Living with anorexia and bulimia
Living With Someone With An Eating Disorder
This page offers tips and guidance for people who live with someone with an eating disorder.
Tips for living with someone with an eating disorder
It’s often difficult to know what to do when you live with someone with an eating disorder. Here are some ideas for everyone — from parents, grandparents and siblings, through to partners and roommates.
Encourage the person to seek professional help
Overcoming an eating disorder can be very difficult without assistance, so accessing professional help is an important goal. Remember that when someone has an eating disorder, they are often protective and private about it. They can feel threatened if someone tells them they need to seek help for it and may lash out in anger or denial. Try not to take it personally and try again later. Reassure them that you are only acting out of concern for them and that you are here to support them.
Encourage the person to recognise their other skills and attributes
Use your knowledge of the person to encourage them to see the positive effects change can bring. Keep communication positive and open — take time to talk about a variety of topics. Focusing on the eating difficulties creates a stressful environment, which may result in the person withdrawing from contact with you. Try and focus on their positive behaviours, rather than the more destructive ones. Don’t compliment their physical appearance; comment on their personality, their intelligence, their talents, their dreams. Get excited when they express an interest in something outside of food, dieting or body image. Ask them questions about the topic.
Use laughter as a means of communication
Humour is a great communication tool. Laughter helps a person to relax and let their guard down a bit. This doesn’t mean you should pounce on them about their eating disorder after a good laugh but you might be able to get them to start talking a bit more openly about what they are going through.
Take the focus off food and weight
The person with the eating disorder is already overly focused on food and weight issues. Don’t talk negatively about your own body or appearance around someone with an eating disorder. Try not to put emphasis on the things you ate (for example, don’t ‘pat yourself on the back’ for eating a salad or berate yourself for eating chocolate). Don’t change your own eating habits around the person with an eating disorder but try not to make a big deal of it either.
Mealtimes should not become a battleground
Frustrations and emotions need to be expressed but not at meal times; this is already likely to be a very difficult time. Try to keep the conversation away from the eating disorder when there is food on the table. If you are doing meal support for someone with an eating disorder, give authentic encouragement, such as “I’m really proud of your hard work” and empathise with how they are feeling (“I know this is very difficult for you”).
Accept limitations in your responsibilities
The support and encouragement of family and friends is vital; however, it is the person with the eating disorder’s responsibility to take the necessary steps towards recovery. You cannot deal with all the problems associated with the disorder. Your role as a family member or friend is unique and something that a therapist can’t be — just as the therapist’s role is something a family member or friend can’t take on. Don’t blame yourself when things go wrong or the person you care about relapses or has a bad day.
Consider promoting independence as a long-term goal
It is healthy and developmentally appropriate for adolescents and young adults to work towards increasing independence; however, this can be difficult if the person is unwell and unable to make good decisions for themselves. It is well-recognised that family members can play an important role in supporting recovery of an eating disorder, however the level of family intervention and involvement will depend on the person’s age, the degree to which their health might be compromised, and other factors such as living arrangements and meal support.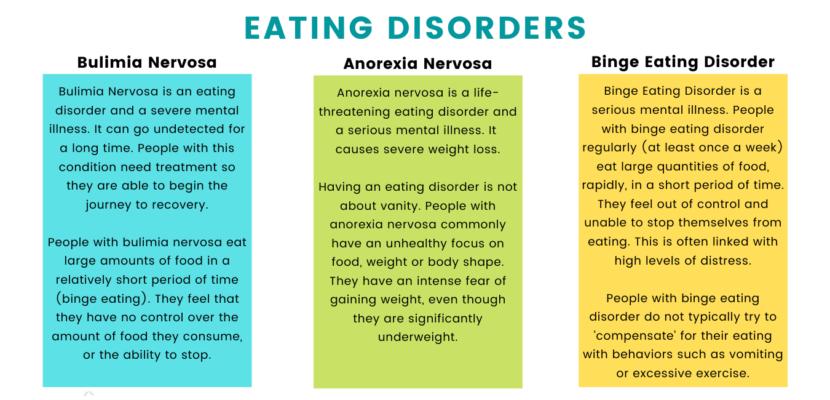 Having a goal of being able to live independently and support themselves may act as an incentive to keep working towards recovery.
Having a goal of being able to live independently and support themselves may act as an incentive to keep working towards recovery.
Set boundaries
If someone is behaving in a way that is difficult for you, it is okay to let them know that their behaviour is not acceptable or you aren’t able to assist at this time. Only set boundaries you can enforce. For example, if the person with an eating disorder asks you to support them when you are having a bad day or need some alone time, it is best to be honest. Respectfully tell them that while you aren’t able to help today, perhaps they could ask another friend or family member. Boundaries are a huge part of self-care and actually strengthen a relationship, rather than hurt it.
Do things as you usually would
The person with the eating disorder needs to learn to co-exist with food and with other people, rather than you learning to co-exist with the eating disorder. Try not to make any changes to meal times, food shopping, outings, topics of conversation, or other interests.
Remind yourself that the person’s behaviour is often a symptom of the eating disorder, rather than a reflection of their character. By separating the person from the disorder, we are reminded of the person we knew before and also the person they can become again. That person is still very much present but their illness is preventing them from being themselves fully.
Enjoy things together
It is important not to let the eating disorder become the focus of the family or relationship. Continue to enjoy things together that you have always done. Tell them about your own life and what is exciting or interesting to you. This may give them more hope towards recovery, when their mind won’t be preoccupied with their body or food.
