How long does it take for antidepressants to kick in
Why Do SSRIs (Antidepressants) Take So Long To Work?
It can be challenging to find an antidepressant that works for you. Learn more about your treatment options for depression, including esketamine for faster relief.
Antidepressants are one of the most commonly prescribed medications in the United States, as more than 1 in 5American adults will experience depression in their lifetimes. Antidepressants can start working within one to two weeks, but for many individuals, relief may not come soon enough. With no end to their suffering in sight, far too many people resort to taking their own lives.
Suicide remains one of the leading causes of death in the nation. Among American teens and young adults, suicide rates are now among the highest on record. Such startling statistics beg the questions: Why does it take so long for antidepressants to work? And what treatment options are available for faster relief?
Feelings of depression or anxiety can lead to suicidal thinking. If you or a loved one is experiencing suicidal thoughts or tendencies, call the National Suicide Prevention Hotline at 1-800-273-8255.
Time Until Initial Improvement
Initial improvement of depressive symptoms can occur in one to two weeks of starting an antidepressant. However, many people who take antidepressants do not notice a significant improvement in their symptoms with the first drug they try. Moreover, many individuals who do not improve with their first trial of antidepressants fail to respond to subsequent trials. These statistics are concerning because the poor response to antidepressants is predictive of higher rates of chronic depression and poorer overall health.
Timeline for Full Benefits
Generally, most people achieve maximum relief of depressive symptoms within two to three months of antidepressant use. If an individual does not show improvement within four to six weeks of starting an antidepressant, further steps are usually taken. Such steps may include increasing drug dosage, or switching to or adding another antidepressant. Additional steps may include adding other kinds of psychiatric medications, psychotherapy or somatic treatments to care.
Such steps may include increasing drug dosage, or switching to or adding another antidepressant. Additional steps may include adding other kinds of psychiatric medications, psychotherapy or somatic treatments to care.
Variables in Antidepressant Response Time
Some individuals respond more quickly to antidepressants than others, leaving many people wondering, “Why does it take so long for antidepressants to work?” Still, many people do not respond to antidepressants at all. What determines who will and who won’t respond to an antidepressant? To understand the answers to these questions, some basic understanding of how antidepressants work is needed.
The most commonly prescribed antidepressants are known as SSRIs, or selective serotonin reuptake inhibitors. SSRIs work by elevating the amount of serotonin in the brain. Serotonin is the contentment neurotransmitter, a chemical messenger in the brain that activates brain signaling associated with experiencing pleasure and feelings of well-being. The caveat is that for serotonin to be available for brain signaling, it must be on the outside of the brain’s cells, known as neurons. SSRIs work to inhibit the transporter that recycles serotonin by preventing the transport of serotonin back into the neurons from which it was released.
The caveat is that for serotonin to be available for brain signaling, it must be on the outside of the brain’s cells, known as neurons. SSRIs work to inhibit the transporter that recycles serotonin by preventing the transport of serotonin back into the neurons from which it was released.
Antidepressants take so long to work because they inactivate not just individual serotonin transporters, but also the genes in our DNA that code for the transporter. The result over time is fewer serotonin transporters in the brain and more serotonin around to experience pleasant stimuli. SSRIs work better for some people than others because of individual variations in gene expression of the serotonin transporter. However, we do not yet have enough evidence to support the use of individual genetic testing to treat depression on a case-by-case basis. Additional variables that affect antidepressant response time include those related to drug metabolism: genetic differences in liver enzyme function, liver disease, age, sex, hormones, pregnancy, and nutritional status.
Length of Antidepressant Treatment
Antidepressants are prescribed not just to achieve maximum short-term relief of depressive symptoms, but also as a maintenance treatment to prevent future depressive episodes. Without treatment, a typical major depressive episode will last for approximately six months, has a 50% chance of recurring in six months and an 85% chance of recurring within a decade. For these reasons, antidepressant treatment is typically continued for at least six to twelve months after the resolution of depressive symptoms. In more severe cases, antidepressant treatment may be continued for up to three years, or indefinitely.
Options for Improving the Effectiveness of Antidepressants
There are several treatment options to improve the effectiveness of antidepressants once an antidepressant has been tried for four to six weeks, including:
- Increasing dosage: Antidepressants are started at low doses and then slowly increased.
 The dose is titrated up until relief of depressive symptoms is optimized and side effects of the drug are minimized.
The dose is titrated up until relief of depressive symptoms is optimized and side effects of the drug are minimized. - Combining medication: When full relief of depressive symptoms is not achieved at the maximum dose of one antidepressant, another antidepressant or an atypical antipsychotic may be added for additional benefit.
- Changing medication: Individuals may switch from one antidepressant to another when they receive no benefit from the first antidepressant or cannot tolerate its side effects. The first antidepressant must be tapered down before it can be completely discontinued.
- Beginning concurrent psychotherapy: It is recommended that treatment with antidepressants be paired with psychotherapy for maximum benefit.
- Engage in somatic treatments: Electrical stimulation of the brain is a common and effective treatment for depression. Common somatic treatments include electroconvulsive therapy (ECT) and repetitive transcranial magnetic stimulation (rTMS).
 These treatments work by stimulating neurons in the brain that are responsible for mood and reality processing.
These treatments work by stimulating neurons in the brain that are responsible for mood and reality processing.
Esketamine for Faster Relief
Finally, for individuals with severe depression who have thoughts of suicide or are exhibiting life-threatening behavior, esketamine is recommended for faster relief. Esketamine, like ECT and rTMS, has a rapid onset of antidepressant action. Unique to esketamine, however, is its ability to significantly improve even the most severe of depressive symptoms within just a few hours or a day.
How does esketamine work so quickly? Esketamine acts on a stimulating neurotransmitter known as glutamate. Glutamate accounts for a significant majority of the brain’s neurotransmitters and may be largely responsible for most brain functions, including mood.
When to Talk to Your Doctor
If you are struggling with depression, visit your primary care provider, or establish care with one you trust. Working with an empathetic, compassionate and collaborative healthcare provider is an important first step in treating depression. The best care teams include a primary care provider, a case manager and a mental health specialist such as a psychiatrist. This kind of care has been shown to deliver the best treatment outcomes for people suffering from depression.
The best care teams include a primary care provider, a case manager and a mental health specialist such as a psychiatrist. This kind of care has been shown to deliver the best treatment outcomes for people suffering from depression.
If you or a loved one struggle with depression and co-occurring addiction, The Recovery Village can help. You can receive comprehensive treatment for both conditions simultaneously from one of several facilities located throughout the nation. To learn more about depression and addiction treatment programs, call The Recovery Village to speak with a representative today.
Editor – Megan Hull
Megan Hull is a content specialist who edits, writes and ideates content to help people find recovery. Read more
Baudry, A; Mouillet-Richard, S. “miR-16 targets the serotonin transpor[…]s to antidepressants.” PubMed Central, September 17, 2010. Accessed June 14, 2019.
Centers for Disease Control and Prevention. “Leading Causes of Death. ” March 17, 2017. Accessed June 14, 2019.
” March 17, 2017. Accessed June 14, 2019.
Centers for Disease Control and Prevention. “Suicide Rates in the United States Continue to Increase.” June 14, 2018. Accessed June 14, 2019.
Chen, Jennifer. “How New Ketamine Drug Helps with Depression.” Yale Medicine, March 21, 2019. Accessed June 14, 2019.
Fuentes, Andrea; Pineda, Moises. “Comprehension of Top 200 Prescribed Drug[…]raining and Practice.” PubMed Central, June 2018. Accessed June 14, 2019.
Geddes, JR; Carney, SM. “Relapse prevention with antidepressant d[…] a systematic review.” PubMed Central, February 2003. Accessed June 14, 2019.
Gelenberg, Alan, et al. “Practice Guideline for the Treatment of […] Depressive Disorder.” American Psychiatric Association, November 2010. Accessed June 14, 2019.
Gibson, G. Gordan; Skett, Paul. “Factors affecting drug metabolism: internal factors.” Springer, 1986. Accessed June 14, 2019.
Greden, JF, et al. “Impact of pharmacogenomics on clinical o[…]ed, controlled study. ” PubMed Central, April 2019. Accessed June 14, 2019.
” PubMed Central, April 2019. Accessed June 14, 2019.
Hasin, Deborah, et al. “Epidemiology of Adult DSM-5 Major Depres[…]in the United States.” JAMA Network, April 2018. Accessed June 14, 2019.
