Period depression and anxiety
Premenstrual dysphoric disorder (PMDD) | Office on Women's Health
Premenstrual dysphoric disorder (PMDD) is a health problem that is similar to premenstrual syndrome (PMS) but is more serious. PMDD causes severe irritability, depression, or anxiety in the week or two before your period starts. Symptoms usually go away two to three days after your period starts. You may need medicine or other treatment to help with your symptoms.
What is PMDD?
PMDD is a condition similar to PMS that also happens in the week or two before your period starts as hormone levels begin to fall after ovulation. PMDD causes more severe symptoms than PMS, including severe depression, irritability, and tension.
Who gets PMDD?
PMDD affects up to 5% of women of childbearing age. 1 Many women with PMDD may also have anxiety or depression.2
What are the symptoms of PMDD?
Symptoms of PMDD include:3
- Lasting irritability or anger that may affect other people
- Feelings of sadness or despair, or even thoughts of suicide
- Feelings of tension or anxiety
- Panic attacks
- Mood swings or crying often
- Lack of interest in daily activities and relationships
- Trouble thinking or focusing
- Tiredness or low energy
- Food cravings or binge eating
- Trouble sleeping
- Feeling out of control
- Physical symptoms, such as cramps, bloating, breast tenderness, headaches, and joint or muscle pain
What causes PMDD?
Researchers do not know for sure what causes PMDD or PMS. Hormonal changes throughout the menstrual cycle may play a role. A brain chemical called serotonin may also play a role in PMDD. Serotonin levels change throughout the menstrual cycle. Some women may be more sensitive to these changes.
How is PMDD diagnosed?
Your doctor will talk to you about your health history and do a physical examination. You will need to keep a calendar or diary of your symptoms to help your doctor diagnose PMDD.
You must have five or more PMDD symptoms, including one mood-related symptom, to be diagnosed with PMDD.
How is PMDD treated?
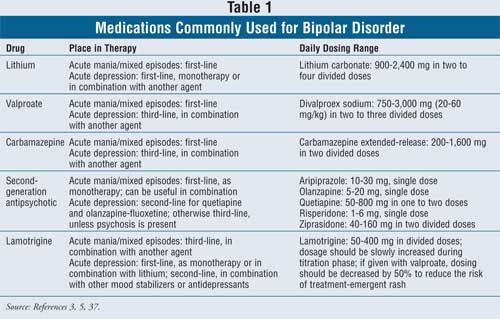
Treatments for PMDD include:
- Antidepressants called selective serotonin reuptake inhibitors (SSRIs). SSRIs change serotonin levels in the brain. The Food and Drug Administration (FDA) approved three SSRIs to treat PMDD:4
- Sertraline
- Fluoxetine
- Paroxetine HCI
- Birth control pills. The FDA has approved a birth control pill containing drospirenone (droh-SPIR-uh-nohn) and ethinyl estradiol (ETH-uh-nil es-truh-DEYE-ohl), to treat PMDD.

- Over-the-counter pain relievers may help relieve physical symptoms, such as cramps, joint pain, headaches, backaches, and breast tenderness. These include:
- Ibuprofen
- Naproxen
- Aspirin
- Stress management, such as relaxation techniques and spending time on activities you enjoy5
Making healthy changes, such as eating a healthy combination of foods across the food groups, cutting back on salty and sugary foods, and getting more physical activity, may also help relieve some PMDD symptoms. But PMDD can be serious enough that some women should go to a doctor or nurse to discuss treatment options. And, if you are thinking of hurting yourself or others, call 911 right away.
Sources
- Potter, J., Bouyer, J., Trussell, J., Moreau, C. (2009). Premenstrual Syndrome Prevalence and Fluctuation over Time: Results from a French Population-Based Survey: Journal of Women’s Health; 18(1): 31–39.
- Pearlstein, T.
 , Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301.
, Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301. - American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: The American Psychiatric Association.
- The Medical Letter. (2003). Which SSRI? Med Lett Drugs Ther; 45(1170):93-5.
- Goodale, I.L., Domar, A.D., Benson, H. (1990). Alleviation of premenstrual syndrome symptoms with the relaxation response. Obstet Gynecol; 75(4):649-55.
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Anxiety, depression and insomnia - the unity or autonomy of functional disorders
It is known that patients with so-called "functional" disorders constitute a significant proportion of patients in the daily practice of doctors of various profiles. Such disorders include insomnia, anxiety and depression, which are common in the practice of neurologists, and which pose the need to resolve the issue of their connection and cause-and-effect relationships.
In practice, we are talking about considering two possibilities: 1) as isolated independent conditions caused by factors specific to each of them, and, accordingly, having features of therapy; 2) as mutually potentiating states that can act as "masks" and continuations of each other and require a unified approach when choosing therapy. nine0003
In addition, there is another important aspect of the problem - the differentiation of organic and functional disorders of the CNS. It is generally accepted that organic diseases are based on structural disorders, i.e. an anatomical substrate. The terms "functional diseases" or "functional disorders of the nervous system" are used to refer to diseases and syndromes that do not have an anatomical substrate. It should be noted that over time, ideas about the nature of organic brain disorders have changed significantly. These now include not only gross anatomical pathology, but also biochemical disorders (impaired metabolism of biologically active substances, etc.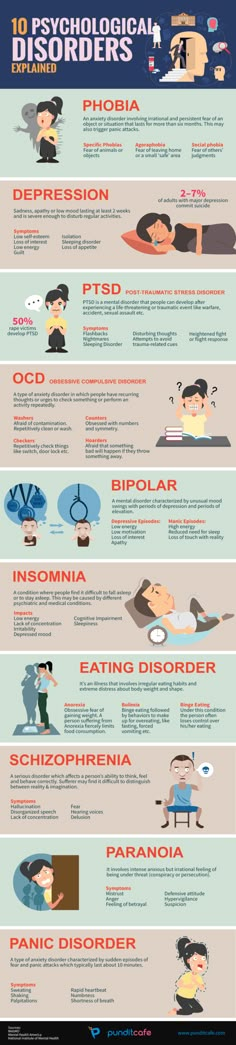 ), which can change the interaction of the functional systems of the brain. However, in clinical medicine, organic and functional diseases and syndromes are distinguished. At the same time, the latter include those disorders in which organic disorders are minimal and cannot be determined without the use of special research methods. In the practice of a neurologist, these include, among others, anxiety disorders, depression, and insomnia. nine0003
), which can change the interaction of the functional systems of the brain. However, in clinical medicine, organic and functional diseases and syndromes are distinguished. At the same time, the latter include those disorders in which organic disorders are minimal and cannot be determined without the use of special research methods. In the practice of a neurologist, these include, among others, anxiety disorders, depression, and insomnia. nine0003
This review is devoted to the consideration of these disorders in terms of the prevalence of these forms of pathology, the frequency and combination of features of their pathogenesis.