Spend time with other members of the family or friendship group
The person with the eating disorder is important, but no more so than other people. Don’t neglect your other relationships while caring for someone with an eating disorder. Make sure you give yourself time with people who are completely separate to the person with an eating disorder, so you get a break and don’t burn out.
Make sure you give yourself time with people who are completely separate to the person with an eating disorder, so you get a break and don’t burn out.
Become informed
Information about eating disorders, recovery stories, developing coping strategies and attending support groups can be useful. There are many resources and books written for families and friends. The more educated you are, the more you’ll be able to empathise and understand what they are going through, which may help you to better support them and yourself.
Look after yourself
Get as much support and information as you need. Support groups, relatives, friends, counsellors, telephone support lines and other professionals may be useful. Looking after yourself is as important as looking after the person with the eating disorder.
Be patient
Eating disorders are complicated and recovery can take some time. Sometimes it’s important to remind yourself that the person does not want to be unwell, but they lack the ability to overcome the disorder quickly. There is no specific timeframe for recovery.
There is no specific timeframe for recovery.
FAMILY AND FRIENDS STORIES
India's story - make Dane proud
"It helped a great deal for me to understand that while yes it was hard knowing he had lost a lot of control in his life - I knew he was fighting as hard as he could, that his ED was not his fault, and that I was proud of him."
Read India's Story
Was the page helpful?
NIMH » Eating Disorders
Overview
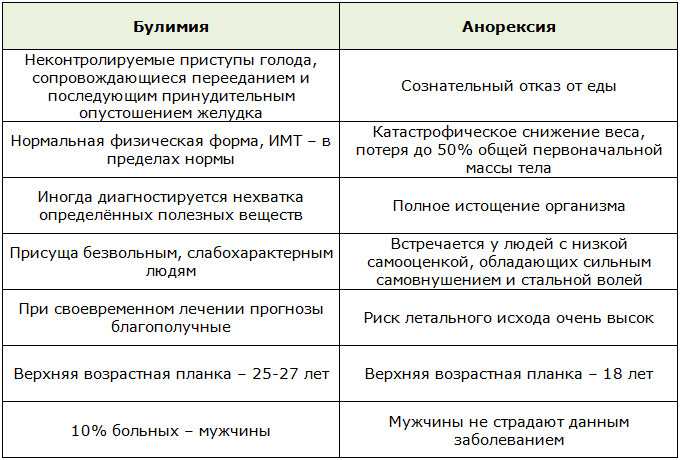
There is a commonly held misconception that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that are associated with severe disturbances in people’s eating behaviors and related thoughts and emotions. Preoccupation with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder.
Signs and Symptoms
Anorexia nervosa
Anorexia nervosa is a condition where people avoid food, severely restrict food, or eat very small quantities of only certain foods. They also may weigh themselves repeatedly. Even when dangerously underweight, they may see themselves as overweight.
There are two subtypes of anorexia nervosa: a restrictive subtype and a binge-purge subtype.
Restrictive: People with the restrictive subtype of anorexia nervosa severely limit the amount and type of food they consume.
Binge-Purge: People with the binge-purge subtype of anorexia nervosa also greatly restrict the amount and type of food they consume. In addition, they may have binge-eating and purging episodes—eating large amounts of food in a short time followed by vomiting or using laxatives or diuretics to get rid of what was consumed.
Anorexia nervosa can be fatal. It has an extremely high death (mortality) rate compared with other mental disorders.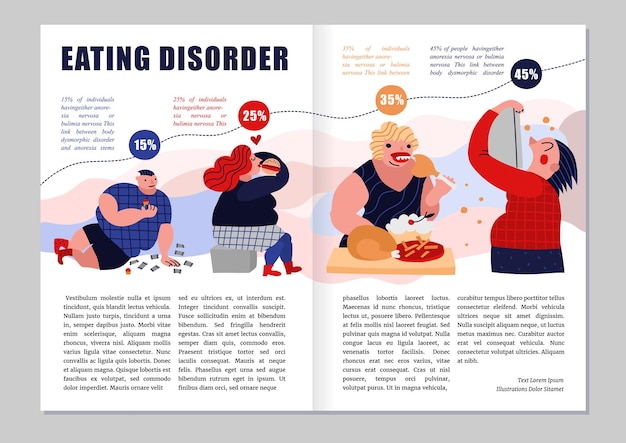 People with anorexia are at risk of dying from medical complications associated with starvation. Suicide is the second leading cause of death for people diagnosed with anorexia nervosa.
People with anorexia are at risk of dying from medical complications associated with starvation. Suicide is the second leading cause of death for people diagnosed with anorexia nervosa.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. In life-threatening situations, call 911.