Machado-Vieira, Rodrigo, et al. “The Timing of Antidepressant Effects: A […]d Somatic Treatments.” PubMed Central, January 6, 2010. Accessed June 14, 2019.
McIntyre, RS. “When should you move beyond first-line t[…]rapy for depression?” PubMed Central, 2010. Accessed June 14, 2019.
Papakostas, GI, et al. “A meta-analysis of early sustained respo[…] depressive disorder.” PubMed Central, February 2006. Accessed June 14, 2019.
Quitkin, FM, et al. “When should a trial of fluoxetine for ma[…]n be declared failed?” PubMed Central, April 2003. Accessed June 14, 2019.
Serretti, A, et al. “Meta-analysis of serotonin transporter g[…]n depressed patients.” PubMed Central, March 2007. Accessed June 14, 2019.
Sim, Kang, et al. “Prevention of Relapse and Recurrence in […]of Controlled Trials. ” PubMed Central, February 2016. Accessed June 14, 2019.
” PubMed Central, February 2016. Accessed June 14, 2019.
Simon, Gregory. “Unipolar major depression in adults: Cho[…]ng initial treatment.” UpToDate, November 12, 2017. Accessed June 14, 2019.
Thase, Michael; Connolly, Ryan. “Unipolar depression in adults: Choosing […]resistant depression.” UpToDate, May 10, 2019. Accessed June 14, 2019.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
How Long Does it Take for Depression Medication to Work?
It is estimated that 1 in 5 Americans will experience a major depressive episode at some point in their life. Roughly 1 in 10 adults in the United States has had moderate to severe depression symptoms within the past year. For individuals who are living with depression, antidepressant medications can give substantial relief from depressive symptoms.
Roughly 1 in 10 adults in the United States has had moderate to severe depression symptoms within the past year. For individuals who are living with depression, antidepressant medications can give substantial relief from depressive symptoms.
Treating depression symptoms is critical for mental health and preventing suicide, which is one of the leading causes of death in the United States. But medications used to treat depression don’t work right away. It can take several weeks for a person to start to feel better on antidepressants. This frequently causes people struggling with depression to become discouraged during treatment.
Please continue reading to learn how long it takes pharmaceutical therapy to relieve depression. Also, find out why it takes antidepressants so long to work and what other treatment options can offer faster relief.
How long do antidepressants take to work?
Most patients get some improvement in their symptoms of depression about 1 to 2 weeks after starting antidepressant medicine. However, the first drug that is tried often does not lead to significant improvement in depression symptoms. Therefore, it can take a bit of trial and error to identify the antidepressant medicine that works for you.
However, the first drug that is tried often does not lead to significant improvement in depression symptoms. Therefore, it can take a bit of trial and error to identify the antidepressant medicine that works for you.
How long after taking antidepressants will I feel better?
Generally speaking, you should start to feel better within 4 to 6 weeks and obtain maximum benefit 2 to 3 months after starting antidepressant use. With that said, a person’s response to a specific medicine cannot be predicted. Suppose you do not show any improvement in symptoms of depression after 6 weeks. In that case, your psychiatrist or doctor may change the dose of the drug, switch you to another antidepressant, or add other treatments such as therapy.
Why does it take so long for antidepressant medications to work?
Everyone is different. Some people may experience quick relief of symptoms, while others can take considerably longer to benefit from a drug. Many people do not respond to antidepressants at all. To understand why we need to have some background in how brain chemistry works.
To understand why we need to have some background in how brain chemistry works.
The most commonly prescribed antidepressants are selective serotonin reuptake inhibitors or SSRIs (examples include Prozac, Zoloft, Celexa, Lexapro, Paxil). These medications work by increasing the amount of serotonin available in the brain. Serotonin is a neurotransmitter that is a mood elevator. SSRIs prevent the reuptake or transport of serotonin back into the neurons. These medicines take so long to work because they inactivate not only the individual serotonin transporters in brain cells but also the genes that code for making the transporters. In this way, over time, SSRIs lead to fewer serotonin transporters in the brain, thus making more serotonin available.
Different people respond differently to antidepressants because each person’s gene expression of the serotonin transporter varies. The response to antidepressants is also affected by other factors such as an individual’s metabolism rate, liver function, age, sex, and nutritional status.
Can antidepressants work immediately?
Antidepressants will not work immediately. Most patients start to feel better about 6 weeks after starting treatment with antidepressants. It takes this much time for the drug to build up in the body. Your psychiatrist or doctor may increase the dose during this time, depending on your response. It’s important to understand this before starting antidepressants so that you don’t feel discouraged.
If you need faster relief of symptoms, especially if you have anxiety and depression, your doctor may prescribe short-term treatment with medications such as benzodiazepines (examples include Valium, Ativan, Klonopin). These medicines can provide relief much faster than SSRIs or other antidepressants. However, caution is advised because benzodiazepines can be habit-forming (there is a risk of addiction). You should talk to your doctor about safer alternatives for faster relief of depressive symptoms, such as propranolol (Inderal) or hydroxyzine (Vistaril).
What works faster - tricyclic antidepressants TCAs or selective serotonin reuptake inhibitors SSRIs?
There are several different classes of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), serotonin-norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), and others. Some of these antidepressants work by affecting serotonin, while others affect serotonin and norepinephrine levels in the brain. Different types of antidepressants can take different amounts of time to work.
Some of the most commonly prescribed antidepressants include SSRIs (Prozac, Zoloft) and SNRIs (Effexor, Cymbalta). These types of antidepressants take about 2 weeks to begin working and produce a full effect in around 2 months. However, tricyclic antidepressants are less selective than the other two classes of drugs, i.e., they affect more body systems and cause more side effects.
What if I don’t improve on an antidepressant?
As noted above, antidepressants don’t work right away. In someone with mild depression, the effects of the medication may be felt faster. More severe depression can take longer to respond. It could be that you don’t improve even after you take an antidepressant for a few weeks. Don’t let this dishearten you. And don’t stop taking your medicine without consulting your doctor. Just because one medicine didn’t work doesn’t mean your depression is not treatable. It requires patience. Some people may need to change to another medicine because of intolerable side effects from a specific drug. You will need to work with your doctor to figure out what medicine effectively relieves your symptoms without causing side effects.
If you have not experienced relief of depressive symptoms with a particular medicine, your doctor may increase the dose of your medicine, combine it with another medicine, change you to another antidepressant, or recommend starting concurrent psychotherapy or other treatments for depression.
How long does it take to treat depression with medication?
Antidepressants are not designed to provide only short-term relief from depression symptoms. They also prevent future episodes of depression. An untreated episode of major depression can last for around 6 months and has a high chance of recurrence. For this reason, treatment with antidepressants is usually continued for 6 to 12 months, even after obtaining symptom relief. Depending on the severity of your symptoms, your doctor may continue treatment for 3 years or longer.
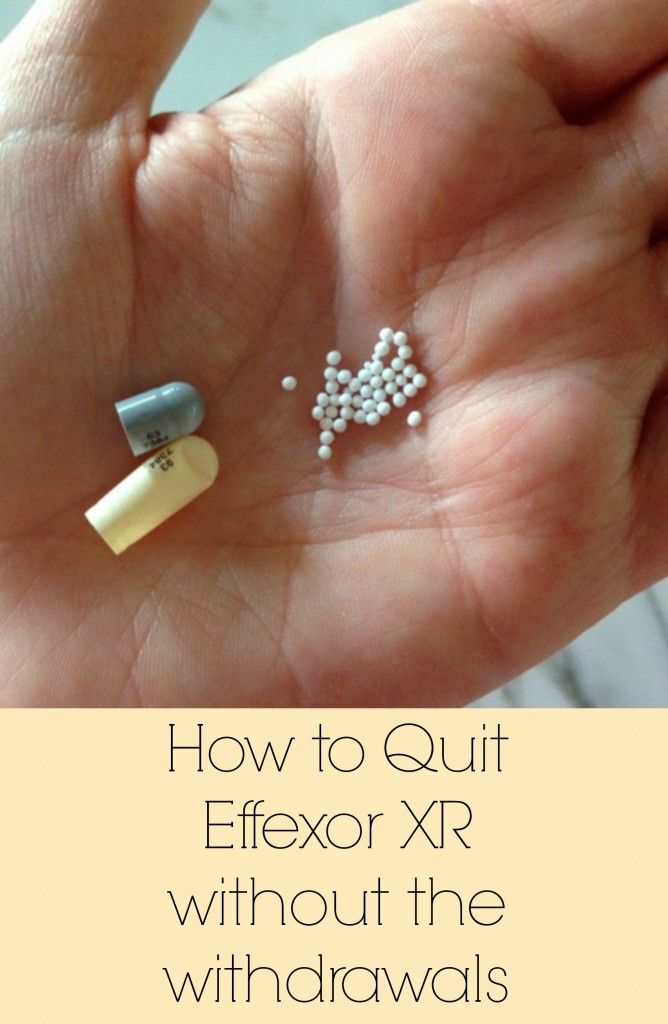
It is important not to stop treatment as soon as you start feeling better. There is a high chance that your depressive symptoms will return if you discontinue your medication before your doctor says so. To obtain maximum benefits for your mental health, you should take the medication as prescribed. Discuss coming off the medication with your doctor when you feel ready. Your doctor will gradually reduce the dose of your antidepressant medication. This is to prevent unpleasant withdrawal symptoms that can occur if you stop taking the medication suddenly.