Insomnia
Insomnia is defined as a clinical syndrome characterized, on the one hand, by the presence of sleep disorders in the form of disturbances in its onset (difficulty falling asleep), consolidation (frequent nocturnal awakenings and long periods of wakefulness) or quality (dissatisfaction with the depth of sleep, lack of refreshing effect of night sleep), provided that these disorders occur when there is sufficient time for sleep and have consequences in the form of disturbances in daytime activities of various kinds.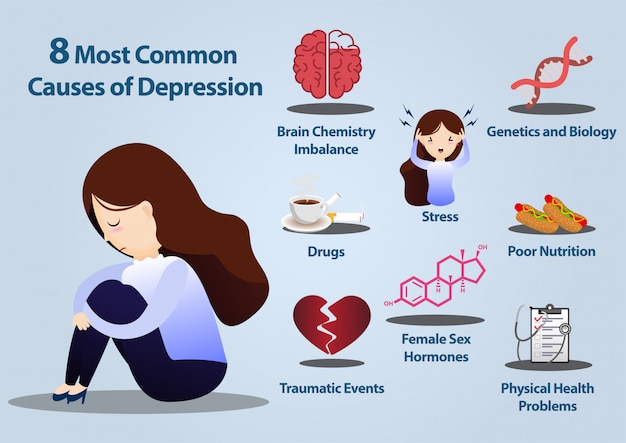 nine0003
nine0003
Existing studies [1-7] show a high prevalence of sleep disorders among the population of different countries. Thus, according to a population study [1], conducted in the United States with the involvement of 3,000 respondents among the adult population, sleep disorders were detected in 35% of the respondents. Among the European population, the prevalence of insomnia is characterized by indicators ranging from 10 to 30% [2]. Canadian researchers [3], who analyzed data on 2000 healthy people over the age of 18, identified at least one symptom of insomnia in 40% of them. In Pakistan, during a survey of 1488 adult urban residents, sleep disorders were noted in 31.3% [4], in India - in 18.6%. In Japan, the frequency of sleep disorders was 20.3% [5]. nine0003
In Russian neurology, epidemiologically, the work of A.V. Wayne [6], conducted in 1989 in Moscow, which summarized the data obtained on a sample of 5,500 respondents over 14 years of age: more than 45% had dissatisfaction with sleep. One of the latest works in this direction is the study of sleep disorders in residents of Chuvashia [7], in which sleep disorders were studied in 2004 residents of this region of our country. Often or constantly complaining about sleep disorders turned out to be 20%. nine0003
One of the latest works in this direction is the study of sleep disorders in residents of Chuvashia [7], in which sleep disorders were studied in 2004 residents of this region of our country. Often or constantly complaining about sleep disorders turned out to be 20%. nine0003
The causes of insomnia can be a number of factors (acute and chronic stress, anxiety, comorbidities, pain, etc.), leading to a hyperactivation reaction with the mobilization of the body's adaptive resources at different levels - cerebral, sympathetic, endocrine. One of the constant manifestations of such activation is the quantitative and qualitative changes in the sleep process. With short-term exposure to stress, episodic insomnia develops (lasting up to one week), while persistence of stress is the leading factor in the chronification of insomnia. The persistence of stress with the subsequent development of a number of diseases can be facilitated by: high intensity or duration of the stress reaction, culminating in the depletion of adaptive reserves; personal or biological characteristics that determine the weakness of anti-stress protection.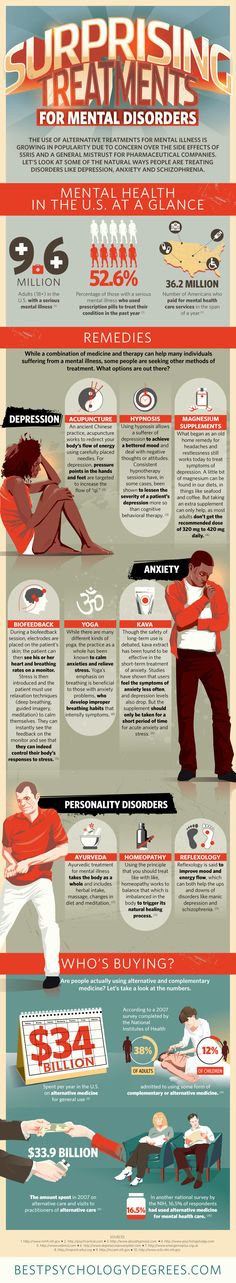 nine0003
nine0003
Insomnia disorders can consist both in a violation of falling asleep (presomnic nature of disorders), maintaining sleep (intrasomnic), and in difficulties with awakening, dissatisfaction with the quality of sleep, daytime manifestations (postsomnic).
Sleep disorders can be recorded by various methods, the most common of which is polysomnography. Polysomnographic curves for these disorders register an increase in sleep latency, the duration of nocturnal wakefulness, the index of awakenings and micro-awakenings, a reduction in the density of delta sleep with a compensatory increase in the representation of superficial sleep phases. nine0003
The presence of cerebral hyperactivation in insomnia was confirmed [8] by the data of functional magnetic resonance imaging (fMRI): in violation of sleep, the absence of a decrease in the level of metabolism in brain areas associated with emotional response was revealed, primarily the mesiotemporal cortex and the anterior cingulate gyrus. The presence of sympathetic activation in insomnia was confirmed [9] by the results of a study of heart rate variability, which showed an increase in the ratio between the low-frequency (sympathetic) and high-frequency (parasympathetic) components of the spectral power of heart rate variability towards increase. In patients with insomnia, this ratio turned out to be higher than in healthy people both in the state of wakefulness and at various stages of non-REM and REM sleep. nine0003
The presence of sympathetic activation in insomnia was confirmed [9] by the results of a study of heart rate variability, which showed an increase in the ratio between the low-frequency (sympathetic) and high-frequency (parasympathetic) components of the spectral power of heart rate variability towards increase. In patients with insomnia, this ratio turned out to be higher than in healthy people both in the state of wakefulness and at various stages of non-REM and REM sleep. nine0003
Particular attention is paid to the activation of the endocrine system in insomnia. It is expressed primarily in an increase in cortisol production during the day. When comparing the levels of cortisol and adrenocorticotropic hormone (ACTC) in blood plasma, it was shown that the maximum differences in these indicators in patients with insomnia and well-sleeping people are observed in the evening and at night. The presence of hyperactivation interferes with falling asleep and maintaining sleep at this level of regulation [10]. In addition, the release of "stress hormones" during insomnia is also extremely important due to the fact that there are reciprocal relationships between norepinephrine in the periphery and norepinephrine in the brain: an increase in the level of the peripheral hormone counteracts an increase in the level of norepinephrine in the brain tissues, and its deficiency in the central nervous system leads to an increase in the basal level of corticosteroids [11]. The latter (especially glucocorticoids) activate the tryptophan pyrrolase enzyme located in the liver, which converts tryptophan to the kynurenine metabolic pathway, which can lead to a decrease in serotonin synthesis. There are separate reports indicating that corticosteroids induce tyrosine transaminase, as a result of which the content of tyrosine in the blood decreases and the synthesis of norepinephrine in the brain decreases [12]. Thus, a decrease in the level of norepinephrine triggers a whole cascade of biochemical reactions.