Symptoms include:
- Extremely restricted eating
- Extreme thinness (emaciation)
- A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight
- Intense fear of gaining weight
- Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape, or a denial of the seriousness of low body weight
Other symptoms may develop over time, including:
- Thinning of the bones (osteopenia or osteoporosis)
- Mild anemia and muscle wasting and weakness
- Brittle hair and nails
- Dry and yellowish skin
- Growth of fine hair all over the body (lanugo)
- Severe constipation
- Low blood pressure
- Slowed breathing and pulse
- Damage to the structure and function of the heart
- Brain damage
- Multiorgan failure
- Drop in internal body temperature, causing a person to feel cold all the time
- Lethargy, sluggishness, or feeling tired all the time
- Infertility
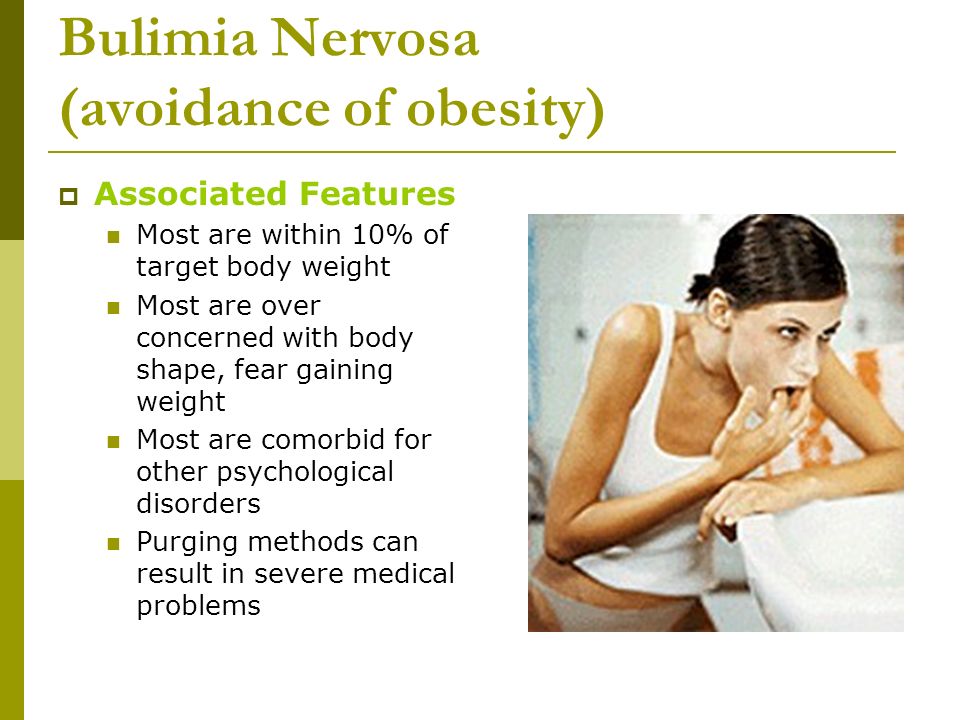
Bulimia nervosa
Bulimia nervosa is a condition where people have recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
Symptoms include:
- Chronically inflamed and sore throat
- Swollen salivary glands in the neck and jaw area
- Worn tooth enamel and increasingly sensitive and decaying teeth as a result of exposure to stomach acid
- Acid reflux disorder and other gastrointestinal problems
- Intestinal distress and irritation from laxative abuse
- Severe dehydration from purging of fluids
- Electrolyte imbalance (too low or too high levels of sodium, calcium, potassium, and other minerals) which can lead to stroke or heart attack
Binge-eating disorder
Binge-eating disorder is a condition where people lose control over their eating and have reoccurring episodes of eating unusually large amounts of food. Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
Symptoms include:
- Eating unusually large amounts of food in a specific amount of time, such as a 2-hour period
- Eating even when you're full or not hungry
- Eating fast during binge episodes
- Eating until you're uncomfortably full
- Eating alone or in secret to avoid embarrassment
- Feeling distressed, ashamed, or guilty about your eating
- Frequently dieting, possibly without weight loss
Avoidant restrictive food intake disorder
Avoidant restrictive food intake disorder (ARFID), previously known as selective eating disorder, is a condition where people limit the amount or type of food eaten. Unlike anorexia nervosa, people with ARFID do not have a distorted body image or extreme fear of gaining weight. ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
Symptoms include:
- Dramatic restriction of types or amount of food eaten
- Lack of appetite or interest in food
- Dramatic weight loss
- Upset stomach, abdominal pain, or other gastrointestinal issues with no other known cause
- Limited range of preferred foods that becomes even more limited (“picky eating” that gets progressively worse)
Risk Factors
Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Eating disorders frequently appear during the teen years or young adulthood but may also develop during childhood or later in life.
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors. Researchers are using the latest technology and science to better understand eating disorders.
Researchers are using the latest technology and science to better understand eating disorders.
One approach involves the study of human genes. Eating disorders run in families. Researchers are working to identify DNA variations that are linked to the increased risk of developing eating disorders.
Brain imaging studies are also providing a better understanding of eating disorders. For example, researchers have found differences in patterns of brain activity in women with eating disorders in comparison with healthy women. This kind of research can help guide the development of new means of diagnosis and treatment of eating disorders.
Treatments and Therapies
It is important to seek treatment early for eating disorders. People with eating disorders are at higher risk for suicide and medical complications. People with eating disorders can often have other mental disorders (such as depression or anxiety) or problems with substance use. Complete recovery is possible.
Treatment plans are tailored to individual needs and may include one or more of the following:
- Individual, group, and/or family psychotherapy
- Medical care and monitoring
- Nutritional counseling
- Medications
Psychotherapies
Family-based therapy, a type of psychotherapy where parents of adolescents with anorexia nervosa assume responsibility for feeding their child, appears to be very effective in helping people gain weight and improve eating habits and moods.