This is to prevent unpleasant withdrawal symptoms that can occur if you stop taking the medication suddenly.
Talk to your doctor about depression treatment
If you have depression symptoms, it is important to be medically reviewed and treated. Taking an antidepressant could be critical for your mental health. You should follow your doctor’s advice, diagnosis, or treatment for depression. As noted, it may take 4-6 weeks for antidepressants to start working. Complete benefit can take 2-3 months. If you don’t get relief with the first drug you try, you may find that switching to another type of antidepressant does the trick.
Keep in mind also that antidepressant medications work best when used in combination with psychotherapy. With a multi-pronged treatment plan in place, your depressive symptoms have a very good chance of improving.
References:
1. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2671413
2. https://www.cdc. gov/nchs/fastats/leading-causes-of-death.htm
gov/nchs/fastats/leading-causes-of-death.htm
A Brief History of Antidepressants
The average person knows about psychiatry only that in every city there are wonderful parks at mental hospitals, and also that there used to be punitive psychiatry. In fact, psychiatry is a deep science with a rich history. The article talks about drugs that can save our mental health, as well as today's views on what human mental health is and why we can improve it with the help of pharmacological drugs. nine0003
Part one, in which we look with amazed children's eyes and do not understand anything at all
There have always been many questions about antidepressants. Unlike "ordinary" medicines, they cannot be understood with the mind, you just need to believe. For example, all antidepressants begin to work only by the second week of taking. Traditionally, guidelines explain this by saying that "during this time, the drug accumulates." But what does "accumulate" mean? After all, the drug either works immediately or does not work at all. All other psychotropic substances act almost immediately. Sleeping pills act immediately. Tranquilizers act immediately. Antipsychotics, mood stabilizers, anticonvulsants, stimulants - they all begin to act quickly. And "stubborn" antidepressants - only after two weeks. The question is why? nine0003
For an explanation of some terms from the field of psychopharmacology, see the Glossary at the end of the article. - Ed.
Figure 1 Advertisement for Thorazine (US trade name for chlorpromazine) recommends the drug for schizophrenic delusions and hallucinations.
Antidepressants improve the emotional background of patients with depression and do not affect the mood of healthy people. This not normal. If a substance has a psychoactive effect, it has the same effect on both pathological and physiological processes. If a sleeping pill is given to a person suffering from insomnia, he will fall asleep. And if you give sleeping pills to a healthy person, he will fall asleep in the same way. If an anxious and agitated patient is given a benzodiazepine tranquilizer, then the person will calm down and calm down. What if it's for an ordinary person? The same thing - a person will calm down and calm down. The "evil old" classic antipsychotics (the same chlorpromazine - "Aminazine") are still indispensable in acute psychoses: in fact, they have a carpet bombing effect on the rebellious brain, stopping mental activity through a break in dopamine transmission. nine0003
And if a healthy person is tied up and stabbed with antipsychotics, then the same thing will happen to his mental processes - the brain will turn into a scorched desert. But with antidepressants, the picture is completely different. They have an effect on a depressive mood background, but not on a normal one. A healthy person will only experience side effects, but no change in consciousness. So how does the pill know which person is depressed and which is not?
A key symptom of depression is decreased mood. This in itself is not a problem: there are a lot of substances that quickly and guaranteed to improve mood - for example, a 40% solution of ethyl alcohol or psychostimulants, and they will not work in two weeks, but from the very first dose. Why then does medicine not use them? The fact is that they absolutely do not help with depression: neither alcohol nor amphetamines have an antidepressant effect, no matter what people say. And antidepressants - such as serotonin reuptake inhibitors Prozac, Zoloft, Paxil, Cipramil - help. Why? nine0003
This in itself is not a problem: there are a lot of substances that quickly and guaranteed to improve mood - for example, a 40% solution of ethyl alcohol or psychostimulants, and they will not work in two weeks, but from the very first dose. Why then does medicine not use them? The fact is that they absolutely do not help with depression: neither alcohol nor amphetamines have an antidepressant effect, no matter what people say. And antidepressants - such as serotonin reuptake inhibitors Prozac, Zoloft, Paxil, Cipramil - help. Why? nine0003
Molecular basis of psychoses
An increase in the flow of dopamine and, to a lesser extent, serotonin is associated with the development of psychosis. According to the dopamine hypothesis of schizophrenia, the antipsychotic effect of antipsychotics is due to their ability to block dopamine receptors. However, since there are many varieties of these receptors in the brain and they perform a wide variety of functions, it is impossible to completely drown them out, as classic antipsychotics do (chlorpromazine, haloperidol, chlorprothixene and others), - there will be a lot of unpleasant side effects. Therefore, modern atypical antipsychotics selectively block some types of dopamine and serotonin receptors, and they have much fewer side effects.
Therefore, modern atypical antipsychotics selectively block some types of dopamine and serotonin receptors, and they have much fewer side effects.
Symptoms of depression
The main symptom of clinical depression (or major depressive disorder ) is a persistent decrease in emotional background, not just a "bad mood" that any person can have. Clinical depression is a disease that has clear criteria and is described by a whole bunch of symptoms. Depression manifests itself in a decrease in mood, feelings of guilt and hopelessness, loss of interest and pleasure, a decrease in energy, and as a result in increased fatigue and a decrease in activity, all of which should persist for at least two weeks. nine0003
Monoamine oxidase (MAO)
This is an enzyme involved in the destruction of monoamines (more precisely, the catabolism of monoamines by oxidative deamination). Monoamines include a mass of endogenous hormones and neurotransmitters, including all of which we are interested in: dopamine, adrenaline, norepinephrine, serotonin and histamine; as well as exogenous psychoactive substances (for example, phenylethylamine and narcotic substances derived from it).
MAO is one of the key enzymes of the human brain, and there are about forty related proteins in the family of monoamine receptors. If you block MAO, monoamines will stop being destroyed and begin to accumulate in the synaptic transmission system, which is not always good. Therefore, even modern selective MAO inhibitors - very powerful antidepressants - are quite dangerous to use and are allowed only in a hospital setting, where there is constant monitoring and control over the patient's condition. nine0003
Part two, in which we ask for advice from the spirits of our ancestors, but instead listen to boring old man's tales about the affairs of bygone days
Where did psychopharmacology come from? It dates back to 1876, when BASF invented methylene blue. This is the first substance from the group of phenothiazines, but then this was not yet suspected. Methylene blue is a very popular molecule. For example, pyoctannin - a 1-2% solution of methylene blue - is known to us as medical blue, although it has now been replaced by brilliant green, yellow iodine and colorless hydrogen peroxide. Even methylene blue was once treated for malaria, carbon monoxide poisoning, insecticides were obtained from it and used to treat worms in veterinary medicine. In 1883, phenothiazine itself was obtained from diphenylamine. Phenothiazine is the biblical Adam, from which twelve tribes of various useful substances have grown. Since the beginning of the 20th century, its derivatives have been used in veterinary medicine as an anthelmintic. Since the 30s, they began to try it as an anti-allergic agent, and in 19In 1947, promethazine was invented - one of the first antihistamines, along with Dimedrol discovered in 1943. These medicines are still used today.
Even methylene blue was once treated for malaria, carbon monoxide poisoning, insecticides were obtained from it and used to treat worms in veterinary medicine. In 1883, phenothiazine itself was obtained from diphenylamine. Phenothiazine is the biblical Adam, from which twelve tribes of various useful substances have grown. Since the beginning of the 20th century, its derivatives have been used in veterinary medicine as an anthelmintic. Since the 30s, they began to try it as an anti-allergic agent, and in 19In 1947, promethazine was invented - one of the first antihistamines, along with Dimedrol discovered in 1943. These medicines are still used today.
