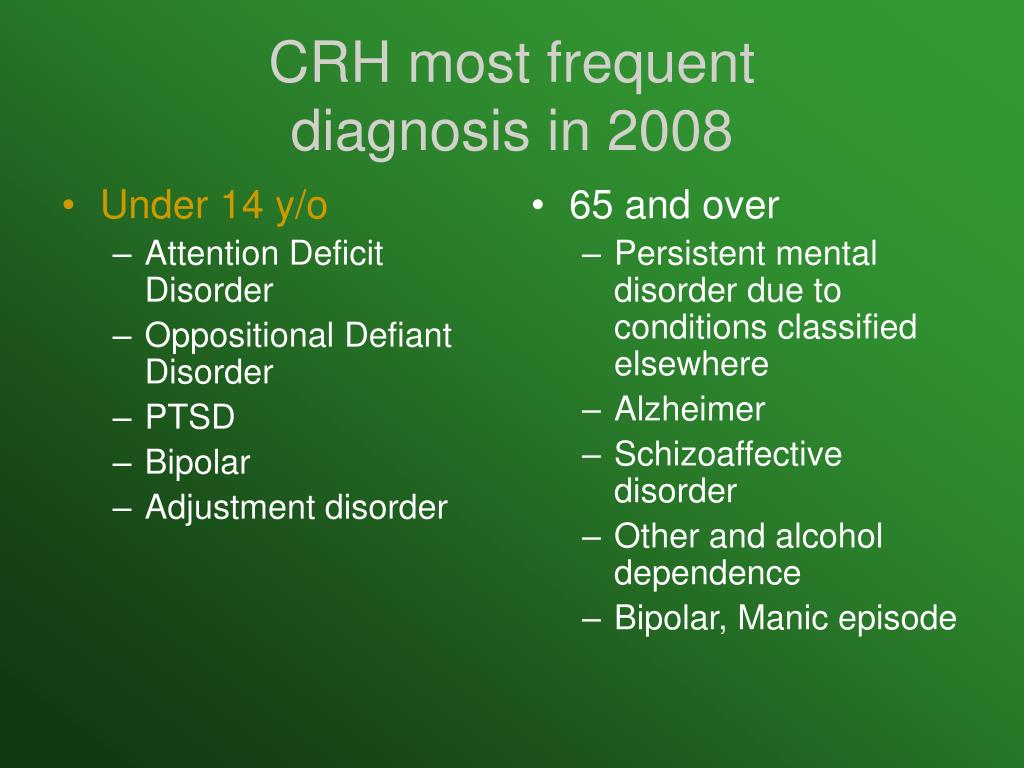 [10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
[10] Researchers have also found reduced hippocampal volumes and distinct deformations in the medial and lateral thalamic regions in those with schizoaffective disorder in comparison to controls.[11][12]
History and Physical
The first step in evaluation is obtaining a complete medical history while focusing on the diagnostic criteria for schizoaffective disorder.
The specific DSM-5 criteria for schizoaffective disorder are as follows[1]:
A. An uninterrupted duration of illness during which there is a major mood episode (manic or depressive) in addition to criterion A for schizophrenia; the major depressive episode must include depressed mood.
Criterion A for schizophrenia is as follows[13]:
Two or more of the following presentations, each present for a significant amount of time during a 1-month period (or less if successfully treated). At least one of these must be from the first three below.
Delusions
Hallucinations
Disorganized speech (e.
 g., frequent derailment or incoherence).
g., frequent derailment or incoherence).Grossly disorganized or catatonic behavior
Negative symptoms (i.e., diminished emotional expression or avolition.)
B. Hallucinations and delusions for two or more weeks in the absence of a major mood episode (manic or depressive) during the entire lifetime duration of the illness.
C. Symptoms that meet the criteria for a major mood episode are present for most of the total duration of both the active and residual portions of the illness.
D. The disturbance is not the result of the effects of a substance (e.g., a drug of misuse or a medication) or another underlying medical condition.
The following are specifiers based on the primary mood episode as part of the presentation.
Bipolar type: includes episodes of mania and sometimes major depression.
Depressive type: includes only major depressive episodes.
Please note the patient must meet the criteria for A-D above to be diagnosed with schizoaffective disorder.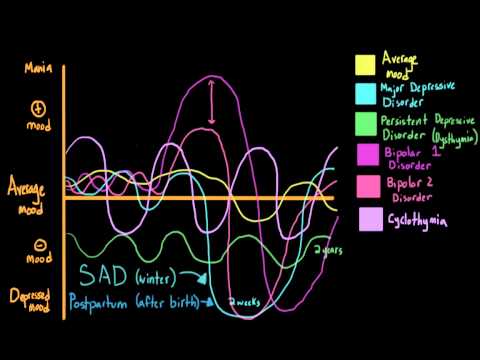 It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
It is not enough to symptoms of schizophrenia while meeting the criteria for a major mood episode. Please see the differential diagnoses and pearls sections below for more information.
The next step of evaluation is the objective and physical portion. A thorough mental status examination (MSE), physical examination, and neurologic examination should be completed to help rule out other differential diagnoses.
Evaluation
The following workup is optional and typically not needed to make the diagnosis. The history and physical are the mainstays of diagnosis. However, some elect to include additional tests or imaging to aid in the diagnosis, such as MRI (magnetic resonance imaging), EEG (electroencephalography), or CT (computed tomography).
Laboratory studies are tailored to the patient’s history, especially for those who have an atypical presentation.
Complete blood count (CBC)
Lipid panel
Urine drug screen
Urine pregnancy test
Urinalysis
Thyroid-stimulating hormone (TSH) level
Rapid plasma reagent
HIV test
If the patient's neurologic exam is found to be aberrant, performing a brain MRI or CT to rule out any suspected intracranial abnormalities may be considered.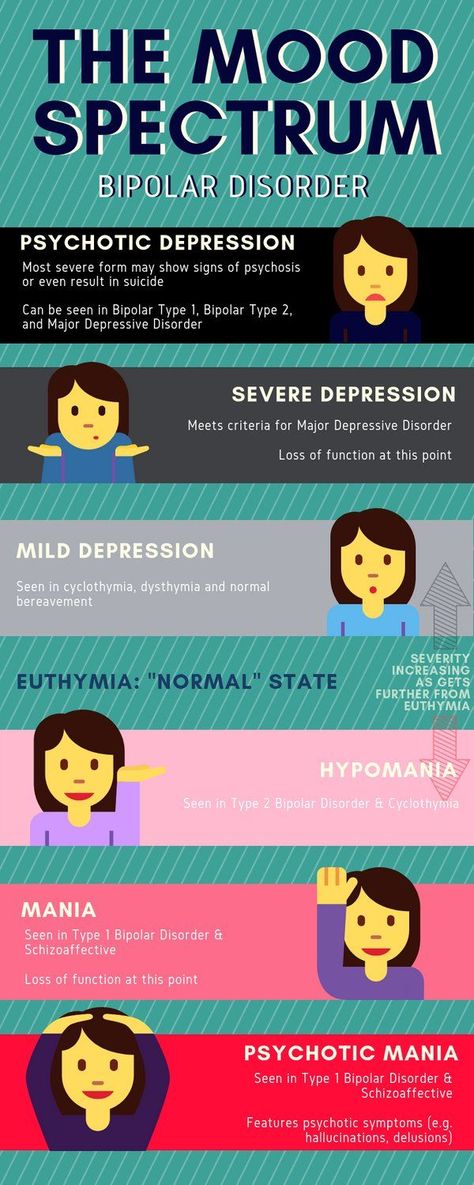
Treatment / Management
The treatment of schizoaffective disorder typically involves both pharmacotherapy and psychotherapy. The mainstay of most treatment regimens should include an antipsychotic, but the choice of treatment should be tailored to the individual.[14] A study that reported obtained data on treatment regimens for schizoaffective showed that 93% of patients received an antipsychotic. 20% of patients received a mood-stabilizer in addition to an antipsychotic, while 19% received an antidepressant along with an antipsychotic.[15] Prior to initiating treatment, if a patient with schizoaffective disorder is a danger to themselves or others, inpatient hospitalization should be considered; this includes patients who are neglecting activities of daily living or those who are disabled well below their baseline in terms of functioning.