To reduce or eliminate binge-eating and purging behaviors, people may undergo cognitive behavioral therapy (CBT), which is another type of psychotherapy that helps a person learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
Medications
Evidence also suggests that medications such as antidepressants, antipsychotics, or mood stabilizers may also be helpful for treating eating disorders and other co-occurring illnesses such as anxiety or depression.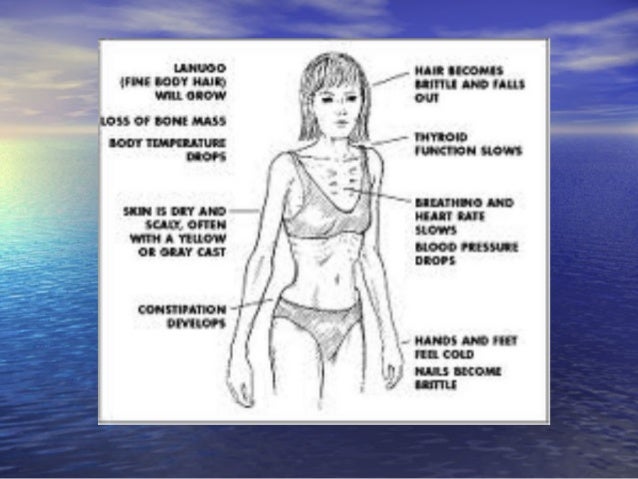 The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.
 gov: Current Studies on Eating Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
gov: Current Studies on Eating Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Learn More
Free Brochures and Shareable Resources
- Eating Disorders: About More Than Food: A brochure about the common eating disorders anorexia nervosa, bulimia nervosa, and binge-eating disorder, and various approaches to treatment. Also available en español.
- Let’s Talk About Eating Disorders: An infographic with facts that can help shape conversations around eating disorders. Also available in en español.
- Shareable Resources on Eating Disorders: Help support eating disorders awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about eating disorders.
Research and Statistics
- NIMH Eating Disorders Research Program: This program supports research on the etiology, core features, longitudinal course, and assessment of eating disorders.
- Journal Articles: References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Eating Disorders
Multimedia
- Mental Health Minute: Eating Disorders: Take a mental health minute to watch this video on eating disorders.
- Let’s Talk About Eating Disorders with NIMH Grantee Dr. Cynthia Bulik: Learn about the signs, symptoms, treatments, and the latest research on eating disorders.
Last Reviewed: December 2021
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Eating problems
Eating behavior is the totality of our eating habits - our taste preferences, eating habits, diet, etc. Eating behavior depends on many factors - cultural, ethnic, family traditions and values, the characteristics of the upbringing and behavior of family members and the biological characteristics of the body, the standards and standards of norm and beauty that have developed in this society. These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
Eating behavior depends on many factors - cultural, ethnic, family traditions and values, the characteristics of the upbringing and behavior of family members and the biological characteristics of the body, the standards and standards of norm and beauty that have developed in this society. These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
Anorexia nervosa (lat. anorexia neurosa) (from other Greek ἀν- - “without-”, “non-” and ὄρεξις - “urge to eat, appetite”) - eating disorder , characterized by deliberate weight loss, caused and / or supported by the patient, in order to lose weight or to prevent weight gain. In anorexia, there is a pathological desire to lose weight, accompanied by a strong fear of obesity. The patient has a distorted perception of their physical form and there is a concern about weight gain, even if this is not actually observed.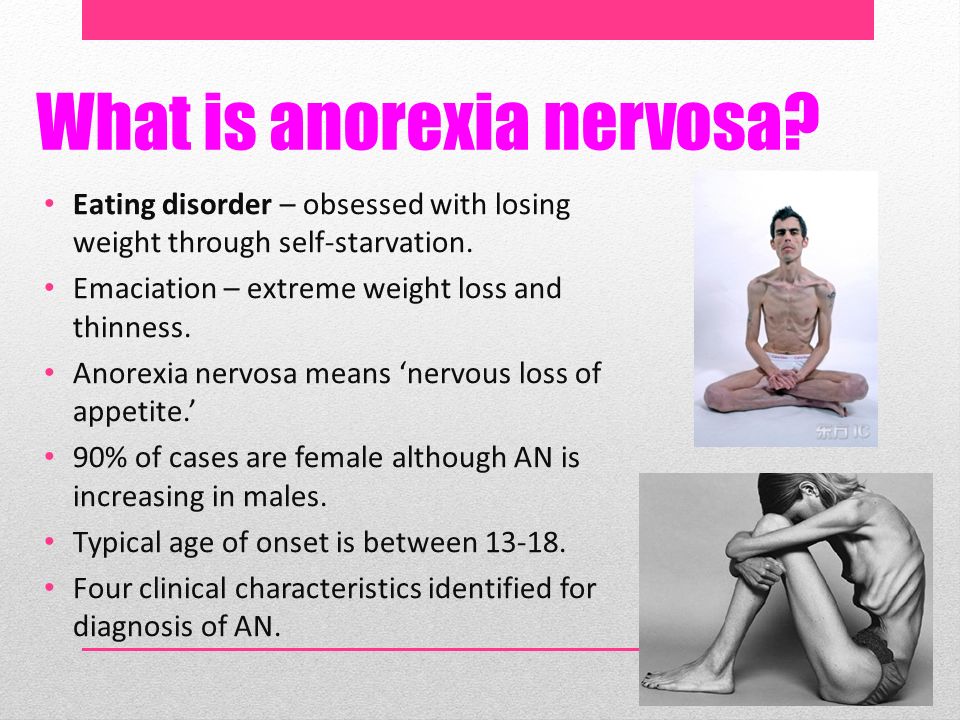 The overall prevalence of anorexia nervosa is 1.2% among women and 0.29% among men. About 90% of patients with anorexia are girls aged 12-24 years. The remaining 10% includes men and women of more mature age up to menopause.
The overall prevalence of anorexia nervosa is 1.2% among women and 0.29% among men. About 90% of patients with anorexia are girls aged 12-24 years. The remaining 10% includes men and women of more mature age up to menopause.