Promethazine had a pronounced sedative, suppressive effect, and surgeons began to use it in cocktails for anesthesia. In an attempt to enhance the inhibitory effect, in 1950 chlorpromazine was obtained, and in 1951 it fell into the hands of psychiatrists. Thus began the era of psychopharmacology: chlorpromazine is now known to us under the name of chlorpromazine. This is the very first neuroleptic, the gold standard of antipsychotic effect. Until now, the potency of all antipsychotics is measured through the "chlorpromazine equivalent", just like the potency of all tranquilizers is measured through the diazepam equivalent. nine0003
This is the very first neuroleptic, the gold standard of antipsychotic effect. Until now, the potency of all antipsychotics is measured through the "chlorpromazine equivalent", just like the potency of all tranquilizers is measured through the diazepam equivalent. nine0003
Parallel to this, in 1952, iproniazid, a drug for the treatment of tuberculosis, was invented. At that time, an open form of tuberculosis almost always meant a death sentence. Naturally, the prospect of imminent death caused some depression and sadness in patients. The situation was aggravated by the fact that the drugs did not help much, but the observation of phthisiatricians was all the more paradoxical that patients under the influence of iproniazid become inadequately happy. Iproniazid was the first ever antidepressant from the group of monoamine oxidase inhibitors; it is currently not used due to difficulties with its application in medical practice. nine0003
At the same time, in the 50s, they began to actively look for other psychotropic drugs like chlorpromazine. So, in 1955, imipramine appeared - a tricyclic benzozepine analogue of chlorpromazine. It did not have an antipsychotic effect, but it turned out by chance that imipramine has an antidepressant effect. Thus began the era of tricyclic antidepressants, which before the advent of Prozac were by far the dominant group in their class, and now find the widest use. In 1961, a derivative of imipramine was registered under the name amitriptyline - the greatest antidepressant of all times and peoples. At 19In 1955, the first bezodiazepine tranquilizer, chlordiazepoxide (Elenium), was found by random selection, and in 1963 diazepam (Valium, Sibazon, Seduxen, Relanium) was obtained from it. So, quite by chance, the "big trinity" of psychopharmacology has developed - chlorpromazine, amitriptyline and diazepam. Antipsychotic, antidepressant and tranquilizer.
So, in 1955, imipramine appeared - a tricyclic benzozepine analogue of chlorpromazine. It did not have an antipsychotic effect, but it turned out by chance that imipramine has an antidepressant effect. Thus began the era of tricyclic antidepressants, which before the advent of Prozac were by far the dominant group in their class, and now find the widest use. In 1961, a derivative of imipramine was registered under the name amitriptyline - the greatest antidepressant of all times and peoples. At 19In 1955, the first bezodiazepine tranquilizer, chlordiazepoxide (Elenium), was found by random selection, and in 1963 diazepam (Valium, Sibazon, Seduxen, Relanium) was obtained from it. So, quite by chance, the "big trinity" of psychopharmacology has developed - chlorpromazine, amitriptyline and diazepam. Antipsychotic, antidepressant and tranquilizer.
Figure 2. In One Flew Over the Cuckoo's Nest, one of the main literary works of beatnik and hippie culture, the action takes place in an American psychiatric hospital. nine0014
nine0014
As for depression, before the first psychopharmacological revolution, they were treated with drugs. Opiates were used until the late 50s, amphetamines until the mid-60s. Then amitriptyline and the company came into our world, and drugs gradually faded into the shadows due to their obvious side effects. Since the late 50s, it has become known about biogenic amines - norepinephrine, dopamine, serotonin. Since the late 1960s, there have been strong suspicions that serotonin is responsible for the development of depressive states. In the 70s, a biological theory was formed, according to which, during depression, the concentration of certain mediators in the synapse decreases in the brain. At 1977 fluoxetine was synthesized, but it passed the tests only by 1987, and went on sale in 1991 under the name "Prozac" (14 years from synthesis to the counter - compare with a year or two that took 50-60 -e). Thus, the world's first selective serotonin reuptake inhibitor appeared, which unleashed the second pharmacological revolution and made the Eli-Lilly company rich.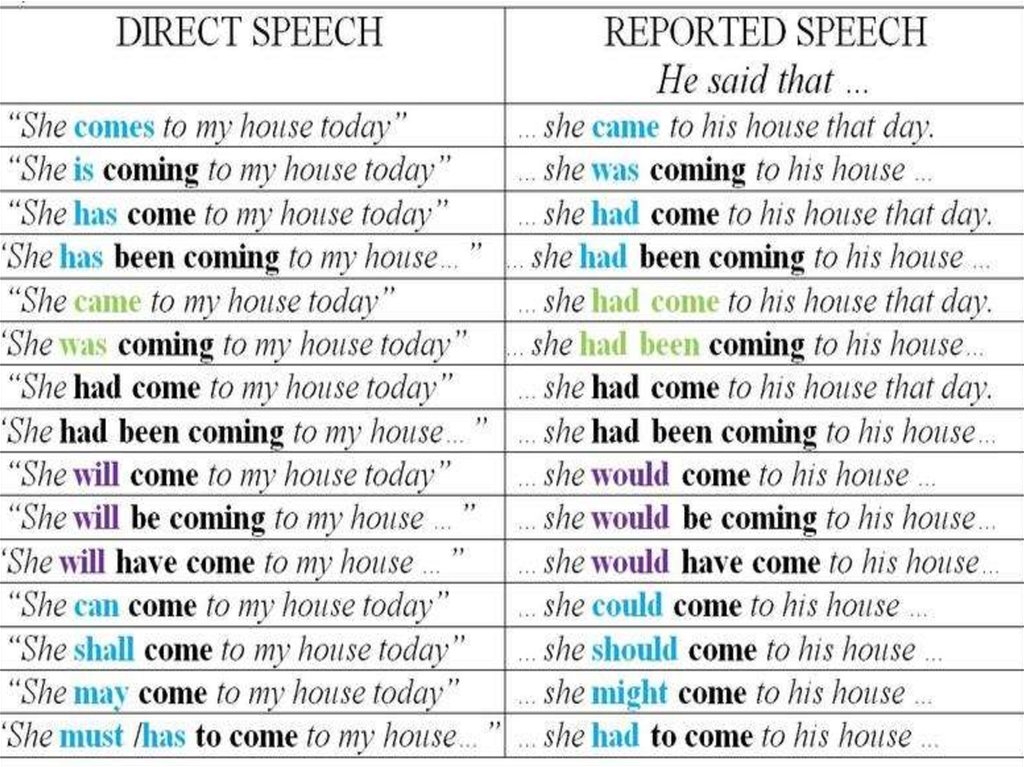 Figure 3 shows a brief history of the development of antidepressants.
Figure 3 shows a brief history of the development of antidepressants.