Pharmacotherapy
Antipsychotics: Used to target psychosis and aggressive behavior in schizoaffective disorder.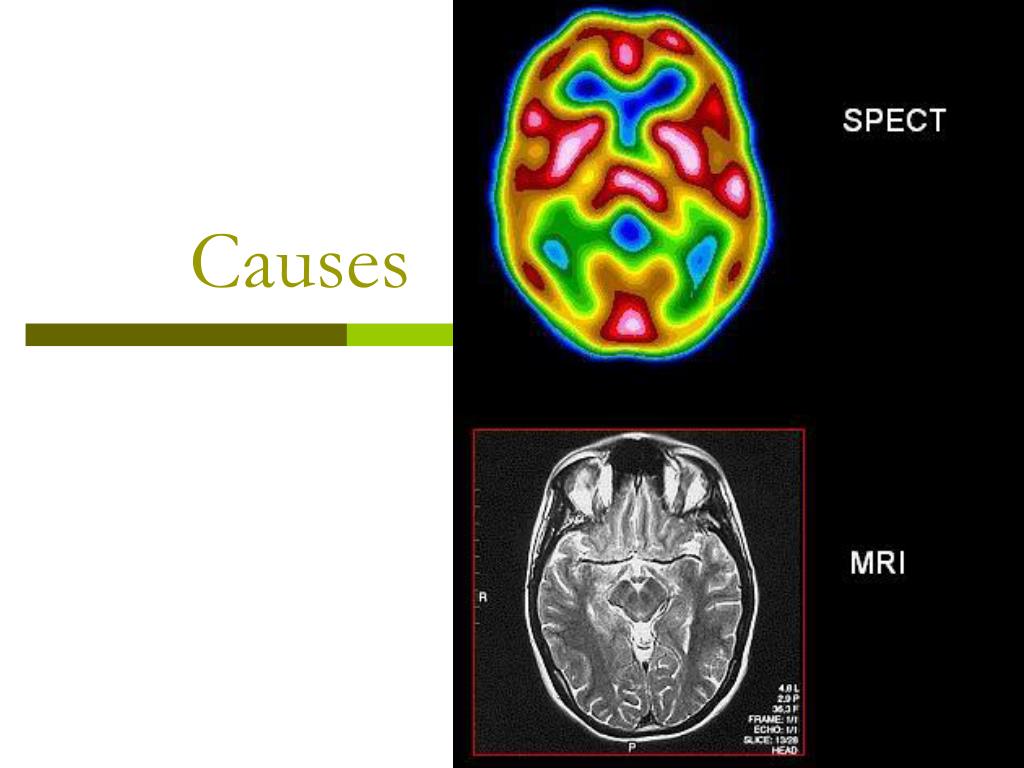 Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
Other symptoms include delusions, hallucinations, negative symptoms, disorganized speech, and behavior. Most first and second-generation antipsychotics block dopamine receptors. While second-generation antipsychotics have further actions on serotonin receptors. Antipsychotics include but are not limited to paliperidone (FDA approved for schizoaffective disorder), risperidone, olanzapine, quetiapine, ziprasidone, aripiprazole, and haloperidol.[16][17][18][19][20] Clozapine is a consideration for refractory cases, much like in schizophrenia.[18]
Mood-stabilizers: Patients who have periods of distractibility, indiscretion, grandiosity, a flight of ideas, increased goal-directed activity, decreased need for sleep, and who are hyper-verbal fall under the bipolar-specifier for schizoaffective disorder. Consider the use of mood-stabilizers if the patient has a history of manic or hypomanic symptoms. These include medications such as lithium, valproic acid, carbamazepine, oxcarbazepine, and lamotrigine which target mood dysregulation. [21][22][23][24]
[21][22][23][24]
Antidepressants: Used to target depressive symptoms in schizoaffective disorder. Selective-serotonin reuptake inhibitors (SSRIs) are preferred due to lower risk for adverse drug effects and tolerability when compared to tricyclic antidepressants and selective norepinephrine reuptake inhibitors.[25] SSRIs include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. It is vital to rule out bipolar disorder before starting an antidepressant due to the risk of exacerbating a manic episode.[26]
Psychotherapy
Patients who have schizoaffective disorder can benefit from psychotherapy, as is the case with most mental disorders.
Treatment plans should incorporate individual therapy, family therapy, and psychoeducational programs. The aim is to develop their social skills and improve cognitive functioning to prevent relapse and possible rehospitalization.[27] This treatment plan includes education about the disorder, etiology, and treatment.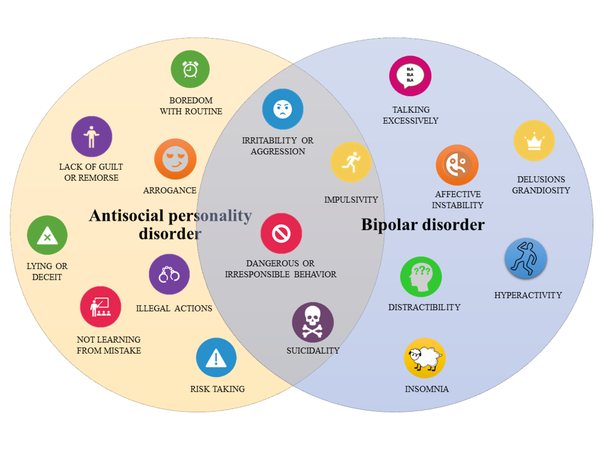
Individual therapy: This type of treatment aims to normalize thought processes and better help the patient understand the disorder and reduce symptoms. Sessions focus on everyday goals, social interactions, and conflict; this includes social skills training and vocational training.
Family and/or group therapy: Family involvement is crucial in the treatment of this schizoaffective disorder.[28] Family education aids in compliance with medications and appointments and helps provide structure throughout the patient's life, given the dynamic nature of the schizoaffective disorder. Supportive group programs can also help if the patient has been in social isolation and provides a sense of shared experiences among participants.
ECT (Electroconvulsive Therapy)
ECT is usually a last resort treatment. However, not only has it been used in urgent cases and treatment resistance, but it should also merit consideration in augmentation of current pharmacotherapy.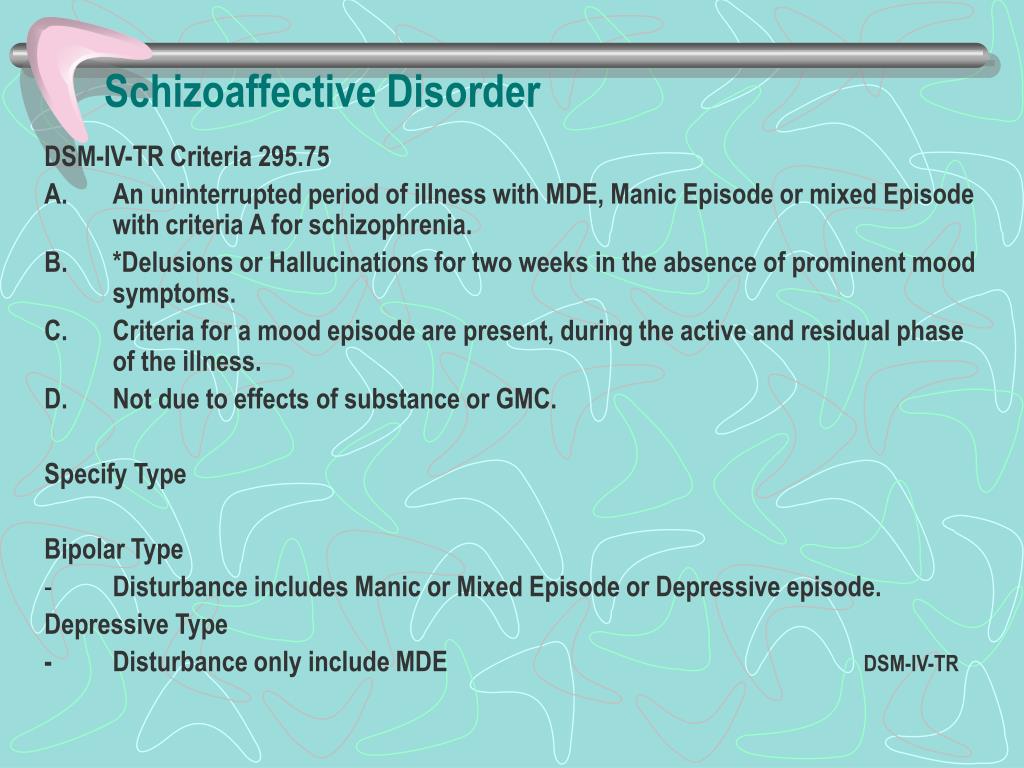 [29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
[29] The most common indicated symptoms are catatonia and aggression. ECT is safe and effective for most chronically hospitalized patients.[30]
Differential Diagnosis
Because of criteria that encompass both psychotic and mood symptoms, schizoaffective disorder is easy to mistake for other mental disorders. Disorders that must be ruled out during the workup of schizoaffective disorder include:
Schizophrenia and Schizoaffective Disorder: There has to be a definite period of at least two weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms to diagnose schizoaffective disorder. However, a major mood episode (depression or mania) is present for the majority of the total duration of the illness. Once the psychotic symptoms predominate the majority of the total duration of the illness, the diagnosis leans towards schizophrenia. Also, schizophrenia requires 6 months of prodromal or residual symptoms; schizoaffective disorder does not require this criterion.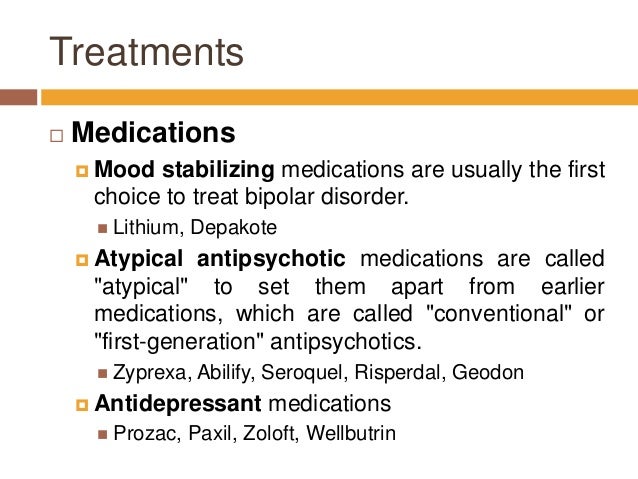
Major Depressive Disorder Psychotic Features and Schizoaffective Disorder: Patients with major depression with psychotic features (MDD with PF) only experience psychotic features during their mood episodes. In contrast, schizoaffective requires at least 2 weeks in which there are only psychotic symptoms (delusions and hallucinations) without mood symptoms. Patients with MDD with PF do not meet criterion A of schizoaffective disorder.