The causes of anorexia and bulimia are divided into biological, psychological (family influence and internal conflicts), and social (environmental influence: expectations, standards and standards of beauty, social stereotypes, diets). Biological factors - overweight and early onset of the first menstruation. In addition, the cause of the disease may lie in the dysfunction of neurotransmitters regulating eating behavior, such as serotonin, dopamine, norepinephrine. Family factors - More likely to develop an eating disorder in those who have relatives or loved ones suffering from anorexia nervosa, bulimia nervosa or obesity. Having a family member or relative with depression, alcohol or drug abuse or addiction, also increases the risk of an eating disorder. Personality factors - Psychological risk factors include perfectionism and obsessive personality, especially for the restrictive type of anorexia nervosa. Low self-esteem and frustration tolerance, feelings of inferiority, insecurity and inadequacy are risk factors. Cultural factors - these include: living in an industrialized country and an emphasis on harmony (thinness) as an important and significant sign of female beauty. Stressful events, such as the death of a close relative or friend, or sexual or physical abuse, can also be risk factors for developing an eating disorder. The self-esteem of an anorexic patient depends on the figure and weight, and the weight is not assessed objectively, the perception of the norm is reduced inadequately. Losing weight is regarded as an achievement, weight gain is regarded as insufficient self-control. Such views persist even in the last stage (“my height is 170, weight 39kilogram, I want to weigh 30”).
Personality factors - Psychological risk factors include perfectionism and obsessive personality, especially for the restrictive type of anorexia nervosa. Low self-esteem and frustration tolerance, feelings of inferiority, insecurity and inadequacy are risk factors. Cultural factors - these include: living in an industrialized country and an emphasis on harmony (thinness) as an important and significant sign of female beauty. Stressful events, such as the death of a close relative or friend, or sexual or physical abuse, can also be risk factors for developing an eating disorder. The self-esteem of an anorexic patient depends on the figure and weight, and the weight is not assessed objectively, the perception of the norm is reduced inadequately. Losing weight is regarded as an achievement, weight gain is regarded as insufficient self-control. Such views persist even in the last stage (“my height is 170, weight 39kilogram, I want to weigh 30”).
Stages of anorexia
- Dysmorphomanic — thoughts about one's own inferiority and inferiority predominate, due to imaginary fullness.
 Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet.
Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet. - Anorectic - occurs against the background of persistent starvation. A weight loss of 20-30% is achieved, which is accompanied by euphoria and a tightening of the diet, "to lose even more weight." At the same time, the patient actively convinces himself and those around him that he has no appetite and exhausts himself with great physical exertion. Due to a distorted perception of his body, the patient underestimates the degree of weight loss. The volume of fluid circulating in the body decreases, which causes hypotension and bradycardia. This condition can be accompanied by chilliness, dry skin, and even alopecia (baldness). Another clinical sign is the cessation of the menstrual cycle in women and a decrease in libido and spermatogenesis in men. Adrenal function is also impaired, up to adrenal insufficiency.
 Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body.
Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body. - Cachectic — period of irreversible dystrophy of internal organs. Comes in 1.5-2 years. During this period, weight loss reaches 50 percent or more of its mass. In this case, protein-free edema occurs, the water-electrolyte balance is disturbed, and the level of potassium in the body sharply decreases. This step is usually irreversible. Dystrophic changes lead to irreversible inhibition of the functions of all systems and organs and death.
Bulimia Nervosa (from other Greek βοῦς, bus - "bull" and other Greek λῑμός, limos - "hunger") (literally bullish hunger, kinorexia) - an eating disorder characterized by a sharp increase in appetite (wolfish appetite), usually coming in the form of an attack and accompanied by a feeling of excruciating hunger, general weakness, sometimes pain in the epigastric region. This violation of eating behavior is manifested mainly by recurring bouts of gluttony, food "spree". To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day.
To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day. Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
The treatment of anorexia and bulimia requires the combined efforts of doctors from different specialties. Integral components of treatment are alimentary rehabilitation and measures aimed at restoring body weight. Nutritional rehabilitation programs typically use emotional care and support, as well as a variety of behavioral psychotherapy techniques that involve a combination of reinforcing stimuli that integrates exercise, a strict exercise regimen and rest, in addition, prioritizing target body weight, desirable behaviors and informative feedback.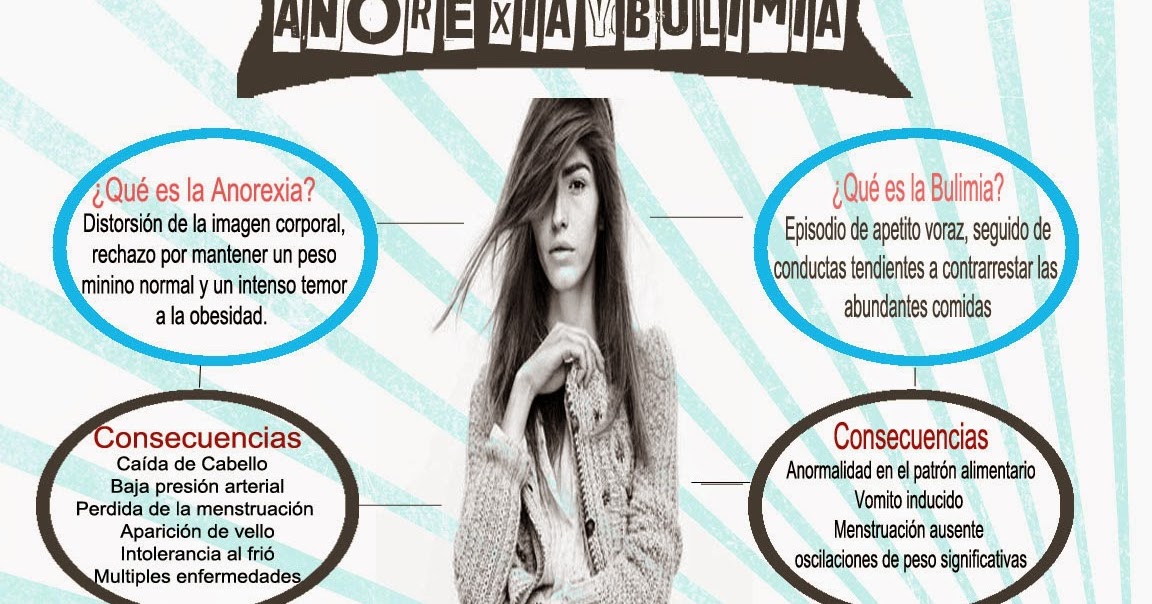 The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures .
The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures . .. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach.
.. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach. Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior.
Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior. Another element of cognitive therapy is focused problem solving . In this procedure, the patient identifies a specific problem, develops different solutions, considers the likely effectiveness and feasibility of each solution to the problem, chooses the best one, determines the steps to implement this solution, implements it, and then evaluates the entire process of solving the problem based on the result. Another essential element of cognitive therapy is monitoring: the patient should make daily records of food intake, including the type of food eaten, the time of the meal, and a description of the environment in which the meal was taken. Family therapy is especially effective in children and those under 18 years of age. It is aimed at correcting disturbed relationships in the family, leading to the development of an eating disorder in a child.
Another element of cognitive therapy is focused problem solving . In this procedure, the patient identifies a specific problem, develops different solutions, considers the likely effectiveness and feasibility of each solution to the problem, chooses the best one, determines the steps to implement this solution, implements it, and then evaluates the entire process of solving the problem based on the result. Another essential element of cognitive therapy is monitoring: the patient should make daily records of food intake, including the type of food eaten, the time of the meal, and a description of the environment in which the meal was taken. Family therapy is especially effective in children and those under 18 years of age. It is aimed at correcting disturbed relationships in the family, leading to the development of an eating disorder in a child.
ANOREXIA AND BULIMIA IS DANGEROUS!
ANOREXIA OR "DEATH BEAUTY"
To have a slender and beautiful figure is the dream of any representative of the beautiful half of humanity.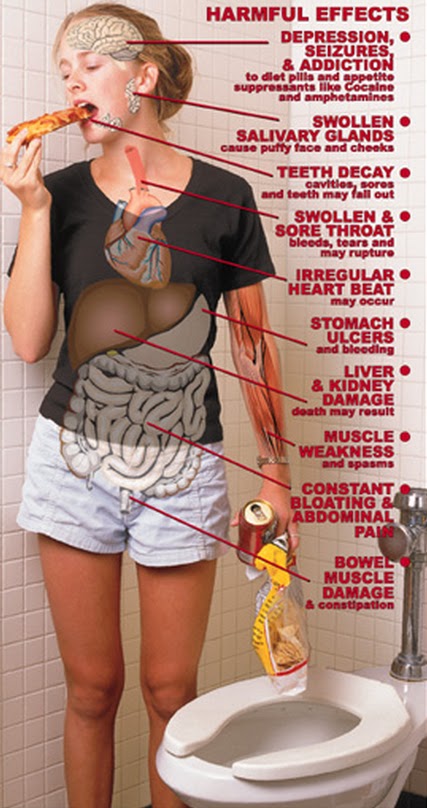 But sometimes the desire to lose weight goes so far that it can lead to anorexia.
But sometimes the desire to lose weight goes so far that it can lead to anorexia.
Anorexia is a psychological (according to other estimates - mental) disease (delusional state) in the form of fear of gaining weight. According to statistics, this "weight phobia" most often affects girls aged 13-35 years. The disease begins with an inadequate assessment of your figure. Even with protruding ribs and a blatant lack of weight, the "fat cow" does not fit into modern beauty formulas. At the first stage, anorexia is hardly noticeable. The weight deficit increases gradually, and if you see a person every day, then it is not so easy to notice, but you can. Girls suffering from anorexia begin to behave very strangely at the table. They talk a lot, gesticulate too actively, ask a lot of questions, often jump from one topic of conversation to another. In the process of a table conversation, food on a plate is almost always ground to the state of gruel. Sometimes they eat standing up. As a result of these manipulations with one’s own body, a noticeable “to the naked eye”, a mass deficit that is growing day by day, appears. Sometimes weight loss reaches 30% of the original. Heavy artillery enters the war with extra pounds in the form of diuretics, laxatives and immoderate physical exertion.
Sometimes weight loss reaches 30% of the original. Heavy artillery enters the war with extra pounds in the form of diuretics, laxatives and immoderate physical exertion.
In addition, anorexia is the most severe mental disorder, when the inner self-perception does not match the outward appearance. It is often accompanied by depression, and approximately 15-20% of patients attempt suicide. In 2015, about 10 people applied for anorexia at the Volgograd Center for Mental Health of Children and Adolescents. In 50% of cases, after recovery, former patients suffer from the consequences of the disease and cannot fully restore their health.
