Depressed and cant sleep
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Why I wake up early and can't fall asleep: causes of insomnia in the morning | v1.ru
All newsThere is money for this: Volgograd officials and deputies will have their salaries increased by 8%
Not native Russian? 10 simplest words that everyone misspelled
Why does a man lose his strength and desire to have sex? It's all about one hormone
In the south of Volgograd in Arafatka: a teenager missing in Volzhsky was found
Kicked out of the house, but did not let her into the camp: the police took away her son from Volgograd with a congenital disease
“At first there were breakdowns and I persuaded myself to stay fat”: how a fitness trainer lost 50 kg without surgery and strict diets City»
It's not a sore throat: five non-obvious causes of a sore throat
No one is safe: a Volgograd woman complained to the People's Front about the denial of a survivor's pension to a disabled child
Developers in Sochi have found a gold mine. What is the city being turned into, which once had the title of All-Russian health resort
What is the city being turned into, which once had the title of All-Russian health resort
A glow and a roar: an unidentified military flying object that fell from the sky was blown up near Volgograd
The Ministry of Defense for the first time published footage with Putin at the headquarters of the special operation: NVO news for December 17
“The whole city is sick. What did you want”: Volgograd residents complain about the lack of antibiotics in pharmacies
“I don’t want to return to that body”: what a girl looks like after losing 200 kilos (before and after photos) exhibition dedicated to animals at the front
Thinner and blooming: Kabaeva appeared at the opening of the Academy of Gymnastics - the media noted that she had changed a lot
He worked for six years: a famous restaurant on the Alley of Heroes closed in Volgograd apartments
New Year's dress for three million: showing the most expensive holiday outfits
A traveler who disappeared without a trace was found near Volgograd
"It turned out she dated both of us. " The story of a guy whose first relationship turned into hell
" The story of a guy whose first relationship turned into hell
“We have been waiting for repairs for half a year”: since mid-December, Volgograd residents have been forced to walk along flooded streets
A video about the increase in the term of military service is circulating on the Web. It's true? We called the author of the application
You’ll break your head: 10 logical tasks that you can’t cope with
There was even a Christmas tree-Z: an exhibition of Christmas trees was held in Volgograd
The Ministry of Health named four signs that indicate a worsening of SARS
“This is how depression begins”: a Volgograd doctor spoke about the first sign of a dead immune system
What about garlic? Doctors explained what would happen if you eat lemons and garlic every day
Kota traveled around: near Volgograd, three people were injured after a collision with a tree
“Heavy luxury is in the past”: why Russian women are left without mink coats and are offered to wear green eco-fur coats
The EU imposed sanctions against a State Duma deputy and the ruins of a factory in Volgograd
They are not afraid of anyone and run for nuts: a Volgograd man discovered wild animals in the Komsomol garden
Volgograd City Hall demanded to collect dozens of signatures in order to open a memorial plaque to the hero who died in Ukraine
Will remote work be banned? How those who have gone abroad will be able to work
“Welcome back to a brighter future”: a peasant from Volgograd spoke about the return of the deficit0003
A window to Europe: now how to buy a new iPhone and Nike sneakers through parallel imports
I had to open the door: a rotten corpse of a man was found in Volgograd photo
All news
After a short rest, our brain begins to solve the problems that disturb us during the day, and we can no longer fall asleep
Photo: Artem Lents / NGS24.RU
Share
According to the somnologist Roman Buzunov, early awakenings at night with the impossibility of falling asleep again in more than half of the cases is the first symptom of a depressive state. Depression as such may not yet exist, but the first bell has already appeared.
Roman Buzunov — sleep medicine doctor, head of the Center for Sleep Medicine, Professor, Honored Doctor of the Russian Federation, MD.
— A person often says that he used to have problems falling asleep, but when he fell asleep, he slept until the morning. And then he began to paradoxically fall asleep better, but early awakenings appeared. This is a very typical situation for the development of an anxiety-depressive state. When anxiety first appears, stresses that interfere with sleep. And, if stress continues, a depressive component joins or depression generally develops. And she has a very specific symptom - early awakenings. In a person, 3–4 hours after falling asleep, the brain turns on and a complex thought process begins that cannot be stopped. And in the morning I wanted to sleep, but it's time to get up, - said Roman Buzunov in his telegram channel. nine0089
In a person, 3–4 hours after falling asleep, the brain turns on and a complex thought process begins that cannot be stopped. And in the morning I wanted to sleep, but it's time to get up, - said Roman Buzunov in his telegram channel. nine0089
If you begin to notice such sleep problems in yourself, the somnologist advises you not to hesitate and consult a specialist doctor. He will help to assess the cause of depression and prescribe the necessary treatment. In such cases, doctors use cognitive behavioral therapy, stress resilience techniques, and drug therapy, including antidepressants.