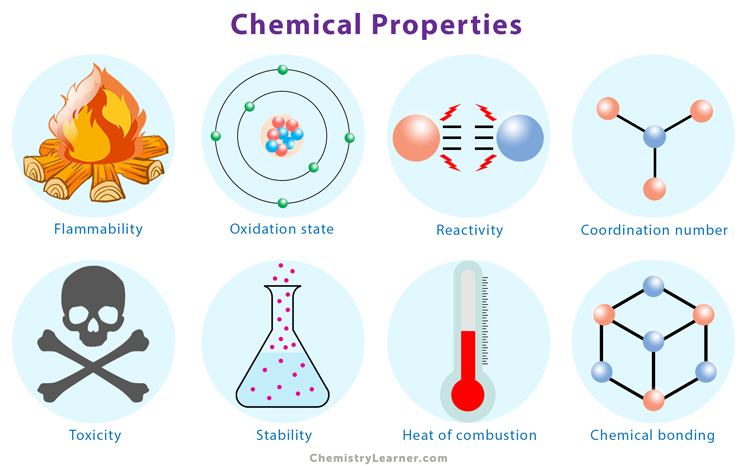
Figure 3. A brief history of the development of antidepressants. nine0014 The past decade has not brought revolutions in antidepressants. Although it is worth noting that licenses for all important drugs expired in the 2000s, and they began to be produced in generics and began to be widely used in Russian medicine. Meanwhile, a lot of things happened with the “neighbors” in the pharmacological reference book: “zero” is a revolution in atypical antipsychotics. Risperidone, Seroquel, Zyprexa - these names are not as well known to the general public as Prozac, but for the treatment of psychosis (primarily schizophrenia) this is a very big step. nine0003 Together, a number of reasons have been formulated for which depression develops. But the further facts did not fit into the theory. Many varieties of serotonin receptors - 7 types, 13 subtypes - made it difficult to explain why drugs with the same biochemical activity have a different effect on the patient's consciousness. The 5-HT receptor blocker 2A mirtazapine (rimeron) is an antidepressant, and the blocker of the same 5-HT 2A quetiapine (seroquel) is an atypical antipsychotic. But if serotonin receptor blockers are antidepressants, is it reasonable to assume that agonists will be depressants? No matter how. Many bad things can be said about serotonin receptor agonists - mescaline, psilocybin, LSD and the like - but they do not cause depression, that's for sure. nine0003 Serotonin receptors have a huge number of functions. By the mid-2000s, some mechanisms for the formation of emotions began to be clarified, and the monoamine theory began to quickly lose ground. At the same time, as can be seen from the table of biological theories of the development of depression, there is still no single view of the problem. 0009 neuroplastic theory , which has practically supplanted the theory of biogenic amines at the present time. Its main postulate is that the formation of the emotional background (and, accordingly, all its pathological deviations) is not determined by the level of individual neurotransmitters, but is formed as a result of the combined activity of various parts of the brain. The interaction of these neuronal complexes is regulated by long-term potentiation (sustained increase in synaptic transmission between neurons), synaptic plasticity (change in the strength of interneuronal transmission) and excitotoxicity (damage and death of nerve endings during overactivation of glutamate receptors). It has been proven that during prolonged depression, the gray matter of the brain (the layer where the actual nerve cells are located) becomes thinner, the connectivity and branching of nerve endings decrease. It turned out that all this functions, is regulated and maintained by special neurotrophin proteins (growth factors that ensure the development and viability of brain cells). There are many neurotrophins, but in the aspect of this article, we are mainly interested in neurotrophic growth factor (aka BDNF), which is involved in the formation of new connections between neurons; it is also effective in disorders characteristic of depressive and anxiety disorders. And its synthesis, in turn, is regulated by serotonin receptors. Therefore, serotonin-active antidepressants are effective in both depressive and anxiety states (Fig. 4). nine0003 Figure 4. Beyond the Monoamine Hypothesis , according to which the main cause of depression is a violation of serotonin or norepinephrine signaling in the brain. Serotonin (5-hydroxytryptamine, 5-HT; left half of the figure) and norepinephrine (right half of the figure), the main mediators of monoamine transmission, are secreted by presynaptic neurons. In a postsynaptic neuron, serotonin and norepinephrine each bind to their own type of G-protein coupled receptors that trigger adenylate cyclase (AC) and phospholipase C (PL-C). In support of the monoamine hypothesis, the following observations made in patients suffering from depression speak: 1) inhibition of tryptophan or tyrosine hydroxylases or exclusion of a source of tryptophan from the diet leads to a return of depression; 2) an increased frequency of mutations in the gene for the brain form of tryptophan hydroxylase; 3) an increase in the affinity of MAO-A to its substrates; 4) disruption of the "feedback" receptors 5-HT 1A and 5-HT 1B ; 5) serotonin transporter polymorphism; 6) disruption of postsynaptic GPCR receptors; and 7) decreased levels of cAMP, IF 3 , and nuclear factor COE (cAMP response element). Antidepressants in various ways increase the release of serotonin (some also norepinephrine and dopamine) into the synaptic cleft, where it acts on serotonin receptors. It is possible that, in addition to the above, depression in the nervous tissue increases the concentration of pro-inflammatory cytokines that trigger neurotoxic processes (similar to autoimmune ones). And their activity is also suppressed by neurotrophic factors. This is not a quick matter, and thus the long period of unfolding of the therapeutic effect of the antidepressant can be explained. Of course, this explanation is also lame, but it looks much more convincing. An interesting article was published in 2009 entitled “Why do antidepressants take such a long time to work? Cognitive neuropsychological model of the action of antidepressants. The authors of this article express the paradoxical idea that antidepressants do not affect a person's mood at all. Through the release of neurotrophins and the suppression of interleukins, antidepressants restore the normal functioning of the limbic system and the prefrontal cortex. (It is these parts of the brain that are responsible for the formation of emotions, the balance of positive and negative emotional responses, for assessments and evaluative distortions / errors, as well as for the correlation of emotional and cognitive processes.) Research data are given that changes were observed in patients with depression from the first days the first week, i.e. much earlier than the effect of treatment was clinically manifested and the background of mood was restored. Figure 5. Scheme of action of antidepressants. , It turns out that not raising the mood leads to a decrease in emotional distortions (as is drawn on top of ). Everything is just the opposite - this reduction in emotional-cognitive distortions entails the restoration of mood ( below ). Why is the cognitive neuropsychological theory expressed in the article good? It is fully consistent with the biological views of the neuroplastic model and with the psychotherapeutic approach, since it explains at what point psychology and the drug come together, and why psychotherapy works as well (if not better) than pharmacotherapy. There is, however, one slippery place, which the authors of the mentioned article quickly slip through. The fact is that there is no reason to think that our abstract verbal thinking is somehow able to influence the neuronal processes of deep-lying parts of the brain. Rather, there are reasons to think that no, thinking does not affect emotions. But let's leave that for future researchers. There is still no absolute and generally accepted answer to the question of how and why antidepressants work. The article was originally published on the author's personal blog. Part three, in which we continue to not understand a single thing, but not in the same way as we did not understand before, but in a different way, but then a diagram and a table appear in the narrative, which, as you know, calms down and increases the rating of trust in the text
 For example, the monoamine hypothesis postulates that a deficiency of certain neurotransmitters (primarily serotonin, but also noradrenaline and dopamine) is responsible for the characteristic mental disturbances in depression. nine0003
For example, the monoamine hypothesis postulates that a deficiency of certain neurotransmitters (primarily serotonin, but also noradrenaline and dopamine) is responsible for the characteristic mental disturbances in depression. nine0003  Through them, a huge number of drugs and drugs realize their effect. And all this could somehow be ignored, if not for the fact that serotonin is not particularly involved in the formation of mood at all. The main excitatory neurotransmitter in the human brain is the amino acid glutamate. The main inhibitor is γ-aminobutyric acid (GABA), which is obtained from the same glutamate. Serotonin, dopamine, norepinephrine and other hormones perform auxiliary modulating function.
Through them, a huge number of drugs and drugs realize their effect. And all this could somehow be ignored, if not for the fact that serotonin is not particularly involved in the formation of mood at all. The main excitatory neurotransmitter in the human brain is the amino acid glutamate. The main inhibitor is γ-aminobutyric acid (GABA), which is obtained from the same glutamate. Serotonin, dopamine, norepinephrine and other hormones perform auxiliary modulating function.
Theory Arguments for Arguments against Distribution of glutamate gear The level of glutamate and glutamine in the prefrontal cortex reduced
intravenous administration of ketamin (antagonist NMDA receptors) causes the antidepressant effect of the level of glutamate in the occipital core can be connected dopamine receptor Reduced GABA transmission Decreased GABA levels in plasma, cerebrospinal fluid, prefrontal and occipital cortex
Antidepressants interfere with GABA transmission GABA works at >30% of synapses in the brain, implying nonspecific action Circadian rhythm disorder Sleep deprivation and sleep light therapy have an antidepressant effect
Many patients with depression suffer from depression body temperature and neuroendocrine secretion Association between " clock genes" and depression is not detected Endogenous opioid dysfunction Agonists Δ-opioid receptors have an antidepressant effect on primates and increase the level of neurotrophin in the brain Large-scale studies confirming such a relationship as well as: Monoamine imbalance, citizenship and nervous exchange.  , violation of thyroxine functions, disruption of the work of some “circuits” of the brain, etc.