In addition, the release of "stress hormones" during insomnia is also extremely important due to the fact that there are reciprocal relationships between norepinephrine in the periphery and norepinephrine in the brain: an increase in the level of the peripheral hormone counteracts an increase in the level of norepinephrine in the brain tissues, and its deficiency in the central nervous system leads to an increase in the basal level of corticosteroids [11]. The latter (especially glucocorticoids) activate the tryptophan pyrrolase enzyme located in the liver, which converts tryptophan to the kynurenine metabolic pathway, which can lead to a decrease in serotonin synthesis. There are separate reports indicating that corticosteroids induce tyrosine transaminase, as a result of which the content of tyrosine in the blood decreases and the synthesis of norepinephrine in the brain decreases [12]. Thus, a decrease in the level of norepinephrine triggers a whole cascade of biochemical reactions.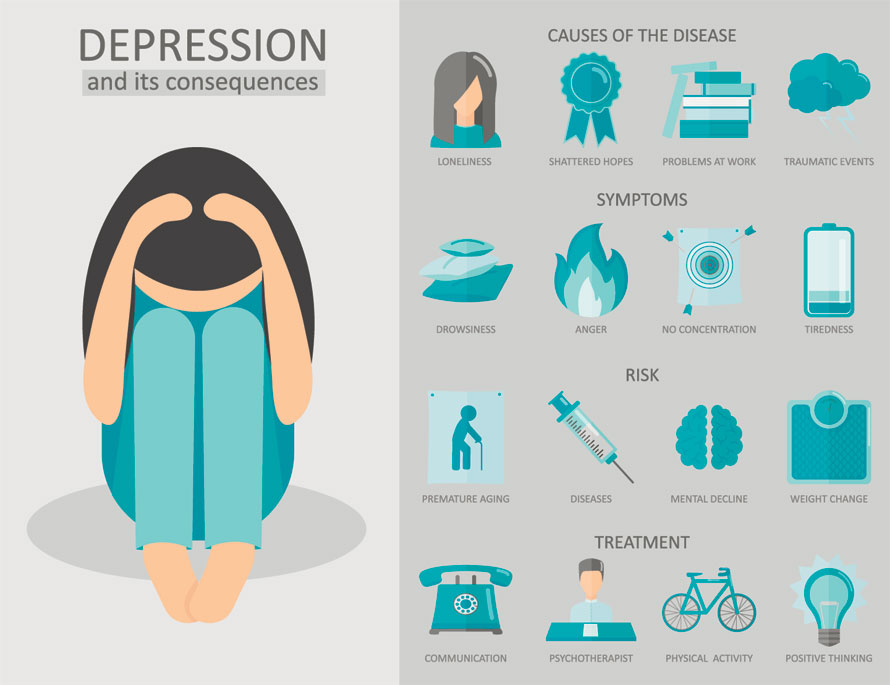 nine0003
nine0003
Obviously, there are other ways in which glucocorticoids and ACTH can affect the metabolism and activity of monoamines, since cortisol induces or inhibits a number of enzyme systems. But the above facts show that a positive feedback relationship (a kind of vicious circle) can be established between the increased secretion of cortisol and a deficiency of serotonin and norepinephrine in the brain: a deficiency of these monoamines leads to hypercorticism and disruption of the circadian rhythm of secretion, and an excess of cortisol disrupts synthesis, as a result what their deficiency is formed, which subsequently can become one of the mechanisms for the development of endogenous depression, according to one of the main theories of its formation - monoamine. nine0003
It can be seen from the above that the generality and universality of biological changes at the brain level play an important role in maintaining the sleep-wake cycle, and any quantitative (mainly deficient) and qualitative (metabolic disorders) changes can form complex pathological conditions that need to be carried out.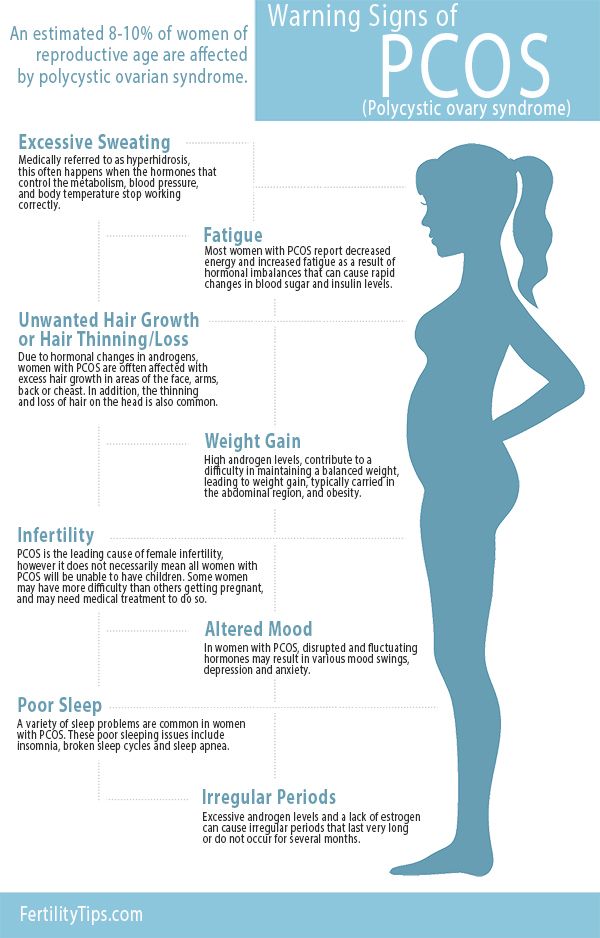 differential diagnosis and choice of treatment tactics.
differential diagnosis and choice of treatment tactics.