Tatyana Karavaeva, Head of the Department for the Treatment of Borderline Mental Disorders and Psychotherapy, NMRC them. Bekhterev. Endogenous depressions are associated with a chemical malfunction in the brain - because of it, the level of the main neurotransmitters in the body, more often serotonin, decreases. nine0089
According to the doctor, it is in the pre-morning hours that the level of serotonin in the body is lowest, and during depression it is below the usual minimum - such a decline just “throws you out” of sleep, wakes you up. Therefore, in people with endogenous depression, a lowered mood is more pronounced in the first half of the day - the level of serotonin begins to rise only by the middle of the day, and the person becomes a little easier.
Therefore, in people with endogenous depression, a lowered mood is more pronounced in the first half of the day - the level of serotonin begins to rise only by the middle of the day, and the person becomes a little easier.
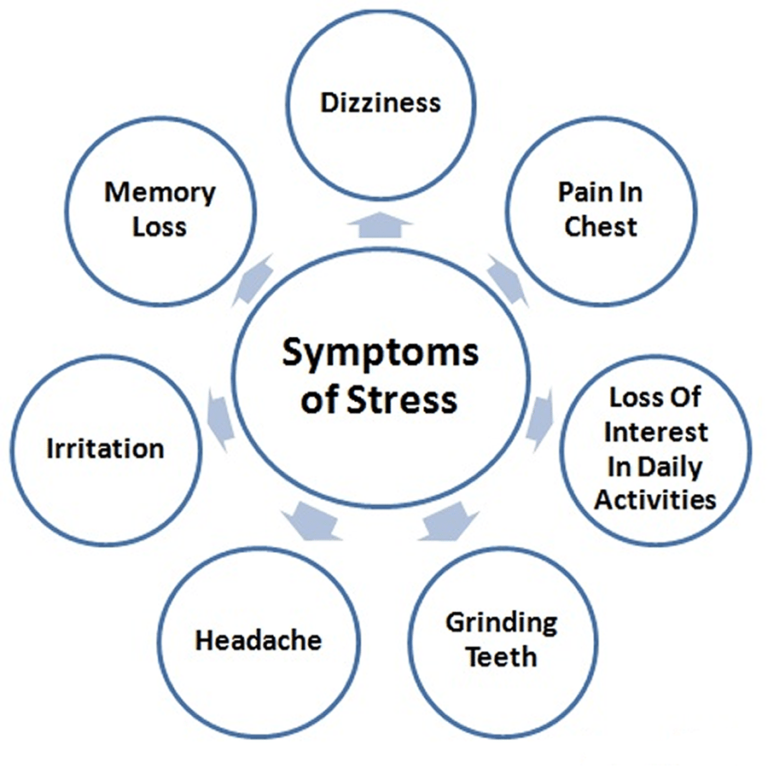
In addition to sleep disorders, the doctor mentioned other symptoms of classic depression:
- Decreased mood. According to the doctor, if a bad mood does not have a specific cause and it is reduced for two weeks, most days of the week and most of the day, this is an occasion to see a doctor as soon as possible.
- Difficulty thinking.
- Decreased activity, unwillingness to do anything - for example, getting out of bed in the morning, cooking, socializing.
- Change in appetite. It can both decrease and, conversely, increase.
- Change in body weight. Sometimes weight loss can be quite noticeable - up to 10-15 kg. nine0111
In addition to the onset of depression, there are other reasons for early awakenings. According to neurologist Elena Shenderova, banal reasons can wake you up in the middle of the night - physical or psycho-emotional overwork. Sleep problems and frequent awakenings are also possible with organic damage to the brain, with various somatic diseases - it is quite understandable that sleep will suffer if your knees hurt or your stomach twists.
According to neurologist Elena Shenderova, banal reasons can wake you up in the middle of the night - physical or psycho-emotional overwork. Sleep problems and frequent awakenings are also possible with organic damage to the brain, with various somatic diseases - it is quite understandable that sleep will suffer if your knees hurt or your stomach twists.