The most important causes of anorexia are biological, psychological, and social and cultural factors. Hereditary predisposition does not necessarily lead to the development of the disease. But if a teenage girl suffers from anorexia, the risk of developing this disease in her sisters is several times higher than in other peers. Doctors say that eating disorders usually affect both mother and daughter.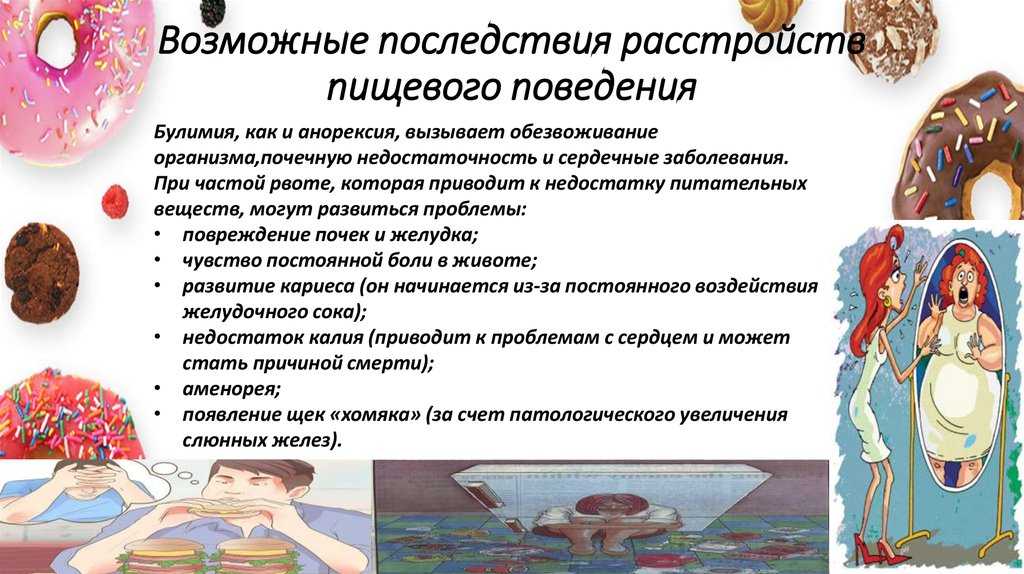
There are biologically active chemicals in the brain - neurotransmitters. They act as intermediaries in the transmission of impulses between brain cells. With anorexia, there is a decrease in the level of some of them, in particular, the hormone of happiness and pleasure - serotonin and the hormone of "genius" - norepinephrine. Their quantity in the body determines the speed and quality of information transmission within the central nervous system. That is why anorexics are unfortunate people who are in prolonged depression and are prone to suicide.
Cultural stereotypes of modern society actually impose strict criteria for appearance. According to them, a modern person who wants to be successful must be slim, fit, dressed in branded clothes. "It is very difficult for an overweight girl to successfully marry. Successful men will always prefer a slim girl to a plump one" - the slogan of today's gloss. We must not forget that almost all fashion designers - men, prefer communication within their gender and try to bring others to their "tastes", strict requirements for appearance deprive models of female attractiveness. At employment, they are met not by clothes, but by its size - S, XS. They evaluate the appearance and degree of development of the muscles, and not the intellectual potential of the applicant. "No one will be friends with you because you are fat" - the child is inspired. This social and psychological pressure can crush any kind of reinforced concrete psyche. And rarely is it mentioned that excess weight does not threaten a person with healthy eating habits. A characteristic feature of patients suffering from anorexia is the desire for excellence in everything (perfectionism). Anorexics are excellent students, smart and sensitive people. They are ambitious, they strive to be the best in everything, they strive to please everyone, to become successful in absolutely everything. They confidently go to the goal. As long as the body, exhausted by hunger, has physical strength ... But in pursuit of the ideal, it is difficult for them to live in harmony with themselves, with their bodies and stop improving themselves every minute.
At employment, they are met not by clothes, but by its size - S, XS. They evaluate the appearance and degree of development of the muscles, and not the intellectual potential of the applicant. "No one will be friends with you because you are fat" - the child is inspired. This social and psychological pressure can crush any kind of reinforced concrete psyche. And rarely is it mentioned that excess weight does not threaten a person with healthy eating habits. A characteristic feature of patients suffering from anorexia is the desire for excellence in everything (perfectionism). Anorexics are excellent students, smart and sensitive people. They are ambitious, they strive to be the best in everything, they strive to please everyone, to become successful in absolutely everything. They confidently go to the goal. As long as the body, exhausted by hunger, has physical strength ... But in pursuit of the ideal, it is difficult for them to live in harmony with themselves, with their bodies and stop improving themselves every minute. On the basis of extreme dissatisfaction with themselves, they have a very low level of self-esteem. Psychological factors also include severe stress, which can serve as a "trigger" for the onset of the disease.
On the basis of extreme dissatisfaction with themselves, they have a very low level of self-esteem. Psychological factors also include severe stress, which can serve as a "trigger" for the onset of the disease.
Anorexics stubbornly hide their condition from others. They usually explain excessive weight loss by lack of appetite, pain in the stomach and intestines, and other fictitious reasons. If there is a loved one near you who is losing weight, take a closer look at him. Perhaps excessive thinness is caused by a deliberate violation of eating behavior. Therefore, you should be aware of several main symptoms of anorexia that will help recognize the disease:
- a stable decrease in body weight by 15% or more from the minimum allowable level or a body mass index of 17.5 and below;
- a symptom of a mirror: close attention to the face and figure in the mirror with the aim of once again assessing how much he has lost weight or gained weight;
- photo symptom: refusal to be photographed even for documents due to "excessive fullness";
- the desire to eat separately, and not at a common table, not to advertise what and how much he eats;
- the desire to independently cook delicious food, feeding relatives with a sharp self-restraint in nutrition, a passion for cooking unusual dishes;
- regular weighing, strict calorie counting, exhausting, absurd workouts in terms of duration and load;
- constant use of laxatives, artificial induction of vomiting, frequent use of enemas;
- changes in character, which are manifested by previously unusual irritability and irascibility, reaching the point of absurdity, if there is compulsion to a normal meal or a ban on artificially inducing vomiting.
