Hallucinations before death
The Last Stages of Life
- Withdrawal from the External World
- Visions and Hallucinations
- Loss of Appetite
- Change in Bowel and Bladder Functions
- Confusion, Restlessness, and Agitation
- Changes in Breathing, Congestion in Lungs or Throat
- Change in Skin Temperature and Color
- Hospice Death
- Saying Goodbye
- Being Present at the Moment of Death
The last stages of life can be very stressful for the dying person and those caring for him/her. You will observe changes that may be upsetting and unfamiliar. Learning about the dying process will help. Many physical changes occur during the process of dying that affect the emotional, social, and spiritual aspects of a person’s life.
There are some signs and symptoms of dying that are observable, although not everyone follows a predictable sequence of events or stages.
Health professionals speak of “dying trajectories” that suggest how persons with specific diseases will die. For example, those with a terminal illness, such as advanced cancer, will show a steady decline toward death. Those with serious chronic illnesses may have peaks and valleys that sometimes give the impression of recovery.
Remember that each person’s death is unique.
It is helpful to understand the common symptoms experienced in people who are dying. You may observe none, some, or all of these symptoms in the dying erson’s last days and hours on earth. You will also learn things to do that can help ease physical pain and suffering.
As the end of life approaches, there is a feeling of detachment from the physical world and a loss of interest in things formerly found pleasurable. There is a tendency to sleep more. There is less desire to talk. This is the beginning of letting go of life and preparing for death.
Days or hours before death, the dying person becomes less and less responsive to voice and touch and may not awaken. Sometimes, quite unexpectedly, the person may appear well and even look as if he/she is going to recover.
Sometimes, quite unexpectedly, the person may appear well and even look as if he/she is going to recover.
The person may be alert and talkative. This does not mean that there will be recovery; the person is still dying. Use this as a “window of opportunity” to say what you need to say and have closure.
What you can do:- Always speak gently, and identify yourself before speaking.
- Use gentle touch and provide reassurance.
- Dying requires energy and focus. Try not to distract the dying person from this necessary preparation. Allow time for silence.
- Remember that you are supporting the person to “let go.”
Visual or auditory hallucinations are often part of the dying experience. The appearance of family members or loved ones who have died is common. These visions are considered normal. The dying may turn their focus to “another world” and talk to people or see things that others do not see. This can be unsettling, and loved ones may not know how to respond.
This can be unsettling, and loved ones may not know how to respond.
- Do not judge or be critical of what is happening. Just be as silent and supportive as possible.
- Refrain from discounting the experience and orienting the dying person to “reality.” This is their reality. Most often, these “visions” are reassuring, and they comfort the dying. Rarely do they upset the dying person.
- It is important to differentiate visions from hallucinations or “bad dreams” that may be caused by medications or metabolic changes. While visions of loved ones are generally comforting, “bad dreams” may frighten the dying person. Alert the doctor or nurse about “bad dreams.” An adjustment in medication may correct this.
As death nears, the dying person may lose interest in food and drink. The ability to swallow becomes impaired. Loss of appetite and reduced intake are normal parts of dying. In the early stages of dying, the dying person may prefer only soft foods and liquids.
In the early stages of dying, the dying person may prefer only soft foods and liquids.
In the very last stages of life, however, they may not want any food or drink. A dying person may want to suck on ice chips or take a small amount of liquid, just to wet and freshen the mouth, which can become very dry. In the last stages of dying, forcing food when the body says “no” may be harmful or painful to the dying person. Many dying persons will exhibit the “clenched jaw” sign as a way of saying “no.” Forcing fluid may cause choking, or the dying person may draw liquid into the lungs, making matters worse.
It is hard for most people to respect the dying person’s lack of appetite. That’s because many of us equate food
with caring. Family members may feel that withholding nutrition is cruel or neglectful. They may worry that they
are “killing” their loved one.
It is important to remember that as the physical body is dying, the vital organs are shutting down, and nourishment is no longer required to keep them functioning. This is the wisdom of dying, and the body knows exactly what to do.
This is the wisdom of dying, and the body knows exactly what to do.
- Refrain from giving liquids or food unless requested.
- Wet the lips and mouth with a small amount of
- water, ice chips, or a sponge-tipped applicator
- dipped in water.