Given the impact of insomnia on the body, it becomes clear the connection between insomnia disorders and a number of mental illnesses. So, in generalized anxiety disorder, their frequency reaches 56-75%, in bipolar affective disorder during a depressive episode - 80% [13]. nine0003
Alarm
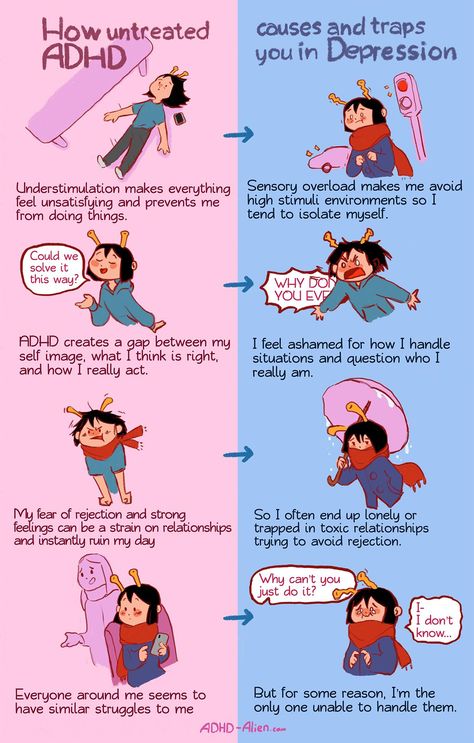
Anxiety initially reflects the normal reaction of the body, in particular the psyche, to changing environmental conditions and the effects of stress. But with their prolonged exposure or inadequate adaptive behavior, it loses its sanogenic property, turning into an anxiety disorder, often combined with depression and insomnia.
During the formation and consolidation of such a pathological reaction, anxiety is characterized by constant anxiety, often associated with a sense of impending danger, internal tension, and the expectation of unforeseen events. In general, we are talking about hypertrophied and maladaptive reactions to stress. nine0003
nine0003
According to one of the American studies [13], the annual prevalence of anxiety disorders in the general population is 18.1%, and during the lifetime - 28.2%, which is significantly higher than the prevalence of any other mental disorder [14] . In a study conducted in Morocco [15], the prevalence of this disease during the year was higher than the above figures - 25.5%.
The frequency of the considered pathology depends on a number of cultural factors. Thus, post-traumatic stress disorder occurs in 1-2% of the population of Western Europe and in 6-9% of the inhabitants of North America and in more than 10% of the inhabitants of countries involved in religious conflicts [16].
In an international study conducted under the auspices of WHO [17], the incidence of anxiety disorders in the world at the level of primary care was determined to be 8%, while in Italy this figure was 3.8%, and in Greece - 14.8% .
In addition to the above, it can be added that in institutions of the general medical network the frequency of anxiety disorders reaches 23-78%, in outpatient services - an average of 45. 9% [eighteen].
9% [eighteen].
It is noted that the frequency of anxiety disorders depends on the presence of chronic somatic diseases, especially cardiovascular diseases. Fear of having a heart disease and associated death (cardiophobia) is diagnosed in 80% of patients in general medical practice who seek pain in the heart area [19]. In patients with coronary heart disease (CHD), anxious hypochondriacal reactions are detected in 28.2%, somatized reactions in 3%, anxiety-phobic reactions in 2.9%%; anxiety disorders are recorded in 98.6% of patients with arterial hypertension and in 89.6% of patients with chronic heart failure [20]. According to the American Psychiatric Association, the incidence of early generalized anxiety disorder (GAD) in patients with acute cerebrovascular accident reaches 27%, late (after 3 months) - 23% [21].
There are three main approaches to explaining the causes of anxiety disorders; psychological, neurobiological and genetic. nine0003
The psychoanalytic approach is based on the well-known works of S. Freud on the nature of neurotic anxiety, which they opposed to realistic anxiety. Under realistic anxiety, they consider [22] a rational and understandable reaction to danger, which performs an adaptive function. From the point of view of cognitive-behavioral therapy, pathological anxiety arises as a result of maladaptive and dysfunctional cognitions, which are either inherent in the individual from birth or arise in the process of his development. If an individual has dysfunctional beliefs, any event or stimulus can be seen as threatening life or personal freedom, which triggers an anxiety reaction. However, such anxiety does not contribute to adaptation and subsequently leads to an even stronger fixation of dysfunctional disorders. nine0003
Freud on the nature of neurotic anxiety, which they opposed to realistic anxiety. Under realistic anxiety, they consider [22] a rational and understandable reaction to danger, which performs an adaptive function. From the point of view of cognitive-behavioral therapy, pathological anxiety arises as a result of maladaptive and dysfunctional cognitions, which are either inherent in the individual from birth or arise in the process of his development. If an individual has dysfunctional beliefs, any event or stimulus can be seen as threatening life or personal freedom, which triggers an anxiety reaction. However, such anxiety does not contribute to adaptation and subsequently leads to an even stronger fixation of dysfunctional disorders. nine0003
Genetic predisposition plays a role in the occurrence and persistence of an anxiety disorder. There is evidence of a gene responsible for the risk of developing anxiety disorders. This was revealed in an Icelandic study [23] by genotyping 353 people. Information has been obtained on the association of anxiety disorder with the gene 9q31 [23]. A high level of concordance in the development of GAD in monozygotic twins was also revealed [24] - 37.9% (in contrast to the risk of developing panic disorders - 22.6%). nine0003
Information has been obtained on the association of anxiety disorder with the gene 9q31 [23]. A high level of concordance in the development of GAD in monozygotic twins was also revealed [24] - 37.9% (in contrast to the risk of developing panic disorders - 22.6%). nine0003
There are ideas that the hippocampus and amygdala play an important role in the neurobiological substrate of anxiety disorders. According to neuroimaging research methods, individuals with anxiety disorders have increased activation of the amygdala in response to threatening stimuli compared to controls [25]. If we talk about the hippocampus, then, as animal studies show, it is involved in the formation of the fear response and avoidance of danger. In the case of prolonged exposure of an animal to threatening stimuli, a decrease in the volume of the hippocampus and a change in behavior towards avoiding any new stimuli occur [26]. nine0003
It is also known that anxiety realizes its function of quick response to changing environmental conditions through the activation of the hypothalamic-pituitary-adrenal system, which has an indirect effect on sleep [27]. For example, in rats under conditions of acute stress, REM sleep primarily reacts, changes in which are associated with changes in the secretion of corticotropin-releasing hormone (CRH), or corticoliberin [28]. In different models of stress in rats, an increase in the phase of REM sleep and a reduction in slow-wave sleep were noted [29]. The subjects also showed an increase in the representation of the REM phase when exposed to a stress factor [30]. At the same time, with an increase in the activity of the sympathetic nervous system and, in fact, a decrease in the number of non-REM sleep phases to 2 (NREM1, NREM2), there is an increase in periods of superficial sleep with frequent awakenings and "micro-awakenings". This is reflected in the polysomnographic picture of sleep (see figure): a characteristic “palisade of anxiety” appears on the hypnogram (frequent awakenings - falling asleep, not deeper than the 2nd stage of sleep.