Bulimia is a psychopathological condition in which a person feels intense hunger, which is not able to satisfy even a huge amount of food. A bulimic differs from an anorexic in that he always wants to eat very much, satisfies this need in excess, absorbing in huge quantities everything that catches his eye. The amount eaten causes feelings of guilt and fear of gaining weight. In order to somehow compensate for the condition, patients try to quickly get rid of the absorbed food. At the onset of the disease with normal weight, a sharp change in the usual diet, "looping" on the calculation of calories consumed, a change in tastes and food preferences attract attention. The myth of switching to a healthy diet or avoiding sweets is spreading. Bulimics are embarrassed to eat in public, eat alone and carefully hide their disorder. For example, at a party, they eat in moderation, no different from the rest. After the end of the meal, everything eaten is removed from the stomach with the help of artificially induced vomiting.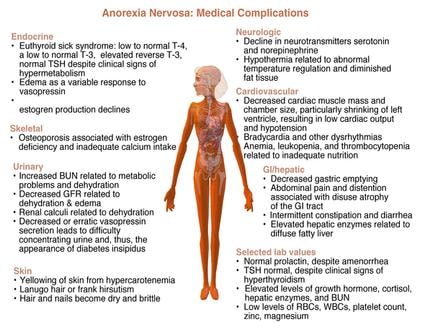 Due to frequent attempts to cleanse your body, scratches from the teeth appear on the knuckles of the hands, the phalanx of the index finger is deformed, and the nails are damaged due to contact with gastric juice. This is the main proof that an eating disorder has already formed. Patients with bulimia, as well as anorexics, closely monitor their weight and figure, daily measure weight, waist and hips. The desire to have a beautiful, slender body is where it all starts. For self-assessment, weight indicators occupy almost the first place and determine the attitude towards oneself. Looking too critically at yourself in the mirror, comparing yourself to actresses, models, or slimmer peers becomes an obsession. But in bulimics, weight fluctuations rather than weight loss are noted as a direct consequence of complex eating disorders, strict diets, breakdowns and hunger strikes. Weight changes can be significant in one direction or another with a range of up to ten kilograms per month. They occur because: "terribly" beautiful: with dull split ends; with thin dry skin, of a yellowish tint, on which bruises form from even the lightest touch; with brittle, exfoliating nails.
Due to frequent attempts to cleanse your body, scratches from the teeth appear on the knuckles of the hands, the phalanx of the index finger is deformed, and the nails are damaged due to contact with gastric juice. This is the main proof that an eating disorder has already formed. Patients with bulimia, as well as anorexics, closely monitor their weight and figure, daily measure weight, waist and hips. The desire to have a beautiful, slender body is where it all starts. For self-assessment, weight indicators occupy almost the first place and determine the attitude towards oneself. Looking too critically at yourself in the mirror, comparing yourself to actresses, models, or slimmer peers becomes an obsession. But in bulimics, weight fluctuations rather than weight loss are noted as a direct consequence of complex eating disorders, strict diets, breakdowns and hunger strikes. Weight changes can be significant in one direction or another with a range of up to ten kilograms per month. They occur because: "terribly" beautiful: with dull split ends; with thin dry skin, of a yellowish tint, on which bruises form from even the lightest touch; with brittle, exfoliating nails. The glands in the face and neck swell, as in mumps;
The glands in the face and neck swell, as in mumps;
- from the side of the internal organs, there is a weakening of the heart muscle, a violation of the heart rhythm, a persistent decrease in blood pressure. The tragic outcome of cardiac changes is acute heart failure.
- violation of salt metabolism in the body increases the risk of dystrophic changes in the kidneys, promotes stone formation up to the development of renal failure. Disturbed bone structure leads to frequent fractures;
- there are serious hormonal disorders: menstruation stops in women, impotence occurs in men. At a young age, the symptoms of menopause develop, which accelerates the premature aging of the whole organism. Hormonal failure greatly affects the emotional sphere, irritability, tearfulness, nervousness appear, young girls behave like "old hysterics". And it turns out that those suffering from anorexia and bulimia are girls according to their passport, and grandmothers due to their health and nervous system;
- frequent vomiting irritates the pharynx and esophagus, leads to the formation of ulcers in the oral cavity, esophagus, and uncontrolled use of various laxatives can cause diarrhea or constipation, ulcerative lesions of the lower parts of the gastrointestinal tract. Due to the constant exposure to gastric contents and lack of calcium, the teeth become weak: the enamel is damaged, caries often occurs. Inevitably, the balance of electrolytes is disturbed, dehydration may develop.
Due to the constant exposure to gastric contents and lack of calcium, the teeth become weak: the enamel is damaged, caries often occurs. Inevitably, the balance of electrolytes is disturbed, dehydration may develop.
We invite you to answer a few questions to determine if you are prone to eating disorders.
1. Do you agree with people who say that you are thin?
2. Does the possibility of gaining extra pounds scare you?
3. Do you lie about the food you eat?
4. Do your loved ones know your taste preferences?
5. Do your family and friends worry about your weight, appearance, or eating habits?
6. When overeating, do you use any special drugs that cause diarrhea, vomiting?
7. Do you enjoy being hungry, exercising a lot, or doing laxative cleansing?
8. How much do you look and how much do you weigh?
If you answered yes to three or more questions, it's time for you to sound the alarm!
And in conclusion, I would like to note that a balanced meal is only a source of energy for a person to live and work fruitfully.