- Protect lips from dryness with a protective lip balm.
- Continue to be a caring and loving presence.
Now, I have no choice but to see with your eyes,
so I am not alone, so you are not alone.
–Yannis Ritsos
Change in Bowel and Bladder Functions
The two major concerns are constipation and incontinence (loss of control over bowel and bladder functions). Constipation may be caused by lack of mobility, pain medication, and decreased fluid intake. If left untreated, fecal impaction may occur and can become uncomfortable. Laxatives are generally needed to keep the bowels clean.
Incontinence, or loss of bowel/bladder control, is likely to be distressing to the dying person and those in attendance. In the early stages, “accidents” can occur. As death nears, the muscles in these areas relax further and contents are released. This is normal. Urine is highly concentrated and sparse and may look tea-colored.
In the early stages, “accidents” can occur. As death nears, the muscles in these areas relax further and contents are released. This is normal. Urine is highly concentrated and sparse and may look tea-colored.
Sometimes a urinary catheter is inserted, or the dying person may wear “diapers” or briefs. This will help keep linen clean (changing linen may be more disturbing to the dying person than the catheter or the diapers).
What you can do:- Keep affected areas clean and dry to avoid rashes or bedsores.
- Watch for signs of constipation and incontinence, and help loved ones report this to the physician or nurse.
- Talk to the doctor or nurse about the advantages of reducing food and fluid in the last stages of dying.
Restlessness and agitation are common. These symptoms may be caused by reduced oxygen to the brain, metabolic changes, dehydration, and pain medications.![]()
“Terminal delirium” is a condition that may be seen when the person is very close to death, marked by extreme restlessness and agitation. Although it may look distressing, this condition is not considered to be painful.
There are medications available to control symptoms. Be aware there may be unfinished business. Dying persons may try to hold on until they feel a sense of security and completion. Picking, pulling, and fidgeting behaviors may also be seen. This can result from medications, metabolic changes, or decreased oxygen to the brain.
What you can do:- Never startle the dying with bright lights, harsh tones, or abrupt movement.
- Always identify yourself. Even if the dying person
- knows you well, he/she might not recognize you at
- this time.
- Use a gentle voice and reassuring touch.
- With mindful awareness, be sensitive to any cues that might signal that there is something the person wants to resolve before he/she can let go.
 Offer support.
Offer support. - Consider the use of light massage and soothing music.
- Ask the doctor if there are any medications that might help relieve the agitation.
You may observe that breathing is shallow and quickened, or slow and labored. The person may make gurgling sounds, sometimes referred to as the “death rattle.” These sounds are due to the pooling of secretions and an inability to cough them up. The air passing through the mucus causes this sound.
The breathing pattern most disturbing to witnesses, called Cheyne-Stokes breathing, is marked by periods of no breathing at all (up to 45 seconds), followed by deeper and more frequent respirations. These respirations are common and result from decreased oxygen supply to the vital organs and a build-up of waste products in the body.
This condition is not uncomfortable or painful for the dying person, although it may be unsettling to observe. The “death rattle” or Cheyne-Stokes breathing indicate that death is near.
The “death rattle” or Cheyne-Stokes breathing indicate that death is near.
- Do not panic. This can increase any fear that may already be present for the dying person.
- Raise the head of the bed (mechanically or with pillows) to help breathing.
- If secretions are pooling in the mouth, turn the head and position the body so that gravity can drain them. Suctioning rarely helps and is not recommended.
- If appropriate, wipe out the mouth with a soft, moist cloth to cleanse excess secretions.
- Speak gently and lovingly, and use gentle reassuring
- touch to ease fear.
- Alert the doctor or nurse if breathing is especially labored or if you notice the “death rattle” and Cheyne-Stokes breathing.
As the body dies, the blood moves away from the extremities toward the vital organs. You may notice that while the extremities are cool, the abdomen is warm. You may notice changes in body temperature.
You may notice changes in body temperature.
The dying person may feel hot one minute and cold the next. As death approaches, there may be high fever. You also may see purplish-bluish blotches and mottling on the legs, arms or on the underside of the body where blood may be collecting. As death nears, the body may appear yellowish or waxen in color.