, violation of thyroxine functions, disruption of the work of some “circuits” of the brain, etc.  nine0003
nine0003 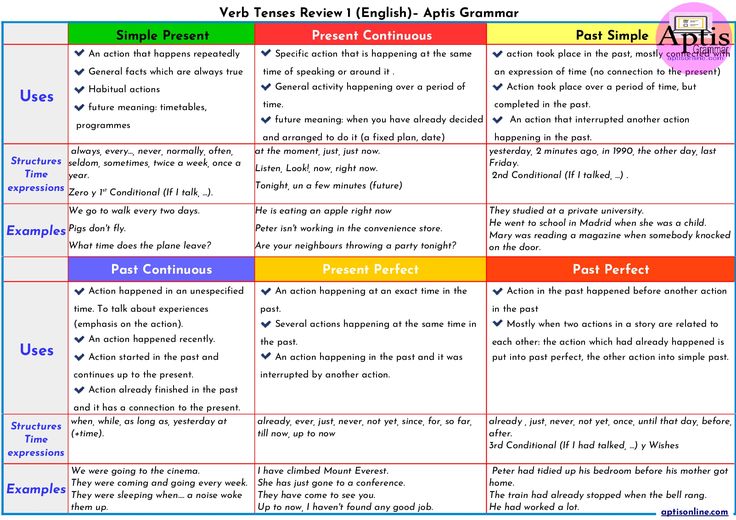 Serotonin is synthesized in them from tryptophan, and norepinephrine is synthesized from tyrosine with the participation of the corresponding hydroxylase enzymes. Both of these substances are stored in vesicles (vesicles) near the presynaptic membrane of the neuron, and when a signal arrives, they are secreted into the synaptic cleft. The normal interruption of the action of mediators in the gap between neurons occurs due to the reuptake of serotonin and norepinephrine by the corresponding transporter proteins, as well as through feedback (regulatory receptors that monitor the level of serotonin are involved here (receptors 5-HT 1A and 5-HT 1B ) or norepinephrine (α 2 -noradrenoreceptors)). In addition, monoamine oxidase A (MAO-A) works in the presynaptic neuron, which breaks down neurotransmitters and, consequently, regulates the number of synaptic vesicles.
Serotonin is synthesized in them from tryptophan, and norepinephrine is synthesized from tyrosine with the participation of the corresponding hydroxylase enzymes. Both of these substances are stored in vesicles (vesicles) near the presynaptic membrane of the neuron, and when a signal arrives, they are secreted into the synaptic cleft. The normal interruption of the action of mediators in the gap between neurons occurs due to the reuptake of serotonin and norepinephrine by the corresponding transporter proteins, as well as through feedback (regulatory receptors that monitor the level of serotonin are involved here (receptors 5-HT 1A and 5-HT 1B ) or norepinephrine (α 2 -noradrenoreceptors)). In addition, monoamine oxidase A (MAO-A) works in the presynaptic neuron, which breaks down neurotransmitters and, consequently, regulates the number of synaptic vesicles. 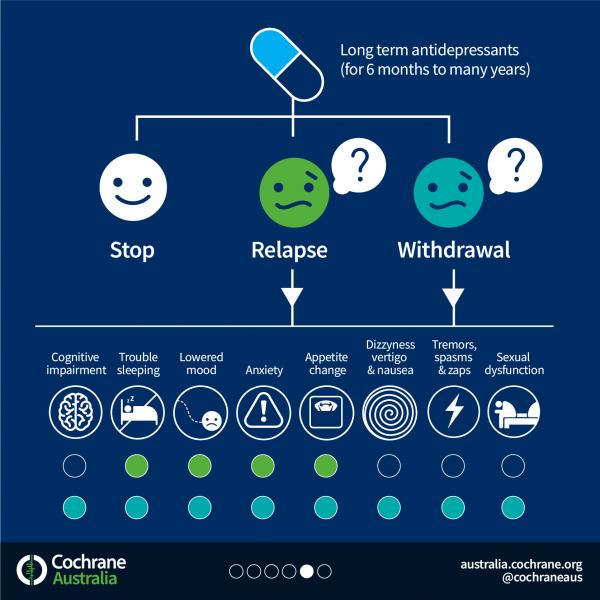 Both of these enzymes initiate signaling cascades involving cyclic adenosine monophosphate (cAMP) and inositol triphosphate (IF 3 ), respectively, multiplying the signal from the receptors and transmitting it to the cell nucleus.
Both of these enzymes initiate signaling cascades involving cyclic adenosine monophosphate (cAMP) and inositol triphosphate (IF 3 ), respectively, multiplying the signal from the receptors and transmitting it to the cell nucleus.  The subsequent cascade of signaling reactions, amplifying many times, reaches the cell nucleus, where it activates the transcription factor CEF (cAMP response element-binding, CREB). COE triggers the expression of genes responsible for the synthesis of neurotrophic factor, and the cell begins to produce BDNF, which then acts on its own TrkB receptor (type B tyrosine kinase receptor), which triggers the processes of synaptic plasticity, differentiation and resistance to damaging effects that we need so much. nine0003
The subsequent cascade of signaling reactions, amplifying many times, reaches the cell nucleus, where it activates the transcription factor CEF (cAMP response element-binding, CREB). COE triggers the expression of genes responsible for the synthesis of neurotrophic factor, and the cell begins to produce BDNF, which then acts on its own TrkB receptor (type B tyrosine kinase receptor), which triggers the processes of synaptic plasticity, differentiation and resistance to damaging effects that we need so much. nine0003 
Part four, in which the author supposed to tear off the covers and completely expose black magic, but it turned out as always
 At this “pre-clinical” stage, a change in activity on fMRI was already detected, patients achieved better results in a battery of tests for face recognition (where it is proposed to interpret different expressions - neutral / happy / unhappy), and they had a decrease in the frequency and magnitude of cognitive distortions (such as the tendency to to negative thinking). An improved understanding of the effect of antidepressants is shown in Figure 5.
At this “pre-clinical” stage, a change in activity on fMRI was already detected, patients achieved better results in a battery of tests for face recognition (where it is proposed to interpret different expressions - neutral / happy / unhappy), and they had a decrease in the frequency and magnitude of cognitive distortions (such as the tendency to to negative thinking). An improved understanding of the effect of antidepressants is shown in Figure 5.  It resolves the "paradox of two weeks" because, according to these views, antidepressants are exactly the same drugs as all the others, and they begin their action immediately, from the very first doses. This concept also explains why drugs help the sick and do not affect the healthy. These ideas give insight into why different patients show different and difficult to predict responses to the same drug, because mood improvement is a distant and by no means necessary side effect. nine0003
It resolves the "paradox of two weeks" because, according to these views, antidepressants are exactly the same drugs as all the others, and they begin their action immediately, from the very first doses. This concept also explains why drugs help the sick and do not affect the healthy. These ideas give insight into why different patients show different and difficult to predict responses to the same drug, because mood improvement is a distant and by no means necessary side effect. nine0003 Epilogue, in which, if someone does not understand, we will summarize that there will be no answer, because this problem has no solution
 And more importantly, why they often don't work. And why are the reactions so individual and, at first glance, drugs that are identical in mechanism may or may not work. We are constantly narrowing the circle, and every time the answer seems to be found, it slips away again. Today we know more than yesterday, and yesterday we knew more than the day before yesterday. And still, the final decision is still very far away. nine0003
And more importantly, why they often don't work. And why are the reactions so individual and, at first glance, drugs that are identical in mechanism may or may not work. We are constantly narrowing the circle, and every time the answer seems to be found, it slips away again. Today we know more than yesterday, and yesterday we knew more than the day before yesterday. And still, the final decision is still very far away. nine0003 Glossary
 nine0210
nine0210 
:max_bytes(150000):strip_icc()/prozac-withdrawal-symptoms-timeline-and-treatment-4766892_final_edit-ddf616fc766d4651afa6b5d804721eea.png) The classic representative is amphetamine.
The classic representative is amphetamine. 
 Pharmacology & Therapeutics . 117 , 30-51;
Pharmacology & Therapeutics . 117 , 30-51;  CNS Drugs . 24 , 1-7; nine0292
CNS Drugs . 24 , 1-7; nine0292 
Guide to antidepressants: how do they work?
Treatment
Depression of the Head of the States
Daniil Davydovspid. Center
13 July 2022
213802
AIDS Center
“AIDS Center” often writes about depression, and, unfortunately, for many of our readers, this is a habitable problem. This time, with the help of Maria Danina, Candidate of Psychological Sciences, our authors have compiled a short guide to antidepressants. Their types, principles of operation and device. All basic concepts in one text.