Anastasia Romanova
DepressionSomnologistSleepHealth
- LIKE3
- LAUGHTER0
- SURPRISE0
- ANGER0
- SAD0
See the typo? Select a fragment and press Ctrl+Enter
COMMENTS17
Read all comments
What can I do if I log in?
Media news2
Media news2
Treatment of insomnia with neurosis, depression, stress in St. Petersburg
- Home
- Neurology
- Treatment of sleep disorders
- Treatment of insomnia
- For neurosis
Insomnia is a symptomatic manifestation characterized by sleep disturbance or inability to fall asleep. There are many causes of insomnia, but they are divided into only 2 groups: physiological and psychological factors.
In order to prescribe the right treatment, our specialists first determine the true cause of the disorder. If a patient has insomnia against a background of neurosis, we begin to treat the underlying disease that caused the sleep disorder. Otherwise, the therapeutic effect will be ineffective: the eliminated symptoms will return again after a certain time. nine0003
nine0003
Insomnia in neurosis requires long-term complex treatment, in severe cases of manifestation of the disease - with the use of medications (hypnotics and sedatives). Tranquilizers can also be shown to the patient - when prescribing a remedy for insomnia, stress and depression to the patient, the doctor takes into account the clinical picture of the disease and the characteristics of the patient's body.
It is worth noting that in some cases, treatment can be carried out without the use of drugs, but with the help of psychotherapeutic influence, both group and individual. nine0003
At the same time, the main task of psychotherapy is to change the patients' perception of the environment, which helps to weaken the influence of traumatic factors on them. In the case of observation of insomnia in a patient with neurosis, therapy includes the patient's compliance with sleep hygiene.
Causes of insomnia in neurosis, depression, stress
The psychological causes of insomnia include the following:
- Stress associated with the patient's professional activities, difficulties within the family and domestic conflicts.
 Under their influence, the patient's nervous system works inefficiently, resulting in insomnia due to stress; nine0111
Under their influence, the patient's nervous system works inefficiently, resulting in insomnia due to stress; nine0111 - Psychotrauma. As practice shows, insomnia, depression, neurosis go away on their own when a person accepts a problem;
- Strong mental experiences accompanying the loss of loved ones. Of the non-drug methods of therapy in this case, only time and the support of loved ones help. Often, insomnia after stress is treated with antidepressants prescribed strictly by a specialist;
- Personality traits. In the risk group, patients are prone to anxiety - unreasonable fear. Anxiety before the next day negatively affects the psycho-emotional state of the patient, causing sleep disorders. nine0111
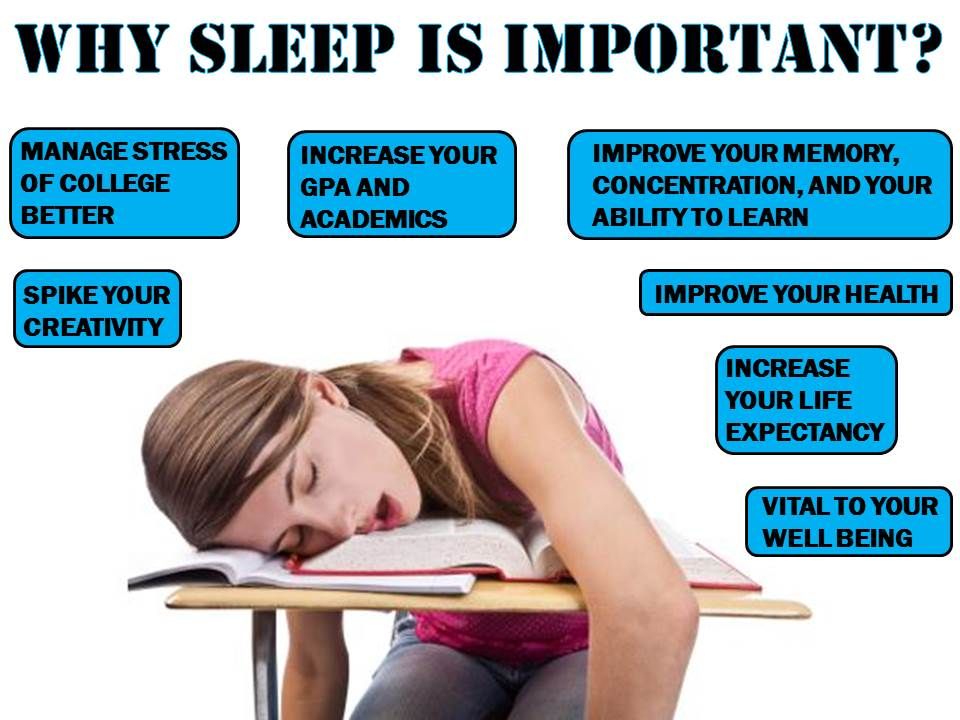
Symptoms of insomnia
You can easily recognize insomnia by the appearance of a person. Insomnia is characterized by redness of the eyes, pallor of the skin, the appearance of bags under the eyes, dry lips. A person suffering from insomnia shows lethargy, depression, and in some cases apathy.