What you can do:- Try to keep the person as comfortable as possible.
- Use a damp, cool washcloth to cool a person who feels too hot (be alert to signs such as kicking off the blankets).
- Cover the dying person with a blanket if he/she feels too cold. Don’t use electric blankets or heating pads, as these may burn the skin.
- Alert the doctor or nurse if you notice changes in skin color. This may be a sign that death is near.
- Using a fan to circulate air may make the person more comfortable.
You can be a caring presence throughout the dying process. Your presence for the dying person and his/her loved ones indicates loving kindness, compassion, and
Your presence for the dying person and his/her loved ones indicates loving kindness, compassion, and
willingness to provide practical help.
Learn. Learn what you can about the dying person’s illness and the dying process so you can provide comfort and assurance.
Realize your limitations. No one is perfect. No one can do everything. Get help when you need it. Take a break when you need one. Encourage the dying person and his/her loved ones to call the doctor or nurse with questions.
Managing Physical PainMost physical pain can be controlled. No one should die in pain when the means to relieve it are available. All persons have the right to have their pain controlled.
Pain is real. Always believe a person who says he/she has pain. Remember that each person is an individual and perceptions of pain differ.
Talking to the doctor. People should expect their doctors and nurses to ask these questions about pain:
- Do you have pain?
- Where is it? What does it feel like: dull, stabbing, throbbing, etc.
 ?
? - How intense is the pain? Please rate it on a scale from 0 to 10, with 10 being the worst pain you’ve ever had.
- What makes the pain better or worse? The answers to these questions will help the doctor prescribe the right medicine in the right amount. Before the conversation is over, make sure that the dying person and his/her caregivers understand:
- What may be causing the pain
- The recommended treatment
- The possible side effects
- What to do if there are questions or concerns
True love is not a feeling by which we are overwhelmed.
It is a committed, thoughtful decision.
– M. Scott Peck
Hospice Death
Hospice care can be given in the home, nursing home, hospital, or residential facility. There are 7 hospice programs in Hawaii. Hospice care is available on every island except Niihau and Lanai. On Oahu, there are 3 dedicated hospice facilities, two affiliated with St. Francis Hospice (The Sister Maureen Kelleher Center and the Maurice J. Sullivan Family Hospice Center), and the Hospice Hawaii Kailua home. Several hospitals across the state work with local hospices to provide hospice carein the hospital. In the hospice philosophy, death is held as a natural event, not a medical event. “Care” not “cure” is the goal.
Francis Hospice (The Sister Maureen Kelleher Center and the Maurice J. Sullivan Family Hospice Center), and the Hospice Hawaii Kailua home. Several hospitals across the state work with local hospices to provide hospice carein the hospital. In the hospice philosophy, death is held as a natural event, not a medical event. “Care” not “cure” is the goal.
When hospice is provided in the home, family members become the primary caregivers. When possible, at least two family members or loved ones should share the responsibilities of caregiving. Hospice staff visit the home on a regular schedule. They are on-call (available round-the-clock) to provide support to the entire family. The hospice interdisciplinary staff includes doctors, registered nurses, social workers, chaplains, home health aides, and volunteers so that the dying may receive holistic, comprehensive care. Hospice nurses and doctors specialize in easing pain and suffering.
Physical and occupational therapists also can assist patients to be as mobile and self-sufficient as possible.
Music therapy, art therapy, counseling, and other therapies are also available. Hospice believes that emotional and spiritual pain are just as real. Counselors, including clergy, are available to assist family members as well as patients.
You can give your whole attention only when you care,
which means that you really love.
– J. Krishnamurti
Saying Goodbye
Persons who are dying often want “permission to die” from those they love. Often, they want to be assured of five things:
- Things they were once responsible for will be taken care of.
- The survivors will survive without them.
- All is forgiven.
- Their life had meaning.
- They will be remembered.
Saying good-bye is not easy. Yet, it is important for the dying person and his/her loved ones to do so. Take advantage of opportunities when the person is awake and communicative to facilitate the “saying good-bye” process.
If the dying person is not lucid, or in a coma, remember that hearing is the last sense to leave. Assume everything you say can be heard and understood, even if the person is not responsive. Never speak about the dying person as if he/she was not in the room.