Bipolar Disorder and Schizoaffective Disorder: Similar to the contrasts of MDD w/ PF, patients with bipolar disorder with psychotic features only experience psychotic features (delusions and hallucinations) during a manic episode. Again, schizoaffective requires a period of at least 2 weeks in which there are only psychotic symptoms without mood symptoms. Psychotic features in bipolar disorder do not meet criterion A of schizoaffective disorder.
Prognosis
Given that the diagnostic criteria of schizoaffective disorder change periodically, prognostic studies have been challenging to conduct. However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
However, a study by Harrison et al., 2001 on the overall prognosis of those with psychotic illness showed that 50% of cases showed favorable outcomes.[31] The defined favorable as minimal or no symptoms and/or employment. These outcomes were highly reliant on the early initiation of treatment and optimized treatment regimens as outlined above.
Complications
Left untreated, schizoaffective disorder has many ramifications in both social functioning and activities of daily living. These include unemployment, isolation, impaired ability to care for self, etc. Untreated mental disorders have more than just social and functional consequences. Some studies show that as many as 5% of people with a psychotic illness will commit suicide over their lifetime.[32] Research has shown that among all completed suicides, ten percent are attributable to those with a psychotic illness.[33]
Deterrence and Patient Education
Patients and their families can benefit from education regarding the condition and steps to manage it.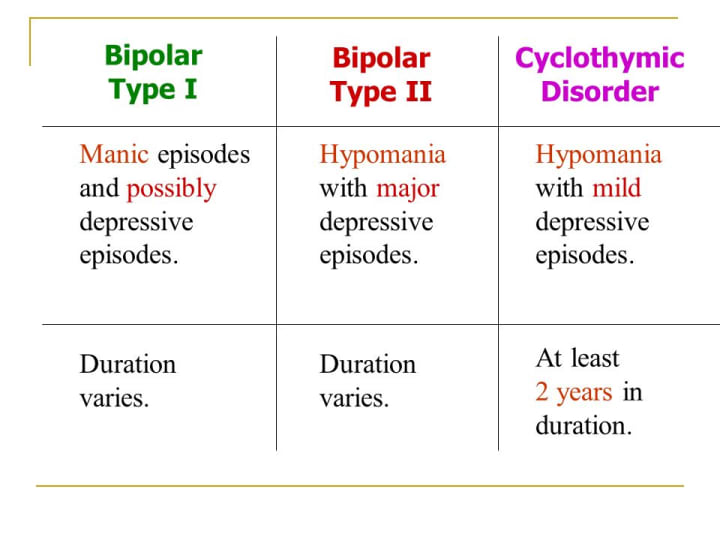
Encourage the patient to undergo treatment and rehabilitation
Cognitive behavior therapy
Interventions for drug and alcohol misuse
Social skills training
Provide emotional and life support
Teach them skills and measures that promote self-care and independence
Supported employment
Pearls and Other Issues
Working through the differential of schizoaffective disorder is often a daunting task, and many clinicians continue to have trouble making the diagnosis.[2] A few considerations when working through the differential diagnosis include:
Observe the criteria for each diagnosis carefully.
Do not "fill in blanks" with preconceived notions about the patient's history. Take what the patient tells you and what family/collateral information tells you when working through a differential.
Time frames often give clues towards one specific diagnosis.
 Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.
Symptom course also plays a role; did mood symptoms or psychotic symptoms come first? For how long did the symptoms last? History-taking is an essential skill necessary for all clinicians; it is even more imperative in psychiatry.Criterion B of schizoaffective disorder is key for the following reasons. One must tease out a 2 week or longer period of just psychotic symptoms in the patient's history. If one finds that the patient has always had mood symptoms during their entire illness, the diagnosis by definition is not a schizoaffective disorder.
Enhancing Healthcare Team Outcomes
As with most mental disorders, schizoaffective disorder is best managed by an interprofessional team including psychiatric specialty nurses and pharmacists, and clinicians that practice close interprofessional communication. [Level 5] Pharmacotherapy, psychotherapy, skills training, and vocational training work in tandem to create a holistic treatment plan. In addition to what the information alluded to in previous sections, psychotherapy strongly influences medication compliance.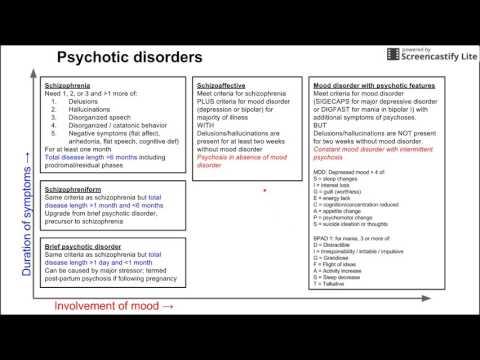 [34] An ideal treatment course to improve outcomes around patient-centered care may include:
[34] An ideal treatment course to improve outcomes around patient-centered care may include:
Early detection of mental disorder in the primary care setting
Referral to a psychiatrist for further evaluation
A psychiatrist would stabilize the patient with pharmacotherapy or defer to a clinical psychologist for diagnosis or additional therapy
If the patient requires inpatient hospitalization, the nursing staff and case management become crucial in providing optimal patient care
It is critical to determine if the patient is competent to make healthcare decisions independently; otherwise, a proxy must be a consideration.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malaspina D, Owen MJ, Heckers S, Tandon R, Bustillo J, Schultz S, Barch DM, Gaebel W, Gur RE, Tsuang M, Van Os J, Carpenter W.
 Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]
Schizoaffective Disorder in the DSM-5. Schizophr Res. 2013 Oct;150(1):21-5. [PubMed: 23707642]- 2.
Wilson JE, Nian H, Heckers S. The schizoaffective disorder diagnosis: a conundrum in the clinical setting. Eur Arch Psychiatry Clin Neurosci. 2014 Feb;264(1):29-34. [PMC free article: PMC4207055] [PubMed: 23625467]
- 3.
Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009 Mar;35(2):383-402. [PMC free article: PMC2659306] [PubMed: 19011234]
- 4.
Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry. 2006 Jan;163(1):115-24. [PubMed: 16390898]
- 5.
Laursen TM, Munk-Olsen T, Nordentoft M, Bo Mortensen P. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a danish population-based cohort.
 J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]
J Clin Psychiatry. 2007 Nov;68(11):1673-81. [PubMed: 18052560]- 6.
Marneros A, Deister A, Rohde A. Psychopathological and social status of patients with affective, schizophrenic and schizoaffective disorders after long-term course. Acta Psychiatr Scand. 1990 Nov;82(5):352-8. [PubMed: 2281805]
- 7.
Abrams DJ, Rojas DC, Arciniegas DB. Is schizoaffective disorder a distinct categorical diagnosis? A critical review of the literature. Neuropsychiatr Dis Treat. 2008 Dec;4(6):1089-109. [PMC free article: PMC2646642] [PubMed: 19337453]
- 8.
Azorin JM, Kaladjian A, Fakra E. [Current issues on schizoaffective disorder]. Encephale. 2005 May-Jun;31(3):359-65. [PubMed: 16142051]
- 9.
Meltzer HY, Arora RC, Metz J. Biological studies of schizoaffective disorders. Schizophr Bull. 1984;10(1):49-70. [PubMed: 6422546]
- 10.
Antonius D, Prudent V, Rebani Y, D'Angelo D, Ardekani BA, Malaspina D, Hoptman MJ.
 White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]
White matter integrity and lack of insight in schizophrenia and schizoaffective disorder. Schizophr Res. 2011 May;128(1-3):76-82. [PMC free article: PMC3085627] [PubMed: 21429714]- 11.
Radonić E, Rados M, Kalember P, Bajs-Janović M, Folnegović-Smalc V, Henigsberg N. Comparison of hippocampal volumes in schizophrenia, schizoaffective and bipolar disorder. Coll Antropol. 2011 Jan;35 Suppl 1:249-52. [PubMed: 21648342]
- 12.
Smith MJ, Wang L, Cronenwett W, Mamah D, Barch DM, Csernansky JG. Thalamic morphology in schizophrenia and schizoaffective disorder. J Psychiatr Res. 2011 Mar;45(3):378-85. [PMC free article: PMC2996474] [PubMed: 20797731]
- 13.