Depression is quite common: according to WHO, more than 300 million people of all ages and genders suffer from it worldwide. nine0003
As defined by the American Psychiatric Association, this serious condition can take many forms, vary in severity from person to person, and coexist with other conditions that cause similar symptoms, such as anxiety disorders.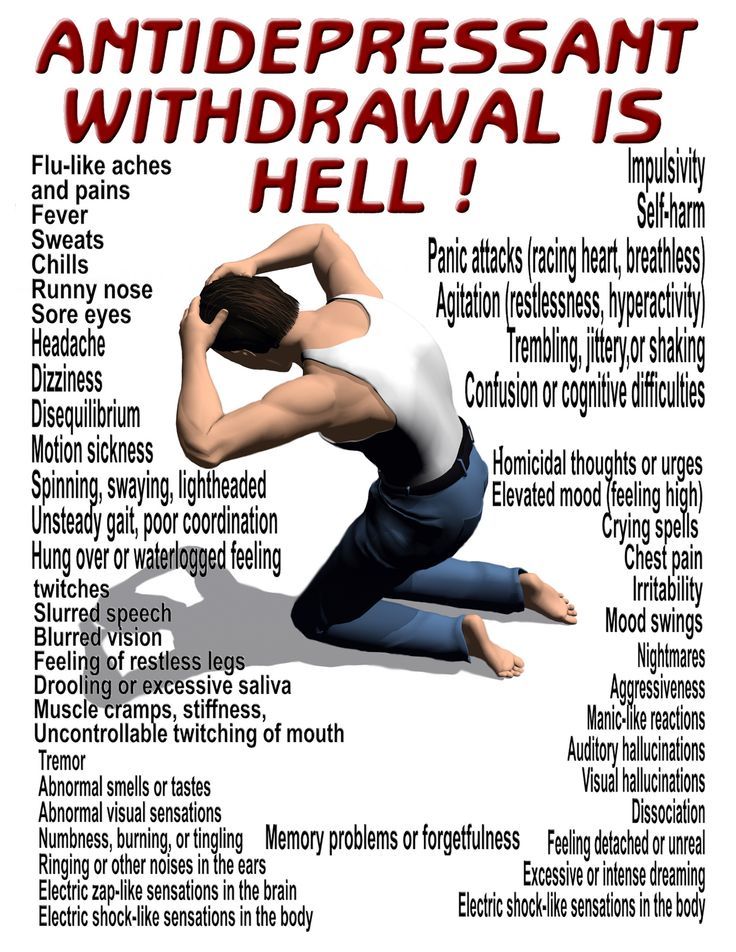
Since the causes of depression are related to disorders of the brain, it is useless to call on patients with depression to "pull themselves together" - its symptoms cannot be overcome by willpower, just as it is impossible to influence the brain by willpower. nine0003
“Mood is our subjective experience, that is, what we can become aware of and what we can give an account of. At the heart of any psychological phenomenon are complex and multi-level processes that take place in our nervous system. In particular, neurochemical ones,” explains Maria Danina, senior researcher at the Laboratory of the Scientific Foundations of Psychotherapy, Candidate of Psychological Sciences.
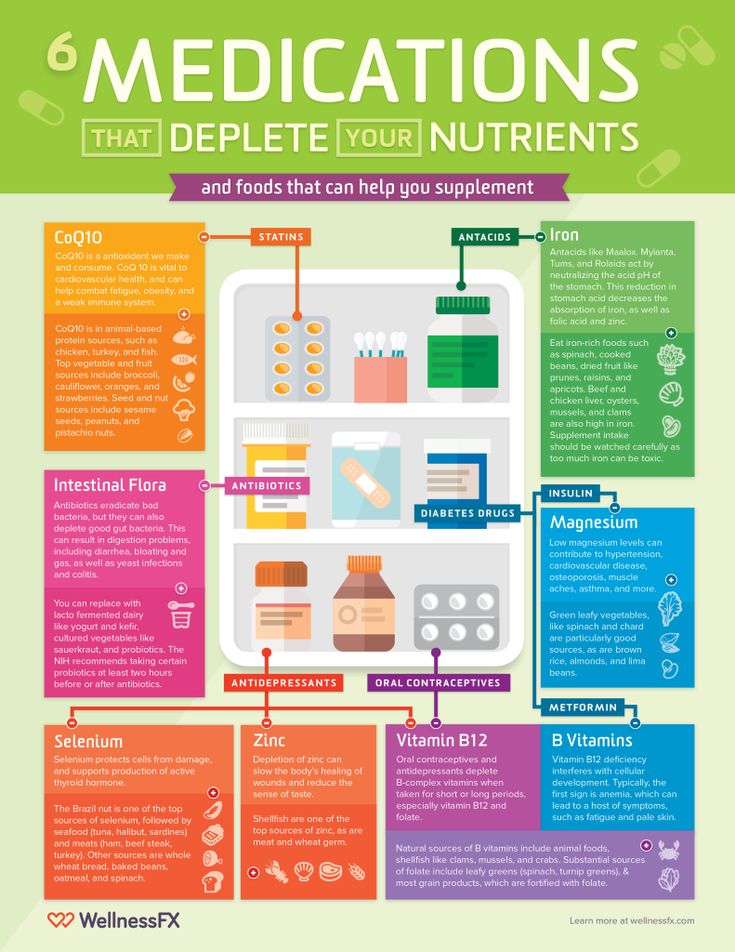
According to her, according to the monoamine theory, three different monoamine neurotransmitters contribute to depressive symptoms. Moreover, neurotransmitters do not "trigger" the disease by themselves, but affect certain processes, which, in fact, lead to depression. nine0003
First, it is dopamine, which is involved in the motivation system. A lack of dopamine can lead to anhedonia—that is, the inability to experience pleasure.
A lack of dopamine can lead to anhedonia—that is, the inability to experience pleasure.
Secondly, it is norepinephrine. It is involved in the regulation of our daily activities. Its deficiency is associated with psychomotor retardation (when a person begins to move and speak more slowly than usual).
And third, serotonin. Which is involved in the control of the sensitivity of the pain system, suppresses pain signals and negative emotions. nine0003
Lack of serotonin leads to increased pain, negative emotions and anxiety. In addition, due to a lack of serotonin, obsessive states develop, associated with constantly recurring thoughts about the past and the causes of one's current state, which are difficult to get rid of - psychiatrists call this rumination.
“In addition to lowering the level of neurotransmitters, other groups of biologically active substances, such as glucocorticoids, can contribute to depression,” says Maria Danina. - Let's say that the level of the famous "stress hormone" cortisol also increases with depression - and this in turn leads to a lack of dopamine. Monoamine levels can be affected by thyroid hormones and the sex hormones estrogen and progesterone.” nine0003
Monoamine levels can be affected by thyroid hormones and the sex hormones estrogen and progesterone.” nine0003
However, many factors can trigger clinical depression, such as hereditary predisposition, low self-esteem, difficult life circumstances, severe stress, and chronic diseases. And therefore, we cannot “shift all the blame” only on violations in the brain, emphasizes Maria Danina.
Neurotransmitters and their effects depending on deficiency or excessLife in the "serotonin pit"
An alternative to the monoamine theory, which, from the point of view of many scientists, can no longer be considered the main one, is the biopsychosocial model of depression. In accordance with it, the development of the disease is influenced not only by biological, but also by psychological factors. nine0003
“A person may experience loss (grief) or severe frustration of their needs (stress). As a result, his neurochemistry also changes,” explains Danina. “But this is the so-called normal “mourning process. ” Doctors talk about reactive depression only if, even after months, a person continues to experience all the same unpleasant sensations, and over time, his condition only worsens.
” Doctors talk about reactive depression only if, even after months, a person continues to experience all the same unpleasant sensations, and over time, his condition only worsens.
In some people, however, the functional characteristics of their neurons make them more prone to depression. Such patients "start" the process does not require external circumstances. And their depression has a non-reactive "endogenous" character. nine0003
In both cases, in addition to psychotherapy, doctors prescribe antidepressants, that is, drugs that can affect neurotransmitters in the brain, as medical help.
There are five classes in total. Each of which affects the brain in its own way.
1. Selective serotonin reuptake inhibitors (SSRIs).
SSRI drugs increase serotonin levels. This helps to more accurately regulate mood and gradually overcome moderate to severe depression. These drugs do their job by "forbidding" neurons to absorb serotonin from the synaptic gap between neurons. As a result, neurons are able to communicate better. nine0003
As a result, neurons are able to communicate better. nine0003
SSRIs have fewer side effects than other classes of antidepressants. For example, in case of an overdose, they do not disrupt cardiac conduction and do not lead to convulsions.
However, the side effects are still there and quite serious - from increased suicidal thoughts to sexual dysfunction, drowsiness, dry mouth, dizziness and headache.