Some people feel comfortable lying in bed next to their
loved one as they say their parting words. Others may want to simply hold hands. If music, chanting, or prayer is used to assist the dying, let it be comforting and familiar,
making way for gentle passage. The dying person’s
b ody language will let you know if these sounds are welcome and soothing.
Even with all the preparation and knowledge that death is coming, the moment of death is not easy to see. Even those people who are closest to the dying person may choose to be absent. The decision to be present at the moment of death depends on many things. Do not judge others if they choose not to be present at the moment of death.
Being Present at the Moment of DeathIt is not uncommon for the dying person to wait to die until loved ones have left the room.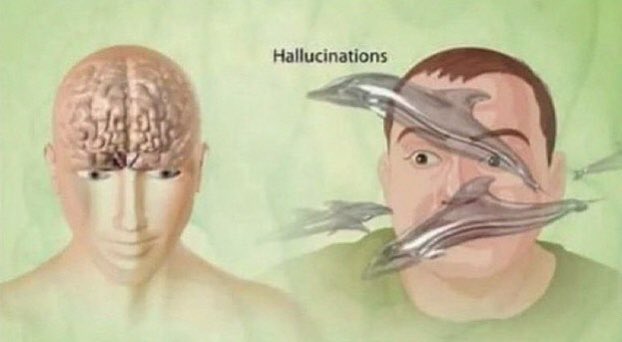 Make sure you allow for this. Sometimes, if a person seems to be holding on, you may simply say, “I’m going to leave the room for awhile. I love you.”
Make sure you allow for this. Sometimes, if a person seems to be holding on, you may simply say, “I’m going to leave the room for awhile. I love you.”
In some cultures, specific prayers, sutras, or other rituals, may ease the passage to death. These may be comforting both to the dying person and to his/her family. Ask your clergy person for assistance.
Work of sight is done.
Now do heart work on the pictures within you.
–Rainer Maria Rilke
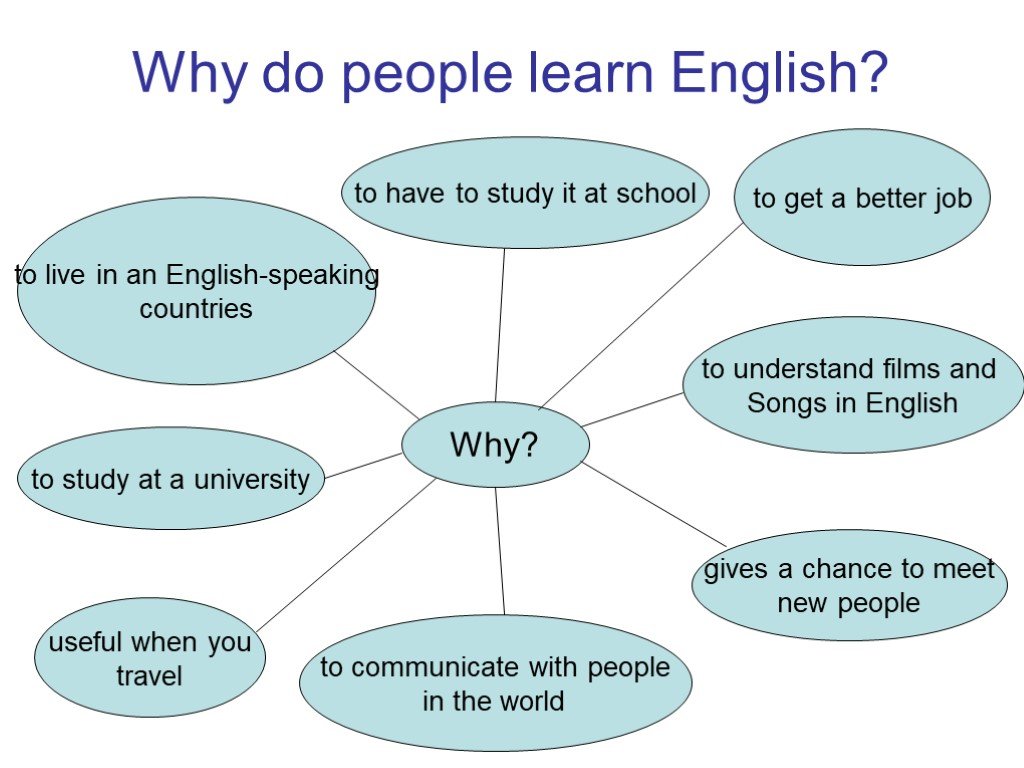
Understanding End-of-Life Visions
Posted on Wednesday July 19, 2017 in Caregiving Tips
When reading about signs and symptoms of end of life, there are many clinical descriptions: changes in breathing, mottling, decreased intake of fluid and food. One sign often stands out as being decidedly not clinical: visions before death. Yet, if you ask anyone working in end-of-life care about this, they’ll assure you that it is a common occurrence.