For example, in rats under conditions of acute stress, REM sleep primarily reacts, changes in which are associated with changes in the secretion of corticotropin-releasing hormone (CRH), or corticoliberin [28]. In different models of stress in rats, an increase in the phase of REM sleep and a reduction in slow-wave sleep were noted [29]. The subjects also showed an increase in the representation of the REM phase when exposed to a stress factor [30]. At the same time, with an increase in the activity of the sympathetic nervous system and, in fact, a decrease in the number of non-REM sleep phases to 2 (NREM1, NREM2), there is an increase in periods of superficial sleep with frequent awakenings and "micro-awakenings". This is reflected in the polysomnographic picture of sleep (see figure): a characteristic “palisade of anxiety” appears on the hypnogram (frequent awakenings - falling asleep, not deeper than the 2nd stage of sleep.
Characteristic graphic "palisade of anxiety", detected during polysomnography in a patient with anxiety-depressive syndrome.
The presence of sleep disorders is a "core" symptom of generalized anxiety disorder - about 60-70% of patients with this diagnosis have sleep disorders [31].
Depression
In general medical practice, depression ranks second after arterial hypertension, occurring in approximately one in 10 outpatients, and the overall prevalence rate is about 50% [32]. In a large international study [33], conducted at the end of the last century, depression was detected on average in 69% (45-95%) of patients seeking medical help for somatic disorders. There is also evidence that depression is the only cause of 10-20% of visits to general practitioners [34], and their prevalence among patients with severe somatic diseases reaches 20-60% [35].
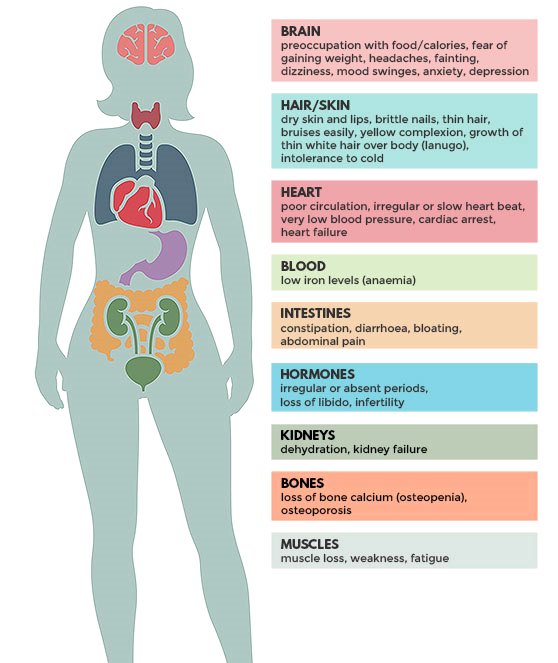
Of all the diagnostically significant manifestations of depression, two symptoms of the current depressive episode are of a somatic nature: fatigue/weakness/apathy, observed in 73% of patients, insomnia/drowsiness - in 63% [36].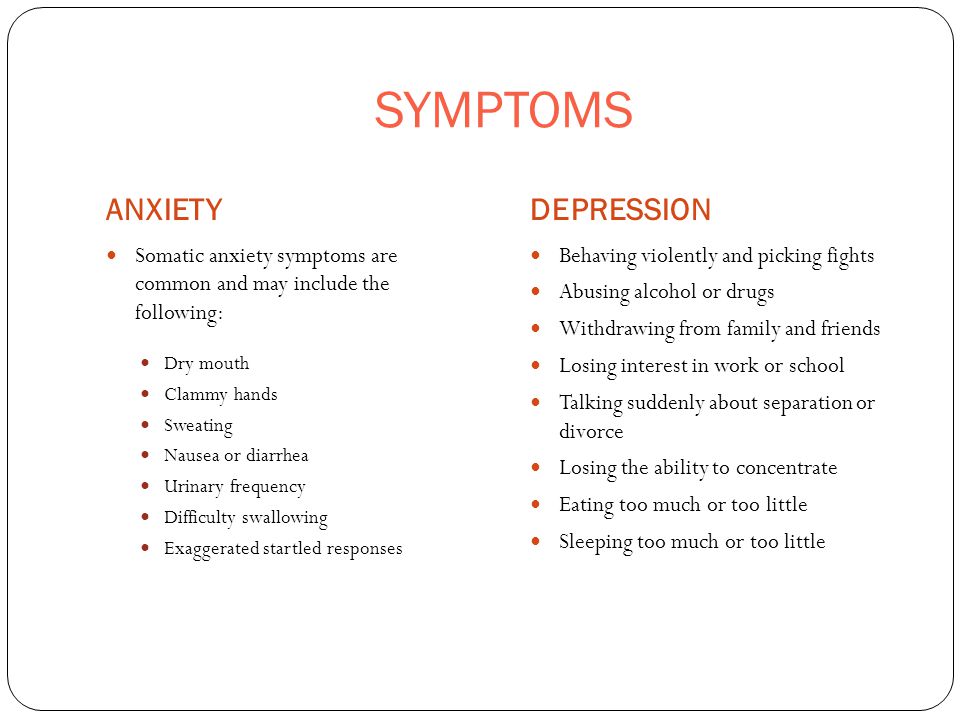 nine0003
nine0003
As for insomnia, in some cases it is so pronounced that patients perceive depression as a sleep disorder [37].