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013 Oct;150(1):3-10. [PubMed: 23800613]
- 14.
Vieta E. Developing an individualized treatment plan for patients with schizoaffective disorder: from pharmacotherapy to psychoeducation.
 J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]
J Clin Psychiatry. 2010;71 Suppl 2:14-9. [PubMed: 21190648]- 15.
Cascade E, Kalali AH, Buckley P. Treatment of schizoaffective disorder. Psychiatry (Edgmont). 2009 Mar;6(3):15-7. [PMC free article: PMC2719459] [PubMed: 19724749]
- 16.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, Ali MW. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002 Sep;63(9):763-71. [PubMed: 12363115]
- 17.
Addington DE, Pantelis C, Dineen M, Benattia I, Romano SJ. Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry. 2004 Dec;65(12):1624-33. [PubMed: 15641867]
- 18.
Ciapparelli A, Dell'Osso L, Bandettini di Poggio A, Carmassi C, Cecconi D, Fenzi M, Chiavacci MC, Bottai M, Ramacciotti CE, Cassano GB.
 Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]
Clozapine in treatment-resistant patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder: a naturalistic 48-month follow-up study. J Clin Psychiatry. 2003 Apr;64(4):451-8. [PubMed: 12716249]- 19.
Ghaemi SN, Goodwin FK. Use of atypical antipsychotic agents in bipolar and schizoaffective disorders: review of the empirical literature. J Clin Psychopharmacol. 1999 Aug;19(4):354-61. [PubMed: 10440464]
- 20.
Gunasekara NS, Spencer CM, Keating GM. Spotlight on ziprasidone in schizophrenia and schizoaffective disorder. CNS Drugs. 2002;16(9):645-52. [PubMed: 12153335]
- 21.
Baethge C, Gruschka P, Berghöfer A, Bauer M, Müller-Oerlinghausen B, Bschor T, Smolka MN. Prophylaxis of schizoaffective disorder with lithium or carbamazepine: outcome after long-term follow-up. J Affect Disord. 2004 Apr;79(1-3):43-50. [PubMed: 15023479]
- 22.
Bogan AM, Brown ES, Suppes T. Efficacy of divalproex therapy for schizoaffective disorder.
 J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]
J Clin Psychopharmacol. 2000 Oct;20(5):520-2. [PubMed: 11001235]- 23.
Dietrich DE, Kropp S, Emrich HM. [Oxcarbazepine in the treatment of affective and schizoaffective disorders]. Fortschr Neurol Psychiatr. 2003 May;71(5):255-64. [PubMed: 12740757]
- 24.
Leucht S, McGrath J, White P, Kissling W. Carbamazepine for schizophrenia and schizoaffective psychoses. Cochrane Database Syst Rev. 2002;(3):CD001258. [PubMed: 12137621]
- 25.
Koenig AM, Thase ME. First-line pharmacotherapies for depression - what is the best choice? Pol Arch Med Wewn. 2009 Jul-Aug;119(7-8):478-86. [PubMed: 19776688]
- 26.
McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. Prim Care Companion CNS Disord. 2014;16(5) [PMC free article: PMC4321017] [PubMed: 25667812]
- 27.
Fitzgerald P, de Castella A, Arya D, Simons WR, Eggleston A, Meere S, Kulkarni J. The cost of relapse in schizophrenia and schizoaffective disorder.
 Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]
Australas Psychiatry. 2009 Aug;17(4):265-72. [PubMed: 19585288]- 28.
Pharoah FM, Rathbone J, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2003;(4):CD000088. [PubMed: 14583908]
- 29.
Phutane VH, Thirthalli J, Kesavan M, Kumar NC, Gangadhar BN. Why do we prescribe ECT to schizophrenia patients? Indian J Psychiatry. 2011 Apr;53(2):149-51. [PMC free article: PMC3136018] [PubMed: 21772648]
- 30.
Iancu I, Pick N, Seener-Lorsh O, Dannon P. Patients with schizophrenia or schizoaffective disorder who receive multiple electroconvulsive therapy sessions: characteristics, indications, and results. Neuropsychiatr Dis Treat. 2015;11:853-62. [PMC free article: PMC4384746] [PubMed: 25848283]
- 31.
Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, Dube KC, Ganev K, Giel R, an der Heiden W, Holmberg SK, Janca A, Lee PW, León CA, Malhotra S, Marsella AJ, Nakane Y, Sartorius N, Shen Y, Skoda C, Thara R, Tsirkin SJ, Varma VK, Walsh D, Wiersma D.
 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001 Jun;178:506-17. [PubMed: 11388966]- 32.
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010 Nov;24(4 Suppl):81-90. [PMC free article: PMC2951591] [PubMed: 20923923]
- 33.
Suominen K, Isometsä E, Heilä H, Lönnqvist J, Henriksson M. General hospital suicides--a psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002 Nov-Dec;24(6):412-6. [PubMed: 12490343]
- 34.
Stentzel U, van den Berg N, Schulze LN, Schwaneberg T, Radicke F, Langosch JM, Freyberger HJ, Hoffmann W, Grabe HJ. Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry. 2018 May 29;18(1):155. [PMC free article: PMC5975380] [PubMed: 29843676]
Not Found (#404)
hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
- nine0009
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.
 A. Kramar
A. Kramar -
Screening, diagnosis and treatment of diabetic sensorimotor polyneuropathy: consensus recommendations
-
Influx of mass information on delinquent behavior
R. І. Isakov
-
Stopping programs for rukhovo's rehabilitation for the normalization of the psychoemotional sphere of patients with Parkinson's disease
N.P. Voloshin, I.V. Bogdanova, I.K. Voloshin-Gaponov, S.V. Fedosiev, L.P. Tereshchenko, T.V. Bogdanova
-
Trauma management algorithm
-
Type of neuropathic pain according to the International classification of orofacial pain
-
Management of patients with dementia: key provisions for diagnosis, examination and observation for example of life
-
Significant Pre-Raphaelism: John Ruskin and Effi Gray
5-6 (135)
3-4 (134)
2 (133)
1 (132)
Other projects of the Health of Ukraine publishing house
Specialization medical portal
nine0009 Child doctorMedical aspects of women's health
Clinical Immunology, Allergology, Infectology
Rational pharmacotherapy
nine0000 Esme Weijun Wang "Pretending to be normal.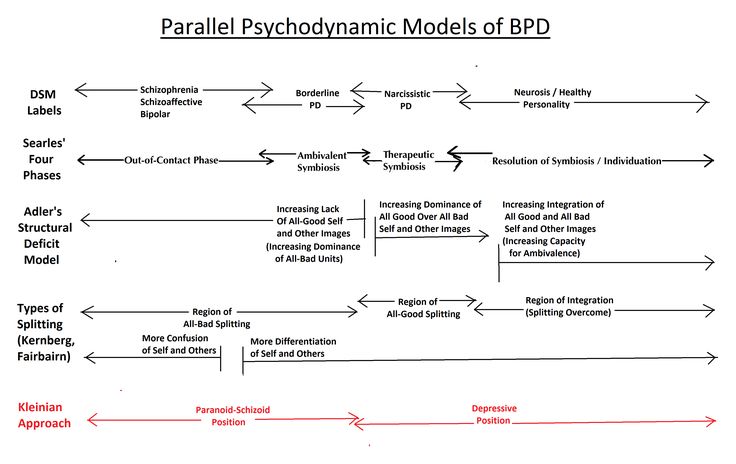 The story of a girl living with schizophrenia." Read online for free.
The story of a girl living with schizophrenia." Read online for free. Pretending to be normal. The story of a girl living with schizophrenia
Esme Weijun Wang
Strange but Normal. Neighborhood Books
A book by Chinese-American Esme Weijun Wang dispels numerous myths about schizophrenia. Based on personal experience, the writer talks about the facets of mental illness, conflicting diagnoses, treatment options and the fate of people who have become victims of mental illness. The owner of a disappointing diagnosis, Esme Weijun Wang is able to look at her problems from the outside. This gives her the opportunity to be an impartial researcher of her own ailment, and in ordinary life makes her highly functional and empathic. The dramatic experience of the writer is a positive example of what heights of personal and social development a person with a mental disorder can achieve with a developed intellect, reflection and self-discipline. nine0004
Editor's design preserved in PDF A4 format.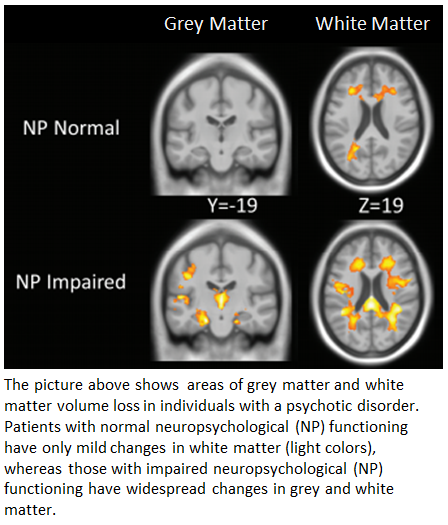
Esme Weijun Wang
Pretending to be normal. The story of a girl living with schizophrenia
© Melnik E., translated into Russian, 2022
© Design. LLC Eksmo Publishing House, 2022
* * *
Chris and everyone affected by schizophrenia
Remission from schizophrenia, almost never complete, covers the whole spectrum: from a level tolerable for society to one that, even if not requires constant hospitalization, but does not allow even the semblance of a normal life. The most striking symptom, the defining characteristic of this disease, is the deep feeling of incomprehensibility and inaccessibility that people suffering from it cause in others. nine0004
Sylvia Nazar, A Beautiful Mind
How can I continue on this path?