One sign often stands out as being decidedly not clinical: visions before death. Yet, if you ask anyone working in end-of-life care about this, they’ll assure you that it is a common occurrence.
Experiencing end-of-life visions.
“I’ve been with many patients who see loved ones,” Crossroads Hospice & Palliative Care Chaplain Ann O’Shea shares. “Recently, a patient sat up and said ‘hello’ to someone I couldn’t see and began talking to them.”
Many nurses, hospice aides, and family caregivers providing end-of-life care to patients and family members share similar experiences of visions before death.
“Sometimes patients don’t see a loved one, but they say they see spirits they don’t know popping in to visit. Sometimes, it is many people. They’ll say the room is crowded,” Crossroads Nurse Carolyn Quach-Huynh adds. “It’s also not always a vision. It can be a deceased spouse or parent appearing in dreams. Or a familiar smell – like cigars or a certain perfume.”
It can be a deceased spouse or parent appearing in dreams. Or a familiar smell – like cigars or a certain perfume.”
The terminally ill patient may also share that they are getting ready to go on a journey or that they recently visited places with a deceased parent or spouse.
All of these situations are very common, not just in the final hours of person’s life, but often in the days and weeks leading up to it.
What to do if your loved one is experiencing visions at end of life.
These visions are not hallucinations or a reaction to medication. The most important thing to do if your loved one is seeing visions or having visitation dreams is to acknowledge and support them. Do not argue with your loved one about the experience, correct them, or try to explain the vision. Do not panic as that can upset your loved one. Instead, take them at their word and encourage them to share the experience with you.
“As a caregiver, it is not our job to prove, disprove, or do experiments,” says Carolyn. “We are there to provide support and comfort.
“We are there to provide support and comfort.
In most cases, these end-of-life visions are indeed a source of great comfort to the person experiencing them.
If this is not the case and your loved one is becoming agitated by the visions or nightmares, talk through what the source of their fear is. Are they afraid of dying? Are they afraid of the person in the vision because of past bad acts? Let your hospice care team know about your loved one’s agitation. Chaplains and other trained hospice staff can help alleviate many concerns.
“This is the beauty of Crossroads Hospice & Palliative Care,” says Carolyn. “We are available to support families 24 hours a day, 7 days a week, and we can come out at any time if the patient or their family needs extra assistance.”
While it can be very hard to accept that the end is near for someone you love, these visions before death often signal to your loved one that their time has come. A vision of a parent or other loved one waiting for them can provide a feeling of peace about the experience, bringing comfort to both the patient and those around them.
A vision of a parent or other loved one waiting for them can provide a feeling of peace about the experience, bringing comfort to both the patient and those around them.
If you know someone who could use the support of hospice or has been diagnosed with six months or less to live, please call us a 1-888-564-3405 to arrange for a hospice evaluation.
Recommended Reading:
A Guide to Understanding End-of-Life Signs & Symptoms
Is Dying Easier for the Faithful?
After Death: What Happens Next?
If you found this information helpful, please share it with your network and community.
Copyright © 2017 Crossroads Hospice & Palliative Care. All rights reserved.
The nature of the dying visions established? - BBC News Russian service
Sign up for our 'Context' newsletter: it will help you understand the events.
Patients sometimes report seeing themselves during near-death experiences from outside
New research is shedding light on the nature of a mysterious phenomenon known from the stories of near-death survivors.
Scientists from Slovenia examined 52 patients who were brought back to life after a heart attack.