Polysomnographic abnormalities are detected in 40-60% of outpatients and 90% of hospitalized patients with a depressive episode, among which are sleep continuity disorders (increased sleep latency, total wake time during sleep, frequency of early morning awakenings, reduced total sleep duration). The absolute and relative (from the total sleep time) deficit of slow-wave sleep is characteristic. Quantitative and qualitative changes in REM sleep include a reduction in REM latency, an increase in the duration of the first period of REM sleep, an increase in REM activity (total number of eye movements during the night), an increase in REM density (ratio - REM activity / total REM time -sleep) and an increase in the proportion of REM sleep from total sleep time [38]. Sleep in patients with depression in remission may also remain disturbed: the duration of delta sleep is reduced, and the time to the onset of REM sleep is reduced (the latter is associated with an increased risk of relapse of depression).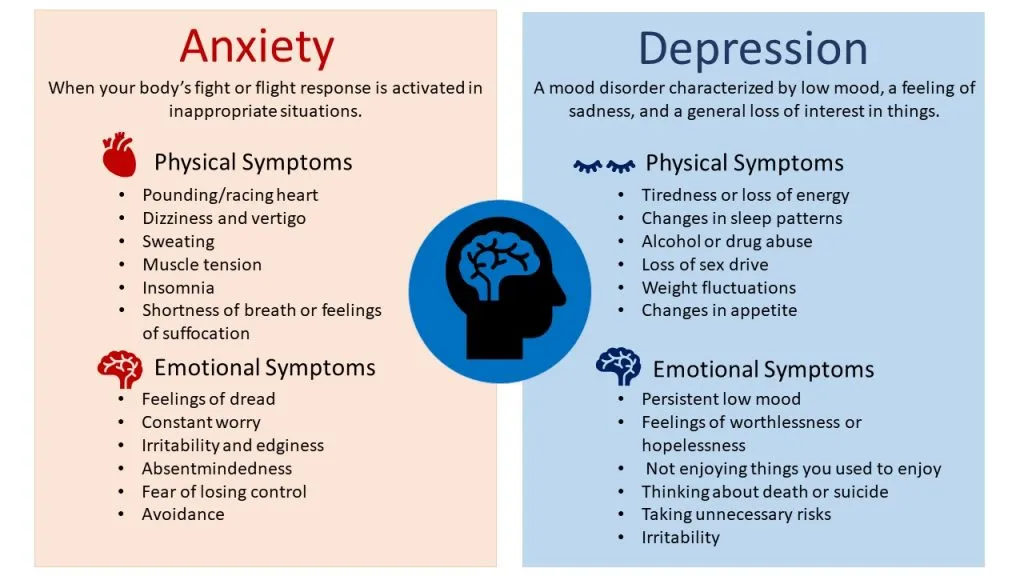 nine0003
nine0003
Polysomnographic studies conducted in individuals at high risk of developing depression have shown that the shortened time of the onset of the REM sleep phase and the lack of slow-wave sleep are familial and polysomnographic abnormalities may precede the clinical manifestation of depression [39]. It is believed that the role of genetic factors is about 30-40%. The remaining 60-70% are attributed to behavioral factors and determined by the interaction of the genome with the environment.
Among the neurobiological theories of depression, serotonergic and noradrenergic theories dominate, which are confirmed by the fact that any agent that inhibits the reuptake of serotonin and norepinephrine (which is the basis of the effect of a number of antidepressants) leads to a clinically significant improvement in the condition of patients with depression. The role of corticoliberin and stress hormones in the formation of depressive disorders is also noted. Currently, neurotrophic GABA-, glutamate-mediated, dopaminergic theories of depression are being considered [40].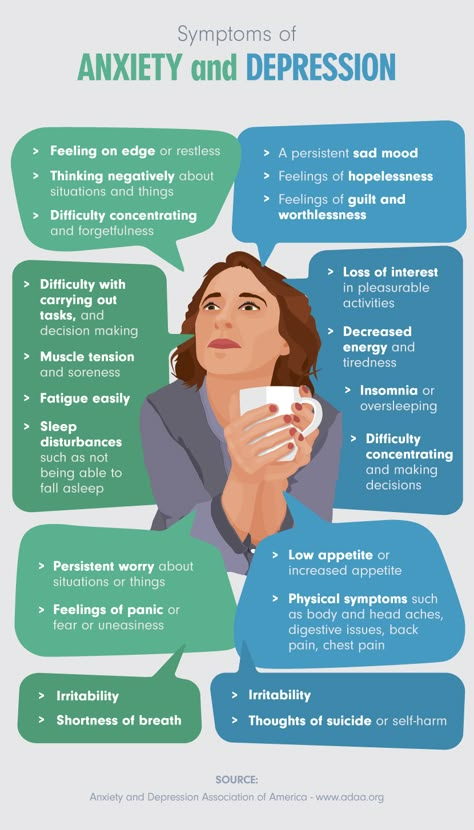 nine0003
nine0003
The circadian hypothesis is also widespread, according to which manifestations of abnormal circadian rhythms characteristic of depression, including diurnal fluctuations in symptoms, disturbances in sleep and other behavioral and physiological functions, are not only typical clinical manifestations of a depressive disorder, but also one of the key pathogenetic factors of depression. Since the leading role in the regulation of these rhythms belongs to melatonin, much attention is currently paid to it in the study of depression, including in the therapeutic aspect: it is believed that the correction of melatonin levels in patients with depression can be an important additional component of treatment. If we take into account the violation of the circadian rhythm, then it is also advisable to prescribe a drug such as melaxen (Unipharm). nine0003
Summarizing the above materials, we can state that such functional disorders as anxiety, depression and insomnia, often combined, are widespread in the practical work of a neurologist, and they are often comorbid somatic pathology. At the basis of their development, they have similar mechanisms, the main component of which is the hyperactivation of the sympathetic nervous system. This corresponds to general changes in the structure of sleep (an increase in the representation of the fast phase, a decrease in its latency, a reduction in slow-wave sleep), but at the same time, there are signs that characterize each of the conditions studied: "alpha-delta rhythm" in depression, which necessitates a differentiated approach to the diagnosis of these conditions and their therapy with the development of uniform standards for diagnosis and treatment. nine0003
At the basis of their development, they have similar mechanisms, the main component of which is the hyperactivation of the sympathetic nervous system. This corresponds to general changes in the structure of sleep (an increase in the representation of the fast phase, a decrease in its latency, a reduction in slow-wave sleep), but at the same time, there are signs that characterize each of the conditions studied: "alpha-delta rhythm" in depression, which necessitates a differentiated approach to the diagnosis of these conditions and their therapy with the development of uniform standards for diagnosis and treatment. nine0003
What do we know about anxiety and depression?
Evgeniy Gennadievich Ilchenko, psychotherapist of the Department for the Treatment of Borderline Mental Disorders and Psychotherapy of the National Research Center for Psychiatry and Neurology. V.M. Bekhterev.