And how can I not continue it?
Susan Sontag
Book Reviews
“With this collection of wonderful, gripping essays by Esme, Weijun Wang gives us a universal pass into her beautiful, troubled mind, and it can only be called an act of incredible generosity.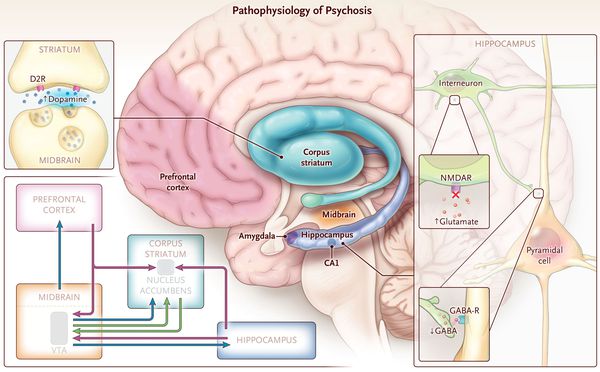 Rarely is a book about living with a mental illness so direct, unadorned, and powerful.” nine0004
Rarely is a book about living with a mental illness so direct, unadorned, and powerful.” nine0004
Dani Shapiro
“This collection of spellbinding essays is a rarity. The theme, which for a very long time was shrouded in a veil of both deep disgust and strong attraction, is expressed in them in a meaningful and rich language. Everything is over the edge here: both poetry, and painful questions, and a big pulsating heart.
Jenny Zhang
“A book that is both broad and nuanced, strong and bold. She made me reconsider my idea of what it means to be healthy or sick, what it means to feel your body, and therefore, to be alive. Powerful, outstanding book. nine0004
R.O. Kwon, author of The Incendiaries
Diagnosis
Schizophrenia is terrifying. This is the destruction of the original structure of personality. Madness terrifies us because we are creatures that crave logic and meaning; we divide endless days into years, months and weeks. We strive to control bad luck, sickness, misfortune, discomfort, and death—all inevitable outcomes that we do not admit to ourselves.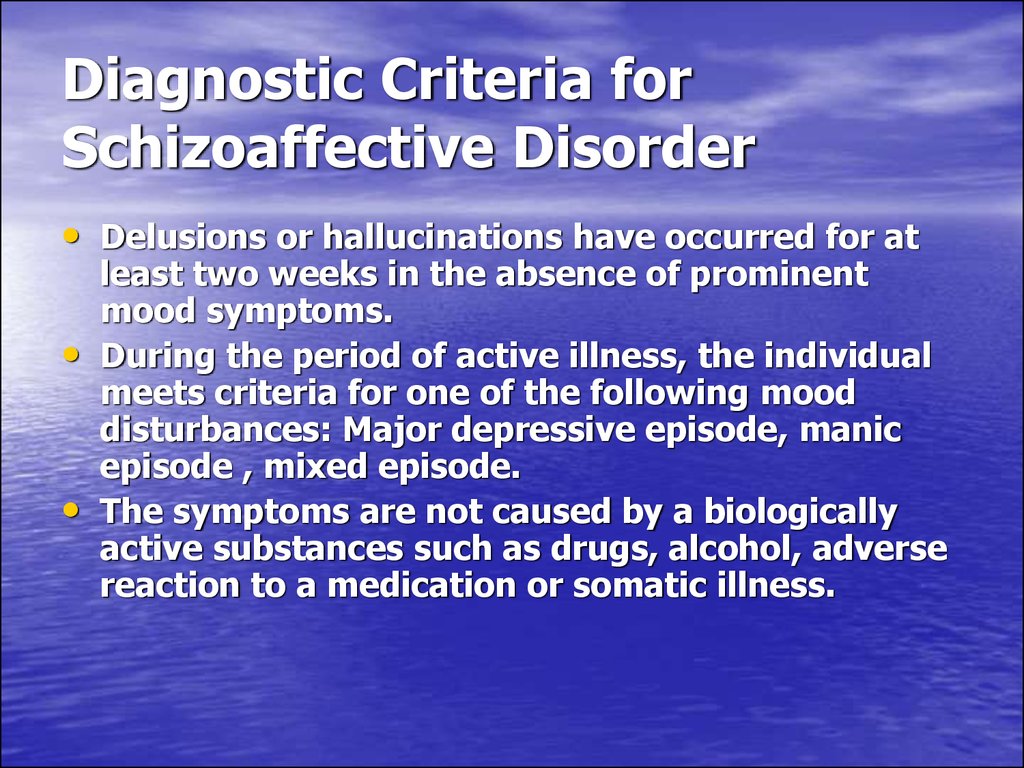 And yet the struggle against entropy seems absolutely fruitless in the face of schizophrenia, which evades reality in favor of its own internal logic. nine0004
And yet the struggle against entropy seems absolutely fruitless in the face of schizophrenia, which evades reality in favor of its own internal logic. nine0004
Schizophrenics are spoken of as if they were already dead, although they did not die; from the point of view of others, they are dead. Schizophrenics are victims of that force that in Russian is called "death", a synonym for doom and disaster. Death is not only actual death or suicide, but also a destructive cessation of existence; we are destroyed in such a way that others are hurt. Psychoanalyst Christopher Bollas defines the "schizophrenic presence effect" as the psychodynamic experience of "being near a person who seems to have passed from the human world to the non-human world." Other catastrophes - war, kidnapping, death - can be told in a coherent and meaningful way, but the built-in chaos of schizophrenia resists common sense. Both concepts - "death" and "the effect of schizophrenic presence" - imply the suffering of those who are close to the sufferer.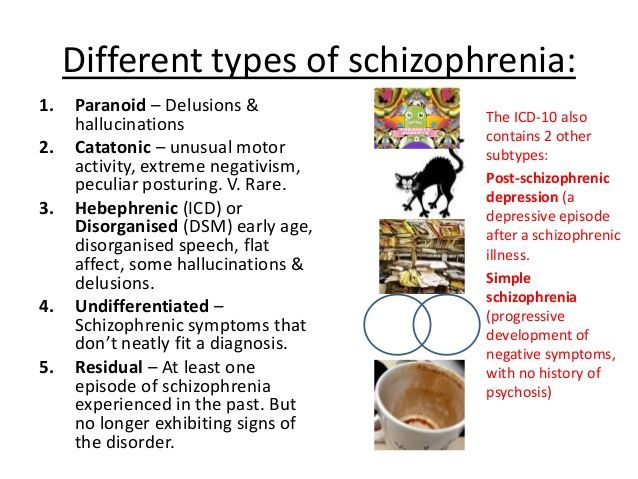 nine0004
nine0004
For the schizophrenic really suffers. I was physically lost in an impenetrable dark room. It has a floor that can only be under my feet. These anchors, shaped like my numb feet, are the only trustworthy landmarks. Any wrong move will lead to a monstrous result. In this hopeless abyss, the main thing is not to be afraid, because fear, despite its inevitability, only exacerbates the terrible feeling of being lost.
According to the US National Institute of Mental Health (NIMH), schizophrenia affects 1.1% of American adults. This number increases when considering the full psychotic spectrum, also known as "schizophrenia" (plural): 0.3%[1 - The National Alliance on Mental Illness.] of Americans are living with a diagnosis of schizoaffective disorder[2 - Mental a disease in which symptoms characteristic of both schizophrenia and affective disorders are observed. - Approx. ed.]; 3.9%[3 - Daniel R. Rosell et al., "Schizotypal Personality Disorder: A Current Review", Current Psychiatry Reports 16.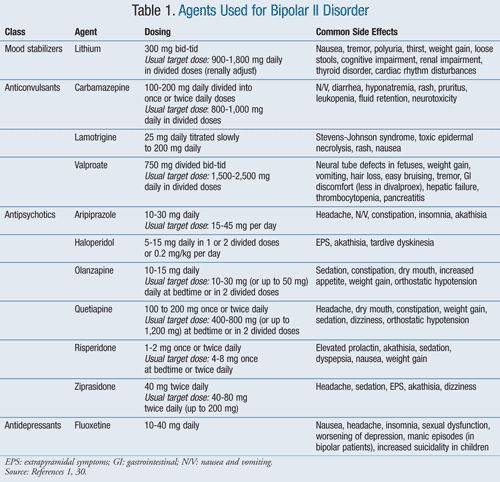 7 (2014): 452. PMC.Web. Oct 26 2017.] - with schizotypal personality disorder [4 - A disorder characterized by eccentric behavior, anomalies in thinking and emotions; according to diagnostic criteria, it is not suitable for the diagnosis of "schizophrenia" at any stage of development, since it does not have all the necessary symptoms or they are mild. - Approx. ed.]. I understand the meaning of the word "affecting" that can confirm neurotypicals in their prejudice, but I'm not going to deny that people who are diagnosed with schizophrenia do suffer. nine0004
7 (2014): 452. PMC.Web. Oct 26 2017.] - with schizotypal personality disorder [4 - A disorder characterized by eccentric behavior, anomalies in thinking and emotions; according to diagnostic criteria, it is not suitable for the diagnosis of "schizophrenia" at any stage of development, since it does not have all the necessary symptoms or they are mild. - Approx. ed.]. I understand the meaning of the word "affecting" that can confirm neurotypicals in their prejudice, but I'm not going to deny that people who are diagnosed with schizophrenia do suffer. nine0004
Schizophrenia affects 1.1% of American adults.