Those 11 who had near-death visions had significantly higher levels of carbon dioxide in their blood than those who did not see anything.
From the recollections of "eyewitnesses" it is known that at the moment of clinical death, many observe approximately similar pictures.
Some see a bright light at the end of a long tunnel, while others see life flash before their eyes from the very moment of birth. Often people say that their soul was separated from the body, soared up to the ceiling and they watched what was happening as if from the side.
Some describe encounters with long-dead relatives or say they experienced a sense of unparalleled peace.
According to statistics, from 10 to 25% of patients who survived clinical death as a result of a heart attack experienced near-death visions.
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of story Podcast
There is still no exact scientific explanation for this phenomenon. Some scientists associate it with the action of drugs, others refer to religious prejudice.
Religion has nothing to do with it?
One of the most common theories is that dying people experience hallucinations caused by anoxia, or lack of oxygen, which in turn leads to the death of brain cells.
But researchers from the University of Maribor in Slovenia found no signs of anoxia in patients who had visions of death.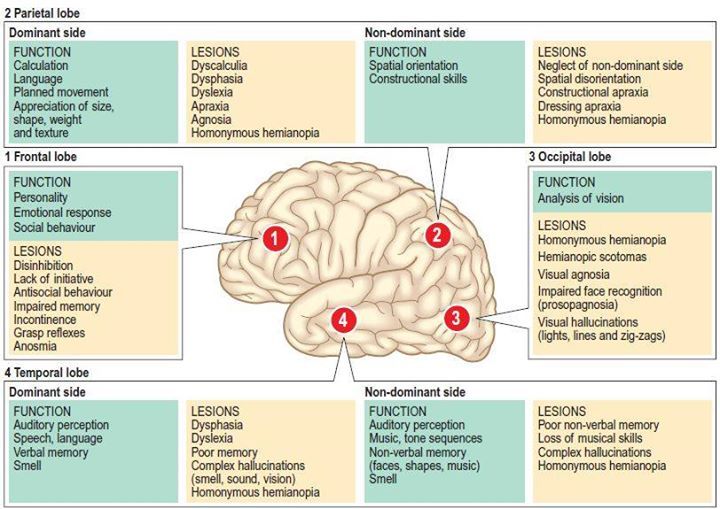
But the level of carbon dioxide in the blood of all these patients was elevated. It is known that inhalation of carbon dioxide often causes hallucinations similar to the descriptions.
However, it remains unclear whether the high level of carbon dioxide in the blood is a consequence of a heart attack or, on the contrary, its cause.
"We have a new mystery ahead of us, and further research is needed," says Zalika Clemens-Kethis, co-author of a scientific article in the medical journal Critical Care.
The well-known Dutch cardiologist Pim van Lommel, who has been studying the phenomenon of deathbed visions for a long time, called the studies of colleagues from Slovenia interesting.
"But they found only a connection, not a cause. I think that this topic will remain one of the greatest mysteries of mankind. The means that scientists have are clearly insufficient to explain the nature of this phenomenon," says Dr. van Lommel.
van Lommel.
British doctors are also trying to solve this riddle. In one of the experiments, scientists place various objects in the surgical ward that can only be seen from under the ceiling.
If near-death episodes with the separation of the soul from the body are true, and not a hallucination, then it is quite logical that, upon returning to life, patients will be able to indicate the location of these objects.
As part of the experiment, scientists are monitoring one and a half thousand patients, each of whom can see the light at the end of the tunnel at any time.
Before death, the whole life flashes before the eyes: scientists for the first time deciphered the activity of the brain of a dying person
Komsomolskaya Pravda
ScienceScience: Curious Club
Yaroslav KOROBATOV
February 24, 2022 7:00
Scientists saw in the brain activity of a dying person an attempt to reproduce memories
Scientists saw in the brain activity of a dying person an attempt to reproduce memories survived clinical death, describe their condition in approximately the same way. They talk about the feeling of flying or moving in a dark tunnel towards the light, they see themselves from the side (out of the body) and often use the phrase “the whole life flashed before my eyes”.
They talk about the feeling of flying or moving in a dark tunnel towards the light, they see themselves from the side (out of the body) and often use the phrase “the whole life flashed before my eyes”.