Anxiety, depression are conditions that are characteristic of disturbances in the state of the emotional sphere.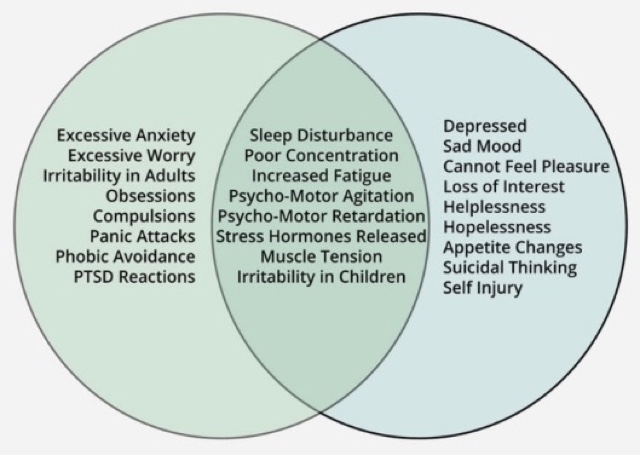 Today, about 110 million people in the world suffer from depression. According to the World Health Organization, one in five women and one in fifteen men suffer from depression in major cities around the world. It is believed that by 2020 depression will take one of the first places among all diseases. Approximately 70% of depressed patients show suicidal tendencies, and depressed patients older than 75 have the highest rate of suicide. nine0003
Today, about 110 million people in the world suffer from depression. According to the World Health Organization, one in five women and one in fifteen men suffer from depression in major cities around the world. It is believed that by 2020 depression will take one of the first places among all diseases. Approximately 70% of depressed patients show suicidal tendencies, and depressed patients older than 75 have the highest rate of suicide. nine0003
I am suffering, I am afraid…
What is depression? Depression is a disease that can throw a person out of emotional balance for a long time and significantly impair the quality of his life. It can be difficult for you to concentrate, nothing is interesting, nothing pleases, doubts and fears are constantly overcome. Depression usually comes after a psychological trauma or negative event. Often it develops as if for no apparent reason. It can be caused by constant stress, accumulating fatigue, fears. Depression is more than just low mood. In this case, the work of the whole organism changes, as a person suffers from insomnia or early awakenings, he loses his appetite or begins to seize his anxiety, which leads to obesity and the development of metabolic syndrome, there is a hormonal imbalance. A person changes his attitude towards others and himself. nine0003
In this case, the work of the whole organism changes, as a person suffers from insomnia or early awakenings, he loses his appetite or begins to seize his anxiety, which leads to obesity and the development of metabolic syndrome, there is a hormonal imbalance. A person changes his attitude towards others and himself. nine0003
Longing, apathy, anxiety…
How does depression manifest itself? The first symptoms include weakness, fatigue, unwillingness to do anything, strain once again, contact and communicate with people, go to work. Later, bodily symptoms may join these complaints - palpitations, sweating, trembling in the body, hot or cold flashes.
Three areas are involved in depression - emotional, mental and physical. At the emotional level, depression, melancholy, apathy, and anxiety are observed. On the mental level - thoughts about one's guilt, self-accusations, a negative vision of the future, a feeling of hopelessness, that "no one will help me.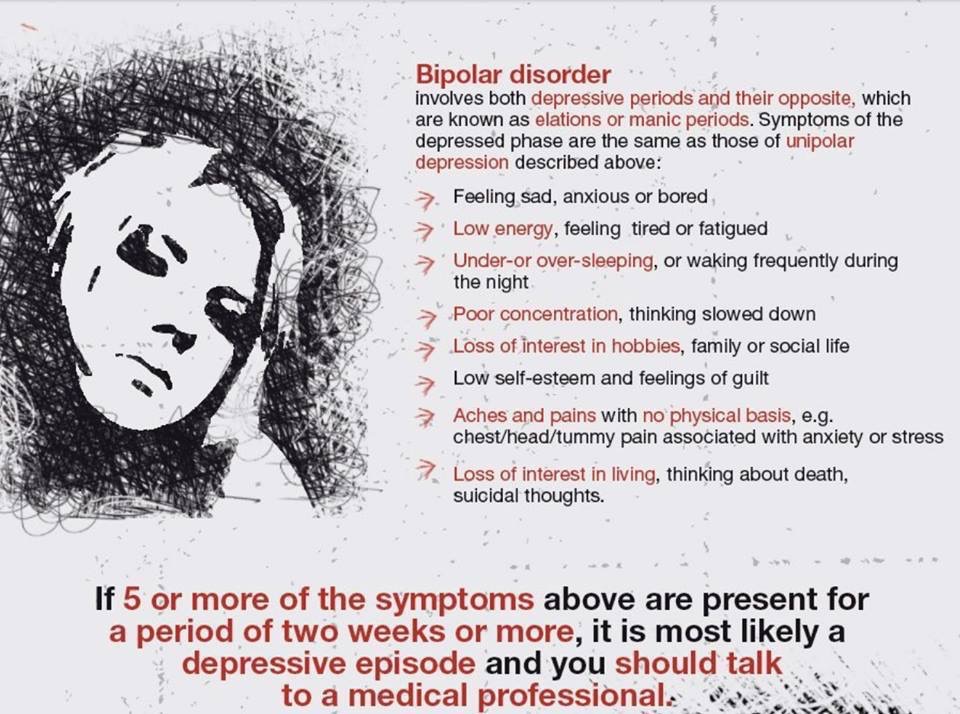 " On the physical level - chronic pain, muscle tension, constipation, dizziness, heaviness in the head. And all these symptoms can constantly change: “Today my head hurts, and yesterday my joints hurt, the day before yesterday my heart hurt.” nine0003
" On the physical level - chronic pain, muscle tension, constipation, dizziness, heaviness in the head. And all these symptoms can constantly change: “Today my head hurts, and yesterday my joints hurt, the day before yesterday my heart hurt.” nine0003
Maybe it's psychosomatics?
It is worth noting that there are different types of depression. According to the classification, depressions are diverse: major, minor, neurotic, autumnal, endogenous, psychogenic, reactive, etc. There is depression associated with the reproductive function of a woman, this is prenatal and postnatal. There is age-related depression associated with the physiological restructuring of the body, there is an obvious one that occurs with a sharply reduced mood, melancholy, and depression. There is a masked depression that hides under the guise of another disease. For example, chronic pain syndrome - pain in different parts of the body. There is depression, which is masked by gastrointestinal symptoms - diarrhea, constipation, stomach pain.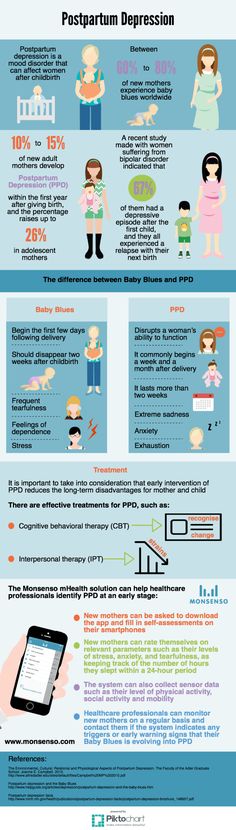 Patients go to doctors for a long time and unsuccessfully, are treated by different specialists. But there is no improvement. At this stage, it is important to recognize psychosomatic disorders. It is worth looking, but what gives a person a disease? How is she good for him? It is quite possible that in this way a person attracts attention to himself, seeks location, manipulates loved ones and relatives. nine0003
Patients go to doctors for a long time and unsuccessfully, are treated by different specialists. But there is no improvement. At this stage, it is important to recognize psychosomatic disorders. It is worth looking, but what gives a person a disease? How is she good for him? It is quite possible that in this way a person attracts attention to himself, seeks location, manipulates loved ones and relatives. nine0003
How can I help?