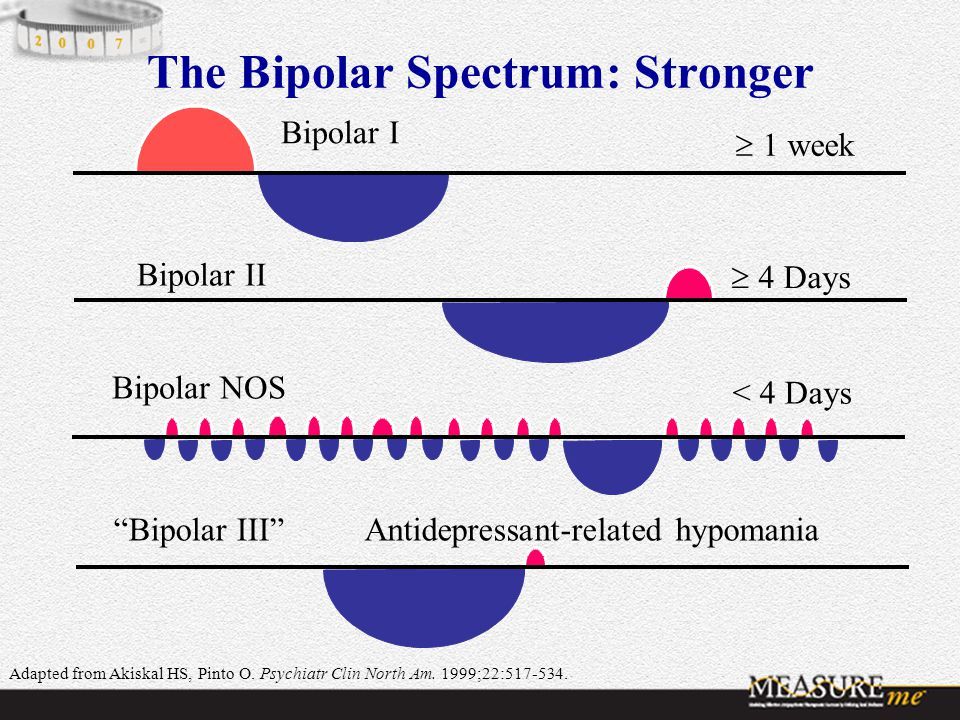
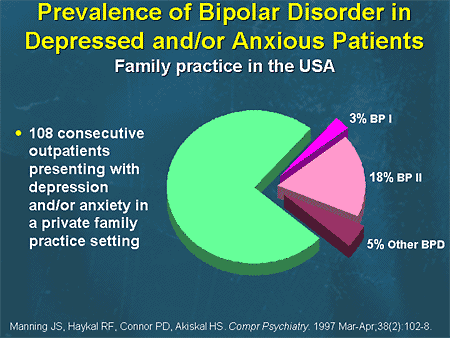
I was formally diagnosed with bipolar schizoaffective disorder eight years after I had my first hallucinations and suspected neonatal hell in my brain. It's amazing how long it took! I was diagnosed with bipolar disorder in 2001, but I had my first auditory hallucinations—a voice—in 2005, in my early 20s. I was familiar enough with psychopathology to know that people with bipolar disorder can show symptoms of psychosis, but they are not supposed to be "supposed" to experience these symptoms outside of an affective episode.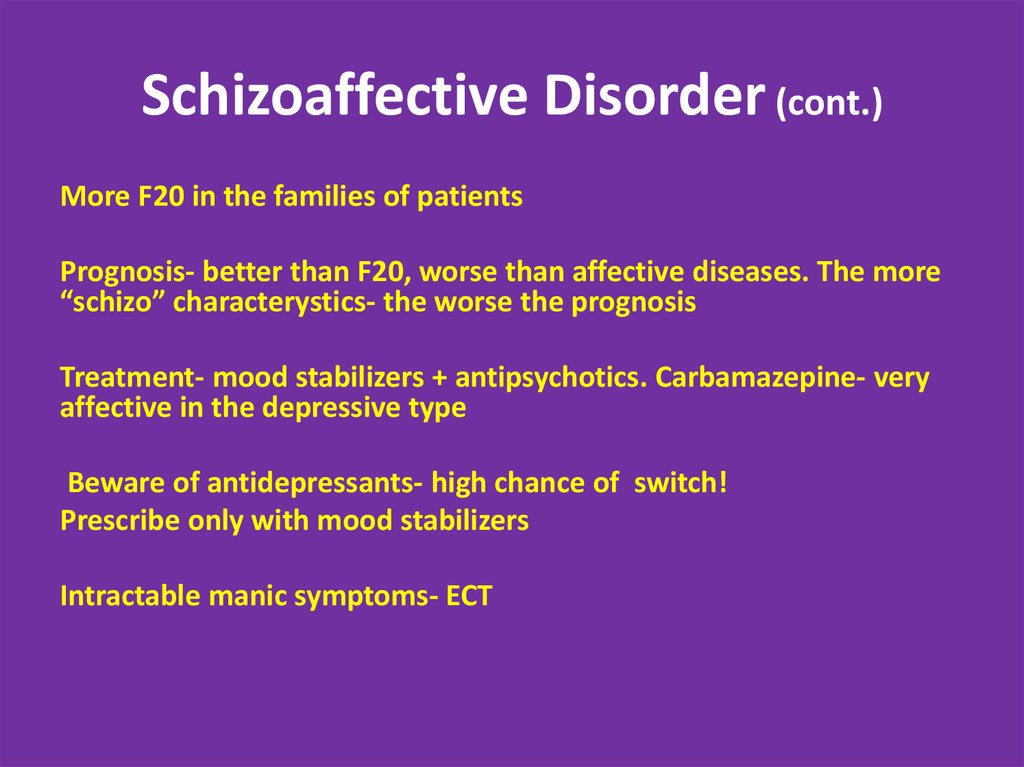 I was talking to Dr. K., my psychiatrist, at the time, but she never once uttered the term "schizoaffective disorder." Even after I reported that on college campus I sometimes dodged invisible demons and once in reality I saw a completely material engine roaring towards me, and then disappeared. I started calling these experiences sensory distortions. Dr. K readily picked up the name and used it in my presence instead of the term hallucinations. Although in fact my "distortions" were hallucinations. nine0004
I was talking to Dr. K., my psychiatrist, at the time, but she never once uttered the term "schizoaffective disorder." Even after I reported that on college campus I sometimes dodged invisible demons and once in reality I saw a completely material engine roaring towards me, and then disappeared. I started calling these experiences sensory distortions. Dr. K readily picked up the name and used it in my presence instead of the term hallucinations. Although in fact my "distortions" were hallucinations. nine0004
Some people don't like being labeled and boxed in by diagnoses. But I was always reassured by predetermined conditions. I like to know that I am not forging a new path into the unknown. For years I have hinted to Dr. K that perhaps schizoaffective disorder would be a better diagnosis for me than bipolar, but to no avail. I suppose she was wary of moving me out of the more familiar territory of anxiety and affective disorders into the wild land of schizophrenia. Perhaps this would make me feel guilty and suspicious of other people - including those who had access to my diagnostic card.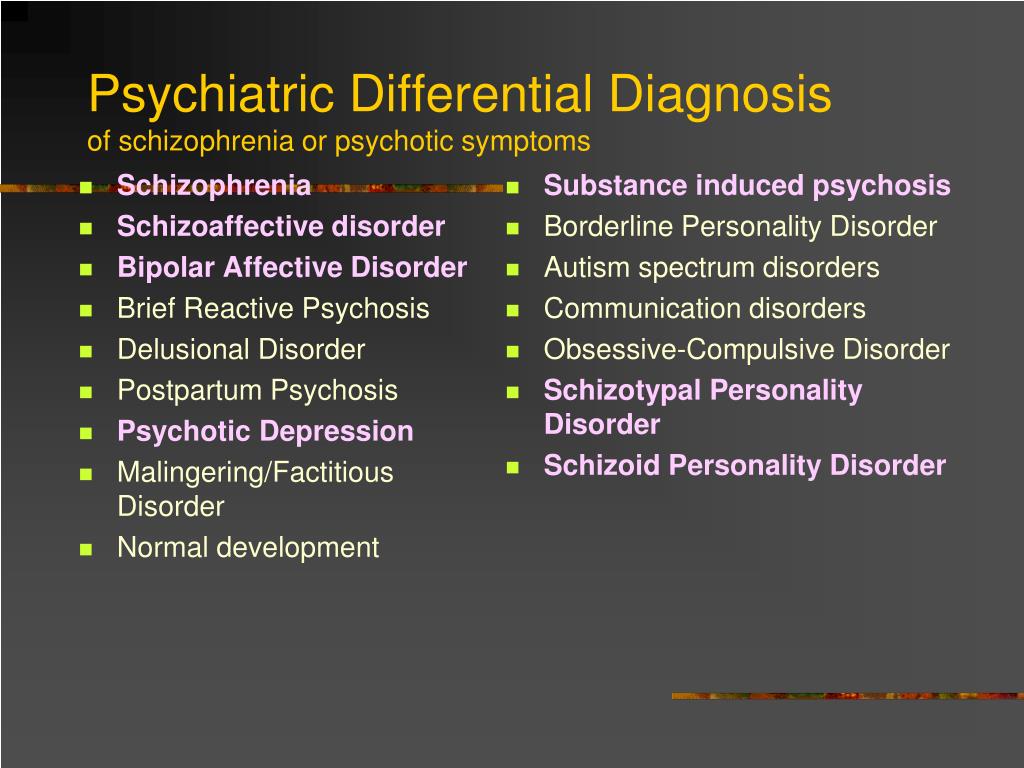 Dr. K. continued to prescribe mood stabilizers for me [5 - Psychotropic drugs that stabilize mood. - Approx. ed.] and antipsychotics [6 - Psychotropic drugs that suppress anxiety and eliminate the manifestations of psychosis. - Approx. ed.] for another eight years, never once suggesting that he was treating the wrong disease. Then I began to literally fall apart and turned to a new psychiatrist. Dr. M reluctantly diagnosed me as having bipolar schizoaffective disorder, which remains my main psychiatric diagnosis to this day. It's a label I'm fine with - for now. nine0004
Dr. K. continued to prescribe mood stabilizers for me [5 - Psychotropic drugs that stabilize mood. - Approx. ed.] and antipsychotics [6 - Psychotropic drugs that suppress anxiety and eliminate the manifestations of psychosis. - Approx. ed.] for another eight years, never once suggesting that he was treating the wrong disease. Then I began to literally fall apart and turned to a new psychiatrist. Dr. M reluctantly diagnosed me as having bipolar schizoaffective disorder, which remains my main psychiatric diagnosis to this day. It's a label I'm fine with - for now. nine0004
Diagnosis is reassuring because it points to the essence - commonality, origin - and, with luck, provides treatment or healing. The diagnosis says that I am crazy, but in a special way - this is such madness that not only doctors of our time, but also the ancient Egyptians, faced and wrote about. They described a condition similar to schizophrenia in the Book of Hearts [7 - One of the chapters of the Ebers Papyrus, a medical treatise dating from the 16th century. BC e. - Approx. trans.] and associated psychosis with the dangerous influence of poison in the heart and uterus. The ancient Egyptians understood the importance of noticing patterns of behavior. A sick uterus gives rise to hysteria, a heart - weakness of associations. They saw the utility of naming these algorithms. nine0004
BC e. - Approx. trans.] and associated psychosis with the dangerous influence of poison in the heart and uterus. The ancient Egyptians understood the importance of noticing patterns of behavior. A sick uterus gives rise to hysteria, a heart - weakness of associations. They saw the utility of naming these algorithms. nine0004
The new diagnosis, bipolar schizoaffective disorder, was the result of a correspondence I had with Dr. M through my insurance company's website.
From: Wang, Esme Weijun