Scientists explain such visions as hallucinations that occur against the background of a lack of oxygen in the brain. Against the background of clinical death, the cerebral cortex is depressed, peripheral vision is lost and tunnel vision develops - only the central region of the retina works. This creates the illusion of a flash of light somewhere straight ahead. However, there are citizens who believe that surreal near-death experiences are proof of the existence of an afterlife.
One way or another, the phenomenon of strange sensations at the moment when the question of life and death is decided has not been well studied. When a person dies in the arms of doctors, they try to save him, and there is no time for experiments and research.
Recently, however, an unfortunate accident has brought unique scientific data to an international team of scientists. An 87-year-old man was admitted to the emergency room and hit his head hard on the floor in a fall. As a result, the patient developed an extensive hematoma and began to develop signs of epilepsy. Dr. Raul Vicente from the University of Tartu (Estonia) and colleagues used continuous electroencephalography (EEG) to diagnose and treat a seizure. During this recording, the patient had a heart attack and died. Thus, for the first time, records of 900 seconds (15 minutes) of brain activity of a dying person.
An 87-year-old man was admitted to the emergency room and hit his head hard on the floor in a fall. As a result, the patient developed an extensive hematoma and began to develop signs of epilepsy. Dr. Raul Vicente from the University of Tartu (Estonia) and colleagues used continuous electroencephalography (EEG) to diagnose and treat a seizure. During this recording, the patient had a heart attack and died. Thus, for the first time, records of 900 seconds (15 minutes) of brain activity of a dying person.
- We focused on studying what happened within 30 seconds before and 30 seconds after the man's heart stopped beating, - said one of the authors of the study, Dr. Ajmal Zemmar, neurosurgeon from the University of Louisville (USA). - And got very interesting results.
During this minute, the equipment recorded a change in the activity of brain neurons. In the general frequency of the electrical activity of the brain, several groups of rhythms are distinguished: Gamma, Beta, Alpha, Delta, and so on.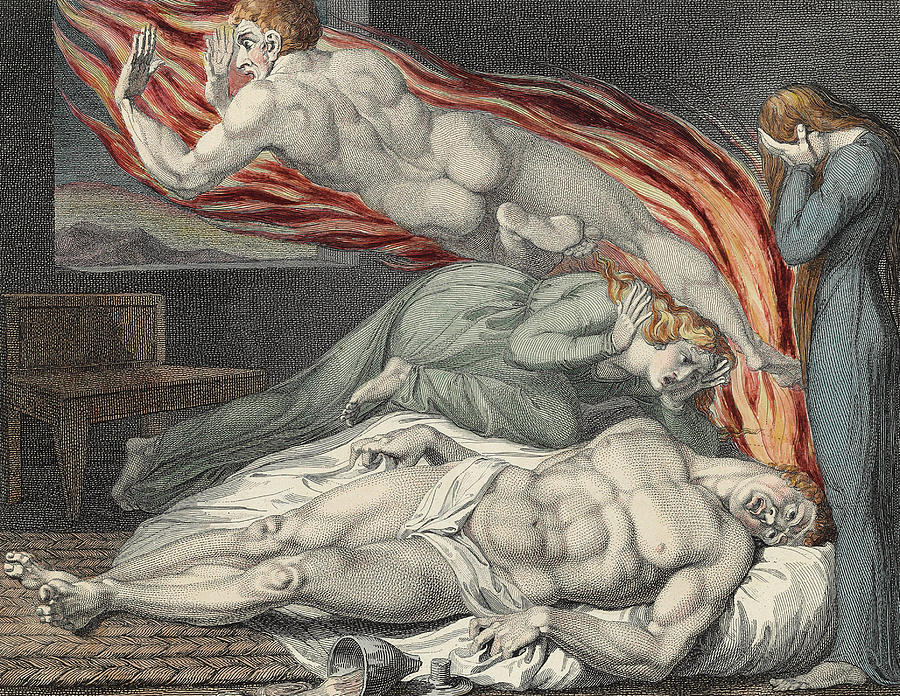 Each of them is associated with the solution of certain problems. For example, Alpha rhythms occur in a relaxed state of wakefulness and rest. If you close your eyes and try to relax, your brain will register Alpha rhythms. In turn, Gamma rhythms occur when you solve tasks that require maximum concentration. Different types of brain waves are involved in processes such as concentration, dreams, meditation, and memories. And by the "handwriting" of brain activity, you can determine what a person is currently doing.