Sometimes depressed patients try to alleviate their mental state through physical pain, inflicting injuries and injuries on themselves. This is definitely not an option. How can others help such patients? First of all, do not ignore or forbid complaining, do not try to cheer up the patient, do not appeal to conscience and faith, do not demand the adoption of any important decisions, but simply be there and listen patiently. As for direct treatment, there is no “magic” remedy for depression. Various methods are used here: psychotherapy, pharmacotherapy, electroconvulsive therapy, physiotherapy, aroma and color therapy, physical activity.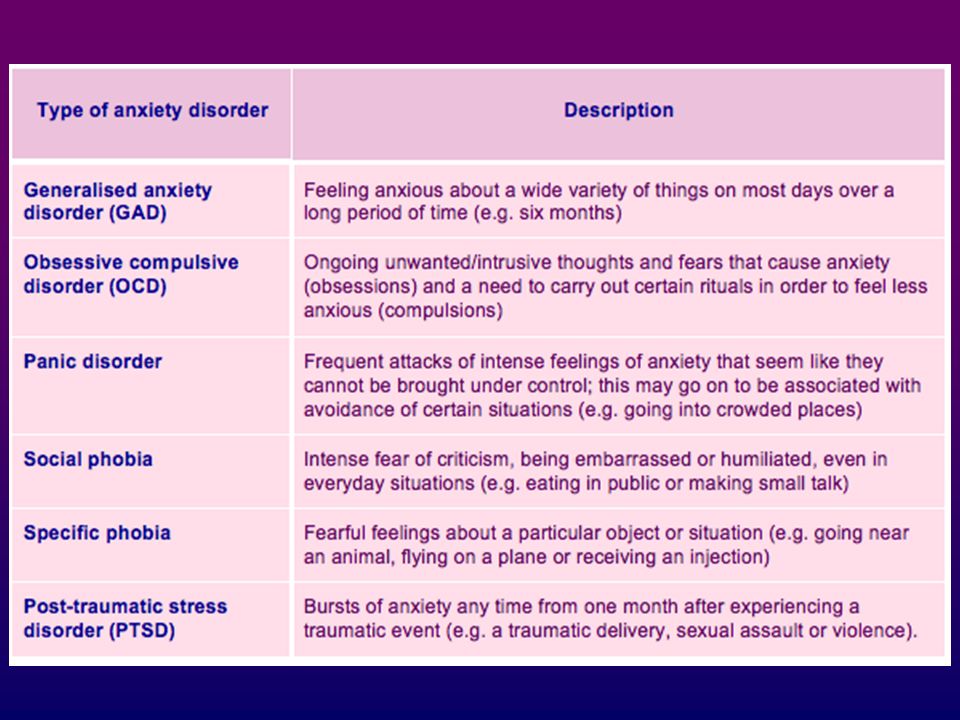 If we talk about the prevention of depression, then this is a healthy lifestyle and a positive attitude, communication with nature. nine0003
If we talk about the prevention of depression, then this is a healthy lifestyle and a positive attitude, communication with nature. nine0003
Feelings about the future
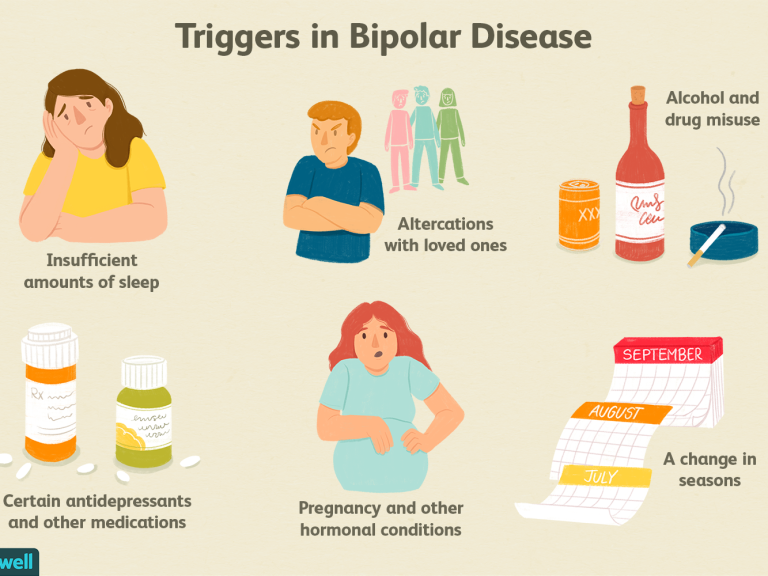
Depression is a negative experience of past life events that we cannot change, while anxiety is an experience for the future, this is a vague, unpleasant emotional state characterized by the expectation of an unfavorable development of events, the presence of bad forebodings, tension and anxiety. It is directed to the future, it is the expectation of something indefinite. The state of anxiety is pointless, but anxiety is a personality trait of a person prone to experiencing anxiety, and constantly experiencing it. Most often, a person's anxiety is associated with the expectation of the social consequences of his success or failure. nine0099 Risk factors for the development of anxiety include childhood trauma, stress, personality traits, genetic predisposition, alcohol and psychoactive substances. Anxiety can be normal or excessive. In pathological cases, anxiety becomes constant and harmful, appearing not only in stressful situations, but also for no apparent reason, and then anxiety not only does not help a person, but begins to interfere with his daily activities.
Anxiety can be normal or excessive. In pathological cases, anxiety becomes constant and harmful, appearing not only in stressful situations, but also for no apparent reason, and then anxiety not only does not help a person, but begins to interfere with his daily activities.
Panic attacks
The largest category of anxiety disorders are phobias, with about a hundred variants. Anxiety disorders include post-traumatic stress disorder, social anxiety, panic attacks, and separation anxiety. Speaking of anxiety, it is worth mentioning panic attacks separately. How do they appear? Unexpected internal tension, pointless fear, timidity, stiffness, feeling of danger, unreality of what is happening, "lump in the throat", chills, sweating, heart palpitations, suffocation, nausea, diarrhea, dizziness, goosebumps, restlessness. What to do in such cases? It is necessary to focus on the real situation, to calm down, to be distracted, to understand that there is no real threat.