The main symptoms of the disease are as follows:
- Difficulty falling asleep, lasting up to several hours;
- Partial or complete lack of sleep at night; nine0111
- Light sleep, which does not give the body and psyche a good rest;
- Interrupted sleep or early awakening, after which it is impossible to fall asleep again.
Remember that frequent lack of sleep is dangerous for the body. Insomnia during depression causes malfunctions of the central nervous system, which is accompanied by irritability, decreased performance. With persistent sleep disturbances, there is a risk of premature death.
Insomnia associated with various types of depression
There are several types of depressive conditions characterized by sleep disorders:
- Endogenous depression. In this case, falling asleep is normal, but there are sharp nocturnal awakenings, and further attempts to fall asleep remain fruitless. Upon awakening, there are often bouts of anxiety, fear, hopelessness, which do not allow you to fall asleep again.
 A state of drowsiness may occur, but it does not give a good rest. In the morning the patient experiences a bad mood, heaviness in the head. nine0111
A state of drowsiness may occur, but it does not give a good rest. In the morning the patient experiences a bad mood, heaviness in the head. nine0111 - Latent depression (masked). With it, early awakenings occur, sleep is often interrupted, the patient feels tired and exhausted.
- Seasonal depression. The patient often experiences bouts of weakness and drowsiness in the morning and afternoon hours, sleep at night is normal, but does not bring rest.
- Sad depression. It is characterized by a feeling of fatigue and a breakdown that occurs towards the end of the day. The patient's sleep becomes sensitive, during which a person cannot fully relax. Usually there are early awakenings, but the person cannot find the strength to get out of bed, and continues to lie until the sound of the alarm clock. nine0111
Fatigue and lethargy do not go away even after getting up, they can often be accompanied by headaches. During sleep, the patient often sees painful, monotonous dreams of a gloomy nature, usually associated with his problems and defeats.
- Apathetic depression. In this case, the patient's sleep differs in duration - the rise occurs much later than usual, but during the day the person is overcome by drowsiness and a feeling of severe fatigue. The patient may not get out of bed all day because of a breakdown. Dreams occur rarely, they are faded and not emotional, but often the patient can lose the border between dreams and reality. nine0111
- Anxious depression. It is accompanied by the appearance of disturbing thoughts, often preventing sleep. Sleep is mostly intermittent, with a negative emotional coloring, nightmares are possible.
Diagnosis of insomnia
Comprehensive examination of the patient helps our specialists to reliably determine the cause of insomnia. It includes examination of the patient by the doctors of the clinic, questioning, history taking, laboratory and instrumental examinations. Our patients are usually assigned the following types of examinations:
- Magnetic resonance imaging;
- Ultrasonic examination;
- Electrocardiography;
- Laboratory tests.

Treatment of insomnia in depression in the clinic Dr. SAN
Before starting the treatment of insomnia in neurosis, the doctors of the clinic conduct a thorough comprehensive examination of the patient. Based on the indications, specialists establish the necessary type of therapeutic effect, taking into account the characteristics of the patient's body, the mechanism of the development of the disease and the reasons why insomnia, stress, and depression developed. In some cases, patients are prescribed psychotherapeutic sessions or treatment of insomnia neurosis with hypnosis. In extreme cases, the treatment of insomnia in depression requires the appointment of a number of medications by a specialist. nine0003
If there is a suspicion of damage to the patient's internal organs caused by overwork and lack of quality sleep, the patient is assigned an additional examination, with the involvement of specialized specialists: an endocrinologist, a therapist, a neurologist-epileptologist.