Each of them is associated with the solution of certain problems. For example, Alpha rhythms occur in a relaxed state of wakefulness and rest. If you close your eyes and try to relax, your brain will register Alpha rhythms. In turn, Gamma rhythms occur when you solve tasks that require maximum concentration. Different types of brain waves are involved in processes such as concentration, dreams, meditation, and memories. And by the "handwriting" of brain activity, you can determine what a person is currently doing.
After cardiac arrest, against the background of suppression of neuron activity in both hemispheres, a surge in the absolute power of gamma rhythms was recorded. At the same time, a cross-relationship between alpha and gamma activity was observed. Such processes are typical for various types of intellectual activity, for example, for the reproduction of memories. Therefore, scientists have suggested that such activity may be associated with an attempt to scroll through the memory of key moments of life before death.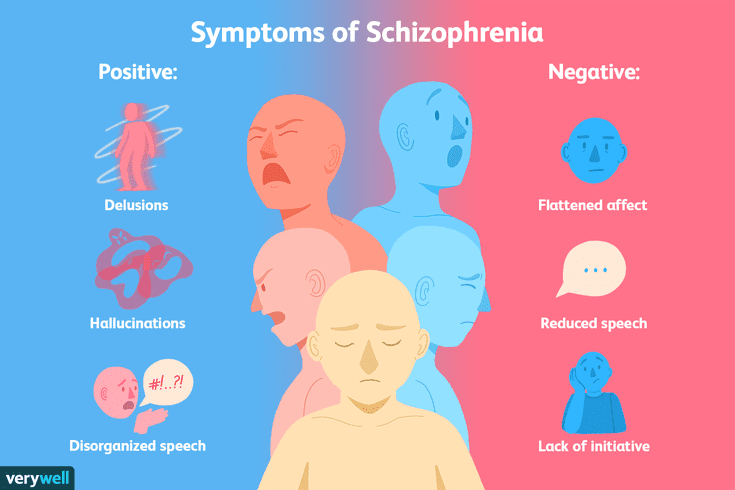 This pattern was observed from the time of cardiac arrest until the cessation of cerebral blood flow.
This pattern was observed from the time of cardiac arrest until the cessation of cerebral blood flow.
- The brain activity that we have studied may correspond to the sensations that patients report in near-death experiences, says Professor Zemmar. - It is likely that when the eyes of our loved ones are closed and they are ready to leave this world, their brain recalls memories of the best days of life. These findings challenge our understanding of exactly when life ends. And this, in turn, raises important questions, for example, related to the timing of organ donation (since a person is still aware of himself after death for some time - Ed).
The authors of the study mention that similar changes in brain activity were recorded in laboratory mice. At the same time, scientists clarify that it is too early to draw far-reaching conclusions, because the study describes the experience of only one patient who received a traumatic brain injury, suffered from epilepsy and was under the influence of a number of drugs.
Age category of the site 18+
Online publication (website) registered by Roskomnadzor, certificate El No. FS77-80505 dated March 15, 2021
CHIEF EDITOR OLESIA VYACHESLAVOVNA NOSOVA.
EDITOR-IN-CHIEF OF THE SITE - KANSK VICTOR FYODOROVICH.
THE AUTHOR OF THE MODERN VERSION OF THE EDITION IS SUNGORKIN VLADIMIR NIKOLAEVICH.
Messages and comments from site readers are posted without preliminary editing. The editors reserve the right to remove them from the site or edit them if the specified messages and comments are an abuse of freedom mass media or violation of other requirements of the law.
JSC "Publishing House "Komsomolskaya Pravda". TIN: 7714037217 PSRN: 1027739295781 127015, Moscow, Novodmitrovskaya d. 2B, Tel. +7 (495) 777-02-82.
Exclusive rights to materials posted on the website www.kp.ru, in accordance with the legislation of the Russian Federation for the Protection of the Results of Intellectual Activity belong to JSC Publishing House Komsomolskaya Pravda, and do not be used by others in any way form without the written permission of the copyright holder.