Date: February 19, 2013, 09:28
To: Dr. M.
Unfortunately, the last couple of days (since Sunday) I feel unwell
by Sunday evening I was upset because the day passed in a “fog”, i.e. I didn’t realize what I was doing all day, despite the fact that I diligently made a to-do list for the day, I don’t remember doing anything, I seemed to have “lost time”. I was also very tired and went to sleep 2 times (that day I took no more clonazepam than usual, I would even say that I took less, about 2 mg)
realized on Monday that I have the same problem; it is difficult to function at work, especially when concentration is required, I look at one sentence for a long time and it does not make sense; taking a nap on the couch in the office.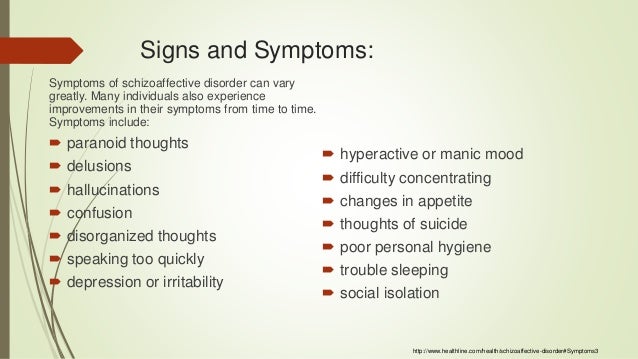 again it seemed as if the day had passed and I was not in it. by 4 o’clock didn’t know if I was real and if anything else was real, and was also worried about whether I had a face, but didn’t want to look in the mirror and felt very anxious at the thought of other faces. symptoms continued. today
again it seemed as if the day had passed and I was not in it. by 4 o’clock didn’t know if I was real and if anything else was real, and was also worried about whether I had a face, but didn’t want to look in the mirror and felt very anxious at the thought of other faces. symptoms continued. today
From: Dr. M
Received: Feb 19, 2013 12:59 pm
Okay, just re-read this - definitely more like psychosis is the problem. The solution may be to increase the dose of Seroquel (up to 1.5 tablets - a maximum dose of 800 mg). I think you might have schizoaffective disorder, a variant slightly different from bipolar I.
By the way, have you read Elin Sax's Core Can't Hold? It would be interesting to know what you think of this book. nine0004
Years later, I see a double meaning in Dr. M.'s laconic reply. She describes schizoaffective disorder as "a variant slightly different from bipolar I" but does not specify what she means: a variant of what? According to the Diagnostic and Statistical Manual (DSM), both schizophrenia and bipolar disorder belong to the first axis of mental disorders, or DSM clinical disorders. It is likely that "option" refers to this broad area, which includes the worlds of depression and anxiety in all their geography. nine0004
It is likely that "option" refers to this broad area, which includes the worlds of depression and anxiety in all their geography. nine0004
The most famous memoir about schizophrenia was written by Elin R. Sachs, an Oxford and Yale graduate and professor of law and psychiatry. The disease did not prevent her from getting three higher educations and starting a family. She describes her experience in the book The Core Doesn't Hold: Notes on My Schizophrenia (2007). MacArthur. A sort of attempt to soften the news about a possible terrible diagnosis. Perhaps in this way Dr. M. tried to emphasize my normality: you may have schizoaffective disorder, but we can still talk about books. What’s more, in four years, schizoaffective disorder will become the diagnosis that Ron Powers, in his impressive study of schizophrenia, No One Cares about Crazy People, repeatedly calls more severe than schizophrenia. And in four years, I'll be taking marginal notes and arguing with Powers in absentia. Yet there is a predecessor that I admire, Sachs, who used her MacArthur money to create a center for research into problems affecting mental health. Schizophrenia shaped Sachs' vocation. Those who tweet about "everything has a reason" can point to Sacks and her research as confirmation. They probably wouldn't have existed if the Lord had made her neurotypical. nine0004
Schizophrenia shaped Sachs' vocation. Those who tweet about "everything has a reason" can point to Sacks and her research as confirmation. They probably wouldn't have existed if the Lord had made her neurotypical. nine0004
This is how the Diagnostic and Statistical Manual (DSM-5), the clinical bible of the American Psychiatric Association (APA), describes schizophrenia:
Schizophrenia, 295.90 (F20.9)
A Two (or more) of the following symptoms, each of which is present for a significant period of time for one month (or less if treated successfully). At least one of these symptoms[8 - The first two are symptoms of psychosis. I haven't come across the third yet.] should be item (1), (2) or (3):
1. Nonsense.
2. Hallucinations.
3. Disorganized speech (for example, frequent deviations from the topic or slurring).
4. Severely disorganized or catatonic [9 - Catatonic behavior in the clinical sense is not the same as catatonia in the understanding of the average person.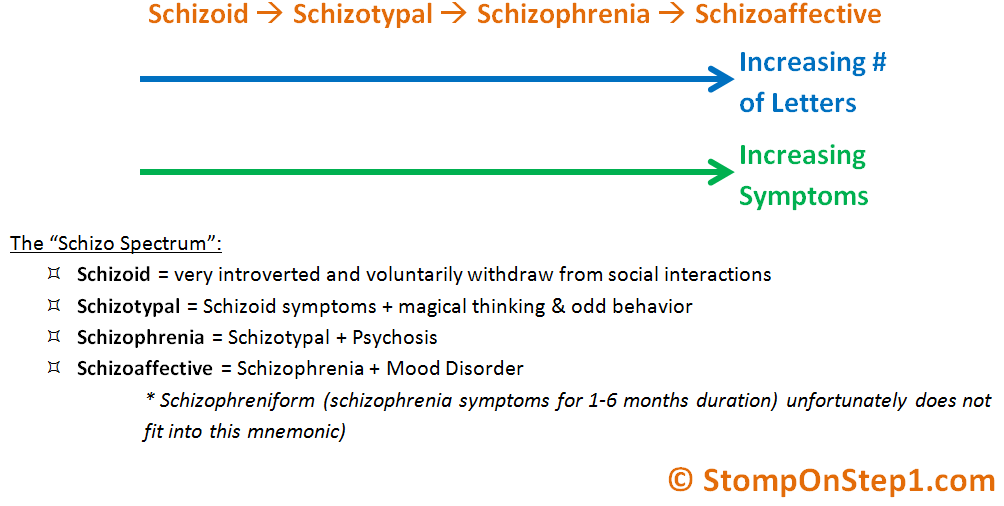 According to DSM-5, catatonia can also include excessive motor activity.] behavior.