In addition, all drugs that increase the level of serotonin in the brain can cause serotonin syndrome - a situation where the neurotransmitter becomes too much. nine0003 Serotonin and signal transmission through nerve cells.
In serotonin syndrome, the person becomes overexcited, restless, sweats and has an increased heart rate. That is why being treated simultaneously with two antidepressants that increase serotonin levels is dangerous to life and health.
2. Selective serotonin and norepinephrine reuptake inhibitors (SNRIs).
SNRIs work in much the same way as SSRIs, with one difference.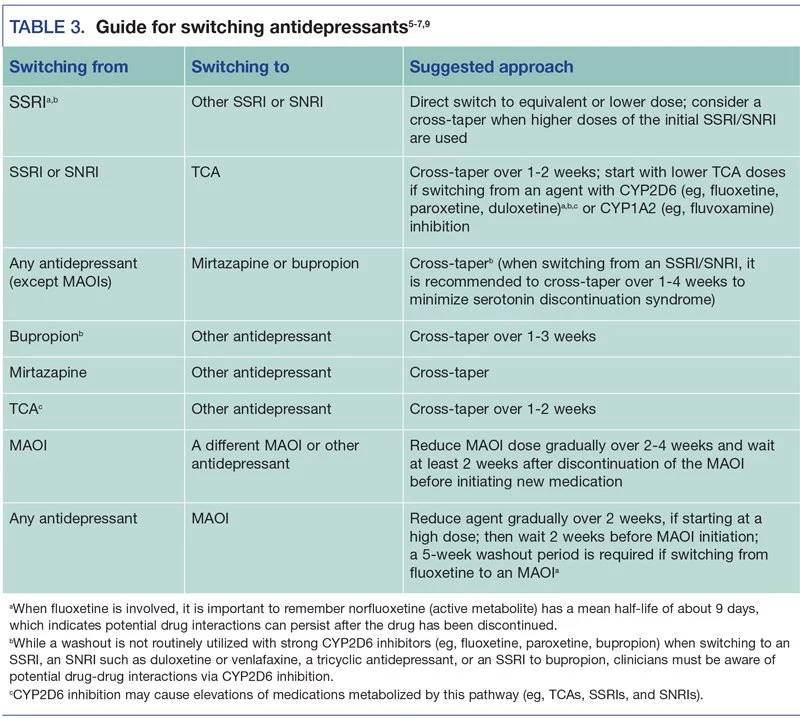 Drugs “forbid” neurons to absorb not only serotonin, but also norepinephrine, a neurotransmitter that is involved in the regulation of emotions and thought processes. nine0003
Drugs “forbid” neurons to absorb not only serotonin, but also norepinephrine, a neurotransmitter that is involved in the regulation of emotions and thought processes. nine0003
And since norepinephrine works closely with serotonin and dopamine, SNRIs are thought to increase attention, focus, and improve memory.
The indications and side effects of SNRIs are very similar to those of SSRIs. There are few advantages of this class of drugs over SSRIs, but for some patients they are better suited.
3. Atypical antidepressants.
This class includes drugs with different modes of action that have only one thing in common - these drugs are not like SSRIs and SNRIs. nine0003
Although some drugs in this class also "prohibit" neurons from taking up serotonin, like reuptake inhibitors, some of them can act on receptors for other neurotransmitters. This allows you to fine-tune the sensitivity of neurons to one or another substance.
It is worth noting that the components of some atypical antidepressants - say, bupropion - are listed in the note to the list of psychotropic substances subject to control in the Russian Federation. And although this tool is approved by reputable international medical organizations - for example, the US Food and Drug Administration (FDA), it cannot be legally purchased in Russia. nine0003
And although this tool is approved by reputable international medical organizations - for example, the US Food and Drug Administration (FDA), it cannot be legally purchased in Russia. nine0003
The side effects of this class of drugs depend on the specific drug. For example, some atypical antidepressants make you sleepy, while others, on the contrary, invigorate. To choose the right medicine, the doctor must take into account the peculiarities of the legislation, individual symptoms and the patient's health status.
4. Tricyclic antidepressants (TCAs).
All drugs in this class are thought to increase the levels of norepinephrine and serotonin in the brain, much like SNRIs do. nine0003
But TCAs have a very important difference - they are able to act on brain receptors that bind to other substances. In overdose, this leads to severe side effects, such as seizures and complete heart block. And although TCAs are quite effective, drugs from this group today are trying to use as little as possible.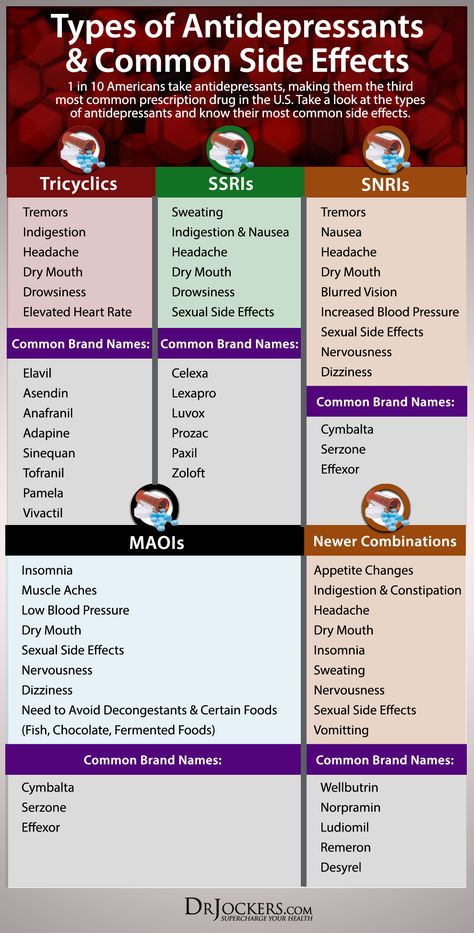
5. Monoamine oxidase inhibitors (MAOIs).
This class of drugs "turns off" monoamine oxidase, an enzyme that breaks down norepinephrine, serotonin, and dopamine in the brain. As a result, neurotransmitters are not destroyed and remain in the synaptic cleft for a long time. nine0003
Unfortunately, MAOIs have many side effects, including high blood pressure, weight gain, swelling, sexual dysfunction, and suicidal ideation. So today, drugs of this class are used only under strict medical supervision and as a last resort - if other antidepressants have not helped.
Is it possible to do without antidepressants?
In medicine, there is the concept of a balance of benefits and harms. This is exactly what the old medical saying about medicines says, which "cure one thing - cripple another." When deciding to prescribe an antidepressant (or any other powerful drug), the doctor always thinks about whether it will benefit a particular patient. nine0003
nine0003
related
Society
"You will burn in paradise!" Is depression really permanent?
- DepressionMedicineRussia
Of course, antidepressants are drugs with serious side effects, the abuse of which will not lead to anything good. However, this does not mean that the life of a person with depression without antidepressants will be any better.
What happens if you stop taking the antidepressants prescribed by your doctor? The biggest risk is the return of depression. Moreover, 80% of patients who abruptly stop taking antidepressants develop a withdrawal syndrome. This condition appears within a few days after discontinuation and can last up to two weeks. nine0003
From a medical point of view, it is not too dangerous, but the sensations can be quite unpleasant.
Withdrawal symptoms can be divided into four groups:
- gastrointestinal: nausea, vomiting, diarrhea and abdominal cramps;
- somatic: headaches, lethargy and sweating;
- sleep-related: insomnia or excessive sleepiness, nightmares;
- affective: restlessness, agitation and bad mood.
 nine0292
nine0292
To avoid withdrawal syndrome, the doctor should gradually reduce the dose of antidepressants. This may take several weeks or even several months.
Moreover, not only giving up antidepressants on your own, but also “prescribing” them to yourself without consulting a specialist is harmful.
“If you have symptoms of depression that do not go away for more than two weeks, this is an occasion to consult a psychiatrist. The sooner the better, because early treatment gives a better prognosis,” Maria Danina sums up. nine0003
Sometimes doctors have to try several different antidepressants to find the right one for you. But it will not be possible to do without a specialist: only during a personal examination, the doctor can confirm the diagnosis and prescribe treatment, she emphasizes.
Where to go for depression?
There are several exits here:
- neuropsychiatric dispensary at the place of residence (free of charge),
- psychiatric hospital (free of charge), nine0287 private clinic (extra charge),
- private doctor (for a fee).