According to DSM-5, catatonia can also include excessive motor activity.] behavior.
5. Negative symptoms (i.e. reduced emotional expression or inability to perform purposeful activities). nine0004
C. Over a significant period of time from the onset of an exacerbation, the level of functioning[10 - To be diagnosed with schizophrenia, a person must be low-functioning, although a person who gets along well with schizophrenia may also be considered high-functioning.] in one or more major areas , such as work, interpersonal relationships, or self-care, is markedly reduced from the level reached before the onset of the flare-up (when the onset is in childhood or adolescence, the person may not achieve the expected level of interpersonal, academic, or professional functioning). nine0004
C. Continuous signs of exacerbation persist for at least six months. This period should include at least one month of symptoms (or less if treated successfully) that meet the criteria for group A (i.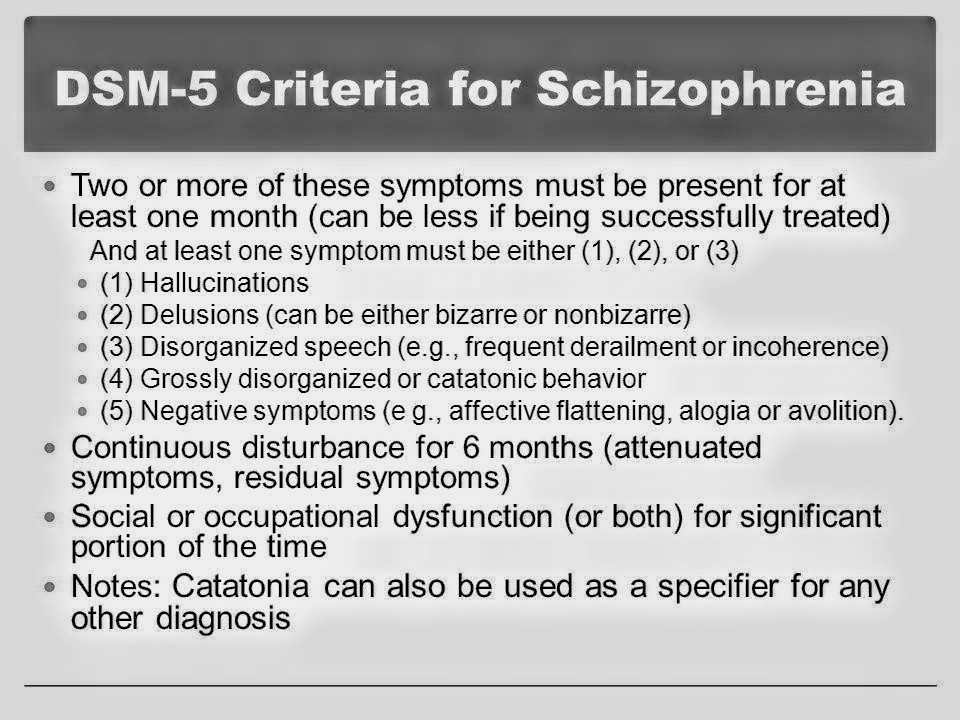 e., active phase symptoms) and may include periods of prodromal [11 - Increasing symptoms of the pathological process preceding the main phase of the disease. - Approx. per.] or residual symptoms. During these prodromal or residual periods, signs of the disorder may present with only negative symptoms or two or more symptoms from Criteria A present in an attenuated form (eg, bizarre beliefs, unusual perceptual sensations). nine0004
e., active phase symptoms) and may include periods of prodromal [11 - Increasing symptoms of the pathological process preceding the main phase of the disease. - Approx. per.] or residual symptoms. During these prodromal or residual periods, signs of the disorder may present with only negative symptoms or two or more symptoms from Criteria A present in an attenuated form (eg, bizarre beliefs, unusual perceptual sensations). nine0004
D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features are excluded for one of the following reasons: 1) no depressive or manic episodes occur concomitantly with symptoms of the active phase; 2) if affective episodes occur during the active phase symptoms, they are present in a smaller part of the total duration of the active and residual periods of the disease.
E. The disorder cannot be attributed to the physiological effects of substances (eg, drug abuse, medication) or other medical condition (disease). nine0004
F.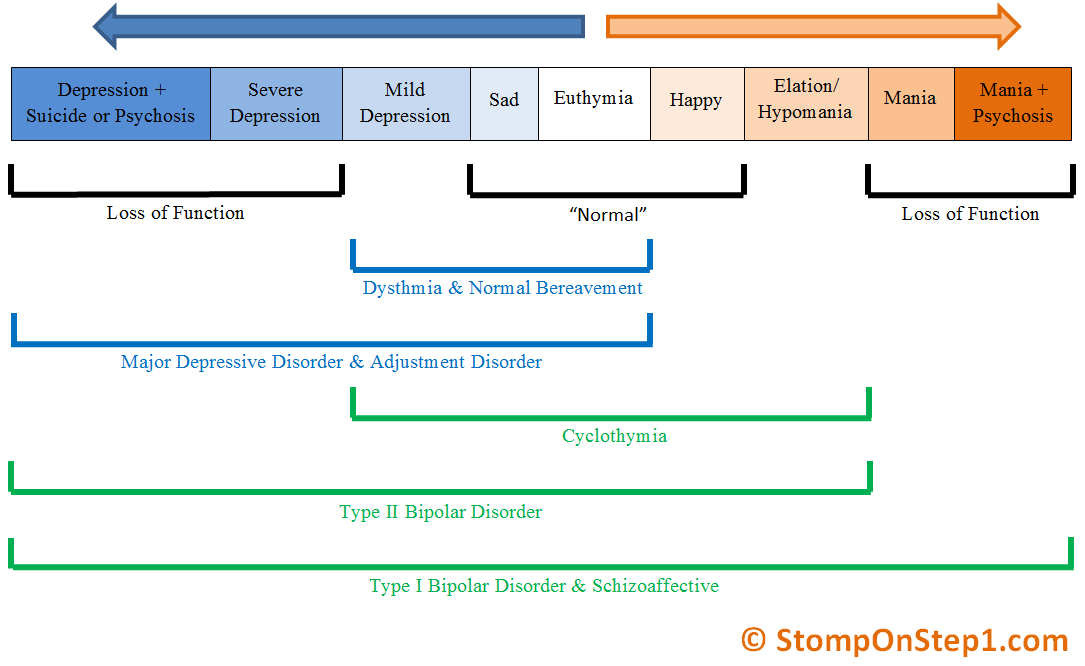 If there is a history of an autism spectrum disorder or communication disorder with onset in childhood, an additional diagnosis of schizophrenia is made only if significant delusions or hallucinations, in addition to other obligatory symptoms of schizophrenia, are also present for at least one month (or less in successful treatment).
If there is a history of an autism spectrum disorder or communication disorder with onset in childhood, an additional diagnosis of schizophrenia is made only if significant delusions or hallucinations, in addition to other obligatory symptoms of schizophrenia, are also present for at least one month (or less in successful treatment).
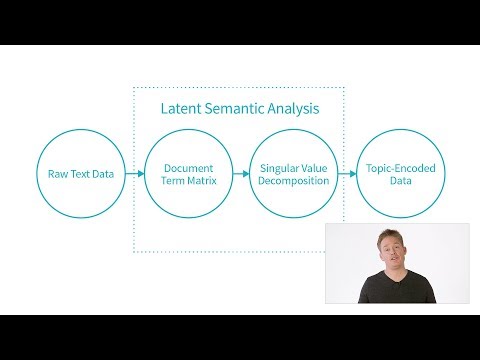
Clinicians diagnose schizophrenia based on these guidelines. Medicine is an inexact science, but psychiatry is doubly inexact. There is no blood test or genetic marker that can tell without a shadow of a doubt that a person is schizophrenic. Schizophrenia itself is nothing more and nothing less than a collection of symptoms that often occur in conjunction. Observing and naming symptoms is mostly useful if these algorithms can talk about a common cause or, better yet, a common treatment or cure. nine0004
Schizophrenia is the best known of the psychotic disorders. Schizoaffective disorder is not so well known to the uninitiated, so I have a whole presentation ready with which I explain the essence of the disease.